BIOL 2402 Unit 4 Reproductive System Overview Male
BIOL 2402 Unit 4 Reproductive System Overview
Male & Female Cells, Hormones, & Processes Use this PPT and your textbook and your Lecture Outline to complete your charts.
Male Cell Types & the process of Spermatogenesis
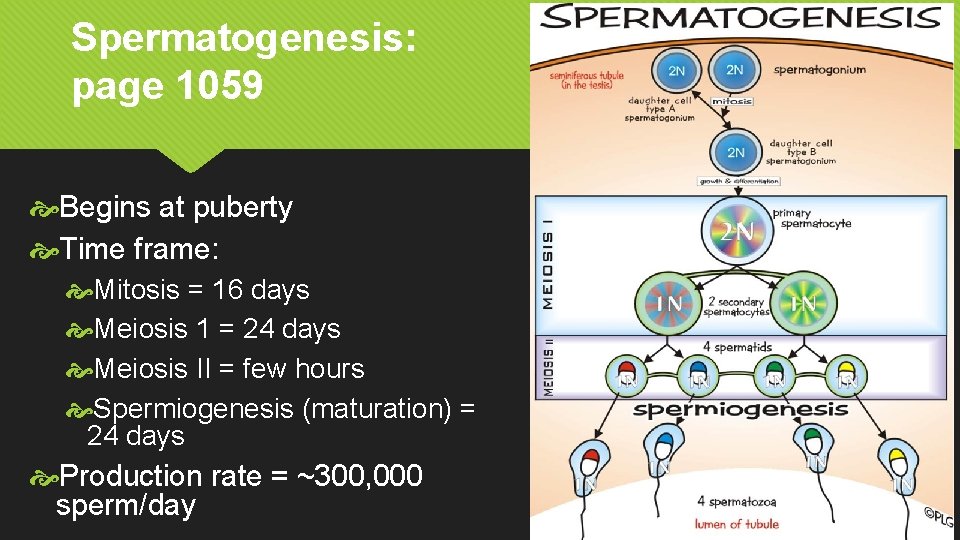
Spermatogenesis: page 1059 Begins at puberty Time frame: Mitosis = 16 days Meiosis 1 = 24 days Meiosis II = few hours Spermiogenesis (maturation) = 24 days Production rate = ~300, 000 sperm/day
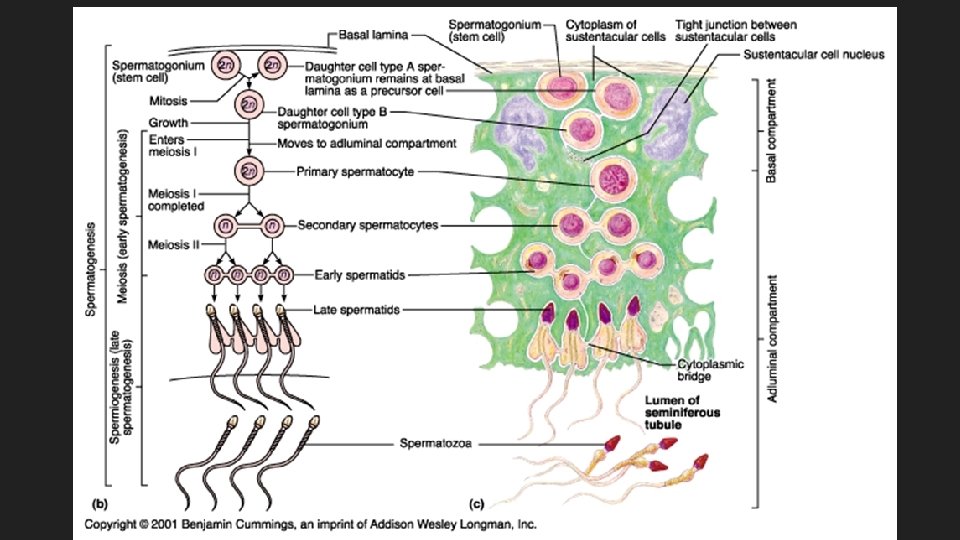
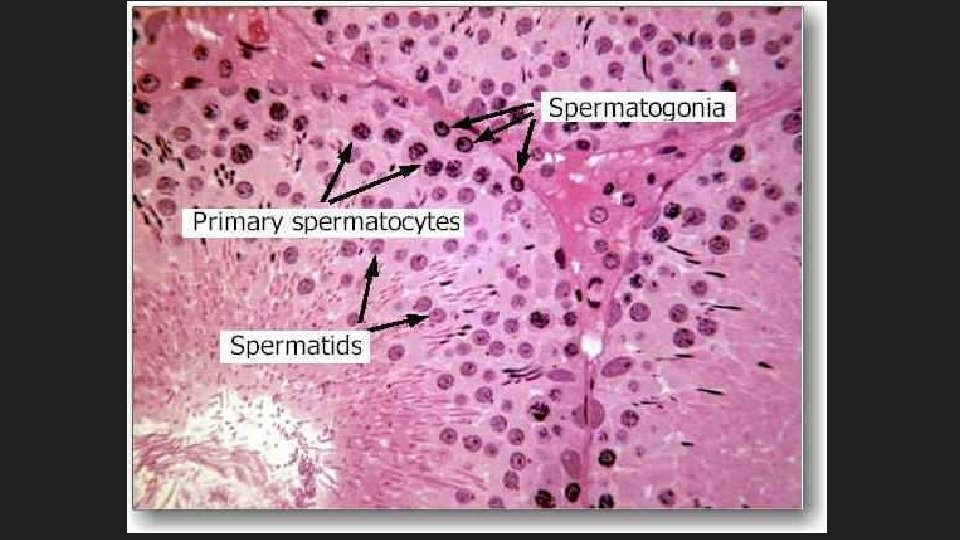
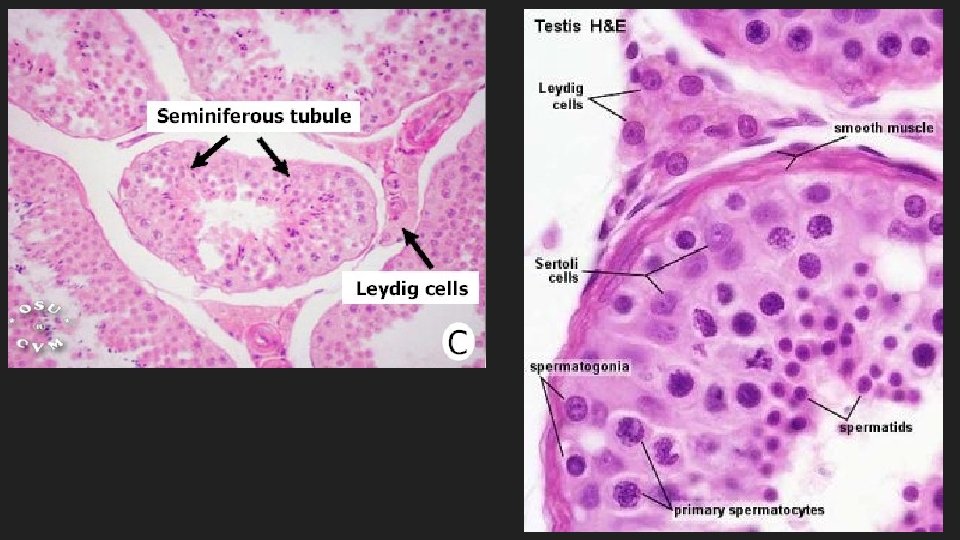
Cell types involved in Spermatogenesis Spermatogonia Stem cell Diploid Produce 2 daughter cells 1 stays as spermatogonia, other differentiates in 1 o spermatocyte
