Best Practices in Sepsis The Nebraska Sepsis Toolkit
Best Practices in Sepsis & The Nebraska Sepsis Toolkit A Panel Discussion www. nebraskahospitals. org
Panelists: • Dr. Amy Vertin, ED Medical Director & Physician Leader – Bryan Health • Anne Timmerman, Director of Quality & Safety – Franciscan Healthcare • Andrew Mc. Carty, Stroke & Sepsis Program Coordinator – Mary Lanning Healthcare • Jenni Meiergerd, Infection Control, Employee Health, Safety Coordinator – Franciscan Healthcare • Kevin Sponsel, Infectious Disease / Antimicrobial Stewardship Clinical Pharmacist Specialist – Bryan Health • Denise Moeschen, Clinical Quality Specialist – Bryan Health 2
Learning Objectives: • Define sepsis and recognize signs / symptoms of sepsis. • Compare sepsis screening tools. • Discuss and review sepsis bundles and Evidence. Based sepsis care. • Relate best practices to sepsis care in rural healthcare. • Describe best practices for patients transferred to a tertiary care center. 3

Question #1 What are the newest / approved sepsis definitions? www. nebraskahospitals. org
Sepsis Definitions: • Sepsis • Severe Sepsis • Septic Shock 5
Question #2 Describe the best sepsis screening tools / processes and how do those tools fit into daily patient care? www. nebraskahospitals. org
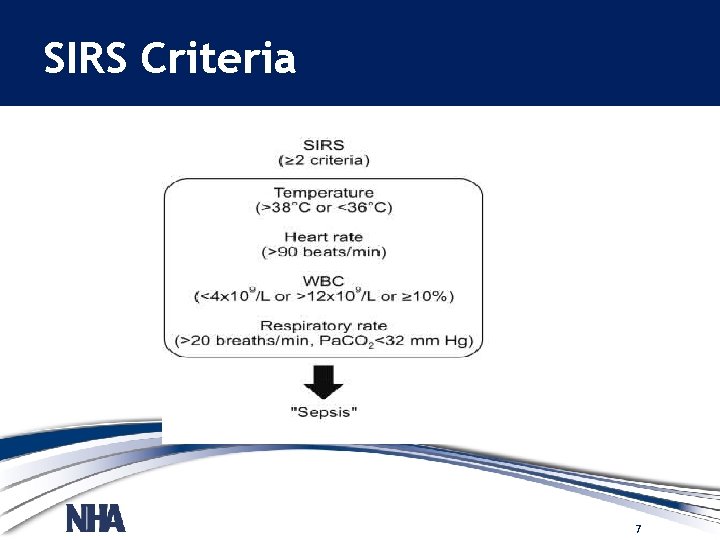
SIRS Criteria 7

q. SOFA 8
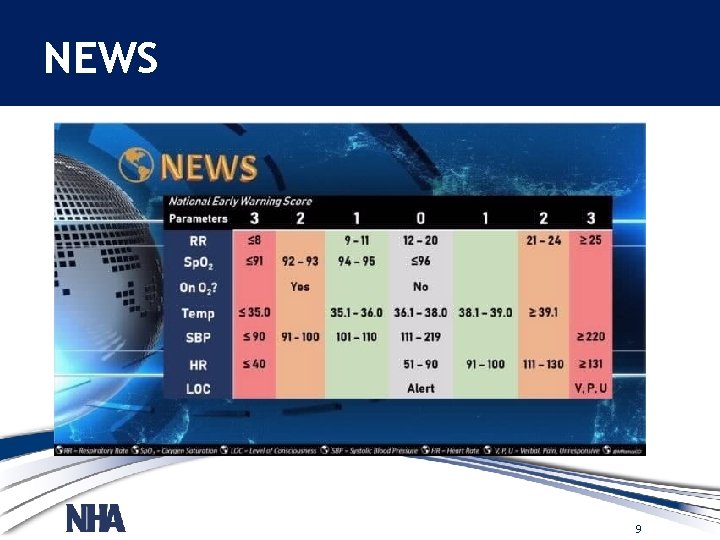
NEWS 9
Other Screening Considerations: 10
Question #3 What are the most current CMS Bundle Requirements and how have those changed over the past 12 -months? www. nebraskahospitals. org
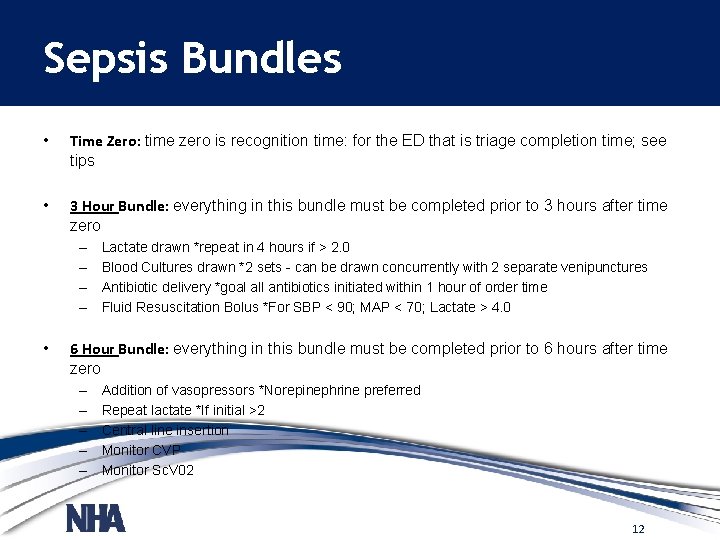
