BLEEDING DISORDERS HEMOSTASIS 1 VASCULAR PHASE 2 PLATELET
BLEEDING DISORDERS

HEMOSTASIS 1. VASCULAR PHASE 2. PLATELET PHASE 3. COAGULATION PHASE 4. FIBRINOLYTIC PHASE

Lab Tests Hemostasis BV Injury Tissue Factor • CBC-Plt • BT, (CT) • PTT Neural Blood Vessel Constriction Platelet Aggregation Coagulation Cascade Primary hemostatic plug Reduced Blood flow Platelet Activation Fibrin formation Plt Study Stable Hemostatic Plug Morphology Function Antibody
NORMAL CLOTTING Response to vessle injury 1. Vasoconstriction to reduce blood flow 2. Platelet plug formation (von willebrand factor binds damaged vessle and platelets) 3. Activation of clotting cascade with generation of fibrin clot formation 4. Fibrinlysis (clot breakdown)
CLOTTING CASCADE Normally the ingredients, called factors, act like a row of dominoes toppling against each other to create a chain reaction. If one of the factors is missing this chain reaction cannot proceed.

VASCULAR PHASE WHEN A BLOOD VESSEL IS DAMAGED, VASOCONSTRICTION RESULTS.

PLATELET PHASE PLATELETS ADHERE TO THE DAMAGED SURFACE AND FORM A TEMPORARY PLUG.

COAGULATION PHASE The clotting cascade occurs through two separate pathways that interact, the intrinsic and the extrinsic pathway. Till conversion of fibrinogen to fibrin is complete
Extrinsic Pathway n The extrinsic pathway is activated by external trauma that causes blood to escape from the vascular system. This pathway is quicker than the intrinsic pathway. It involves factor VII.
Intrinsic Pathway n The intrinsic pathway is activated by trauma inside the vascular system, and is activated by platelets, exposed endothelium, chemicals, or collagen. This pathway is slower than the extrinsic pathway, but more important. It involves factors XII, XI, IX, VIII.
Common Pathway n Both pathways meet and finish the pathway of clot production in what is known as the common pathway. The common pathway involves factors I, II, V, and X.
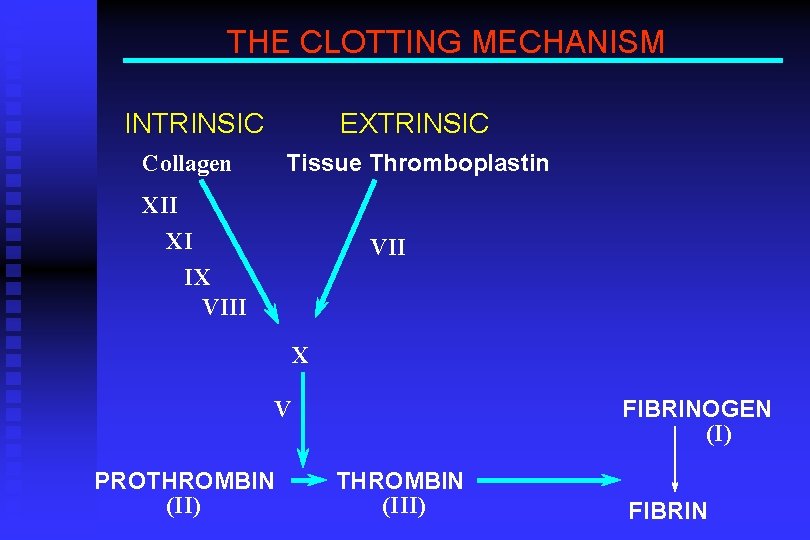
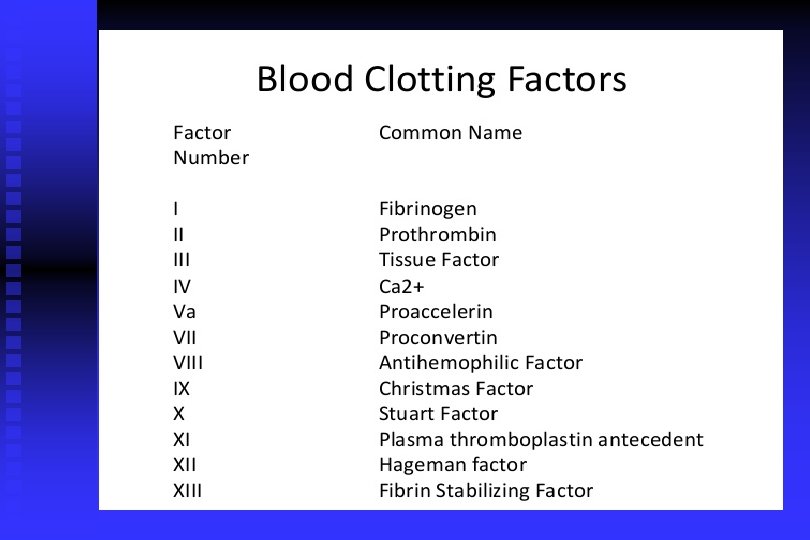
THE CLOTTING MECHANISM INTRINSIC EXTRINSIC Collagen Tissue Thromboplastin XII XI IX VIII VII X FIBRINOGEN (I) V PROTHROMBIN (II) THROMBIN (III) FIBRIN
FIBRINOLYTIC PHASE ANTICLOTTING MECHANISMS ARE ACTIVATED TO ALLOW CLOT DISINTEGRATION AND REPAIR OF THE DAMAGED VESSEL.
HEMOSTASIS DEPENDENT UPON: ¬ Vessel Wall Integrity Adequate Numbers of Platelets ® Proper Functioning Platelets ¯ Adequate Levels of Clotting Factors ° Proper Function of Fibrinolytic Pathway
LABORATORY EVALUATION n PLATELET COUNT n BLEEDING TIME (BT) n PROTHROMBIN TIME (PT) n PARTIAL THROMBOPLASTIN TIME (PTT) n THROMBIN TIME (TT)
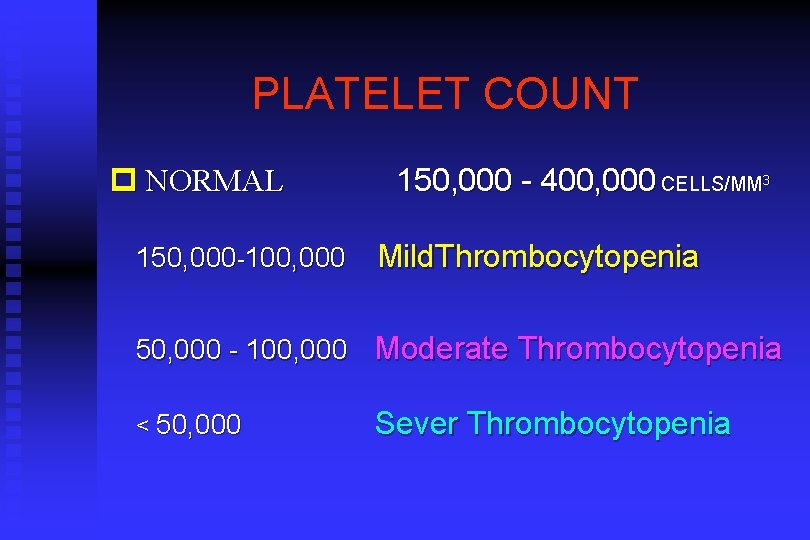
PLATELET COUNT p NORMAL 150, 000 -100, 000 150, 000 - 400, 000 CELLS/MM 3 Mild. Thrombocytopenia 50, 000 - 100, 000 Moderate Thrombocytopenia < 50, 000 Sever Thrombocytopenia
BLEEDING TIME l PROVIDES ASSESSMENT OF PLATELET COUNT AND FUNCTION l Is also affected by certain vascular disorders NORMAL VALUE 2 -8 MINUTES
PROTHROMBIN TIME(PT) l Measures Effectiveness of the Extrinsic Pathway l Mnemonic - PET NORMAL VALUE 12 -13 SECS
International normalized ratio(INR) The INR is the ratio of a patient's prothrombin time to a normal (control) sample. n the INR in absence of anticoagulation therapy is 0. 8 -1. 2. n
PARTIAL THROMBOPLASTIN TIME l Measures Effectiveness of the Intrinsic Pathway l Mnemonic - PITT NORMAL VALUE 25 -40 SECS
THROMBIN TIME l Time for Thrombin To Convert Fibrinogen Fibrin l A Measure of Fibrinolytic Pathway NORMAL VALUE 12 -14 SECS
So What Causes Bleeding Disorders? p. VESSEL DEFECTS p. PLATELET DISORDERS p. COAGULATION FACTOR DEFICIENCIES p. OTHER DISORDERS
Clinical picture Petichea , purpura, Echymosis. n Spontaneous Gingival bleeding n Bleeding after bruching n Prolonged after extraction n Excessive after minor trauma n Epistaxis, hematemesis, melena, hemoptysis, hemarthrosis. n