Cell types involved in Spermatogenesis Primary spermatocyte Diploid Completes meiosis I to form 2 o spermatocytes Secondary spermatocyte Haploid Enter meiosis II Divide & differentiate into spermatids
Cell types involved in Spermatogenesis Spermatids Immature gametes Haploid Differentiate/matures into spermatozoa
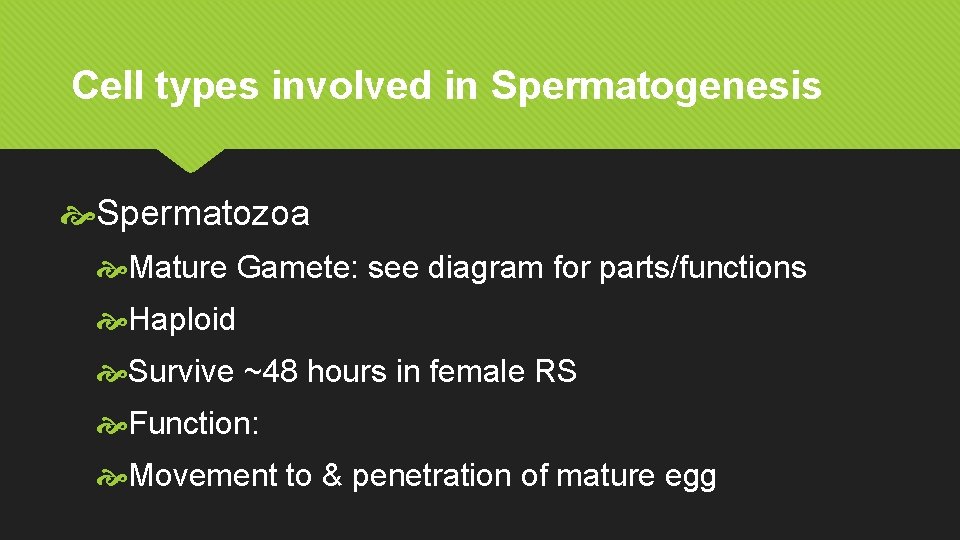
Cell types involved in Spermatogenesis Spermatozoa Mature Gamete: see diagram for parts/functions Haploid Survive ~48 hours in female RS Function: Movement to & penetration of mature egg
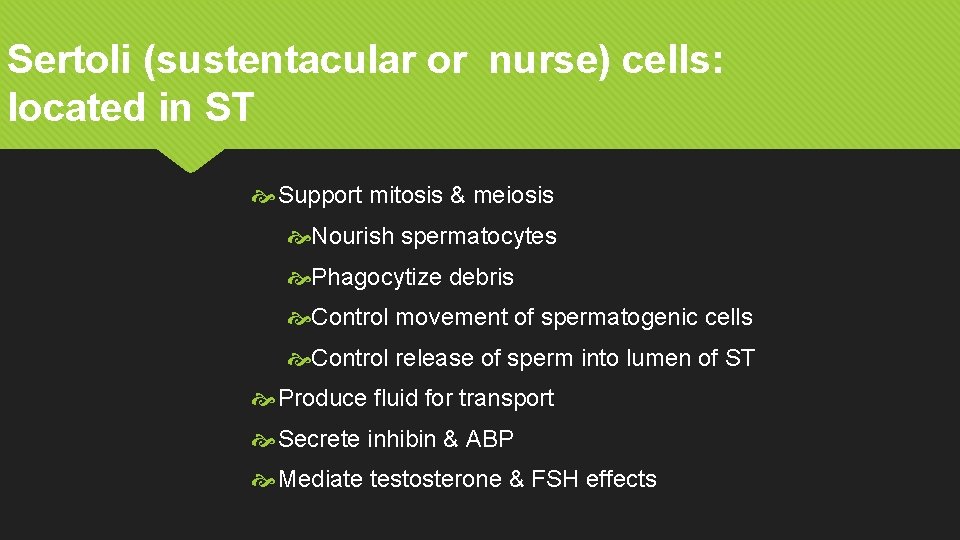
Sertoli (sustentacular or nurse) cells: located in ST Support mitosis & meiosis Nourish spermatocytes Phagocytize debris Control movement of spermatogenic