BIOPSY INTRODUCTION The famous theme that The best
BIOPSY
INTRODUCTION The famous theme that “The best surgeon is a clinical pathologist who performs operations” is repeated throughout the surgical literature.
OBJECTIVES • Know when and how to do a biopsy – Be able to list the indications for a biopsy – Be able to list the characteristics of lesions that raise suspicion of malignancy – Be able to list indications for and describe and draw the techniques • Understand the importance of having a good differential diagnosis before doing a biopsy
DEFINITION • BIOPSY is the removal of tissue from a living organism for the purpose of microscopic examination and diagnosis. • If tissue is removed from dead organism it is called AUTOPSY
INDICATIONS FOR BIOPSY 1. Any lesion that persists for more than 2 weeks with no apparent cause 2. Any inflammatory lesion that does not respond to local treatment after 10 -14 days (after removing local irritant) 3. Persistent hyperkeratotic changes in surface tissues 4. Any persistent tumescence, either visible or palpable beneath relatively normal tissue
INDICATIONS FOR BIOPSY………. . 5. Inflammatory changes of unknown cause that persist for long periods 6. Lesions that interfere with local function (e. g. fibroma) 7. Bone lesions not specifically identified by clinical and radiographic findings 8. Any lesion that has the characteristics of malignancy
CHARACTERISTICS OF LESIONS THAT RAISE SUSPICION OF MALIGNANCY • • Erythroplasia Ulceration Duration more than 2 weeks Rapid growth rate Bleeding lesion on manipulation Induration Fixation

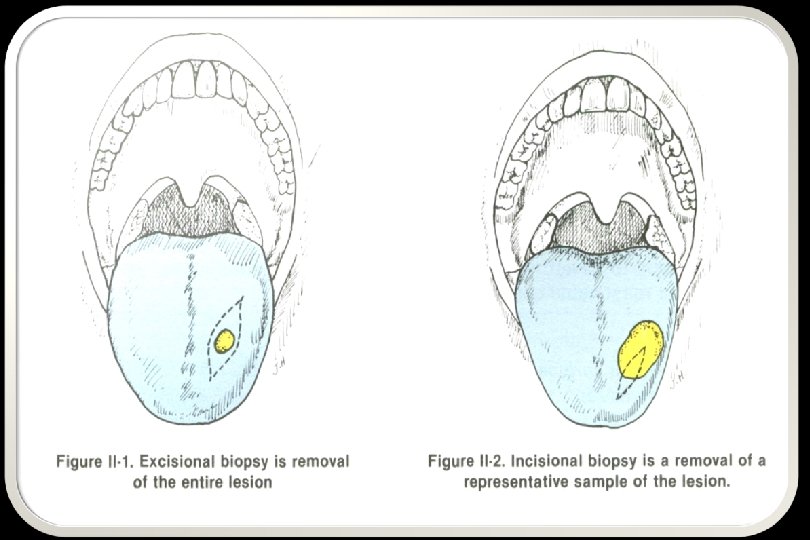
TYPES OF BIOPSY • Incisional biopsy • Excisional biopsy
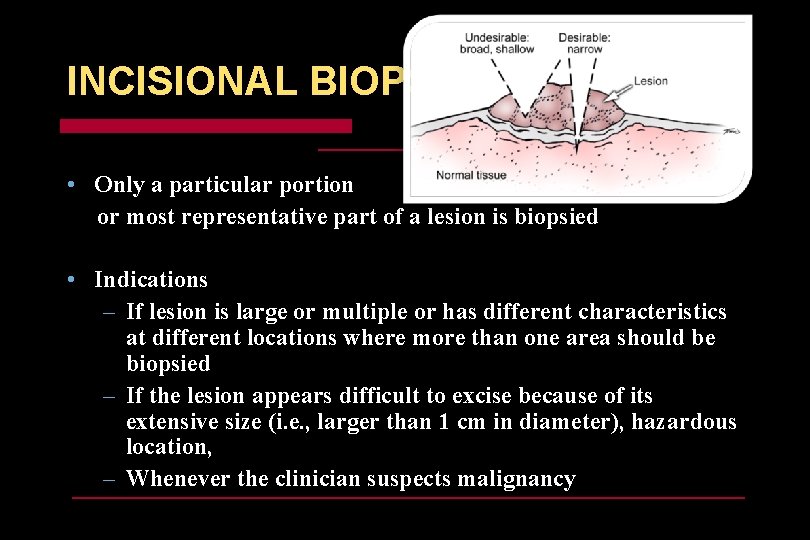
INCISIONAL BIOPSY • Only a particular portion or most representative part of a lesion is biopsied • Indications – If lesion is large or multiple or has different characteristics at different locations where more than one area should be biopsied – If the lesion appears difficult to excise because of its extensive size (i. e. , larger than 1 cm in diameter), hazardous location, – Whenever the clinician suspects malignancy
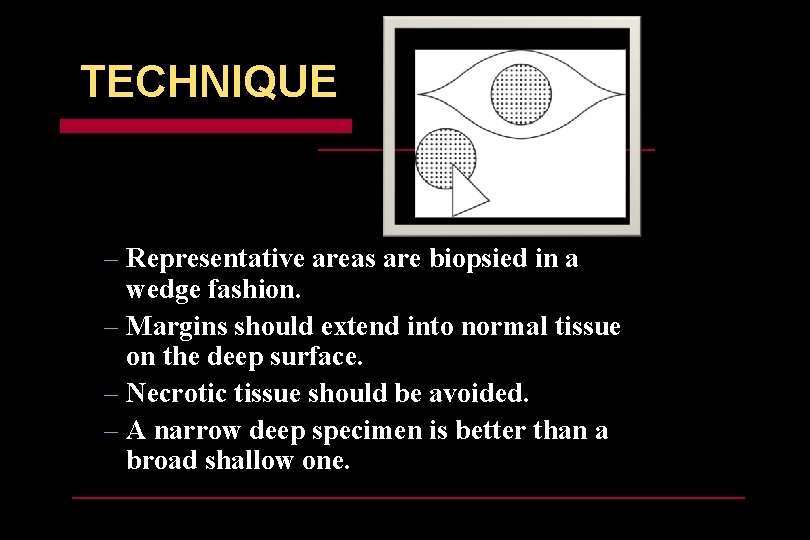
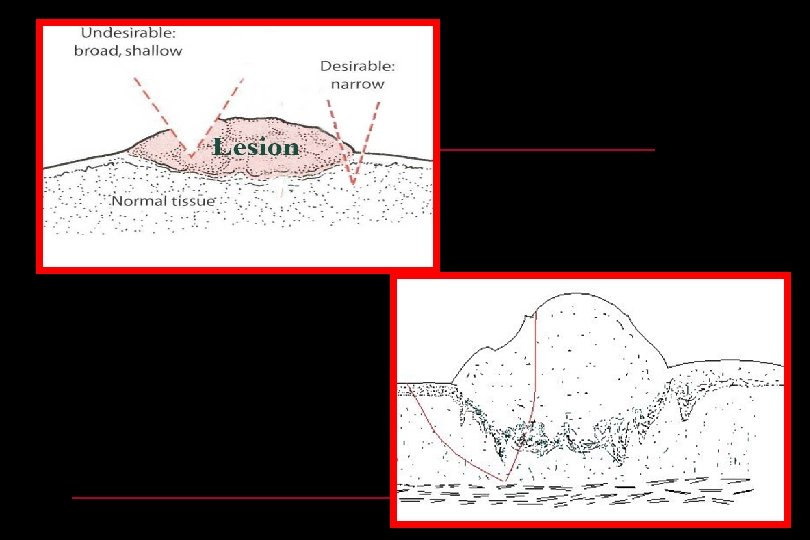
TECHNIQUE – Representative areas are biopsied in a wedge fashion. – Margins should extend into normal tissue on the deep surface. – Necrotic tissue should be avoided. – A narrow deep specimen is better than a broad shallow one.
