Blood Blood Fluid connective tissue Functions include Transporting
Blood

Blood • Fluid connective tissue • Functions include • Transporting dissolved gases, nutrients, hormones, and metabolic wastes • Regulating p. H and ion composition of interstitial fluids • Restricting fluid loss at injury sites • Defending the body against toxins and pathogens • Regulating body temperature by absorbing and redistributing heat
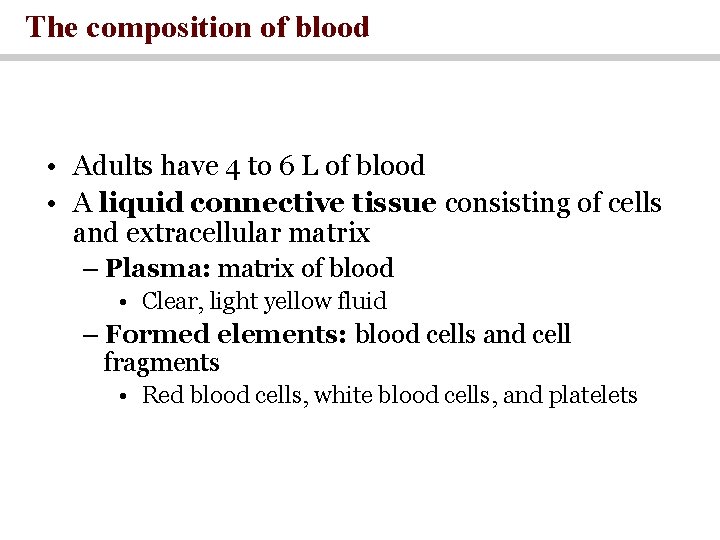
The composition of blood • Adults have 4 to 6 L of blood • A liquid connective tissue consisting of cells and extracellular matrix – Plasma: matrix of blood • Clear, light yellow fluid – Formed elements: blood cells and cell fragments • Red blood cells, white blood cells, and platelets
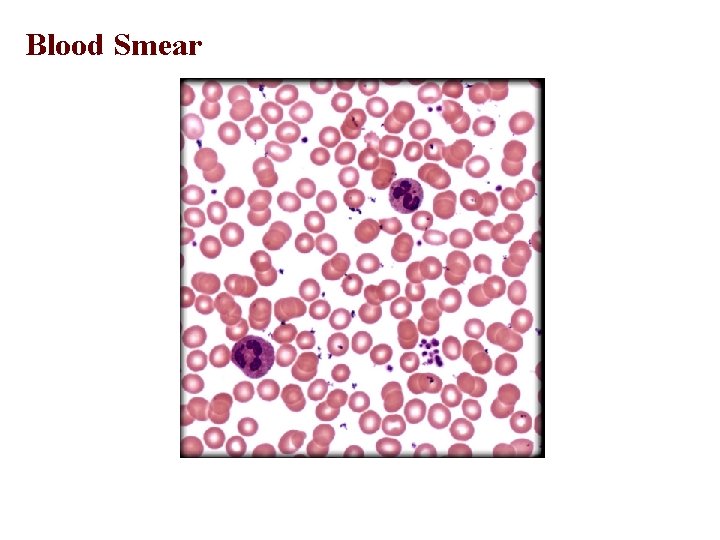
Blood Smear
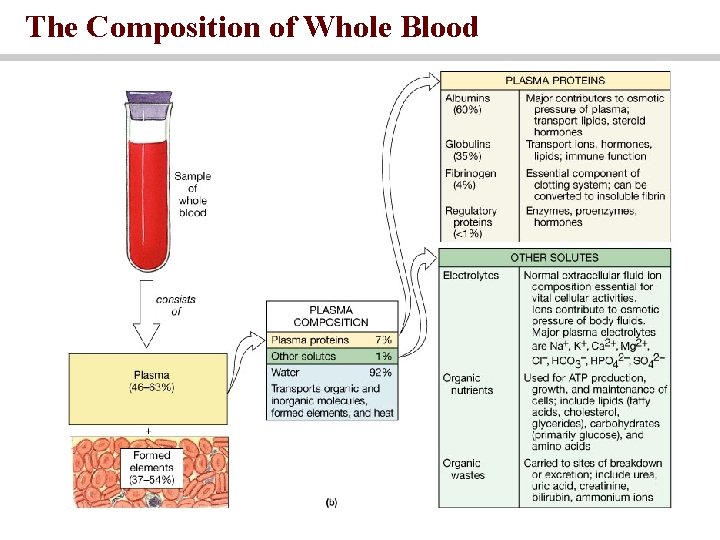
The Composition of Whole Blood
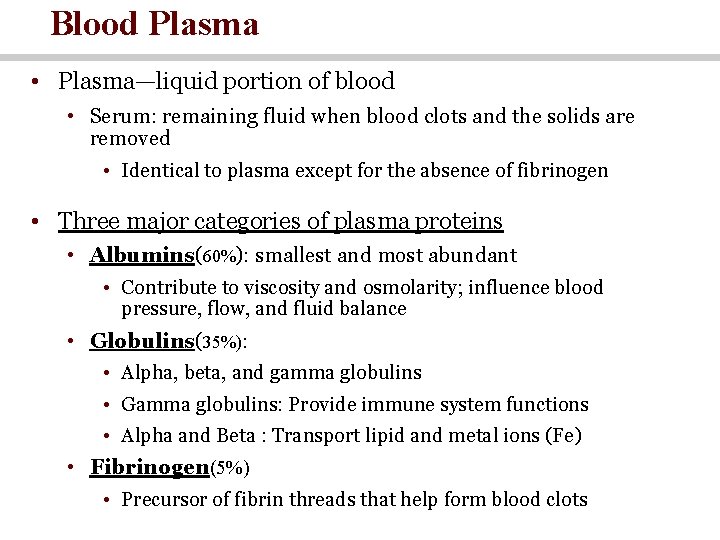
Blood Plasma • Plasma—liquid portion of blood • Serum: remaining fluid when blood clots and the solids are removed • Identical to plasma except for the absence of fibrinogen • Three major categories of plasma proteins • Albumins(60%): smallest and most abundant • Contribute to viscosity and osmolarity; influence blood pressure, flow, and fluid balance • Globulins(35%): • Alpha, beta, and gamma globulins • Gamma globulins: Provide immune system functions • Alpha and Beta : Transport lipid and metal ions (Fe) • Fibrinogen(5%) • Precursor of fibrin threads that help form blood clots
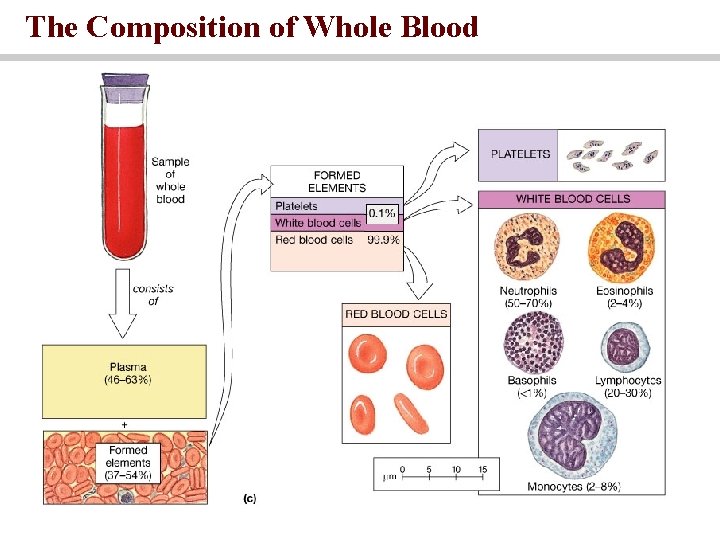
The Composition of Whole Blood
