Biliary system Anatomy Plain x ray GB stone
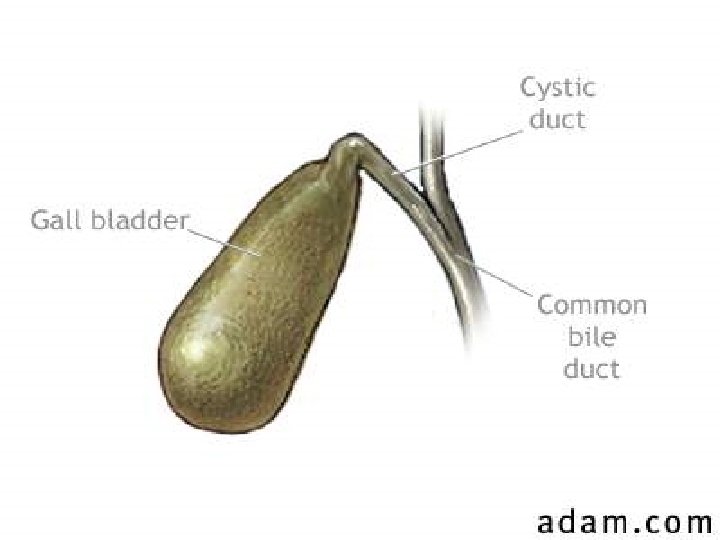
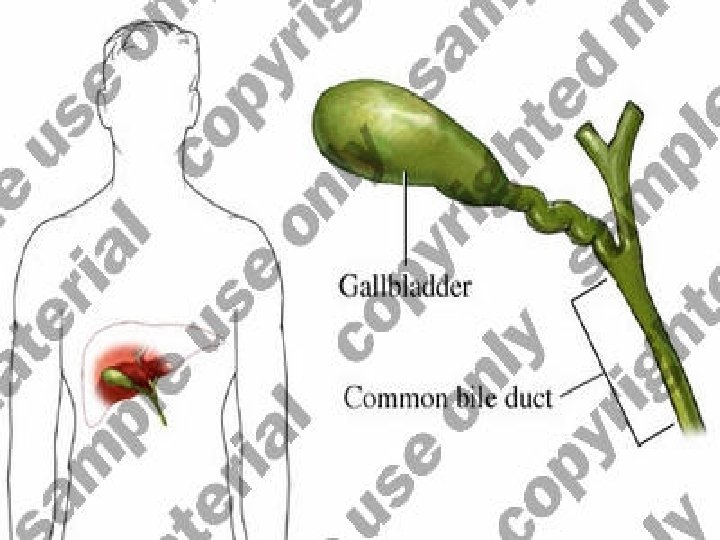
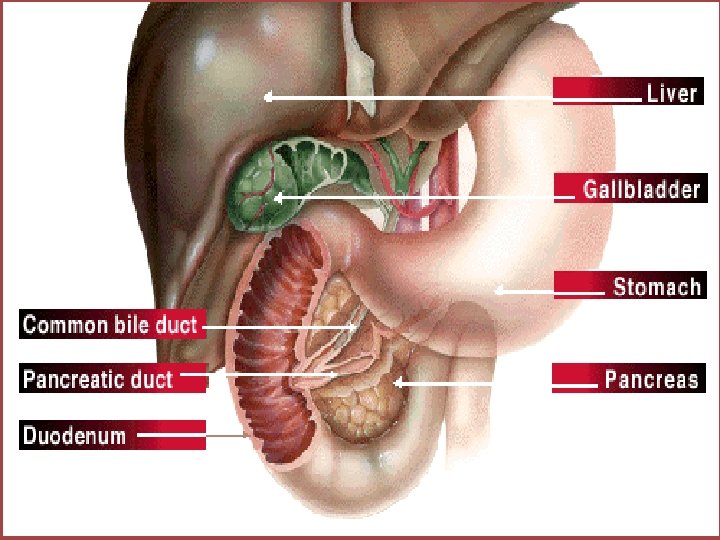
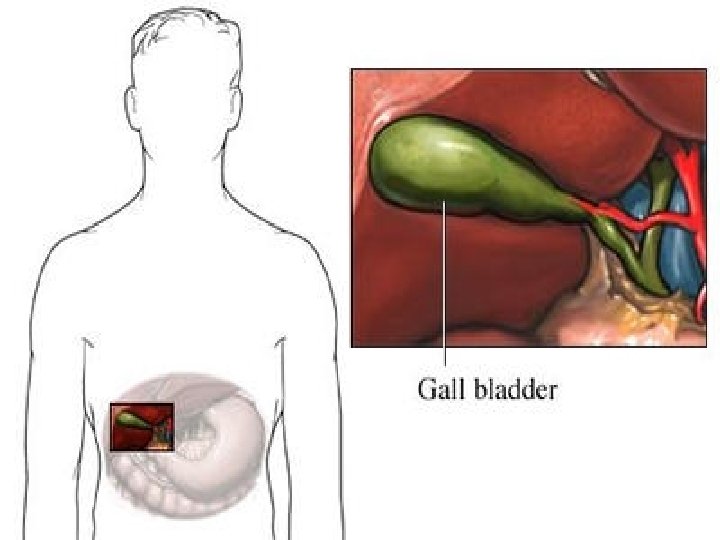
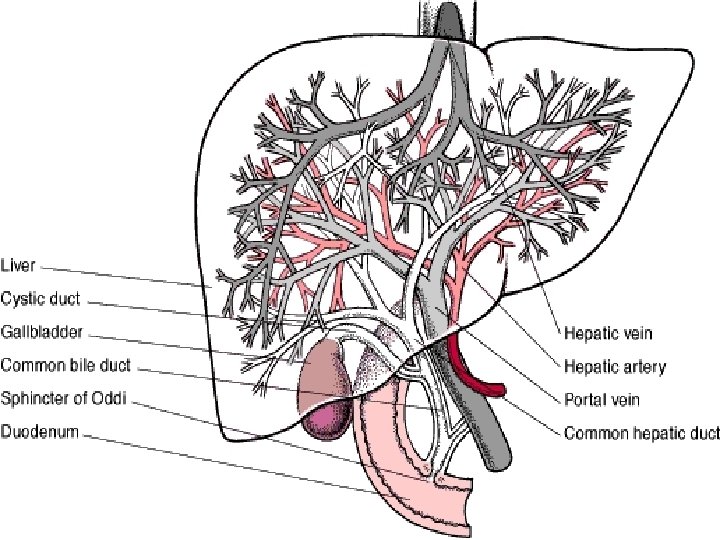
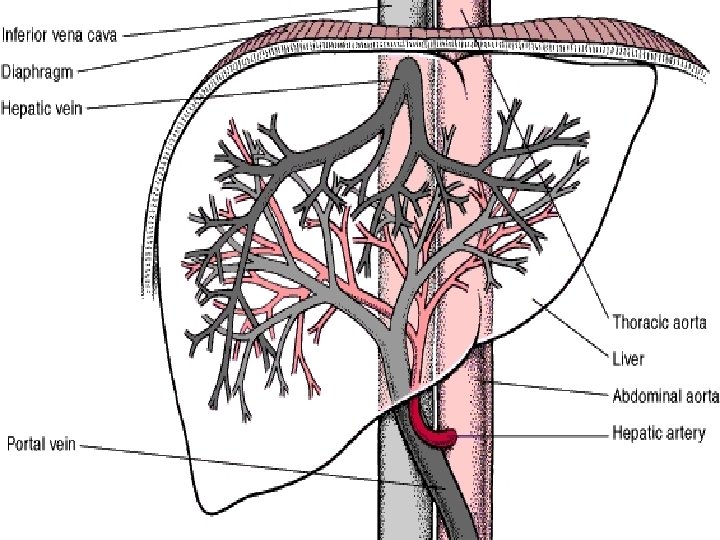
Biliary system
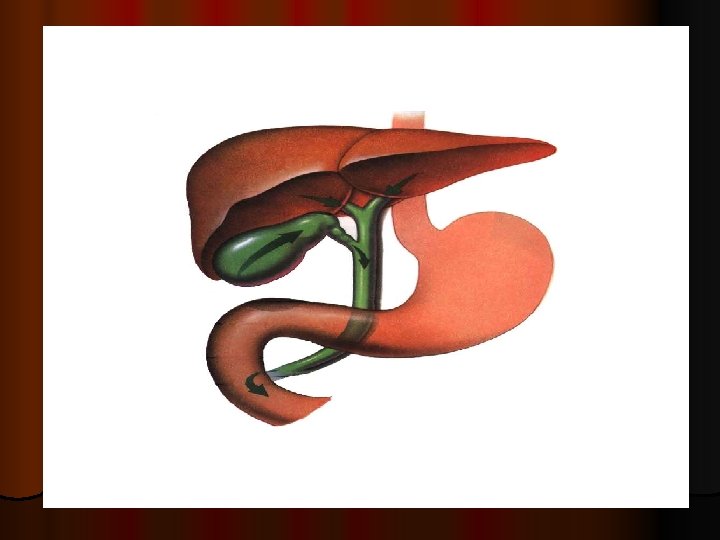
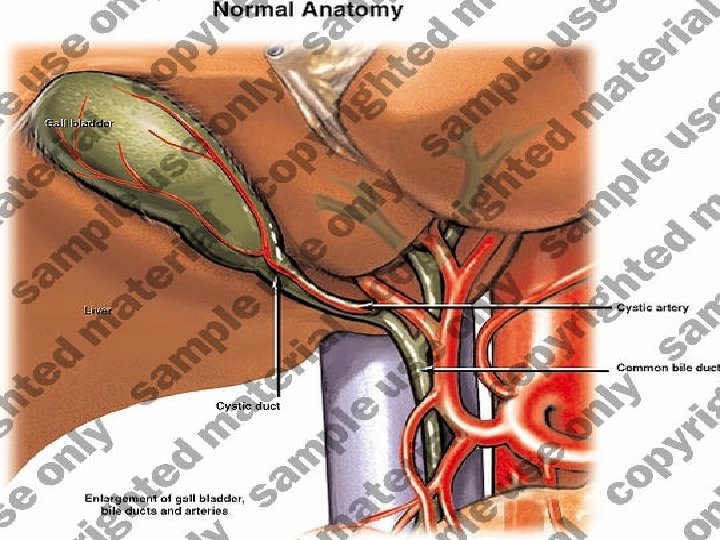
Anatomy
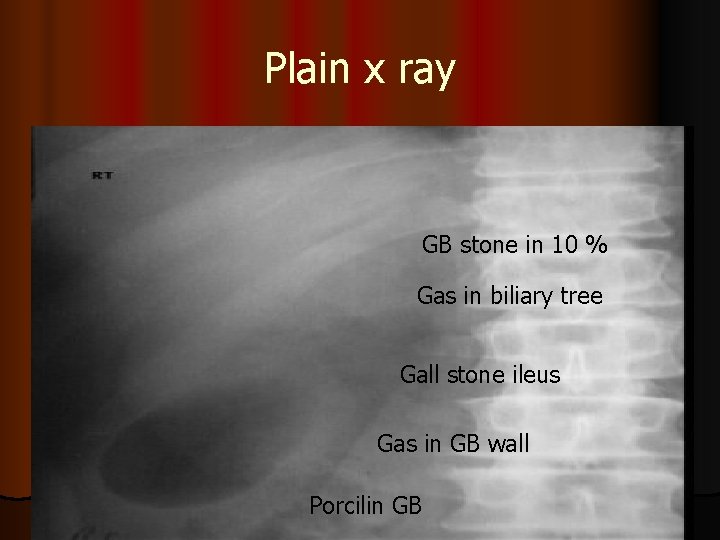
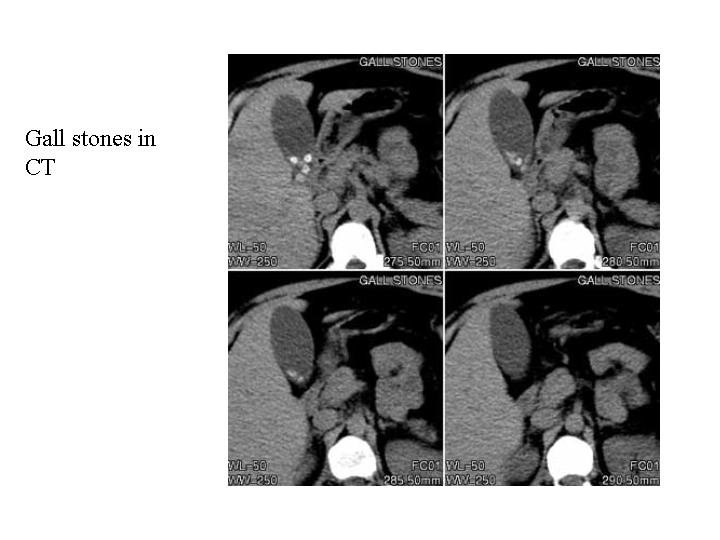
Plain x ray GB stone in 10 % Gas in biliary tree Gall stone ileus Gas in GB wall Porcilin GB
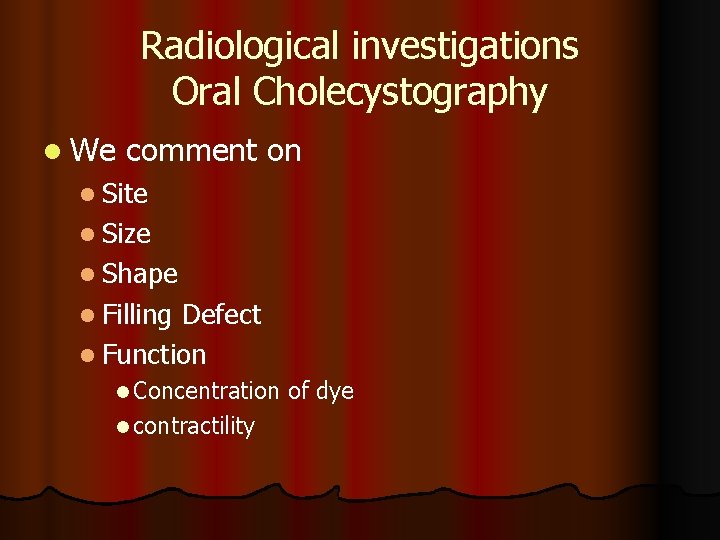
Radiological investigations Oral Cholecystography l We comment on l Site l Size l Shape l Filling Defect l Function l Concentration l contractility of dye
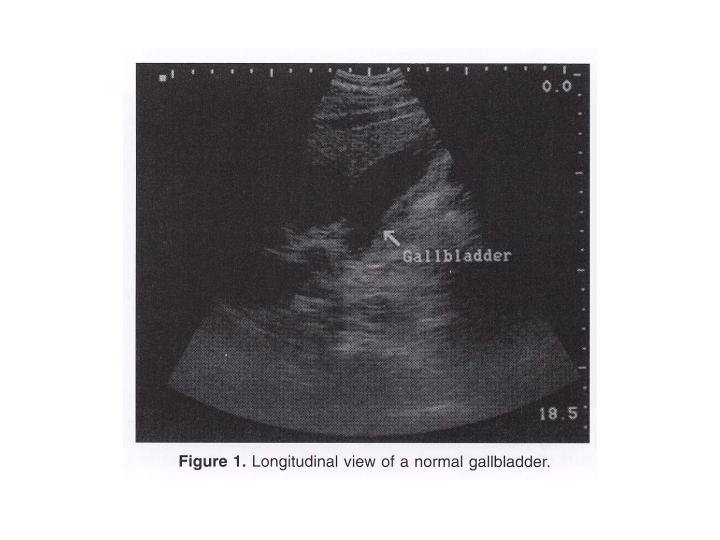
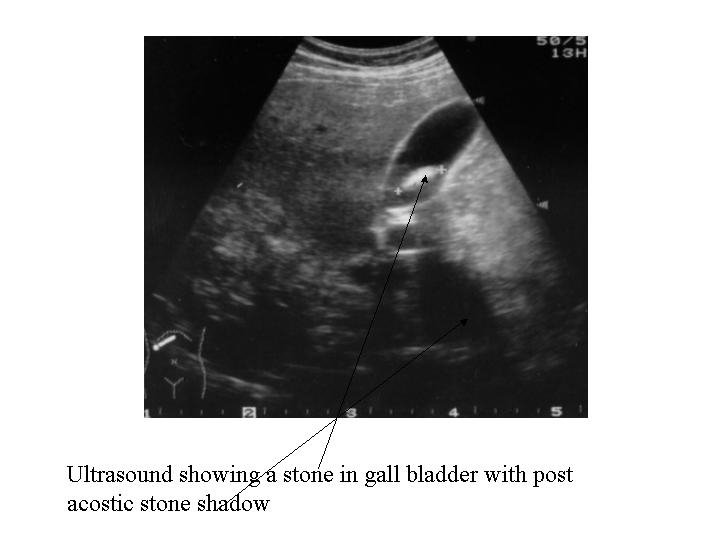
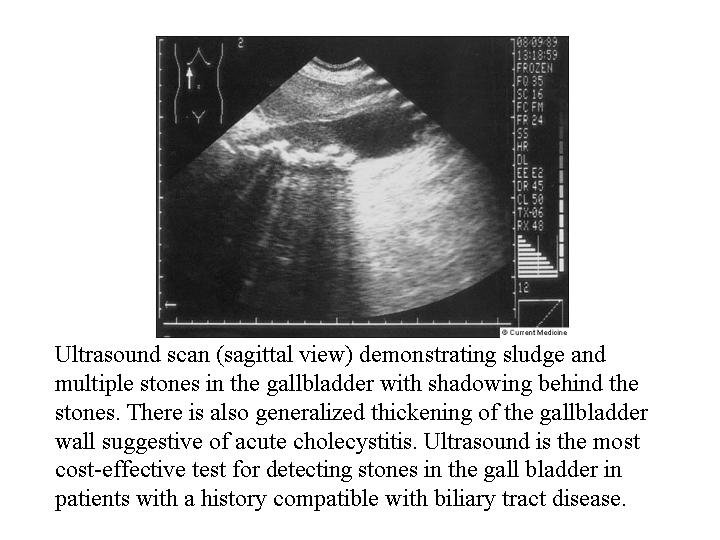
Investigations Imaging techniques Ultrasound this is most useful l Most important to show intrahepatic bile ducts dilatation l Measure the diameter of CBD (normal up to 7 mm) l Comment on the status of the GB and its stones l Visualize CBD diameter, stones or areas of narrowing l Tumors in the region of the pancreas is seen CT (conventional or helical) competes with the U/S especially as regards the pancreatic tumors.

