Better Asthma Care Better Health and Lower Costs
Better Asthma Care, Better Health and Lower Costs – Is it possible? Data, Decision-Making and Improving Outcomes Paul Foreman, Ph. D, MS, MA University of Missouri, School of Medicine Project Director, Asthma Ready® Communities Child Health, Pulmonary Medicine and Allergy foremanp@health. missouri. edu ® July 11, 2012
Disclosure Dr. Foreman will not discuss off label or experimental use of medications or devices. He has no commercial relationships to disclose. His research and presentations have not been supported by pharmaceutical companies or equipment vendors. ®
just do it. ®
Background Charges to insurers result in rich data sets that can define cost-efficient clinical services, identify high risk children who require special care and support evaluation of educational interventions. This presentation will illustrate the usefulness of Medicaid administrative claims data analysis and will describe emerging asthma applications that use claims data. ®
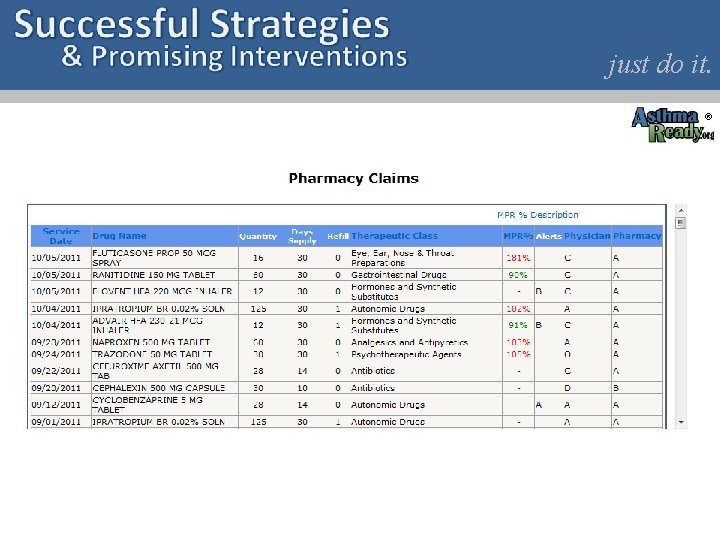
Claims Data Explained Insurers receive bills from health care providers, pharmacies, hospitals, durable medical equipment companies and others who deliver covered products or services to beneficiaries. These charges are collectively called “administrative claims. ” ® March 26, 2012
Electronic Access to Claims Insurers are beginning to provide electronic access to claims records to allow clinicians and others to more accurately assess adherence, risk and control. Clinical histories and interview data often DO NOT agree with claims data. Asthma care is best guided by evaluating claims data along side other data sources. ® March 26, 2012
just do it. ®
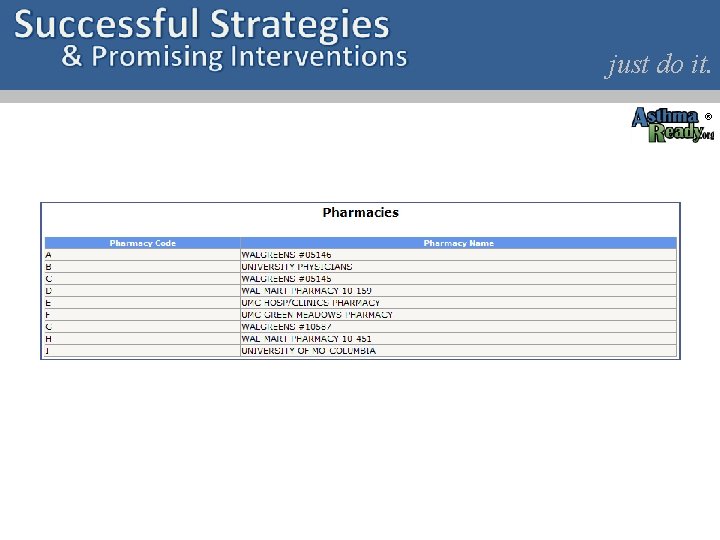
just do it. ®
just do it. ®
