BIOL 2402 Unit 2 Respiratory Physiology 4 distinct
BIOL 2402 Unit 2 Respiratory Physiology

4 distinct events – add to back of notes Pulmonary ventilation: air is moved in and out of the lungs External respiration: gas exchange between blood and alveoli Respiratory gas transport: CV system transports oxygen and carbon dioxide between lungs & tissues Internal respiration: gas exchange between blood & tissue cells Definition: Cellular respiration: actual use of oxygen & production of carbon dioxide in the cells
Overview of Respiration Chart – sketch on back of notes
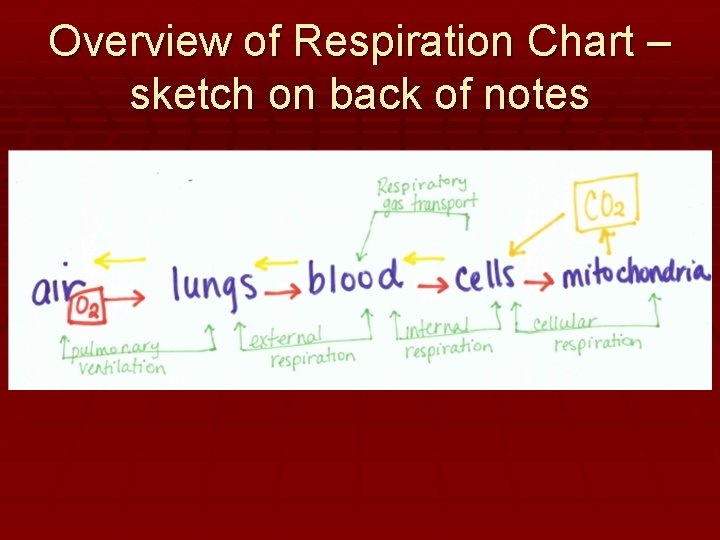
Pulmonary Ventilation
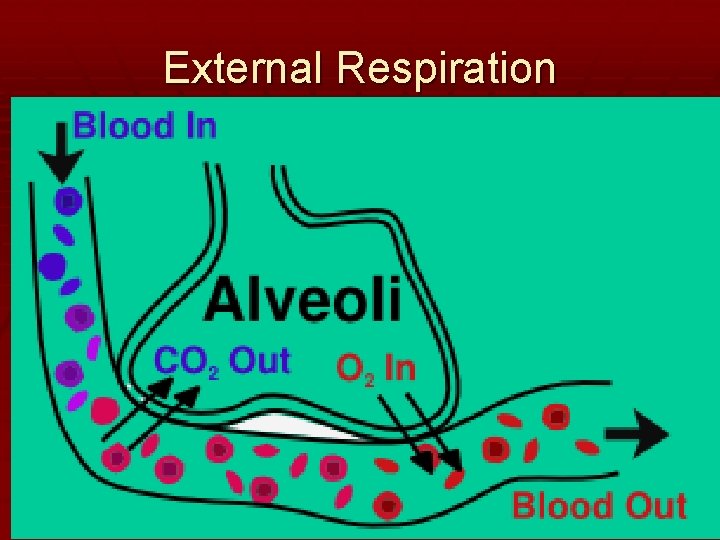
External Respiration
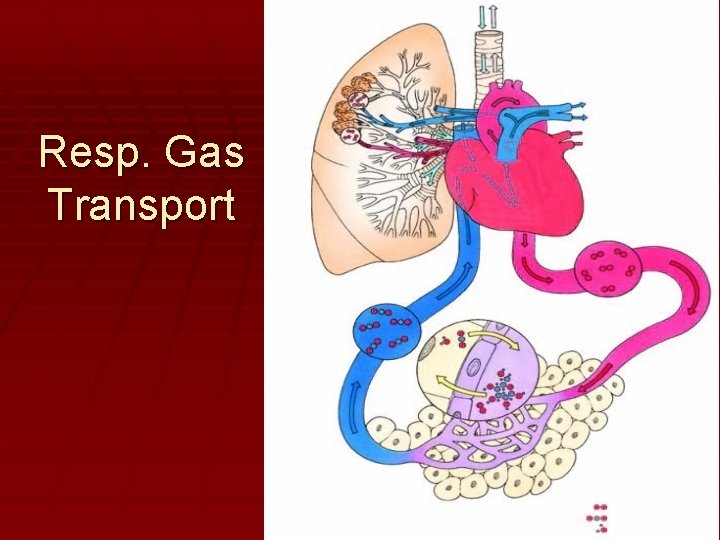
Resp. Gas Transport
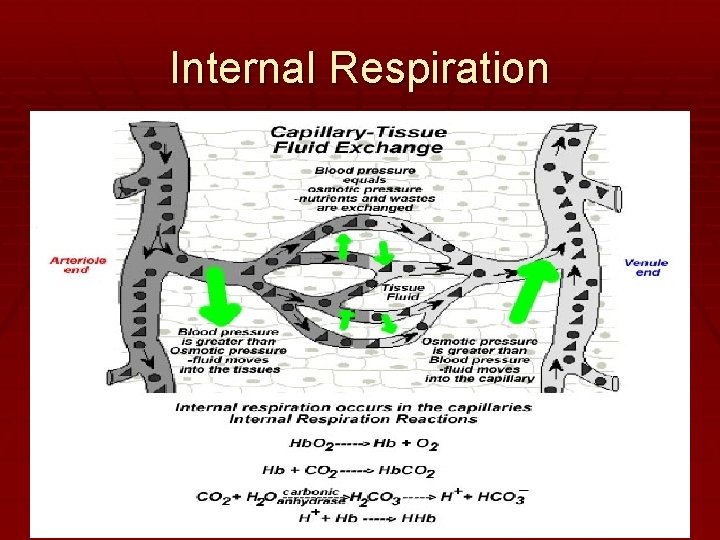
Internal Respiration
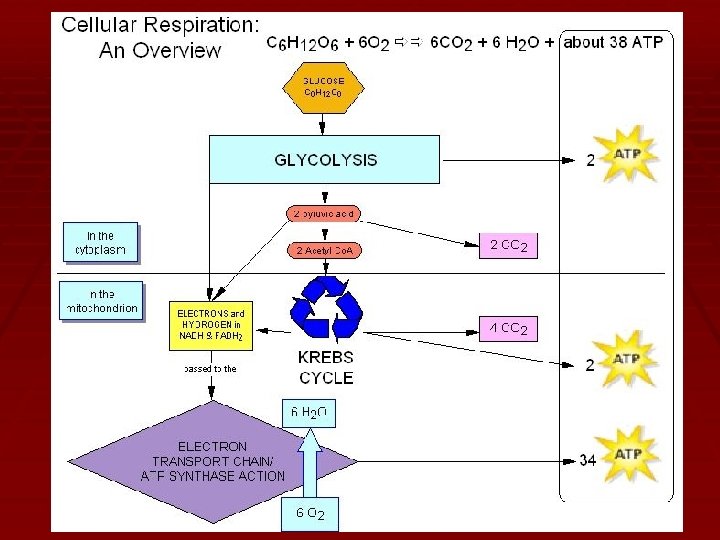
Cellular Respiration
Mechanics of Breathing Pages 10 -12(top)
Introduction Pulmonary ventilation: - Moving air into and out of the lungs Depends on pressure changes Breathing Inspiration = moving air into the lungs Expiration = moving air out of lungs
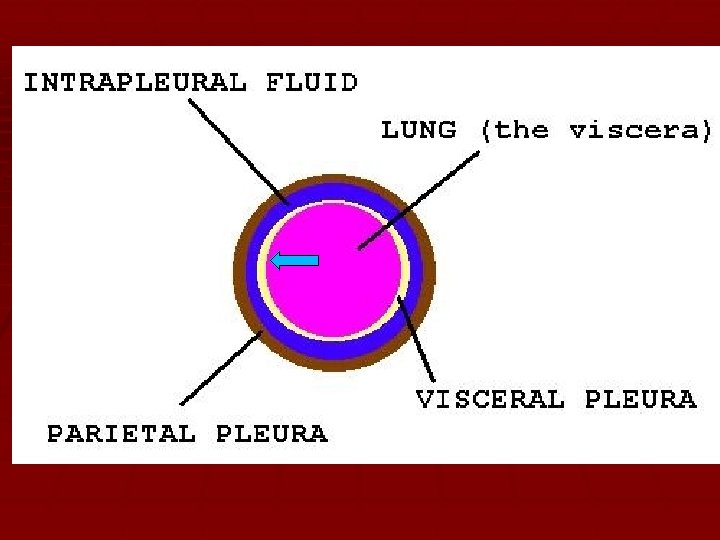
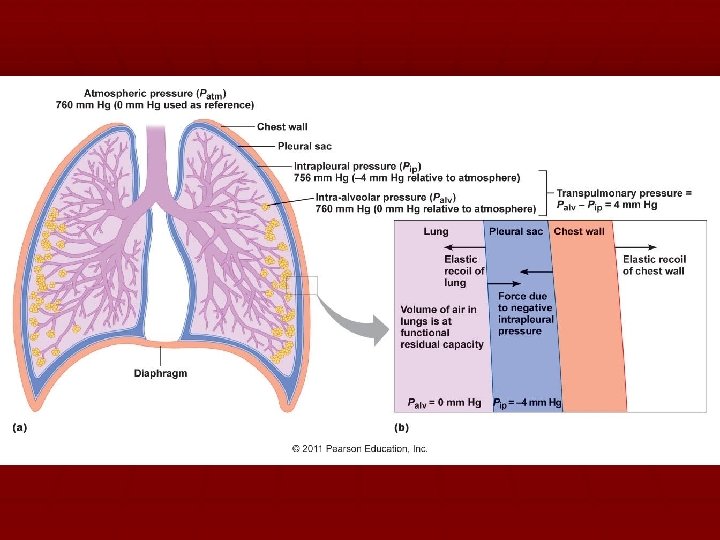
Pressure Relationships Intrapulmonary pressure (Ppul) Pressure within the alveoli (lungs) Fluctuates during phases of breathing Always equalizes itself with atmospheric pressure (Patm) Intrapleural pressure (Pip) Pressure within pleural cavity (between the pleural membranes ) Fluctuates during phases of breathing Always less than Ppul and Patm
Pressure Relationships • Transpulmonary pressure – the difference between Ppul and Pip • 4 mm. Hg • Allows alveoli to remain open and prevents lung from collapsing
