BLOOD Functions Transport of nutrients gases and wastes
BLOOD Functions: • Transport of nutrients, gases, and wastes • Heating and cooling
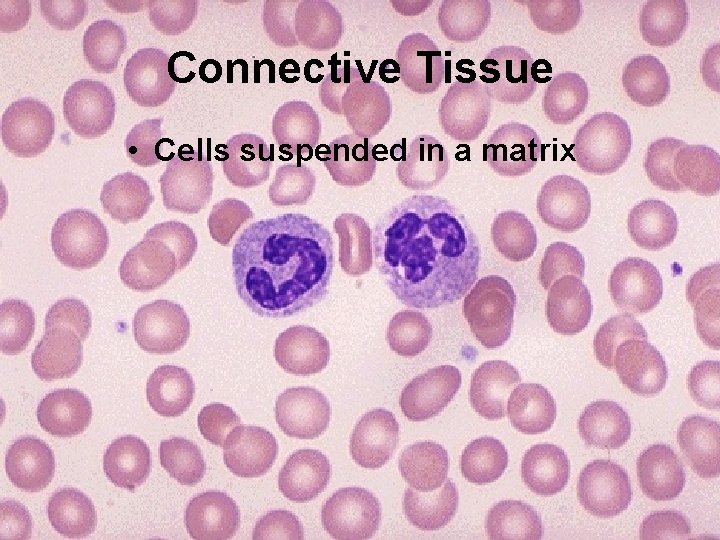
Connective Tissue • Cells suspended in a matrix
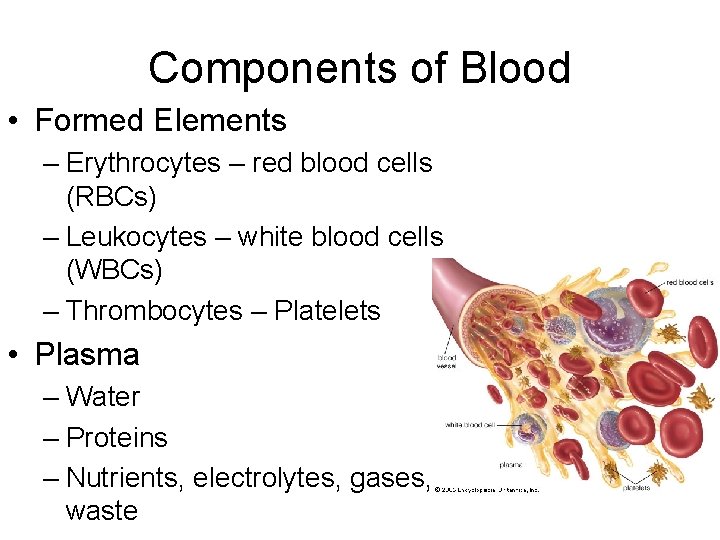
Components of Blood • Formed Elements – Erythrocytes – red blood cells (RBCs) – Leukocytes – white blood cells (WBCs) – Thrombocytes – Platelets • Plasma – Water – Proteins – Nutrients, electrolytes, gases, waste
Centrifuge • Uses centrifugal force to force heavier particles to the bottom • Separates the components of blood.