Petechiae: a haemorrhagic punctate spots in skin 1 -2 mm in diameter

Purpura : red spots on skin 3 -10 mm in diameter
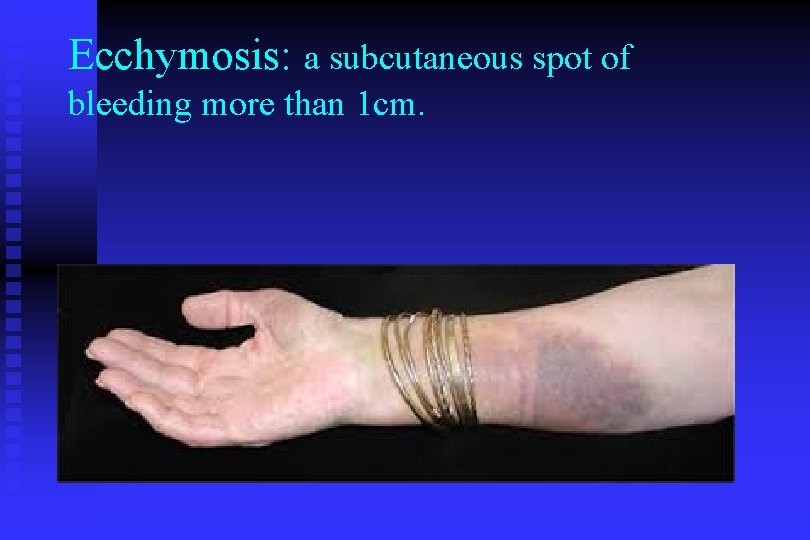
Ecchymosis: a subcutaneous spot of bleeding more than 1 cm.
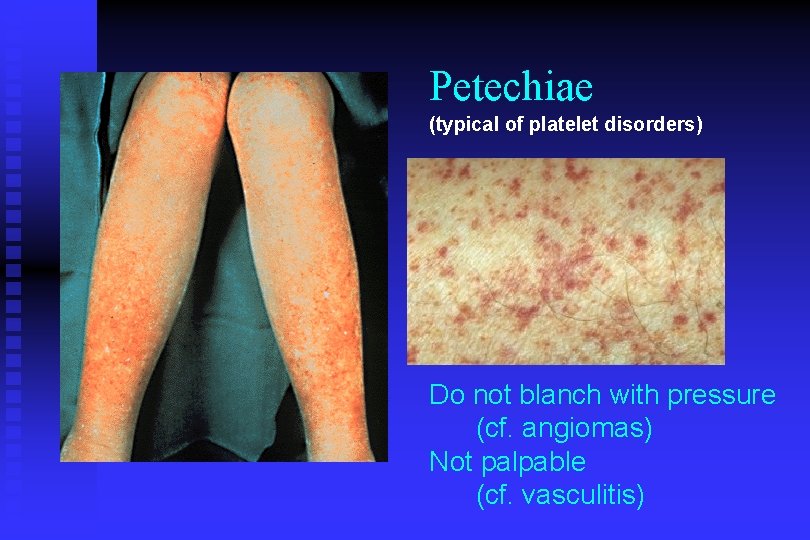
Petechiae (typical of platelet disorders) Do not blanch with pressure (cf. angiomas) Not palpable (cf. vasculitis)

Platelet Petechiae, Purpura Coagulation Hematoma, Joint bl.

Hemarthrosis : bleeding inside joint

Hematoma

VESSEL DEFECTS q Congenital : - Ehler Danlos syndrome q Acquired : - Vitamin c deficiency(scurvy) - steroid. - senile purpura. - Henoch-Schonlein purpura(vasculitis). - Infection ( viral- Bacterial).

