Bladder Cancer Magdy FathAlla 2009 Bladder Cancer Introduction
Bladder Cancer Magdy Fath-Alla, 2009
Bladder Cancer Introduction • Male to Female ratio is 3: 1. • The median age at diagnosis is 60 years. • In developed countries about 90% of bladder tumors are transitional cell carcinoma with 5% squamous cell carcinoma. Squamous cell tumors usually follow chronic inflammation from stones or indwelling catheters. • In developing countries 50% are squamous cell carcinoma, mostly due to Schistosomiasis. The median age at diagnosis is 48 years. • Adenocarcinoma accounts for less than 2%. • Leiomyosarcoma is the commonest sarcoma of the bladder whilst rhabdomyosarcoma is commonest in children. Magdy Fath-Alla, 2009

Bladder Cancer Risk factors • About half of bladder cancers are caused by smoking. • Other risk factors include industrial exposure to aromatic amines in dyes, paints, and textiles. • Radiation to the pelvis and treatment by cyclophosphamide. • A diet high in fruit and vegetables and low in fat may reduce the risk of bladder cancer. Magdy Fath-Alla, 2009
Bladder Cancer Clinical picture • The presenting feature is total painless hematuria that is gross in 80 to 90%. • Painless hematuria must be considered as malignancy of the urinary tract until proved otherwise. This includes carcinoma of the kidney. • Irritative voiding symptoms in carcinoma in situ and in advanced disease. • Physical examination will reveal no abnormality in early disease. • In advanced disease, a bladder mass and signs of obstructive uropathy can be detected. Differential Diagnosis • Other causes of hematuria. Magdy Fath-Alla, 2009