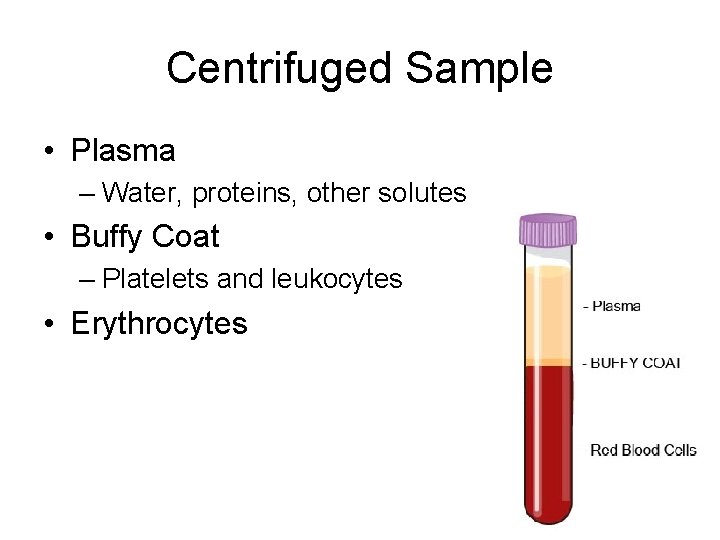
Centrifuged Sample • Plasma – Water, proteins, other solutes • Buffy Coat – Platelets and leukocytes • Erythrocytes
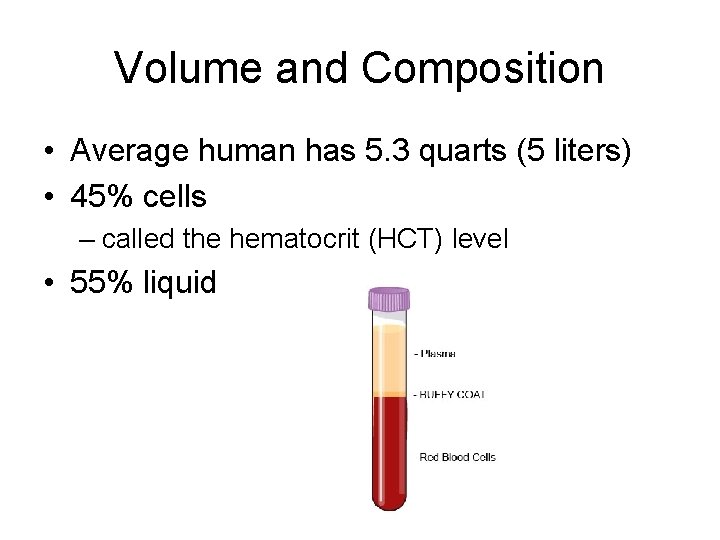
Volume and Composition • Average human has 5. 3 quarts (5 liters) • 45% cells – called the hematocrit (HCT) level • 55% liquid
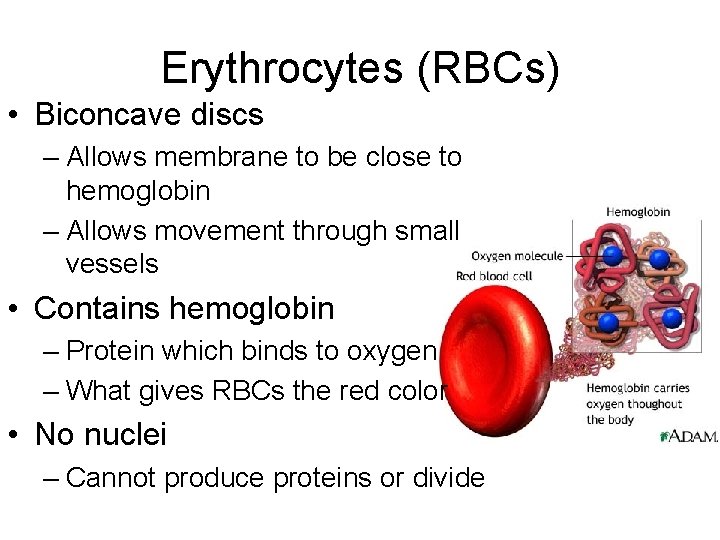
Erythrocytes (RBCs) • Biconcave discs – Allows membrane to be close to hemoglobin – Allows movement through small vessels • Contains hemoglobin – Protein which binds to oxygen – What gives RBCs the red color • No nuclei – Cannot produce proteins or divide
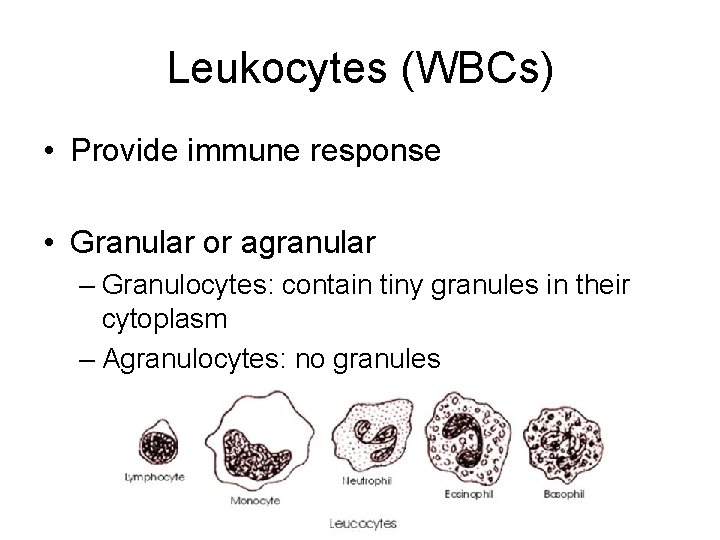
Leukocytes (WBCs) • Provide immune response • Granular or agranular – Granulocytes: contain tiny granules in their cytoplasm – Agranulocytes: no granules
