Blood Capillaries and Homeostasis or Making interstitial Fluid
Blood, Capillaries and Homeostasis or Making interstitial Fluid = “the sea within us” Metro Human Anatomy and Physiology Fall 2016 Stan Misler <latrotox@gmail. com>
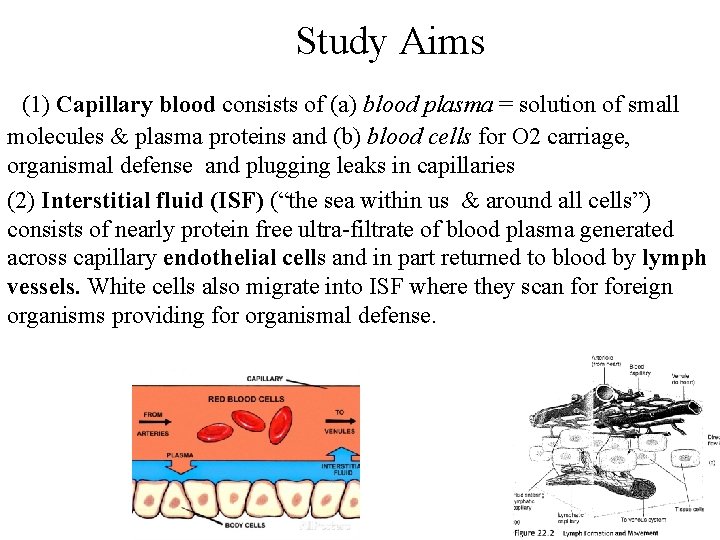
Study Aims (1) Capillary blood consists of (a) blood plasma = solution of small molecules & plasma proteins and (b) blood cells for O 2 carriage, organismal defense and plugging leaks in capillaries (2) Interstitial fluid (ISF) (“the sea within us & around all cells”) consists of nearly protein free ultra-filtrate of blood plasma generated across capillary endothelial cells and in part returned to blood by lymph vessels. White cells also migrate into ISF where they scan foreign organisms providing for organismal defense.
1. Maintenance of ISF volume and composition is central to organism’s function i. e. , is at the heart of homeostasis Organs share function and contribute to a “constant” internal environment, the interstitial fluid (ISF) Tissues interact with metabolic “give and take”: kidney and liver as master excretors of nitrogenous wastes (urea, uric acid, ammonium) and The constant of content of ISF reduces most of general housekeeping function of all cells and frees them for more specialized functions. The migration of white blood cells into the ISF provides a total body response to foreign organisms or tumor cells.
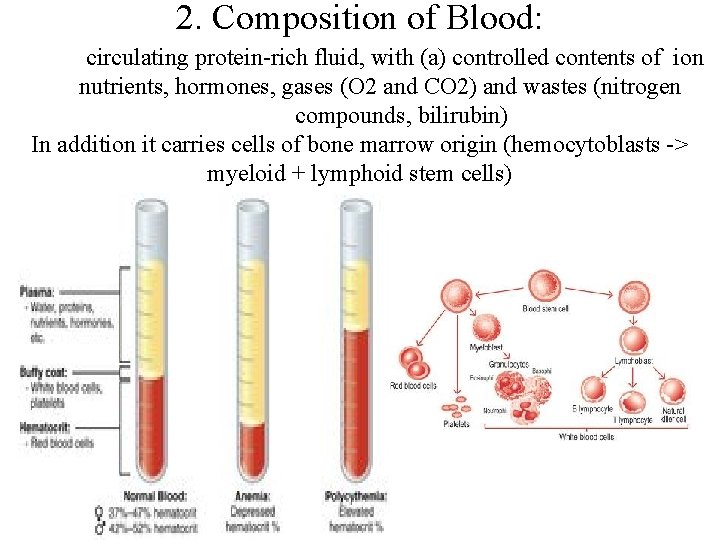