Investigations • Cystoscopy is the inevitable test. It permits direct inspection of the bladder and biopsy of suspicious lesions. • Laboratory: – Urinalysis including culture should be performed to exclude infection. – Full blood count should be arranged to exclude anemia. – Urea and electrolytes to check renal function. – Urine cytology may be helpful but negative results do not exclude disease. – Newer, voided urine assays of tumor markers are being developed. They include bladder tumor antigen (BTA-Stat) and nuclear matrix protein (NMP-22). False positive and false negative rates are high. Magdy Fath-Alla, 2009
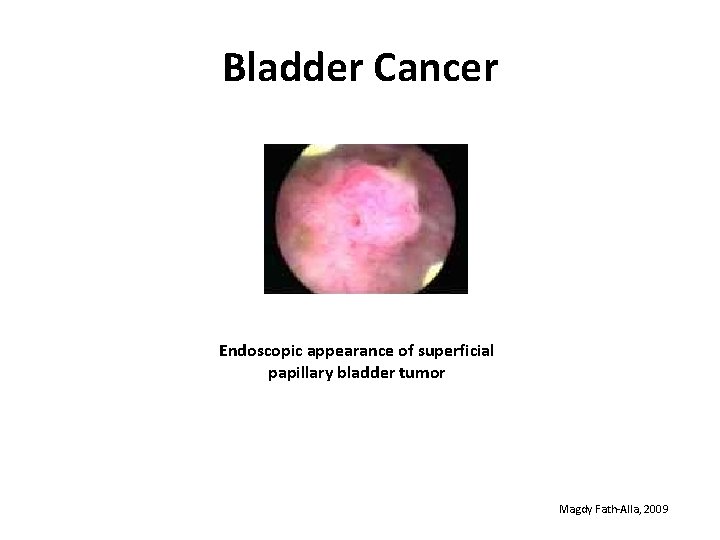
Bladder Cancer Endoscopic appearance of superficial papillary bladder tumor Magdy Fath-Alla, 2009
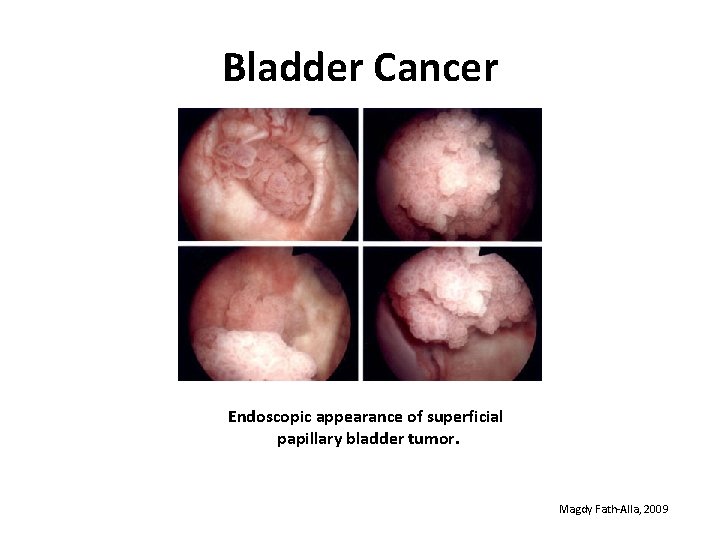
Bladder Cancer Endoscopic appearance of superficial papillary bladder tumor. Magdy Fath-Alla, 2009

Investigations • Imaging: – Intravenous pyelogram (IVP) may show a filling defect in the cystogram. – CT and ultrasound scans are used but they may miss small tumors. Magdy Fath-Alla, 2009

Bladder Cancer IVU: Right lateral wall bladder mass appearing as filling defect in the cystogram. Magdy Fath-Alla, 2009
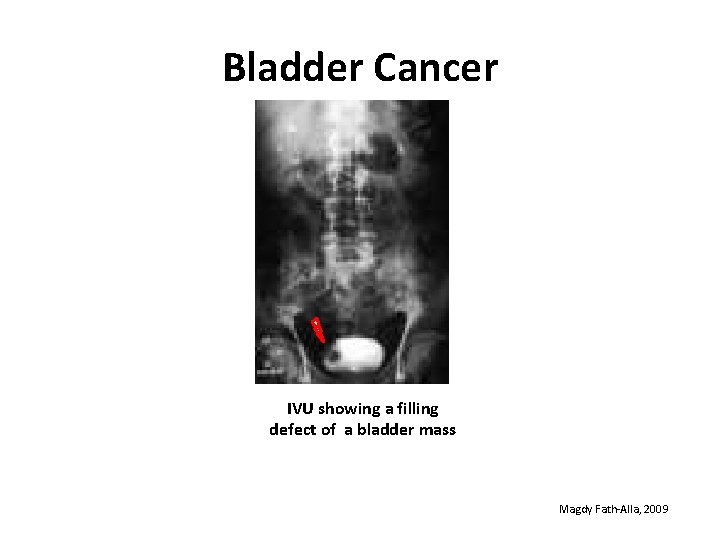
Bladder Cancer IVU showing a filling defect of a bladder mass Magdy Fath-Alla, 2009

Bladder Cancer Cystogram showing a filling defect of a bladder mass Magdy Fath-Alla, 2009
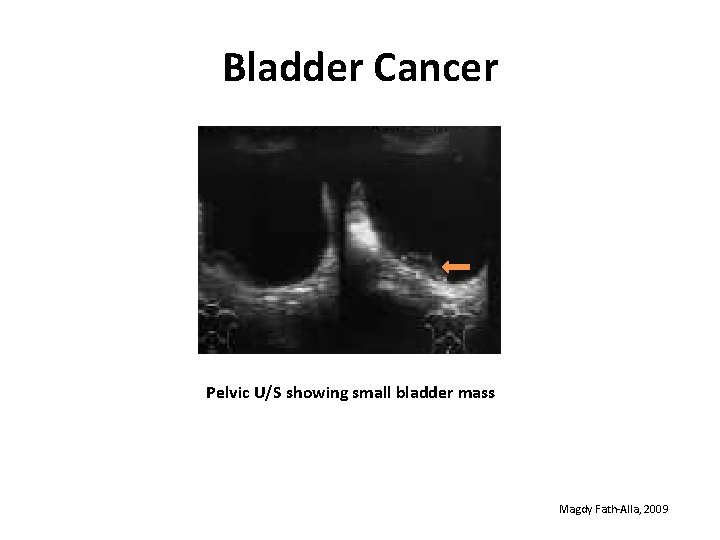