Pressure Relationships All respiratory pressures are relative to Patm Negative respiratory pressure: Presp less than Patm Causes inhalation Postive respiratory pressure: Presp greater than Patm Causes exhalation
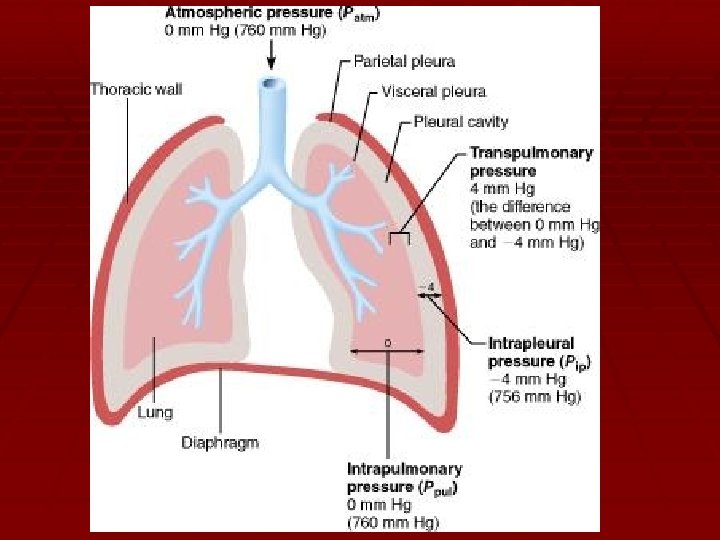
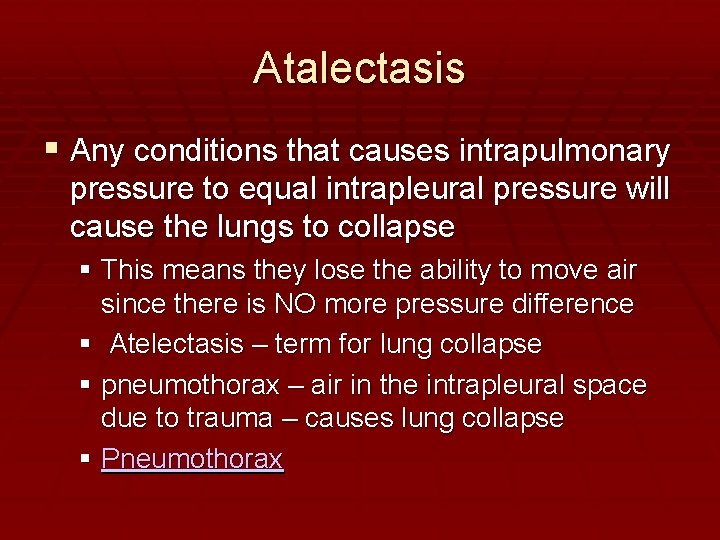
Atalectasis Any conditions that causes intrapulmonary pressure to equal intrapleural pressure will cause the lungs to collapse This means they lose the ability to move air since there is NO more pressure difference Atelectasis – term for lung collapse pneumothorax – air in the intrapleural space due to trauma – causes lung collapse Pneumothorax
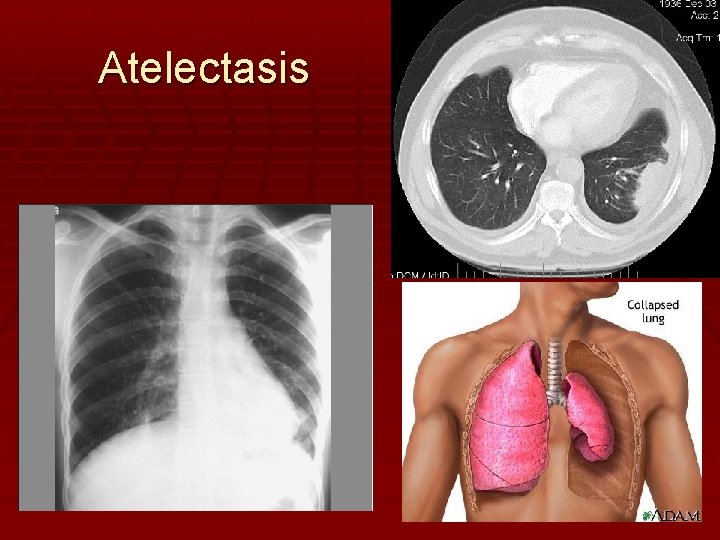
Atelectasis

Pulmonary ventilation Volume changes lead to pressure changes which lead to the flow of gases to equalize the pressure Boyle’s law: Pressure & Volume vary inversely P 1 V 1 = P 2 V 2
Inhalation/inspiration Main inspiratory muscles Diaphragm & external intercostals Thoracic dimensions change to increase volume of thoracic cavity by 0. 5 liters Intrapulmonary pressure drops 1 -3 mm. Hg and air rushes info normal quiet inspiration A deep forced inspiration requires activation of accessory muscles
Expiration A passive process dependent on natural lung elasticity The lungs recoil, volume decreases, alveoli compress, intrapulmonary pressure rises, gas outflows to equalize the pressure with atmospheric pressure Forced expiration requires contraction of muscles of the abdominal wall
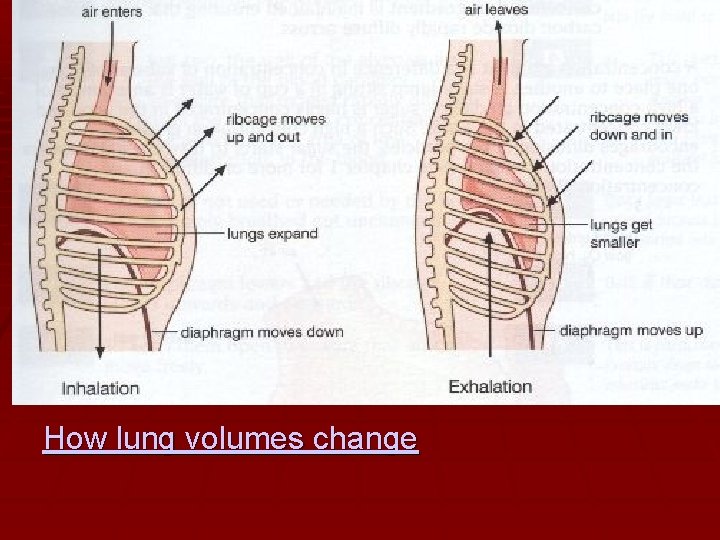
How lung volumes change

Respiratory Sounds Bronchial sounds: produced by air rushing through trachea & bronchi Vesicular sounds: produced by air filling alveoli See Practical Clinical Skills Website
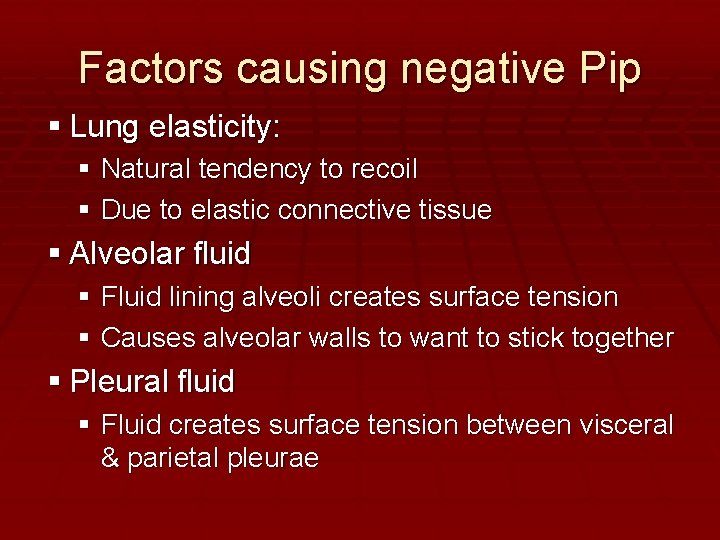