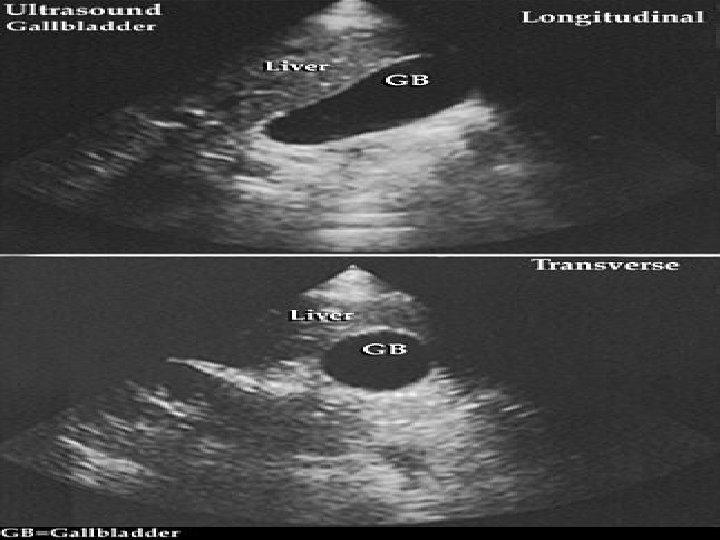
Radiological investigations Ultrasound
cholangiogram l Preoperative cholangiogram l IV cholangiogram l PTC l ERCP l Intra operative l T tube ( post operative )

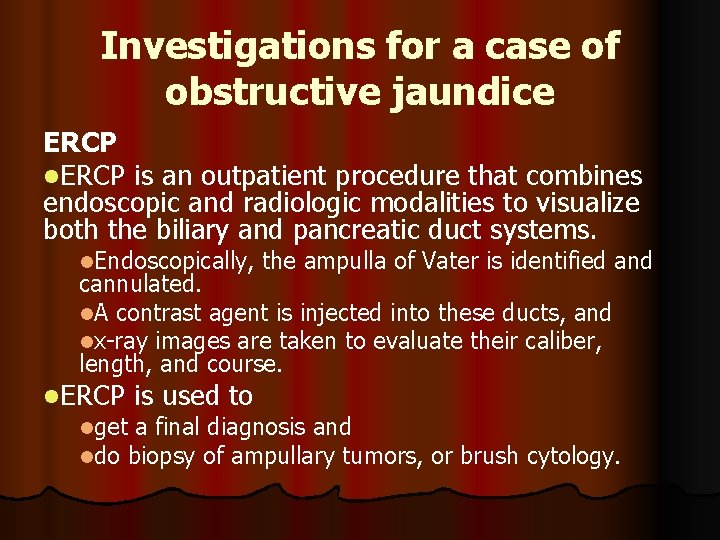
Investigations for a case of obstructive jaundice ERCP l. ERCP is an outpatient procedure that combines endoscopic and radiologic modalities to visualize both the biliary and pancreatic duct systems. l. Endoscopically, the ampulla of Vater is identified and cannulated. l. A contrast agent is injected into these ducts, and lx-ray images are taken to evaluate their caliber, length, and course. l. ERCP is used to lget a final diagnosis and ldo biopsy of ampullary tumors, or brush cytology.
Investigations for a case of obstructive jaundice ERCP l It can be also therapeutic for stone extraction by Dormia basket or linsertion of a stent, both are preceded by sphincterotomy. l l. It has its risks ascending infections, l perforations, lpancreatitis, an lbleeding due to sphincterotomy done routinely before CBD cannulation l
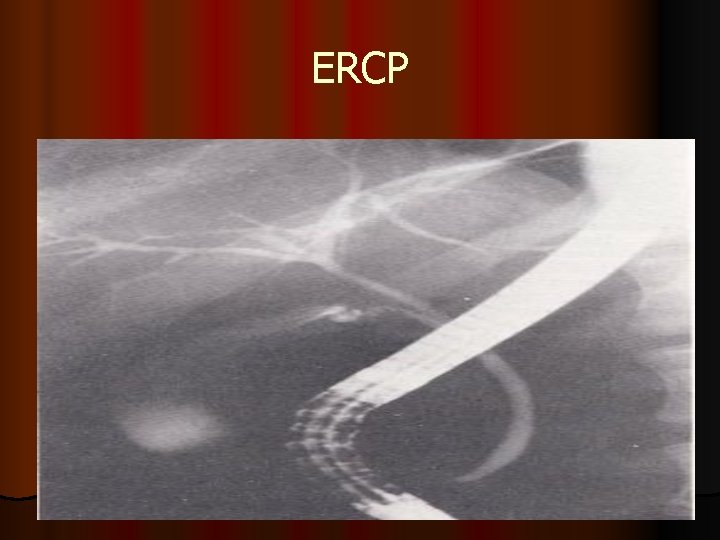
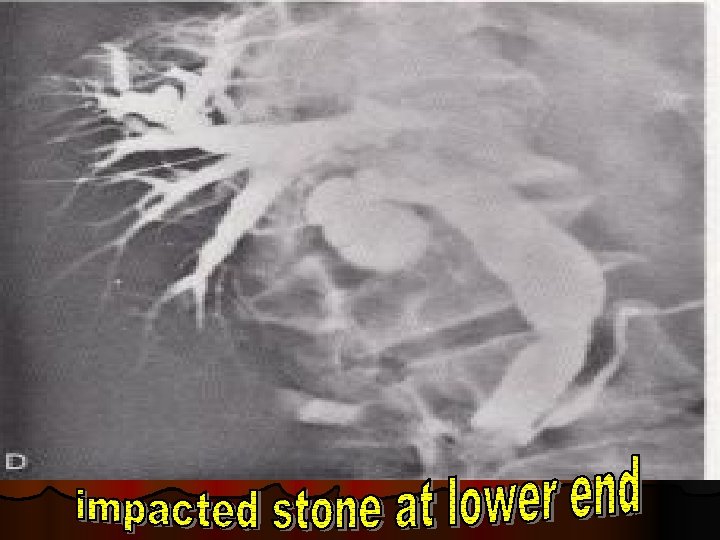
ERCP








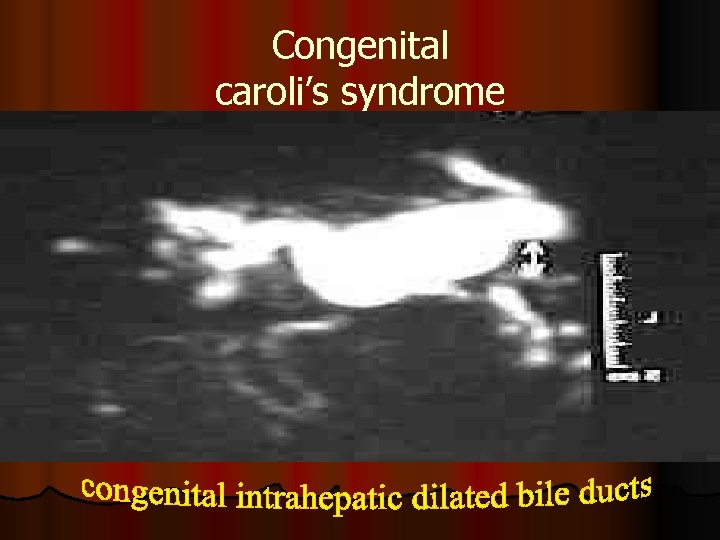
Congenital caroli’s syndrome
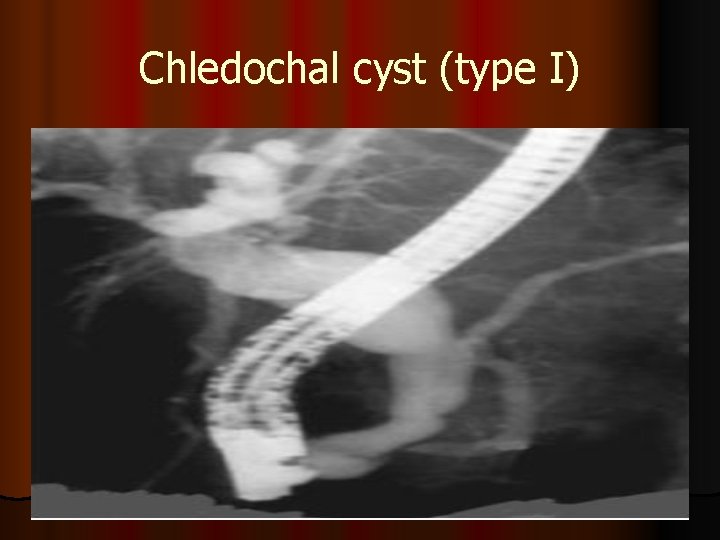
Chledochal cyst (type I)
Investigations for a case of obstructive jaundice MRCP a sensitive noninvasive method of detecting biliary and pancreatic duct stones, strictures, or dilatations within the biliary system. l. It is also sensitive for helping detect cancer. l
Investigations for a case of obstructive jaundice MRCP (contraindications) Absolute include the presence of a cardiac pacemaker, lcerebral aneurysm clips, locular or cochlear implants l ocular foreign bodies. l Relative contraindications include the presence of cardiac prosthetic valves, l neurostimulators, l metal prostheses, l penile implants l
Investigations for a case of obstructive jaundice PTC l performed by a radiologist using fluoroscopic guidance. l. The liver is punctured to enter the peripheral intrahepatic bile duct system. l. An iodine-based contrast medium is injected into the biliary system and flows through the ducts. l. Obstruction can be identified on the fluoroscopic monitor.
Investigations for a case of obstructive jaundice PTC l. It is especially useful for lesions proximal to the common hepatic duct. l. Still, l. PTC ERCP is generally preferred. is reserved for use if ERCP fails or when altered anatomy precludes accessing the ampulla.