PLATELET DISORDERS p THROMBOCYTOPENIA p THROMBOCYTOPATHY
THROMBOCYTOPENIA INADEQUATE NUMBER OF PLATELETS
THROMBOCYTOPATHY ADEQUATE NUMBER BUT ABNORMAL FUNCTION

THROMBOCYTOPATHY l l UREMIA ( Renal Failure) INHERITED DISORDERS MYELOPROLIFERATIVE DISORDERS DRUG INDUCED (Clopidogrel, Aspirin)
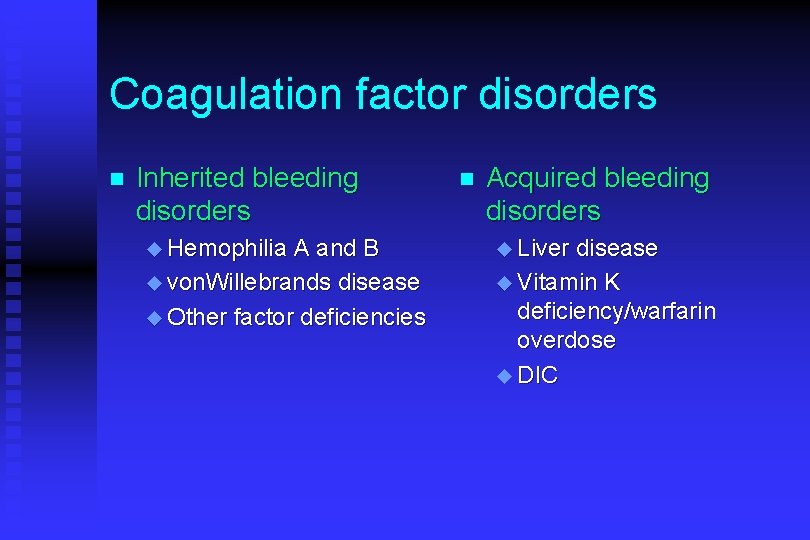
Coagulation factor disorders n Inherited bleeding disorders u Hemophilia A and B u von. Willebrands disease u Other factor deficiencies n Acquired bleeding disorders u Liver disease u Vitamin K deficiency/warfarin overdose u DIC
Coagulation Factor DEFICIENCIES (CONGENITAL) p HEMOPHILIA A p HEMOPHILIA B p von WILLEBRAND’S DISEASE
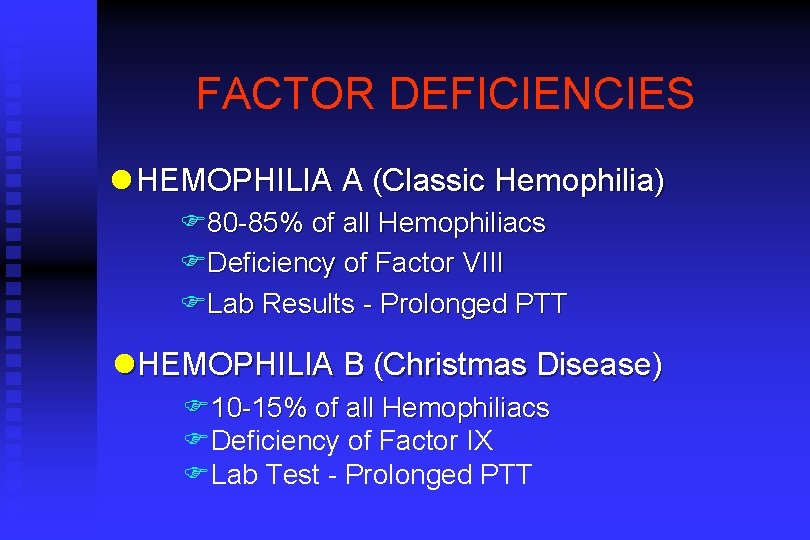
FACTOR DEFICIENCIES l HEMOPHILIA A (Classic Hemophilia) F 80 -85% of all Hemophiliacs FDeficiency of Factor VIII FLab Results - Prolonged PTT l. HEMOPHILIA B (Christmas Disease) F 10 -15% of all Hemophiliacs FDeficiency of Factor IX FLab Test - Prolonged PTT
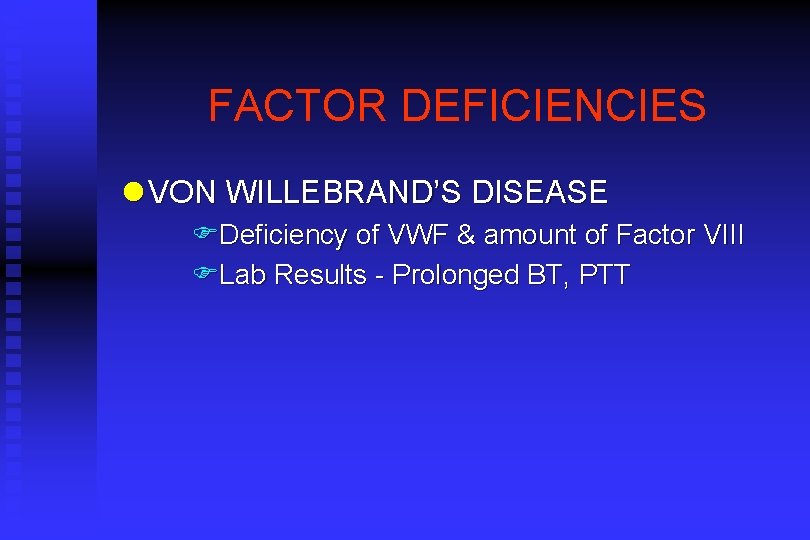
FACTOR DEFICIENCIES l VON WILLEBRAND’S DISEASE FDeficiency of VWF & amount of Factor VIII FLab Results - Prolonged BT, PTT
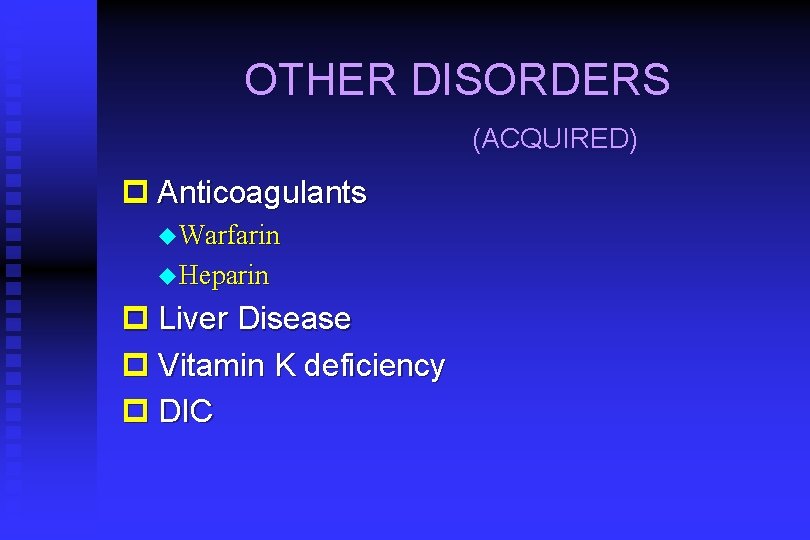
OTHER DISORDERS (ACQUIRED) p Anticoagulants u Warfarin u Heparin p Liver Disease p Vitamin K deficiency p DIC
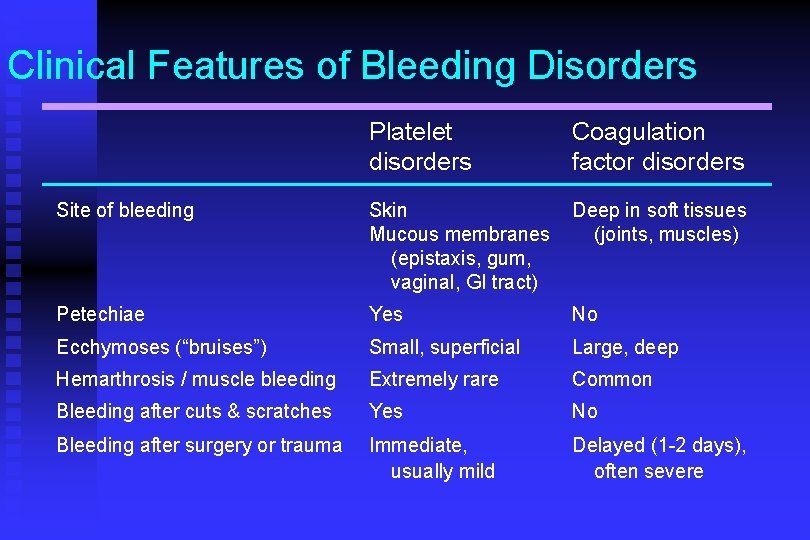
Clinical Features of Bleeding Disorders Platelet disorders Coagulation factor disorders Site of bleeding Skin Mucous membranes (epistaxis, gum, vaginal, GI tract) Deep in soft tissues (joints, muscles) Petechiae Yes No Ecchymoses (“bruises”) Small, superficial Large, deep Hemarthrosis / muscle bleeding Extremely rare Common Bleeding after cuts & scratches Yes No Bleeding after surgery or trauma Immediate, usually mild Delayed (1 -2 days), often severe
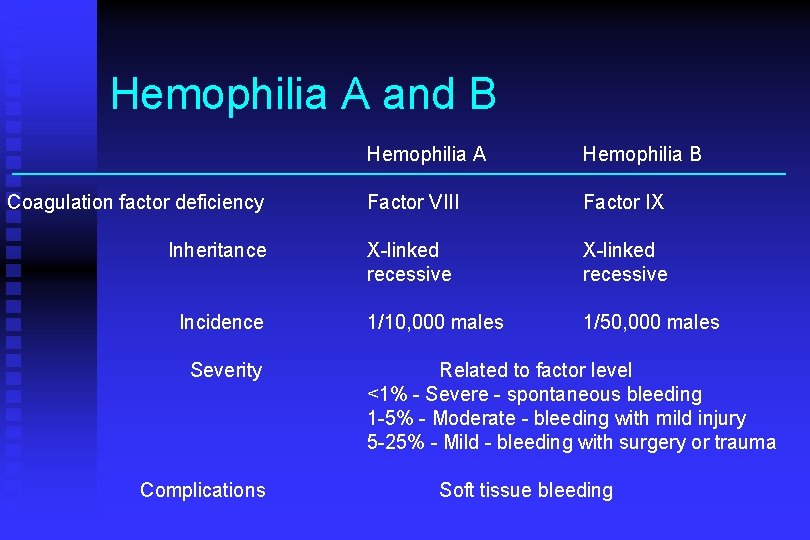
Hemophilia A and B Coagulation factor deficiency Inheritance Incidence Severity Complications Hemophilia A Hemophilia B Factor VIII Factor IX X-linked recessive 1/10, 000 males 1/50, 000 males Related to factor level <1% - Severe - spontaneous bleeding 1 -5% - Moderate - bleeding with mild injury 5 -25% - Mild - bleeding with surgery or trauma Soft tissue bleeding