Factors causing negative Pip Lung elasticity: Natural tendency to recoil Due to elastic connective tissue Alveolar fluid Fluid lining alveoli creates surface tension Causes alveolar walls to want to stick together Pleural fluid Fluid creates surface tension between visceral & parietal pleurae
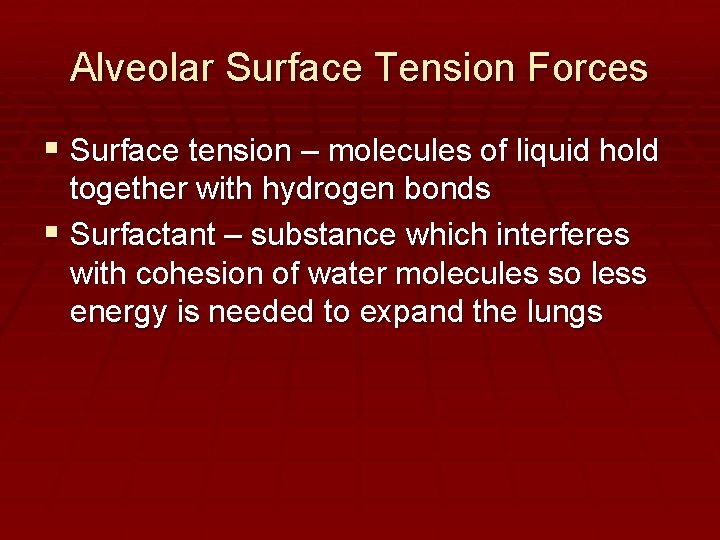
Alveolar Surface Tension Forces Surface tension – molecules of liquid hold together with hydrogen bonds Surfactant – substance which interferes with cohesion of water molecules so less energy is needed to expand the lungs
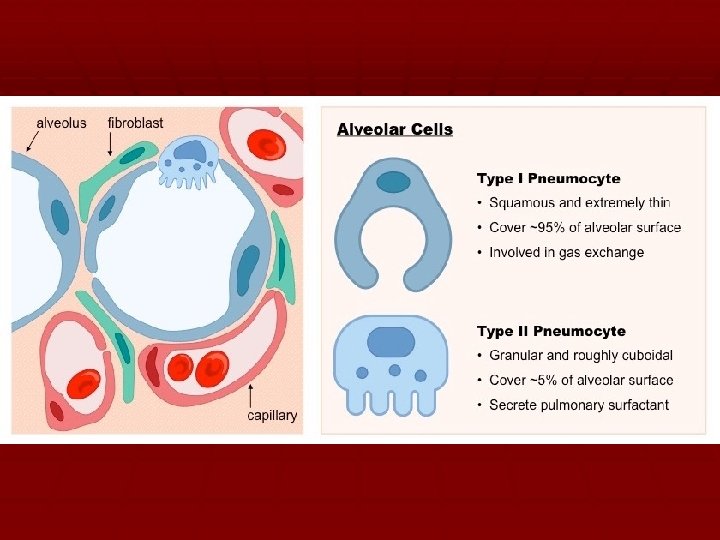
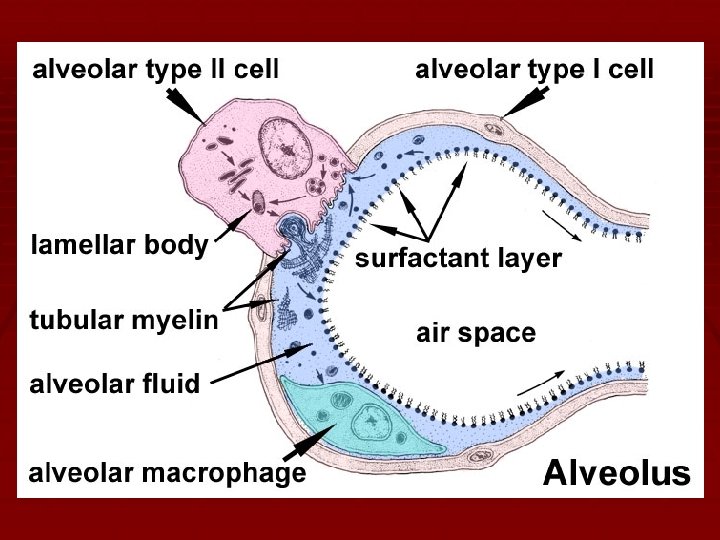
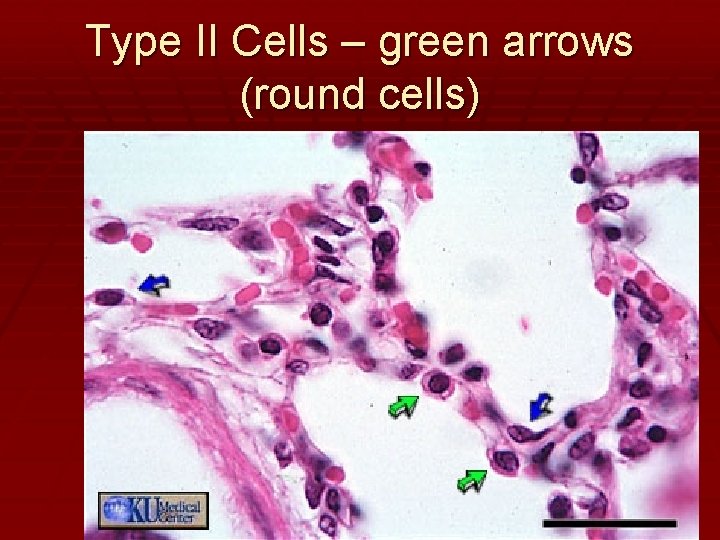
Type II Cells – green arrows (round cells)
Gas Exchanges in the Body External & Internal Respiration Page 12 -13
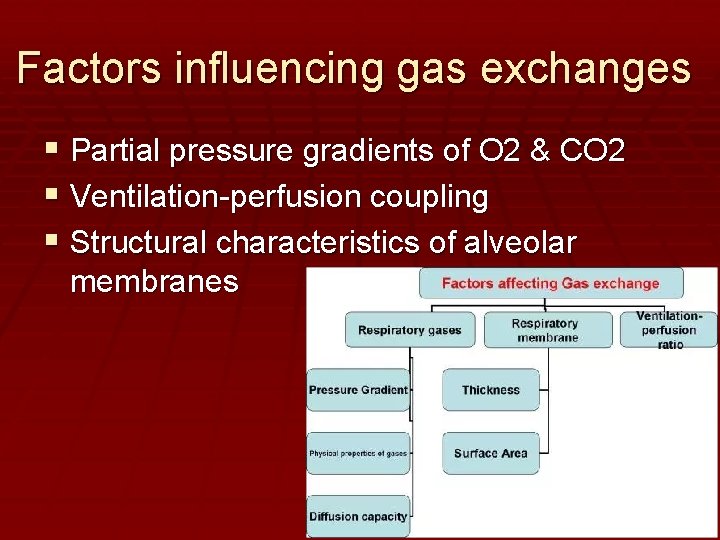
Factors influencing gas exchanges Partial pressure gradients of O 2 & CO 2 Ventilation-perfusion coupling Structural characteristics of alveolar membranes
Partial pressure gradients Gas exchanges occur: Between the blood and the alveoli AND Between the blood and the tissue cells Takes place by simple diffusion Depends on partial pressure gradients of oxygen & carbon dioxide that exist on opposite sides of the exchange membrane (Dalton’s law of partial pressures) Always move from high to low pressures
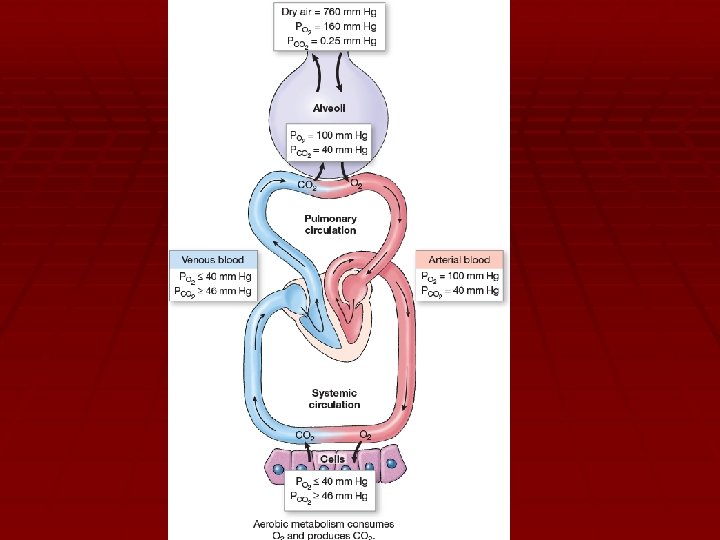
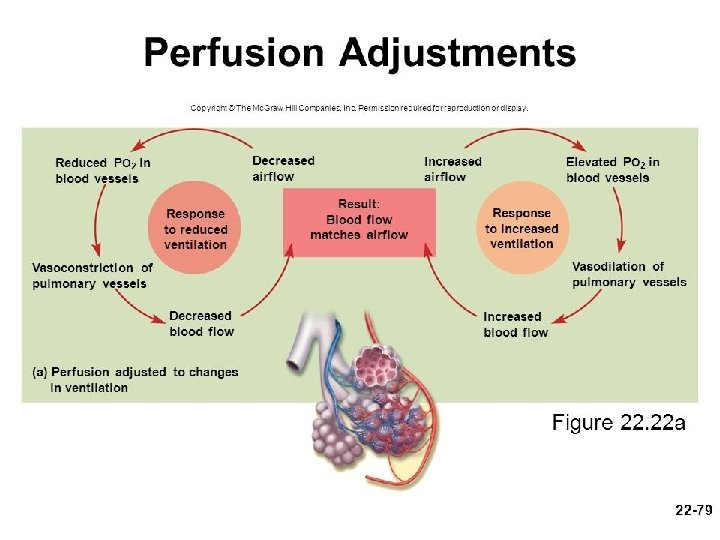
Ventilation-perfusion coupling Ventilation = amount of gas in the alveoli Perfusion = amount of blood flow in pulmonary capillaries Equivalent concentrations of O 2 & CO 2 diffuse from blood to/from alveoli while blood flows through capillaries at a steady rate Accomplished via vasoconstriction & vasodilation of pulmonary arterioles