How Blood Is Produced • Adult production of 400 billion platelets, 200 billion RBCs, and 10 billion WBCs every day • Hemopoiesis—production of blood, especially its formed elements • Hemopoietic tissues produce blood cells • Yolk sac produces stem cells for first blood cells • Colonize fetal bone marrow, liver, spleen, and thymus • Liver stops producing blood cells at birth • Spleen remains involved with lymphocyte production
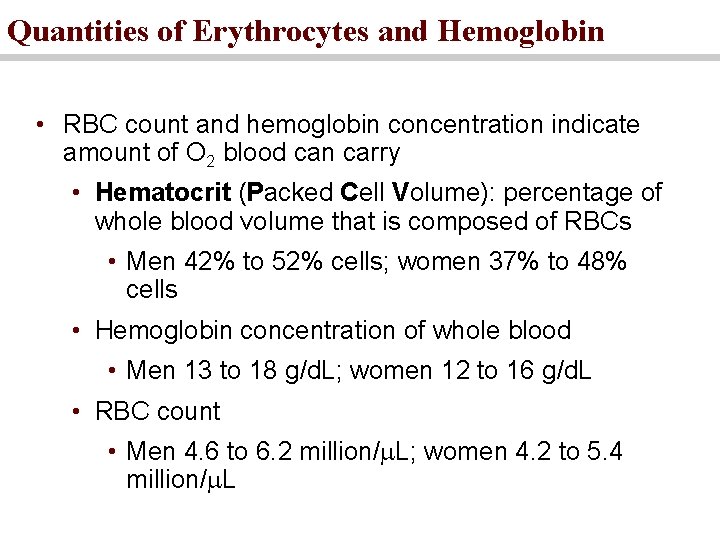
Quantities of Erythrocytes and Hemoglobin • RBC count and hemoglobin concentration indicate amount of O 2 blood can carry • Hematocrit (Packed Cell Volume): percentage of whole blood volume that is composed of RBCs • Men 42% to 52% cells; women 37% to 48% cells • Hemoglobin concentration of whole blood • Men 13 to 18 g/d. L; women 12 to 16 g/d. L • RBC count • Men 4. 6 to 6. 2 million/ L; women 4. 2 to 5. 4 million/ L
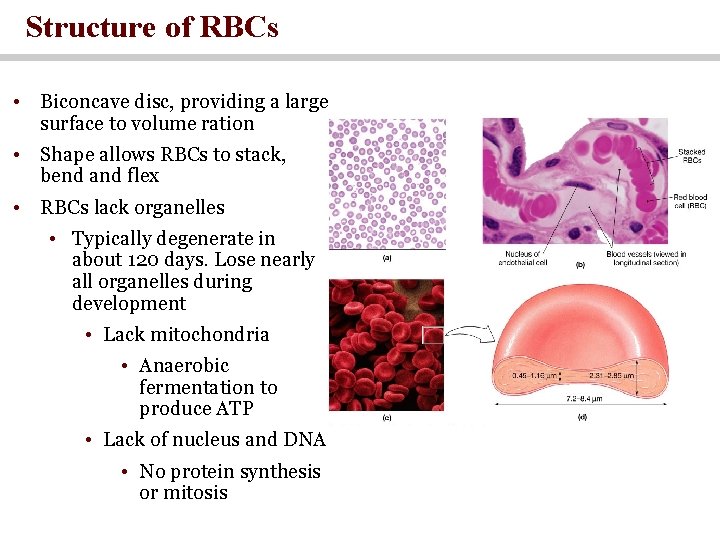
Structure of RBCs • Biconcave disc, providing a large surface to volume ration • Shape allows RBCs to stack, bend and flex • RBCs lack organelles • Typically degenerate in about 120 days. Lose nearly all organelles during development • Lack mitochondria • Anaerobic fermentation to produce ATP • Lack of nucleus and DNA • No protein synthesis or mitosis
Form and Function • Gas transport—major function • 33% of cytoplasm is hemoglobin (Hb) • 280 million hemoglobin molecules on one RBC • O 2 delivery to tissue and CO 2 transport to lungs • Carbonic anhydrase (CAH) in cytoplasm • Produces carbonic acid from CO 2 and water • Important role in gas transport and p. H balance
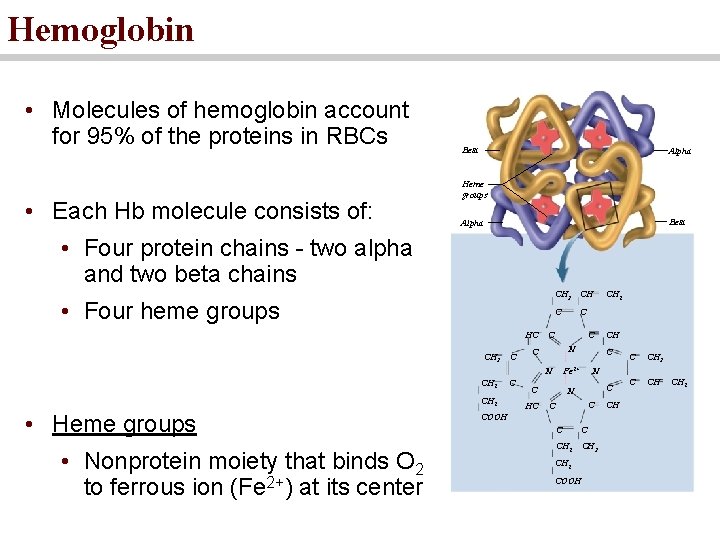
Hemoglobin • Molecules of hemoglobin account for 95% of the proteins in RBCs • Each Hb molecule consists of: Beta Alpha Heme groups Beta Alpha • Four protein chains - two alpha and two beta chains • Four heme groups HC CH 3 CH C C N CH 2 • Heme groups • Nonprotein moiety that binds O 2 to ferrous ion (Fe 2+) at its center C HC CH C Fe 2+ C CH 2 C CH 3 C CH N C C COOH C C CH 2 CH 3 CH 2 COOH CH CH 2