Hemophilia Clinical manifestations (hemophilia A & B are indistinguishable) Hemarthrosis (most common) Fixed joints Soft tissue hematomas (e. g. , muscle) Muscle atrophy Shortened tendons Other sites of bleeding Urinary tract CNS, neck (may be life-threatening) Prolonged bleeding after surgery or dental extractions

Treatment of hemophilia A Recombinant factor VIII n Cryopreciptate n
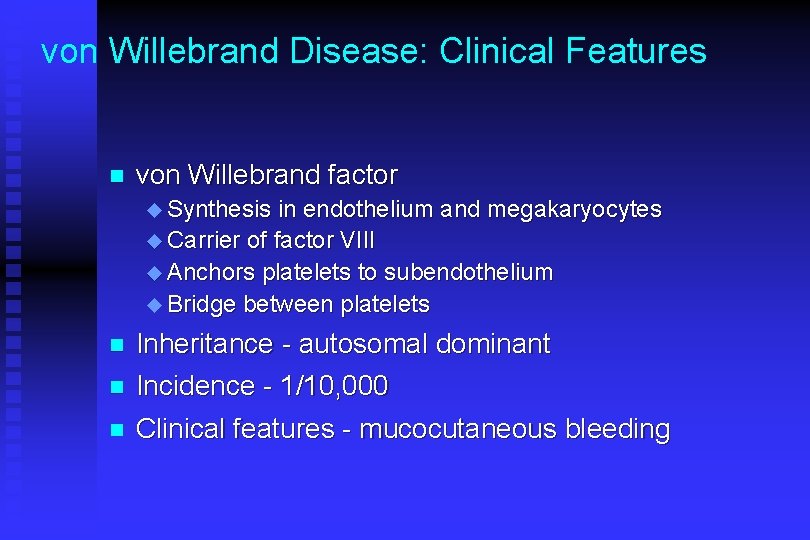
von Willebrand Disease: Clinical Features n von Willebrand factor u Synthesis in endothelium and megakaryocytes u Carrier of factor VIII u Anchors platelets to subendothelium u Bridge between platelets n Inheritance - autosomal dominant Incidence - 1/10, 000 n Clinical features - mucocutaneous bleeding n