cells Control release of sperm into lumen of ST Produce fluid for transport Secrete inhibin & ABP Mediate testosterone & FSH effects
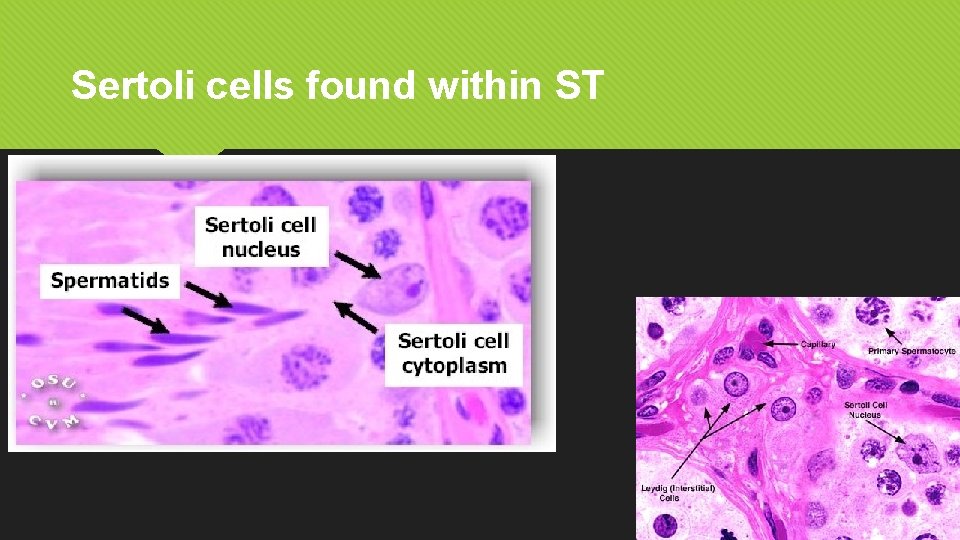
Sertoli cells found within ST
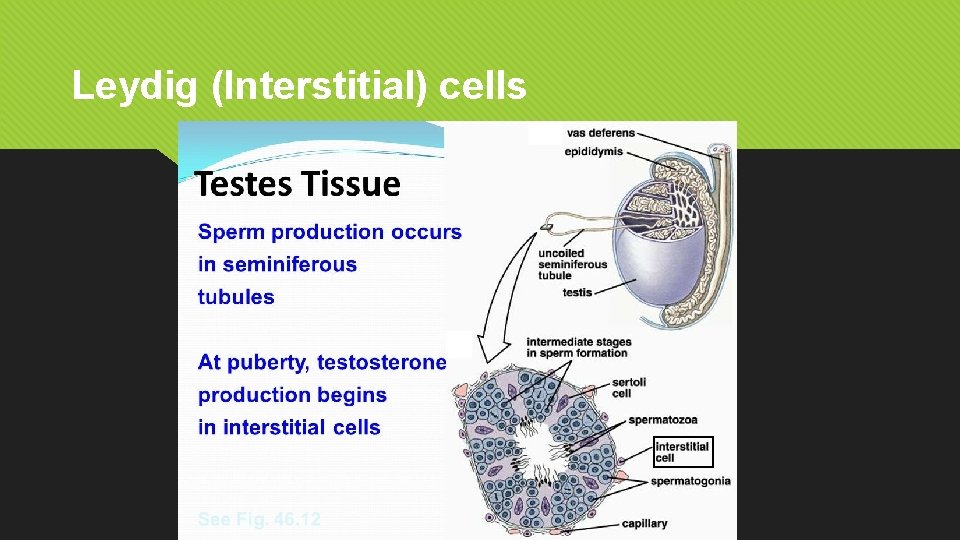
Leydig (Interstitial) cells
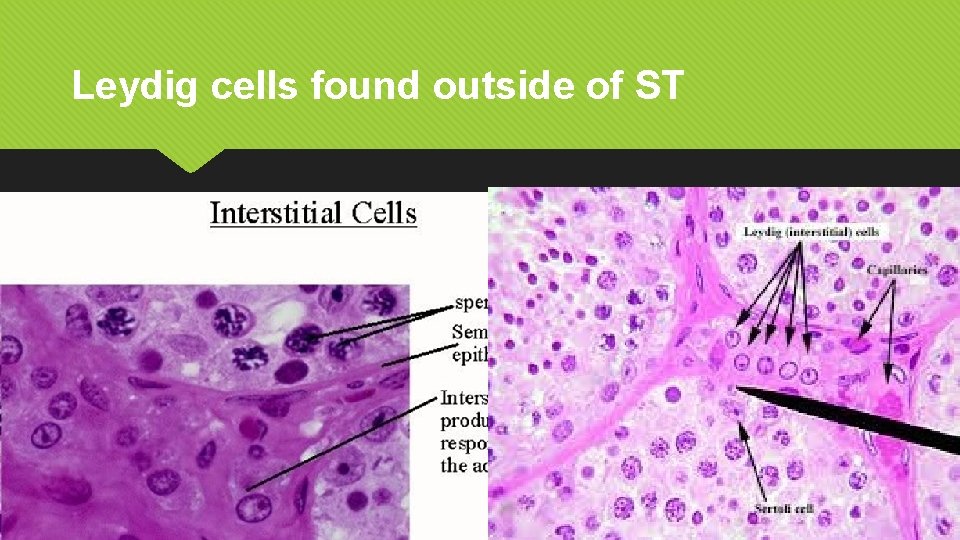
Leydig cells found outside of ST
Female Cell Types & the process of Oogenesis (the Ovarian Cycle)
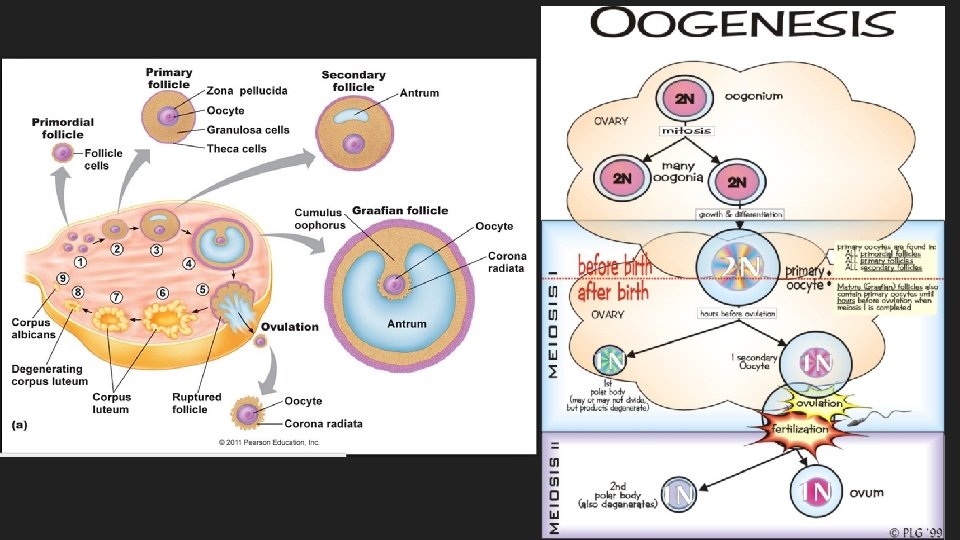
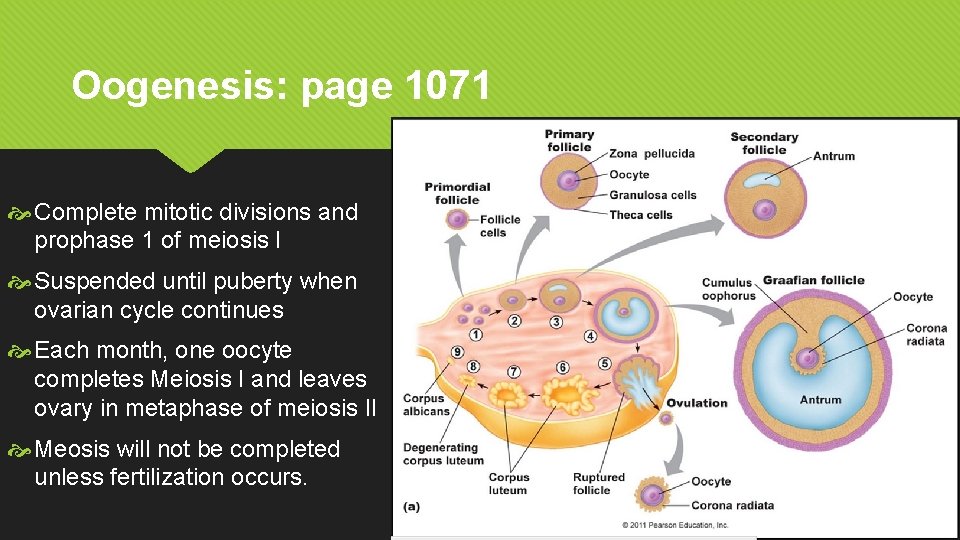
Oogenesis: page 1071 Complete mitotic divisions and prophase 1 of meiosis I Suspended until puberty when ovarian cycle continues Each month, one oocyte completes Meiosis I and leaves ovary in metaphase of meiosis II Meosis will not be completed unless fertilization occurs.