Medication Related Problems Analysis of claims data is being used to identify 17 asthma management and medication-related problems by Missouri Medicaid. These problems are automatically detected by a logic engine and the pharmacist is notified at the time of dispensing a medication that a problem exists. ® March 26, 2012
Medication Related Problems (2) The pharmacist is given the option of accepting an encounter to address the problem. An assessment and counseling guide is provided to structure the encounter and pharmacist’s documentation. If completed within 90 days the pharmacist is reimbursed (99605, 6, 7) in 15 minute increments up to one hour a month for medication therapy management. ® March 26, 2012
Medication Related Problems (3) Examples of MRPs include: 1) low rate of ICS refills 2) albuterol dispensed > 3 times in 6 months 3) No spirometry in 3 years 4) Recent ER visit for asthma 5) >one oral steroid burst in 12 months http: //mediasuite. multicastmedia. com/player. php? v=al 80 y 67 g ® March 26, 2012
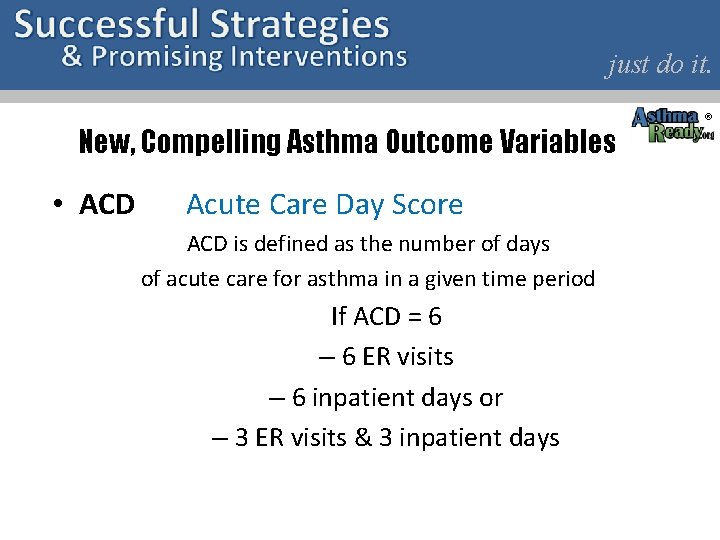
just do it. New, Compelling Asthma Outcome Variables • ACD Acute Care Day Score ACD is defined as the number of days of acute care for asthma in a given time period If ACD = 6 – 6 ER visits – 6 inpatient days or – 3 ER visits & 3 inpatient days ®
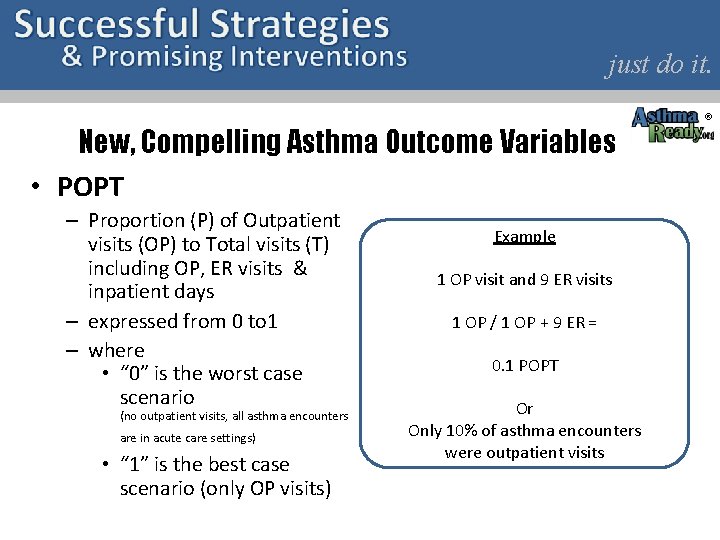
just do it. New, Compelling Asthma Outcome Variables • POPT – Proportion (P) of Outpatient visits (OP) to Total visits (T) including OP, ER visits & inpatient days – expressed from 0 to 1 – where • “ 0” is the worst case scenario (no outpatient visits, all asthma encounters are in acute care settings) • “ 1” is the best case scenario (only OP visits) Example 1 OP visit and 9 ER visits 1 OP / 1 OP + 9 ER = 0. 1 POPT Or Only 10% of asthma encounters were outpatient visits ®
just do it. New, Compelling Asthma Outcome Variables • DPR Daily Possession Rate • Average daily amount of drug (i. e. , inhaled corticosteroids) available over a dispensing interval • Charting ACD, POPT & DPR to model opportunities for family member, PCP and school nurse messaging • These claims data are available within one month of event for timely actions ®