2. Composition of Blood: circulating protein-rich fluid, with (a) controlled contents of ion nutrients, hormones, gases (O 2 and CO 2) and wastes (nitrogen compounds, bilirubin) In addition it carries cells of bone marrow origin (hemocytoblasts -> myeloid + lymphoid stem cells)
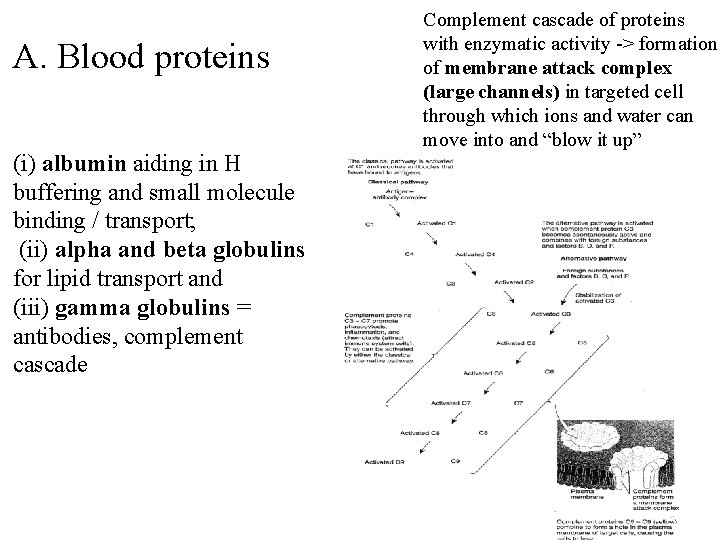
A. Blood proteins (i) albumin aiding in H buffering and small molecule binding / transport; (ii) alpha and beta globulins for lipid transport and (iii) gamma globulins = antibodies, complement cascade Complement cascade of proteins with enzymatic activity -> formation of membrane attack complex (large channels) in targeted cell through which ions and water can move into and “blow it up”

Structure of antibody molecule (Ig. G)
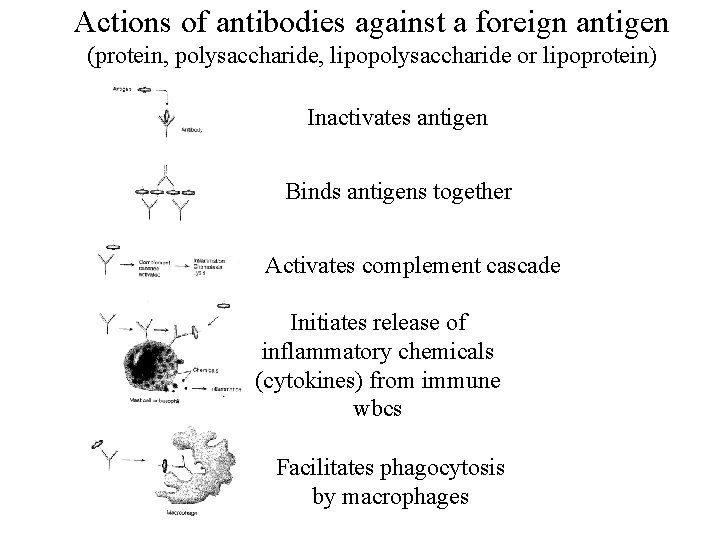
Actions of antibodies against a foreign antigen (protein, polysaccharide, lipopolysaccharide or lipoprotein) Inactivates antigen Binds antigens together Activates complement cascade Initiates release of inflammatory chemicals (cytokines) from immune wbcs Facilitates phagocytosis by macrophages
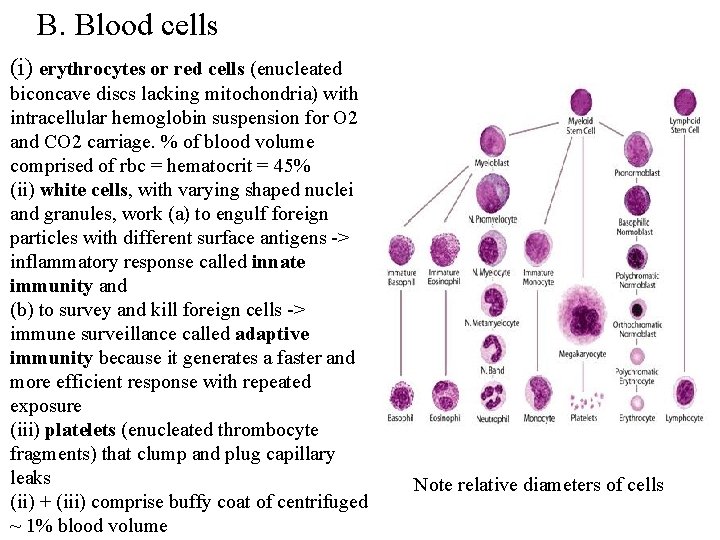
B. Blood cells (i) erythrocytes or red cells (enucleated biconcave discs lacking mitochondria) with intracellular hemoglobin suspension for O 2 and CO 2 carriage. % of blood volume comprised of rbc = hematocrit = 45% (ii) white cells, with varying shaped nuclei and granules, work (a) to engulf foreign particles with different surface antigens -> inflammatory response called innate immunity and (b) to survey and kill foreign cells -> immune surveillance called adaptive immunity because it generates a faster and more efficient response with repeated exposure (iii) platelets (enucleated thrombocyte fragments) that clump and plug capillary leaks (ii) + (iii) comprise buffy coat of centrifuged ~ 1% blood volume Note relative diameters of cells