Investigations for a case of obstructive jaundice PTC Complications of this procedure include l the possibility of allergic reaction to the contrast medium. l peritonitis. l intraperitoneal hemorrhage, sepsis l cholangitis. l subphrenic abscess. l lung collapse. l Severe complications occur in 3% of cases
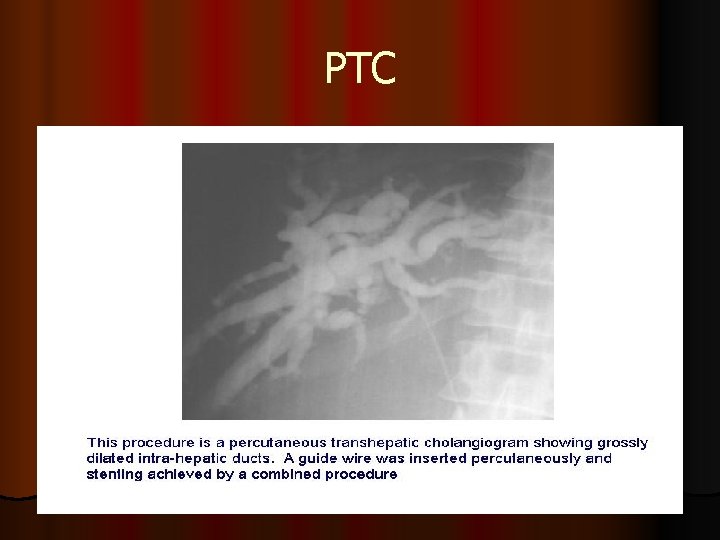
PTC

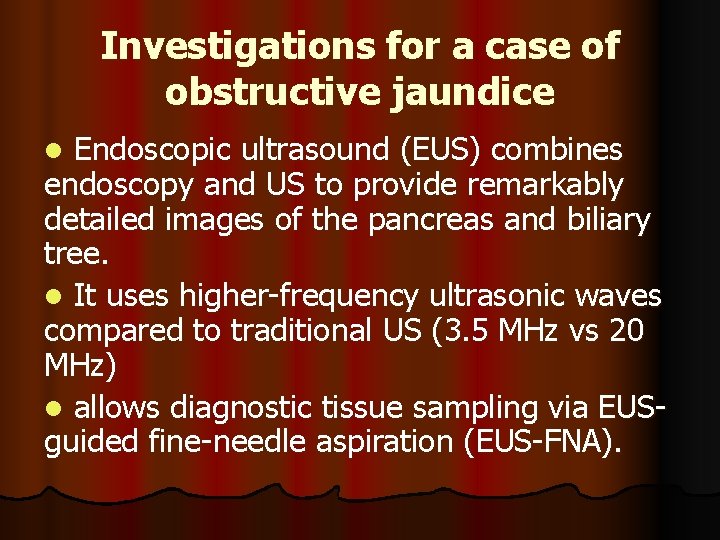
Investigations for a case of obstructive jaundice Endoscopic ultrasound (EUS) combines endoscopy and US to provide remarkably detailed images of the pancreas and biliary tree. l It uses higher-frequency ultrasonic waves compared to traditional US (3. 5 MHz vs 20 MHz) l allows diagnostic tissue sampling via EUSguided fine-needle aspiration (EUS-FNA). l
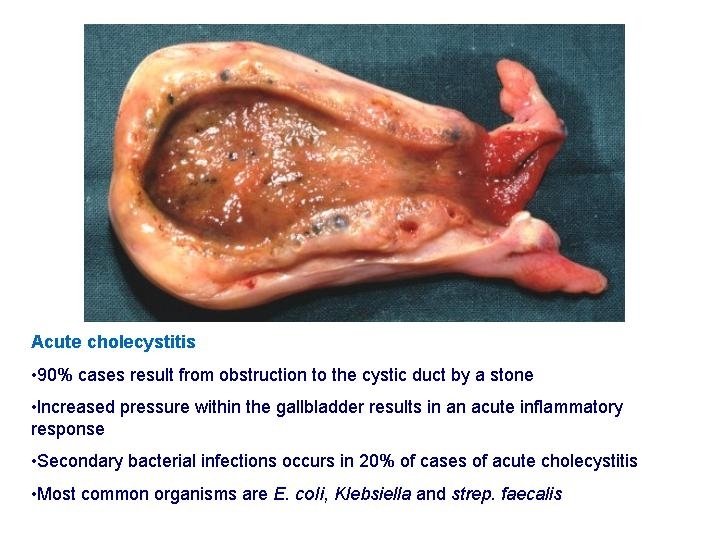
Acute Cholecystitis l. Acute obstructive (Calcular) l. Acute Acalcaus l. Acute emphysematous
Acute obstructive (Calcular) (Pathology) Calcular obstruction l GB become hyperemic, oedematous & distended l Chemical inflammation l Release of Phosphlipases l Act on lecithin which is a mucosal protector transforming it into l Lysolecithin (mucosal toxin l Arachidonic acid (PG precursor) (inflammation) l l Sepsis l Ecoli, klebsilla & strept which occur later on
Acute obstructive (Calcular) (Pathology) l Following acute inflammation the condition end by one of the following l Resolution l Mucocele l Empyema l Gangrene And perforation l Bilo-enteric fistula
Acute Acalcular Cholecystitis l It form 8 % l Risk factors are l Sepsis l Starvation l Prolonged TPN l Ileus l Morphine use > 6 days
Acute Acalcular Cholecystitis l Pathology is not knowen l Prolonged distention of GB , Bile stasis & inspissations lead to mucosal injury and vessel thrombosis l Hypersensitivity to concomitant antibiotics l Gangrene occur in 25 % of cases
Acute emphysematous GB l Caused by mixed poly-microbial infection including gas forming bacteria l 70% male , diabetics l Thrombosis of cystic artery is the cause l It lead tom l Gangrene in 75 % l Perforation in 15 %
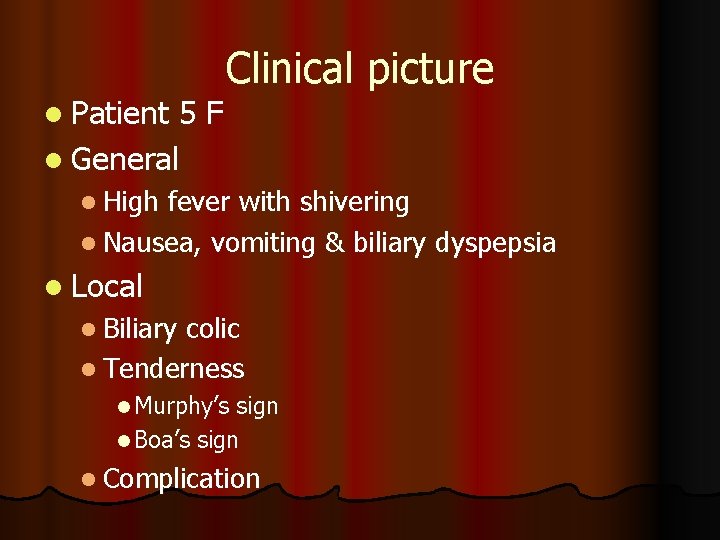
l Patient 5 F l General Clinical picture l High fever with shivering l Nausea, vomiting & biliary dyspepsia l Local l Biliary colic l Tenderness l Murphy’s sign l Boa’s sign l Complication
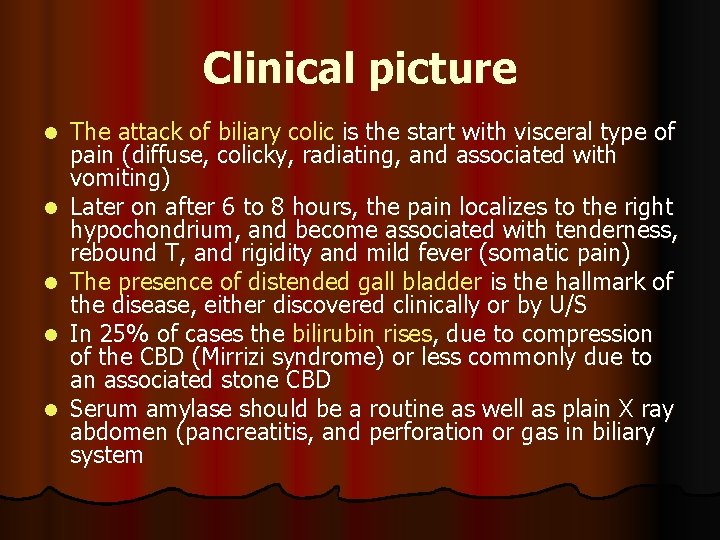
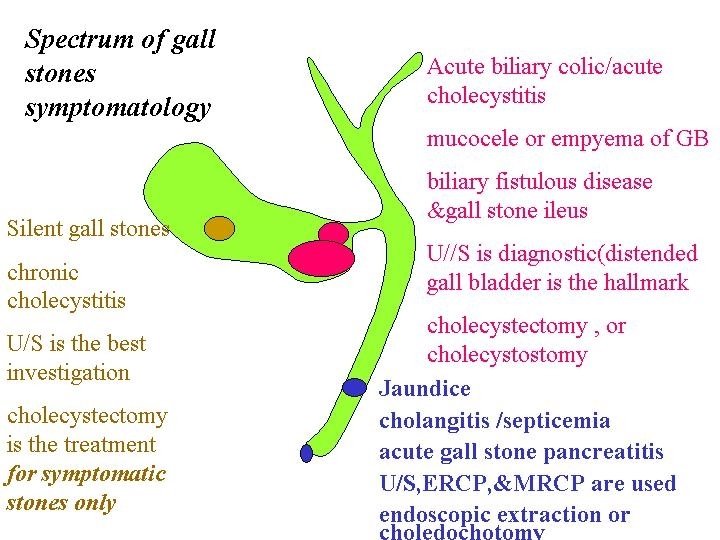
Clinical picture l l l The attack of biliary colic is the start with visceral type of pain (diffuse, colicky, radiating, and associated with vomiting) Later on after 6 to 8 hours, the pain localizes to the right hypochondrium, and become associated with tenderness, rebound T, and rigidity and mild fever (somatic pain) The presence of distended gall bladder is the hallmark of the disease, either discovered clinically or by U/S In 25% of cases the bilirubin rises, due to compression of the CBD (Mirrizi syndrome) or less commonly due to an associated stone CBD Serum amylase should be a routine as well as plain X ray abdomen (pancreatitis, and perforation or gas in biliary system
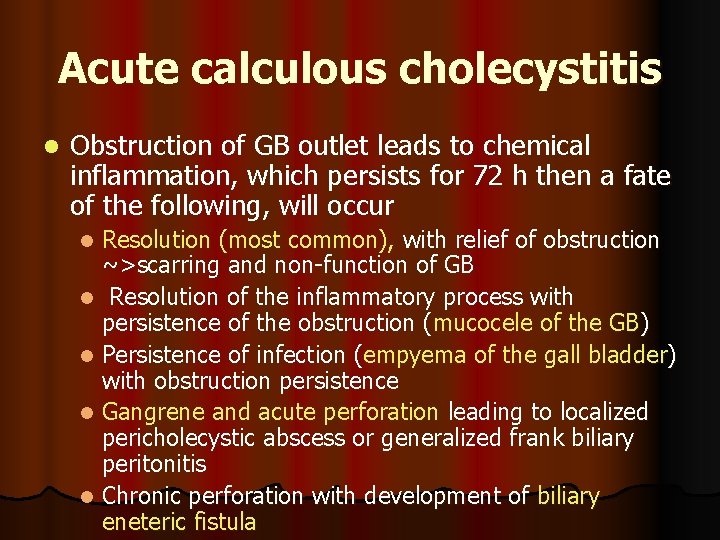
Acute calculous cholecystitis l Obstruction of GB outlet leads to chemical inflammation, which persists for 72 h then a fate of the following, will occur Resolution (most common), with relief of obstruction ~>scarring and non-function of GB l Resolution of the inflammatory process with persistence of the obstruction (mucocele of the GB) l Persistence of infection (empyema of the gall bladder) with obstruction persistence l Gangrene and acute perforation leading to localized pericholecystic abscess or generalized frank biliary peritonitis l Chronic perforation with development of biliary eneteric fistula l
Investigation l Laboratory l Leucocytosis l Liver function l S. amylase l Radiological l Plain xray l US l Doppler US l HIDDA scan l CT scan & MRI
Investigations: the best is ultrasound l An ultrasound is the most common screening test. l It is 90 -95% sensitive for cholecystitis l It is 78 -80% specific. l For simple cholelithiasis, it is 98% sensitive and specific.