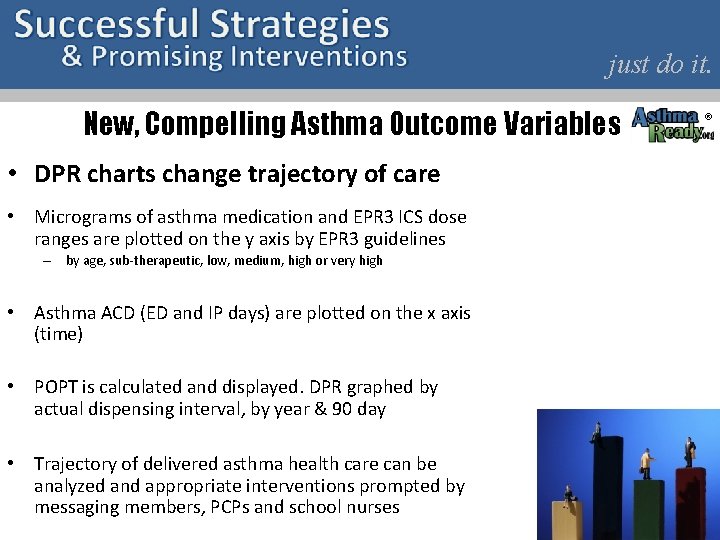
just do it. New, Compelling Asthma Outcome Variables • DPR charts change trajectory of care • Micrograms of asthma medication and EPR 3 ICS dose ranges are plotted on the y axis by EPR 3 guidelines – by age, sub-therapeutic, low, medium, high or very high • Asthma ACD (ED and IP days) are plotted on the x axis (time) • POPT is calculated and displayed. DPR graphed by actual dispensing interval, by year & 90 day • Trajectory of delivered asthma health care can be analyzed and appropriate interventions prompted by messaging members, PCPs and school nurses ®
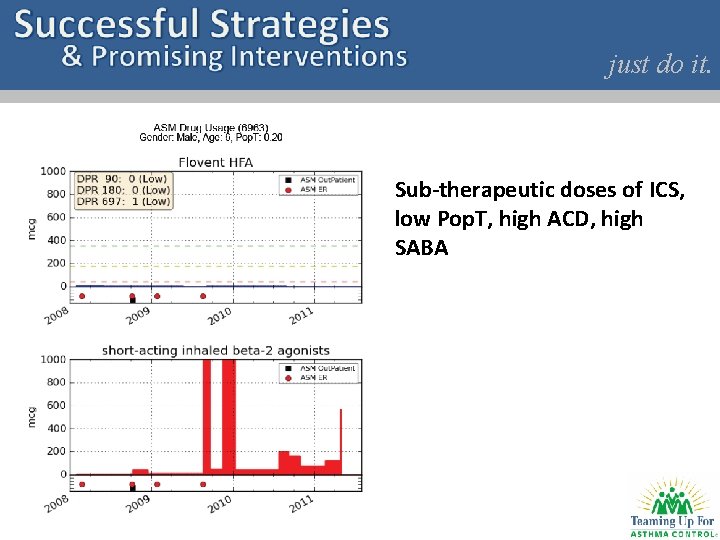
just do it. Sub-therapeutic doses of ICS, low Pop. T, high ACD, high SABA
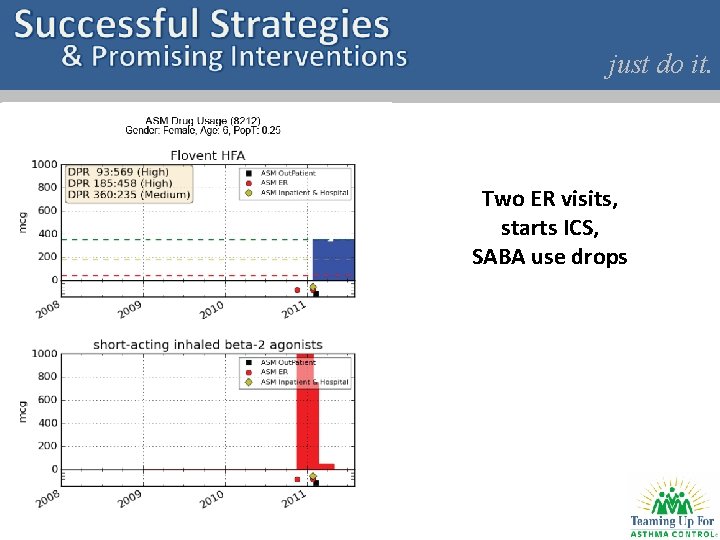
just do it. Two ER visits, starts ICS, SABA use drops
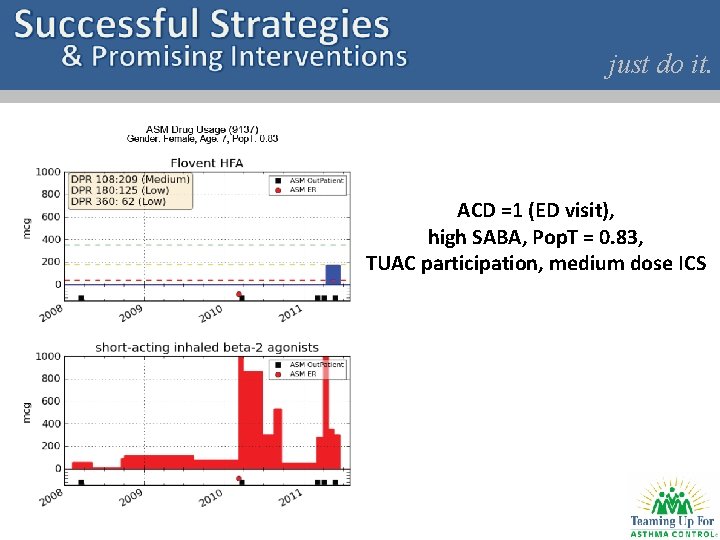
just do it. ACD =1 (ED visit), high SABA, Pop. T = 0. 83, TUAC participation, medium dose ICS
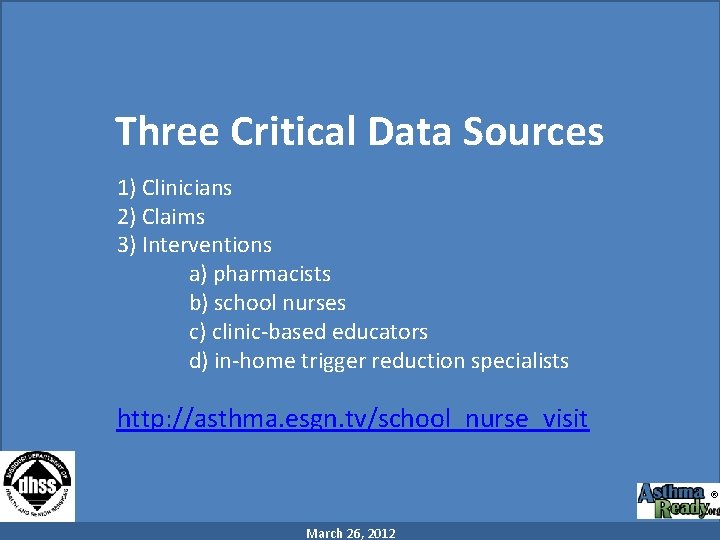
Three Critical Data Sources 1) Clinicians 2) Claims 3) Interventions a) pharmacists b) school nurses c) clinic-based educators d) in-home trigger reduction specialists http: //asthma. esgn. tv/school_nurse_visit ® March 26, 2012
Educator Assessment (ACE©) 1) Custom assessment scan form 2) Before and after playing the ACE© DVD 3) Incorporates CARAT (Childhood Asthma Risk Assessment Tool) 4) For “very poorly controlled asthma” ® March 26, 2012
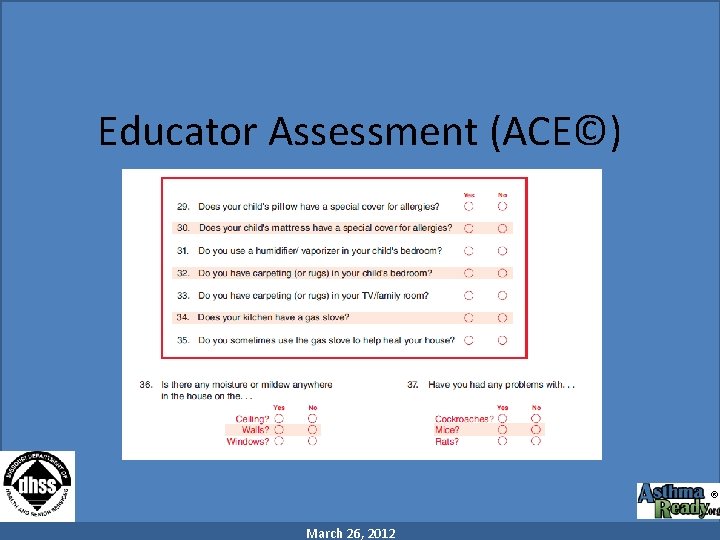
Educator Assessment (ACE©) ® March 26, 2012
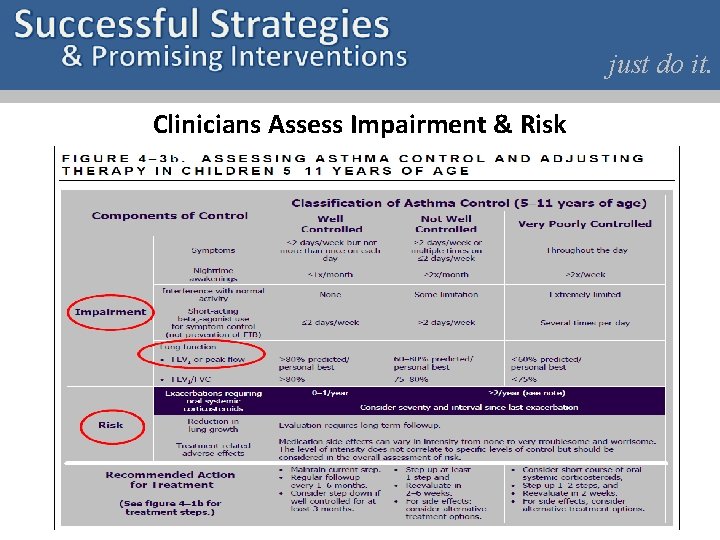
just do it. Clinicians Assess Impairment & Risk
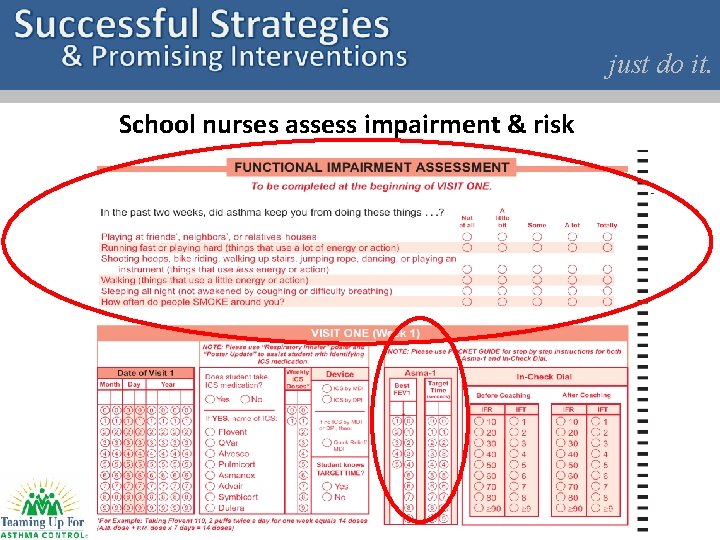
just do it. School nurses assess impairment & risk
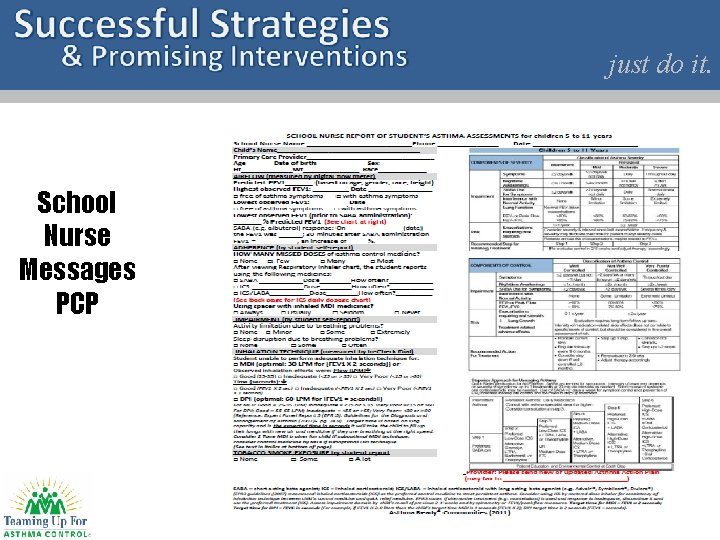
just do it. School Nurse Messages PCP