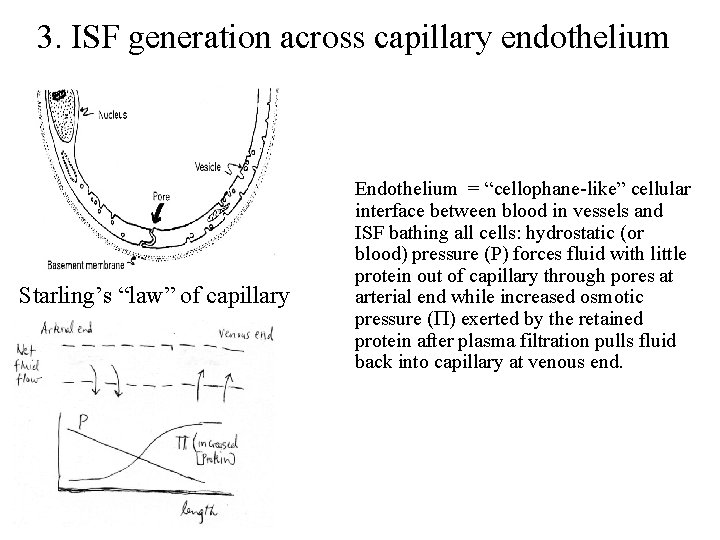
3. ISF generation across capillary endothelium Starling’s “law” of capillary Endothelium = “cellophane-like” cellular interface between blood in vessels and ISF bathing all cells: hydrostatic (or blood) pressure (P) forces fluid with little protein out of capillary through pores at arterial end while increased osmotic pressure (P) exerted by the retained protein after plasma filtration pulls fluid back into capillary at venous end.
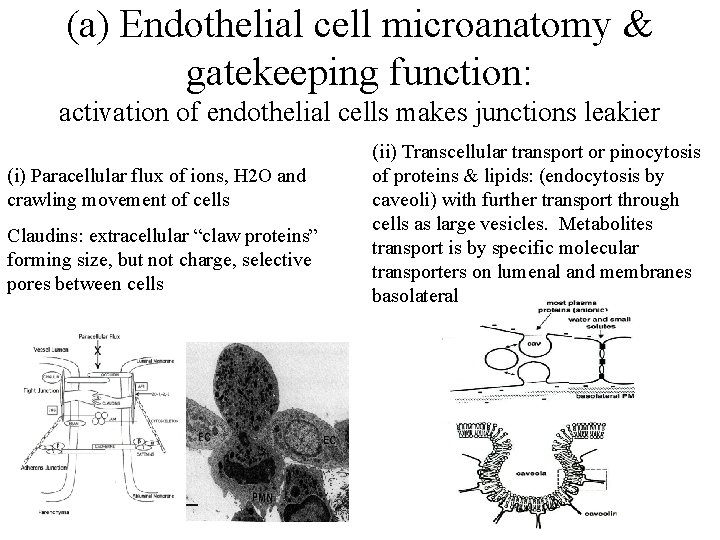
(a) Endothelial cell microanatomy & gatekeeping function: activation of endothelial cells makes junctions leakier (i) Paracellular flux of ions, H 2 O and crawling movement of cells Claudins: extracellular “claw proteins” forming size, but not charge, selective pores between cells (ii) Transcellular transport or pinocytosis of proteins & lipids: (endocytosis by caveoli) with further transport through cells as large vesicles. Metabolites transport is by specific molecular transporters on lumenal and membranes basolateral
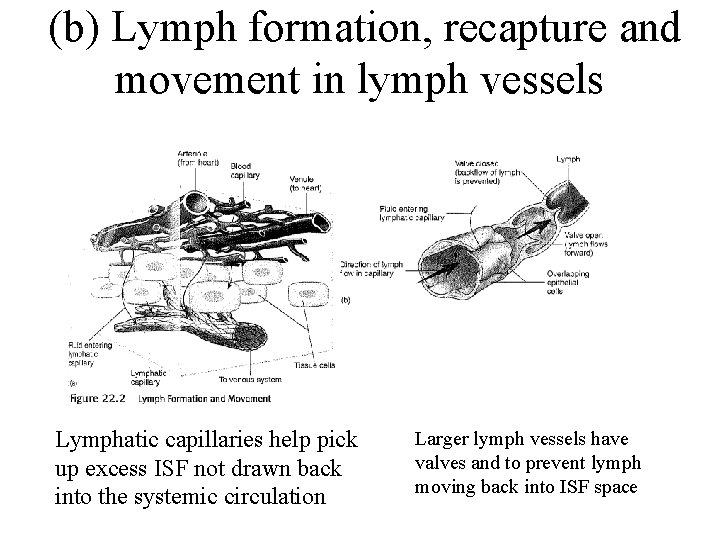
(b) Lymph formation, recapture and movement in lymph vessels Lymphatic capillaries help pick up excess ISF not drawn back into the systemic circulation Larger lymph vessels have valves and to prevent lymph moving back into ISF space
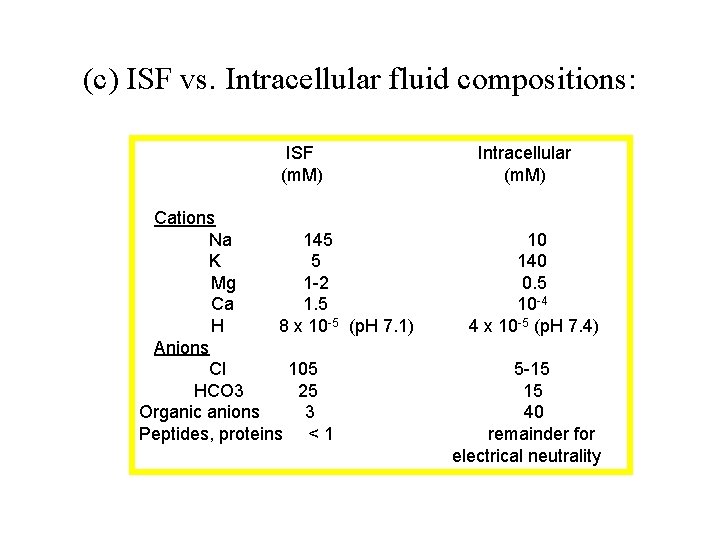