Bladder Cancer Pelvic U/S showing small bladder mass Magdy Fath-Alla, 2009
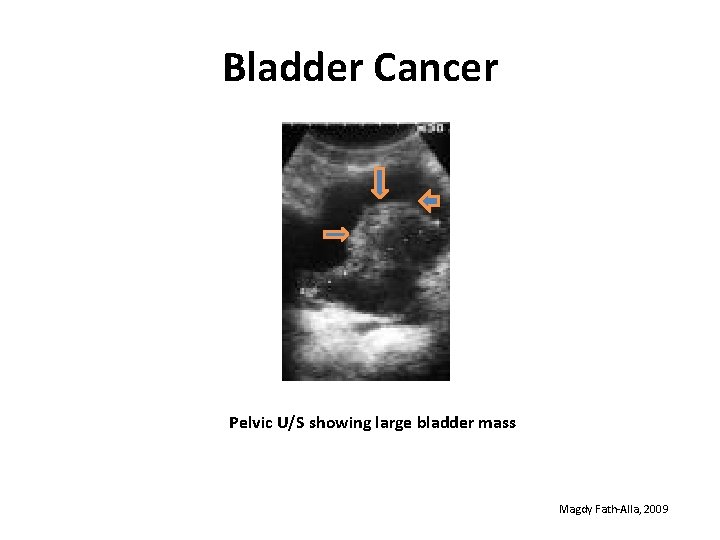
Bladder Cancer Pelvic U/S showing large bladder mass Magdy Fath-Alla, 2009
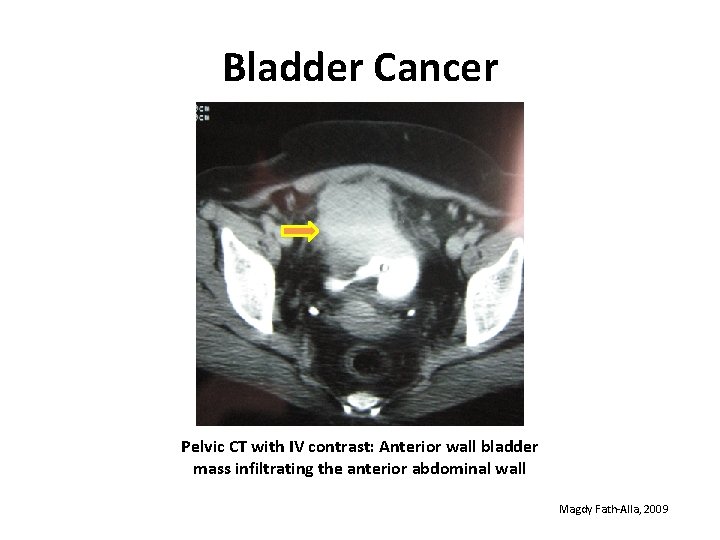
Bladder Cancer Pelvic CT with IV contrast: Anterior wall bladder mass infiltrating the anterior abdominal wall Magdy Fath-Alla, 2009

Bladder Cancer Pelvic C. T. without contrast showing a large posterior and RT lateral wall bladder mass Magdy Fath-Alla, 2009
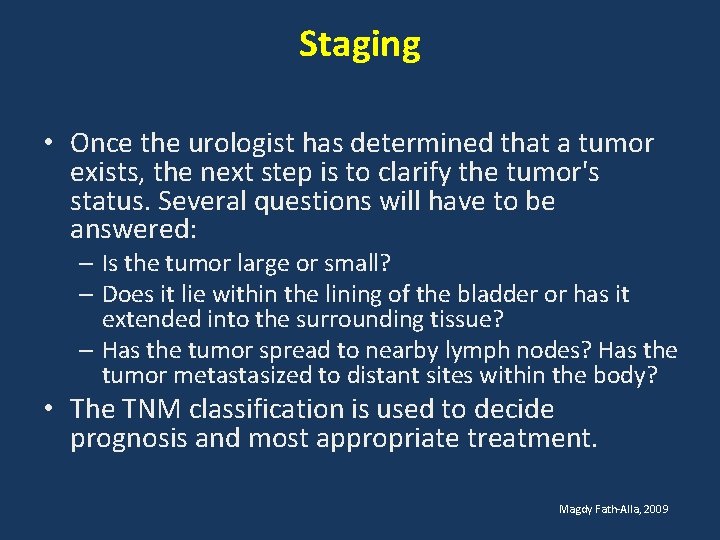
Staging • Once the urologist has determined that a tumor exists, the next step is to clarify the tumor's status. Several questions will have to be answered: – Is the tumor large or small? – Does it lie within the lining of the bladder or has it extended into the surrounding tissue? – Has the tumor spread to nearby lymph nodes? Has the tumor metastasized to distant sites within the body? • The TNM classification is used to decide prognosis and most appropriate treatment. Magdy Fath-Alla, 2009
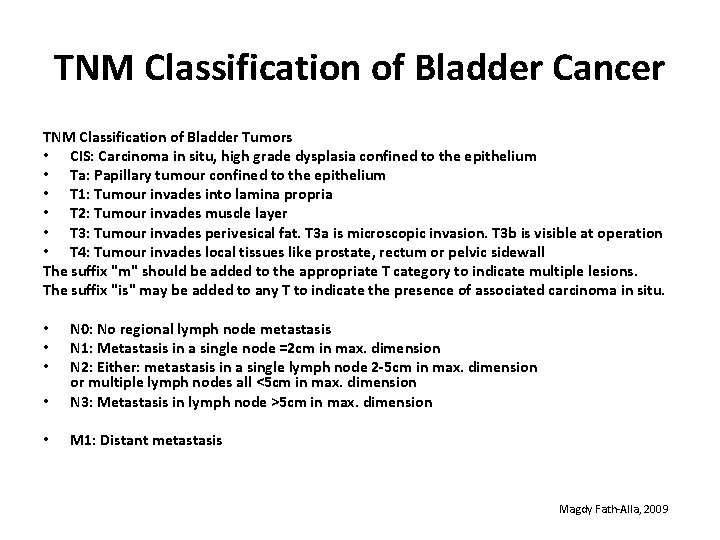
TNM Classification of Bladder Cancer TNM Classification of Bladder Tumors • CIS: Carcinoma in situ, high grade dysplasia confined to the epithelium • Ta: Papillary tumour confined to the epithelium • T 1: Tumour invades into lamina propria • T 2: Tumour invades muscle layer • T 3: Tumour invades perivesical fat. T 3 a is microscopic invasion. T 3 b is visible at operation • T 4: Tumour invades local tissues like prostate, rectum or pelvic sidewall The suffix "m" should be added to the appropriate T category