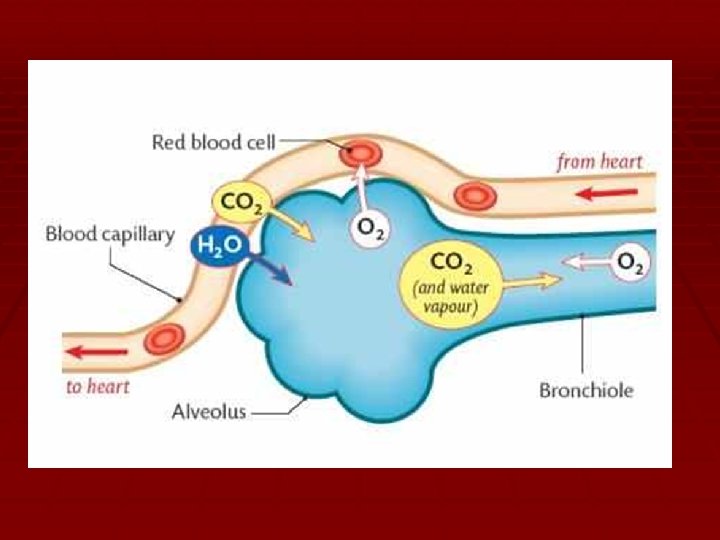
Structural Characteristics of Respiratory Membranes Thickness of respiratory membranes 0. 5 to 1. 0 micrometers Surface area available

Control of Respiration
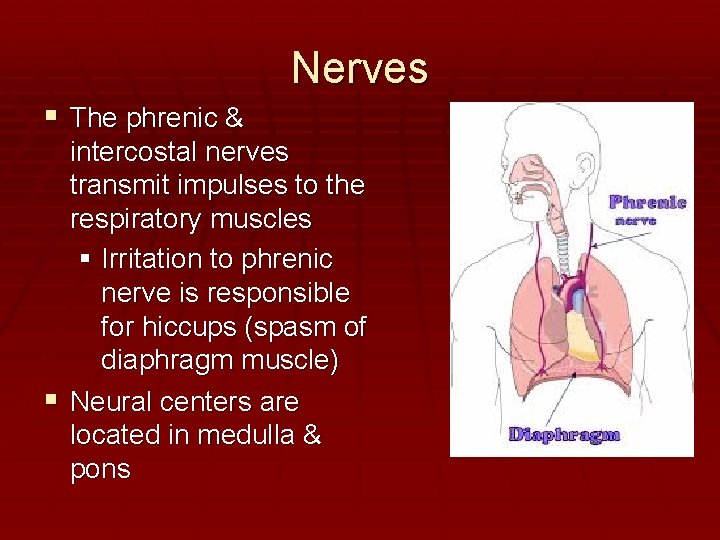
Nerves The phrenic & intercostal nerves transmit impulses to the respiratory muscles Irritation to phrenic nerve is responsible for hiccups (spasm of diaphragm muscle) Neural centers are located in medulla & pons
Breathing Terms Eupnea = normal respiration rate Approx 12 -15 breaths per min Hyperpnea = higher than normal rate Apnea = No rate Dyspnea = general term for abnormal rate Physical factors, conscious control, emotional factors, and chemical factors all influence rate & depth of breathing.
DISCUSSION QUESTION ON TEST: BE ABLE TO DISCUSS/EXPLAIN THE CONDITIONS OF HYPER & HYPOVENTILIATION
Hyperventilation Deep & rapid respiration Too much CO 2 is vented out of the body Not enough acid production H 2 O + CO 2 H 2 CO 3 (carbonic acid) Respiratory alkalosis results
Hyperventilation treatment Trap CO 2 and rebreathe it – building back up the levels of CO 2 until they are normal again. H 2 O + CO 2 H 2 CO 3 reverses equation to make more acid
Hypoventilation Slow & shallow respiration (usually caused by a disease process) Not adequate expiration so CO 2 is not vented out of the body Production of excess acid H 2 O + CO 2 H 2 CO 3 (carbonic acid) Respiratory acidosis results
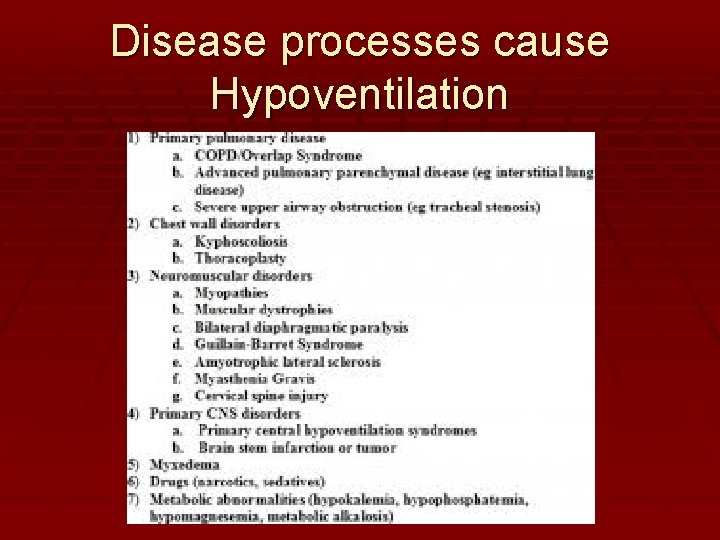
Disease processes cause Hypoventilation
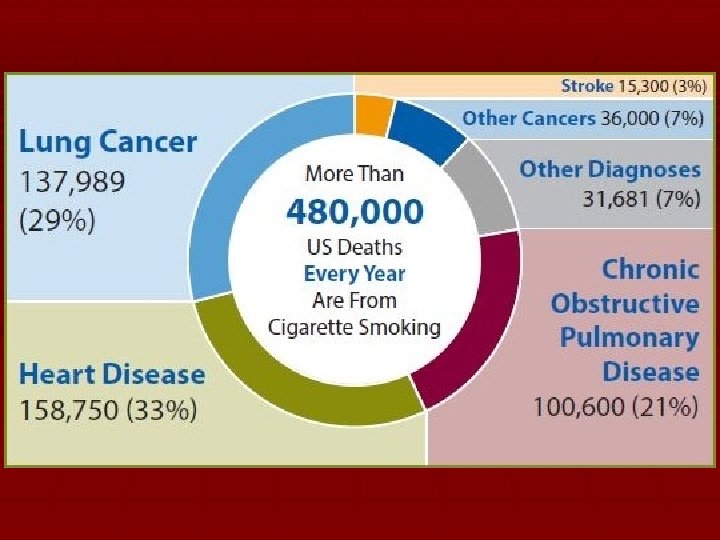
EFFECTS OF SMOKING
Smoking vs. Vaping
Disorders of Respiratory System This is FYI stuff. You will not be tested over this material.
