Blood flow and flow regulation Dr Waleed R
Blood flow and flow regulation Dr. Waleed R. Ezzat
Lecture Objectives: 1. Describe the local mechanism that control blood flow to tissues, including acute and longterm control. 2. Discuss the metabolic and myogenic theory for control of blood flow. 3. Discuss the changes that can develop in long- term regulation, including tissue vascularity, angiogensis and collateral circulation. 4. Discuss humoral regulation of blood flow, by vasoconstrictor and vasodilator agents.
Classification 1. Local control (intrinsic regulation, autoregulation) 2. Extrinsic control (humoral and neural regulation) ■ ■ Local control: (def. ) is the ability of each tissue to control its own local blood flow in proportion to its metabolic needs. In general, the greater the metabolism in an organ, the greater is its blood flow. The cerebral, cardiac, and renal circulations have the highest autoregulation efficacy. Skeletal muscle and intestinal vasculatures exhibit less well-developed autoregulation, whereas autoregulation is essentially absent in the circulation of the skin. Advantage of local control; The tissues never suffer from nutritional deficiency, and yet the workload on the heart is kept at a minimum.
Mechanism of local control of blood flow 1. Acute control – rapid changes in local vasodilation or vasoconstriction of the arterioles. 2. Long-term control – slow changes in flow over a period of days, weeks, or even months. These changes are the result of an increase or decrease in the physiological sizes and numbers of actual blood vessels supplying the tissues.
Theories of acute local control of blood flow 1. The metabolic theory; a. Vasodilator theory (wash away theory) – The suggested vasodilators are adenosine, CO 2, adenosine phosphate compounds, histamine, K+, and H+. They are released in response to O 2 deficiency. b. Oxygen lack (or nutrient lack) theory – It is based on the fact that arteriolar smooth muscle need O 2 to maintain their tone. Hypoxia causes the endothelial release of nitric oxide (NO). NO causes the relaxation of vascular smooth muscle by activating guanylate cyclase within the muscle cells to increase the production of cyclic guanosine monophosphate (c. GMP), and the blood vessels dilate in response. Note: The above theories are supported by the presence of vasodilation in reactive hyperemia and active hyperemia that follows the increase in metabolic activities.
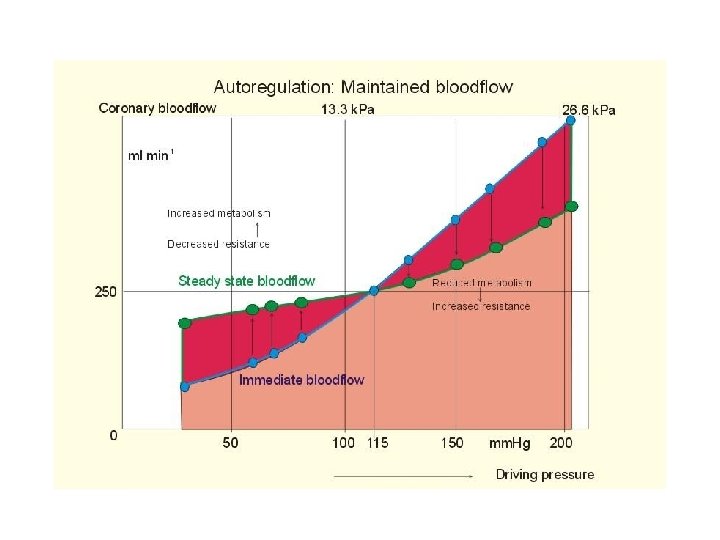
Theories of acute local control of blood flow (Cont. ) 2. The myogenic theory ; The sudden rise in flow that follows the sudden rise in pressure returns to normal within less than a minute, even though the arterial pressure is kept elevated (i. e. autoregulation). This theory is based on the reactive vascular contraction in response to pressure induced stretching of a vessel (La. Place law). The cellular mechanisms responsible for myogenic regulation are not entirely understood. It is believed that arterioles have stretch-activated calcium channels. Adding calcium to the cytoplasm from the extracellular fluid through these channels would activate the smooth muscle cell and result in contraction. Few arterioles exhibit the myogenic response; therefore, this theory is not popular.
Mechanism of long-term regulation of blood flow n n n Chronic ↑ or ↓ in metabolism → ↑ or ↓ in vascularity. This mechanism acts better and faster in young than in old. Vascular growth factors (= angiogenic factors) are released in chronic O 2 deficiency. They cause new vessels to sprout from other small vessels. These factors are; Vascular endothelial growth factor (VEGF) – Fibroblast growth factor – Angiogenin – n The development of collateral vessels follows the same principles of long-term control mechanism.
The extrinsic control 1. The humoral regulation – it means regulation by substances secreted or absorbed into body fluids, such as hormones and ions. A. Humoral vasoconstrictors are norepinephrine (NE) and epinephrine (E), angiotensin, vasopressin, and endothelin (in damaged blood vessels). B. Humoral vasodilators are bradykinin (polypeptides) and histamine (from mast cells and basophils). 2. The neural regulation – sympathetic stimulation during stress or exercise lead to release of NE that activates membrane α 1 -adrenergic receptors in arterioles and veins (vasoconstriction). Sympathetic stimulation as such redistributes blood flow by shifting blood from non-active tissues to active ones.
Intrinsic versus extrinsic regulation Some vascular beds are controlled dominantly by local or intrinsic mechanisms (such as coronary and cerebral circulations), some are dominantly regulated by extrinsic control (such as cutaneous and splanchnic circulations), other exhibit dual control (such as skeletal muscles).
Test: In an experiment, the diameter of the femoral artery was measured prior to and after the arterial endothelium was damaged. The dilator response to injected acetylcholine changed to a constrictor response when the endothelium was damaged. What is the basis for this effect? A. More Na+ is generated. B. More bradykinin is generated. C. The damage elevates c. GMP in the remaining vascular smooth muscle. D. The damage augments the production of endothelin by the endothelium. E. The damage interferes with the production of NO by the endothelium.
- Slides: 11