to indicate multiple lesions. The suffix "is" may be added to any T to indicate the presence of associated carcinoma in situ. • N 0: No regional lymph node metastasis N 1: Metastasis in a single node =2 cm in max. dimension N 2: Either: metastasis in a single lymph node 2 -5 cm in max. dimension or multiple lymph nodes all <5 cm in max. dimension N 3: Metastasis in lymph node >5 cm in max. dimension • M 1: Distant metastasis • • • Magdy Fath-Alla, 2009
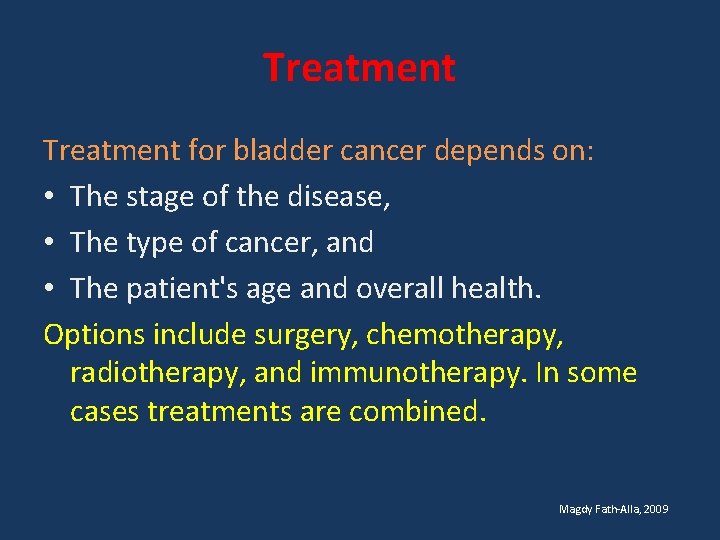
Treatment for bladder cancer depends on: • The stage of the disease, • The type of cancer, and • The patient's age and overall health. Options include surgery, chemotherapy, radiotherapy, and immunotherapy. In some cases treatments are combined. Magdy Fath-Alla, 2009
Treatment • For superficial cancer (CIS, Ta or T 1), endoscopic resection and fulguration of the tumor base is required (Trans-Urethral Resection of bladder tumor, TURT). Magdy Fath-Alla, 2009
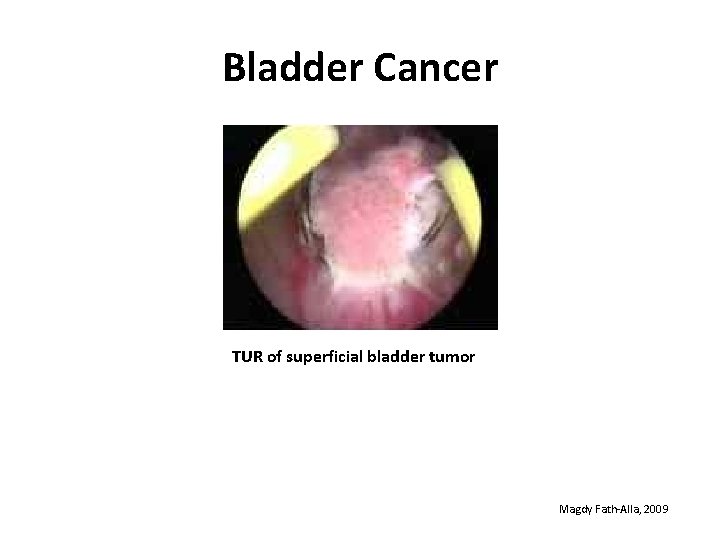
Bladder Cancer TUR of superficial bladder tumor Magdy Fath-Alla, 2009
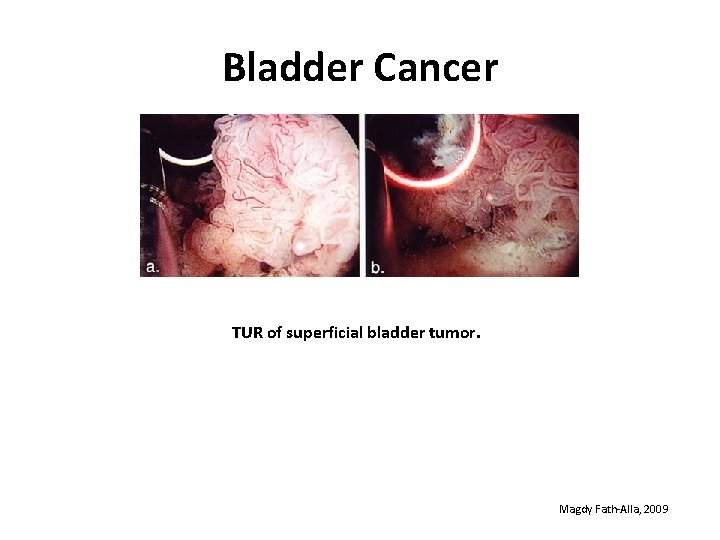
Bladder Cancer TUR of superficial bladder tumor. Magdy Fath-Alla, 2009
Treatment • According to tumor size and multiplicity, postresection intravesical chemotherapy (Mitomycin C) or intravesical immunotherapy (BCG) may be needed. It may reduce recurrence or progression. • Follow up by cystoscopy at scheduled intervals is essential as tumors can recur at the primary site or other sites. Magdy Fath-Alla, 2009
