Best Practices Basic Care in Indwelling Urinary Catheter
Best Practices: Basic Care in Indwelling Urinary Catheter Management January 2016 Mary H. Wilde, Ph. D, RN Professor, School of Nursing, University of Rochester, USA Member of the ICS Nurses’ Committee International Continence Society Teaching Module
Objectives • Our purpose is to educate continence nurses to improve patient care and health outcomes globally. At the conclusion of this presentation, readers should be able to: • 1. Describe best practices for basic care of people using indwelling urinary catheters. • 2. Understand the differences and similarities in shorter‐term care in acute settings as compared with long‐term care in the community. Teaching Module
Prevalence of catheter use Prevalence in the USA: • Acute care, 15‐ 25%; 5% nursing homes (Gould et al. HICPAC, 2009) • Long term catheter users overall estimate is 153, 818. • 9% home care ; 33% hospice (National Home and Hospice Study, 2007 cdc. gov/pub/Health Statistics/NCHS/Datasets/NHHCS/2007) • 34% in home care were long‐term users (Wilde et al, 2010. ) • Spinal cord injury– 23% of those discharged from rehabilitation, but some use an intermittent catheter later. (Cameron et al. , 2010) Prevalence in England: • England & Wales, 19 hospitals 1997 cited by Scottish Nurses Association, 26. 3% in acute care, range 12‐ 40% depending on specialty (Glynn et al. 1997) • England, survey in acute care, 18%, varied by specialty, more in ICU. HPA survey on HCAI and antimicrobial use across acute hospitals in England (2011) • England, 0. 07% community study of 827, 595 over two years (0. 05% > 75 yrs old) (Kohler‐Ochmore & Feneley 1996) Teaching Module
Indications for short-term catheter use § Urinary retention or bladder outlet obstruction § Improving comfort for end‐of‐life care if needed § Critically‐ill and need for accurate measurements of I&O (e. g. , hourly monitoring) § Selected surgical procedures (GU surgery/colorectal surgery) § Assist in healing open sacral or perineal wound in the incontinent patient § Intraoperative monitoring of urinary output during surgery or large volumes of fluid or diuretics anticipated § Prolonged immobilization (e. g. , potentially unstable thoracic or lumbar spine, multiple traumatic injuries such as pelvic fractures) http: //nursingworld. org/CAUTI‐Tool (based on USA CDC guidelines, Gould et al. 2009) Teaching Module
Indications for long-term catheter use § Intractable urinary retention for those who cannot manage an intermittent catheter (and no caregiver to do it) § Bladder outlet obstruction, not surgically treated § Improving comfort for end‐of‐life care if needed § Alternatives to consider: toileting schedule (when no retention), intermittent catheter, condom/sheath catheter (for cooperative males without obstructed urine or persistent retention ) (USA CDC guidelines, Gould et al. 2009) Teaching Module
Short & long-term catheter use defined: § Short term‐ less than 1 months’ expected use § Can be longer, failing trial without catheter § Long term‐ over 1 months use but often extends over many years. § “Indefinite use” would be more accurate term, but no agreement on terminology. § Both “catheter types” and “catheter use” for expected time of catheterization are called short and long‐term, causing confusion. (Cottenden et al. 2013) Teaching Module

Short term catheter types § Short term use—less than 14 days’ expected use § Latex or plastic, but caution related to latex allergy. § Coated catheters (silver alloy, nitrofurazone or minocycline/rifampicin) for up to two weeks § Can decrease bacteriuria but do not prevent symptomatic UTI & evidence is weak. § Can be uncomfortable and are more expensive. (Lam et al. , 2014) § Long term catheter types also can be used. (Cottenden et al. , 2013). Teaching Module