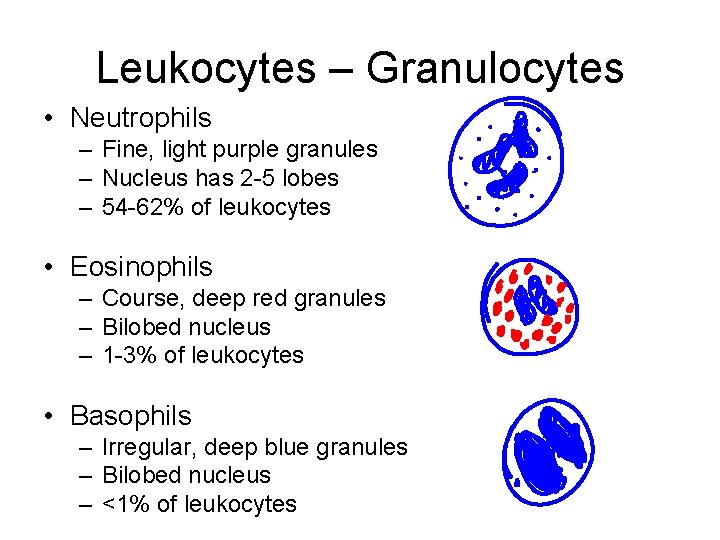
Leukocytes – Granulocytes • Neutrophils – Fine, light purple granules – Nucleus has 2 -5 lobes – 54 -62% of leukocytes • Eosinophils – Course, deep red granules – Bilobed nucleus – 1 -3% of leukocytes • Basophils – Irregular, deep blue granules – Bilobed nucleus – <1% of leukocytes
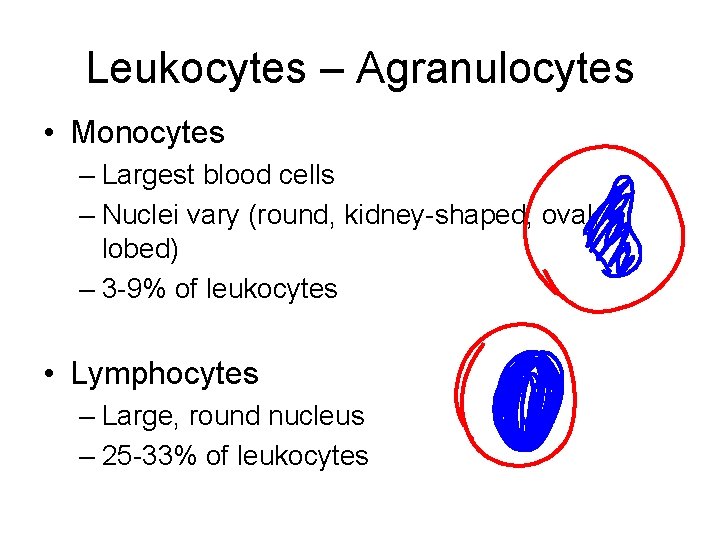
Leukocytes – Agranulocytes • Monocytes – Largest blood cells – Nuclei vary (round, kidney-shaped, oval, lobed) – 3 -9% of leukocytes • Lymphocytes – Large, round nucleus – 25 -33% of leukocytes
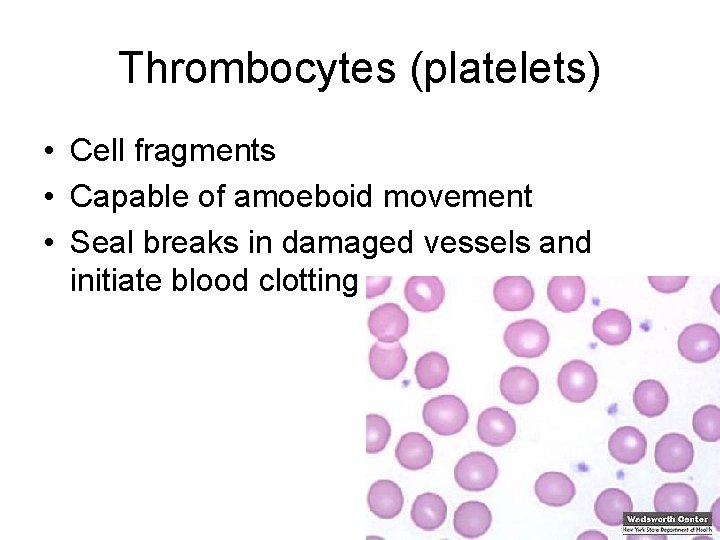
Thrombocytes (platelets) • Cell fragments • Capable of amoeboid movement • Seal breaks in damaged vessels and initiate blood clotting

Plasma • Clear, straw-colored fluid • Matrix in which cells/platelets are suspended
