Blood pressure 1 Regulation of blood flow Local
Blood pressure 1
Regulation of blood flow • Local regulation – Adjustment of blood flow by the tissue • Nervous system – Global implication • Redistribution of blood flow • Increase/decrease in heart activity (pumping) • Rapid control of arterial pressure
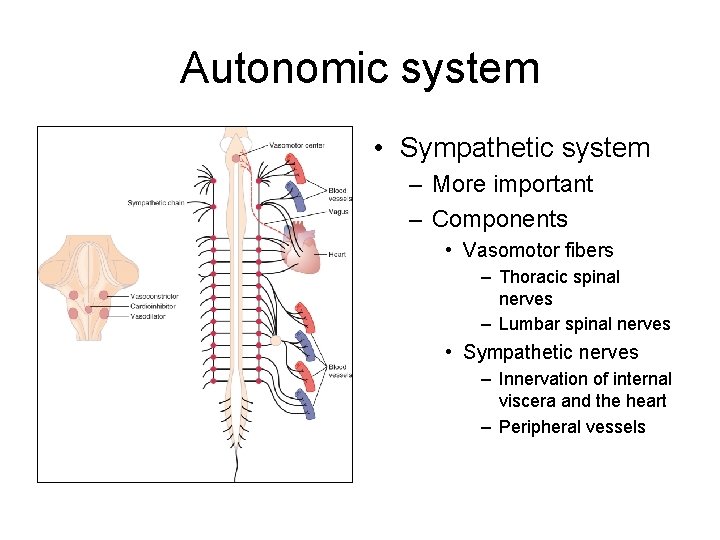
Autonomic system • Sympathetic system – More important – Components • Vasomotor fibers – Thoracic spinal nerves – Lumbar spinal nerves • Sympathetic nerves – Innervation of internal viscera and the heart – Peripheral vessels
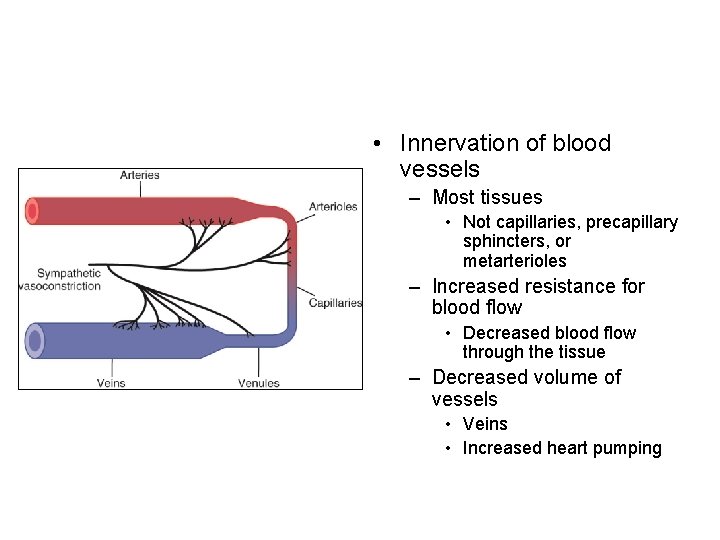
• Innervation of blood vessels – Most tissues • Not capillaries, precapillary sphincters, or metarterioles – Increased resistance for blood flow • Decreased blood flow through the tissue – Decreased volume of vessels • Veins • Increased heart pumping
• Innervation of heart – Sympathetic • Increased heart rate • Increased strength • Increased volume of pumping – Parasympathetic (vagus) • Decreased heart rate
Vasoconstriction • Sympathetic nerve fibers – Vasoconstrictor nerve fibers • Very small number of vasodilators • Wide distribution – Tissue-dependent • More powerful in some organs – Kidney, GI tract, spleen, and skin
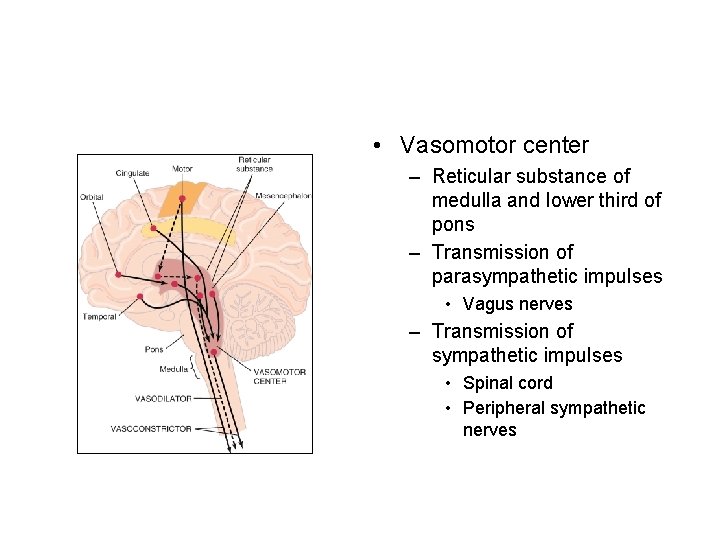
• Vasomotor center – Reticular substance of medulla and lower third of pons – Transmission of parasympathetic impulses • Vagus nerves – Transmission of sympathetic impulses • Spinal cord • Peripheral sympathetic nerves