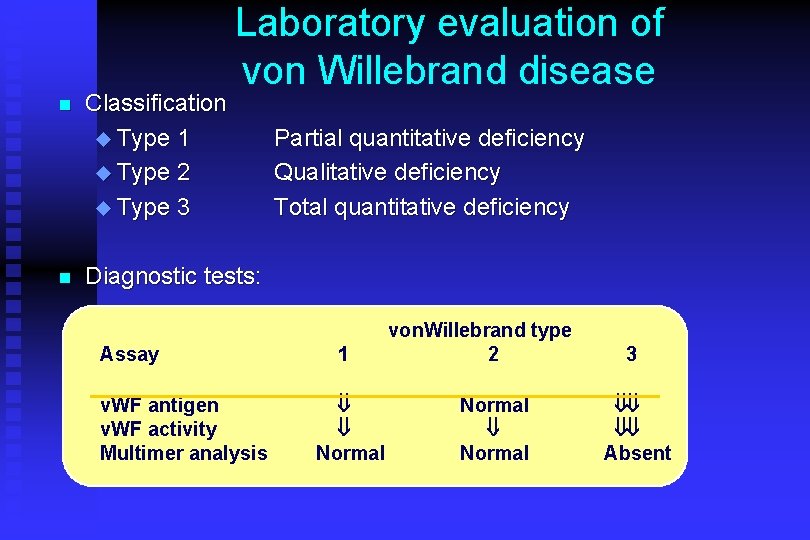
n n Classification u Type 1 u Type 2 u Type 3 Laboratory evaluation of von Willebrand disease Partial quantitative deficiency Qualitative deficiency Total quantitative deficiency Diagnostic tests: Assay v. WF antigen v. WF activity Multimer analysis 1 ß ß Normal von. Willebrand type 2 Normal ß Normal 3 ßß ßß Absent
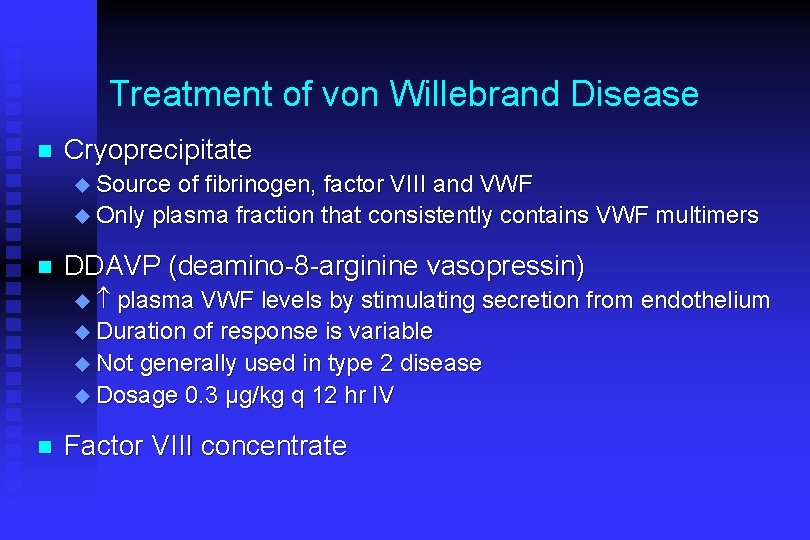
Treatment of von Willebrand Disease n Cryoprecipitate u Source of fibrinogen, factor VIII and VWF u Only plasma fraction that consistently contains VWF multimers n DDAVP (deamino-8 -arginine vasopressin) u plasma VWF levels by stimulating secretion from endothelium u Duration of response is variable u Not generally used in type 2 disease u Dosage 0. 3 µg/kg q 12 hr IV n Factor VIII concentrate
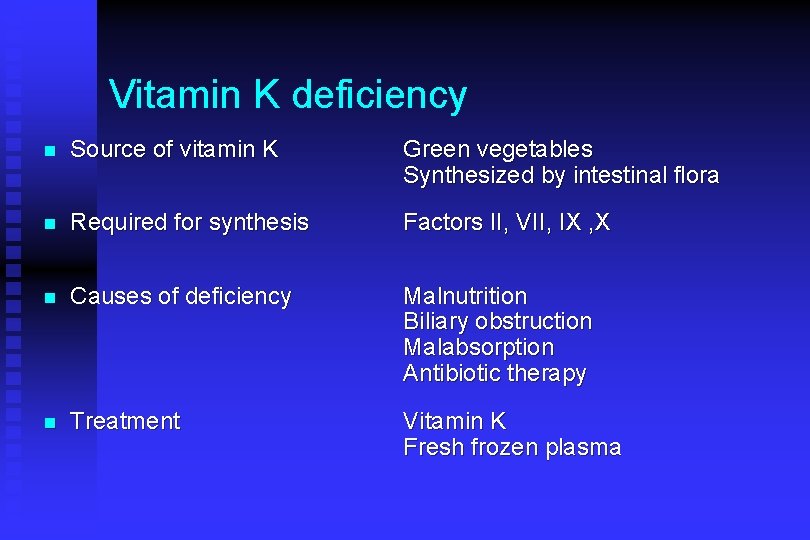
Vitamin K deficiency n Source of vitamin K Green vegetables Synthesized by intestinal flora n Required for synthesis Factors II, VII, IX , X n Causes of deficiency Malnutrition Biliary obstruction Malabsorption Antibiotic therapy n Treatment Vitamin K Fresh frozen plasma
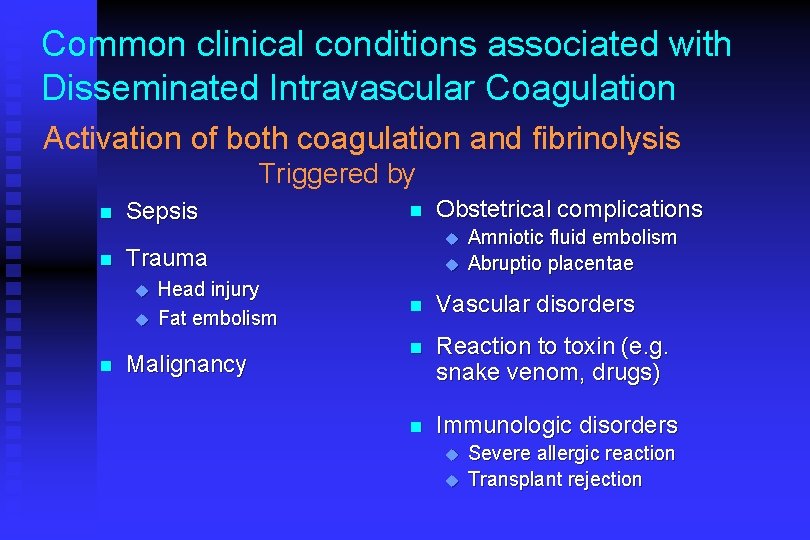