(c) ISF vs. Intracellular fluid compositions: ISF (m. M) Cations Na 145 K 5 Mg 1 -2 Ca 1. 5 H 8 x 10 -5 (p. H 7. 1) Anions Cl 105 HCO 3 25 Organic anions 3 Peptides, proteins < 1 Intracellular (m. M) 10 140 0. 5 10 -4 4 x 10 -5 (p. H 7. 4) 5 -15 15 40 remainder for electrical neutrality
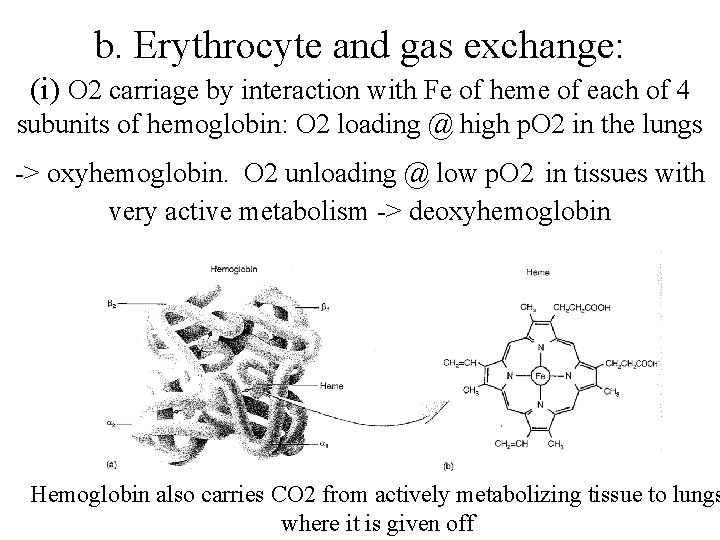
b. Erythrocyte and gas exchange: (i) O 2 carriage by interaction with Fe of heme of each of 4 subunits of hemoglobin: O 2 loading @ high p. O 2 in the lungs -> oxyhemoglobin. O 2 unloading @ low p. O 2 in tissues with very active metabolism -> deoxyhemoglobin Hemoglobin also carries CO 2 from actively metabolizing tissue to lungs where it is given off
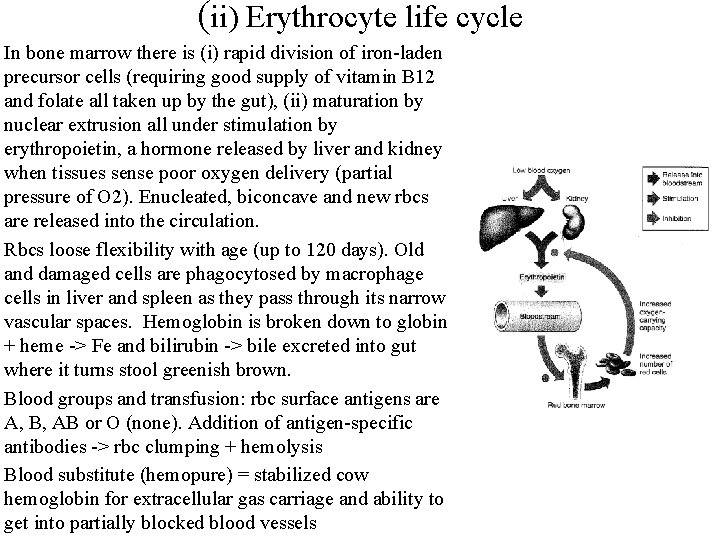
(ii) Erythrocyte life cycle In bone marrow there is (i) rapid division of iron-laden precursor cells (requiring good supply of vitamin B 12 and folate all taken up by the gut), (ii) maturation by nuclear extrusion all under stimulation by erythropoietin, a hormone released by liver and kidney when tissues sense poor oxygen delivery (partial pressure of O 2). Enucleated, biconcave and new rbcs are released into the circulation. Rbcs loose flexibility with age (up to 120 days). Old and damaged cells are phagocytosed by macrophage cells in liver and spleen as they pass through its narrow vascular spaces. Hemoglobin is broken down to globin + heme -> Fe and bilirubin -> bile excreted into gut where it turns stool greenish brown. Blood groups and transfusion: rbc surface antigens are A, B, AB or O (none). Addition of antigen-specific antibodies -> rbc clumping + hemolysis Blood substitute (hemopure) = stabilized cow hemoglobin for extracellular gas carriage and ability to get into partially blocked blood vessels