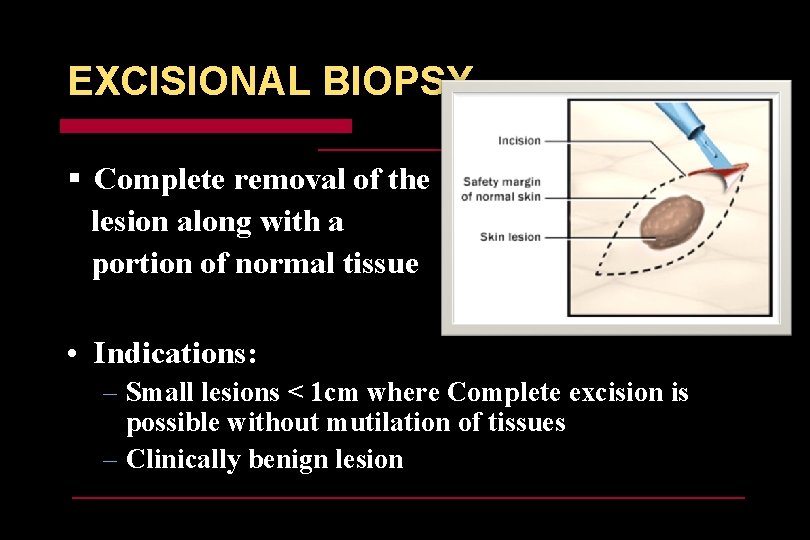
EXCISIONAL BIOPSY § Complete removal of the lesion along with a portion of normal tissue • Indications: – Small lesions < 1 cm where Complete excision is possible without mutilation of tissues – Clinically benign lesion
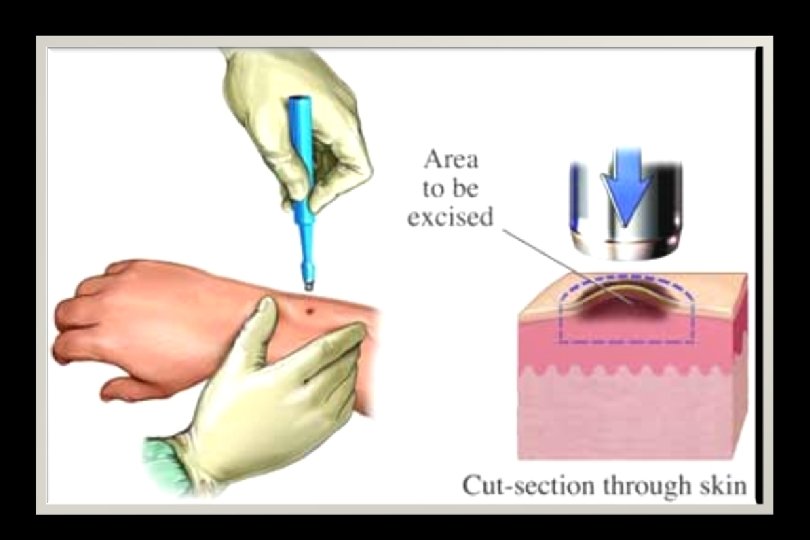
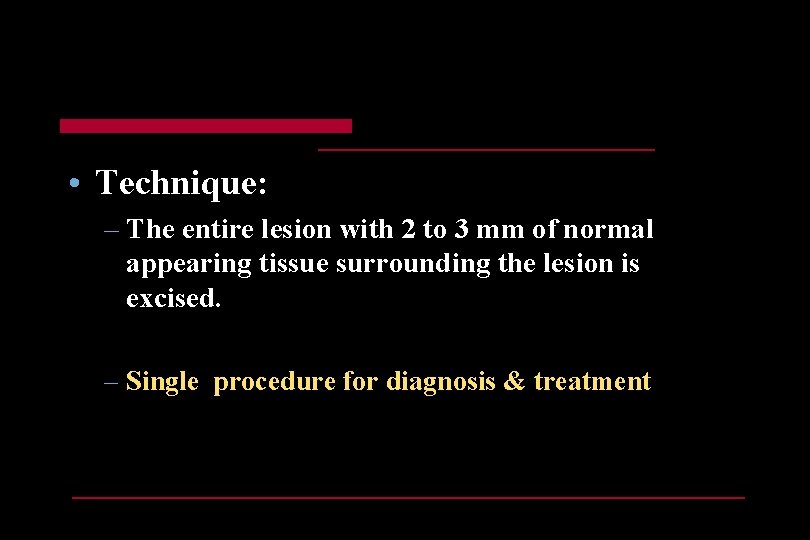
• Technique: – The entire lesion with 2 to 3 mm of normal appearing tissue surrounding the lesion is excised. – Single procedure for diagnosis & treatment
METHODS BY WHICH TISSUE CAN BE OBTAINED FROM LESIONS • Surgical excision by scalpel • Surgical removal by cautery or high frequency cutting knife • Removal by biopsy forceps or biopsy punch • Aspiration using a needle with large lumen • Exfoliative cytology – surface of lesion is scaped
BIOPSY PROCEDURE • 1. Preparation of site to be biopsied • 2. Anesthesia – Block local anaesthesia is preferred to avoid artifactual distortion of the specimen – Infiltration local anaesthesia should be at least 1 cm away from the lesion
BIOPSY PROCEDURE • The most representative site of the wound is identified • A section from the identified site of the wound is removed • Tissue is cleaned and put into 10% formalin solution for fixation • The biopsy site is sutured after achieving hemostasis • The biopsy specimen is sent to the histopathologist for diagnosis after labeling it properly.