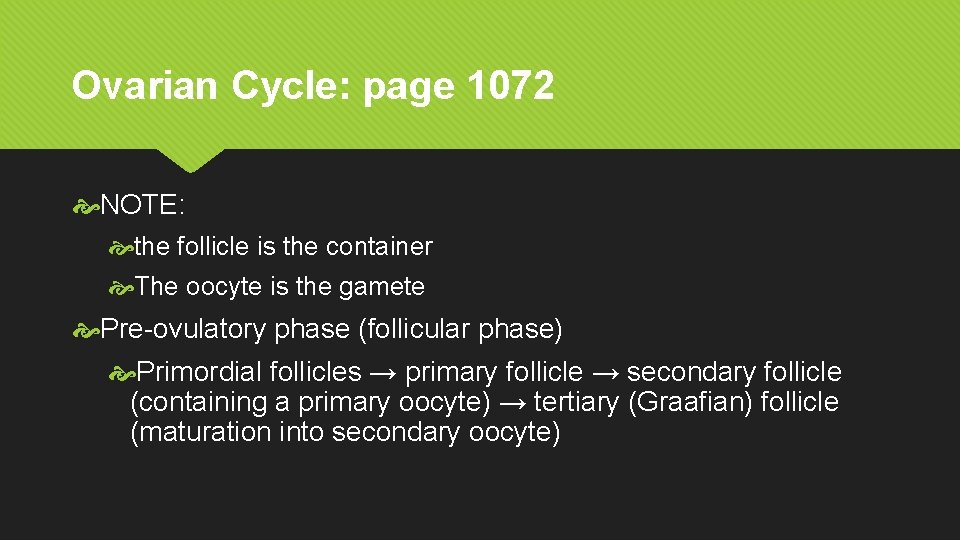
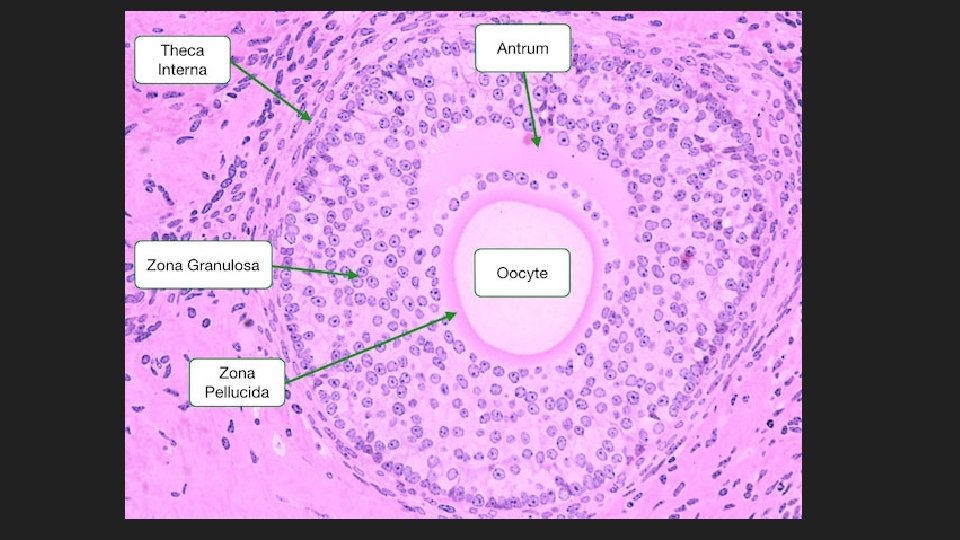
Ovarian Cycle: page 1072 NOTE: the follicle is the container The oocyte is the gamete Pre-ovulatory phase (follicular phase) Primordial follicles → primary follicle → secondary follicle (containing a primary oocyte) → tertiary (Graafian) follicle (maturation into secondary oocyte)
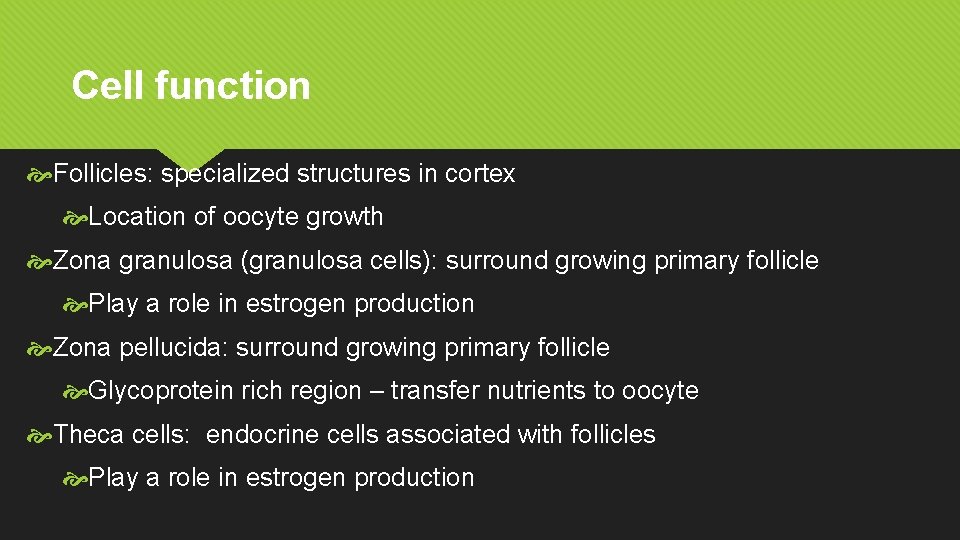
Cell function Follicles: specialized structures in cortex Location of oocyte growth Zona granulosa (granulosa cells): surround growing primary follicle Play a role in estrogen production Zona pellucida: surround growing primary follicle Glycoprotein rich region – transfer nutrients to oocyte Theca cells: endocrine cells associated with follicles Play a role in estrogen production
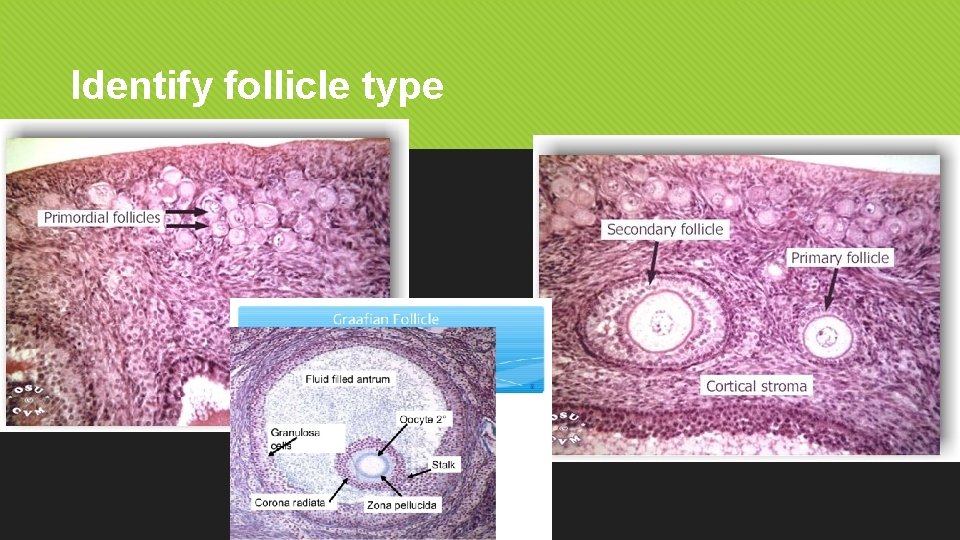
Identify follicle type