c. Leukocytes: Inflammatory + Immune Responses Granulocytes = (i) Neutrophils (polymorphonuclear neutrophils = PMN) rapidly move along surface by amoeboid motility and across capillary wall by diapedesis. Engulf bacteria by phagocytosis (a form of endocytosis). Resultant endosome fuses with cell lysosomes for intracellular digestion; release of chemotactic factors -> chemoattraction for more neutrophils (ii) Basophils and sessile mast cells release mediators such as histamine and heparin and promote inflammation (Latin description of inflammation = calor, dolor, rubor, tumor, functio lasso) & -> pyrogens (iii) Eosinophils inhibit inflammation (push pull with basophils) Agranulocytes = (i) Monocytes -> macrophages -> endocytosing large particles (ii) Natural killer cells -> lysis of tumor and virus infected cells (iii) Immune cells: B cells -> plasma cells = humoral (antibody mediated immune response) vs. T cells -> cytotoxic T cells, helper and suppressor T cells = cell mediated immune response. B cells = binding antigen by their surface antibodies (= antigen receptors) -> cell division to form clones -> memory cells and plasma cells that secrete antibodies against antigen-displaying agents. Complement is activated by tails of antibodies on target cells -> membrane attack complexes on surface of “foreign looking” cells -> osmotic lysis