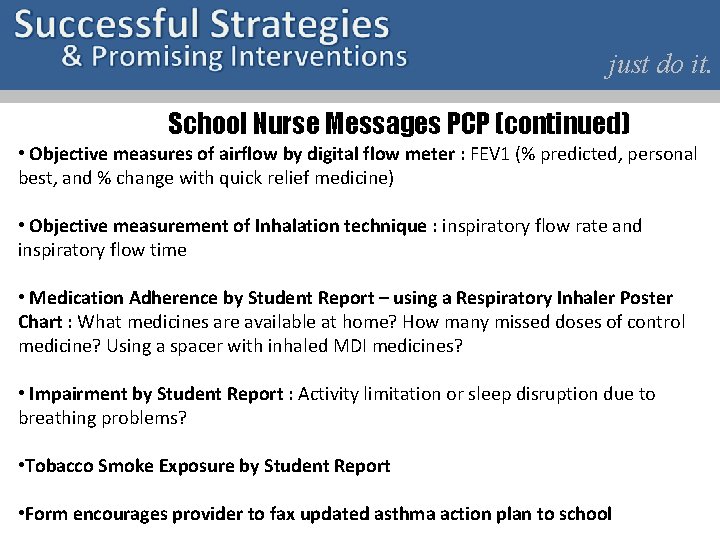
just do it. School Nurse Messages PCP (continued) • Objective measures of airflow by digital flow meter : FEV 1 (% predicted, personal best, and % change with quick relief medicine) • Objective measurement of Inhalation technique : inspiratory flow rate and inspiratory flow time • Medication Adherence by Student Report – using a Respiratory Inhaler Poster Chart : What medicines are available at home? How many missed doses of control medicine? Using a spacer with inhaled MDI medicines? • Impairment by Student Report : Activity limitation or sleep disruption due to breathing problems? • Tobacco Smoke Exposure by Student Report • Form encourages provider to fax updated asthma action plan to school
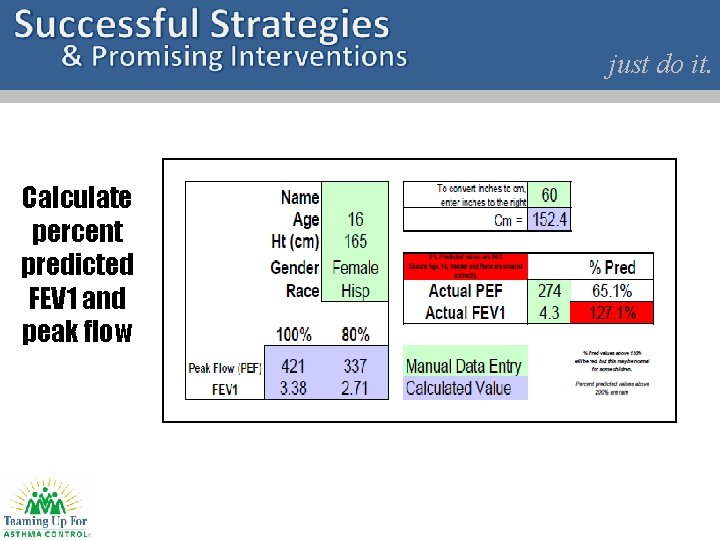
just do it. Calculate percent predicted FEV 1 and peak flow
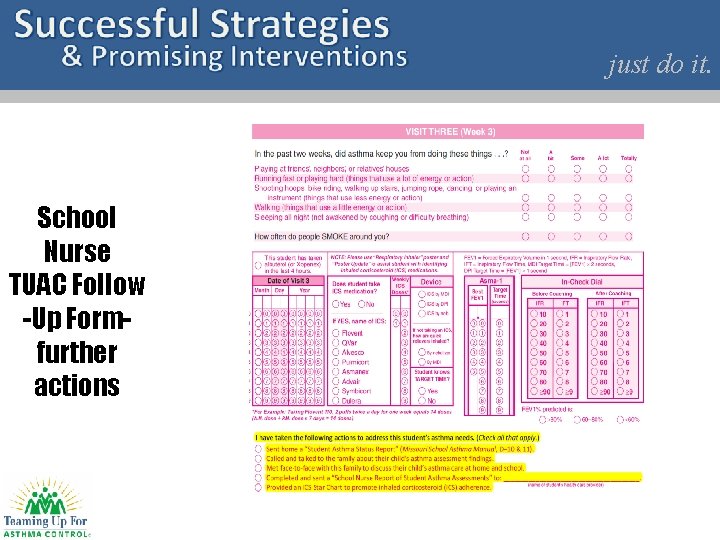
just do it. School Nurse TUAC Follow -Up Formfurther actions
just do it. School Nurse Actions – Levels of Communication • Send home a Student Asthma Status Report Form: Inform family of asthma events at school – includes subjective and objective measures, encourage communication/follow up with provider • Called and talked to the family about their child’s asthma assessment findings • Met face-to-face with this family to discuss their child’s asthma care at home and school • Completed and sent a “School Nurse Report of Student Asthma Assessments” to (name of health care provider) • Provided an ICS Star Chart to promote inhaled corticosteroid (ICS) adherence
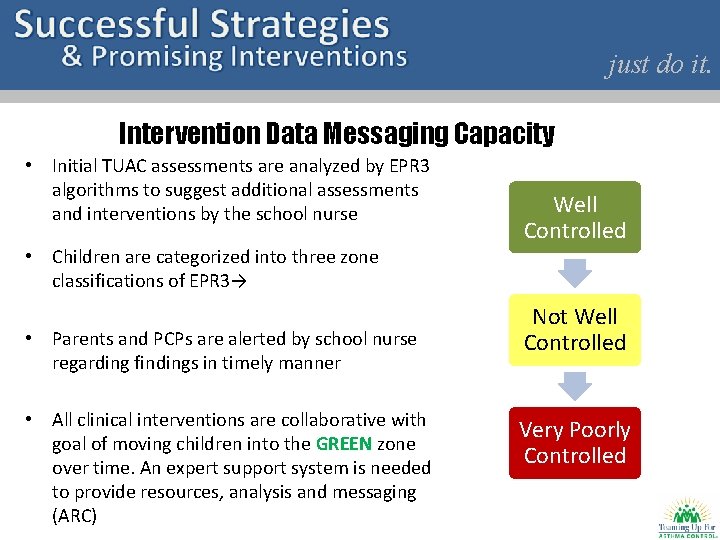
just do it. Intervention Data Messaging Capacity • Initial TUAC assessments are analyzed by EPR 3 algorithms to suggest additional assessments and interventions by the school nurse Well Controlled • Children are categorized into three zone classifications of EPR 3→ • Parents and PCPs are alerted by school nurse regarding findings in timely manner • All clinical interventions are collaborative with goal of moving children into the GREEN zone over time. An expert support system is needed to provide resources, analysis and messaging (ARC) Not Well Controlled Very Poorly Controlled