Sepsis Bundles • Time Zero: time zero is recognition time: for the ED that is triage completion time; see tips • 3 Hour Bundle: everything in this bundle must be completed prior to 3 hours after time zero – – • Lactate drawn *repeat in 4 hours if > 2. 0 Blood Cultures drawn *2 sets - can be drawn concurrently with 2 separate venipunctures Antibiotic delivery *goal all antibiotics initiated within 1 hour of order time Fluid Resuscitation Bolus *For SBP < 90; MAP < 70; Lactate > 4. 0 6 Hour Bundle: everything in this bundle must be completed prior to 6 hours after time zero – – – Addition of vasopressors *Norepinephrine preferred Repeat lactate *If initial >2 Central line insertion Monitor CVP Monitor Sc. V 02 12
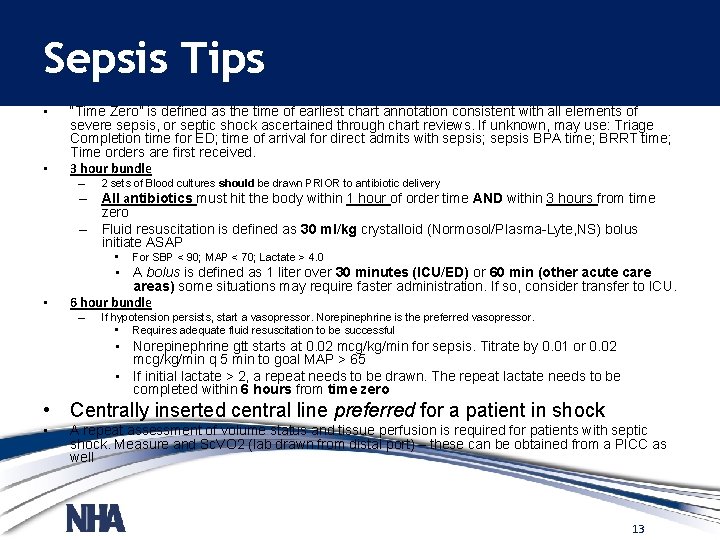
Sepsis Tips • • “Time Zero” is defined as the time of earliest chart annotation consistent with all elements of severe sepsis, or septic shock ascertained through chart reviews. If unknown, may use: Triage Completion time for ED; time of arrival for direct admits with sepsis; sepsis BPA time; BRRT time; Time orders are first received. 3 hour bundle – 2 sets of Blood cultures should be drawn PRIOR to antibiotic delivery – All antibiotics must hit the body within 1 hour of order time AND within 3 hours from time zero – Fluid resuscitation is defined as 30 ml/kg crystalloid (Normosol/Plasma-Lyte, NS) bolus initiate ASAP • • For SBP < 90; MAP < 70; Lactate > 4. 0 • A bolus is defined as 1 liter over 30 minutes (ICU/ED) or 60 min (other acute care areas) some situations may require faster administration. If so, consider transfer to ICU. 6 hour bundle – If hypotension persists, start a vasopressor. Norepinephrine is the preferred vasopressor. • Requires adequate fluid resuscitation to be successful • Norepinephrine gtt starts at 0. 