Better Blood Transfusion Continuing Education Programme Module 1
Better Blood Transfusion Continuing Education Programme Module 1 - Safe Transfusion Practice Generic Programme Transfusion Practitioners, Cathy Collins and Lorna Sinclair 1 STPL 1 GENv 2007 to SNBTS www. learnbloodtransfusion. org. uk
Learning Outcomes By the end of this session you will be able to: • Understand the hazards of transfusion • Understand basic ABO serology • Take a blood sample for pre-transfusion testing correctly • Store blood components correctly • Collect blood components safely • Administer a blood transfusion safely • Take initial action to manage a transfusion adverse event 2 STPL 1 GENv 2007 to SNBTS www. learnbloodtransfusion. org. uk
Further Information • Hospital Blood Transfusion Policy/ Procedure Manual • The Handbook of Transfusion Medicine [4 th Ed] (2007) web site www. transfusionguidelines. org. uk • BCSH Guidelines: web site www. bcshguidelines. com • Serious Hazards of Transfusion Annual Report web site www. shotuk. org • Local Transfusion Practitioner/ Haemovigilance Officer • Hospital Transfusion Laboratory • Local Better Blood Transfusion Team web site wwwtransfusionguidlines. org. uk 3 STPL 1 GENv 2007 to SNBTS www. learnbloodtransfusion. org. uk
www. learnbloodtransfusion. org. uk 4 STPL 1 GENv 2007 to SNBTS www. learnbloodtransfusion. org. uk
Serious Hazards of Transfusion Reporting Scheme 5 STPL 1 GENv 2007 to SNBTS www. learnbloodtransfusion. org. uk
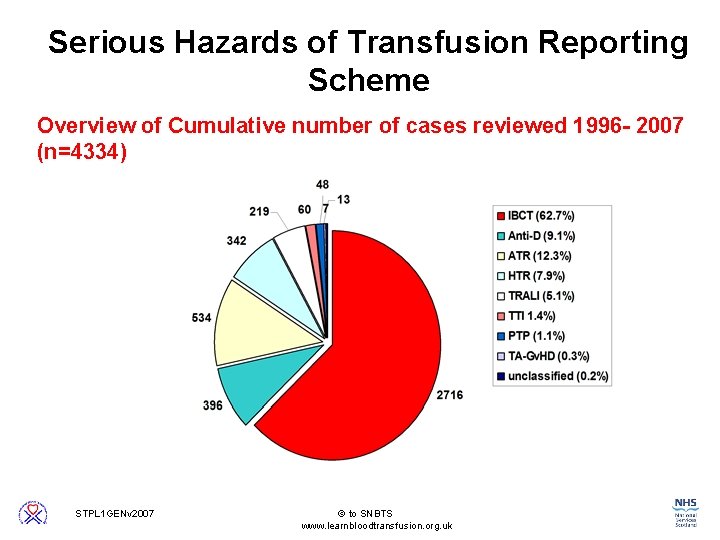
Serious Hazards of Transfusion Reporting Scheme Overview of Cumulative number of cases reviewed 1996 - 2007 (n=4334) 6 STPL 1 GENv 2007 to SNBTS www. learnbloodtransfusion. org. uk
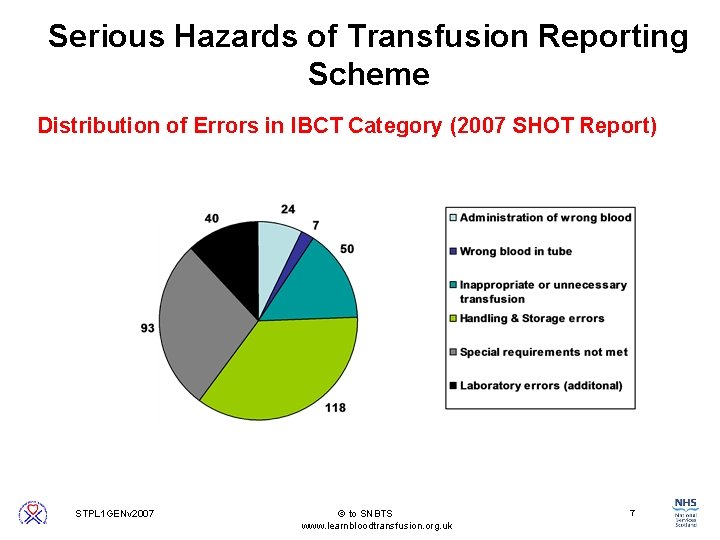
Serious Hazards of Transfusion Reporting Scheme Distribution of Errors in IBCT Category (2007 SHOT Report) 7 STPL 1 GENv 2007 to SNBTS www. learnbloodtransfusion. org. uk