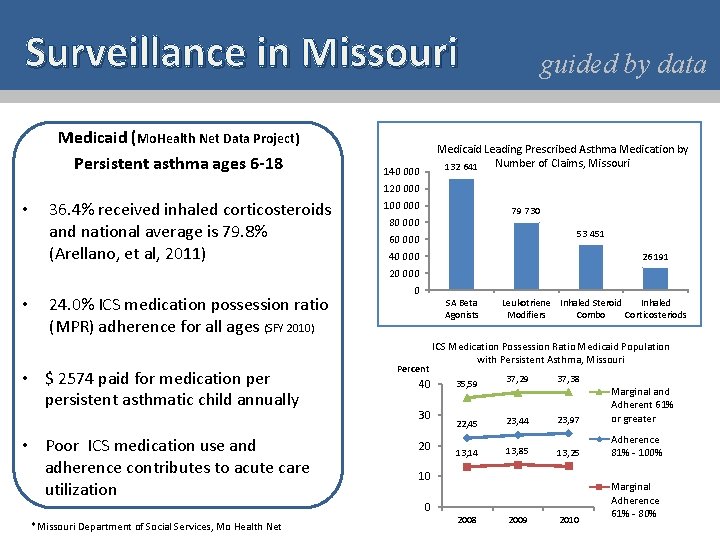
Surveillance in Missouri Medicaid (Mo. Health Net Data Project) Persistent asthma ages 6 -18 guided by data Medicaid Leading Prescribed Asthma Medication by Number of Claims, Missouri 132 641 140 000 120 000 • 36. 4% received inhaled corticosteroids and national average is 79. 8% (Arellano, et al, 2011) 100 000 79 730 80 000 53 451 60 000 40 000 26 191 20 000 • 24. 0% ICS medication possession ratio (MPR) adherence for all ages (SFY 2010) • $ 2574 paid for medication persistent asthmatic child annually • Poor ICS medication use and adherence contributes to acute care utilization 0 SA Beta Agonists Percent 40 30 20 ICS Medication Possession Ratio Medicaid Population with Persistent Asthma, Missouri 35, 59 37, 29 37, 38 22, 45 23, 44 23, 97 Marginal and Adherent 61% or greater 13, 14 13, 85 13, 25 Adherence 81% - 100% 10 0 *Missouri Department of Social Services, Mo Health Net Leukotriene Inhaled Steroid Inhaled Modifiers Combo Corticosteriods 2008 2009 2010 Marginal Adherence 61% - 80%
just do it. Changing Cost Outcomes for Missouri Children with Asthma: MO Health Net Data Project Collaboration • Per member per month (PMPM) costs for children ages 5 -18 identified with persistent asthma was $1, 497 for 6, 577 participants in 2010. • Per member per month costs for children ages 5 -18 was $1044 for 134 patients of an EPR 3 -compliant practice in 2010. • EPR 3 -treated group costs were 9. 6% higher for ICS medication costs and 17% higher costs for treating co-morbid conditions when compared to population mean. • However the total asthma direct costs were 4. 7% lower for EPR 3 treated group. • Remarkably, total asthma medication costs were 33% lower and total cost of care was 30% lower for the EPR 3 -treated patient group.