POINTS TO REMEMBER WHILE PERFORMING BIOPSY • Do not paint the area to be biopsied with any coloured antiseptic agent. • The colour may interfere with staining and may lead to artifacts • Do not inject anesthetic solution directly into the lesion. • Use block technique or inject the solution well away from the lesional tissue
POINTS TO REMEMBER WHILE PERFORMING BIOPSY………. . • Use minimal quantity of local anesthetic solution. • Stay suture should not pass through the lesional tissue rather placed away from the lesional tissue • Because it can cause compression of tissue and may interfere with diagnosis. • Use sharp instrument for biopsy • Repeated cutting of the tissue to be avoided because it may leads to mutilation of tissue
POINTS TO REMEMBER WHILE PERFORMING BIOPSY………. . • Biopsy specimen should be of adequate thickness and depth • Incision should be deep and narrow rather than broad & shallow • Should include both epithelium & connective tissue • Should include margin of adjacent normal tissue • If specimen is thin, place it on a piece of glazed paper and drop in to fixative to prevent curling of the tissue.
• Take care not to mutilate the specimen when grasping tissue with forceps • Place stay sutures to help handling of the tissue • Use small atraumatic forceps cautiously • Hold the tissue in an area away from the lesional tissue • Do not squeeze the tissue into the container