Serious Hazards of Transfusion Reporting Scheme Key Haemovigilance Messages • All of the cases in the wrong blood transfused category would have been prevented had the final bedside check been performed correctly • The majority of inappropriate or unnecessary transfusions were due to knowledge gaps and / or lack of training and education in junior doctors • It is an individual’s professional responsibility to ensure that they have adequate knowledge, skills and understanding before performing any task in the transfusion process 8 STPL 1 GENv 2007 to SNBTS www. learnbloodtransfusion. org. uk
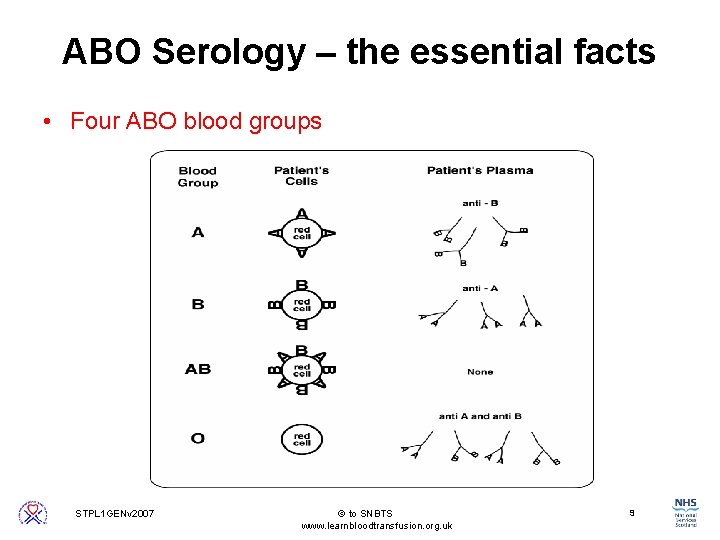
ABO Serology – the essential facts • Four ABO blood groups 9 STPL 1 GENv 2007 to SNBTS www. learnbloodtransfusion. org. uk
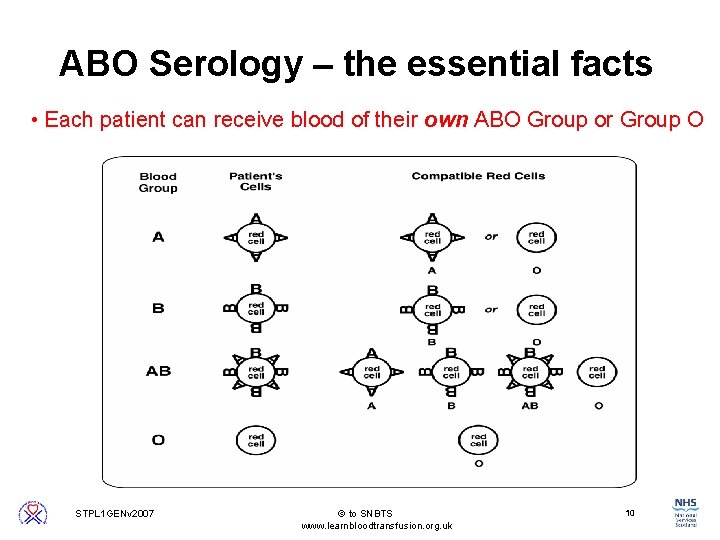
ABO Serology – the essential facts • Each patient can receive blood of their own ABO Group or Group O 10 STPL 1 GENv 2007 to SNBTS www. learnbloodtransfusion. org. uk
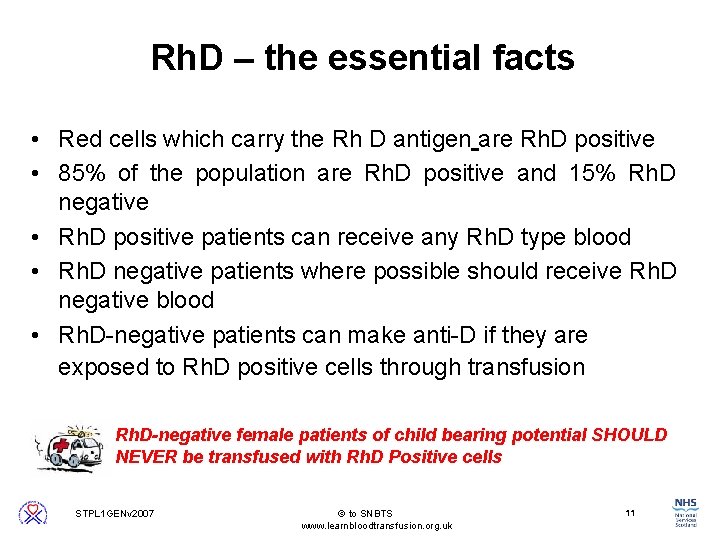
Rh. D – the essential facts • Red cells which carry the Rh D antigen are Rh. D positive • 85% of the population are Rh. D positive and 15% Rh. D negative • Rh. D positive patients can receive any Rh. D type blood • Rh. D negative patients where possible should receive Rh. D negative blood • Rh. D-negative patients can make anti-D if they are exposed to Rh. D positive cells through transfusion Rh. D-negative female patients of child bearing potential SHOULD NEVER be transfused with Rh. D Positive cells 11 STPL 1 GENv 2007 to SNBTS www. learnbloodtransfusion. org. uk
Decision to Transfuse • Communicate with patient • Patient information leaflet • Document in patient notes 12 STPL 1 GENv 2007 to SNBTS www. learnbloodtransfusion. org. uk