just do it. IMPACT Asthma Kids© Care Background • Asthma Ready® Clinics and Medical Homes - clinic staff including physicians, nurse practitioners, nurses, receptionists/billing clerks and respiratory therapists receive asthma standardized medical management curricula, equipment & protocols (EPR 3 compliant care) • Asthma Ready® Schools - School nurses trained, standardized curricula - School assessments and interventions are based on EPR 3 guidelines - Actionable data are documented and sent to the parents and PCP (should be in real time) ®
just do it. IMPACT Asthma Kids© Care Background • Medical Homes and Asthma Ready® Clinics (ARC) -Comprehensive care in the context of individual, cultural, and community needs: ARC address individual patient and family goals each clinic visit and refers to community partners for continuity of care -Emphasize education through system-level protocols and interpersonal interactions: Asthma Ready Educator uses standardized asthma literacy education tools for patients and families and validated assessment protocols for transmitting actionable data -At the center of the Medical/Health Home are the patient and family and their relationship with the primary care team Asthma Ready care is delivered by a team, composed of a clinic provider and a nurse trained as an asthma educator ®
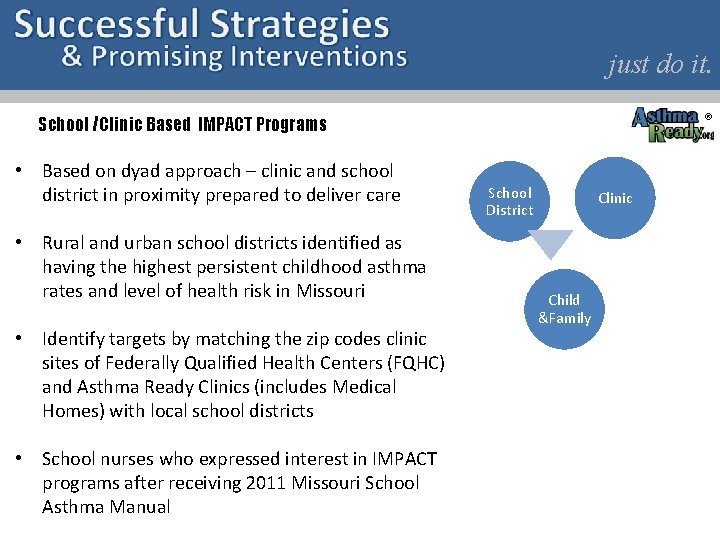
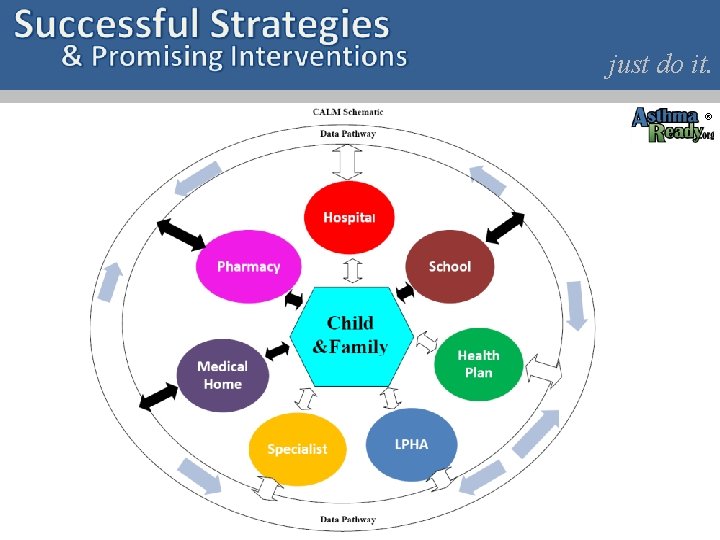
just do it. ® School /Clinic Based IMPACT Programs • Based on dyad approach – clinic and school district in proximity prepared to deliver care • Rural and urban school districts identified as having the highest persistent childhood asthma rates and level of health risk in Missouri • Identify targets by matching the zip codes clinic sites of Federally Qualified Health Centers (FQHC) and Asthma Ready Clinics (includes Medical Homes) with local school districts • School nurses who expressed interest in IMPACT programs after receiving 2011 Missouri School Asthma Manual School District Clinic Child &Family