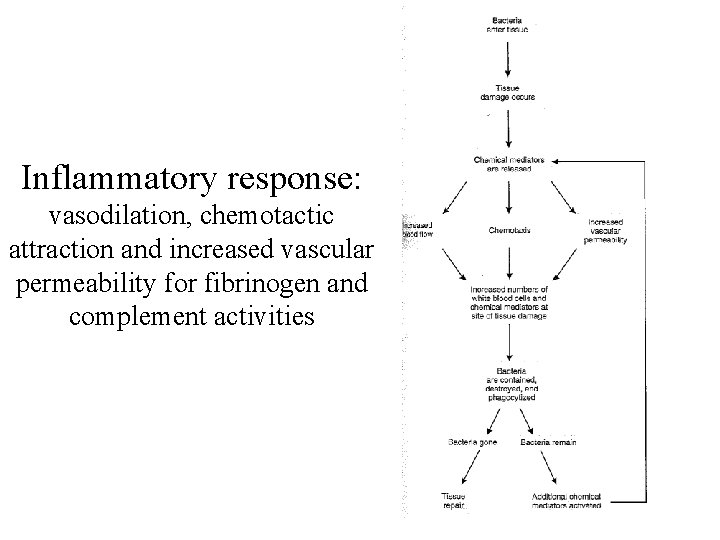
Inflammatory response: vasodilation, chemotactic attraction and increased vascular permeability for fibrinogen and complement activities
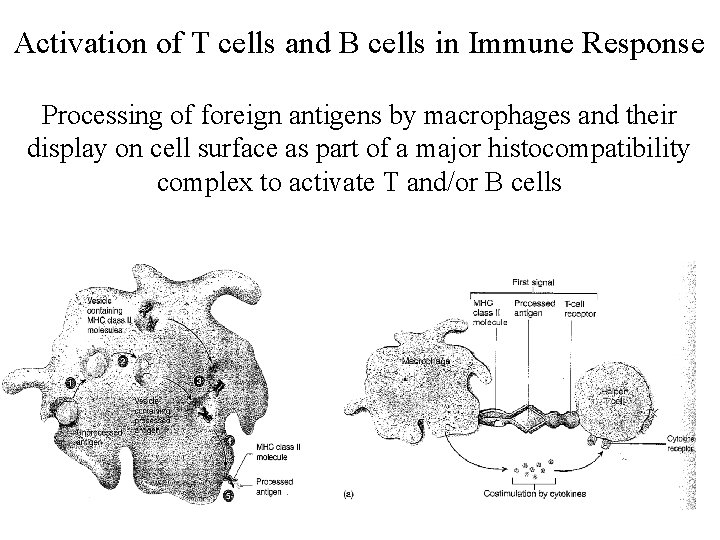
Activation of T cells and B cells in Immune Response Processing of foreign antigens by macrophages and their display on cell surface as part of a major histocompatibility complex to activate T and/or B cells
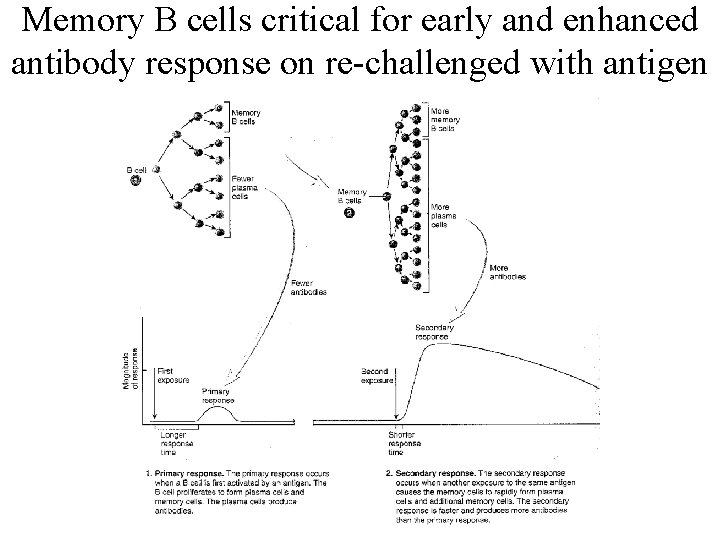
Memory B cells critical for early and enhanced antibody response on re-challenged with antigen
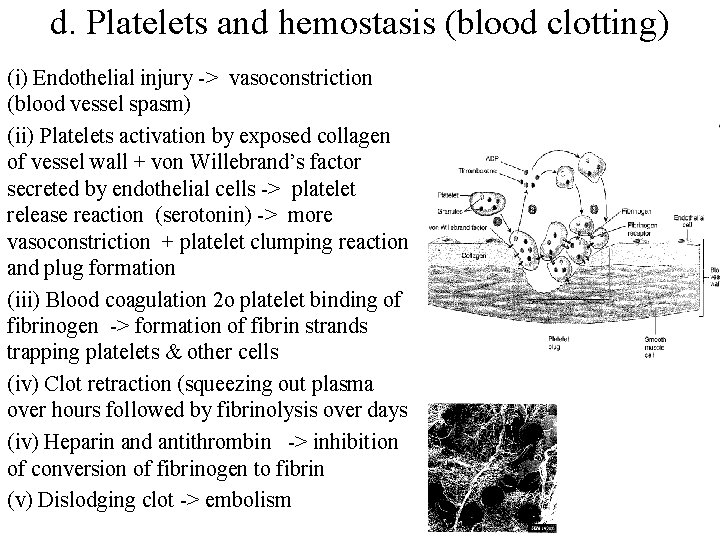
d. Platelets and hemostasis (blood clotting) (i) Endothelial injury -> vasoconstriction (blood vessel spasm) (ii) Platelets activation by exposed collagen of vessel wall + von Willebrand’s factor secreted by endothelial cells -> platelet release reaction (serotonin) -> more vasoconstriction + platelet clumping reaction and plug formation (iii) Blood coagulation 2 o platelet binding of fibrinogen -> formation of fibrin strands trapping platelets & other cells (iv) Clot retraction (squeezing out plasma over hours followed by fibrinolysis over days (iv) Heparin and antithrombin -> inhibition of conversion of fibrinogen to fibrin (v) Dislodging clot -> embolism
5. Some clinical correlations a. Anemias = pale and listless • Nutritional: Fe deficiency = small rbcs (microcytes) with little hemoglobin; B 12 and / or folate deficiency = large rbcs (macrocytes) as rbc precursors divide poorly • Hemolytic : defect in of rbc membrane vs. post-transfusion