Treatment • For invasive non metastatic cancer in men the operation is radical cystoprostatectomy. • This involves removal of bladder, prostate, seminal vesicles and pelvic lymph nodes • An anterior pelvic exenteration is performed in women with invasive non metastatic disease. It involves removal of the bladder, urethra, uterus, ovaries, and anterior vaginal wall. Magdy Fath-Alla, 2009
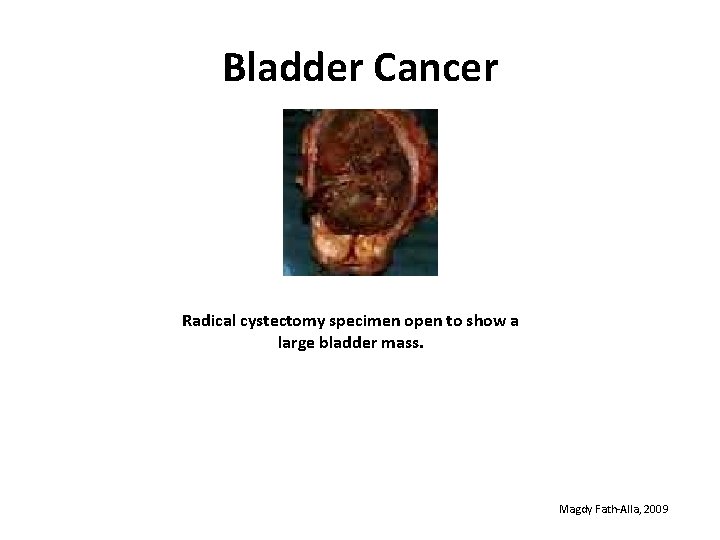
Bladder Cancer Radical cystectomy specimen open to show a large bladder mass. Magdy Fath-Alla, 2009
Treatment • After removal of the bladder urinary diversions are created from various segments of bowel. An ileal conduit, an ileal neobladder, and continent urinary diversion are the most commonly used procedures. • Complications of surgery include bowel obstruction, obstruction of the ureter, pyelonephritis, infection of the wound and erectile dysfunction. Magdy Fath-Alla, 2009
Treatment • External beam radiotherapy for invasive tumors tends to have poorer results than cystectomy. • Chemotherapy: Methotrexate, vinblastine, Adriamycin and cisplatin are used in combination for metastatic disease. Magdy Fath-Alla, 2009
Follow up Even superficial tumors have a very high rate of recurrence and progression. The whole epithelium should be considered as unstable and there is a recurrence rate of 70% within 5 years. Surveillance for superficial transitional cell carcinoma includes cystoscopy and bladder wash cytology every 3 months for 2 years, then every 6 months for a further 2 years, and then at least annually. Magdy Fath-Alla, 2009

Thank You
- Slides: 29