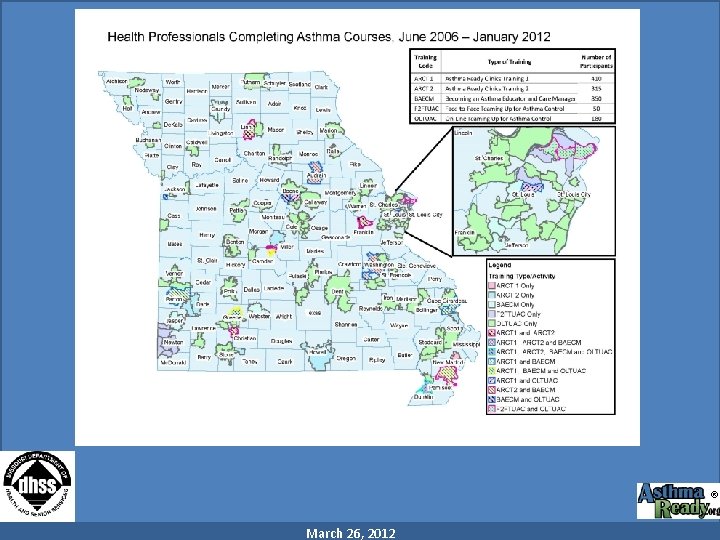
® March 26, 2012
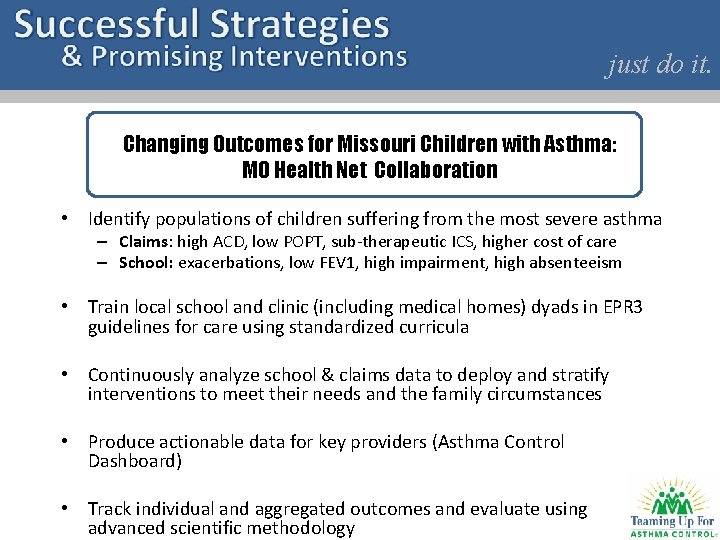
just do it. Changing Outcomes for Missouri Children with Asthma: MO Health Net Collaboration • Identify populations of children suffering from the most severe asthma – Claims: high ACD, low POPT, sub-therapeutic ICS, higher cost of care – School: exacerbations, low FEV 1, high impairment, high absenteeism • Train local school and clinic (including medical homes) dyads in EPR 3 guidelines for care using standardized curricula • Continuously analyze school & claims data to deploy and stratify interventions to meet their needs and the family circumstances • Produce actionable data for key providers (Asthma Control Dashboard) • Track individual and aggregated outcomes and evaluate using advanced scientific methodology
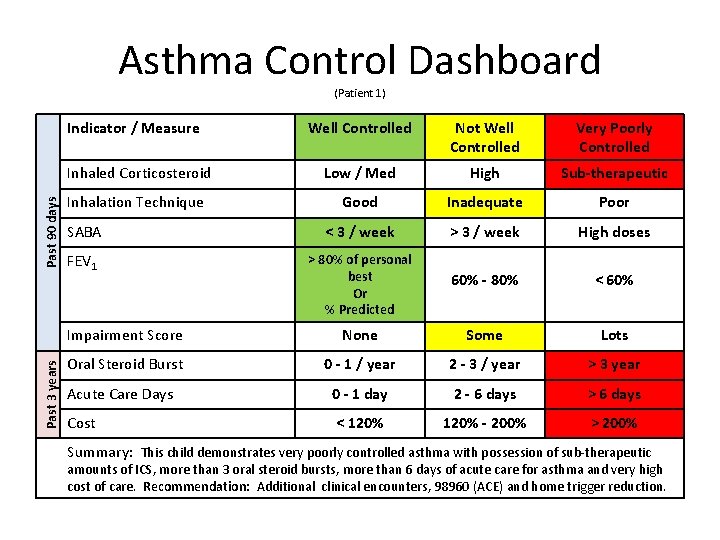
Asthma Control Dashboard (Patient 1) Past 3 years Past 90 days Indicator / Measure Well Controlled Not Well Controlled Very Poorly Controlled Inhaled Corticosteroid Low / Med High Sub-therapeutic Inhalation Technique Good Inadequate Poor SABA < 3 / week > 3 / week High doses FEV 1 > 80% of personal best Or % Predicted 60% - 80% < 60% Impairment Score None Some Lots Oral Steroid Burst 0 - 1 / year 2 - 3 / year > 3 year Acute Care Days 0 - 1 day 2 - 6 days > 6 days Cost < 120% - 200% > 200% Summary: This child demonstrates very poorly controlled asthma with possession of sub-therapeutic amounts of ICS, more than 3 oral steroid bursts, more than 6 days of acute care for asthma and very high cost of care. Recommendation: Additional clinical encounters, 98960 (ACE) and home trigger reduction.