Anemia • Oxygen-carrying capacity is reduced Important types of anemia: • Aplastic anemia: decreased formation of both erythrocytes and hemoglobin synthesis; results from defective red bone marrow perhaps due to toxin, poisons, or radiation exposure • Iron-deficient anemia: Deficiency in iron uptake or use by the body • Pernicious anemia: Deficiency of Vitamin B 12 (failure to absorb vitamin B 12 due to the lack of an intrinsic factor that is secreted by stomach cells) • Hemorrhagic anemia: Results from heavy blood loss (chronic ulcer or prolonged menstrual cycle) • Macrocytic anemia: occurs when the average size of circulating erythrocytes is too large (caused by deficiencies of folic acid and vitamin B 12 ) • Sickle-cell anemia: is an autosomal recessive anemia. Erythrocytes becomes sickle shaped at a lower blood oxygen concentrations making them unable to flow efficiently and also more prone to hemolysis.
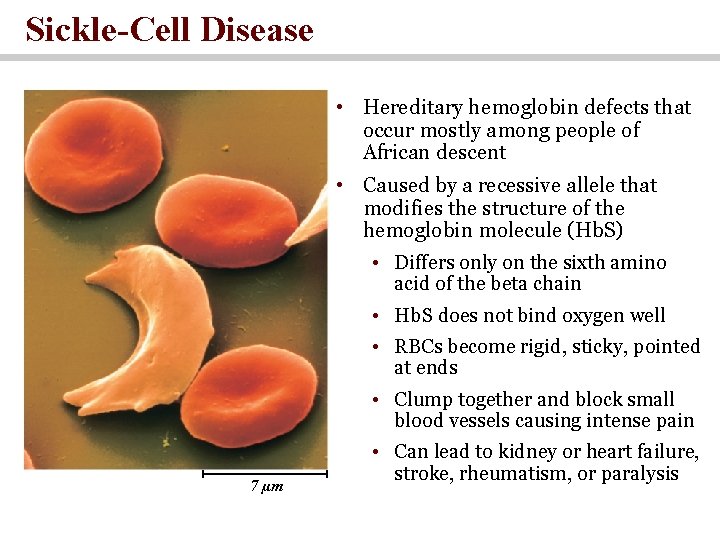
Sickle-Cell Disease • Hereditary hemoglobin defects that occur mostly among people of African descent • Caused by a recessive allele that modifies the structure of the hemoglobin molecule (Hb. S) • Differs only on the sixth amino acid of the beta chain • Hb. S does not bind oxygen well • RBCs become rigid, sticky, pointed at ends • Clump together and block small blood vessels causing intense pain 7 µm • Can lead to kidney or heart failure, stroke, rheumatism, or paralysis
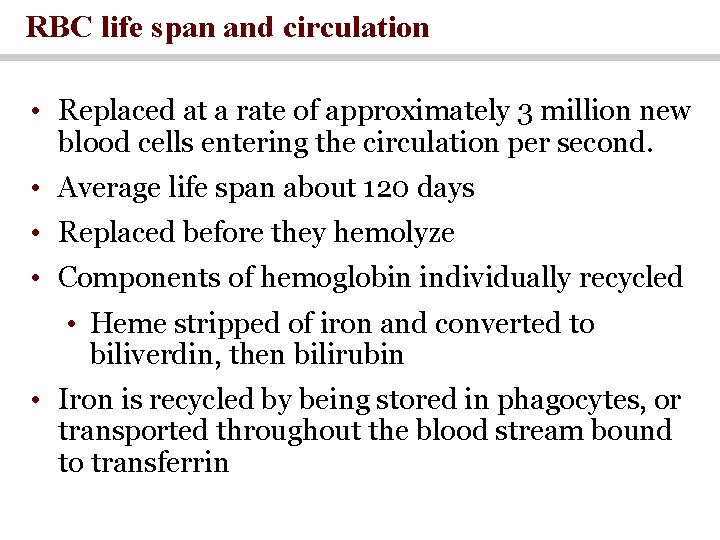