Common clinical conditions associated with Disseminated Intravascular Coagulation Activation of both coagulation and fibrinolysis Triggered by n n Sepsis u Head injury Fat embolism Malignancy Obstetrical complications u Trauma u n n u Amniotic fluid embolism Abruptio placentae n Vascular disorders n Reaction to toxin (e. g. snake venom, drugs) n Immunologic disorders u u Severe allergic reaction Transplant rejection
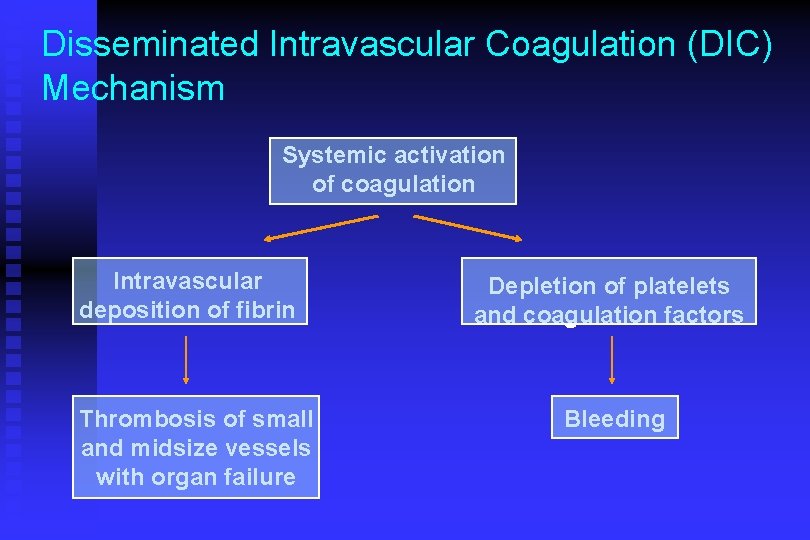
Disseminated Intravascular Coagulation (DIC) Mechanism Systemic activation of coagulation Intravascular deposition of fibrin Thrombosis of small and midsize vessels with organ failure Depletion of platelets and coagulation factors Bleeding
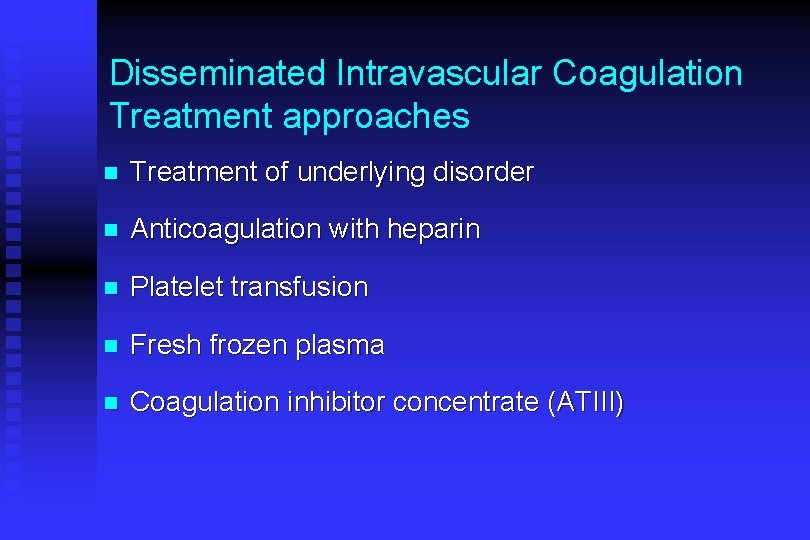
Disseminated Intravascular Coagulation Treatment approaches n Treatment of underlying disorder n Anticoagulation with heparin n Platelet transfusion n Fresh frozen plasma n Coagulation inhibitor concentrate (ATIII)
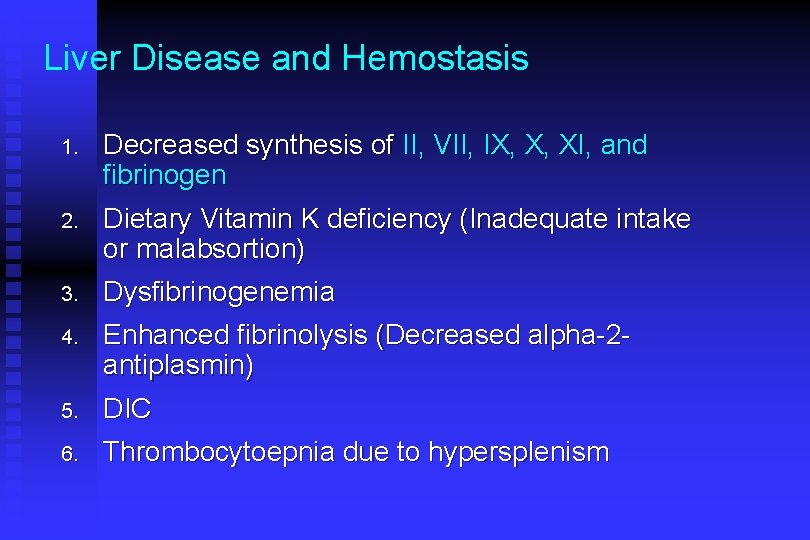
Liver Disease and Hemostasis 1. Decreased synthesis of II, VII, IX, X, XI, and fibrinogen 2. Dietary Vitamin K deficiency (Inadequate intake or malabsortion) 3. Dysfibrinogenemia 4. Enhanced fibrinolysis (Decreased alpha-2 antiplasmin) 5. DIC 6. Thrombocytoepnia due to hypersplenism
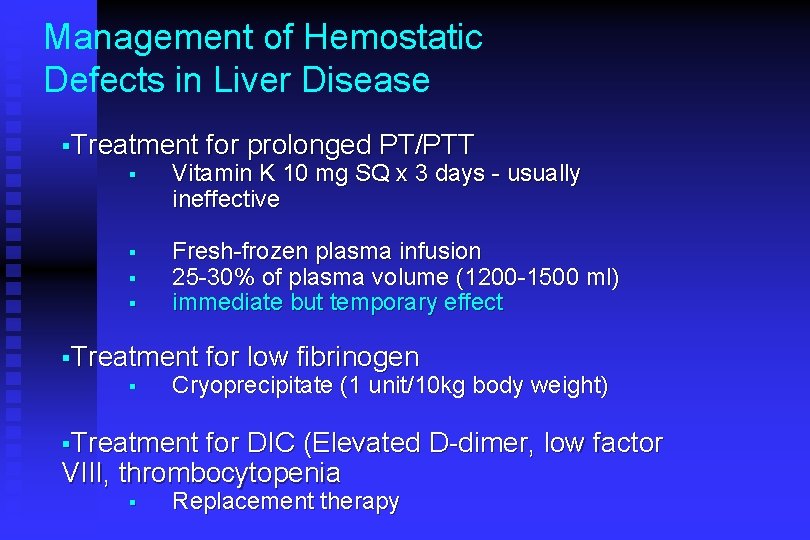