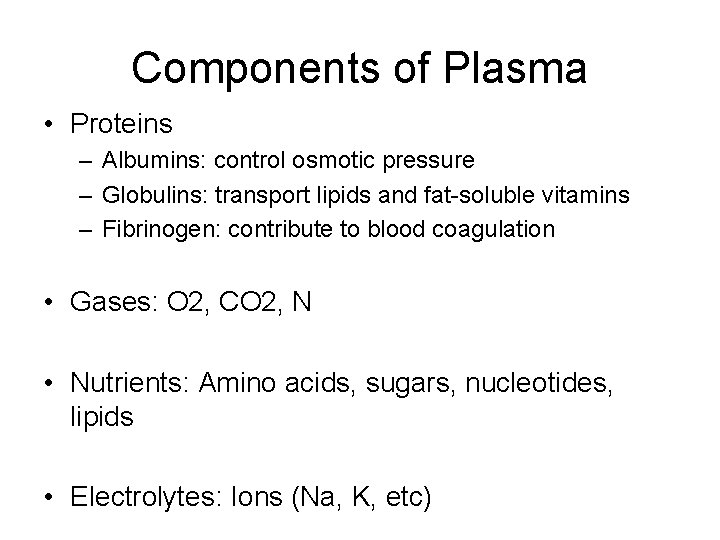
Components of Plasma • Proteins – Albumins: control osmotic pressure – Globulins: transport lipids and fat-soluble vitamins – Fibrinogen: contribute to blood coagulation • Gases: O 2, CO 2, N • Nutrients: Amino acids, sugars, nucleotides, lipids • Electrolytes: Ions (Na, K, etc)
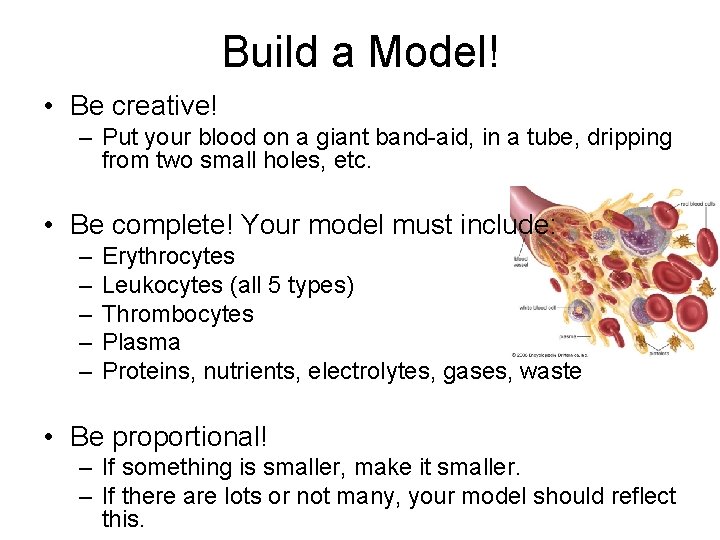
Build a Model! • Be creative! – Put your blood on a giant band-aid, in a tube, dripping from two small holes, etc. • Be complete! Your model must include: – – – Erythrocytes Leukocytes (all 5 types) Thrombocytes Plasma Proteins, nutrients, electrolytes, gases, waste • Be proportional! – If something is smaller, make it smaller. – If there are lots or not many, your model should reflect this.