RBC life span and circulation • Replaced at a rate of approximately 3 million new blood cells entering the circulation per second. • Average life span about 120 days • Replaced before they hemolyze • Components of hemoglobin individually recycled • Heme stripped of iron and converted to biliverdin, then bilirubin • Iron is recycled by being stored in phagocytes, or transported throughout the blood stream bound to transferrin
Hemopoiesis • Process of blood cell formation • Hemocytoblasts are circulating stem cells that divide to form all types of blood cells • Whole blood from anywhere in the body has roughly the same temperature, p. H and viscosity
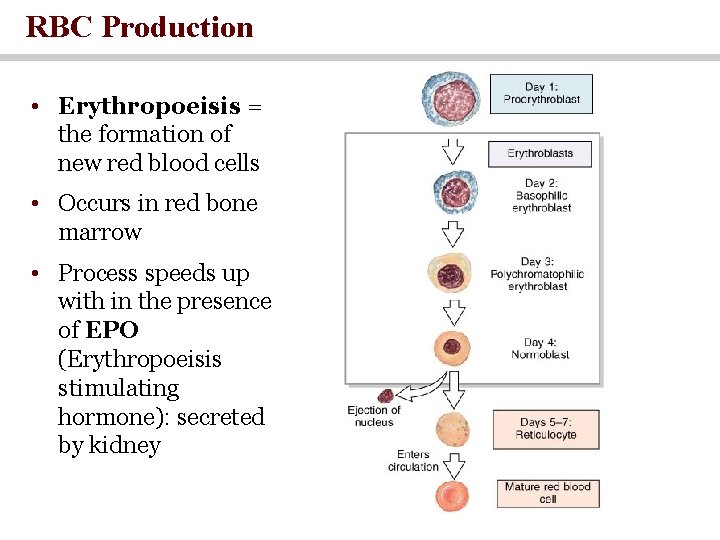
RBC Production • Erythropoeisis = the formation of new red blood cells • Occurs in red bone marrow • Process speeds up with in the presence of EPO (Erythropoeisis stimulating hormone): secreted by kidney
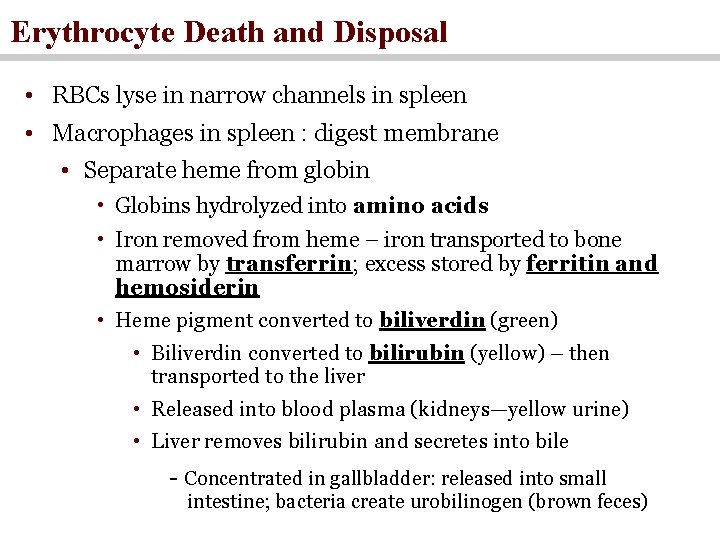
Erythrocyte Death and Disposal • RBCs lyse in narrow channels in spleen • Macrophages in spleen : digest membrane • Separate heme from globin • Globins hydrolyzed into amino acids • Iron removed from heme – iron transported to bone marrow by transferrin; excess stored by ferritin and hemosiderin • Heme pigment converted to biliverdin (green) • Biliverdin converted to bilirubin (yellow) – then transported to the liver • Released into blood plasma (kidneys—yellow urine) • Liver removes bilirubin and secretes into bile - Concentrated in gallbladder: released into small intestine; bacteria create urobilinogen (brown feces)
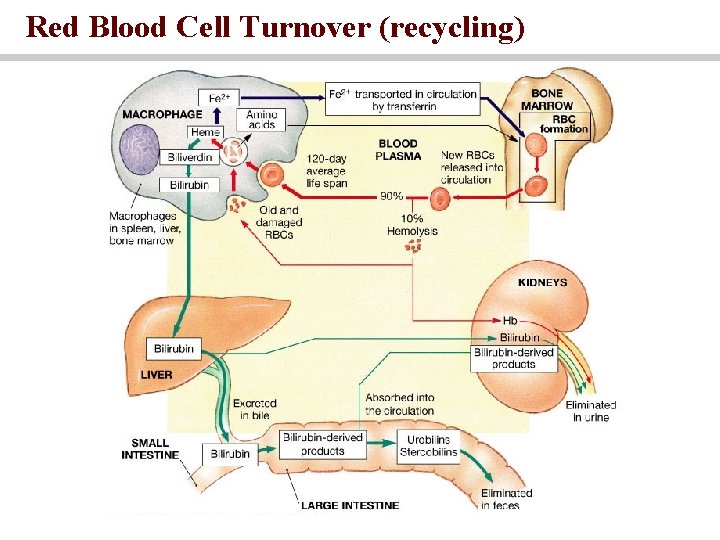
Red Blood Cell Turnover (recycling)
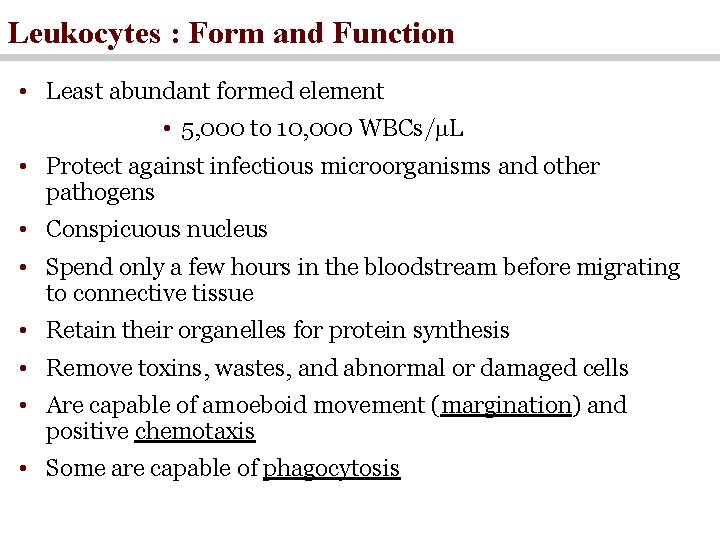