Investigations: the best is ultrasound l Findings include gallstones or sludge and one or more of the following conditions: l Gallbladder wall thickening (>2 -4 mm) l Gallbladder distention (diameter >4 cm, length >10 cm) l Pericholecystic fluid from perforation or exudate l Air in the gallbladder wall (indicating gangrenous cholecystitis) l Sonographic Murphy sign (86 -92% sensitive, 35% specific), pain when the probe is pushed directly on the gallbladder (not related to breathing)
Treatment (conservative) l NPO, nasogastric & IV fluids l Analgesic, antipyretic & spasmolytic l Antibilotic l Broad spectrum ( cephalosporins ) l Metronidazole & aminoglycoside l Follow up and surgery l In the same admission l Interval cholecystectomy
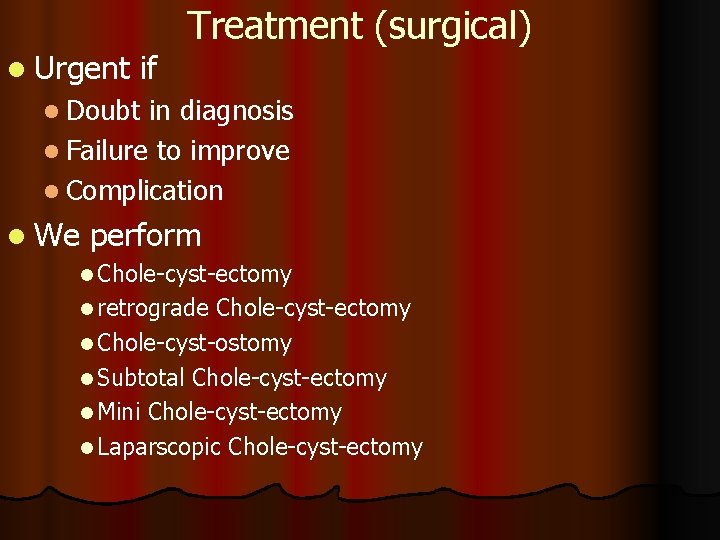
l Urgent if Treatment (surgical) l Doubt in diagnosis l Failure to improve l Complication l We perform l Chole-cyst-ectomy l retrograde Chole-cyst-ectomy l Chole-cyst-ostomy l Subtotal Chole-cyst-ectomy l Mini Chole-cyst-ectomy l Laparscopic Chole-cyst-ectomy
Treatment (surgical) l. Established Non-progressive disease l. Interval Chole-cyst-ectomy l. Early chole-cyst-ectomy
Gall stones
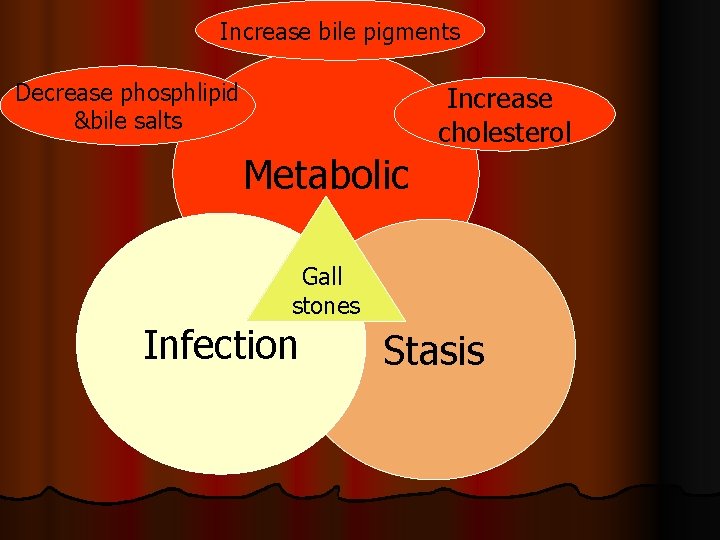
Increase bile pigments Decrease phosphlipid &bile salts Increase cholesterol Metabolic Gall stones Infection Stasis
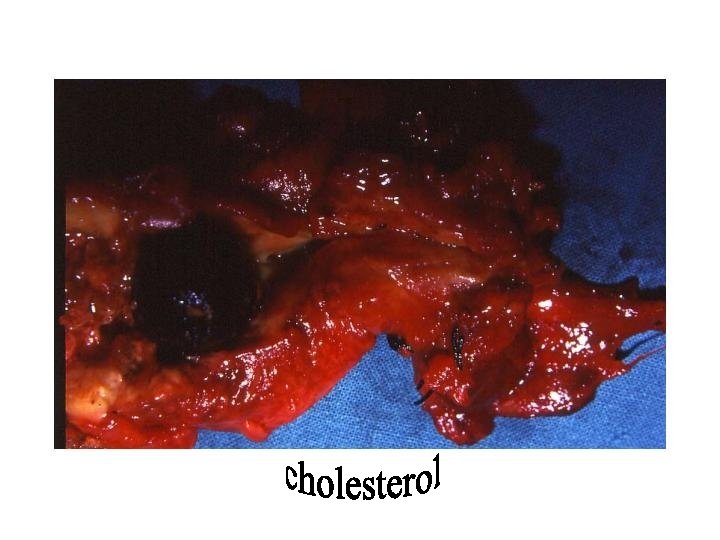
l 75% Cholesterol stone of stones formed in sterile GB (10% infection) l Protein matrix l cholesterol (70%) l bile pigment l Ca carbonate l Ca palmitate (Ca salts deposited at periphery, their amount determine the radiolucency)
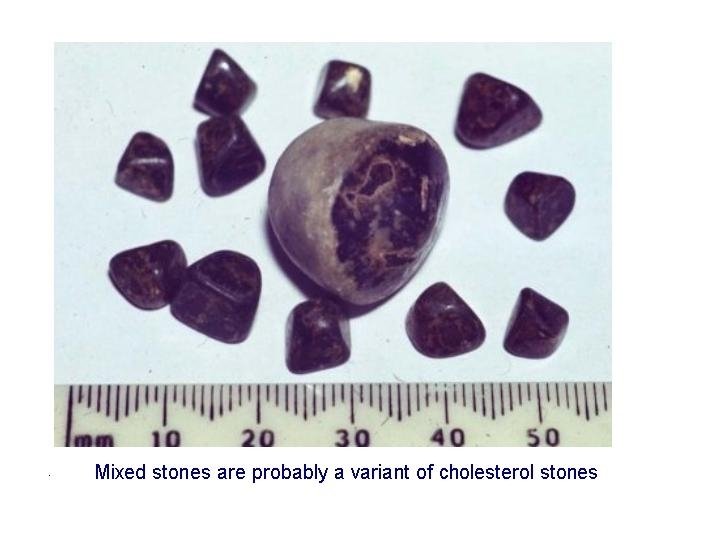
Cholesterol stone l Two types l Pure cholesterol l Oval or rounded l mamillated or mullbery-surfaced l pale yellow in color l solitary big size (100% cholesterol rounded) l 60% cholesterol (mixed) l Multiple mediums sized (60% cholesterol, faceted) l brownish polished surface
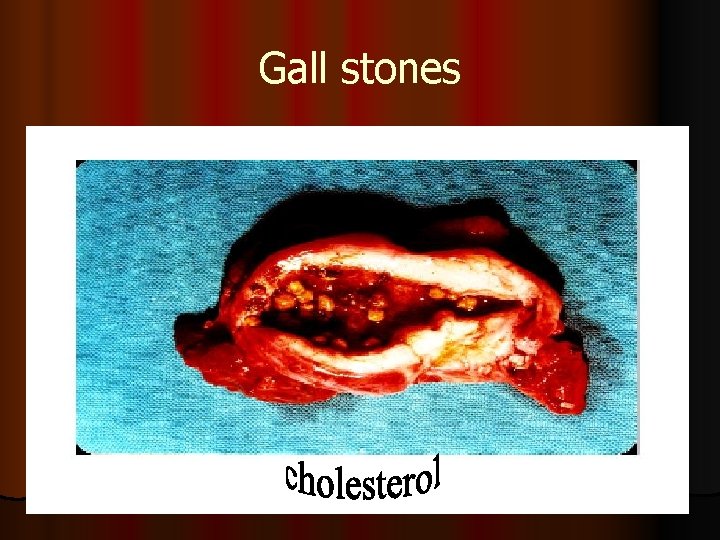
Gall stones
Formation involves 7 processes 1. 2. 3. 4. 5. 6. 7. Super saturation with cholesterol Incomplete transfer of cholesterol from vesicles to micelles Formation of vesicles with high cholesterol Aggregation and fusion of unstable vesicles Cholesterol crystallization (mucin is a nucleating agent) Biliary sludge formation (mucin+ cholesterol+ Ca+pigment ~precursor of stones) Stone growth
Black Pigment Stone 25% of stones. It is common in cirrhotics, after terminal ileum resection and in hemolytic diseases. Formed in a sterile GB (20% infection rate) l Composed of bilirubin polymer without Ca palmitate and +cholesterol (25%)+matrix of organic material l Usually multiple, small, irregular, dark green or black in color l Hard in consistency and cut surface is layered l l l Formation Elevated concentration of mono-conjugated bilirubin lower bile salt concentration is the usual constitution in forming patients l yet the exact pathogenesis is not known l l
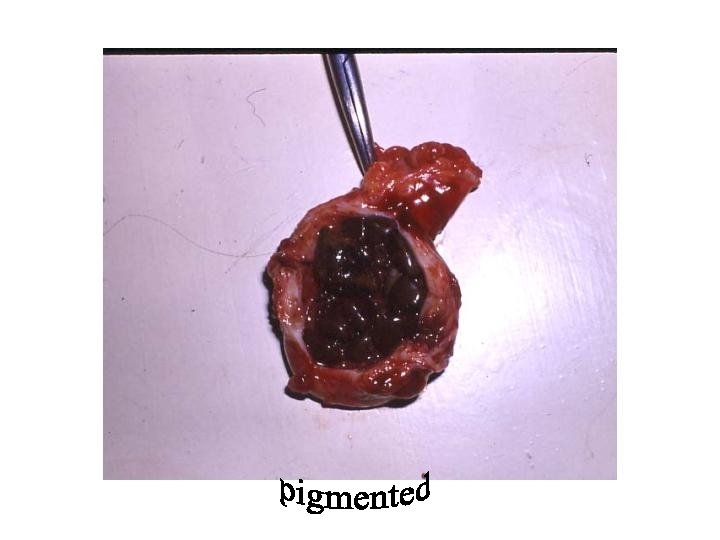
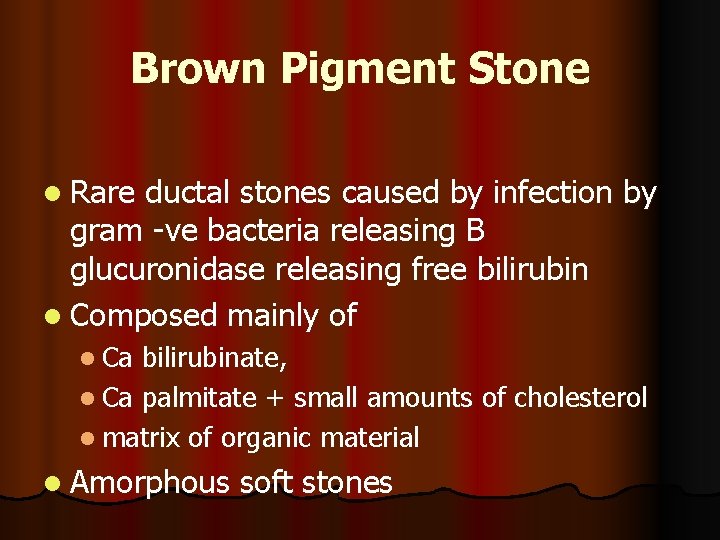
Brown Pigment Stone l Rare ductal stones caused by infection by gram -ve bacteria releasing B glucuronidase releasing free bilirubin l Composed mainly of l Ca bilirubinate, l Ca palmitate + small amounts of cholesterol l matrix of organic material l Amorphous soft stones
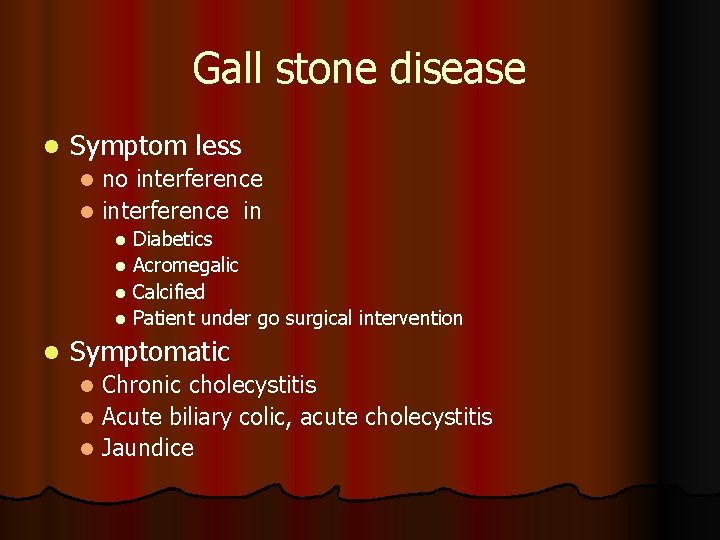
Gall stone disease l Symptom less no interference l interference in l Diabetics l Acromegalic l Calcified l Patient under go surgical intervention l l Symptomatic Chronic cholecystitis l Acute biliary colic, acute cholecystitis l Jaundice l
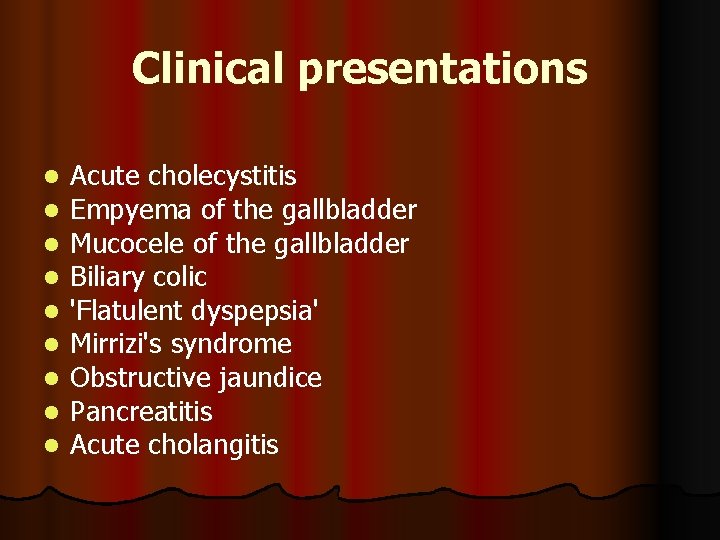
Clinical presentations l l l l l Acute cholecystitis Empyema of the gallbladder Mucocele of the gallbladder Biliary colic 'Flatulent dyspepsia' Mirrizi's syndrome Obstructive jaundice Pancreatitis Acute cholangitis
Chronic calcular cholecystitis Clinical picture l Recurrent attacks of epigastric or right hypochondrial pain (persistent pain) l May be attacks of severe biliary colic l Nausea &vomiting l Flatulent dyspepsia with intolerance to fatty meals l Tenderness in right hypochondrium (Murphy’s
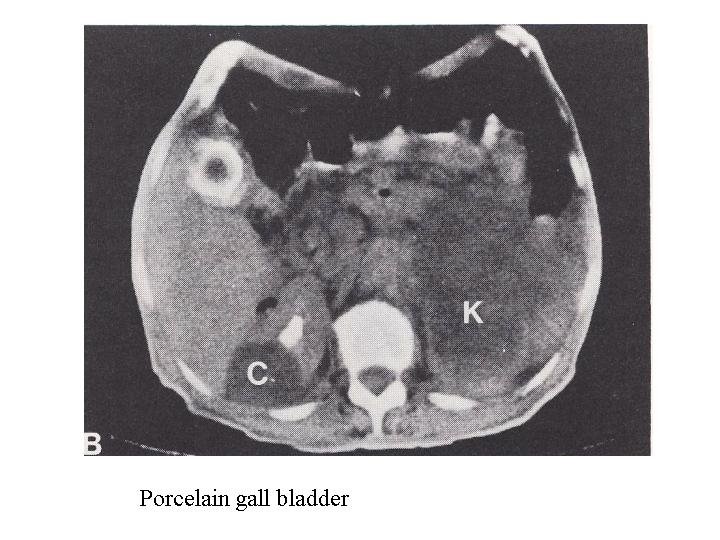
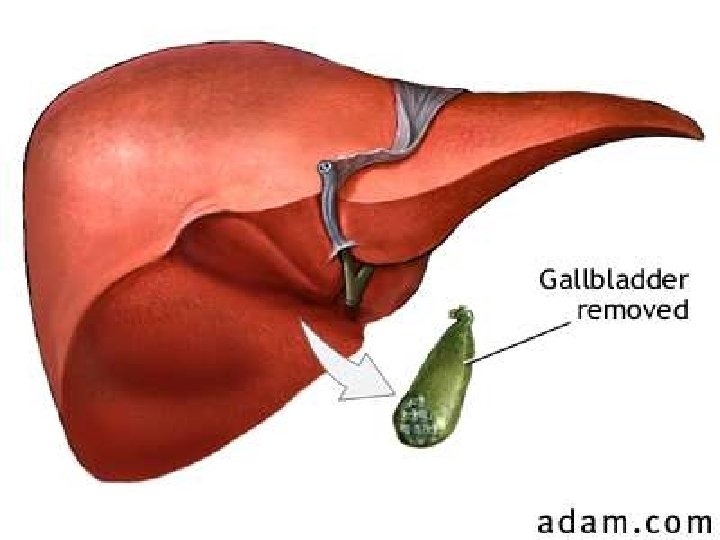
Treatment : l Cholecystectomy either conventional or laparoscopic is the ideal treatment for symptomatic patients. l Patients with asymptomatic gall stones can be left without surgery specially if cirrhotics. l However patients with a calcified or porcelain gallbladder should consider elective cholecystectomy due to the increased risk of carcinoma (25%).