Requesting Procedure • Check the patient case notes – Transfusion history – Special requirements e. g. , irradiated, CMV negative – Complete request form or order com 13 STPL 1 GENv 2007 to SNBTS www. learnbloodtransfusion. org. uk
Sampling Procedure Step 1: Ask the patient to tell you their: Full Name + Date of Birth Check this information against the patient’s identification band Be extra vigilant when checking the identity of the unconscious / compromised patient 14 STPL 1 GENv 2007 to SNBTS www. learnbloodtransfusion. org. uk
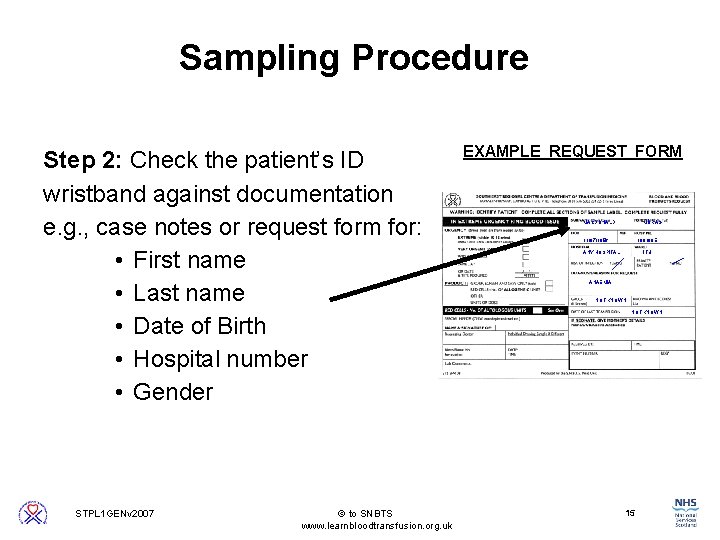
Sampling Procedure Step 2: Check the patient’s ID wristband against documentation e. g. , case notes or request form for: • First name • Last name • Date of Birth • Hospital number • Gender EXAMPLE REQUEST FORM MACDONALD MORAG 11/07/1956 100198 E ANY HOSPITAL ITU ANAEMIA NOT KNOWN 15 STPL 1 GENv 2007 to SNBTS www. learnbloodtransfusion. org. uk
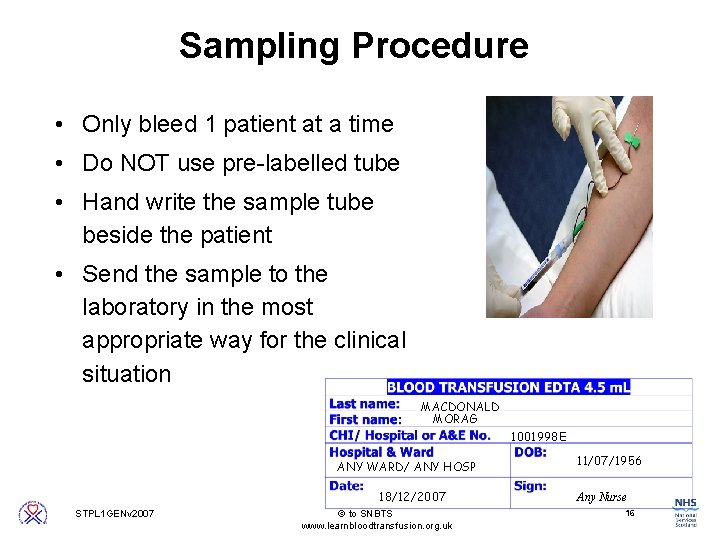
Sampling Procedure • Only bleed 1 patient at a time • Do NOT use pre-labelled tube • Hand write the sample tube beside the patient • Send the sample to the laboratory in the most appropriate way for the clinical situation MACDONALD MORAG 1001998 E ANY WARD/ ANY HOSP 18/12/2007 11/07/1956 Any Nurse 16 STPL 1 GENv 2007 to SNBTS www. learnbloodtransfusion. org. uk
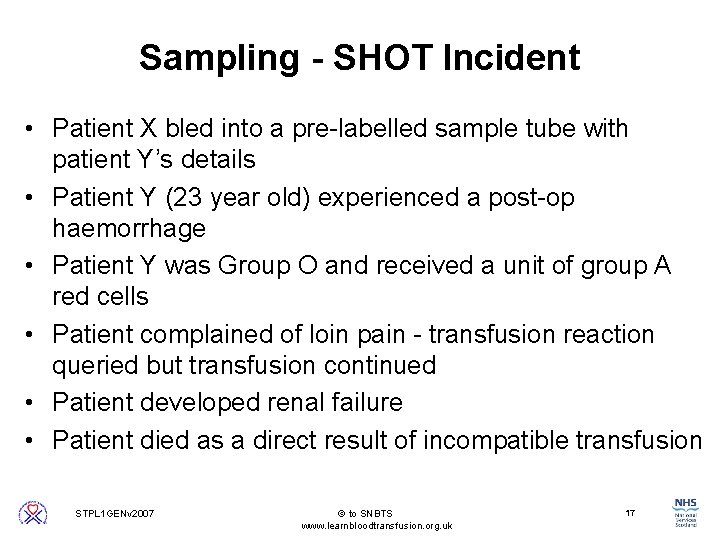
Sampling - SHOT Incident • Patient X bled into a pre-labelled sample tube with patient Y’s details • Patient Y (23 year old) experienced a post-op haemorrhage • Patient Y was Group O and received a unit of group A red cells • Patient complained of loin pain - transfusion reaction queried but transfusion continued • Patient developed renal failure • Patient died as a direct result of incompatible transfusion 17 STPL 1 GENv 2007 to SNBTS www. learnbloodtransfusion. org. uk