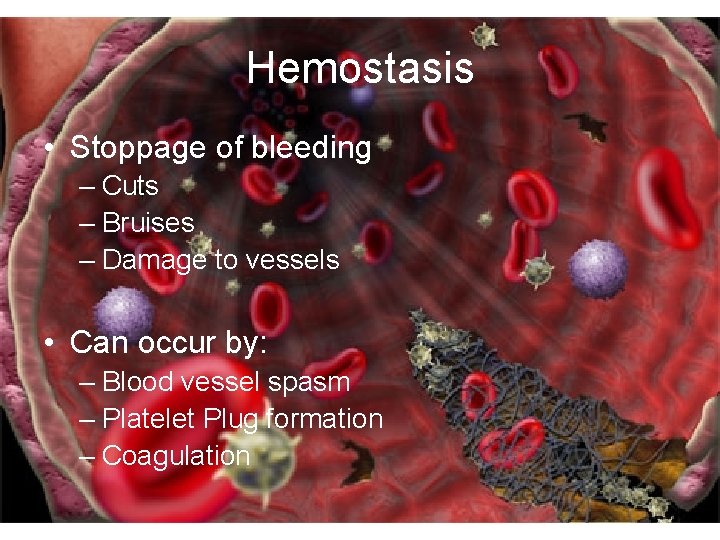
Hemostasis • Stoppage of bleeding – Cuts – Bruises – Damage to vessels • Can occur by: – Blood vessel spasm – Platelet Plug formation – Coagulation

Blood Vessel Spasm • Vessels shrink or close off • Vasospasm: vessel is sealed off completely
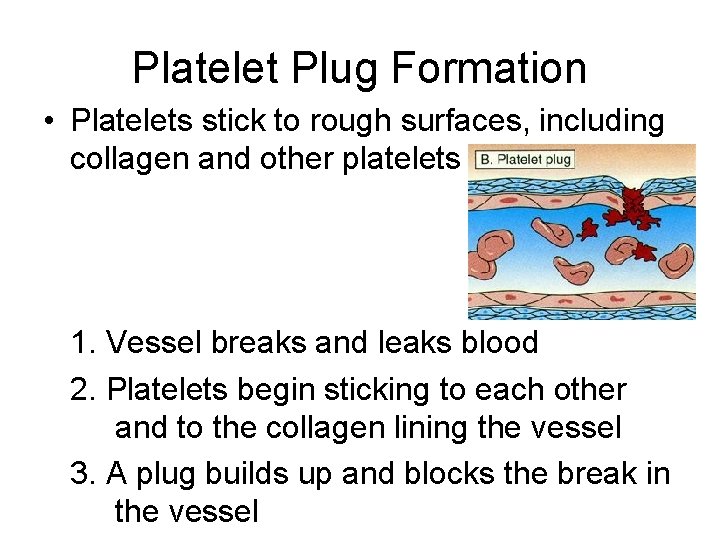
Platelet Plug Formation • Platelets stick to rough surfaces, including collagen and other platelets 1. Vessel breaks and leaks blood 2. Platelets begin sticking to each other and to the collagen lining the vessel 3. A plug builds up and blocks the break in the vessel
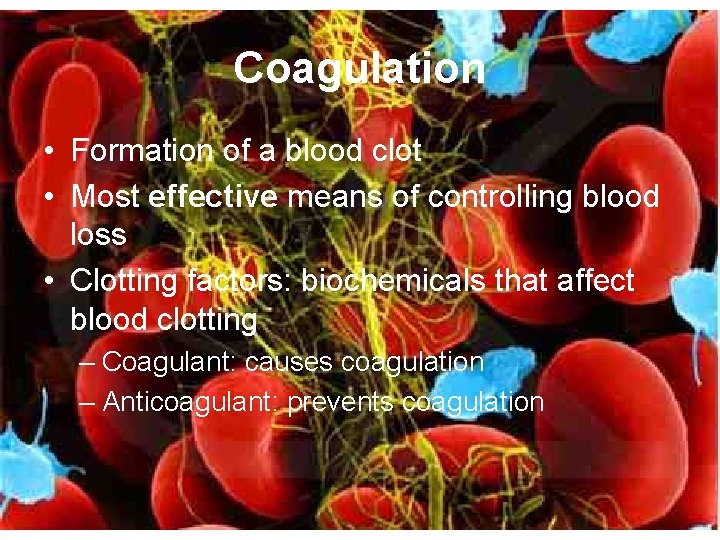
Coagulation • Formation of a blood clot • Most effective means of controlling blood loss • Clotting factors: biochemicals that affect blood clotting – Coagulant: causes coagulation – Anticoagulant: prevents coagulation
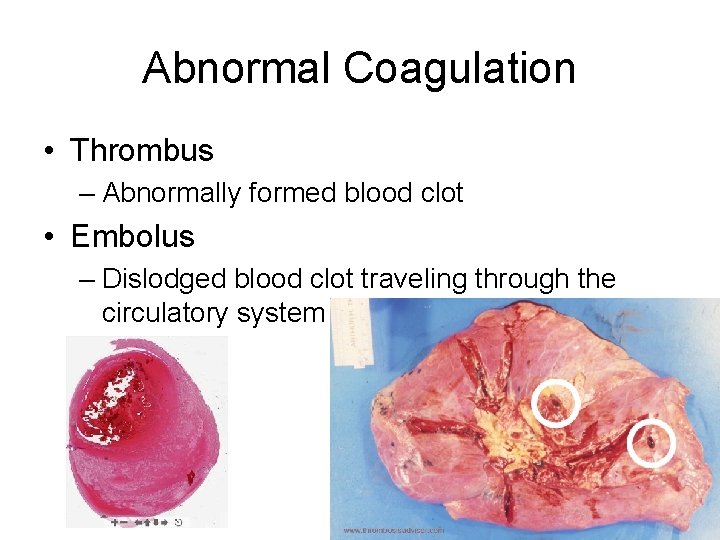
Abnormal Coagulation • Thrombus – Abnormally formed blood clot • Embolus – Dislodged blood clot traveling through the circulatory system
Proteins Involved in Coagulation • Prothrombin – Globulin (plasma protein) – When activated, it is converted to thrombin • Thrombin – Converts fibrinogen to fibrin