02 mcg/kg/min for sepsis. Titrate by 0. 01 or 0. 02 mcg/kg/min q 5 min to goal MAP > 65 • If initial lactate > 2, a repeat needs to be drawn. The repeat lactate needs to be completed within 6 hours from time zero • Centrally inserted central line preferred for a patient in shock • A repeat assessment of volume status and tissue perfusion is required for patients with septic shock. Measure and Sc. VO 2 (lab drawn from distal port) – these can be obtained from a PICC as well 13
Question #4 What does a sepsis alert look like in use on your units? www. nebraskahospitals. org
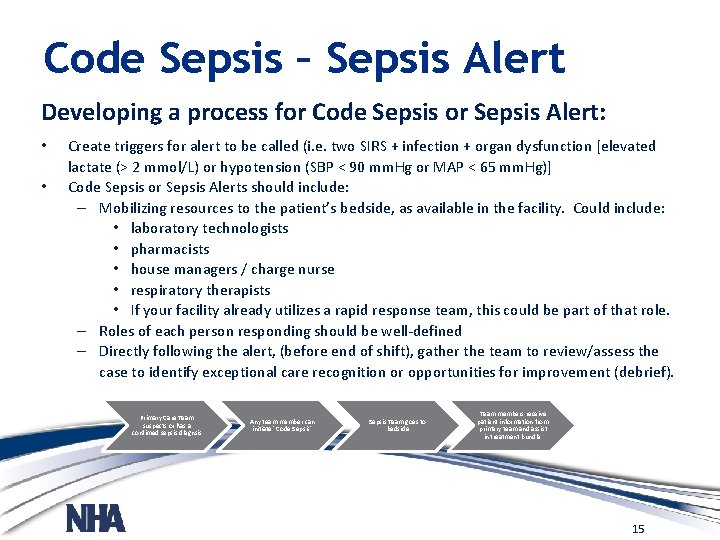
Code Sepsis – Sepsis Alert Developing a process for Code Sepsis or Sepsis Alert: • • Create triggers for alert to be called (i. e. two SIRS + infection + organ dysfunction [elevated lactate (> 2 mmol/L) or hypotension (SBP < 90 mm. Hg or MAP < 65 mm. Hg)] Code Sepsis or Sepsis Alerts should include: – Mobilizing resources to the patient’s bedside, as available in the facility. Could include: • laboratory technologists • pharmacists • house managers / charge nurse • respiratory therapists • If your facility already utilizes a rapid response team, this could be part of that role. – Roles of each person responding should be well-defined – Directly following the alert, (before end of shift), gather the team to review/assess the case to identify exceptional care recognition or opportunities for improvement (debrief). Primary Care Team suspects or has a confimed sepsis diagnsis Any team member can initiate "Code Sepsis" Sepsis Team goes to bedside Team members receive patient information from primary team and assist in treatment bundle. 15