Pre-transfusion Testing – What happens in the Lab? 1. Check Historical Records 2. GROUP – identify ABO and Rh group 3. SCREEN – Check plasma for antibodies 4. CROSSMATCH – Select Component 5. PLASMA – Stored for up to 7 days 18 STPL 1 GENv 2007 to SNBTS www. learnbloodtransfusion. org. uk
Storage Component • Red blood cells • Platelets • Fresh Frozen Plasma • Cryoprecipitate 19 STPL 1 GENv 2007 to SNBTS www. learnbloodtransfusion. org. uk
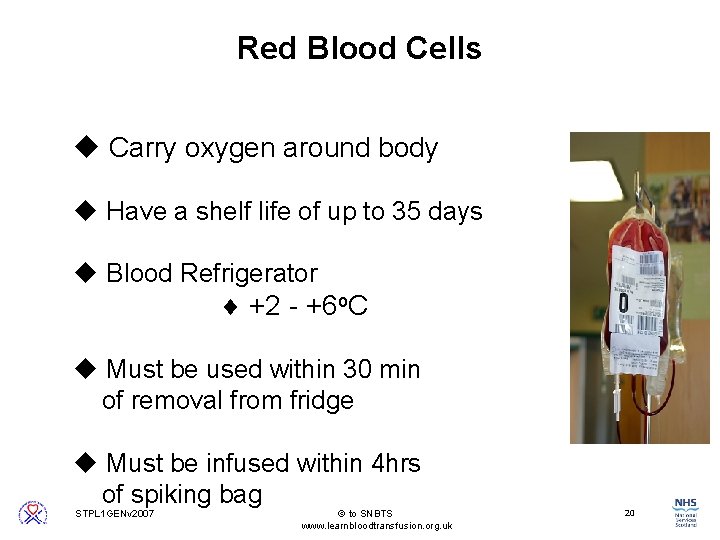
Red Blood Cells u Carry oxygen around body u Have a shelf life of up to 35 days u Blood Refrigerator ¨ +2 - +6 o. C u Must be used within 30 min of removal from fridge u Must be infused within 4 hrs of spiking bag 20 STPL 1 GENv 2007 to SNBTS www. learnbloodtransfusion. org. uk
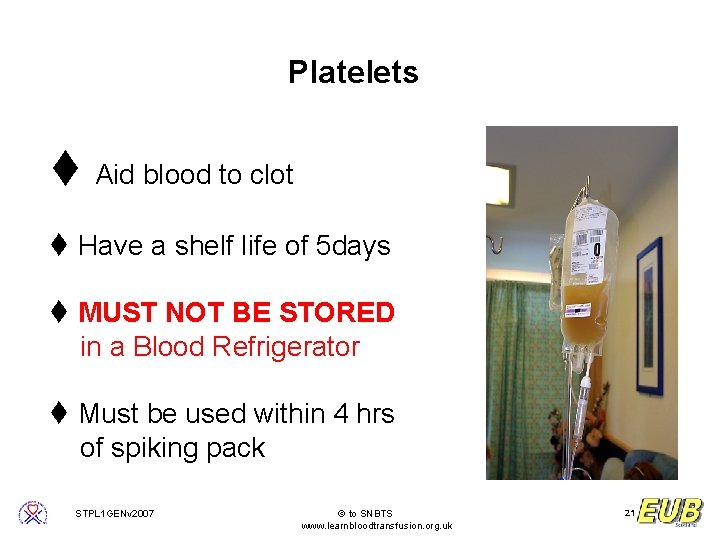
Platelets t Aid blood to clot t Have a shelf life of 5 days t MUST NOT BE STORED in a Blood Refrigerator t Must be used within 4 hrs of spiking pack 21 STPL 1 GENv 2007 to SNBTS www. learnbloodtransfusion. org. uk
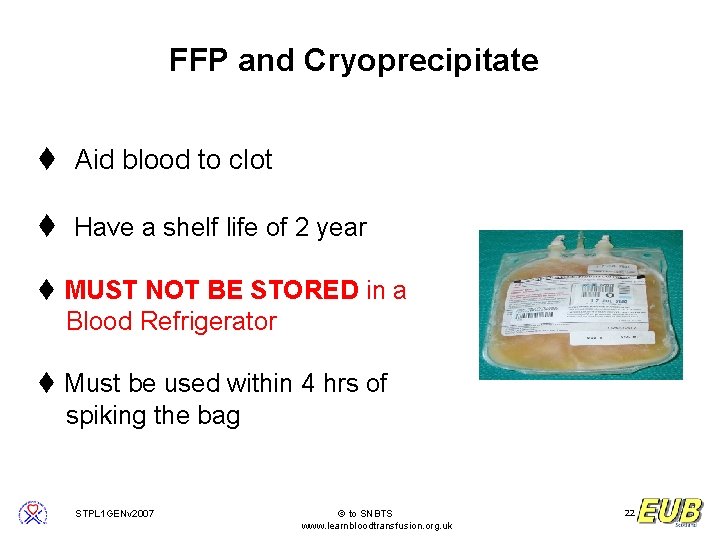
FFP and Cryoprecipitate t Aid blood to clot t Have a shelf life of 2 year t MUST NOT BE STORED in a Blood Refrigerator t Must be used within 4 hrs of spiking the bag 22 STPL 1 GENv 2007 to SNBTS www. learnbloodtransfusion. org. uk
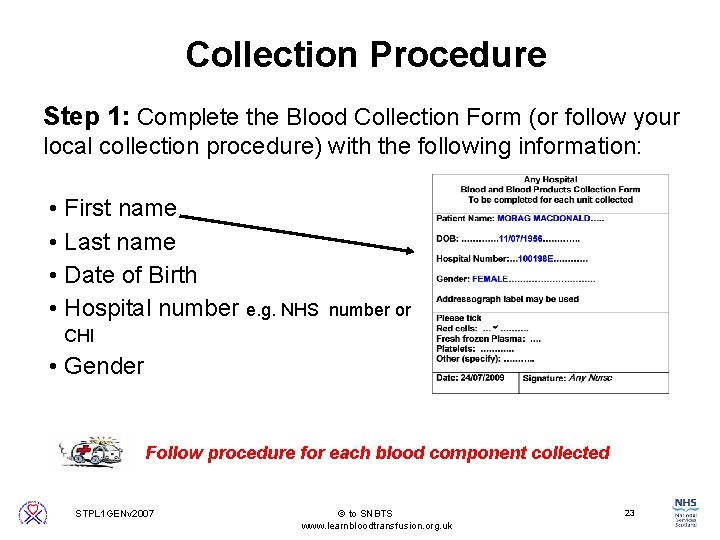
Collection Procedure Step 1: Complete the Blood Collection Form (or follow your local collection procedure) with the following information: • First name • Last name • Date of Birth • Hospital number e. g. NHS number or CHI • Gender Follow procedure for each blood component collected 23 STPL 1 GENv 2007 to SNBTS www. learnbloodtransfusion. org. uk
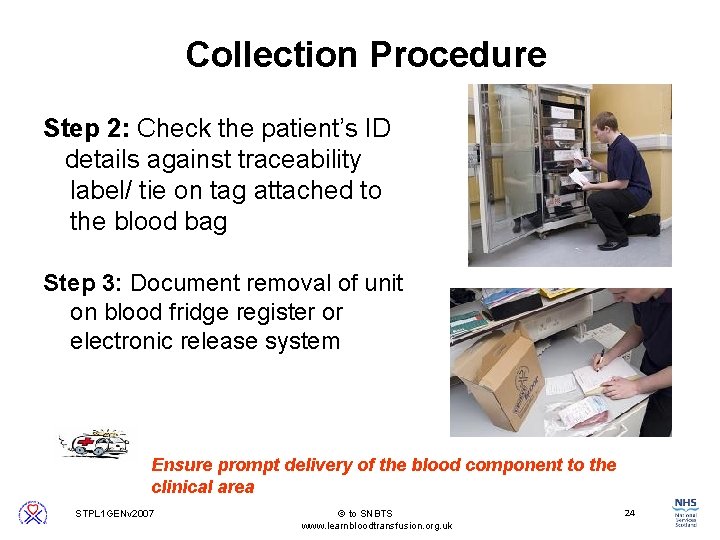
Collection Procedure Step 2: Check the patient’s ID details against traceability label/ tie on tag attached to the blood bag Step 3: Document removal of unit on blood fridge register or electronic release system Ensure prompt delivery of the blood component to the clinical area 24 STPL 1 GENv 2007 to SNBTS www. learnbloodtransfusion. org. uk