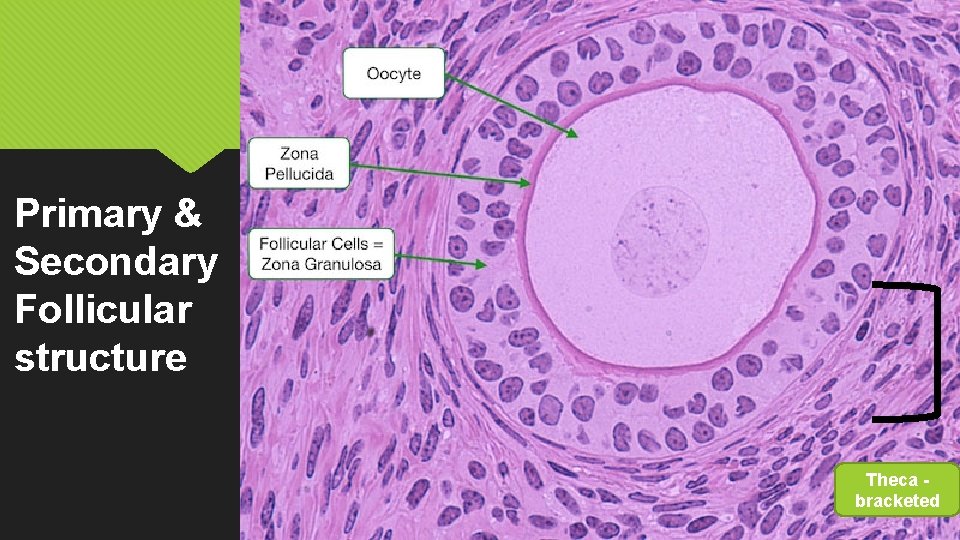
Primary & Secondary Follicular structure Theca bracketed
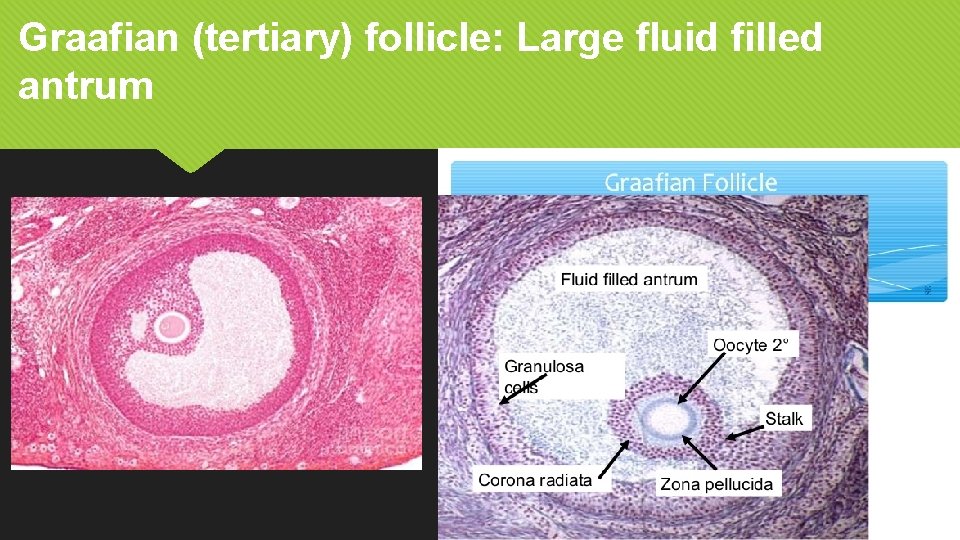
Graafian (tertiary) follicle: Large fluid filled antrum
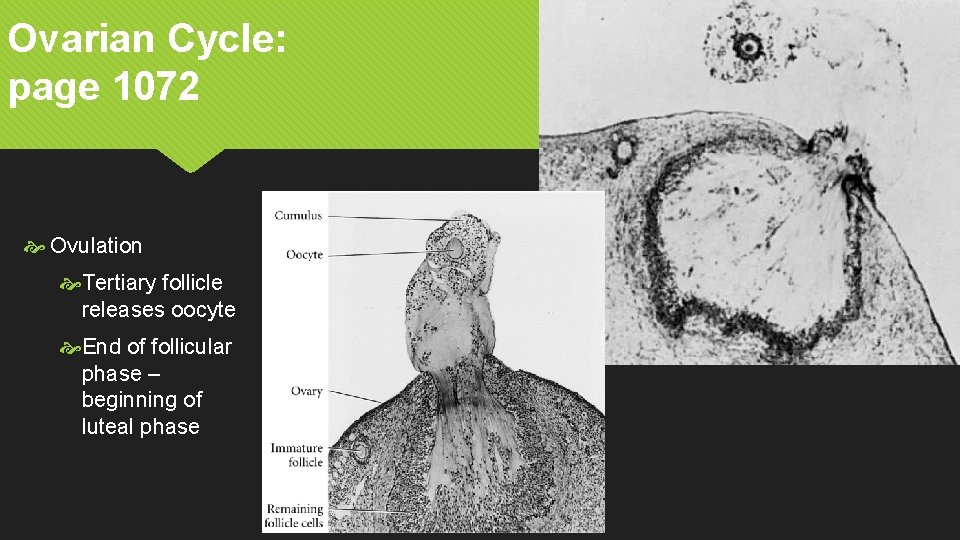
Ovarian Cycle: page 1072 Ovulation Tertiary follicle releases oocyte End of follicular phase – beginning of luteal phase
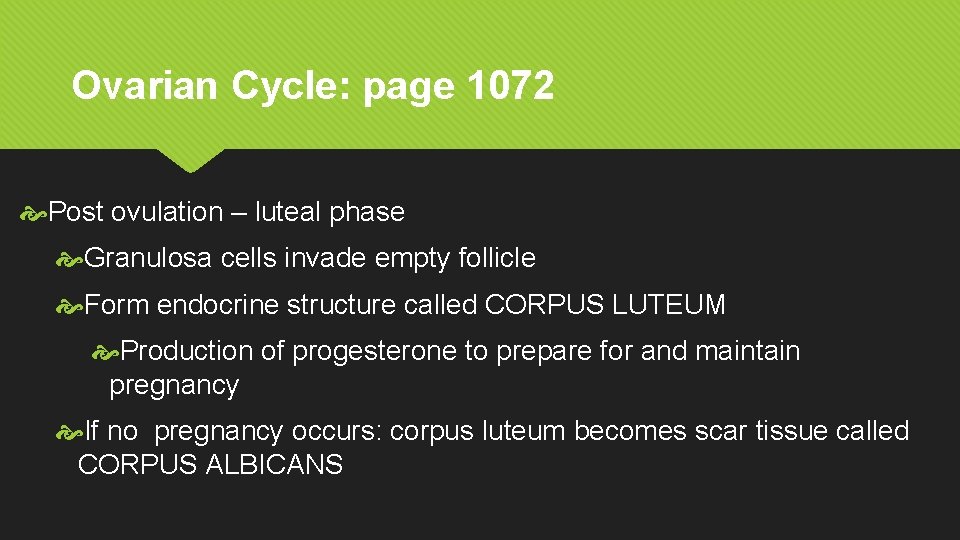
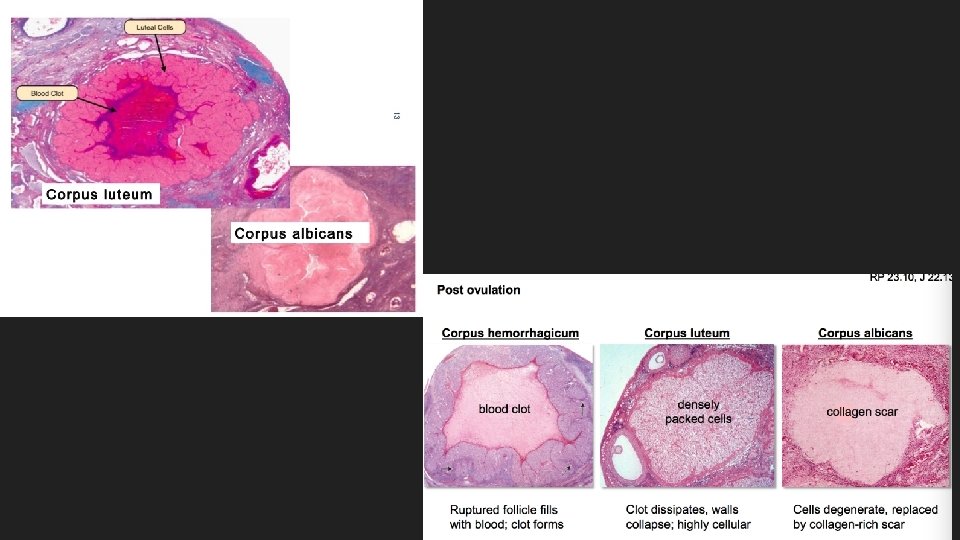
Ovarian Cycle: page 1072 Post ovulation – luteal phase Granulosa cells invade empty follicle Form endocrine structure called CORPUS LUTEUM Production of progesterone to prepare for and maintain pregnancy If no pregnancy occurs: corpus luteum becomes scar tissue called CORPUS ALBICANS
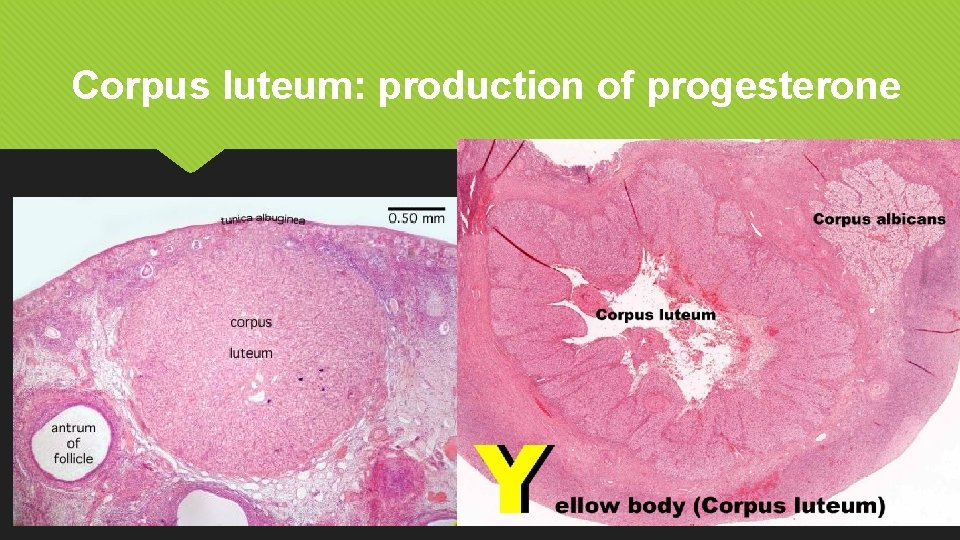
Corpus luteum: production of progesterone
Male Hormones
Male Hormones Gn. RH secreted by hypothalamus Acts on anterior pituitary Triggers release of LH & FSH DHT (type of androgen) Derived from conversion of testosterone stimulates the development of male characteristics
Male Hormones Inhibin secreted by Sertoli cells when sperm production is high Acts on anterior pituitary Inhibits release of FSH to slow down sperm production LH Secreted by anterior pituitary Activates Leydig/ interstitial cells to secrete testosterone
Male Hormones FSH Secreted by anterior pituitary Stimulates testicular growth Enhances the production of ABP by the Sertoli cells Activates seminiferous tubules to produce sperm (gamete production) ABP Secreted by Sertoli cells into lumen & ISF when sperm production is low Binds to testosterone to concentrate it - causing higher levels which enable spermatogenesis in the ST and sperm maturation in the epididymis.