• Area of vasomotor center – Vasoconstrictor area • Signals to all levels of spinal cord – Excitation of preganglionic vasoconstrictive neurons – Vasodilator area • Inhibition of vasoconstrictor area – Sensory area • Receives sensory inputs from vagus and glossopharyngeal nerves • Reflex control of many circulatory functions – Activity of both vasoconstrictor and vasodilator
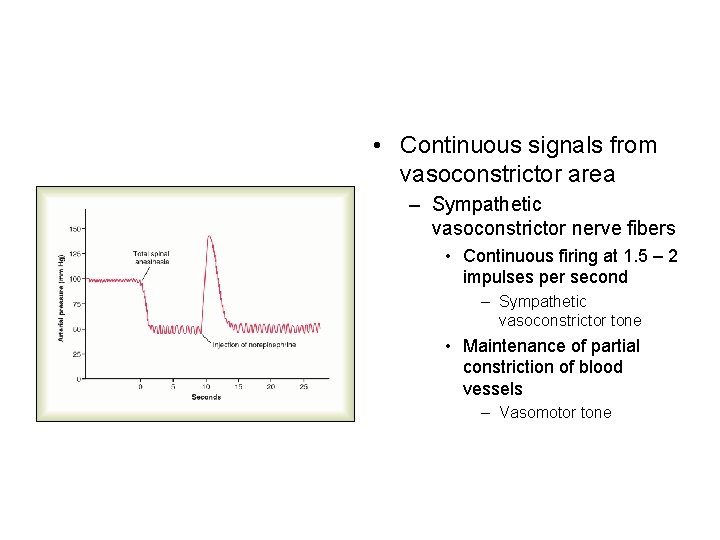
• Continuous signals from vasoconstrictor area – Sympathetic vasoconstrictor nerve fibers • Continuous firing at 1. 5 – 2 impulses per second – Sympathetic vasoconstrictor tone • Maintenance of partial constriction of blood vessels – Vasomotor tone

• Control of heart rate by vasomotor center – Excitatory impulses (sympathetic) • Lateral portion • Increased heart contraction and heart rate – Parasympathetic impulses • Medial portion • Sent via dorsal motor nuclei of the vagus nerves • Decreased heart rate
Control of vasomotor center • The CNS – Reticular substances of the pons, mesencephalon, and diencephalon – Hypothalamus • Posteriolateral – excitation • Anterior – mild excitation/inhibition – Cerebral cortex • Motor cortex • Basal areas of brain

Role of neurotransmitter • Norepinephrine – Sympathetic neurotransmitter • Vasoconstriction – Alpha receptors • Adrenal medulla – Secretion of epinephrine and norepinephrine in response to sympathetic impulses • Vasoconstriction • Vasodilation via beta receptors (epinephrine)

Role of the nervous system in rapid control of arterial blood pressure • Stimulation of sympathetic nervous system and cardioaccelerator – Rapid increase in arterial pressure • 2 X within 5 -10 sec • During exercise or stress • Reciprocal inhibition of parasympathetic vagal inhibitory signals
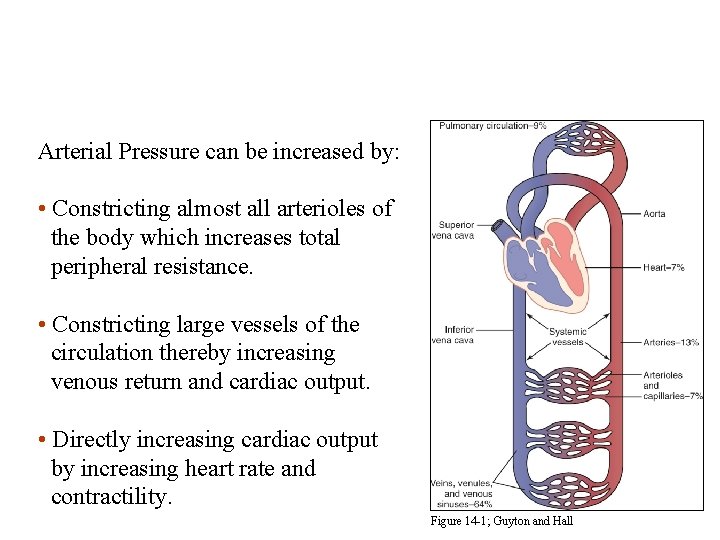