• Transfer the tissue immediately to fixative solutions ( 10% Formalin) • The specimen container should have a wide mouth, so that the specimen can be easily placed & retrieved • Squeezing of the tissue into the container to be avoided
q Proper Labeling of the Biopsy container – – Patient’s name Age Sex Hospital number
SHOULD SEND CLINICAL DATA Includes: • Name, age, sex of the patient • Mention the date and time of the biopsy • Type and nature of biopsy • Site of the biopsy • Mention the brief clinical, radiological and other relevant features of the lesion • Mention the provisional diagnosis
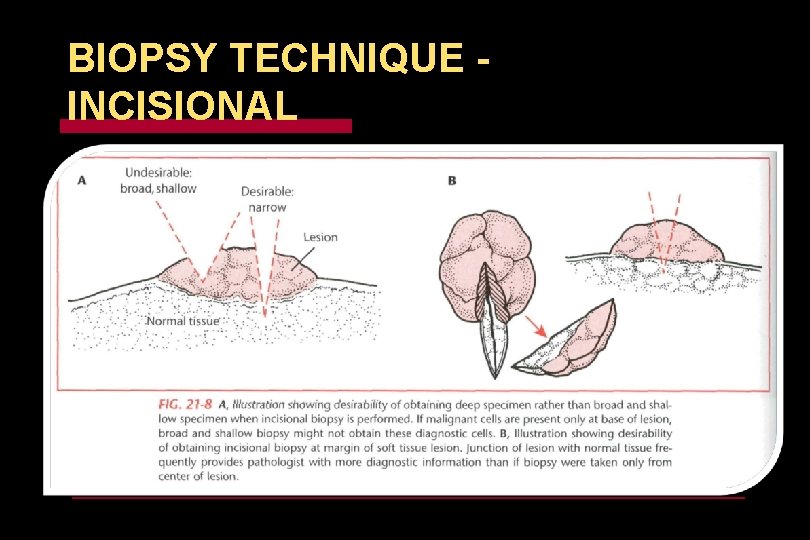
BIOPSY TECHNIQUE INCISIONAL
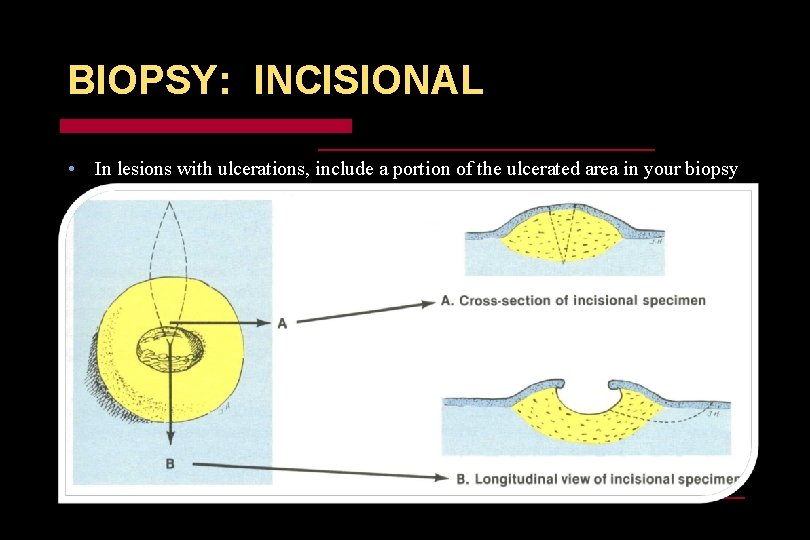
BIOPSY: INCISIONAL • In lesions with ulcerations, include a portion of the ulcerated area in your biopsy
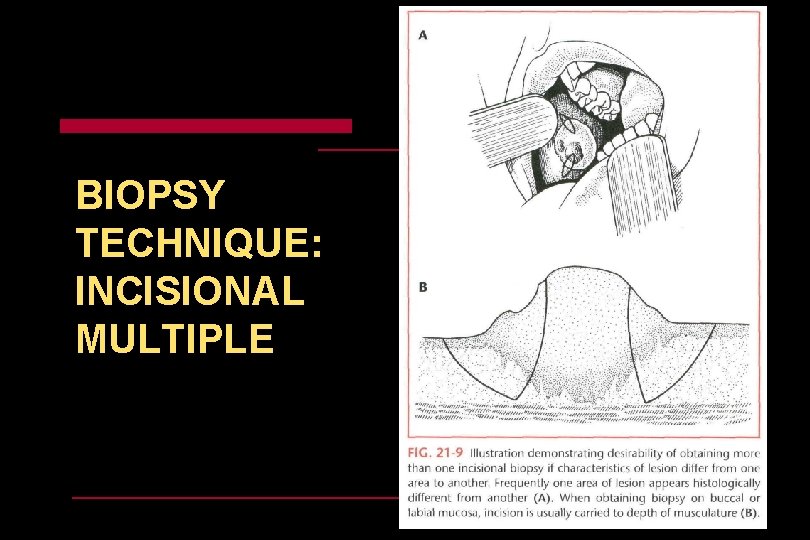
BIOPSY TECHNIQUE: INCISIONAL MULTIPLE
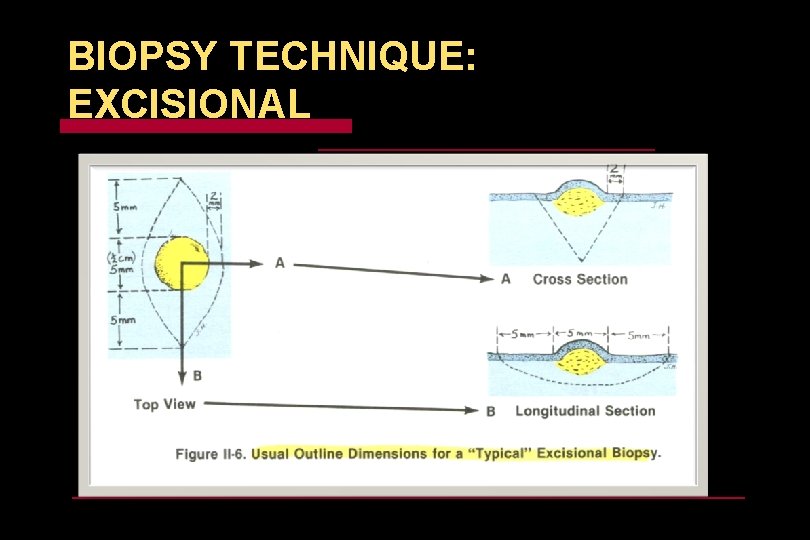
BIOPSY TECHNIQUE: EXCISIONAL
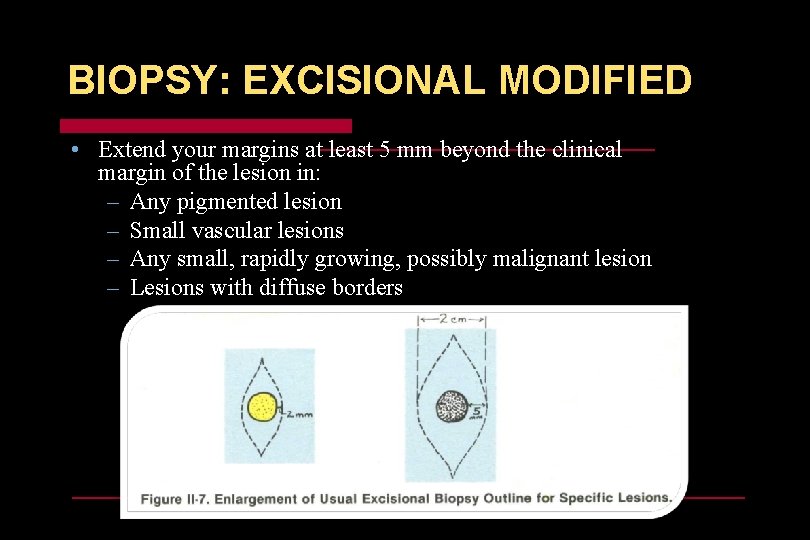
BIOPSY: EXCISIONAL MODIFIED • Extend your margins at least 5 mm beyond the clinical margin of the lesion in: – Any pigmented lesion – Small vascular lesions – Any small, rapidly growing, possibly malignant lesion – Lesions with diffuse borders