Male Hormones Testosterone Secreted by Leydig cells Stimulates final stages of spermatogenesis Promotes development of secondary male sexual characteristics & sexual function Stimulation of anabolism (bone & muscle development) Prenatal development of male RS
Female Hormones
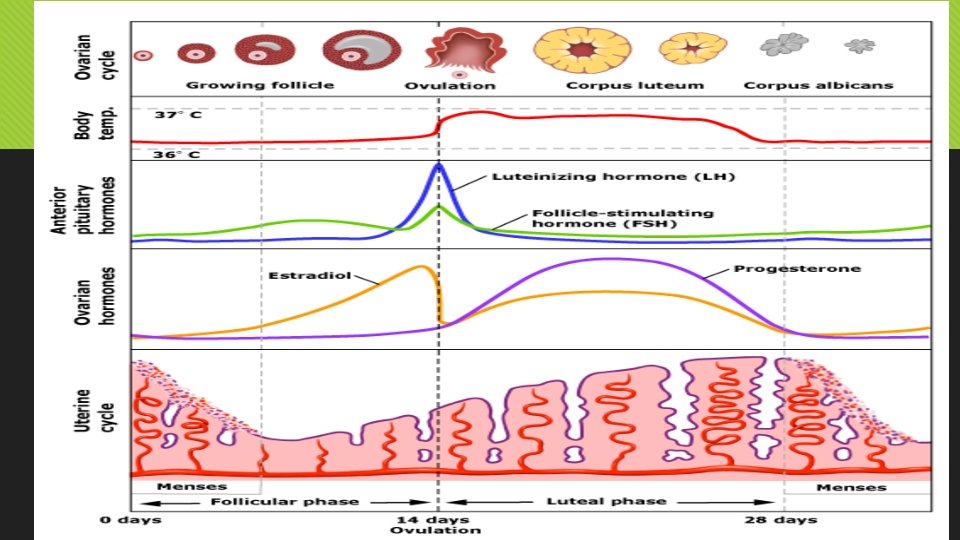
Female Hormones Gn. RH secreted by hypothalamus Acts on anterior pituitary Triggers release of LH & FSH Secreted by anterior pituitary stimulates follicles to grow & mature (egg/oocyte production)
Female Hormones LH Secreted by anterior pituitary triggers ovulation and corpus luteum formation Inhibin secreted by Granulosa cells Acts on anterior pituitary Inhibits release of FSH to regulate oogenesis
Female Hormones Relaxin Secreted by placenta & corpus luteum Prepares pubic symphysis and cervix to make it easier for baby to enter vaginal canal during birth Oxytocin Secreted by pituitary glands Triggers contraction of uterus during childbirth Triggers milk let down during lactation
Female Hormones Estrogen Secreted by thecal and granulosa cells secondary sexual characteristics Progesterone Secreted by corpus luteum Prepare uterus for pregnancy Stimulate uterine lining and secretions of glands