Long term catheter types § Can be used for 28 days and up to 12 weeks, dependent on local policy. § Latex coated poly‐tetrafluoro‐ethylene (PTFE or Teflon) § Silicone elastomer‐coated latex or 100% silicone (harder surface but wider lumen). Balloon water can evaporate quicker in pure silicone catheters. Take care to prevent traction as erosion of penis has occurred with silicone. § Hydrogel polymer‐coated latex (softer which can be of benefit) Hydrogel less likely to form suprapubic catheter “deflation cuff”. (Parkin, 2002; Jahn et al. 2012; Cottenden et al. 2013) Teaching Module
Catheter sizes (Fr= French which is the same as Charrière or Ch) Use the smallest size that permits flow and to prevent potential trauma to urethra and sphincter. • 12‐ 16 Fr for men and 12‐ 14 Fr for women. • Children: 5‐ 6 Fr for newborns ; 5‐ 10 Fr toddlers to children to age 12 Balloons 5‐ 10 m. L. (30 m. L only for postoperative bleeding), 2. 5‐ 5 m. L for children (WOCN, Indwelling Urinary Catheters, Best Practices for Clinicians, 2009; Cottenden et al. 2013) Teaching Module

Catheter insertion • For Males: • Insert all the way to Y (bifurcation) to prevent § Long term catheters often catheter being inflated changed every 4 weeks. People within the urethra. with frequent blockage can need • If resistance is felt, it every 2‐ 3 weeks or more often. encourage deep breaths and distraction. Can extend to 6‐ 8 weeks if no problems. § Observe several changes for • For females: Urethra can be short, “catheter life pattern. ” (Getliffe, especially in older women. 1994) § Good lighting, and help of another if spasticity in legs. § Use sterile gloves. § Lubricate catheter well, especially for males. Teaching Module § Insert 1” further than point of urine flow. § Fill balloon all the way to 10 m. L. (ANA CAUTI prevention, 2015 http: //nursingworld. org/ANA‐CAUTI‐ Prevention‐Tool ; Wilde & Feng, 2013)

Catheter securement § Nurses often recommend but not use it: § Of 82 nurses (8 continence specialists), 98% recommended but only 4% used it. (Siegel, 2006); § 18% secured in acute care in one day point‐ prevalence study (N= 8 of 44) (Appah et al. 2015) § Securement could prevent dislodgement and urethral/bladder neck trauma § Adhesive—good for those likely to dislodge but irritating to skin § Non‐adhesive—prevent constricting circulation (Wilde & Feng, 2013) Teaching Module
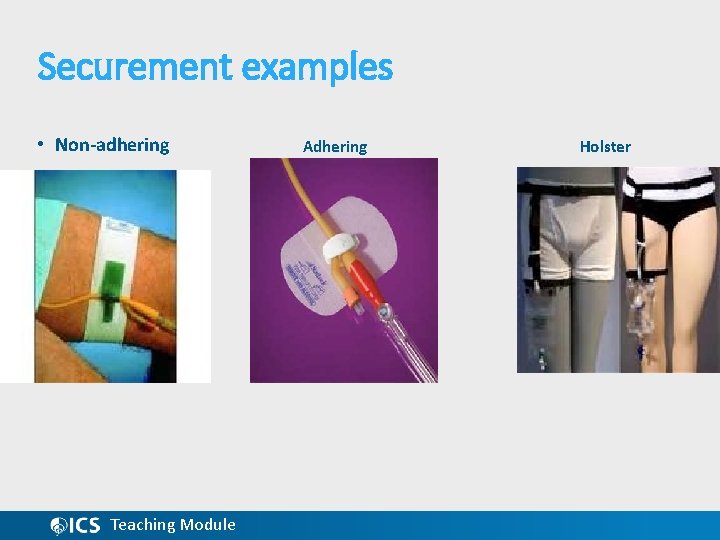
Securement examples • Non-adhering Teaching Module Adhering Holster
General catheter care § Hand hygiene before and after catheter care. In home, teach family. § If breaks in the closed system (e. g. , disconnection, cracked tubing), replace the catheter and tubing. § Perform perineal hygiene at a minimum daily, per facility protocol/procedure and as needed. Soap and water is all that is needed most often. § Use fecal containment device when appropriate for fecal incontinence. ANA CAUTI prevention, 2015 http: //nursingworld. org/ANA‐CAUTI‐Prevention‐Tool Teaching Module
Drainage bags § Closed drainage essential in acute care, short term use. § It is the only proven method of decreasing UTI. (Kunin & Mc. Cormack, 1966) § Types: § Overnight (2000‐ 4000 m. L) § Leg bags (270‐ 1000 m. L. ) § Belly bag (with normal bladder pressure) (WOCN, 2009) § Prevent kinks/twists in tubing: Blocked urine flow can contribute to damage to the kidneys (Feneley et al. 2015) § Keep bag at least 12” below the level of the bladder and off the floor to prevent suction of the catheter eyes on the bladder mucosa. (Glahn et al. 1988) Teaching Module
Care for drainage bags § Empty the drainage bag regularly using a separate, clean collecting container for each patient; avoid splashing, and prevent contact of the drainage spout. http: //nursingworld. org/ANA‐CAUTI‐Prevention‐Tool § Empty when 1/3 to ½ full. § For long‐term catheter users, replace drainage bags weekly. § No evidence that connecting a catheter to a leg bag continuously & then hooking up an overnight bag is beneficial. (Cottenden et al. 2013) Teaching Module