Question #5 What are the most important keys to caring for a septic or suspected sepsis patient? Specifically in a rural cares setting when resources are more limited? www. nebraskahospitals. org
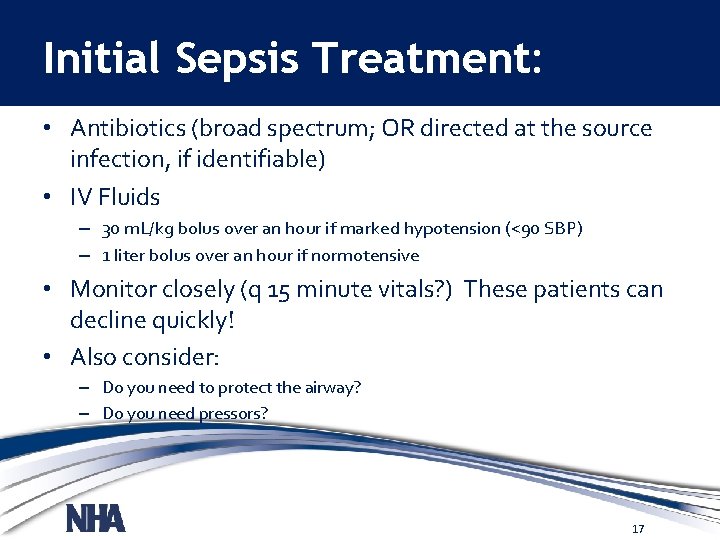
Initial Sepsis Treatment: • Antibiotics (broad spectrum; OR directed at the source infection, if identifiable) • IV Fluids – 30 m. L/kg bolus over an hour if marked hypotension (<90 SBP) – 1 liter bolus over an hour if normotensive • Monitor closely (q 15 minute vitals? ) These patients can decline quickly! • Also consider: – Do you need to protect the airway? – Do you need pressors? 17

Sepsis Algorithm: 18
Question #6 When a rural care team is preparing for the transfer of a sepsis patient, what er the keys to crating the best opportunity for a good outcome? www. nebraskahospitals. org
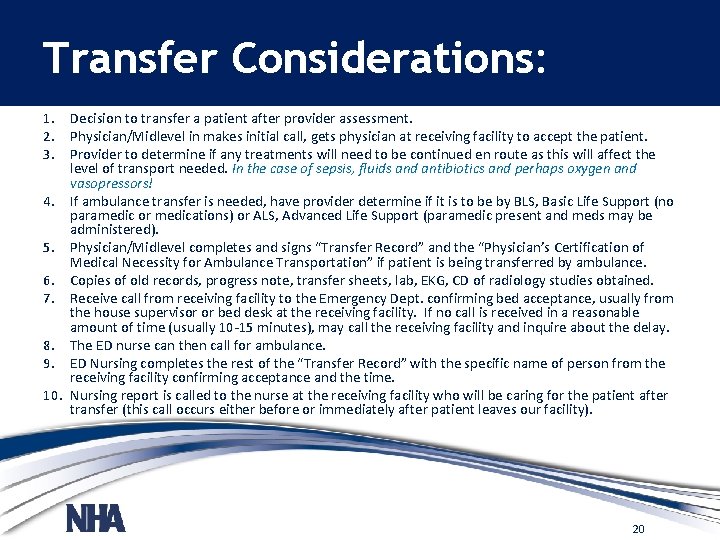
Transfer Considerations: 1. Decision to transfer a patient after provider assessment. 2. Physician/Midlevel in makes initial call, gets physician at receiving facility to accept the patient. 3. Provider to determine if any treatments will need to be continued en route as this will affect the level of transport needed. In the case of sepsis, fluids and antibiotics and perhaps oxygen and vasopressors! 4. If ambulance transfer is needed, have provider determine if it is to be by BLS, Basic Life Support (no paramedic or medications) or ALS, Advanced Life Support (paramedic present and meds may be administered). 5. Physician/Midlevel completes and signs “Transfer Record” and the “Physician’s Certification of Medical Necessity for Ambulance Transportation” if patient is being transferred by ambulance. 