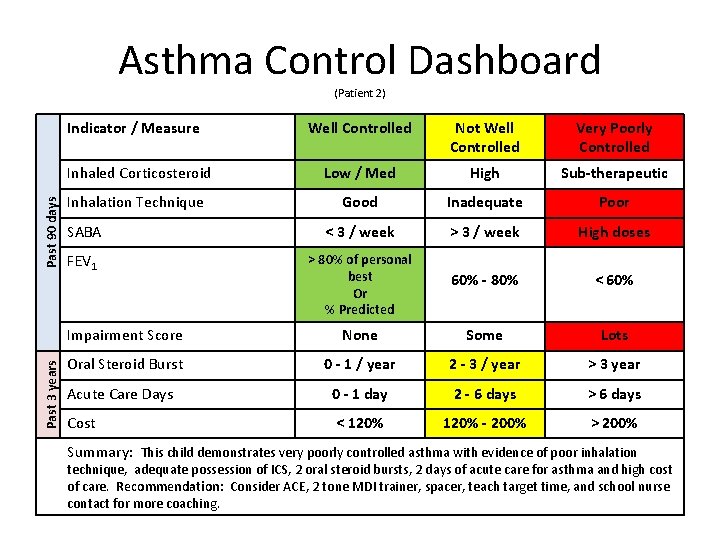
Asthma Control Dashboard (Patient 2) Past 3 years Past 90 days Indicator / Measure Well Controlled Not Well Controlled Very Poorly Controlled Inhaled Corticosteroid Low / Med High Sub-therapeutic Inhalation Technique Good Inadequate Poor SABA < 3 / week > 3 / week High doses FEV 1 > 80% of personal best Or % Predicted 60% - 80% < 60% Impairment Score None Some Lots Oral Steroid Burst 0 - 1 / year 2 - 3 / year > 3 year Acute Care Days 0 - 1 day 2 - 6 days > 6 days Cost < 120% - 200% > 200% Summary: This child demonstrates very poorly controlled asthma with evidence of poor inhalation technique, adequate possession of ICS, 2 oral steroid bursts, 2 days of acute care for asthma and high cost of care. Recommendation: Consider ACE, 2 tone MDI trainer, spacer, teach target time, and school nurse contact for more coaching.
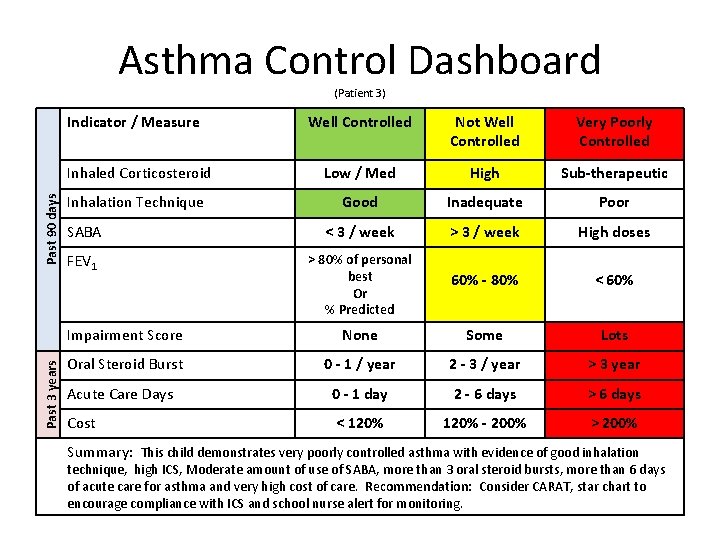
Asthma Control Dashboard (Patient 3) Past 3 years Past 90 days Indicator / Measure Well Controlled Not Well Controlled Very Poorly Controlled Inhaled Corticosteroid Low / Med High Sub-therapeutic Inhalation Technique Good Inadequate Poor SABA < 3 / week > 3 / week High doses FEV 1 > 80% of personal best Or % Predicted 60% - 80% < 60% Impairment Score None Some Lots Oral Steroid Burst 0 - 1 / year 2 - 3 / year > 3 year Acute Care Days 0 - 1 day 2 - 6 days > 6 days Cost < 120% - 200% > 200% Summary: This child demonstrates very poorly controlled asthma with evidence of good inhalation technique, high ICS, Moderate amount of use of SABA, more than 3 oral steroid bursts, more than 6 days of acute care for asthma and very high cost of care. Recommendation: Consider CARAT, star chart to encourage compliance with ICS and school nurse alert for monitoring.
® just do it.
just do it. Students Receiving Award for Finishing Asthma Education Benjamin Francisco, Ph. D, PNP, AE-C Asthma Ready®, University of Missouri
- Slides: 42