attack by preformed antibodies to non-native rbc surface antigens -> easy rupture • Aplastic = poor rbc precursor division due to damage to bone marrow (antibiotics, chemotherapy, radiation) or lack of erythropoietin • Sickle cell disease: deformed rbc (due to defective hemoglobin crystalizing into strands at low p. O 2) reduces chance of rbc passage through liver and spleen without being “chewed up”
b. Acquired immunodeficiency syndrome (AIDS) due to human immunodeficiency virus (HIV) 1. Infection via body fluid (blood, semen, vaginal secretion) coming from unprotected sexual contact (heterosexual & homosexual) contaminated needles, tainted blood products; pregnant woman to fetus or from mother to infant via breast feeding 2. Helper T Cell infection: surface viral protein gp 120 antigen binds to CD 4 surface receptor on helper T cells -> injection of viral RNA and enzymes into helper T cell -> intracellular viral replication -> @ 3 wks to 3 mo after infection-> fever, sweats, fatigue, joint aches, diarrhea, swollen lymph nodes. 3. Later slow rate of viral replication -> slow decrease in helper T cells. With helper T cells below 200/mm 3 opportunistic infection become more likely (tuberculosis, pneumocystis pneumonia & candidiasis). 4. With aggressive treatment, HIV has become chronically treatable. Effective Rx = 2 reverse transcriptase inhibitors (KO viral RNA to DNA) + 1 viral protease inhibitor (breakdown of viral protein). Under investigation is viral integrase inhibitor to prevent viral DNA incorporation into host DNA
- Slides: 21