Laparoscopic cholecystectomy (LC) l Shown to be equally as effective as open cholecystectomy in controlled trials l Pre-operative ERCP is indicated if: l Recent jaundice l Abnormal liver function tests l Significantly dilated common bile duct l Ultrasonic suspicion of bile duct stones
cholecystectomy l Indication l Trauma l Inflammation l Acute & chronic l Mucocele l empyema l Tumor l Torsion l As a part of other operations
cholecystectomy l Incisions l. Subcostal (Kocher’s) l. Upper right paramedian l. Right upper transverse l. Upper midline
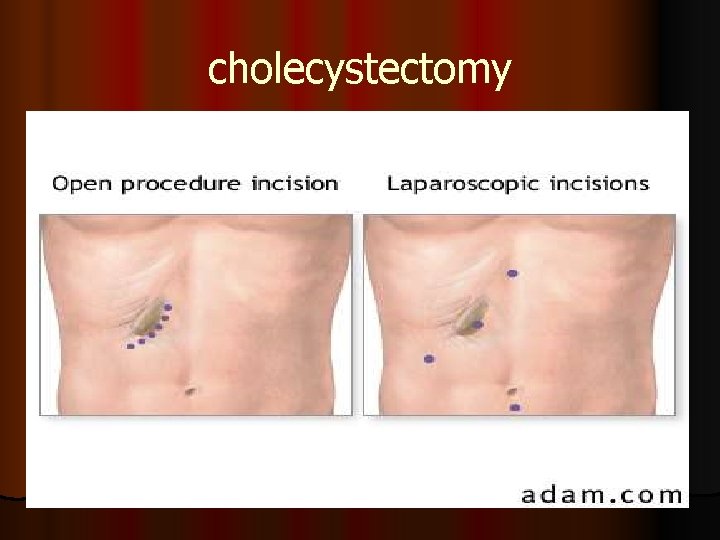
cholecystectomy
Technique l Preliminary exploration l Signs of cholecystitis l Associated pathology l. Saint’s triade l. Welkie’s triade l. Pancrease l. Stone in CBD
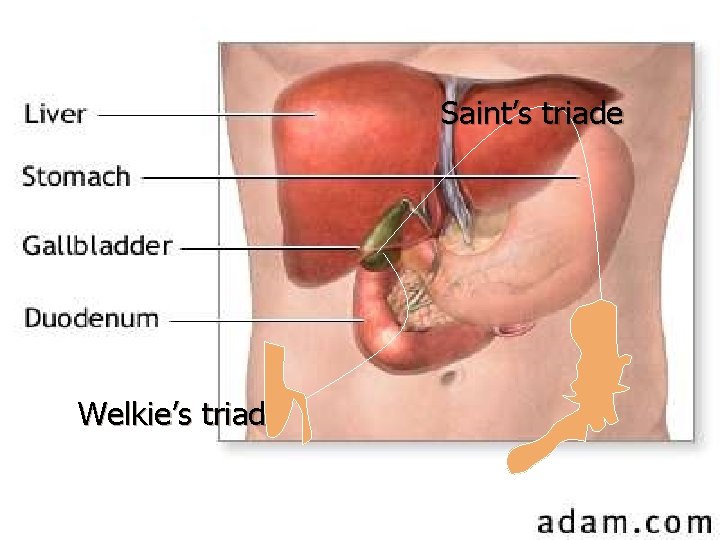
Saint’s triade Welkie’s triade
Technique l Packing of the field & retractors

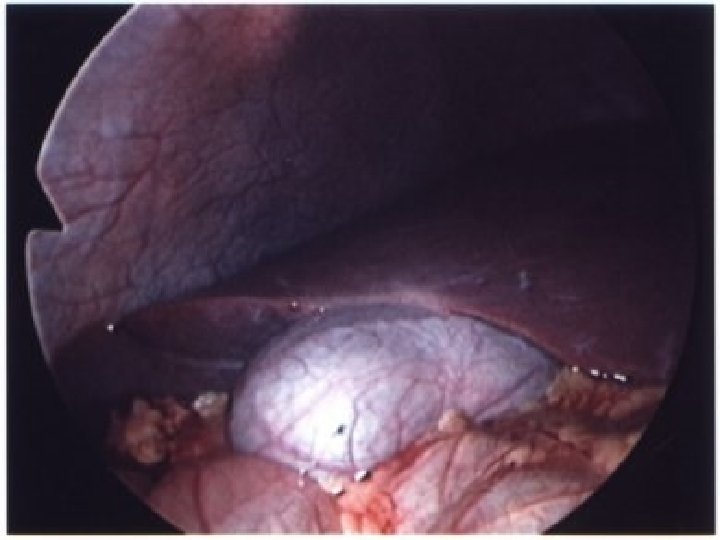
GB is grasped Separation of GB Artery Duct Identification of Calot’s

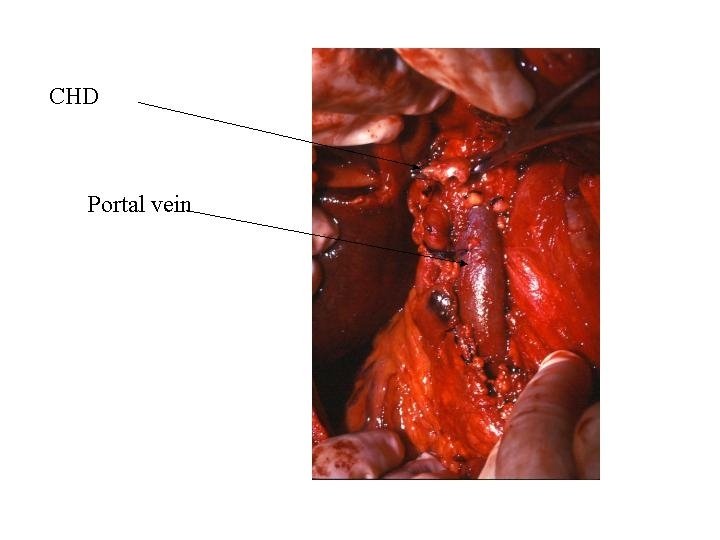
l Operative complications Injury to important structure l Common bile duct injury: observed more frequently in the laparoscopic approach. l Iatrogenic common bile duct injury often results from a combination of inexperience of the surgeon, the presence of anomalous biliary anatomy, and acute inflammation. l Duodenum injury l Pancreatic and liver injury l Ligation of Rt hepatic artery l Primary hge l Injury of cystic artery l Injury of Rt hepatic l Injury portal vein l GB bed l
Post operative complications l General l Chest & abdomen l DVT l Infection: l Spillage of stones into the peritoneal cavity during cholecystectomy increases the risk of infection and abscess formation. l Wound infections also are possible but are less common in the laparoscopic approach. .
Post operative complications l Local l Bleeding: Reactionary slipped ligature l 2 ry hge if infection which may lead to collection above IVC ( Waltman- Walter syndrome) l l Ligation of CBD or CHD l Hepatic artery l Biliary peritonitis l Biliary fistula l Subphrenic collection l Postcholecystectomy syndrome l
Post cholecystectomy syndrome l Organic causes l Long stump of cystic duct l Missed stone l Stricture l Stenos is of sphincter of Oddi l Non organic causes l Psycho-somatic l Biliary dyskinesia
Long stump of cystic duct l If stone is formed l Stump must be excised with l Stone extraction l If l no stones symptomatic treatment
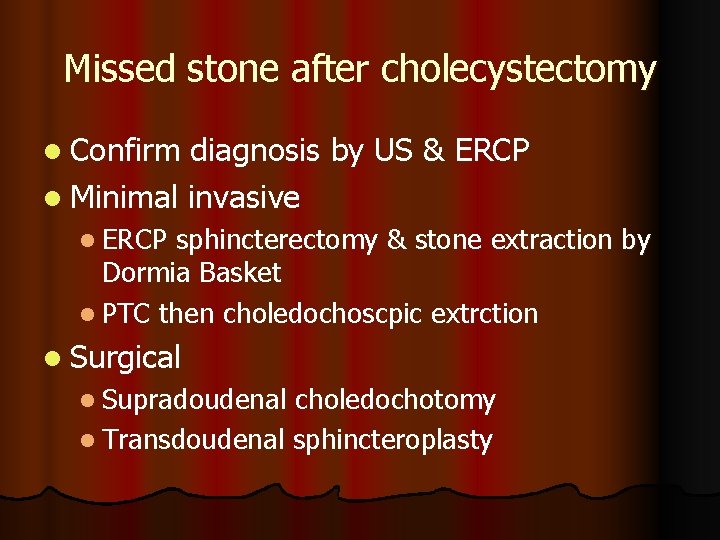
Missed stone after cholecystectomy l Confirm diagnosis by US & ERCP l Minimal invasive l ERCP sphincterectomy & stone extraction by Dormia Basket l PTC then choledochoscpic extrction l Surgical l Supradoudenal choledochotomy l Transdoudenal sphincteroplasty
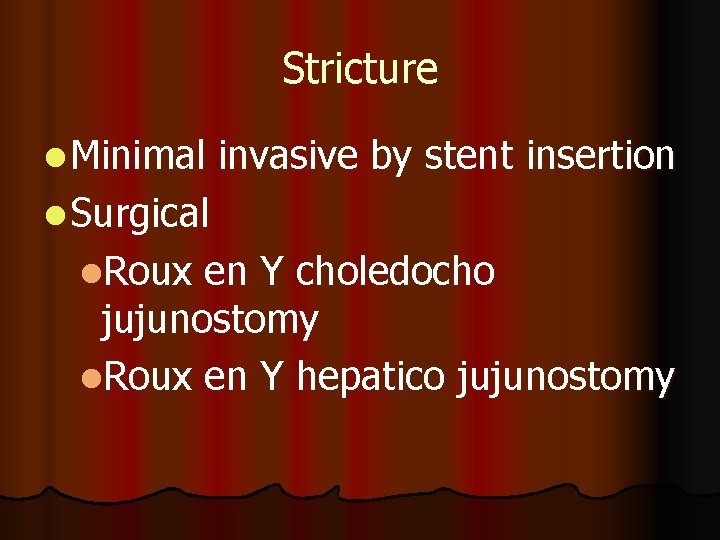
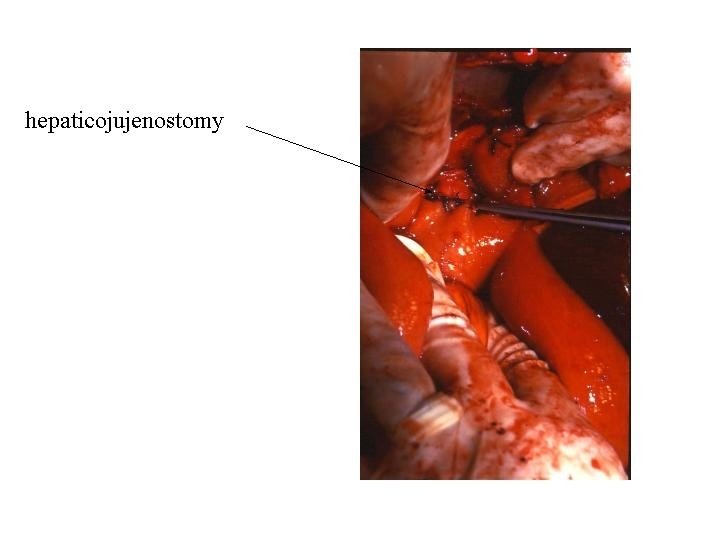
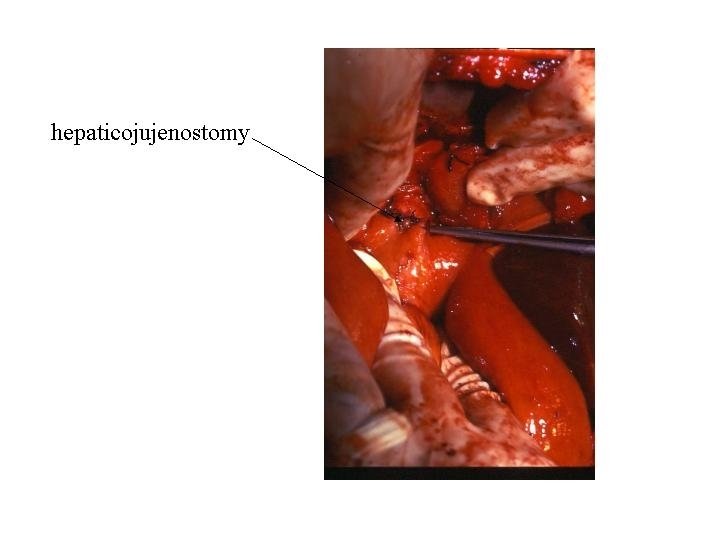
Stricture l Minimal invasive by stent insertion l Surgical l. Roux en Y choledocho jujunostomy l. Roux en Y hepatico jujunostomy
Post cholecystectomy syndrome l Organic causes l Long stump of cystic duct l Missed stone l Stricture l Stenos is of sphincter of Oddi l Non organic causes l Psycho-somatic l Biliary dyskinesia
Post cholecystectomy syndrome l Stenos is of sphincter of Oddi l Endoscopic papillotomy and sphincterotomy l Sphincteroplasty l Choledocho doudenotomy l Biliary dyskinesia l Endoscopic papillotomy and sphincterotomy
Stone in CBD
Aetiology l GB stone (commonest) l Primary stones of CBD usually (Brown) l Parasites l Stasis l FB l cholangitis