Cycles
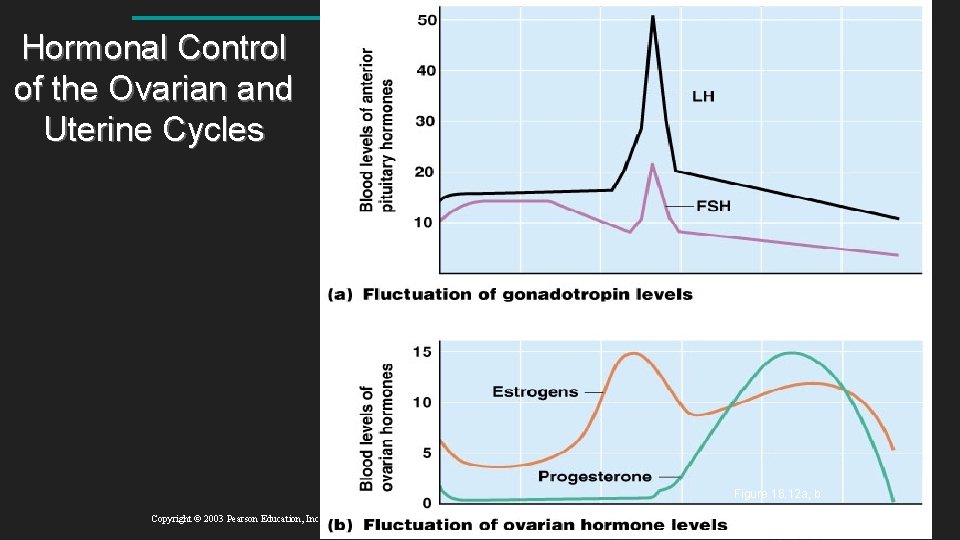
Hormonal Control of the Ovarian and Uterine Cycles Figure 16. 12 a, b Copyright © 2003 Pearson Education, Inc. publishing as Benjamin Cummings Slide
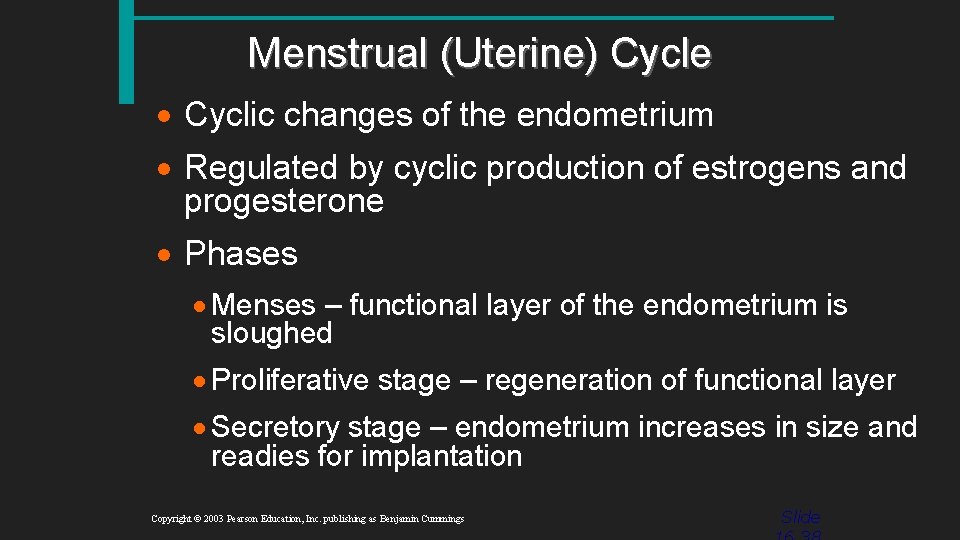
Menstrual (Uterine) Cycle · Cyclic changes of the endometrium · Regulated by cyclic production of estrogens and progesterone · Phases · Menses – functional layer of the endometrium is sloughed · Proliferative stage – regeneration of functional layer · Secretory stage – endometrium increases in size and readies for implantation Copyright © 2003 Pearson Education, Inc. publishing as Benjamin Cummings Slide
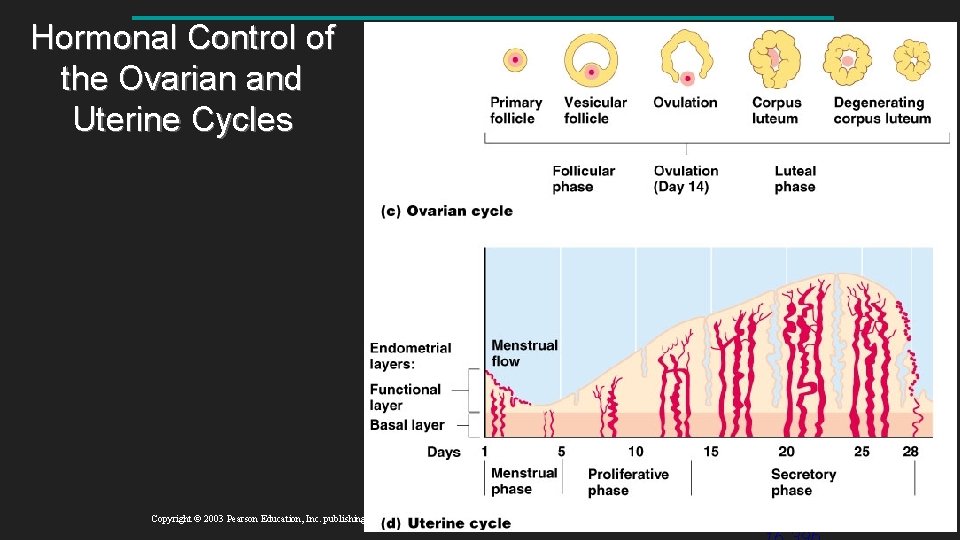
Hormonal Control of the Ovarian and Uterine Cycles Figure 16. 12 c, d Copyright © 2003 Pearson Education, Inc. publishing as Benjamin Cummings Slide

FYI
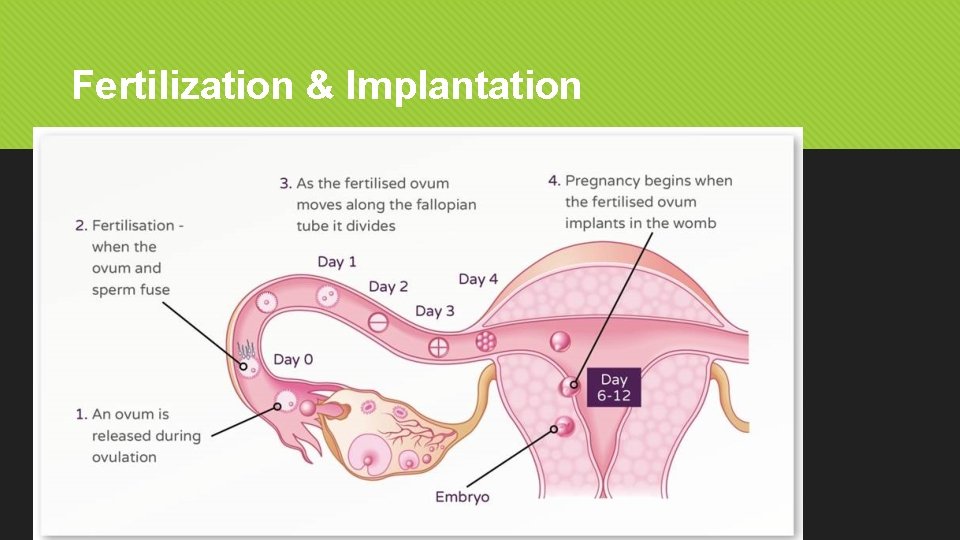
Fertilization & Implantation
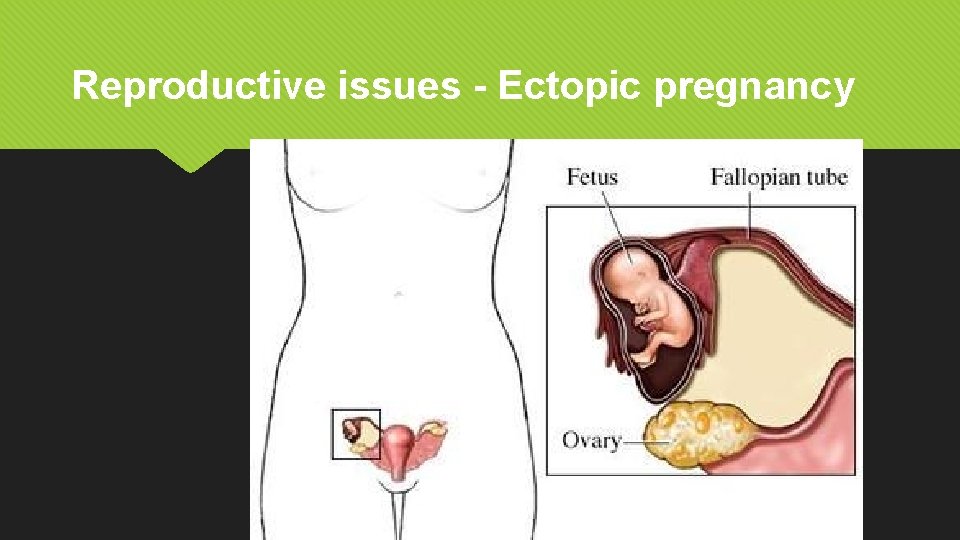
Reproductive issues - Ectopic pregnancy
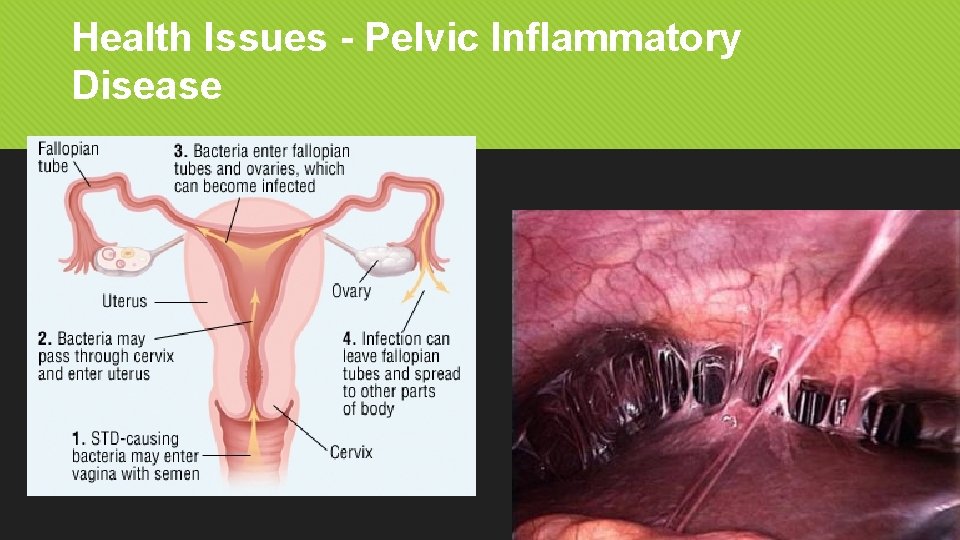
Health Issues - Pelvic Inflammatory Disease
- Slides: 47