6. Copies of old records, progress note, transfer sheets, lab, EKG, CD of radiology studies obtained. 7. Receive call from receiving facility to the Emergency Dept. confirming bed acceptance, usually from the house supervisor or bed desk at the receiving facility. If no call is received in a reasonable amount of time (usually 10 -15 minutes), may call the receiving facility and inquire about the delay. 8. The ED nurse can then call for ambulance. 9. ED Nursing completes the rest of the “Transfer Record” with the specific name of person from the receiving facility confirming acceptance and the time. 10. Nursing report is called to the nurse at the receiving facility who will be caring for the patient after transfer (this call occurs either before or immediately after patient leaves our facility). 20
Question #7 What role does AB stewardship play in sepsis care? How should AB selection process be handled both in rural settings and after transfer to a tertiary care setting? www. nebraskahospitals. org
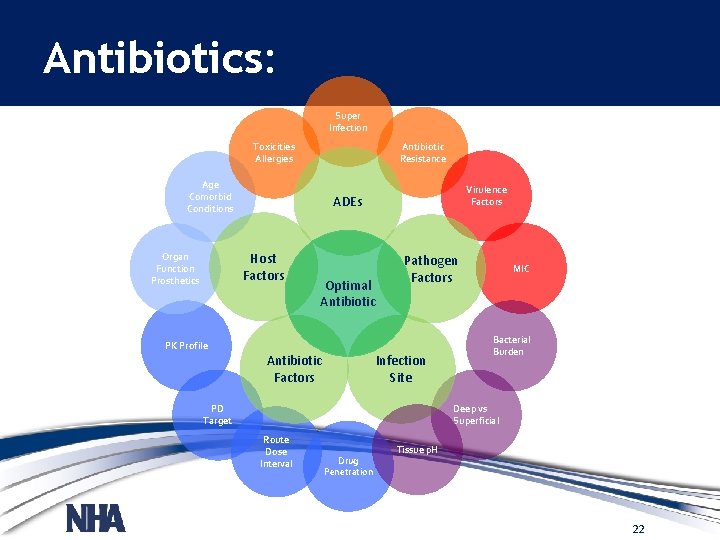
Antibiotics: Super Infection Antibiotic Resistance Toxicities Allergies Age Comorbid Conditions Host Factors Organ Function Prosthetics Virulence Factors ADEs Optimal Antibiotic Pathogen Factors PK Profile Infection Site Antibiotic Factors PD Target MIC Bacterial Burden Deep vs Superficial Route Dose Interval Drug Penetration Tissue p. H 22
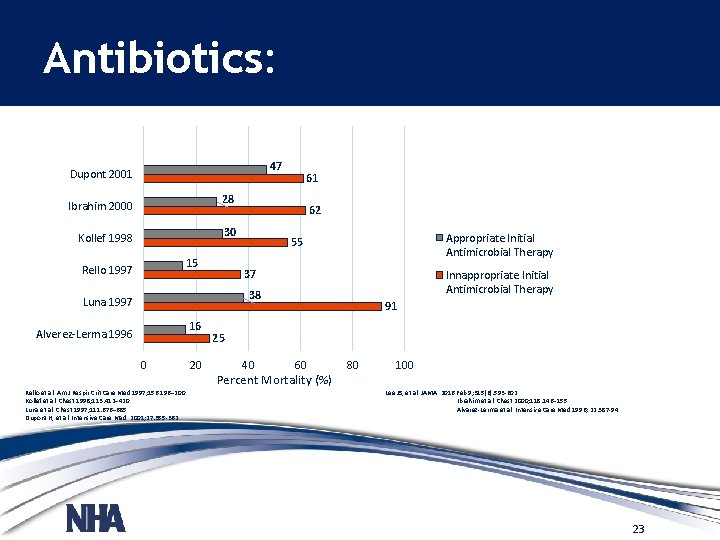