Clinical picture l Symptom less 20 % l Symptoms l Charcot’s triade l Jaundice l Pain l Fever l Raynaud’s pentale l Charcot’s triade l Hypotension l Altered mental status
Investigations l Laboratory l CBC l Liver function l urine l Radiological l US l ERCP l MRCP l PTC
Management of stone CBD l Support liver by correction of the general condition by I. V. fluids for hydration l Support kidney by Mannitol (hypotension and hyperbilirubinemia together causes renal shut down) l Prevent infection by antibiotics, l Prevent bleeding by correction of the avitaminosis K by parentral vitamin administration
Concurrent common bile duct and gallbladder stones l Preoperative ERCP, with clearance of the common bile duct, followed by LC l Open cholecystectomy and common bile duct exploration l Combined laparoscopic-endoscopic management: Endoscopic sphincterotomy and stone extraction are performed on the operation table l after the surgeon has passed a guidewire through the cystic duct into the duodenum l to help the endoscopist because the procedure is performed with the patient in the supine position. l
Management of a case of stone CBD Minimal invasive l Endoscopic extraction of calculi followed by cholecystectomy whether surgical or most commonly laparoscopic l PTC which provide drainage and subsequent choledochoscopy & stone extraction
Management of a case of stone CBD l Conventional choledochtomy l. Chole cystectomy and supra doudenal choledochtomy choledocholithotomy (exploration of the common bile duct) l. Trans doudenal sphincterotomy l. Choledocho douden ostomy
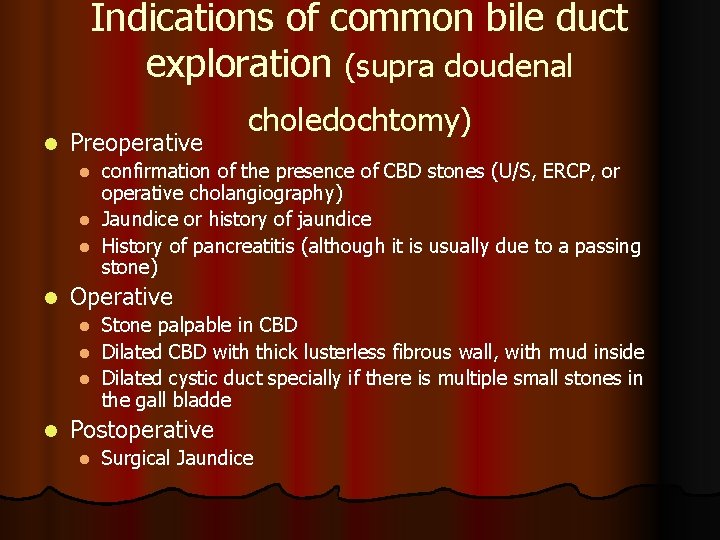
Indications of common bile duct exploration (supra doudenal l Preoperative choledochtomy) confirmation of the presence of CBD stones (U/S, ERCP, or operative cholangiography) l Jaundice or history of jaundice l History of pancreatitis (although it is usually due to a passing stone) l l Operative Stone palpable in CBD l Dilated CBD with thick lusterless fibrous wall, with mud inside l Dilated cystic duct specially if there is multiple small stones in the gall bladde l l Postoperative l Surgical Jaundice
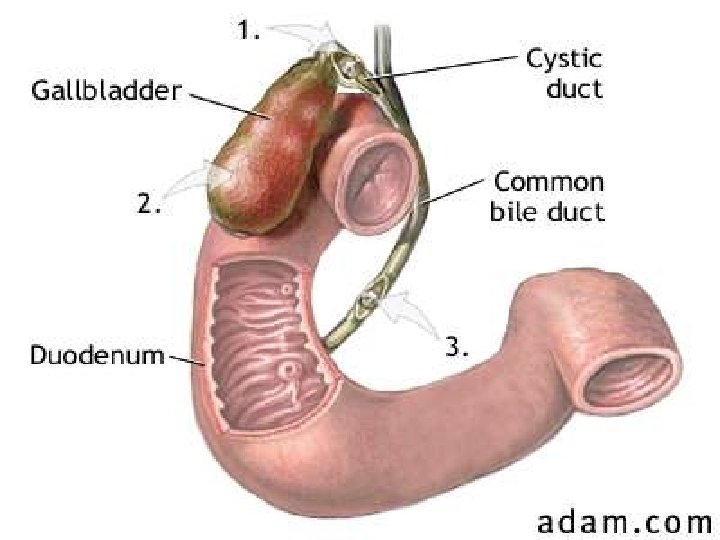
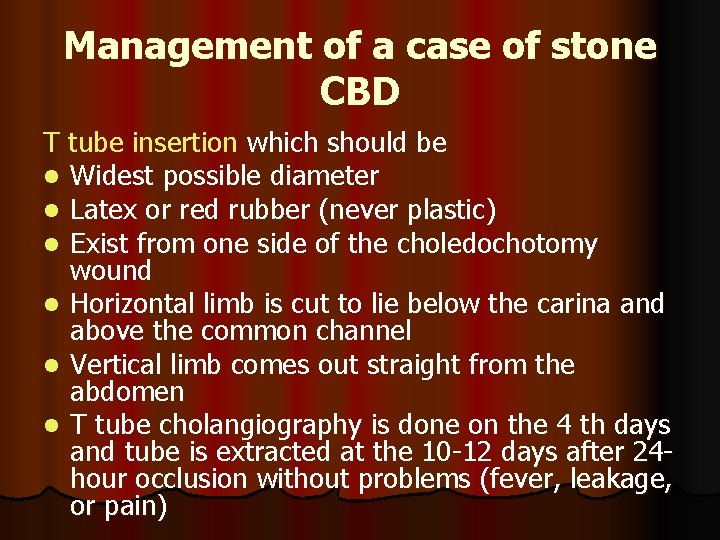
Management of a case of stone CBD T tube insertion which should be l Widest possible diameter l Latex or red rubber (never plastic) l Exist from one side of the choledochotomy wound l Horizontal limb is cut to lie below the carina and above the common channel l Vertical limb comes out straight from the abdomen l T tube cholangiography is done on the 4 th days and tube is extracted at the 10 -12 days after 24 hour occlusion without problems (fever, leakage, or pain)
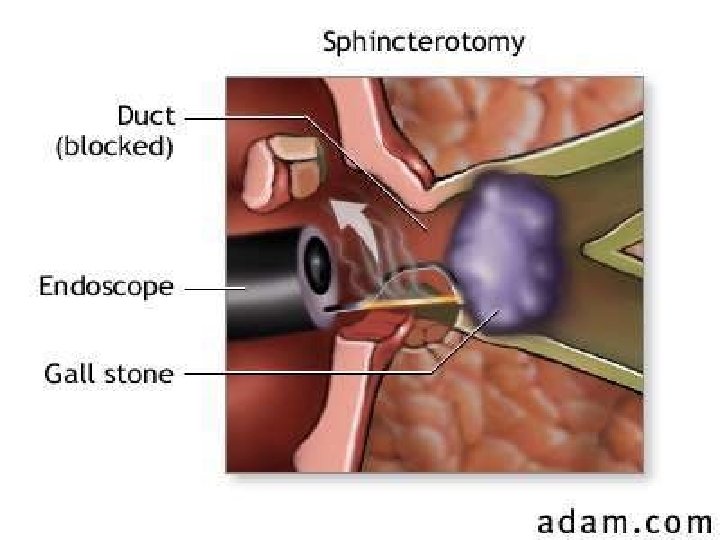
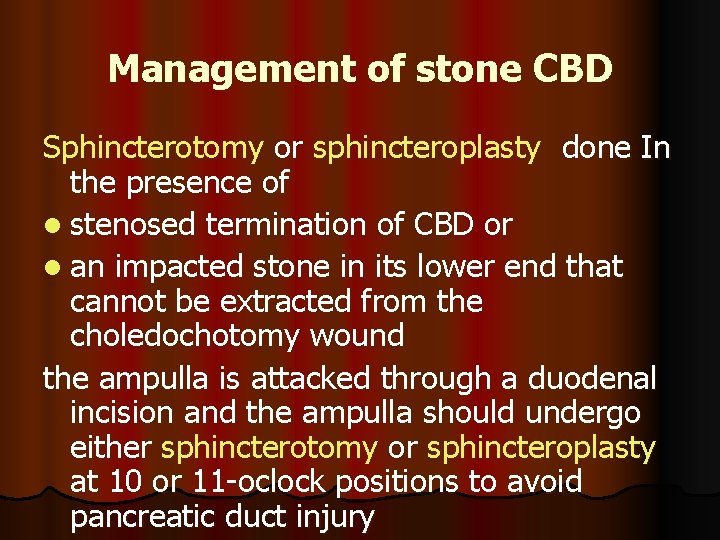
Management of stone CBD Sphincterotomy or sphincteroplasty done In the presence of l stenosed termination of CBD or l an impacted stone in its lower end that cannot be extracted from the choledochotomy wound the ampulla is attacked through a duodenal incision and the ampulla should undergo either sphincterotomy or sphincteroplasty at 10 or 11 -oclock positions to avoid pancreatic duct injury
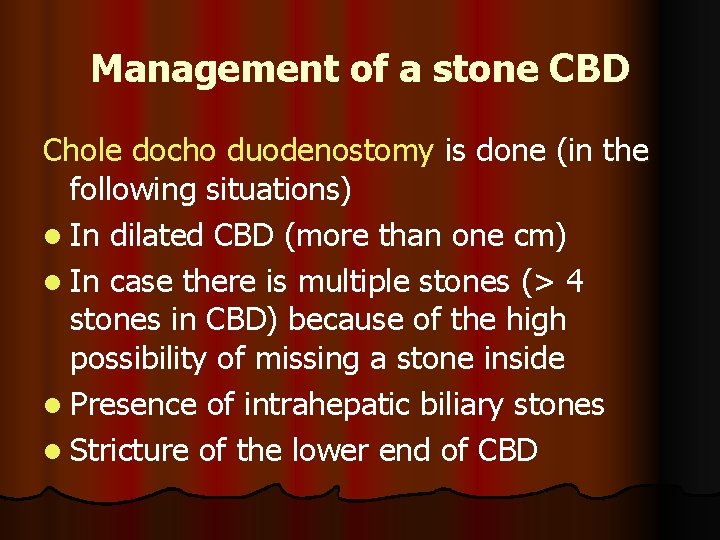
Management of a stone CBD Chole docho duodenostomy is done (in the following situations) l In dilated CBD (more than one cm) l In case there is multiple stones (> 4 stones in CBD) because of the high possibility of missing a stone inside l Presence of intrahepatic biliary stones l Stricture of the lower end of CBD
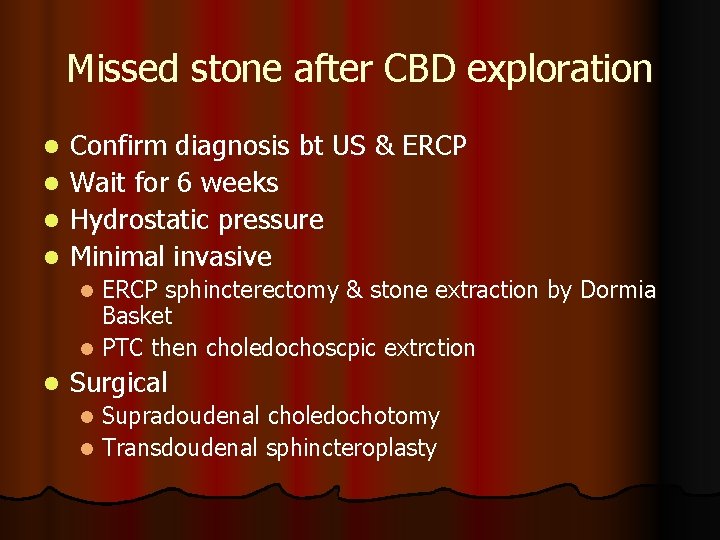