Cleaning & reuse of drainage bags § Systematic review revealed need for research in this area. § Conflicting guidelines and research virtually lacking since 1990 s. (Wilde, Fader et al. 2013) § In a U. S. study of 202 long‐term catheter users, most switched between leg and night bag § 54% cleaned leg bags & 59% night bags. (Wilde , Mc. Donald, et al. 2013) § Rehabilitation nurses have used mild bleach (1 part household bleach to 10 parts water). (Dille & Kirchhoff, 1993; Dille et al. 1993) § In home care in the past: vinegar was recommended (1 part vinegar to 4 parts water) (Wilde, 1986) Teaching Module
Irrigation (also called flushing or washouts) § Irrigation not recommended. Sometimes used in hospitals to remove blood clots post operatively. § In one U. S. study of 202 long term catheter users , 42% irrigated and 18% once or more a day. § Solutions were saline (76%) and sterile water (23%). § Surprising, 9% used plain tap water, which could have bacteria or other impurities in it. § 4% used Renacidin ‐‐not readily available in the US and made fresh in a pharmacy. (Wilde, Mc. Donald et al. 2013) Teaching Module

Irrigation sachets § Irrigation sachets (Suby G and Suby R, called catheter maintenance solutions) are available in the United Kingdom, and in some other countries, to dissolve encrustations if change is not appropriate. These solutions are not available in every country. § Saline or sterile water is not effective in breaking up encrustations. § Research in Canada testing saline, no irrigation and Suby G showed no difference in decreasing time to change but underpowered. (Moore et al. , 2009) § There is a desperate need for irrigation solutions which are effective, easily obtained and used, inexpensive, and safe. Teaching Module
Symptoms CAUTI- short term catheter users • In acute care diagnosis of CAUTI, catheter in place 2> days: • 1. At least one symptom below with no other recognized cause: • fever (>38. 0°C) • suprapubic tenderness • costovertebral angle pain or tenderness • urinary urgency • urinary frequency • dysuria 2. AND urine culture with no more than two microorganism ≥ 105 CFU/m • http: //www. cdc. gov/nhsn/pdfs/psc. Manual/7 psc. CAUTIcurre nt. pdf • Differential diagnosis not simple to identify source of infection • Fever‐‐ without other possible source, comorbidities confound • Bacteriuria (Lo et al. , 2014) Teaching Module
Symptoms CAUTI--long term catheters • Urine Changes: • Color – Discolored, cloudy, dark, blood stained • Odor – Foul smelling, change in smell from usual • Sediment (grit) – Increased amount Temperature – Fever, chills Pain and/or pressure in bladder area or back (Burning possible, not common) Teaching Module Early, mild symptoms of autonomic dysreflexia (e. g. , goosebumps, headaches, sweats) mainly in people with spinal cord injury General Symptoms Blahs!, feeling sick • Functioning or mental changes – weakness, spasticity, change in the level of alertness (Wilde, Mc. Donald et al. , 2013)
CAUTI prevention § Do not insert indwelling catheter if bladder management is possible any other way, e. g. , condom catheter (sheath, external) or intermittent catheter (including caregiver performing or assisting). § Remove catheter as soon as possible. § Track CAUTI rate systematically: Events of symptomatic UTI X 1000 Catheter days’ use (number of persons X days catheter used) § Encourage staff and celebrate when CAUTI rate & usage of catheters decreases. § In acute care, a daily order for catheter continued use is recommended. § In community, assess regularly whether indwelling is still needed. § Check out this important document from the USA, American Nurses’ Association: ANA CAUTI prevention, 2015 http: //nursingworld. org/ANA‐CAUTI‐ Prevention‐Tool Teaching Module