Antibiotics: 47 Dupont 2001 61 28 Ibrahim 2000 62 30 Kollef 1998 15 Rello 1997 Appropriate Initial Antimicrobial Therapy 55 37 Innappropriate Initial Antimicrobial Therapy 38 Luna 1997 16 Alverez-Lerma 1996 0 Rello et al. Am J Respir Crit Care Med 1997; 156: 196– 200. Kollef et al. Chest 1998; 113: 412– 420. Luna et al. Chest 1997; 111: 676– 685. Dupont H, et al. Intensive Care Med. 2001; 27: 355 -362. 20 91 25 40 60 Percent Mortality (%) 80 100 Lee JS, et al. JAMA. 2016 Feb 9; 315(6): 593 -602. Ibrahim et al. Chest 2000; 118: 146– 155. Alvarez-Lerma et al. Intensive Care Med 1996; 22: 387 -94 23
Question #8 Discuss your sepsis team structure and keys to a successful and productive sepsis program / team. www. nebraskahospitals. org
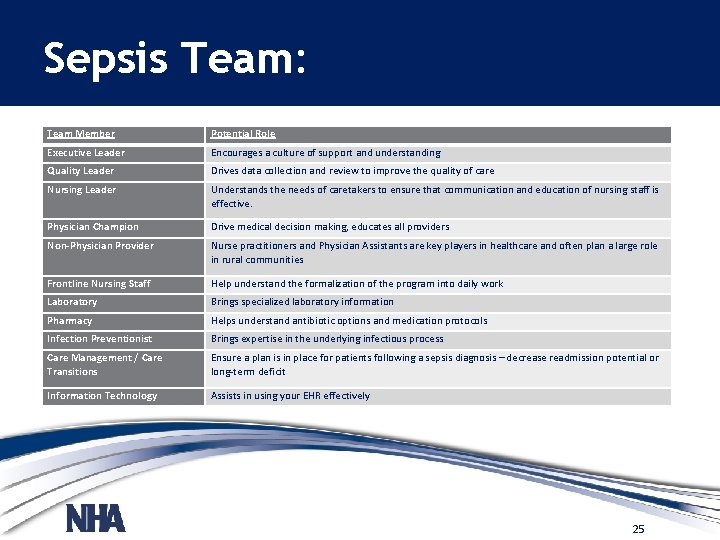
Sepsis Team: Team Member • Executive Leader Potential Role Encourages a culture of support and understanding Quality Leader Drives data collection and review to improve the quality of care Nursing Leader Understands the needs of caretakers to ensure that communication and education of nursing staff is effective. Physician Champion Drive medical decision making, educates all providers Non-Physician Provider Nurse practitioners and Physician Assistants are key players in healthcare and often plan a large role in rural communities Frontline Nursing Staff Help understand the formalization of the program into daily work Laboratory Brings specialized laboratory information Pharmacy Helps understand antibiotic options and medication protocols Infection Preventionist Brings expertise in the underlying infectious process Care Management / Care Transitions Ensure a plan is in place for patients following a sepsis diagnosis – decrease readmission potential or long-term deficit Information Technology Assists in using your EHR effectively 25