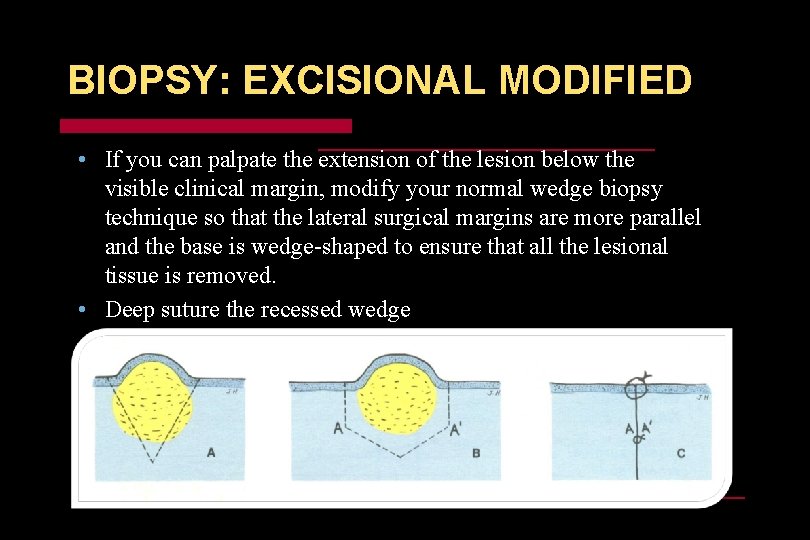
BIOPSY: EXCISIONAL MODIFIED • If you can palpate the extension of the lesion below the visible clinical margin, modify your normal wedge biopsy technique so that the lateral surgical margins are more parallel and the base is wedge-shaped to ensure that all the lesional tissue is removed. • Deep suture the recessed wedge
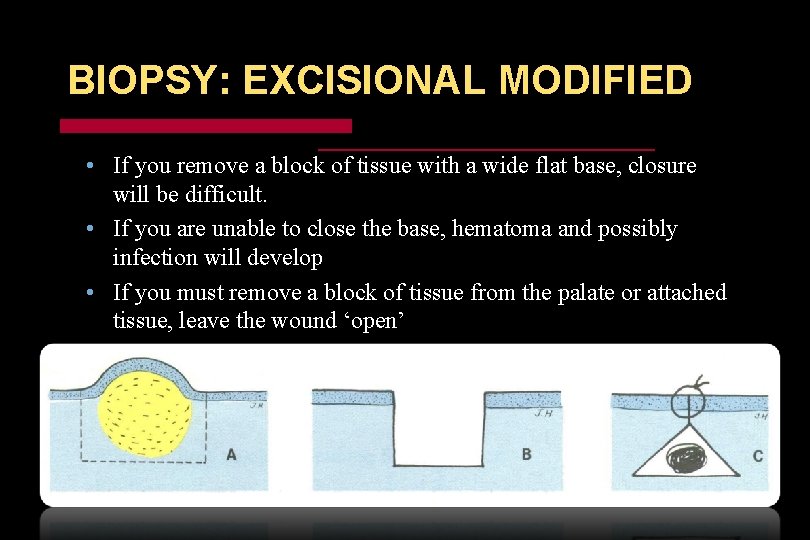
BIOPSY: EXCISIONAL MODIFIED • If you remove a block of tissue with a wide flat base, closure will be difficult. • If you are unable to close the base, hematoma and possibly infection will develop • If you must remove a block of tissue from the palate or attached tissue, leave the wound ‘open’
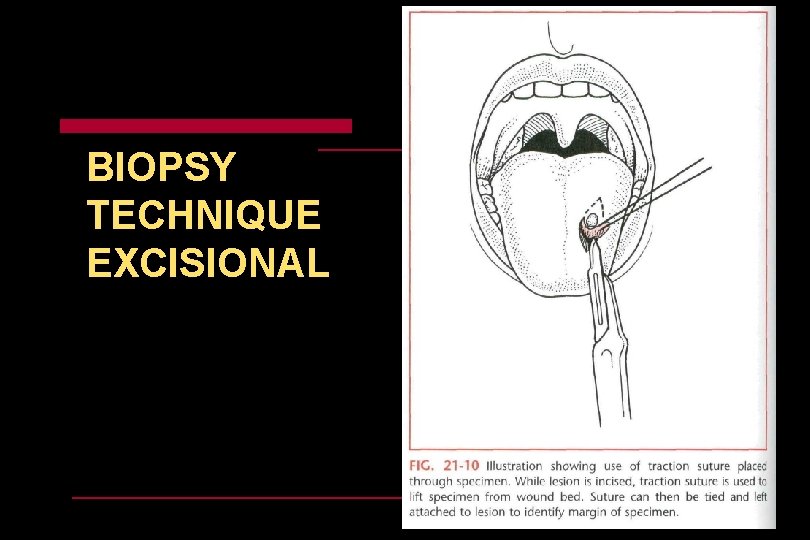
BIOPSY TECHNIQUE EXCISIONAL
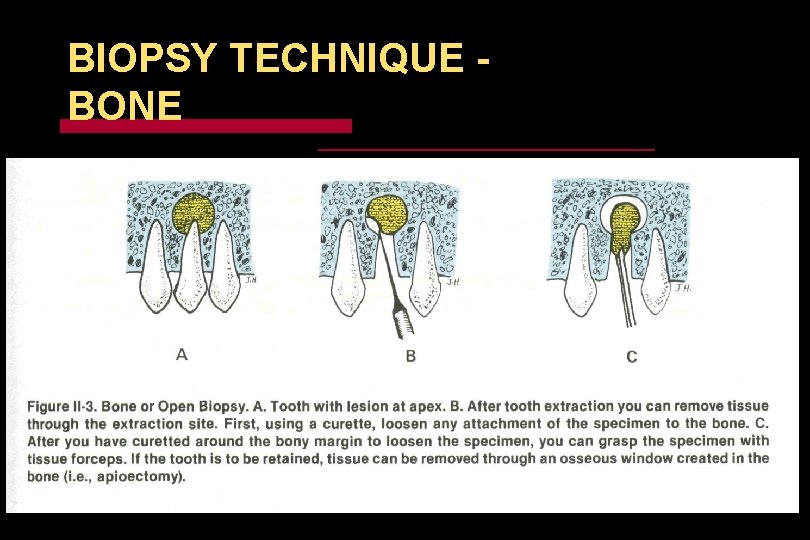
BIOPSY TECHNIQUE BONE
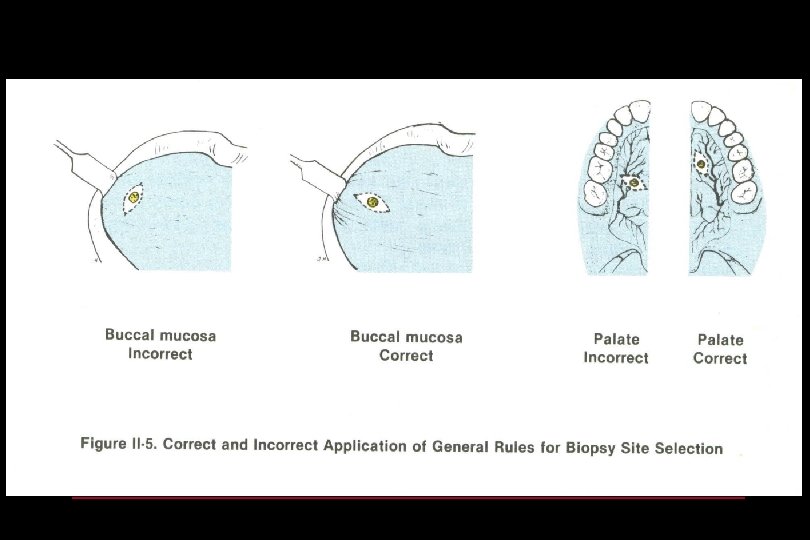
BIOPSY GENERAL RULES • Strive for an elliptical wedge of tissue. • The surgical site should be easier to suture closed • Incise parallel, not perpendicular, to nerves, arteries, and veins • Incise parallel, not perpendicular, to muscle fibres and attachments • If you have a choice, follow the line of stress or tension to minimize visibility of the scar (especially if extending onto vermilion of lips