Management of Hemostatic Defects in Liver Disease §Treatment for prolonged PT/PTT § Vitamin K 10 mg SQ x 3 days - usually ineffective § § § Fresh-frozen plasma infusion 25 -30% of plasma volume (1200 -1500 ml) immediate but temporary effect §Treatment § for low fibrinogen Cryoprecipitate (1 unit/10 kg body weight) §Treatment for DIC (Elevated D-dimer, low factor VIII, thrombocytopenia § Replacement therapy
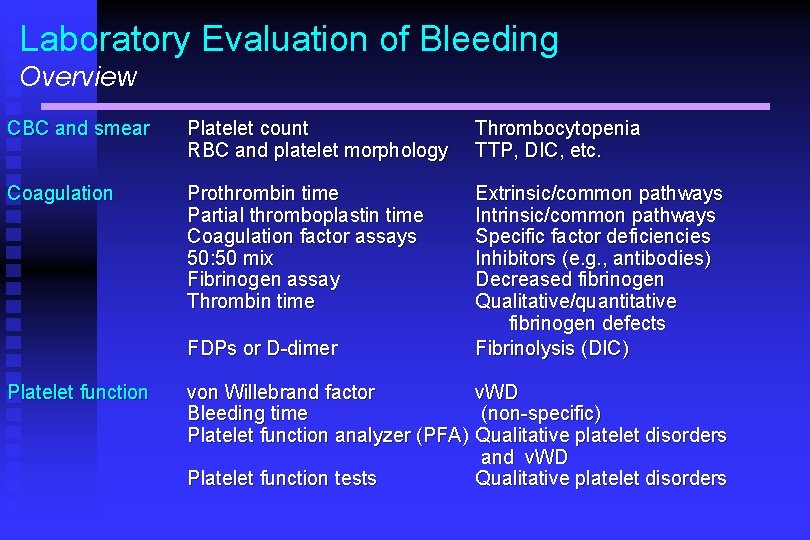
Laboratory Evaluation of Bleeding Overview CBC and smear Platelet count RBC and platelet morphology Thrombocytopenia TTP, DIC, etc. Coagulation Prothrombin time Partial thromboplastin time Coagulation factor assays 50: 50 mix Fibrinogen assay Thrombin time Extrinsic/common pathways Intrinsic/common pathways Specific factor deficiencies Inhibitors (e. g. , antibodies) Decreased fibrinogen Qualitative/quantitative fibrinogen defects Fibrinolysis (DIC) FDPs or D-dimer Platelet function von Willebrand factor v. WD Bleeding time (non-specific) Platelet function analyzer (PFA) Qualitative platelet disorders and v. WD Platelet function tests Qualitative platelet disorders
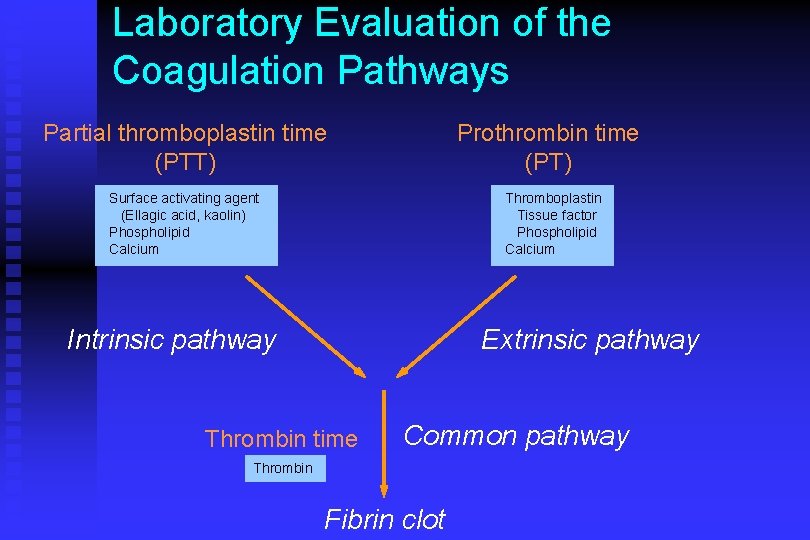
Laboratory Evaluation of the Coagulation Pathways Partial thromboplastin time (PTT) Prothrombin time (PT) Surface activating agent (Ellagic acid, kaolin) Phospholipid Calcium Thromboplastin Tissue factor Phospholipid Calcium Intrinsic pathway Extrinsic pathway Thrombin time Common pathway Thrombin Fibrin clot