Proteins Involved in Coagulation • Fibrinogen – Soluble plasma protein – When activated, it is converted to fibrin • Fibrin – Insoluble threads of protein used to stabilize blood clots – Stick together and form a mesh to catch blood cells
Prothrombin - Thrombin - Fibrinogen - Fibrin 1. Prothrombin is converted to thrombin 2. Thrombin reacts with fibrinogen 3. Fibrinogen is converted to fibrin
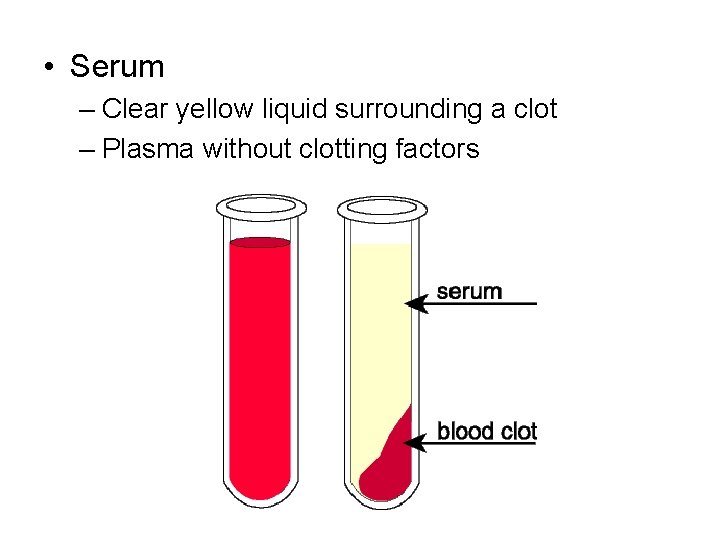
• Serum – Clear yellow liquid surrounding a clot – Plasma without clotting factors
Homeostasis • Blood clotting is a POSITIVE feedback loop • Initiation of clotting causes more clotting
Blood Typing ABO Blood Groups and Rh Factors
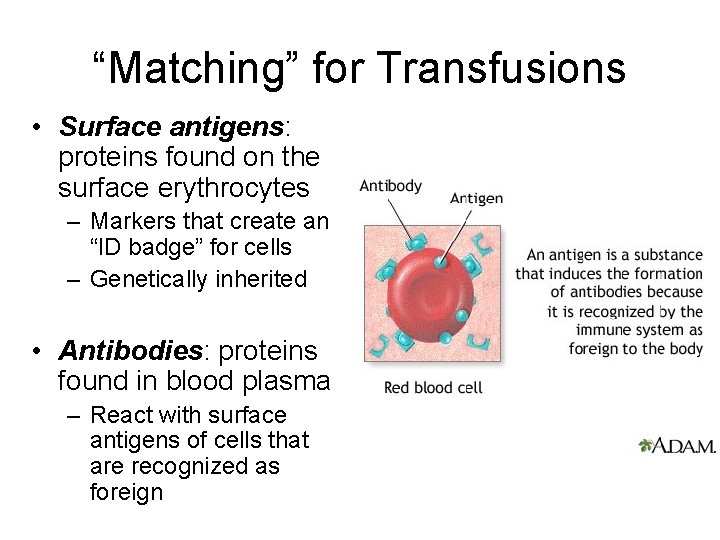
“Matching” for Transfusions • Surface antigens: proteins found on the surface erythrocytes – Markers that create an “ID badge” for cells – Genetically inherited • Antibodies: proteins found in blood plasma – React with surface antigens of cells that are recognized as foreign

• Agglutination: clumping of erythrocytes – Occurs when antibodies detect surface antigens of a different ABO or Rh group