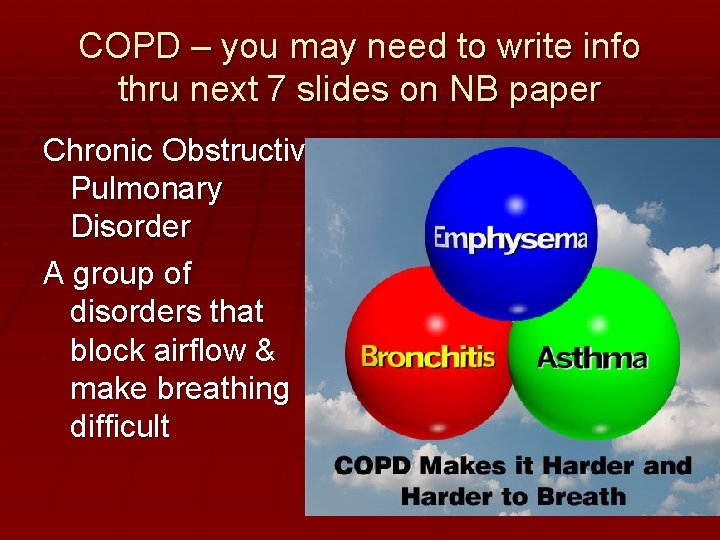
COPD – you may need to write info thru next 7 slides on NB paper Chronic Obstructive Pulmonary Disorder A group of disorders that block airflow & make breathing difficult
4 features in common Both emphysema and chronic bronchitis have: Smoking history Dyspnea = air hunger due to dysfunctional breathing Coughing & pulmonary infections Will develop respiratory failure, hypoxia, acidosis
Chronic Bronchitis Symptoms: inflammation of mucosa – chronic mucus production Impairs ventilation and gas exchange Reduction of airway diameter AKA. “blue bloater” – hypoxia leads to cyanosis – CO 2 retention leads to hyperinflation of chest wall Causative factors: cigarette smoking
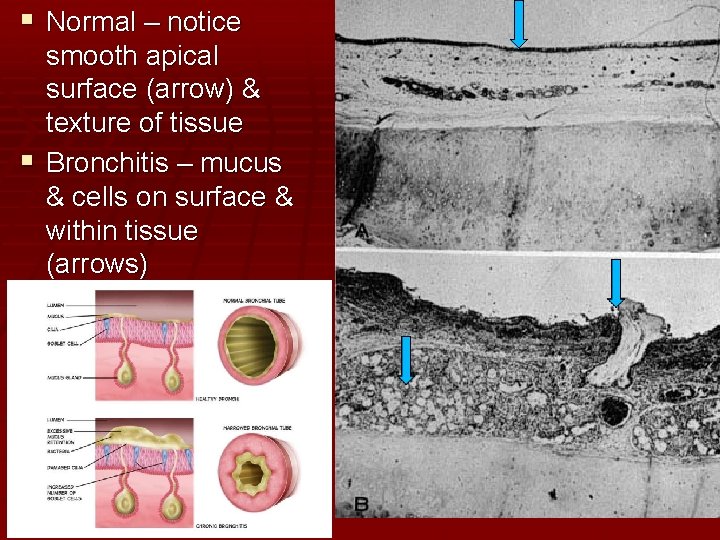
Normal – notice smooth apical surface (arrow) & texture of tissue Bronchitis – mucus & cells on surface & within tissue (arrows)
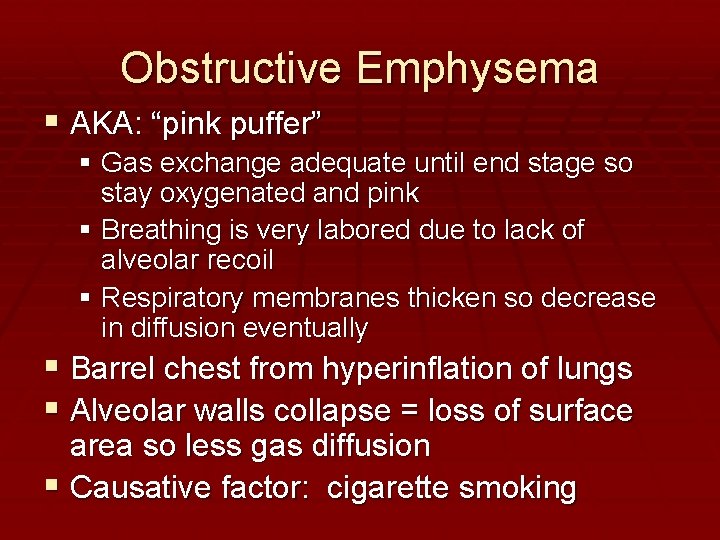
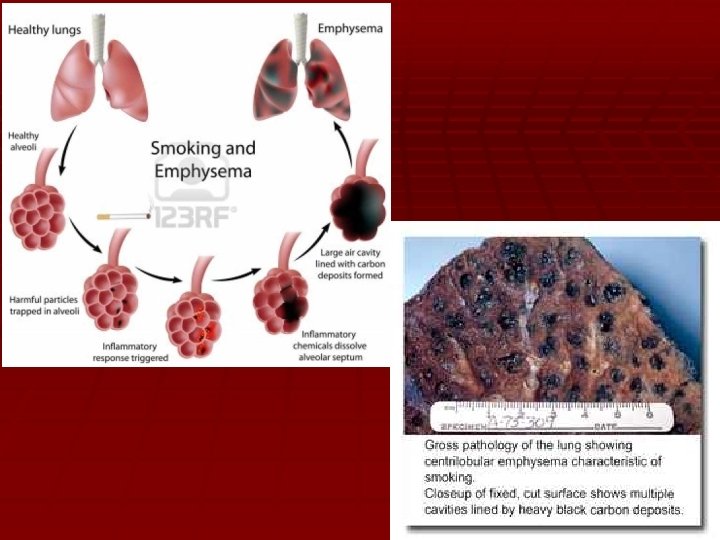
Obstructive Emphysema AKA: “pink puffer” Gas exchange adequate until end stage so stay oxygenated and pink Breathing is very labored due to lack of alveolar recoil Respiratory membranes thicken so decrease in diffusion eventually Barrel chest from hyperinflation of lungs Alveolar walls collapse = loss of surface area so less gas diffusion Causative factor: cigarette smoking
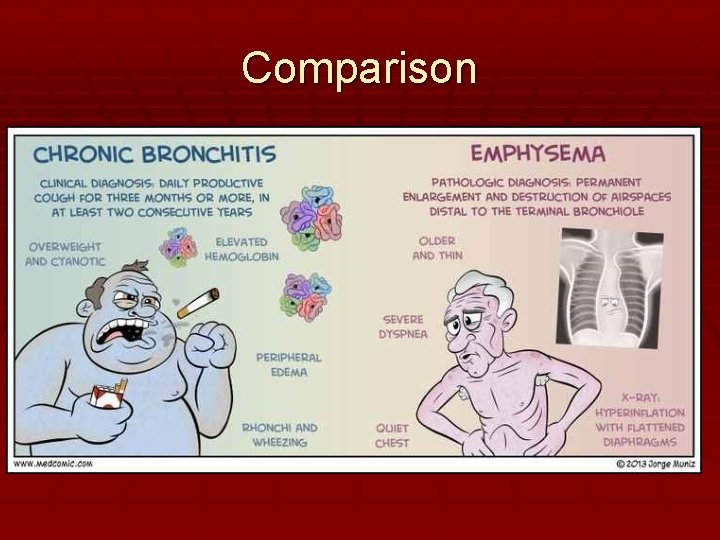
Comparison
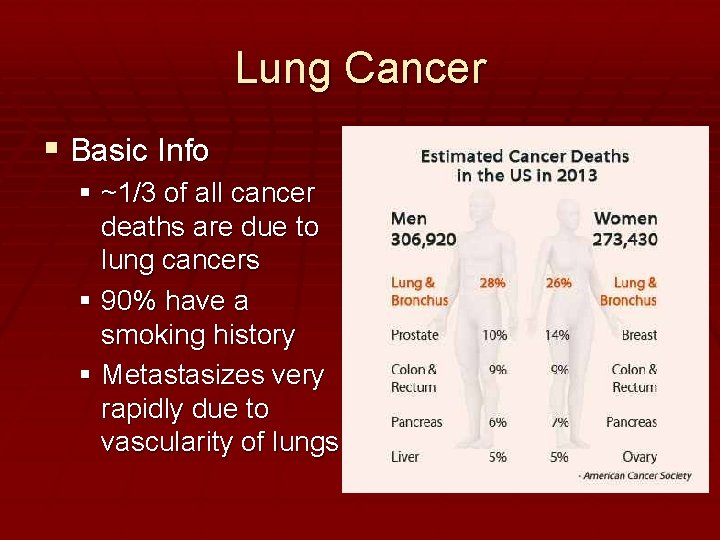
Lung Cancer Basic Info ~1/3 of all cancer deaths are due to lung cancers 90% have a smoking history Metastasizes very rapidly due to vascularity of lungs
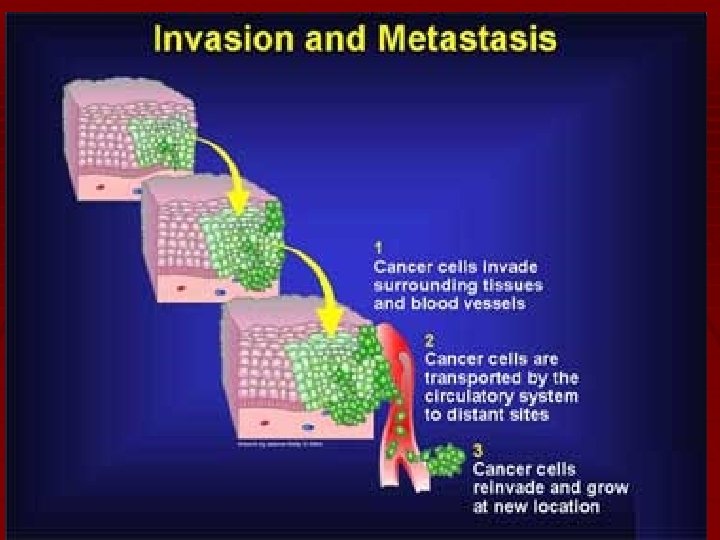
Metastasis
3 types of lung cancer Read the article in the textbook on page 420 about smoking and lung cancer. Then continue on to the next slides to learn about: Squamous cell carcinoma Adenocarcinoma Oat cell (small cell) carcinoma Be able to recognize them by fact AND by picture (pictures will be on lab practical!)