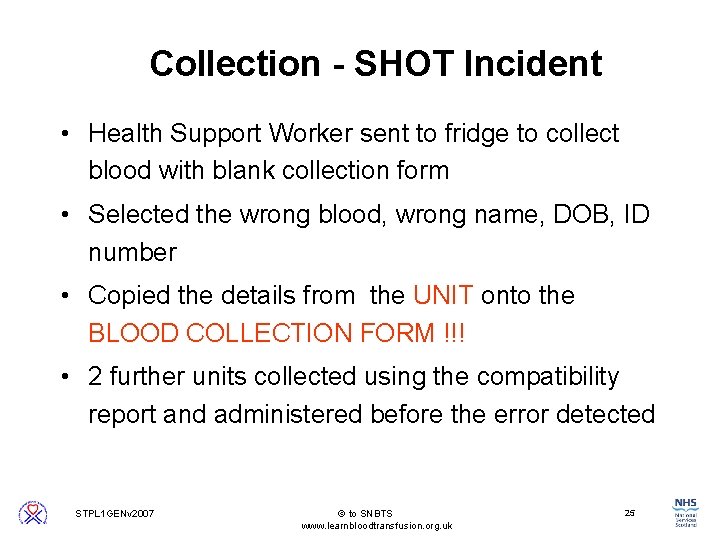
Collection - SHOT Incident • Health Support Worker sent to fridge to collect blood with blank collection form • Selected the wrong blood, wrong name, DOB, ID number • Copied the details from the UNIT onto the BLOOD COLLECTION FORM !!! • 2 further units collected using the compatibility report and administered before the error detected 25 STPL 1 GENv 2007 to SNBTS www. learnbloodtransfusion. org. uk
Administration Process Equipment • Venous access devices • Blood administration sets • Infusion fluids • Infusion devices 26 STPL 1 GENv 2007 to SNBTS www. learnbloodtransfusion. org. uk
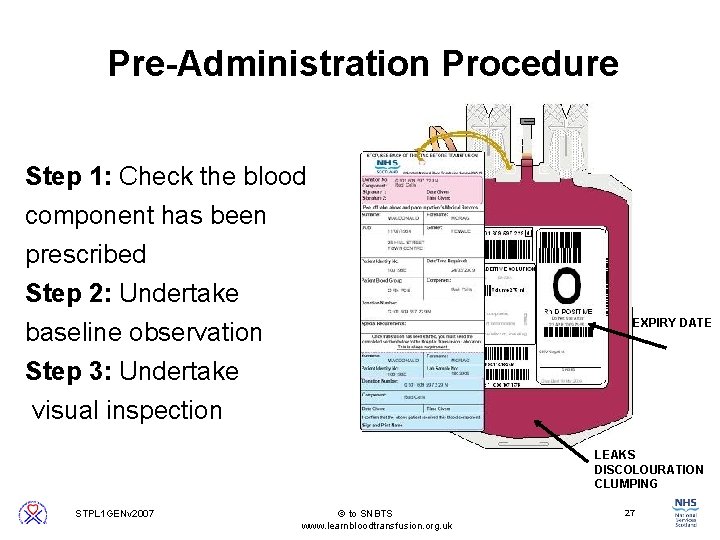
Pre-Administration Procedure Step 1: Check the blood component has been prescribed Step 2: Undertake baseline observation Step 3: Undertake EXPIRY DATE visual inspection LEAKS DISCOLOURATION CLUMPING 27 STPL 1 GENv 2007 to SNBTS www. learnbloodtransfusion. org. uk
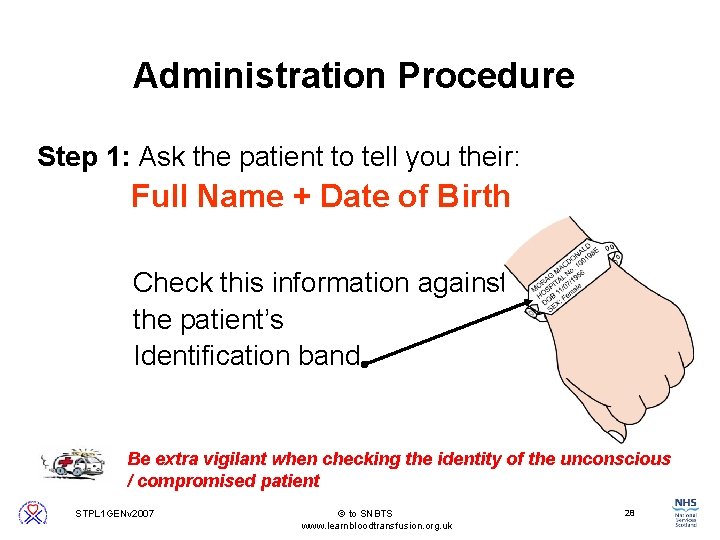
Administration Procedure Step 1: Ask the patient to tell you their: Full Name + Date of Birth Check this information against the patient’s Identification band Be extra vigilant when checking the identity of the unconscious / compromised patient 28 STPL 1 GENv 2007 to SNBTS www. learnbloodtransfusion. org. uk
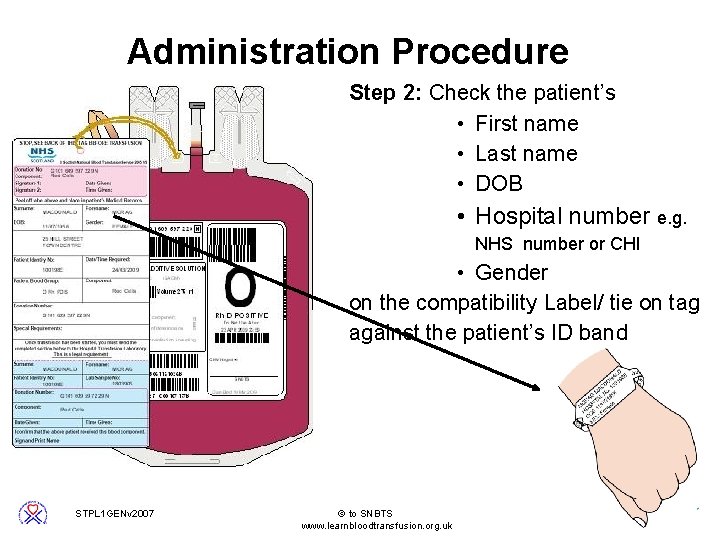
Administration Procedure Step 2: Check the patient’s • First name • Last name • DOB • Hospital number e. g. NHS number or CHI • Gender on the compatibility Label/ tie on tag against the patient’s ID band 29 STPL 1 GENv 2007 to SNBTS www. learnbloodtransfusion. org. uk
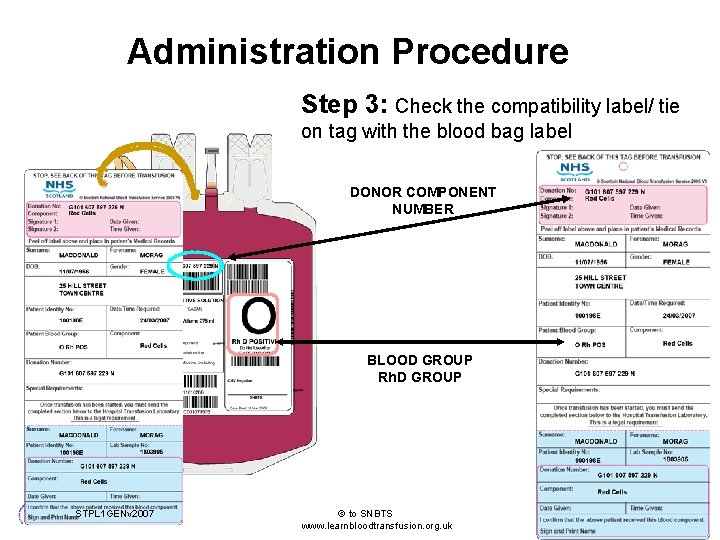
Administration Procedure Step 3: Check the compatibility label/ tie on tag with the blood bag label DONOR COMPONENT NUMBER BLOOD GROUP Rh. D GROUP 30 STPL 1 GENv 2007 to SNBTS www. learnbloodtransfusion. org. uk