Missed stone after CBD exploration l l Confirm diagnosis bt US & ERCP Wait for 6 weeks Hydrostatic pressure Minimal invasive ERCP sphincterectomy & stone extraction by Dormia Basket l PTC then choledochoscpic extrction l l Surgical Supradoudenal choledochotomy l Transdoudenal sphincteroplasty l

Jaundice
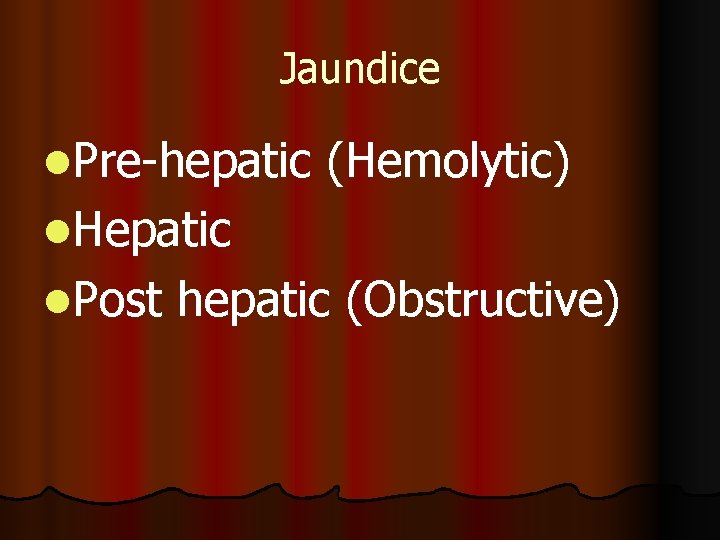
Jaundice l. Pre-hepatic (Hemolytic) l. Hepatic l. Post hepatic (Obstructive)
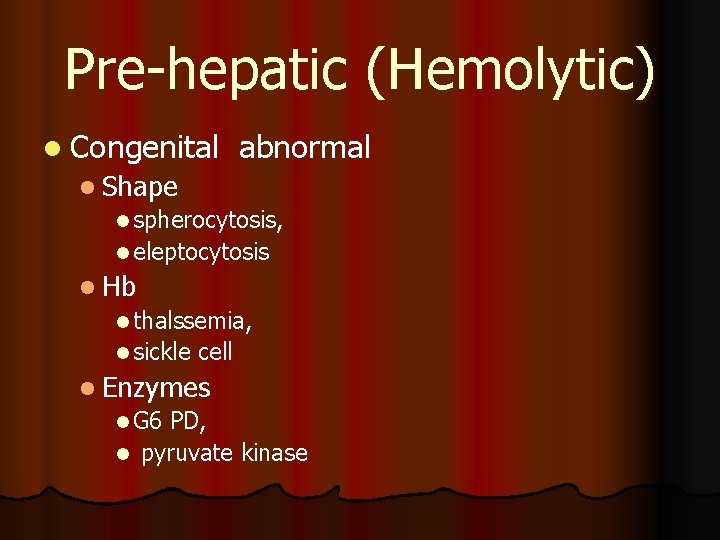
Pre-hepatic (Hemolytic) l Congenital abnormal l Shape l spherocytosis, l eleptocytosis l Hb l thalssemia, l sickle cell l Enzymes l G 6 PD, l pyruvate kinase
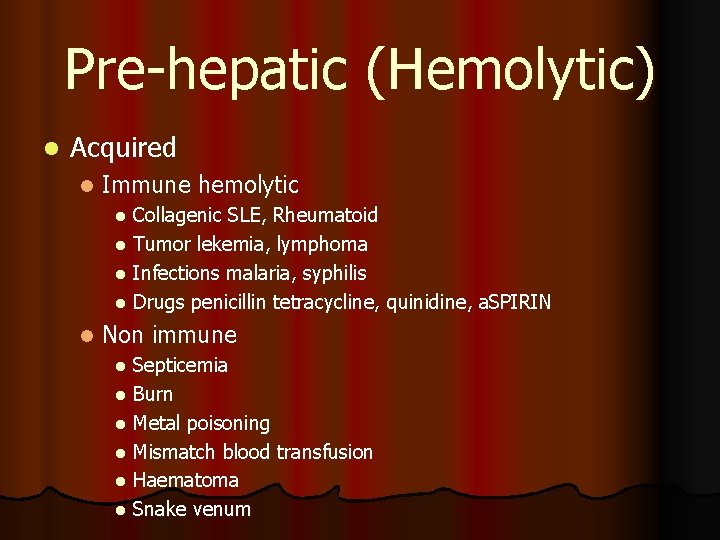
Pre-hepatic (Hemolytic) l Acquired l Immune hemolytic Collagenic SLE, Rheumatoid l Tumor lekemia, lymphoma l Infections malaria, syphilis l Drugs penicillin tetracycline, quinidine, a. SPIRIN l l Non immune Septicemia l Burn l Metal poisoning l Mismatch blood transfusion l Haematoma l Snake venum l
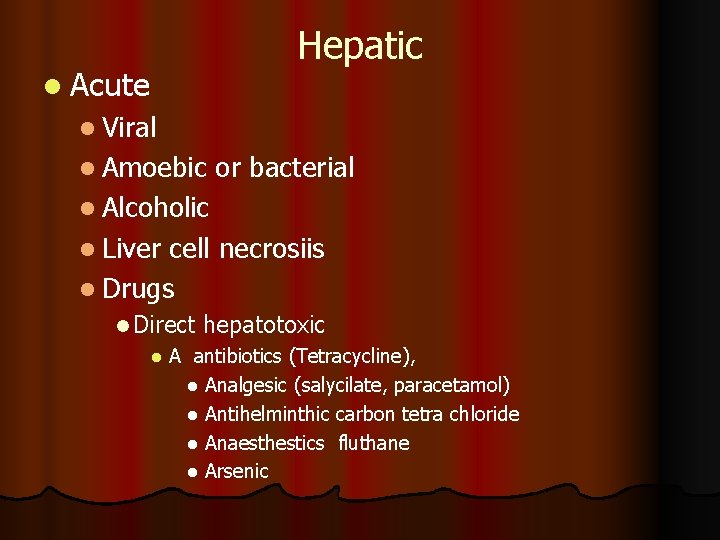
l Acute Hepatic l Viral l Amoebic or bacterial l Alcoholic l Liver cell necrosiis l Drugs l Direct hepatotoxic l A antibiotics (Tetracycline), l Analgesic (salycilate, paracetamol) l Antihelminthic carbon tetra chloride l Anaesthestics fluthane l Arsenic
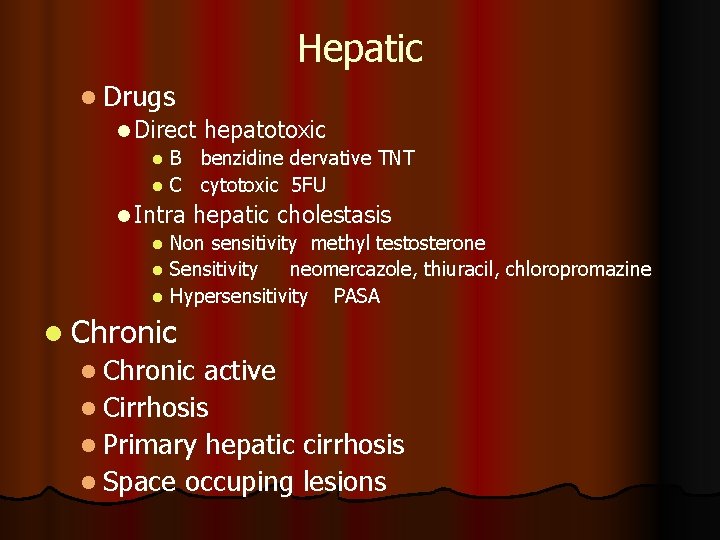
Hepatic l Drugs l Direct hepatotoxic B benzidine dervative TNT l C cytotoxic 5 FU l l Intra hepatic cholestasis l Non sensitivity methyl testosterone l Sensitivity neomercazole, thiuracil, chloropromazine l Hypersensitivity PASA l Chronic active l Cirrhosis l Primary hepatic cirrhosis l Space occuping lesions
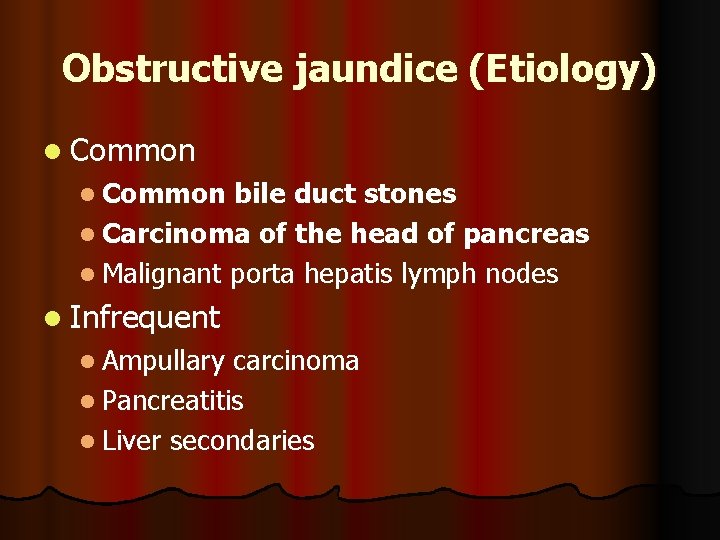
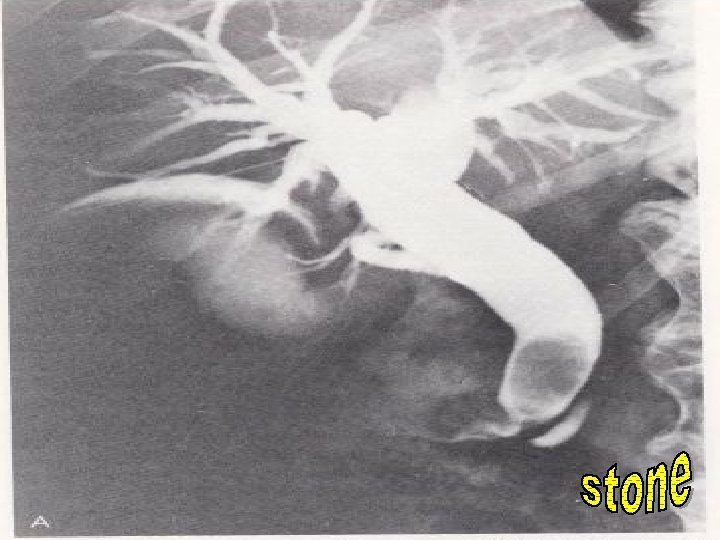
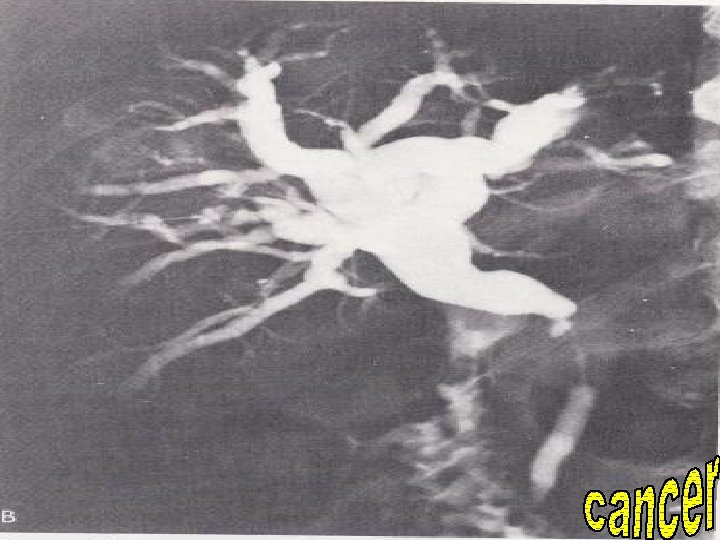
Obstructive jaundice (Etiology) l Common bile duct stones l Carcinoma of the head of pancreas l Malignant porta hepatis lymph nodes l Infrequent l Ampullary carcinoma l Pancreatitis l Liver secondaries
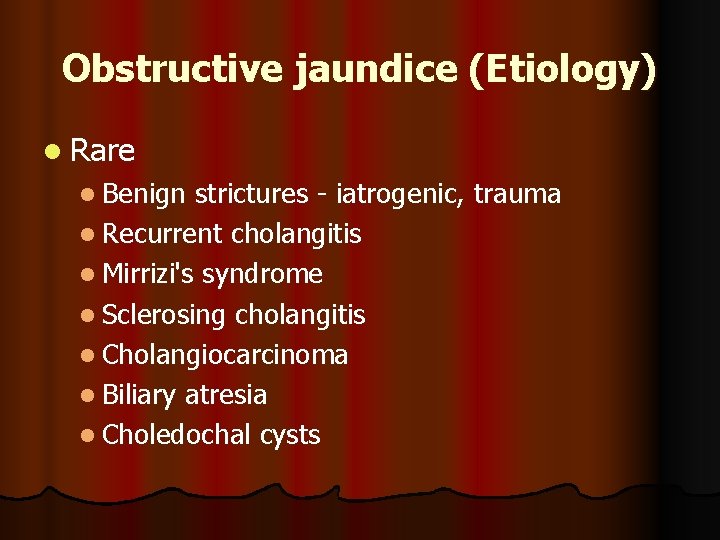
Obstructive jaundice (Etiology) l Rare l Benign strictures - iatrogenic, trauma l Recurrent cholangitis l Mirrizi's syndrome l Sclerosing cholangitis l Cholangiocarcinoma l Biliary atresia l Choledochal cysts
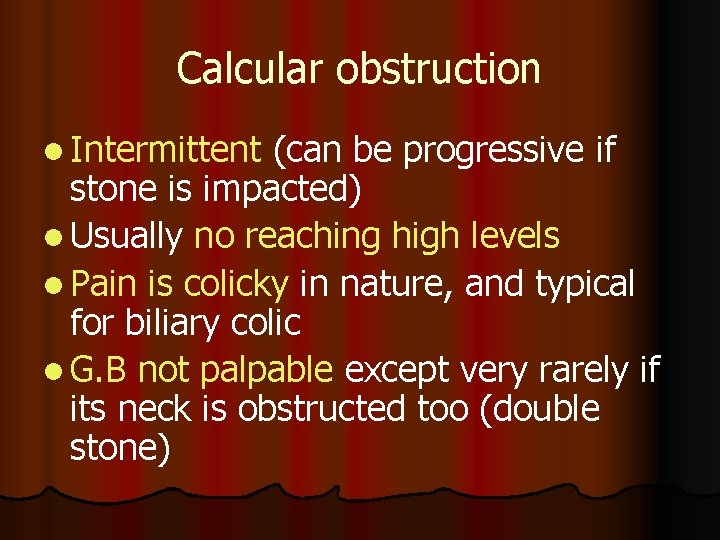
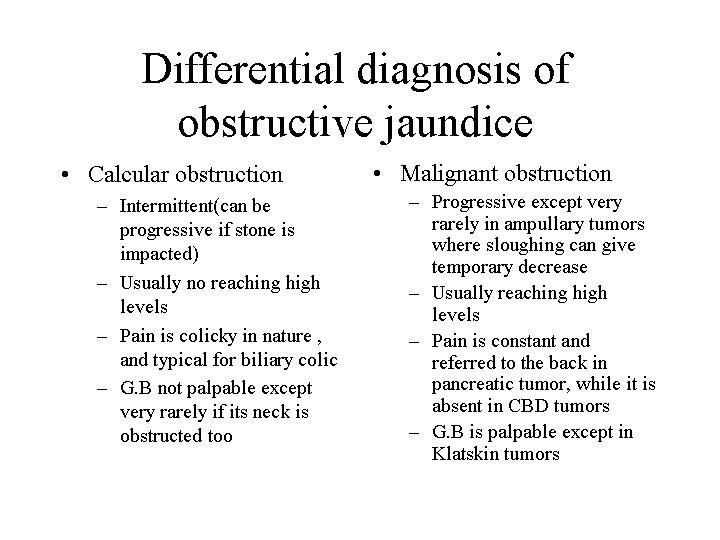
Calcular obstruction l Intermittent (can be progressive if stone is impacted) l Usually no reaching high levels l Pain is colicky in nature, and typical for biliary colic l G. B not palpable except very rarely if its neck is obstructed too (double stone)
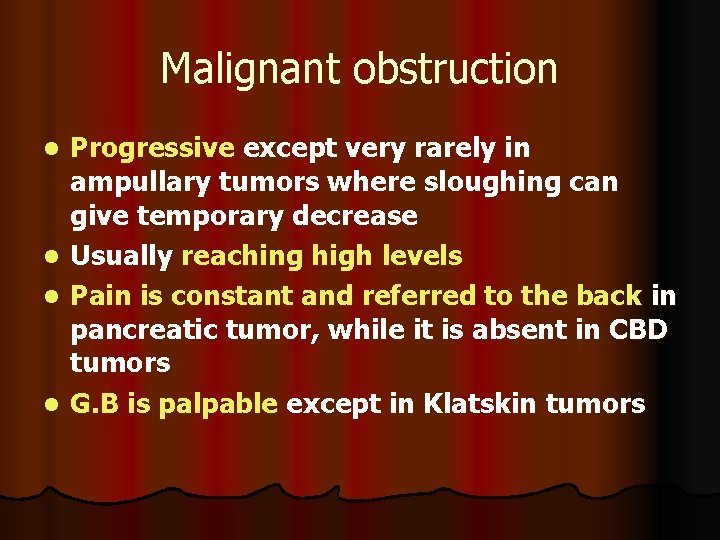
Malignant obstruction Progressive except very rarely in ampullary tumors where sloughing can give temporary decrease l Usually reaching high levels l Pain is constant and referred to the back in pancreatic tumor, while it is absent in CBD tumors l G. B is palpable except in Klatskin tumors l
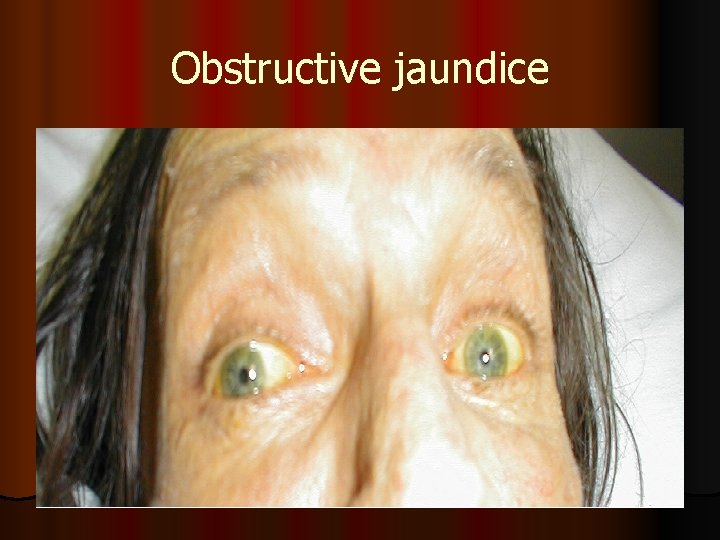
Obstructive jaundice
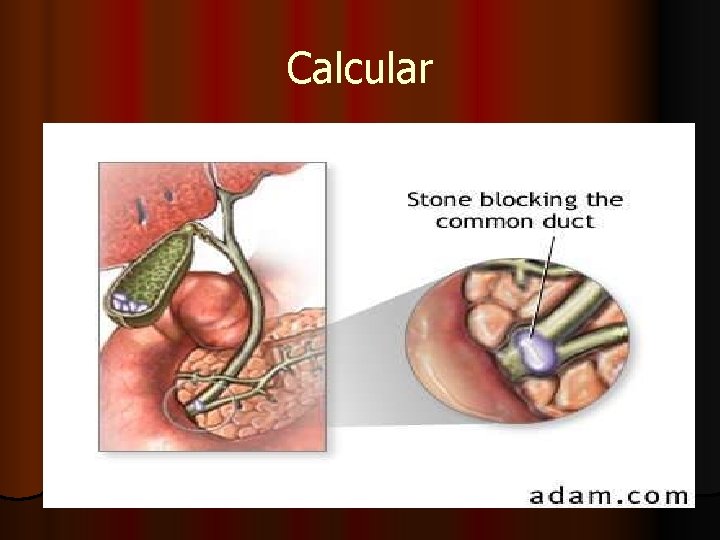
Calcular
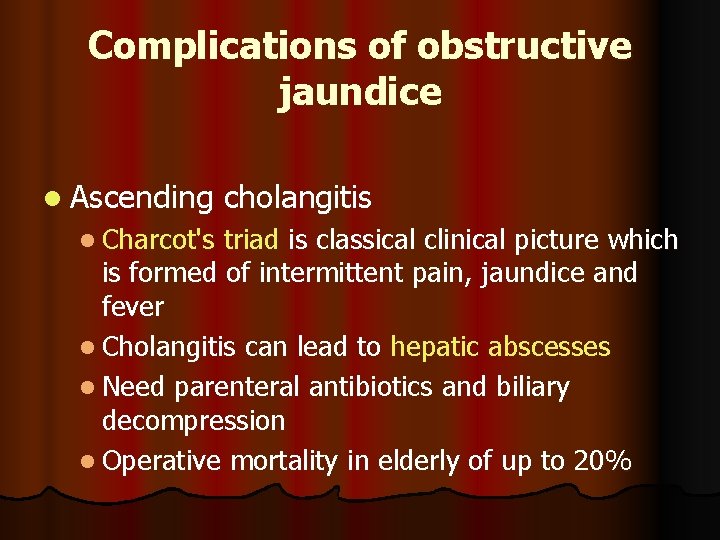
Complications of obstructive jaundice l Ascending l Charcot's cholangitis triad is classical clinical picture which is formed of intermittent pain, jaundice and fever l Cholangitis can lead to hepatic abscesses l Need parenteral antibiotics and biliary decompression l Operative mortality in elderly of up to 20%
Complications of obstructive jaundice l Clotting disorders l Vitamin K required for gamma-carboxylation of Factors II, VII, IX, XI l Vitamin K is fat-soluble. No absorbed. So it needs to be given parenterally l Urgent correction will need Fresh Frozen Plasma l Also endotoxin activation of complement system