n Drugs and blood products used for management of bleeding
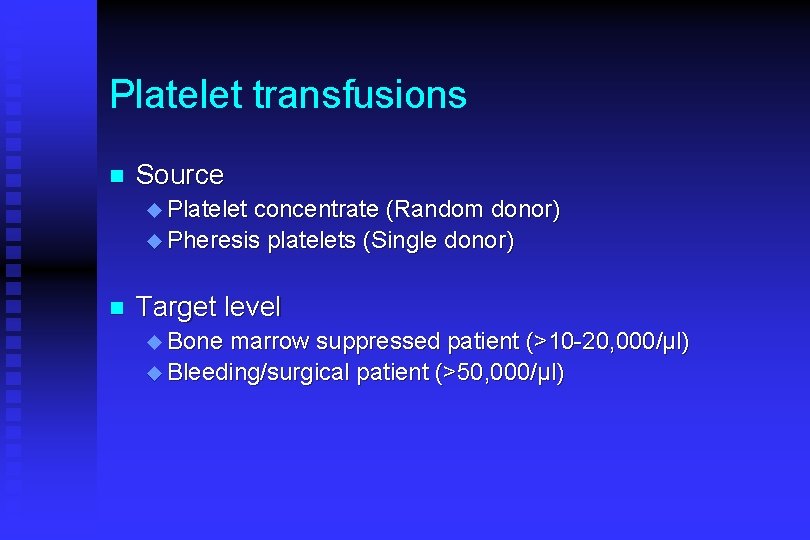
Platelet transfusions n Source u Platelet concentrate (Random donor) u Pheresis platelets (Single donor) n Target level u Bone marrow suppressed patient (>10 -20, 000/µl) u Bleeding/surgical patient (>50, 000/µl)
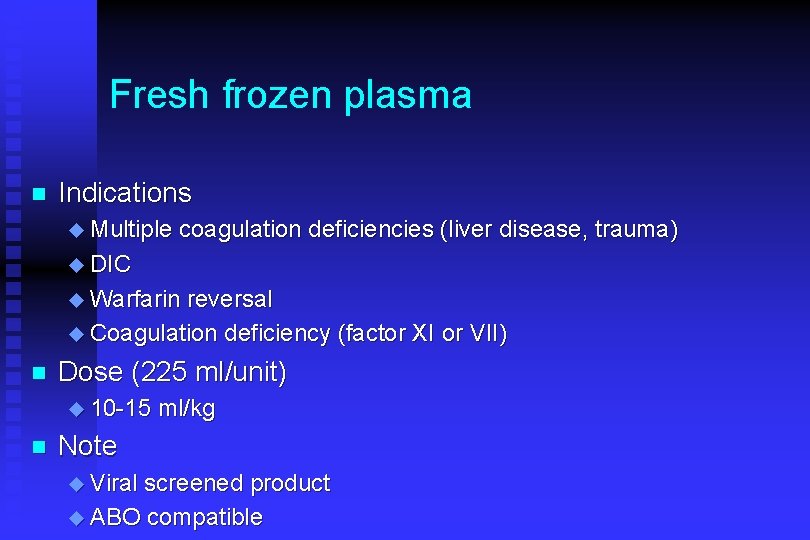
Fresh frozen plasma n Indications u Multiple coagulation deficiencies (liver disease, trauma) u DIC u Warfarin reversal u Coagulation deficiency (factor XI or VII) n Dose (225 ml/unit) u 10 -15 n ml/kg Note u Viral screened product u ABO compatible
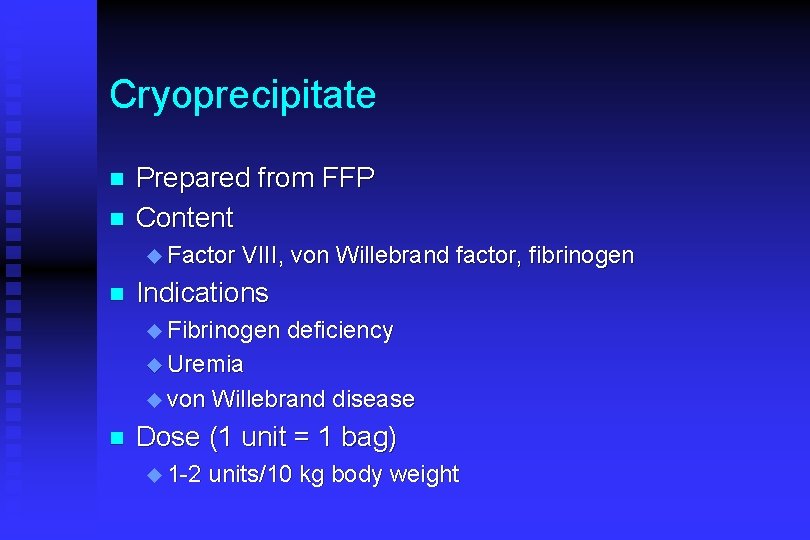
Cryoprecipitate n n Prepared from FFP Content u Factor n VIII, von Willebrand factor, fibrinogen Indications u Fibrinogen deficiency u Uremia u von n Willebrand disease Dose (1 unit = 1 bag) u 1 -2 units/10 kg body weight
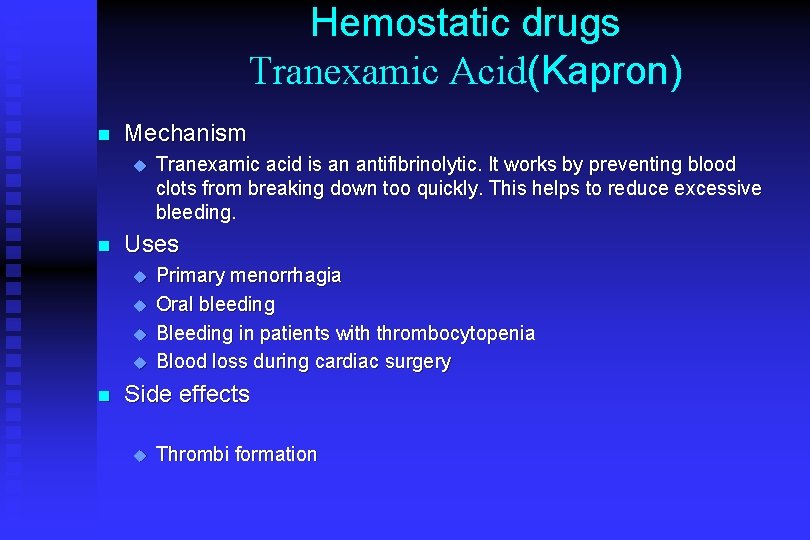
Hemostatic drugs Tranexamic Acid(Kapron) n Mechanism u n Uses u u n Tranexamic acid is an antifibrinolytic. It works by preventing blood clots from breaking down too quickly. This helps to reduce excessive bleeding. Primary menorrhagia Oral bleeding Bleeding in patients with thrombocytopenia Blood loss during cardiac surgery Side effects u Thrombi formation
- Slides: 63