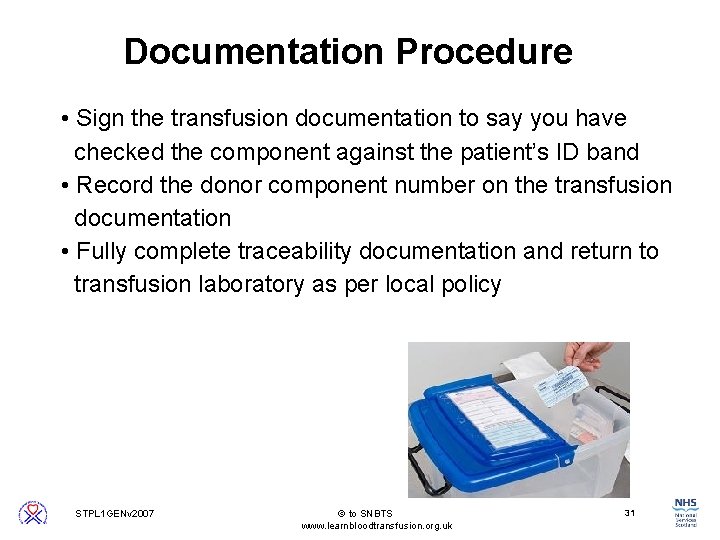
Documentation Procedure • Sign the transfusion documentation to say you have checked the component against the patient’s ID band • Record the donor component number on the transfusion documentation • Fully complete traceability documentation and return to transfusion laboratory as per local policy 31 STPL 1 GENv 2007 to SNBTS www. learnbloodtransfusion. org. uk
Administration - SHOT Incident • Operating department assistant collected 1 unit of red cells from the satellite fridge • Incorrect component collected: wrong name; DOB; Hospital Number • Final patient identification check not undertaken by anaesthetist / ODA • Group O patient received 1 unit Group B red cells • Patient admitted to ICU - but died as a result of ABO incompatible transfusion 32 STPL 1 GENv 2007 to SNBTS www. learnbloodtransfusion. org. uk
Monitoring Procedure • Inform the patient of how to obtain assistance • Record vital signs *Early Check* • Each unit must be infused within 4 hours of removal from blood fridge • Complete documentation 33 STPL 1 GENv 2007 to SNBTS www. learnbloodtransfusion. org. uk
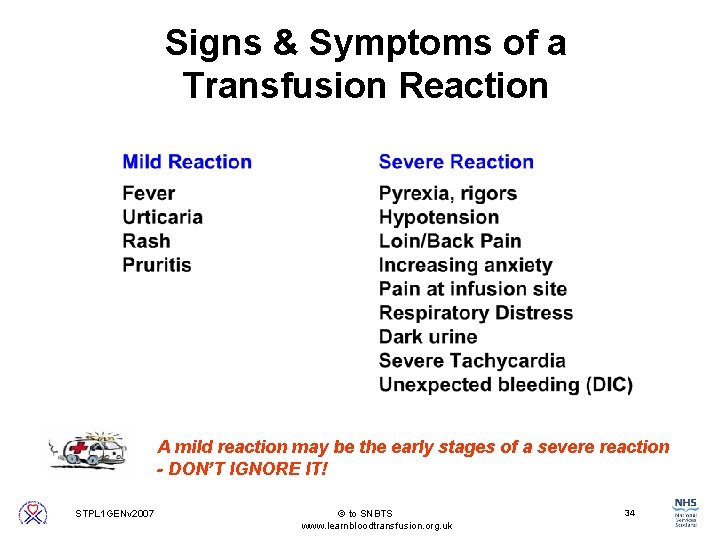
Signs & Symptoms of a Transfusion Reaction A mild reaction may be the early stages of a severe reaction - DON’T IGNORE IT! 34 STPL 1 GENv 2007 to SNBTS www. learnbloodtransfusion. org. uk
Management of a Mild Acute Transfusion Reaction 1. Stop the transfusion (check patient and component compatibility) 2. Seek medical advice 3. Assess patient 4. Commence appropriate treatment If signs & symptoms worsen within 15 minutes treat as a severe reaction 35 STPL 1 GENv 2007 to SNBTS www. learnbloodtransfusion. org. uk