BIOPSY • Do not do a biopsy unless you can make a reasonable differential diagnosis • Your DDx will influence whether you do an incisional or excisional biopsy • An inadequate excisional Bx on a malignant or potentially malignant lesion is not good, since it will be difficult to determine margins for definitive excision
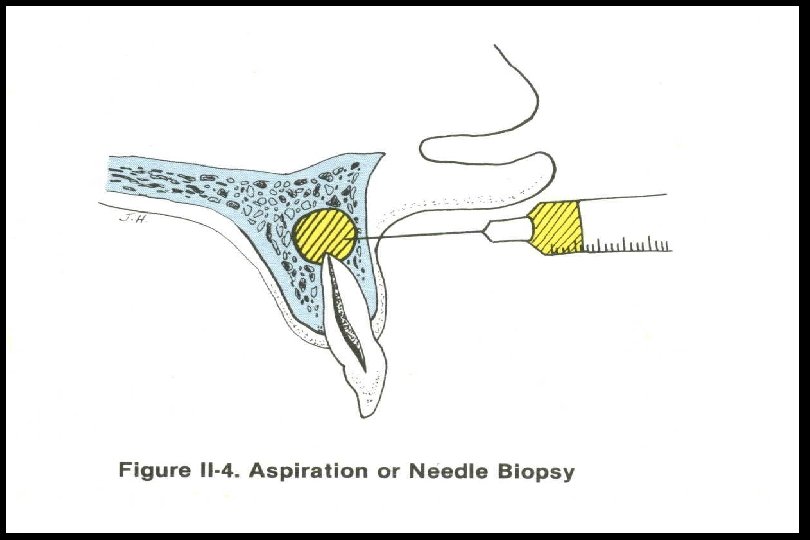
ASPIRATION BIOPSY • The use of a needle and syringe to penetrate a lesion for aspiration of its contents • 2 main types: One type is to determine only whether or not a lesion contains solid, fluid, or air; other type is to remove cellular material for diagnostic examination by a pathologist = Fine needle aspiration • Fine needle aspiration usually done when a soft tissue mass is detected below the surface of the skin or mucosa (e. g. neck masses)
ASPIRATION BIOPSY • Aspiration to determine whether lesion contains fluid is typically done before opening into radiolucent lesions of the jaws – Straw-coloured is most likely cyst – Pus indicates inflammation or infection – Air may represent traumatic bone cyst – Blood may represent vascular lesion
INDICATIONS: ASPIRATION BIOPSY • Aspiration should be carried out on all lesions thought to contain fluid (with the possible exception of a mucocele) or any intraosseous lesion before surgical exploration