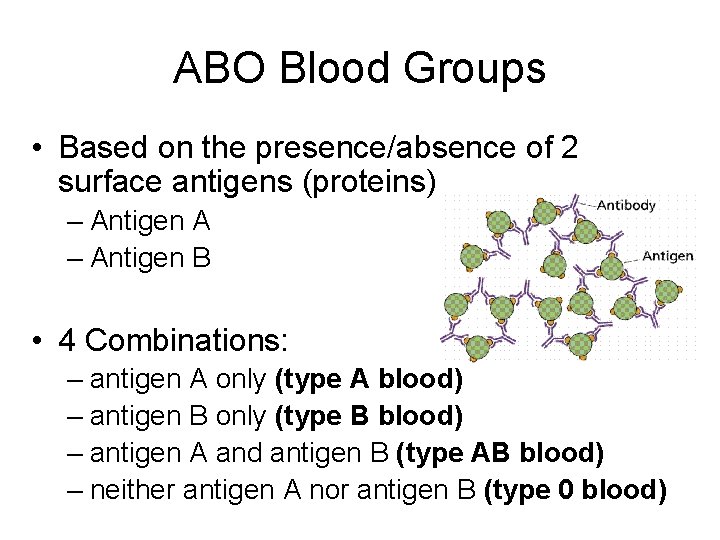
ABO Blood Groups • Based on the presence/absence of 2 surface antigens (proteins) – Antigen A – Antigen B • 4 Combinations: – antigen A only (type A blood) – antigen B only (type B blood) – antigen A and antigen B (type AB blood) – neither antigen A nor antigen B (type 0 blood)
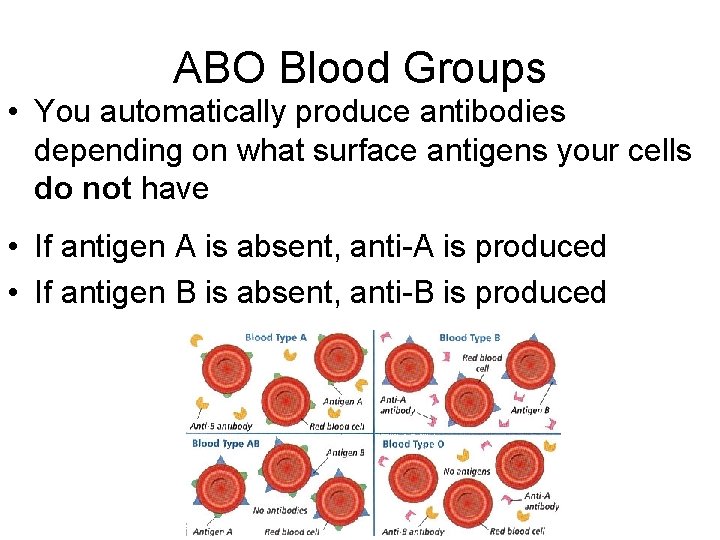
ABO Blood Groups • You automatically produce antibodies depending on what surface antigens your cells do not have • If antigen A is absent, anti-A is produced • If antigen B is absent, anti-B is produced
Blood Transfusions • Antibodies react with their respective surface antigens, causing agglutination • Type AB contains both antigens and produces neither antibodies – Can receive any blood type – Universal recipient • Type O contains neither antigens and produces both antibodies – Can be donated to any blood type – Universal donor

Complete the following table: Blood Type Surface Antigen Present Antibody Produced Possible Blood Type Donors A antigen A anti-B A, O B AB O
Rh Factors • Based on the presence/absence of Rh surface antigens • Rh antigen present: Rh-positive • Rh antigen absent: Rh-negative