Leukocytes : Form and Function • Least abundant formed element • 5, 000 to 10, 000 WBCs/ L • Protect against infectious microorganisms and other pathogens • Conspicuous nucleus • Spend only a few hours in the bloodstream before migrating to connective tissue • Retain their organelles for protein synthesis • Remove toxins, wastes, and abnormal or damaged cells • Are capable of amoeboid movement (margination) and positive chemotaxis • Some are capable of phagocytosis
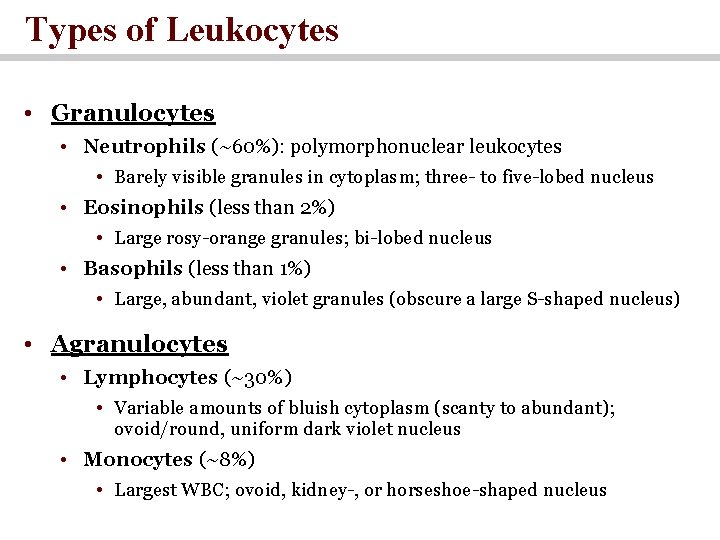
Types of Leukocytes • Granulocytes • Neutrophils (~60%): polymorphonuclear leukocytes • Barely visible granules in cytoplasm; three- to five-lobed nucleus • Eosinophils (less than 2%) • Large rosy-orange granules; bi-lobed nucleus • Basophils (less than 1%) • Large, abundant, violet granules (obscure a large S-shaped nucleus) • Agranulocytes • Lymphocytes (~30%) • Variable amounts of bluish cytoplasm (scanty to abundant); ovoid/round, uniform dark violet nucleus • Monocytes (~8%) • Largest WBC; ovoid, kidney-, or horseshoe-shaped nucleus
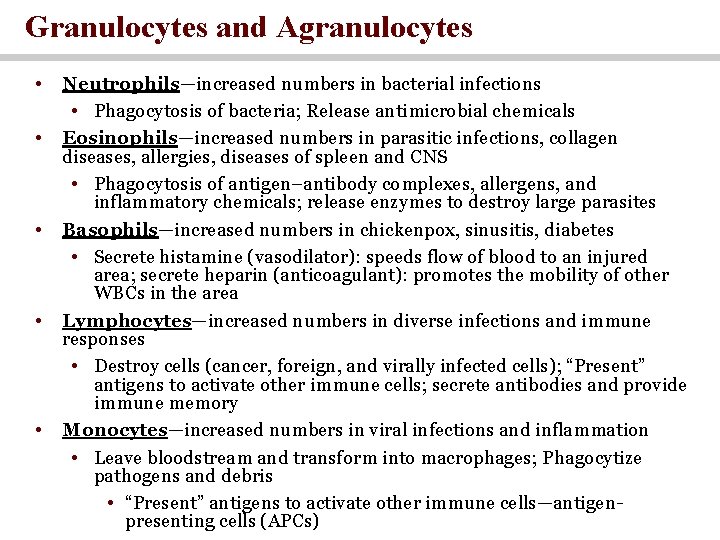
Granulocytes and Agranulocytes • • • Neutrophils—increased numbers in bacterial infections • Phagocytosis of bacteria; Release antimicrobial chemicals Eosinophils—increased numbers in parasitic infections, collagen diseases, allergies, diseases of spleen and CNS • Phagocytosis of antigen–antibody complexes, allergens, and inflammatory chemicals; release enzymes to destroy large parasites Basophils—increased numbers in chickenpox, sinusitis, diabetes • Secrete histamine (vasodilator): speeds flow of blood to an injured area; secrete heparin (anticoagulant): promotes the mobility of other WBCs in the area Lymphocytes—increased numbers in diverse infections and immune responses • Destroy cells (cancer, foreign, and virally infected cells); “Present” antigens to activate other immune cells; secrete antibodies and provide immune memory Monocytes—increased numbers in viral infections and inflammation • Leave bloodstream and transform into macrophages; Phagocytize pathogens and debris • “Present” antigens to activate other immune cells—antigenpresenting cells (APCs)
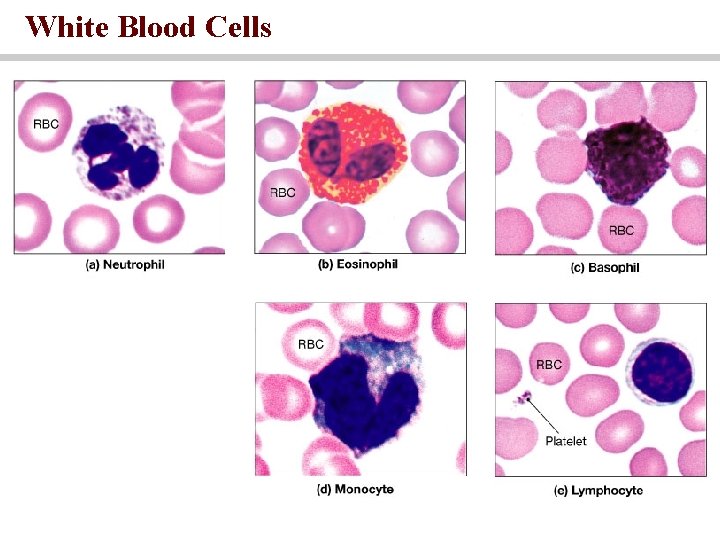
White Blood Cells
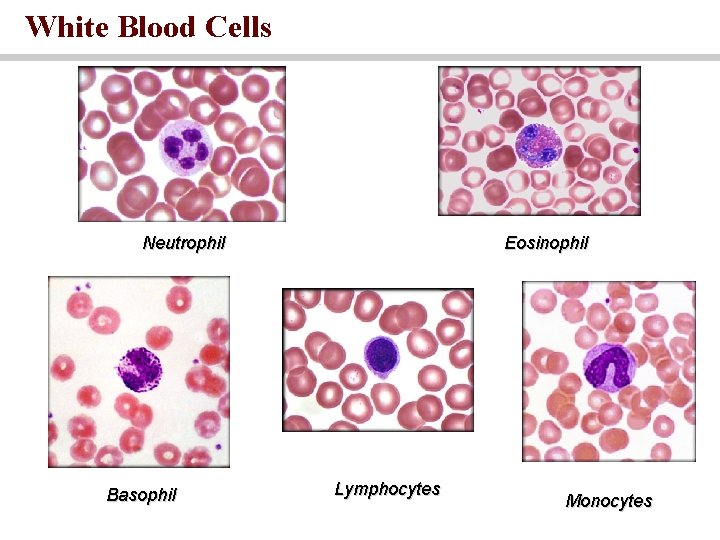
White Blood Cells Neutrophil Basophil Eosinophil Lymphocytes Monocytes
The Leukocyte Life Cycle • Leukopoiesis—production of white blood cells • Pluripotent stem cells (PPSCs) • Myeloblasts—form neutrophils, eosinophils, basophils • Monoblasts—form monocytes • Lymphoblasts give rise to all forms of lymphocytes
Platelets—small fragments of megakaryocyte cells Structure • Flattened discs • Circulate for 9 -12 days before being removed by phagocytes Function • Transporting chemicals important to clotting • Forming temporary patch in walls of damaged blood vessels • Contracting after a clot has formed • Normal platelet count— 130, 000 to 400, 000 platelets/�L
Numbers • Polycynthemia- excess RBC • Anemia- deficiency of RBCs • Leukopenia—low WBC count: < 5, 000/ L • Leukocytosis—high WBC count: >10, 000/ L • Leukemia - cancer of hemopoietic tissue that usually produces an extraordinary high number of circulating leukocytes and their precursors • Diferential WBC count: identifies what percentage of the total WBC count consist of each type of leukocyte • Thrombocytopenia – deficiency in platelets count • Thrombocytosis- high platelets count
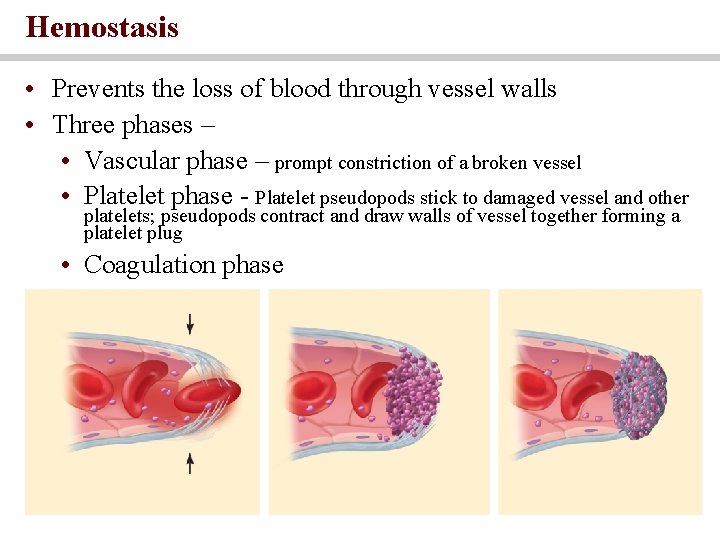