Oral Brush Cytology • “Sensitivity > 96%” • Uses a special brush to collect epithelial cells • Brush is placed in contact with oral epithelium and rotated with firm pressure 510 times • Brush collects cells from all 3 layers of the epithelium: (1) the basal, (2) intermediate, and (3) superficial layers
Oral Brush Cytology • Cellular material on brush is transferred to a glass slide and flooded with fixative • Results: negative, positive, atypical • “Positive” and “atypical” results require scalpel biopsy to characterize the lesion completely • May be a good tool for “monitoring” patients with chronic mucosal changes
Oral Brush Cytology • Chronic mucosal changes, such as leukoplakia, lichen planus, post-irradiation and patients with a history of oral cancer who require longterm surveillance of their ongoing mucosal changes • This is because brush cytology specimens are disaggregated and architectural information to stage and grade the lesion is absent
References • Ellis E. Principles of Differential Diagnosis and Biopsy. Chapter 21 in Contemporary Oral and Maxillofacial Surgery, 4 th Edition. Editors: Peterson, Ellis, Hupp, Tucker. Mosby 2003 • Morton TH, Whitacre RJ, Gehrig JD. A Self-Instructional Guide: Principles of Biopsy. Book eight, in A Self. Instructional Guide to Oral Surgery in General Dentistry, 3 rd edition. Stoma Press Inc. 1983
K N A H Text Here TYour U YO
- Slides: 46