Question #9 Discuss some quality improvement metrics / topics / projects related to sepsis and how that can improve care of the sepsis patient. www. nebraskahospitals. org
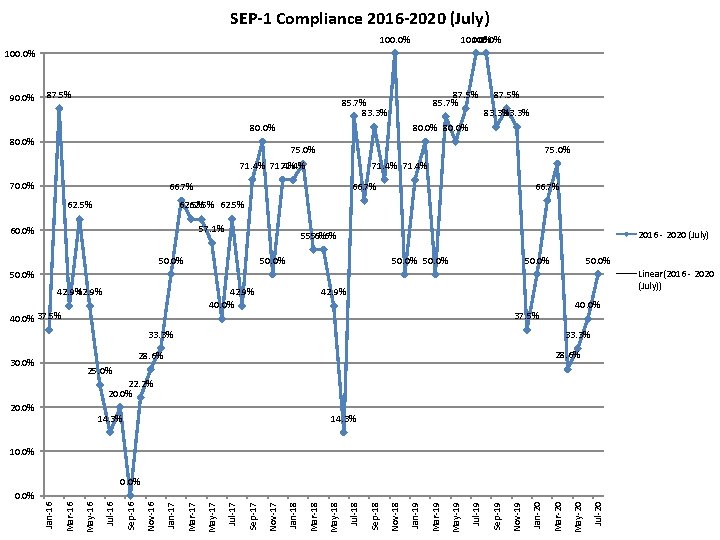
SEP-1 Compliance 2016 -2020 (July) 100. 0% 90. 0% 87. 5% 85. 7% 83. 3% 80. 0% 87. 5% 83. 3% 80. 0% 75. 0% 71. 4% 70. 0% 71. 4% 66. 7% 62. 5% 62. 5% 57. 1% 60. 0% 2016 - 2020 (July) 55. 6% 50. 0% Linear(2016 - 2020 (July)) 50. 0% 42. 9% 40. 0% 37. 5% 42. 9% 40. 0% 37. 5% 33. 3% 28. 6% 30. 0% 25. 0% 22. 2% 20. 0% 14. 3% 10. 0% Jul-20 May-20 Mar-20 Jan-20 Nov-19 Sep-19 Jul-19 May-19 Mar-19 Jan-19 Nov-18 Sep-18 Jul-18 May-18 Mar-18 Jan-18 Nov-17 Sep-17 Jul-17 May-17 Mar-17 Jan-17 Nov-16 Sep-16 Jul-16 May-16 Mar-16 Jan-16 0. 0%
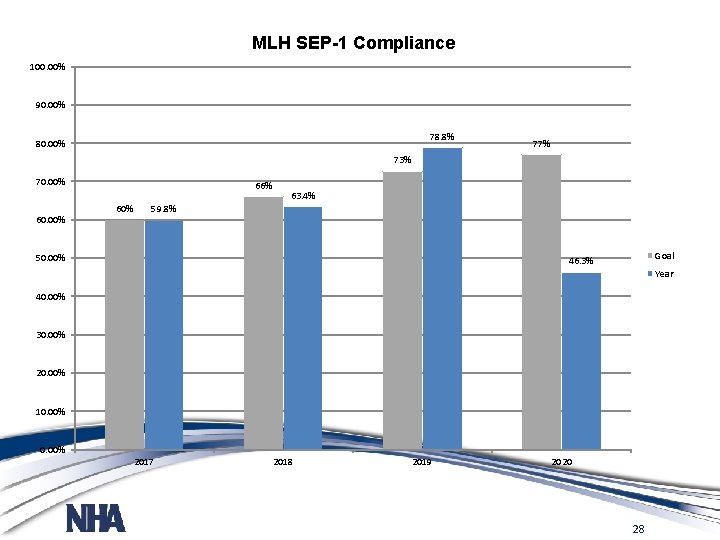
MLH SEP-1 Compliance 100. 00% 90. 00% 78. 8% 80. 00% 77% 73% 70. 00% 66% 60% 63. 4% 59. 8% 50. 00% Goal 46. 3% Year 40. 00% 30. 00% 20. 00% 10. 00% 2017 2018 2019 2020 28
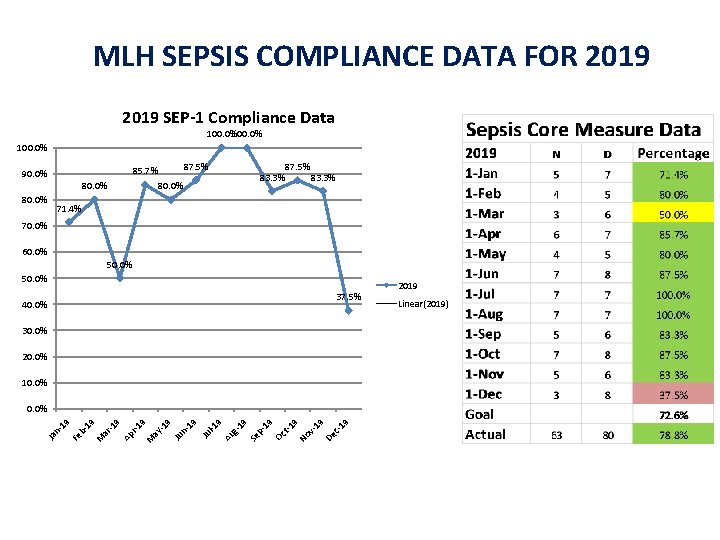
MLH SEPSIS COMPLIANCE DATA FOR 2019 SEP-1 Compliance Data 100. 0% 87. 5% 85. 7% 90. 0% 80. 0% 83. 3% 80. 0% 87. 5% 83. 3% 71. 4% 70. 0% 60. 0% 50. 0% 37. 5% 40. 0% 30. 0% 20. 0% 19 c- De v 19 No t-1 9 19 Oc p- 19 Se 9 Au g- l-1 Ju n 19 Ju -1 9 9 ay M r-1 Ap -1 9 ar 19 M b. Fe Ja n 1 9 0. 0% 2019 Linear(2019)
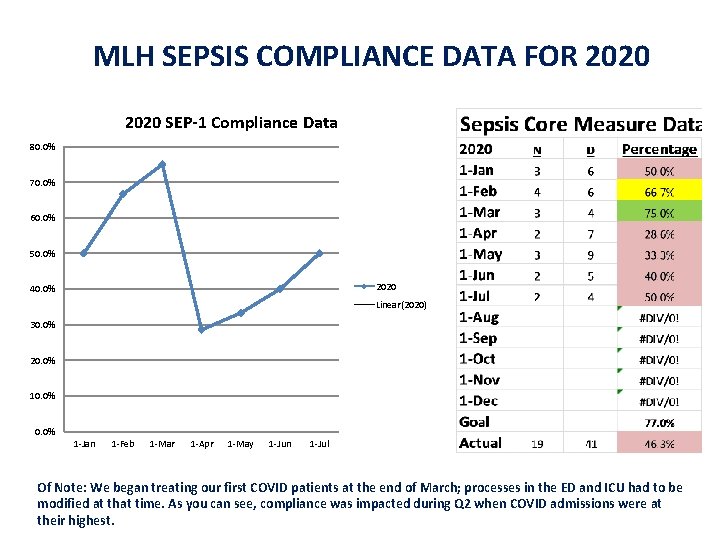
MLH SEPSIS COMPLIANCE DATA FOR 2020 SEP-1 Compliance Data 80. 0% 70. 0% 60. 0% 50. 0% 2020 40. 0% Linear(2020) 30. 0% 20. 0% 10. 0% 1 -Jan 1 -Feb 1 -Mar 1 -Apr 1 -May 1 -Jun 1 -Jul Of Note: We began treating our first COVID patients at the end of March; processes in the ED and ICU had to be modified at that time. As you can see, compliance was impacted during Q 2 when COVID admissions were at their highest.