Management of a Severe Transfusion Reaction 1. Stop the transfusion Replace the administration set IV access should be maintained with normal saline (check patient and component compatibility) 2. Call the doctor to see the patient urgently 3. Assess patient - resuscitate as required 4. Inform the HTL and return the component 5. Document event in patient case notes 36 STPL 1 GENv 2007 to SNBTS www. learnbloodtransfusion. org. uk
Monitoring Procedure. SHOT Incident • 2 patients with same surname in the same ward having a blood transfusion • Patient identification check not undertaken • Group O patient transfused with Group A RBCs • Patient complained of generalised pain • Transfusion continued • Patient became very ill and died 6 hours later 37 STPL 1 GENv 2007 to SNBTS www. learnbloodtransfusion. org. uk
Safer Practice Takes Seconds A consistent, professional approach to safe transfusion practice can save lives I’d like to know who I can blame … I still feel hate. I am furious and angry … someone couldn’t be bothered to treat my child in a professional and safe manner. Mrs Green 15/12/98 38 STPL 1 GENv 2007 to SNBTS www. learnbloodtransfusion. org. uk
Any Questions? 39 STPL 1 GENv 2007 to SNBTS www. learnbloodtransfusion. org. uk
5 STEP GUIDE TO TRANSFUSION TAG & LABEL 40 STPL 1 GENv 2007 to SNBTS www. learnbloodtransfusion. org. uk
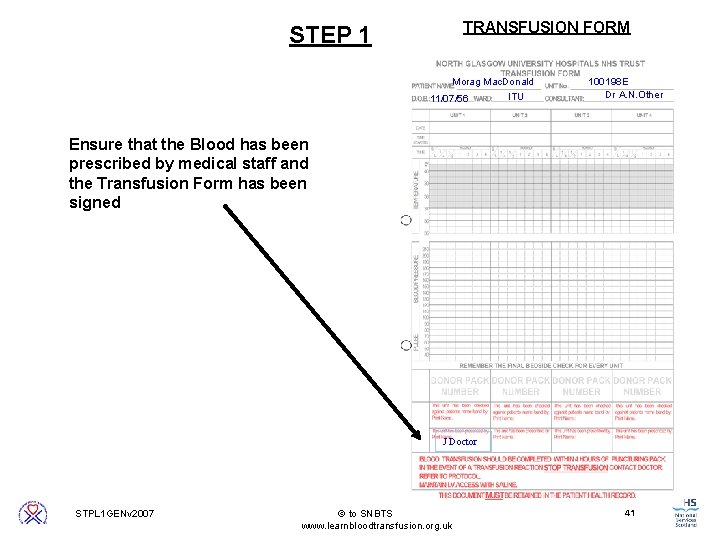
STEP 1 TRANSFUSION FORM Morag Mac. Donald 11/07/56 ITU 100198 E Dr A. N. Other Ensure that the Blood has been prescribed by medical staff and the Transfusion Form has been signed J Doctor 41 STPL 1 GENv 2007 to SNBTS www. learnbloodtransfusion. org. uk
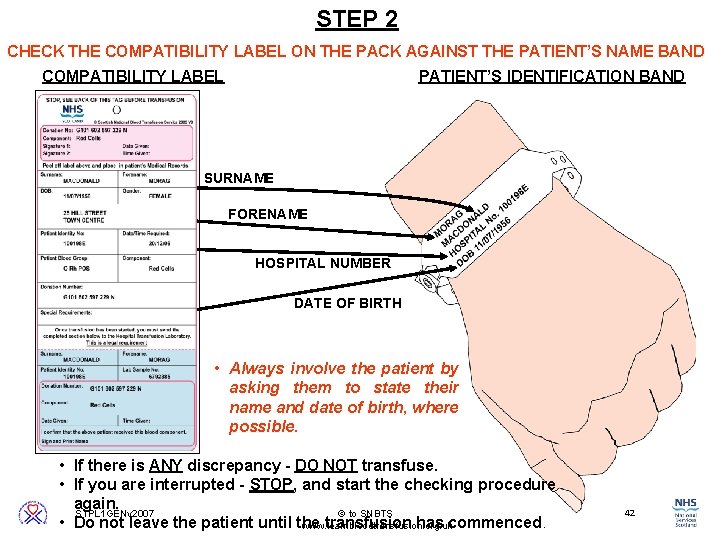
STEP 2 CHECK THE COMPATIBILITY LABEL ON THE PACK AGAINST THE PATIENT’S NAME BAND COMPATIBILITY LABEL PATIENT’S IDENTIFICATION BAND G 101 602 597 229 N MACDONALD SURNAME FORENAME MORAG 100198 E 25 HILL STREET TOWN CENTRE DATE OF BIRTH 11/07/1956 O POS HOSPITAL NUMBER ITU 1 2 • Always involve the patient by asking them to state their name and date of birth, where possible. • If there is ANY discrepancy - DO NOT transfuse. • If you are interrupted - STOP, and start the checking procedure again. 42 STPL 1 GENv 2007 to SNBTS • Do not leave the patient until the transfusion has commenced. www. learnbloodtransfusion. org. uk