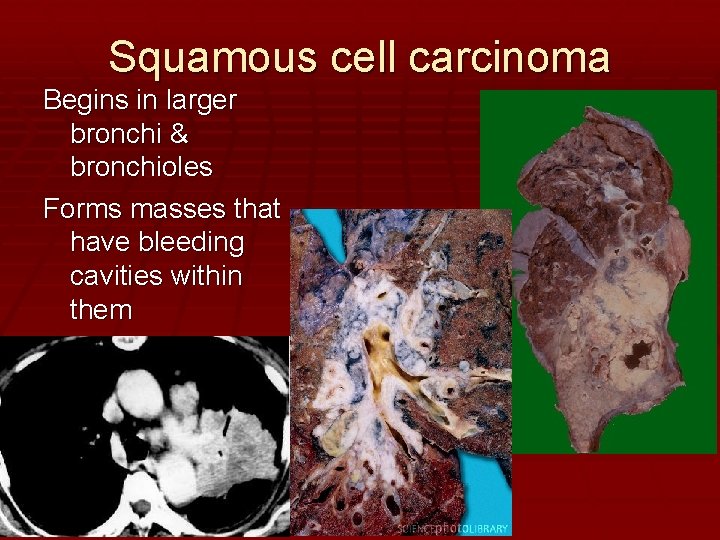
Squamous cell carcinoma Begins in larger bronchi & bronchioles Forms masses that have bleeding cavities within them
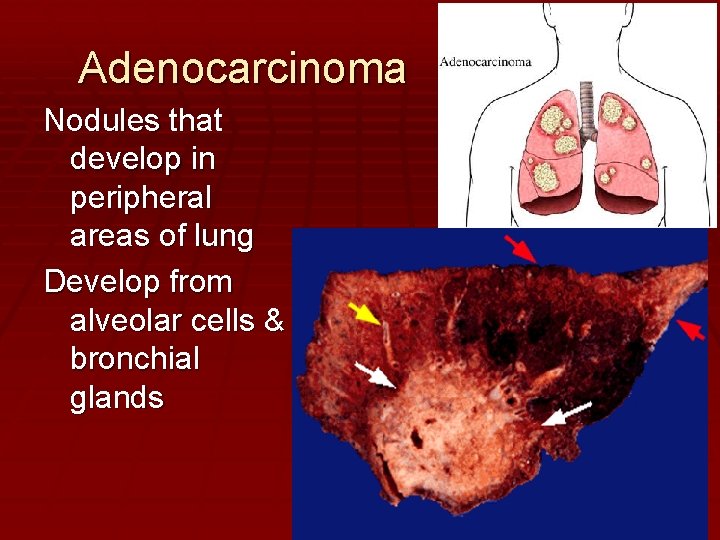
Adenocarcinoma Nodules that develop in peripheral areas of lung Develop from alveolar cells & bronchial glands
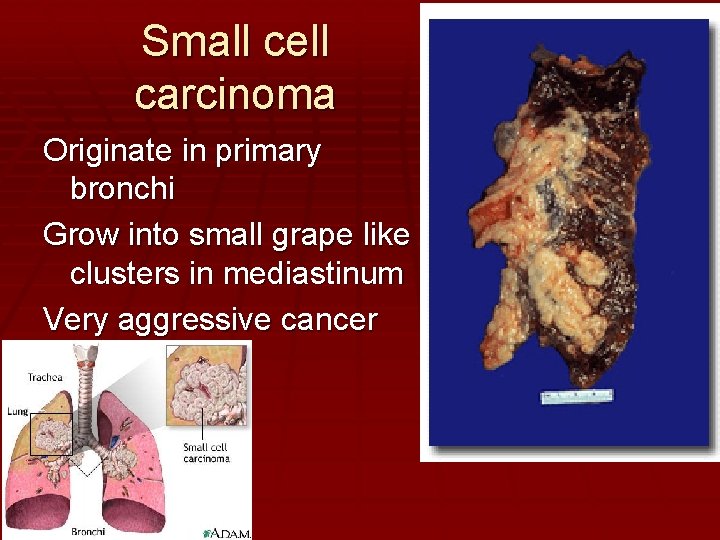
Small cell carcinoma Originate in primary bronchi Grow into small grape like clusters in mediastinum Very aggressive cancer
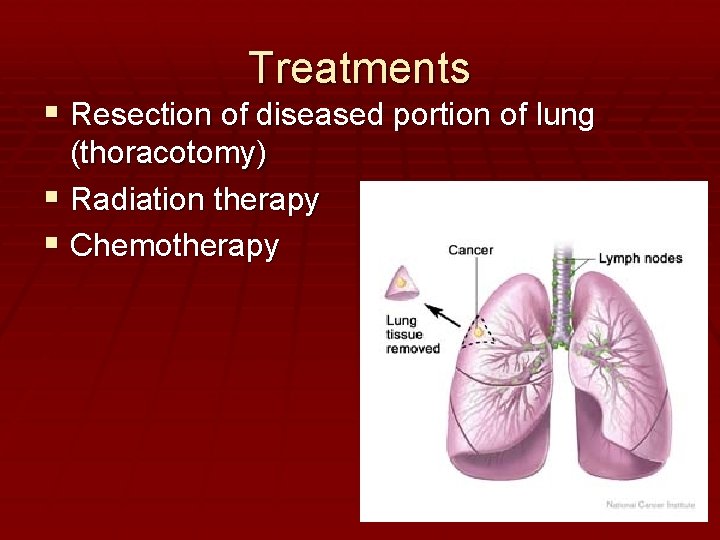
Treatments Resection of diseased portion of lung (thoracotomy) Radiation therapy Chemotherapy
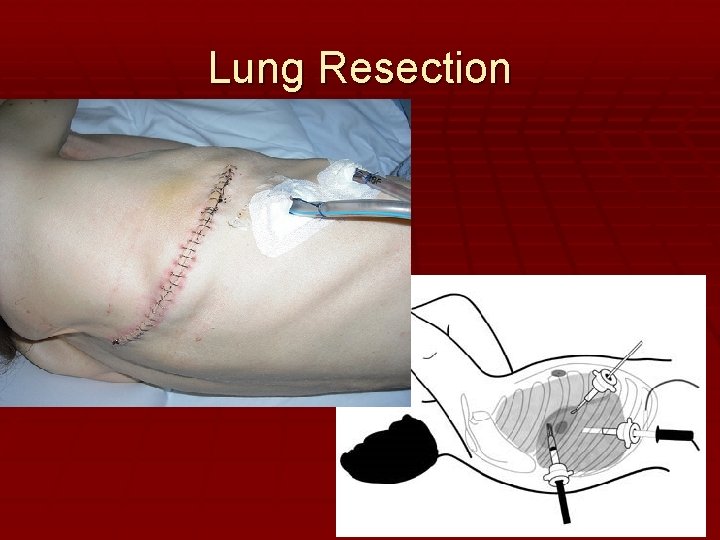
Lung Resection
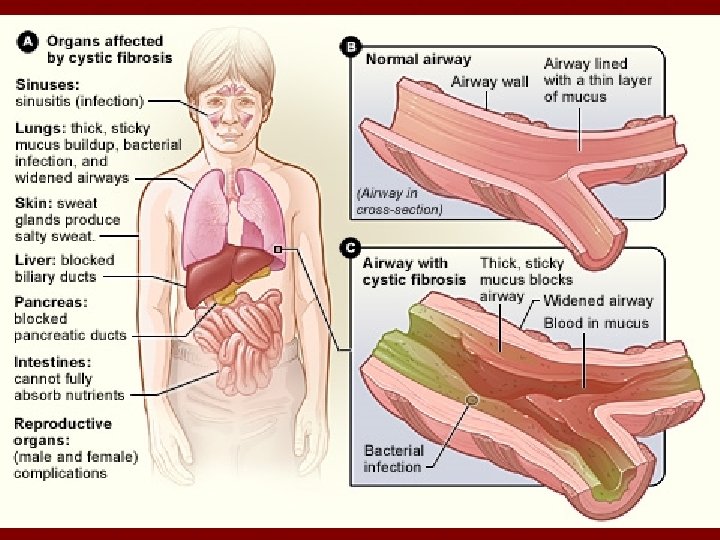
Cystic Fibrosis • Genetic disorder – recessive • Causes oversecretion of thick mucus that clogs respiratory passages & other organs • Impairs food digestion by clogging ducts that secrete enzymes
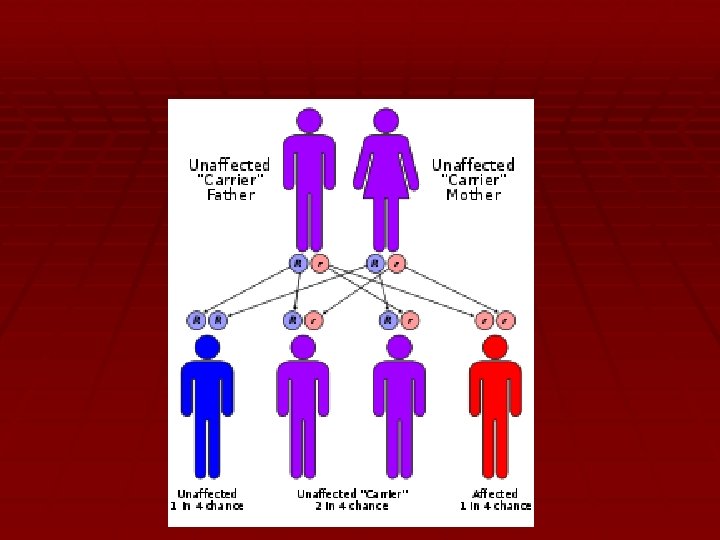
Cystic Fibrosis
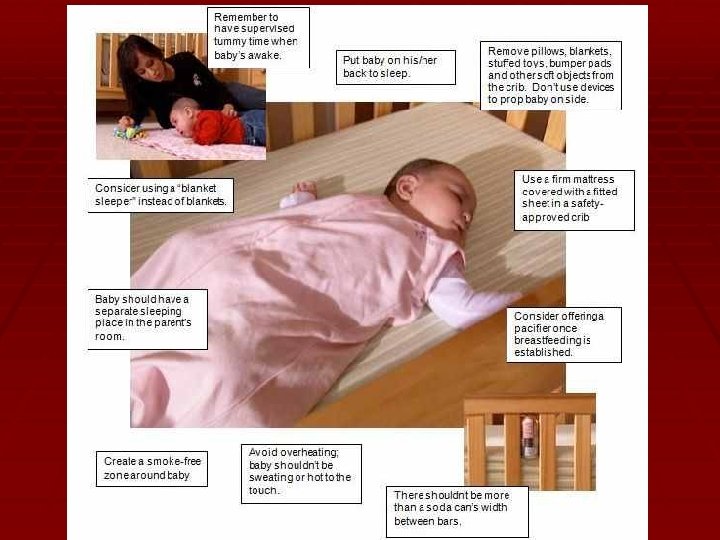