Arterial Pressure = Cardiac Output x Total Peripheral Resistance Arterial Pressure can be increased by: • Constricting almost all arterioles of the body which increases total peripheral resistance. • Constricting large vessels of the circulation thereby increasing venous return and cardiac output. • Directly increasing cardiac output by increasing heart rate and contractility. Figure 14 -1; Guyton and Hall

Maintenance of normal arterial pressure • Negative feedback reflex mechanism – Majority • Baroreceptor reflexes – Reflex initiated by stretching of arterial walls • Increased flow of blood and pressure • Detected by baroreceptors/pressoreceptors • Generation of inhibitory signals
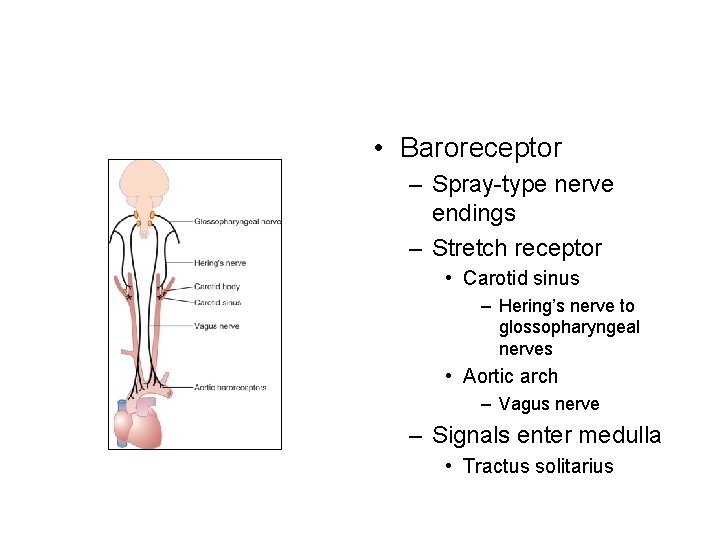
• Baroreceptor – Spray-type nerve endings – Stretch receptor • Carotid sinus – Hering’s nerve to glossopharyngeal nerves • Aortic arch – Vagus nerve – Signals enter medulla • Tractus solitarius
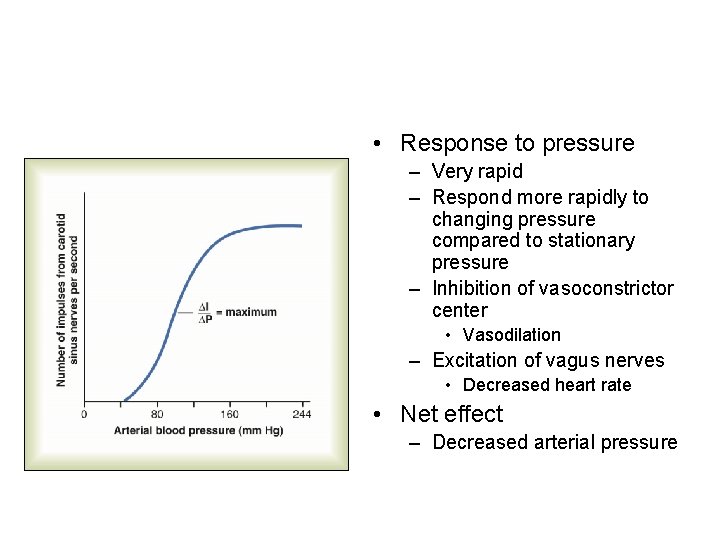
• Response to pressure – Very rapid – Respond more rapidly to changing pressure compared to stationary pressure – Inhibition of vasoconstrictor center • Vasodilation – Excitation of vagus nerves • Decreased heart rate • Net effect – Decreased arterial pressure
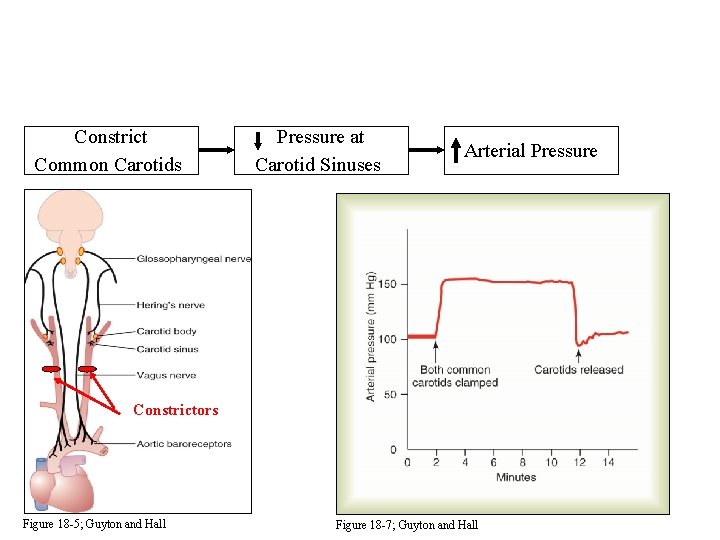
Constrict Common Carotids Pressure at Carotid Sinuses Arterial Pressure Constrictors Figure 18 -5; Guyton and Hall Figure 18 -7; Guyton and Hall
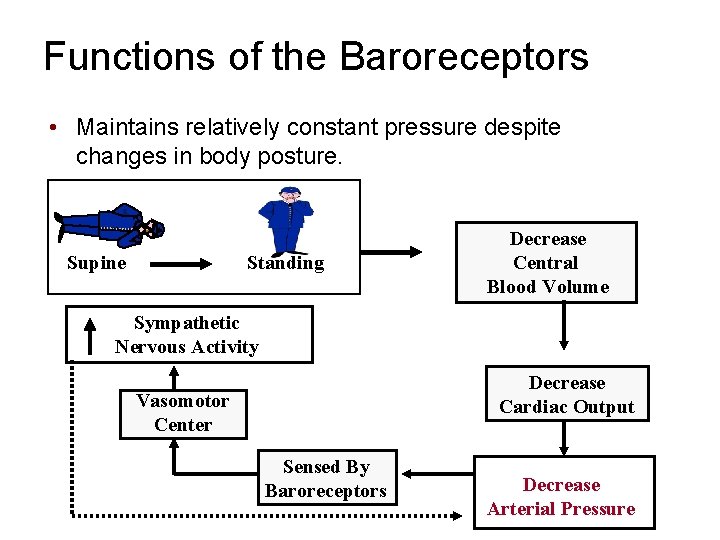
Functions of the Baroreceptors • Maintains relatively constant pressure despite changes in body posture. Supine Standing Decrease Central Blood Volume Sympathetic Nervous Activity Decrease Cardiac Output Vasomotor Center Sensed By Baroreceptors Decrease Arterial Pressure