Hemostasis • Prevents the loss of blood through vessel walls • Three phases – • Vascular phase – prompt constriction of a broken vessel • Platelet phase - Platelet pseudopods stick to damaged vessel and other platelets; pseudopods contract and draw walls of vessel together forming a platelet plug • Coagulation phase
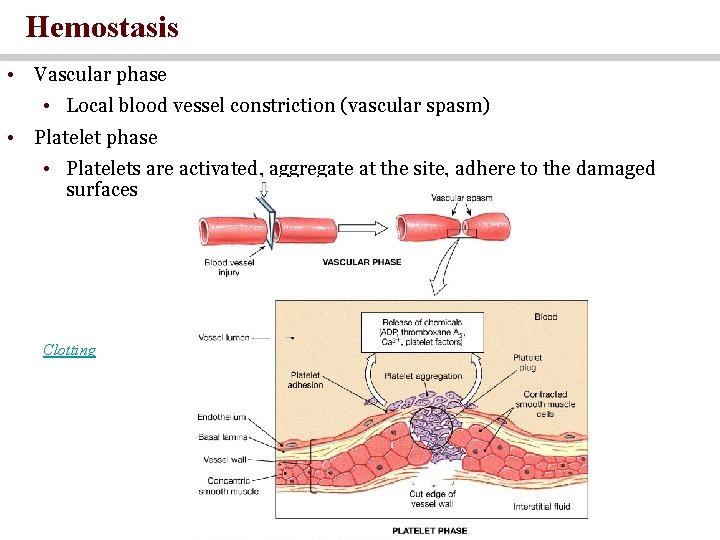
Hemostasis • Vascular phase • Local blood vessel constriction (vascular spasm) • Platelet phase • Platelets are activated, aggregate at the site, adhere to the damaged surfaces Clotting
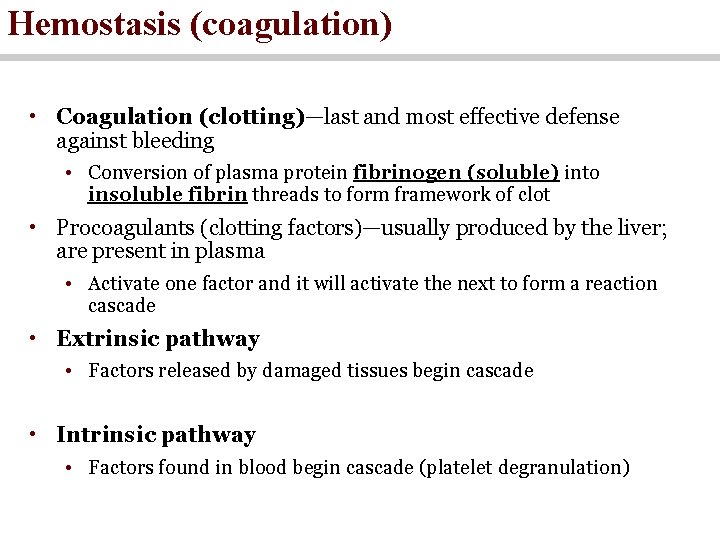
Hemostasis (coagulation) • Coagulation (clotting)—last and most effective defense against bleeding • Conversion of plasma protein fibrinogen (soluble) into insoluble fibrin threads to form framework of clot • Procoagulants (clotting factors)—usually produced by the liver; are present in plasma • Activate one factor and it will activate the next to form a reaction cascade • Extrinsic pathway • Factors released by damaged tissues begin cascade • Intrinsic pathway • Factors found in blood begin cascade (platelet degranulation)
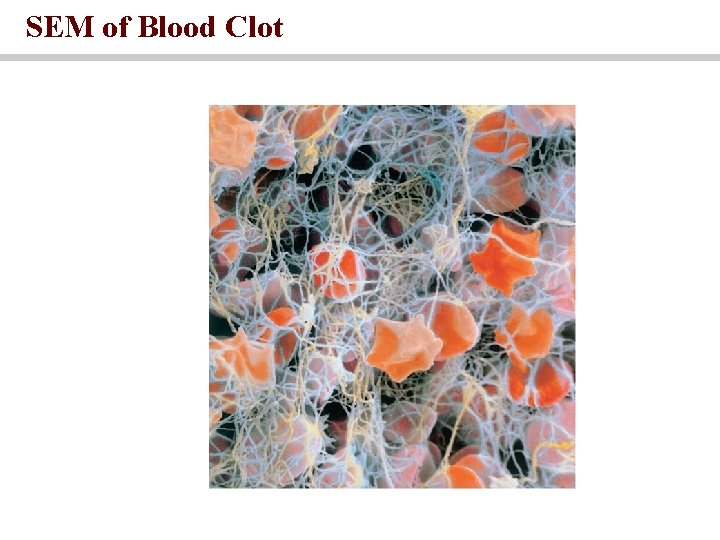
SEM of Blood Clot
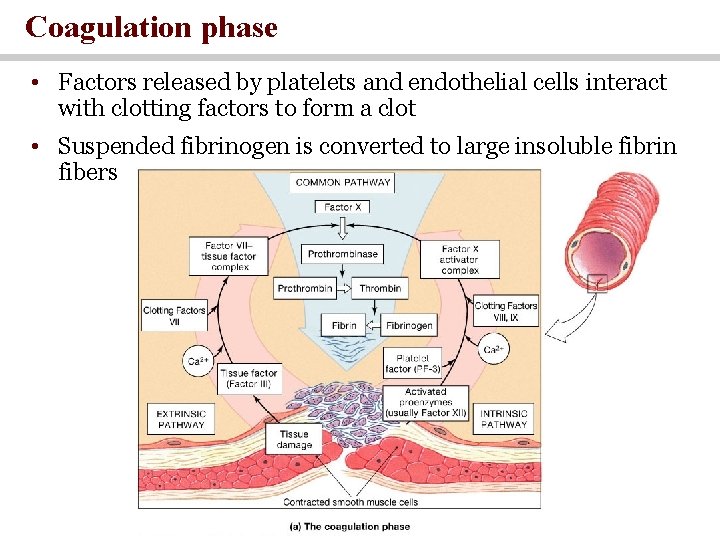
Coagulation phase • Factors released by platelets and endothelial cells interact with clotting factors to form a clot • Suspended fibrinogen is converted to large insoluble fibrin fibers
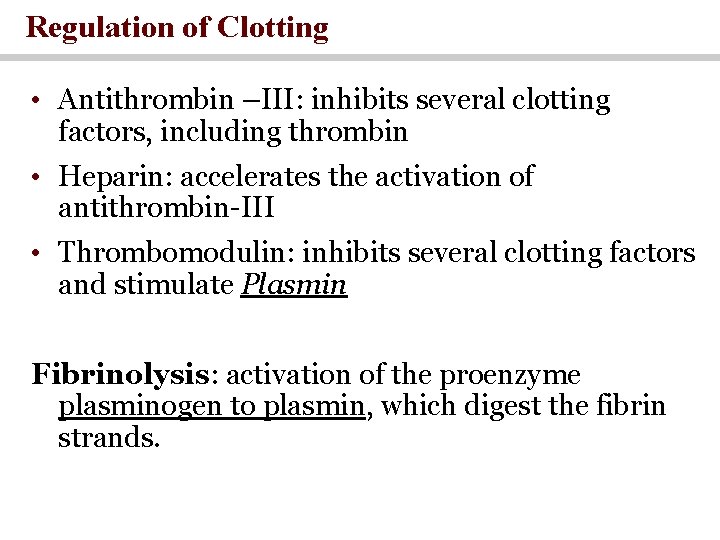
Regulation of Clotting • Antithrombin –III: inhibits several clotting factors, including thrombin • Heparin: accelerates the activation of antithrombin-III • Thrombomodulin: inhibits several clotting factors and stimulate Plasmin Fibrinolysis: activation of the proenzyme plasminogen to plasmin, which digest the fibrin strands.