SIDS - Sudden Infant Death Syndrome • Sudden, unexplained death of an infant less than 1 year old • Possibly caused by brain abnormalities that control respiration, heart rate, or consciousness • Environmental factors to reduce risks – sleep on back not on stomach, firm crib with no blankets or stuffed animals or pillows • Sudden infant death syndrome (SIDS): Risk factors - Mayo. Clinic. com
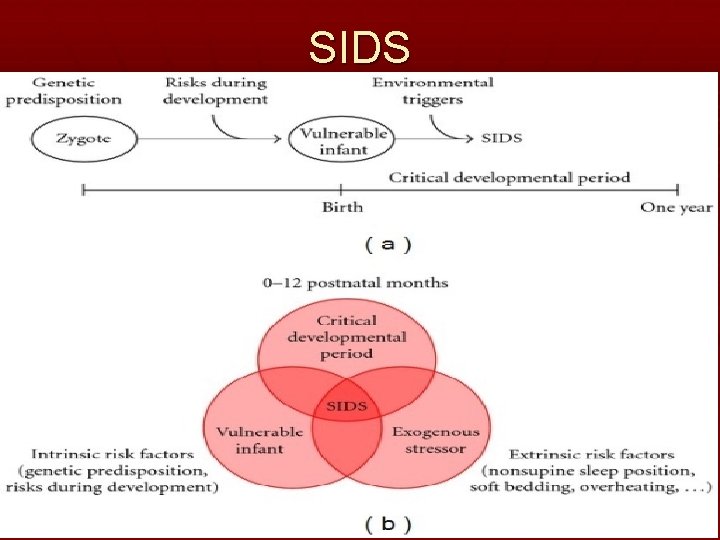
SIDS
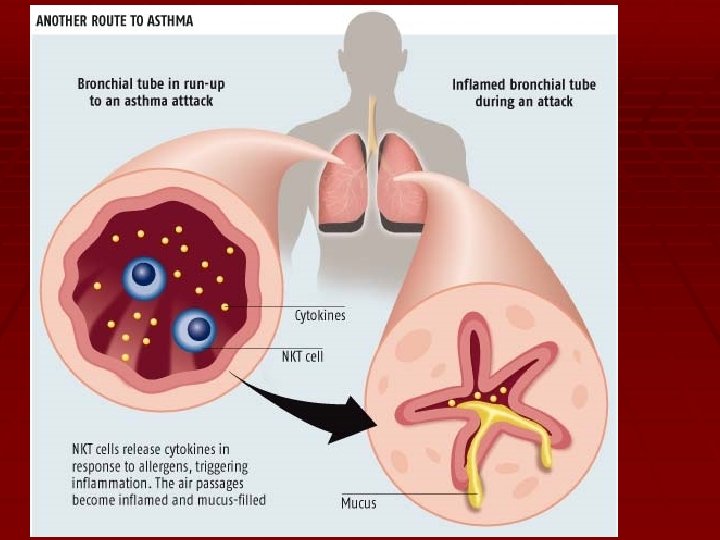
Asthma • Chronically inflamed hypersensitive bronchial passageways (one of the COPD diseases) • Bronchoconstriction of passageways in response to allergen, temperature changes, & exercise • Can be managed with medication
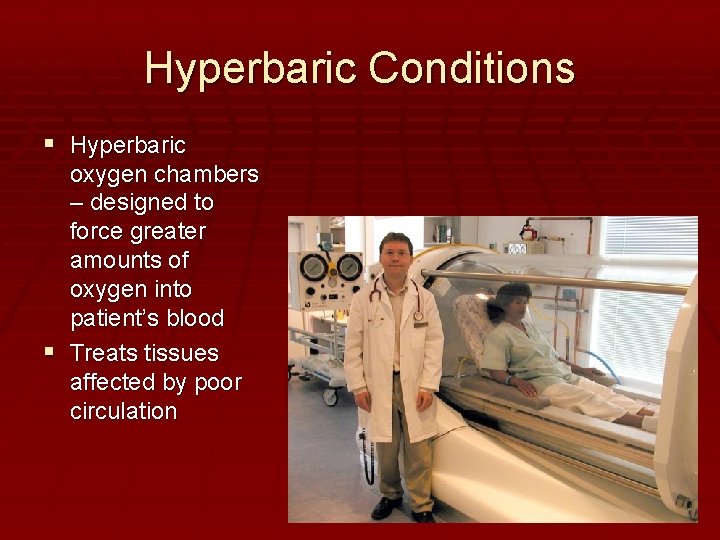
Hyperbaric Conditions Hyperbaric oxygen chambers – designed to force greater amounts of oxygen into patient’s blood Treats tissues affected by poor circulation
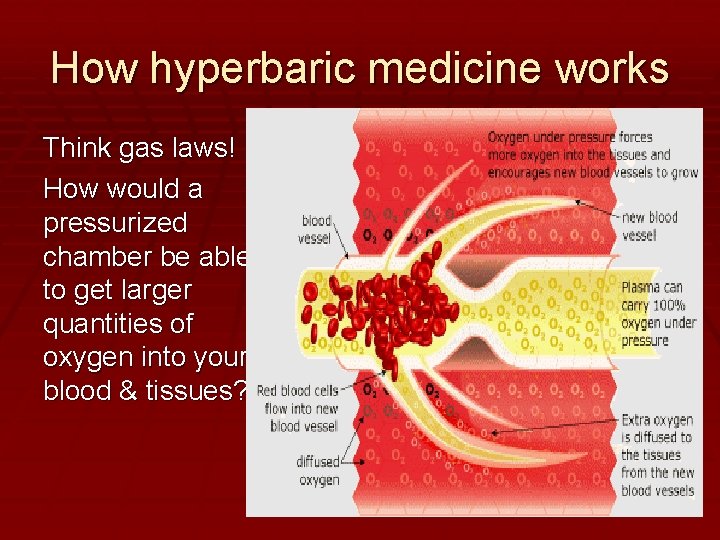
How hyperbaric medicine works Think gas laws! How would a pressurized chamber be able to get larger quantities of oxygen into your blood & tissues?