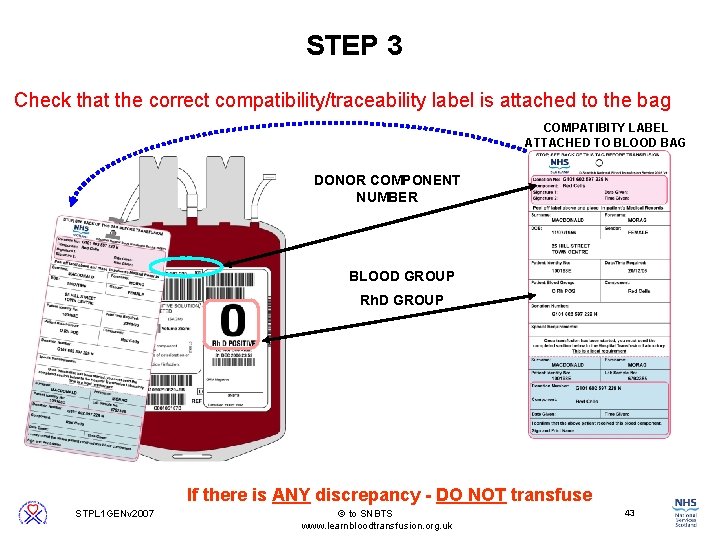
STEP 3 Check that the correct compatibility/traceability label is attached to the bag COMPATIBITY LABEL ATTACHED TO BLOOD BAG DONOR COMPONENT NUMBER BLOOD GROUP Rh. D GROUP If there is ANY discrepancy - DO NOT transfuse 43 STPL 1 GENv 2007 to SNBTS www. learnbloodtransfusion. org. uk
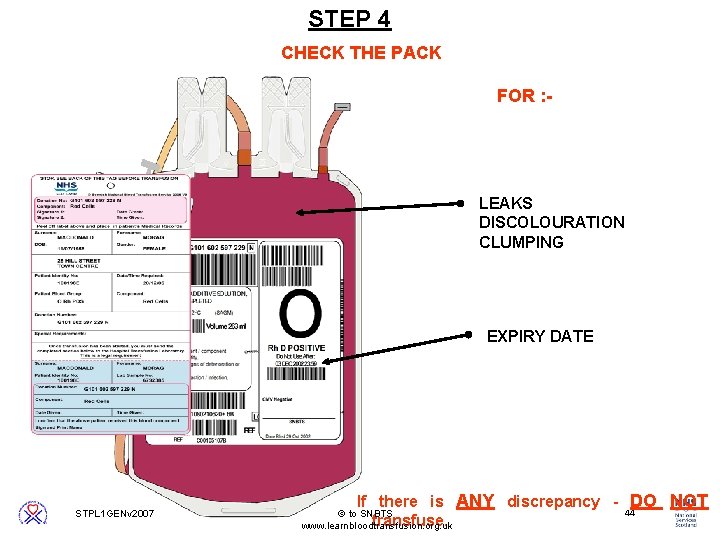
STEP 4 CHECK THE PACK FOR : - LEAKS DISCOLOURATION CLUMPING EXPIRY DATE If there is ANY discrepancy - DO NOT transfuse. 44 STPL 1 GENv 2007 to SNBTS www. learnbloodtransfusion. org. uk

STEP 1 STEP 2 STEP 3 STEP 4 COMMENCE THE TRANSFUSION ! 45 STPL 1 GENv 2007 to SNBTS www. learnbloodtransfusion. org. uk
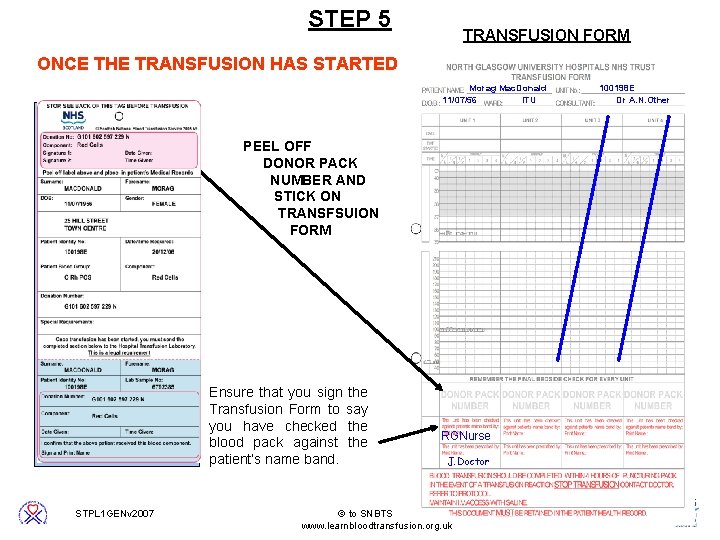
STEP 5 TRANSFUSION FORM ONCE THE TRANSFUSION HAS STARTED Morag Mac. Donald 11/07/56 ITU G 101 602 597 229 N MACDONALD MORAG 100198 E Dr A. N. Other PEEL OFF DONOR PACK NUMBER AND STICK ON TRANSFSUION FORM 100198 E 25 HILL STREET TOWN CENTRE 11/07/1956 O POS ITU 1 2 Ensure that you sign the Transfusion Form to say you have checked the blood pack against the patient’s name band. RGNurse J. Doctor 46 STPL 1 GENv 2007 to SNBTS www. learnbloodtransfusion. org. uk
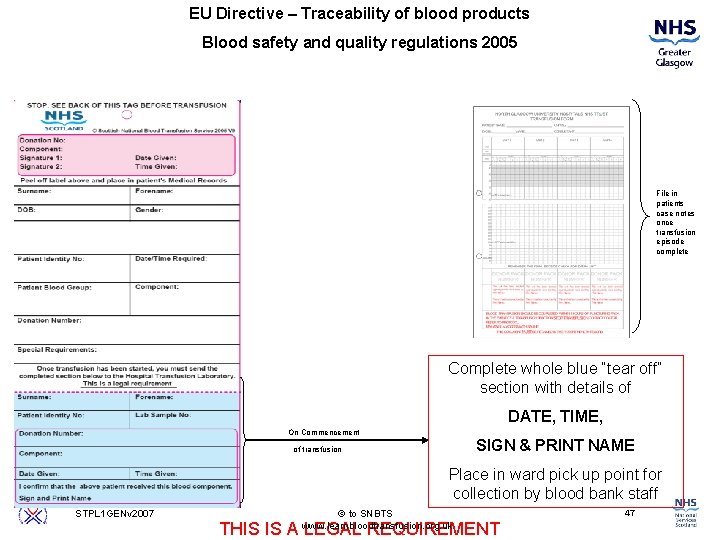
EU Directive – Traceability of blood products Blood safety and quality regulations 2005 File in patients case notes once transfusion episode complete Complete whole blue “tear off” section with details of DATE, TIME, On Commencement of transfusion SIGN & PRINT NAME Place in ward pick up point for collection by blood bank staff 47 STPL 1 GENv 2007 to SNBTS www. learnbloodtransfusion. org. uk THIS IS A LEGAL REQUIREMENT
- Slides: 47