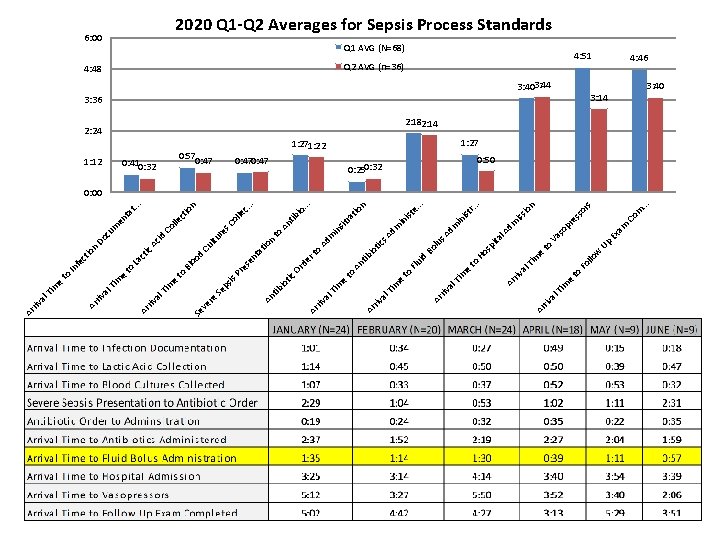
riv al e m Ti to w llo e 3: 36 3: 403: 44 m. . . Co rs es so Q 2 AVG (n=36) am so pr n io iss dm Q 1 AVG (N=68) Ex Va Up to e. . . n in ist r. . . ist in dm l. A sp ita s. A lu Bo Ho m Ti to Fo al riv e m Ti id Flu m Ad tio 0: 250: 32 Ar al to tic s io tib An sit ra in 1: 271: 22 Ar riv e Ti m to Ad m . . . io An tib 2: 24 Ar al e o rt to . 0: 47 riv Ti m de Or n io c. . le s. C ol re n ct io lle Co 4: 48 Ar al riv Ar tic io tib id ltu Ac . ta t. . en m cu Do Cu ta t es en d oo La ct ic Bl Pr to is ps Se e to n io ct fe In 0: 570: 47 An re ve Ti m e m Ti to 0: 410: 32 Se al riv al e m Ti 1: 12 Ar al riv Ar 6: 00 2020 Q 1 -Q 2 Averages for Sepsis Process Standards 4: 51 4: 46 3: 14 3: 40 2: 182: 14 1: 27 0: 50 0: 00
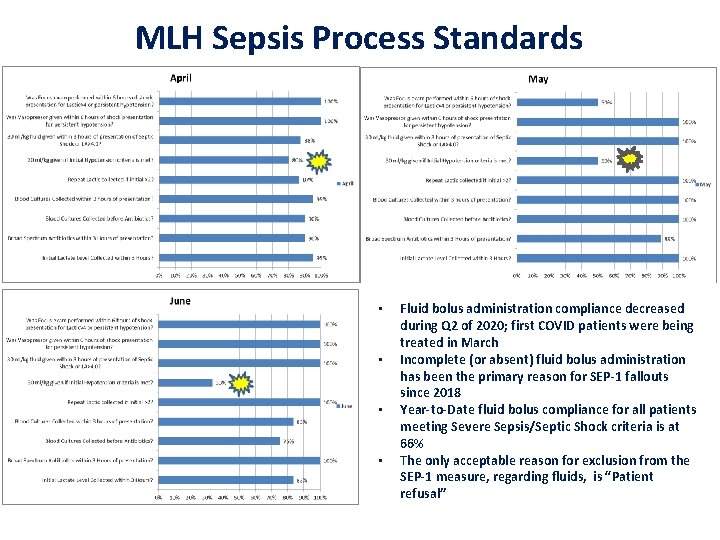
MLH Sepsis Process Standards • • Fluid bolus administration compliance decreased during Q 2 of 2020; first COVID patients were being treated in March Incomplete (or absent) fluid bolus administration has been the primary reason for SEP-1 fallouts since 2018 Year-to-Date fluid bolus compliance for all patients meeting Severe Sepsis/Septic Shock criteria is at 66% The only acceptable reason for exclusion from the SEP-1 measure, regarding fluids, is “Patient refusal”
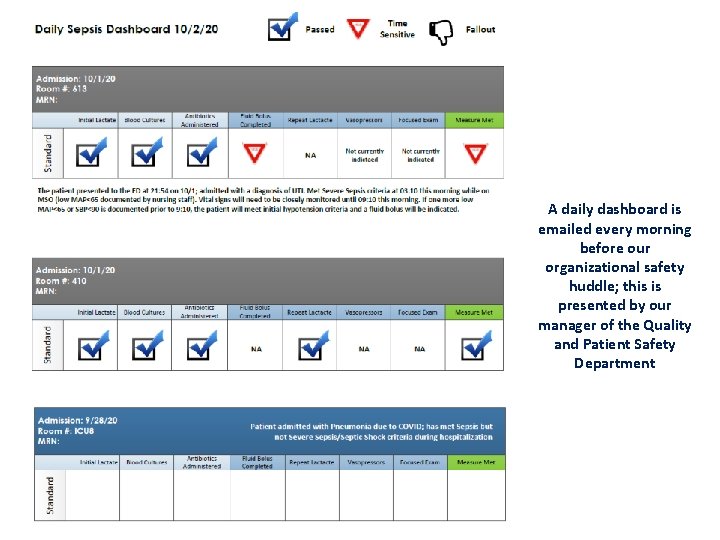
A daily dashboard is emailed every morning before our organizational safety huddle; this is presented by our manager of the Quality and Patient Safety Department
Nebraska Sepsis Toolkit Available www. nebraskahospitals. org
Dana Steiner BSN, MBA dsteiner@nebraskahospitals. org 308. 627. 3086 www. nebraskahospitals. org
- Slides: 35