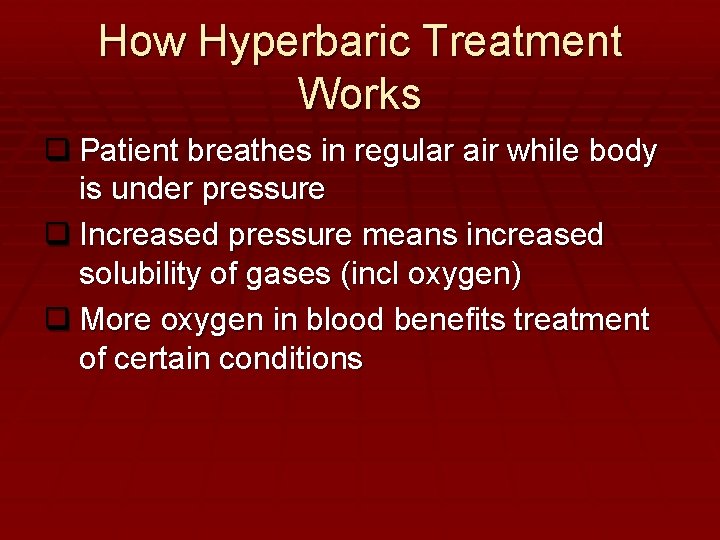
How Hyperbaric Treatment Works q Patient breathes in regular air while body is under pressure q Increased pressure means increased solubility of gases (incl oxygen) q More oxygen in blood benefits treatment of certain conditions
HBOT used to treat: Tetanus Gangrene Migraines Slow healing wounds Burns/skin grafts Stroke Autism Traumatic Brain Injury Decompression Sickness Cerebral Palsy Multiple Sclerosis Fibromyalgia Many other conditions
Scuba Diving The Physics of Diving - Scuba Gas Laws • As you go down in depth, the water puts pressure on your body • Increased pressure = increased solubility of inhaled gases into the blood • Be able to discuss/explain what happens to pressures & solubilities during scuba diving!
Scuba Diving • As you come up at the correct rate, the pressure decreases slowly • So the solubility decreases slowly • So the gases come out of the blood • And you can exhale them
Scuba Diving • If you come up too rapidly, the pressure decreases rapidly • So the solubility decreases rapidly • So the gases come out of the blood too fast to exhale them properly • The excess gas bubbles can collect in joint spaces, arteries, tissues, etc. causing coronary, pulmonary, or brain embolisms
Nitrogen Narcosis • As you descend under the water, the pressure on your body increases, so more nitrogen and oxygen dissolve in your blood. Most of the oxygen gets consumed by your tissues, but the nitrogen remains dissolved. • Excess nitrogen causes a feeling of euphoria similar to laughing gas – impairs judgement
Decompression Sickness • DCS arises when the pressure gradient for nitrogen leaving the tissues is so great that large bubbles form in venous circulation • DCS symptoms are wide-ranging: from skin mottling to mild tingling in the hands or feet to shock and death • Recompression in hyperbaric chamber is only effective treatment
High Altitude Sickness • The higher the altitude, the less the amount of oxygen present in the air. • Headache and difficulty breathing are initial symptoms. • HA pulmonary edema and HA cerebral edema are life threatening symptoms. • Body responds over time by increasing erythropoiesis to give body greater oxygen carrying capacity.
Eustachian tubes: FYI Auditory or eustachian tubes provide an avenue for equalizing middle ear pressure with atmospheric pressure via the flow of gases Air will either move in or out of your ears to cause this equalization This is the cause of your ears “popping”
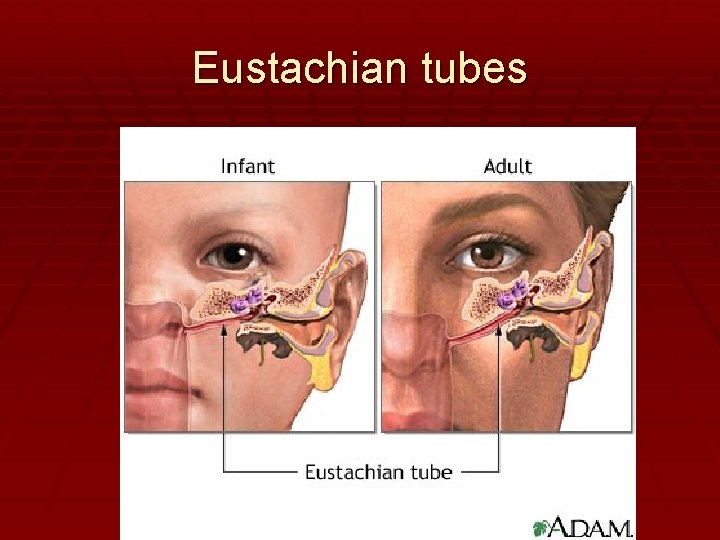
Eustachian tubes
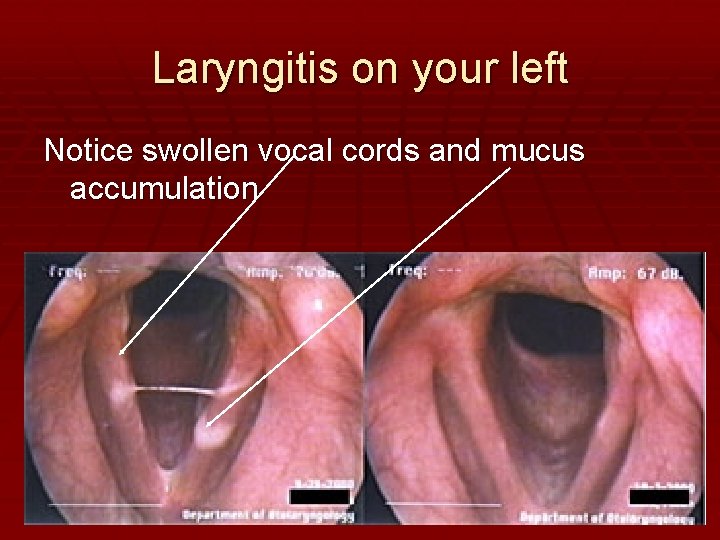
Laryngitis on your left Notice swollen vocal cords and mucus accumulation
Developmental Aspects Read through the Developmental Aspects section of your notes
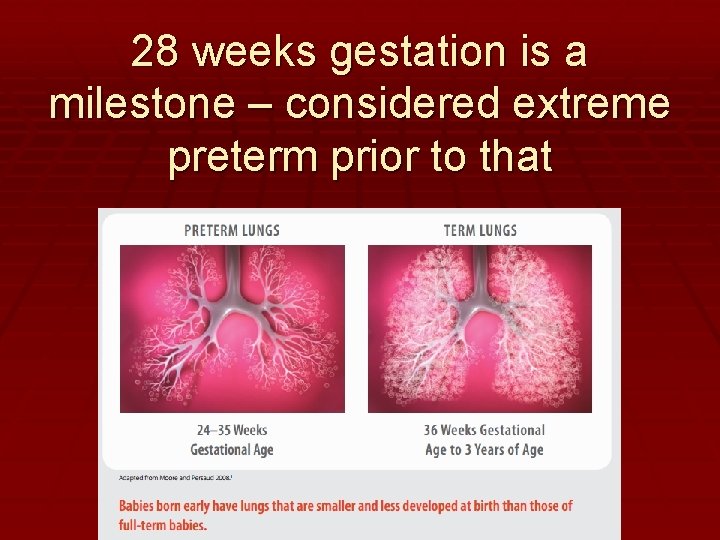
28 weeks gestation is a milestone – considered extreme preterm prior to that

Alexis: Born @ 25 weeks – June 2013 Weight = 11 oz – less than a can full of soda!!
Notes Read through statements B & C in notes
- Slides: 90