BIOARTIFICIAL LIVER EXTRACORPOREAL TEMPORARY LIVER SUPPORT DEVICES Alan
BIO-ARTIFICIAL LIVER (EXTRACORPOREAL TEMPORARY LIVER SUPPORT DEVICES) Alan Golde Jr. BME 181 March 18 th 2013
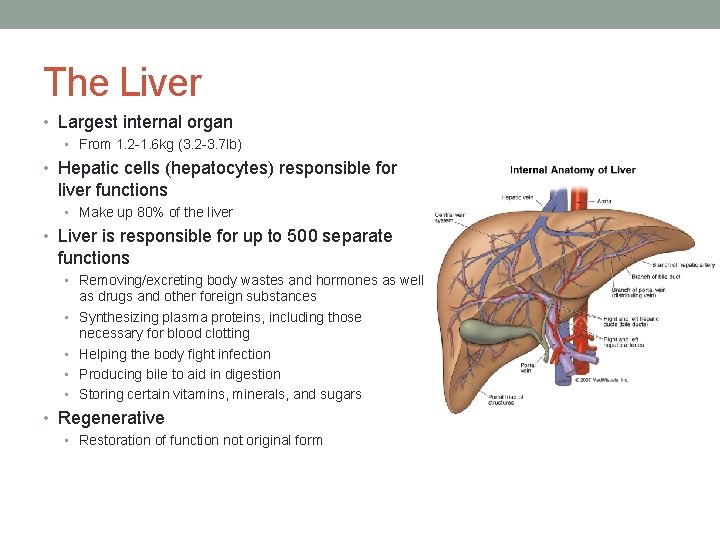
The Liver • Largest internal organ • From 1. 2 -1. 6 kg (3. 2 -3. 7 lb) • Hepatic cells (hepatocytes) responsible for liver functions • Make up 80% of the liver • Liver is responsible for up to 500 separate functions • Removing/excreting body wastes and hormones as well • • as drugs and other foreign substances Synthesizing plasma proteins, including those necessary for blood clotting Helping the body fight infection Producing bile to aid in digestion Storing certain vitamins, minerals, and sugars • Regenerative • Restoration of function not original form
Complications • Most common causes of liver failure • hepatitis A, B, C, D, E • Alcohol damage • Fatty liver • Cirrhosis • Cancer and drug damage
Treatments Liver Transplant • Pros • Most effective treatment for acute liver failure • High survival rates • Cons • Scarcity of donors • Reduced clotting factors • Immunosuppressant's increase risk for infection • Rejection Bio-artificial Liver • Pros • Keep the patient alive until transplant is available • Aid in the livers regeneration • Cons • Are only a temporary fix
Current Work in BAL’s • Molecular Absorbent Recycling System (MARS®) • Teraklin, uses human albumin • Extracorporeal Liver Assist Device (ELAD®) • Vitagen, uses immortalized human hepatocytes • Hepat. Assist 2000 system • Circe Biomedical, uses porcine hepatocytes • Bioartificial Liver Support System (BLSS®) • Excorp Medical, Inc. , uses primary porcine hepatocytes • LIVERX 2000 system • Algenix, Inc. , uses porcine hepatocytes • Modular Extracorporeal Liver System (MELS®) • Charite Virchow Clinic-Berlin, uses human hepatocytes

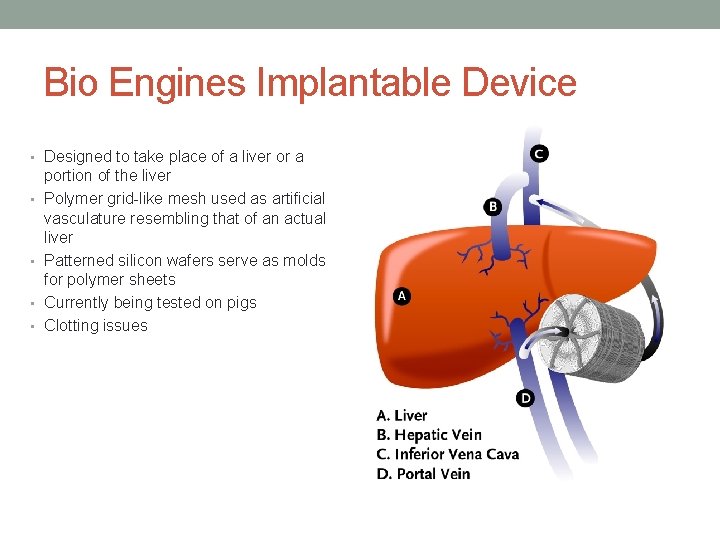
Bio Engines Implantable Device • Designed to take place of a liver or a • • portion of the liver Polymer grid-like mesh used as artificial vasculature resembling that of an actual liver Patterned silicon wafers serve as molds for polymer sheets Currently being tested on pigs Clotting issues
Challenges • Bio-artificial livers should be able to provide at least 10% of liver functioning • This requires approximately 1010 hepatocytes • Very difficult acquiring this many hepatocyte cells • Controversy over the use of porcine cells due to possible transmission of infections • Hepatocytes and plasma have very different physio-chemical properties • Hepatocytes do not perform well when in contact with plasma • Have a very high oxygen uptake rate • Hepatocyte cells undergo a lot of stress inside of bio-artificial liver • Any stress above 5 dyn/cm 2 renders cells useless • Limited volume of the bioreactor • maximum blood/plasma that can be safely drawn out of liver failure patient is one liter • Difficult to achieve 10% of liver functioning within 1 liter • Makes Bio-artificial liver designing very difficult
Future • Research in: • Cell sources • Bioreactor design • Filtering techniques • Packaging for implantable devices
Sources • http: //biomed. brown. edu/Courses/BI 108_2002_Groups/liver/we • • bpage/intro. html Palakkan, A. A. , Hay, D. C. , PR, A. K. , TV, K. and Ross, J. A. (2013), Liver tissue engineering and cell sources: issues and challenges. Liver International. doi: 10. 1111/liv. 12134 http: //www. xconomy. com/boston/2007/09/20/bioengine-one-stepcloser-to-artificial-liver-device/ http: //nyp. org/news/hospital/artificial-liver-lives. html http: //artificial-liver. blogspot. com/2009/11/biological-extracorporealliver-assist. html
- Slides: 10