Rh Antibodies • Anti-Rh is not automatically produced when Rh surface antigens are absent (unlike ABO antibodies) • Produced in Rh-neg blood, in response to the introduction of Rhpos blood
When Rh Causes Agglutination • Rh-neg person receives Rh-pos blood – No reaction takes place – Following donation, anti-Rh is produced • Same Rh-neg person recieves Rh-pos blood again – Agglutination occurs
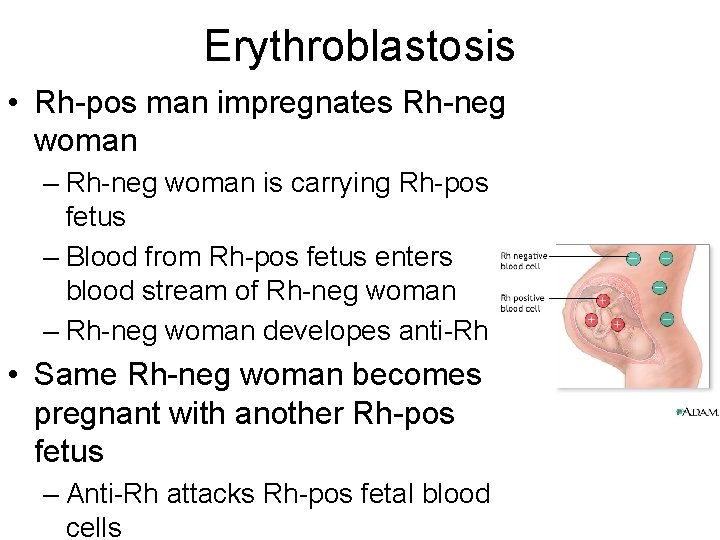
Erythroblastosis • Rh-pos man impregnates Rh-neg woman – Rh-neg woman is carrying Rh-pos fetus – Blood from Rh-pos fetus enters blood stream of Rh-neg woman – Rh-neg woman developes anti-Rh • Same Rh-neg woman becomes pregnant with another Rh-pos fetus – Anti-Rh attacks Rh-pos fetal blood cells
In the U. S. , what blood type do you think is the most common? Least common? List the blood types in order from most to least common. Here are your options: • A+ • A • B+ • B • AB+ • AB • O+ • O-
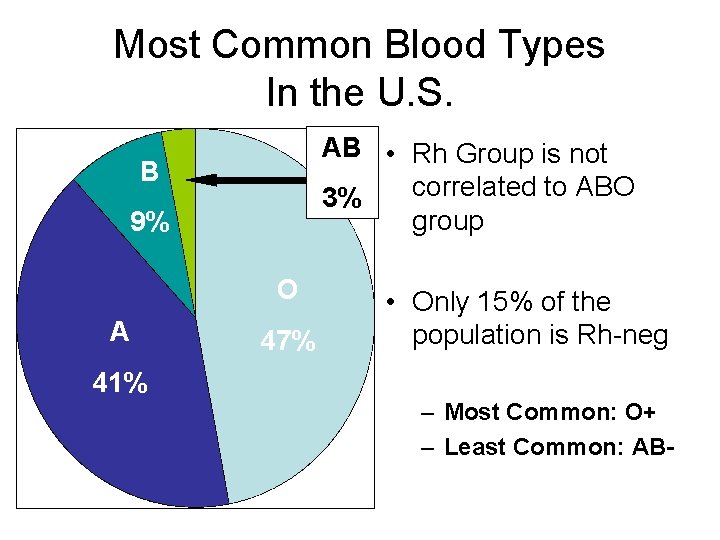
Most Common Blood Types In the U. S. AB • Rh Group is not correlated to ABO 3% group B 9% O A 47% • Only 15% of the population is Rh-neg 41% – Most Common: O+ – Least Common: AB-
- Slides: 37