Blood Types • Antigens • Complex molecules on surface of cell membrane that are unique to the individual • Used to distinguish self from foreign matter • Foreign antigens generate an immune response • Antibodies • Proteins (gamma globulins) secreted by plasma cells • Part of immune response to foreign matter • Bind to antigens and mark them for destruction • Forms antigen–antibody complexes • Agglutinins—antibodies in the plasma that bring about transfusion mismatch • Agglutination • Antibody molecule binding to antigens • Causes clumping of red blood cells
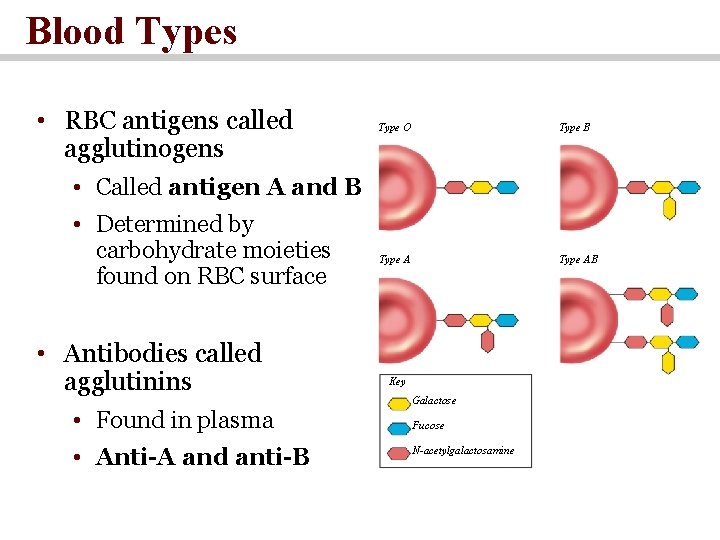
Blood Types • RBC antigens called agglutinogens Type O Type B • Called antigen A and B • Determined by carbohydrate moieties found on RBC surface • Antibodies called agglutinins • Found in plasma • Anti-A and anti-B leaves Type AB Key Galactose Fucose N-acetylgalactosamine
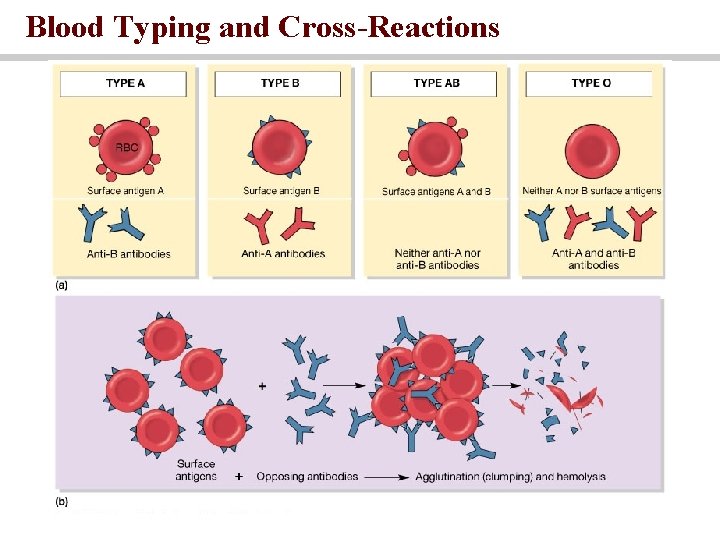
Blood Typing and Cross-Reactions
The ABO Group • Your ABO blood type is determined by presence or absence of antigens (agglutinogens) on RBCs • Blood type A person has A antigens • Blood type B person has B antigens • Blood type AB has both A and B antigens • Blood type O person has neither antigen • Most common: type O (universal donor) • Rarest: type AB (universal recipient)
The Rh Group • Rh (C, D, E) agglutinogens discovered in rhesus monkey in 1940 • Rh D is the most reactive and a patient is considered blood type Rh+ if having D antigen (agglutinogens) on RBCs • Rh frequencies vary among ethnic groups • Anti-D agglutinins not normally present • Form in Rh- individuals exposed to Rh+ blood • Rh- woman with an Rh+ fetus or transfusion of Rh+ blood • No problems with first transfusion or pregnancy 18 -38
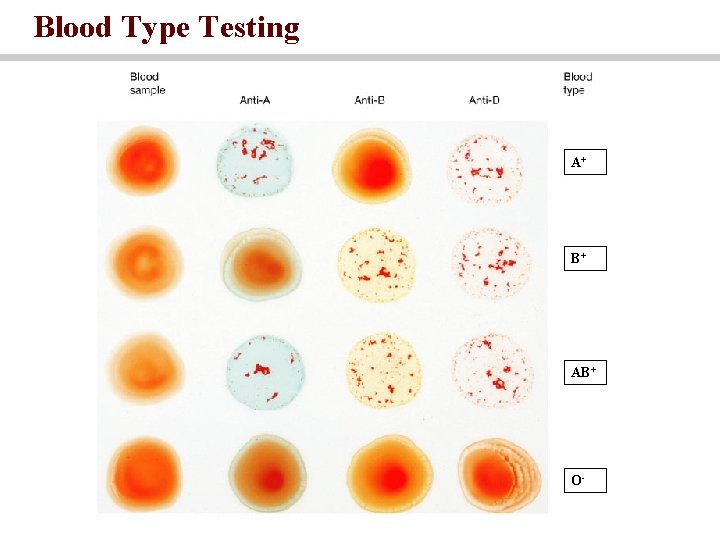
Blood Type Testing A+ B+ AB+ O-
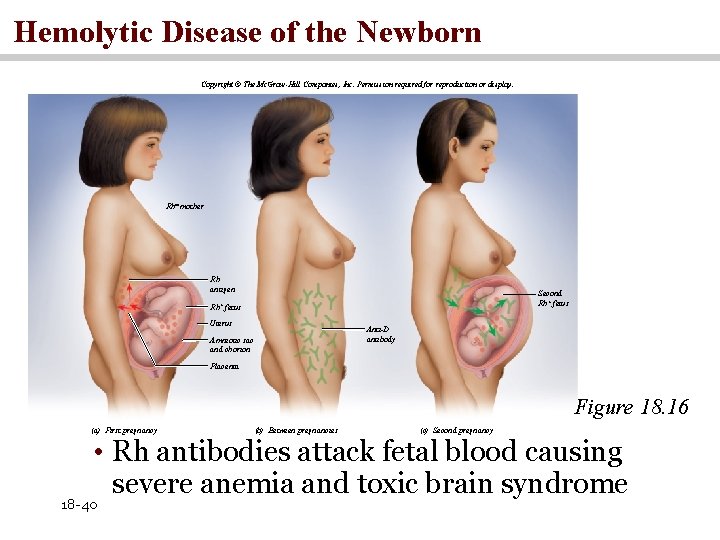
Hemolytic Disease of the Newborn Copyright © The Mc. Graw-Hill Companies, Inc. Permission required for reproduction or display. leaves Rh- mother Rh antigen Second Rh+ fetus Uterus Anti-D antibody Amniotic sac and chorion Placenta Figure 18. 16 (a) First pregnancy (b) Between pregnancies (c) Second pregnancy • Rh antibodies attack fetal blood causing severe anemia and toxic brain syndrome 18 -40
The Rh Group • Occurs if Rh- mother has formed antibodies and is pregnant with second Rh+ child • Anti-D antibodies can cross placenta • Prevention • Rho. GAM given to pregnant Rh- women • Binds fetal agglutinogens in her blood so she will not form anti-D antibodies
- Slides: 41