Complications of obstructive jaundice Hepato-renal syndrome l Poorly understood l Renal failure post intervention l Most probably due to gram negative endotoxinaemia from gut l Preoperative lactulose may improve outcome by improving altered systemic and renal haemodynamics l Drug Metabolism l Half-life of some drugs prolonged. (E. g. morphine) l Impaired wound healing. l
Investigations for a case of obstructive jaundice Laboratory l Raised l Direct bilirubin (in most of the cases the indirect bilirubin also rises due to hepatic cellular malfunction). l Alkaline phosphatase l Gamma glutamyl transferase l 5 nucleotidase
Investigations for a case of obstructive jaundice Laboratory l Mild elevation or normal l SGOT & SGPT (these are shooting in viral hepatitis) l Slightly depressed or normal l Prothrombin time (due to avitaminosis K) l Urine urobilinogen
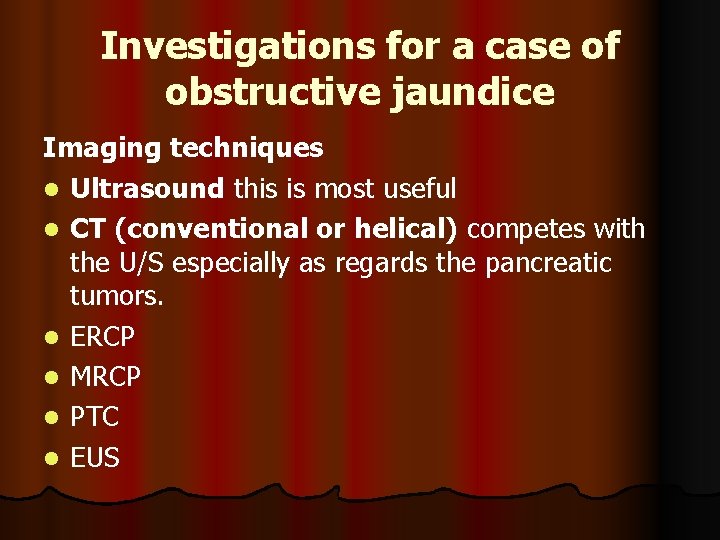
Investigations for a case of obstructive jaundice Imaging techniques l Ultrasound this is most useful l CT (conventional or helical) competes with the U/S especially as regards the pancreatic tumors. l ERCP l MRCP l PTC l EUS
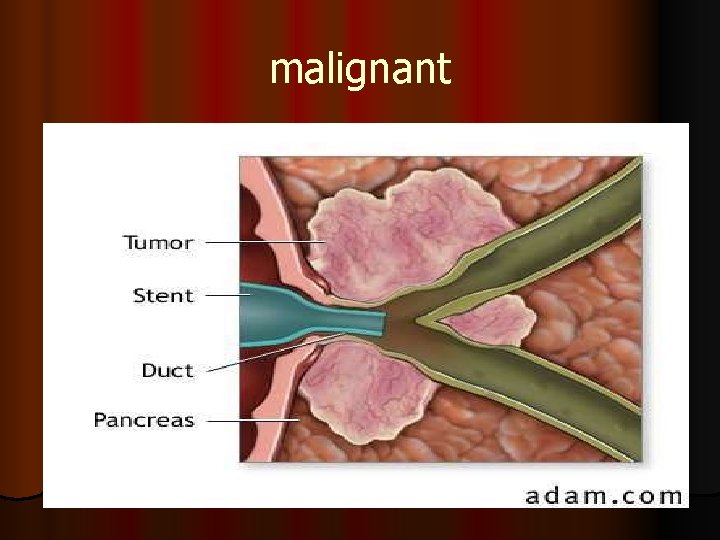
malignant
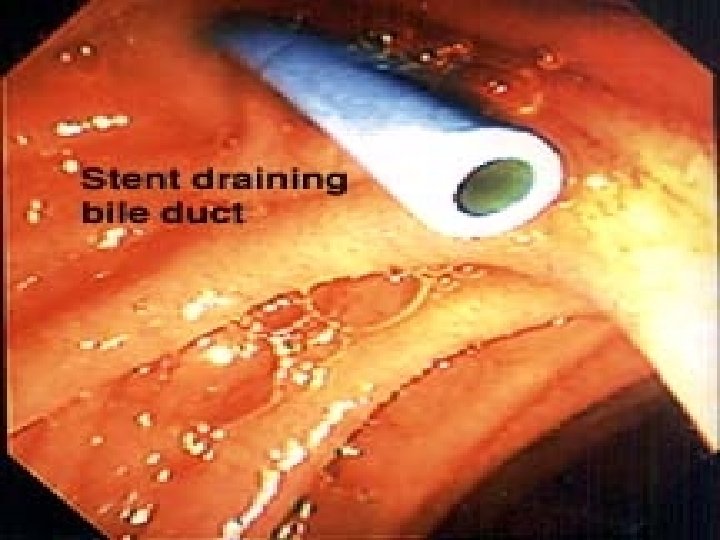
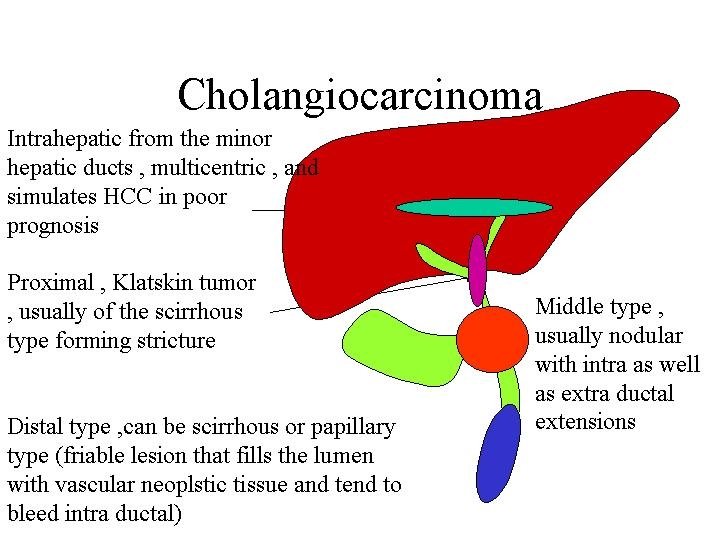
Treatment for cholangiocarcinoma of CBD Palliative l Plastic stent insertion through ERCP l Stent insertion through percutanous transhepatic route l Self-expanding stainless steel wire biliary endoprosthesis is new modality with high patency rate, and less infection rate
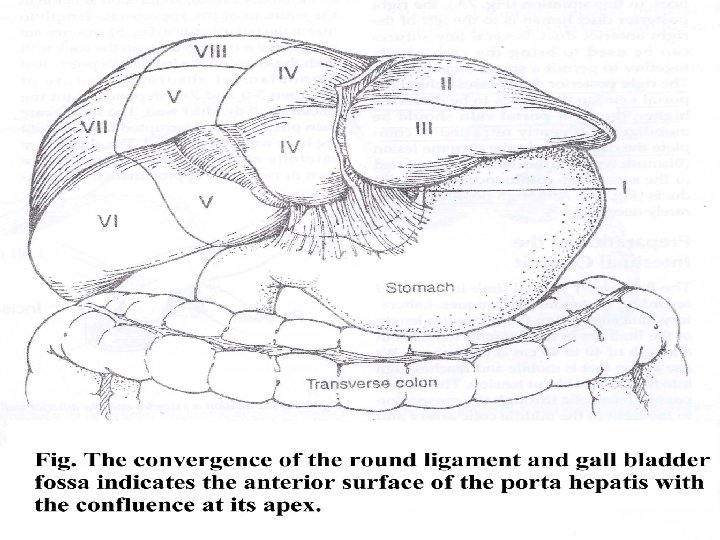
Treatment for cholangiocarcinoma of CBD Palliative l Bypass surgery l Round ligament approach for Klatiskin tumors (on condition that the carina is permitting right to left communication) l Hepatico jujenostomy for middle and low tumors l Cholecystojujenostomy for low tumors. l usually we add gastrojujenostomy and enteroanastomosis (triple anastomosis) for pancreatic head tumors
Treatment for cholangiocarcinoma of CBD For operable cancers l For Klastiskin tumor, segment IV excision provides good access to the confluence l allows good proximal clearance and facilitates hepaticojujenostomy l l For middle tumors excision of the tumor from just below the carina to the duodenum is done with hepaticojujenostomy l For distal tumors. Whipple operation is done
Biliary stricture Etiology Congenital (biliary atresia) l Traumatic (most important, and usually follow cholecystectomy) l Complete ligation of CBD l Narrowing of the duct by partial inclusion in a ligature l Ischemia of the duct, or diathermy injury l Inflammatory Sclerosing cholangitis (multiple strictures separated by normal or dilated segments). l Cholangiocarcinoma l
Sclerosing cholangitis l PSC (primary sclerosing choangitis ) is a chronic cholestatic biliary disease characterized by non suppurative inflammation and fibrosis of the biliary ductal system. l The cause is unknown but is associated with autoimmune inflammatory diseases such as chronic ulcerative colitis.
Sclerosing cholangitis l Most patients present with fatigue and pruritus and, occasionally, jaundice. l The natural history is variable but involves progressive destruction of the bile ducts, leading to cirrhosis and liver failure.
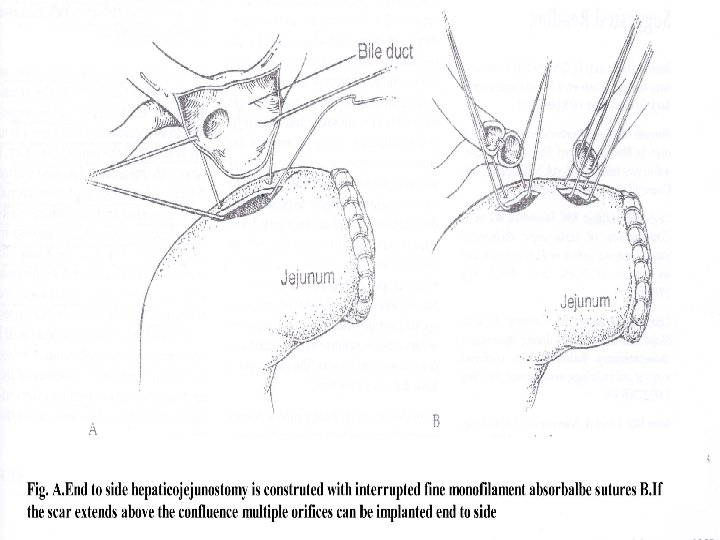
Biliary stricture l Investigations used are similar to those used in any case of obstructive jaundice (U/S then CT, ERCP, MRCP or PTC l Treatment is centered on creating a biliary enteric anastomosis with mucosa-tomucosa sutures without compromising the blood supply of any of the ends.
- Slides: 147