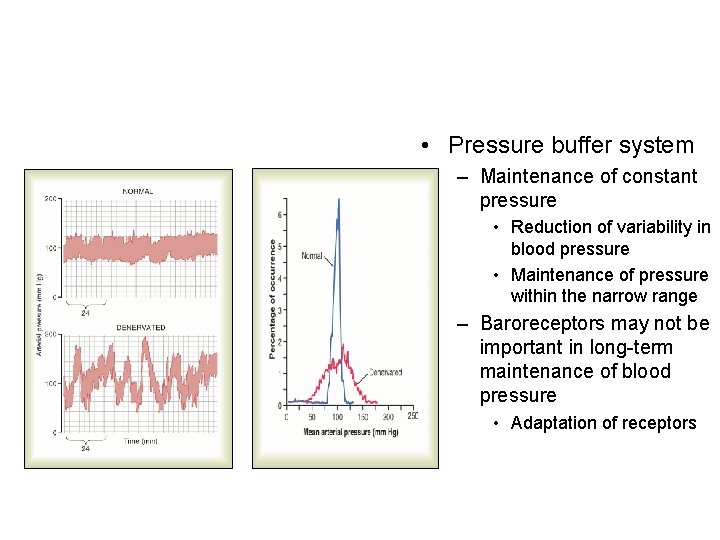
• Pressure buffer system – Maintenance of constant pressure • Reduction of variability in blood pressure • Maintenance of pressure within the narrow range – Baroreceptors may not be important in long-term maintenance of blood pressure • Adaptation of receptors
Other mechanisms • Chemoreceptors – Calotid arteries and aorta • Detection of oxygen concentrations • Detection of carbon dioxide concentrations • Detection of p. H – Detect changes in chemical concentrations • Decreased blood pressure – Excitation of vasomotor center
• Activation of low-pressure receptors – Atria and pulmonary arteries • Detection of increase in pressure caused by increased blood flow • Volume reflex – Increase in glomerular pressure • Increased fluid loss • Decrease blood volume – Secretion of atrial natriaretic peptide • Maintenance of blood volume
• Bainbridge reflex – Increased atrial pressure • Increased heart rate • Caused by increased volume and stretching of sinus node • Triggers increased heart rate – Prevents damming of blood
CNS inschemic response • Loss of blood flow to brain – Cerebral ischemia • Loss of nutrient • Accumulation of carbon dioxide – Activation of vasomotor center • Excitation of vasoconstrictor and cardioaccelerator • Increase in arterial blood pressure
• Cerebral ischemia – Occlusion of blood flow to the peripheral tissues if severe • CNS ischemia response – Emergency pressure control system • Maintenance of blood flow to the brain • Cushing reaction – Special type of CNS ischemia response • Increased CSF pressure around the brain
- Slides: 25