References • Appah, Y. , Hunter, K. F. , & Moore, K. N. (2015). Securement of the indwelling urinary catheter: A prevalence study. Journal of Wound, Ostomy, and Continence Nursing doi: 10. 1097/WON. 0000000176 • Cameron AP, Wallner LP, Tate DG, Sarma AV, Rodriguez GM, Clemens JQ. Bladder management after spinal cord injury in the United States 1972 to 2005. J Urol. 2010 Jul; 184(1): 213‐ 7. doi: 10. 1016/j. juro. 2010. 03. 008. • Cottenden, A. , Bliss, D. , Buckley, B. , Fader, M. , Gartley, C. , Hayer, D , Ostaszkiewicz, J. , Pieters, R. , & Wilde, M. H (2013). Management using continence products. In P. Abrams, L. Cardozo, S. Khoury, & A. Wein A, Eds. , Incontinence: 5 th international consultation on incontinence (pp. 1651 -1786). Arnheim, The Netherlands: ICUD‐EAU Publishers • Dille, C. A. , Kirchhoff, K. T. , Sullivan, J. J. , & Larson, E. (1993). Increasing the wearing time of vinyl urinary drainage bags by decontamination with bleach. Arch Phys Med Rehabil, 74(4), 431‐ 7. Teaching Module
• Dille, C. M. , & Kirchhoff, K. T. (1993). Decontamination of vinyl urinary drainage bags with bleach. Rehabil Nurs, 18(5), 292‐ 5. doi: 10. 1002/14651858. CD 004013. pub 4 • Fisher, E. , Gillies, K. , & Mac. Lennan, S. (2014). Types of indwelling urethral catheters for short‐term catheterisation in hospitalised adults. The Cochrane Database of Systematic Reviews, 9, CD 004013. • Feneley, R. C. , Hopley, I. B. , & Wells, P. N. (2015). Urinary catheters: History, current status, adverse events and research agenda. Journal of Medical Engineering & Technology, 1‐ 12. • Getliffe, K. A. (1994). The characteristics and management of patients with recurrent blockage of long‐term urinary catheters. J Adv Nurs, 20(1), 140‐ 9. • Glahn, B. E. , Braendstrup, O. , & Olesen, H. P. (1988). Influence of drainage conditions on mucosal bladder damage by indwelling catheters. II. histological study. Scand J Urol Nephrol, 22(2), 93‐ 9. Teaching Module
• Glynn A, Ward V, Wilson J, et al. 1997. Hospital Acquired Infection: Surveillance Policies and Practice. A Report of a Study of the Control of Hospital Acquired Infection in 19 Hospitals in England Wales. London: Public Health Laboratory Service. • Gould, C. V. , Umscheid, C. A. , Agarwal, R. K. , Kuntz, G. , Pegues, D. A. , & and the Healthcare Infection Control Practices Advisory Committee (HICPAC). (2009). Guideline for prevention of catheter -associated urinary tract infections 2009. Atlanta, GA: Centers for Disease Control and Prevention. • Jahn, P. , Beutner, K. , & Langer, G. (2012). Types of indwelling urinary catheters for long‐term bladder drainage in adults. The Cochrane Database of Systematic Reviews, 10, CD 004997. doi: 10. 1002/14651858. CD 004997. pub 3 [doi] • Kunin, C. M. , & Mc. Cormack, R. C. (1966). Prevention of catheter‐ induced urinary‐tract infections by sterile closed drainage. The New England Journal of Medicine, 274(21), 1155‐ 1161. doi: 10. 1056/NEJM 196605262742101 Teaching Module
• Lo, E. , Nicolle, L. E. , Coffin, S. E. , Gould, C. , Maragakis, L. L. , Meddings, J. , . . . Yokoe, D. S. (2014). Strategies to prevent catheter‐associated urinary tract infections in acute care hospitals: 2014 update. Infection Control and Hospital Epidemiology, 35 Suppl 2, S 32‐ 47. • Lam, T. B. , Omar, M. I. , Fisher, E. , Gillies, K. , & Mac. Lennan, S. (2014). Types of indwelling urethral catheters for short‐term catheterisation in hospitalised adults. The Cochrane Database of Systematic Reviews, 9, CD 004013. doi: 10. 1002/14651858. CD 004013. pub 4 [doi] • Moore, K. N. , Hunter, K. F. , Mc. Ginnis, R. , Puttagunta, L, Chobanak, J. , Bascu, C. , Fader M. , & Voaklander, D. (2009). Do catheter washouts extend patency time in long term urethral catheters? A randomized controlled trial of acidic washout solution, normal saline washout, or standard care. Journal of Wound, Ostomy and Continence Nursing, 36, 82‐ 90. Teaching Module
• Parkin, J. , Scanlan, J. , Woolley, M. , Grover, D. , Evans, A. , & Feneley, R. C. (2002). Urinary catheter 'deflation cuff' formation: Clinical audit and quantitative in vitro analysis. BJU Int, 90(7), 666‐ 71. • Siegel, T. J. (2006). Do registered nurses perceive the anchoring of indwelling urinary catheters as a necessary aspect of nursing care? : A pilot study. J Wound Ostomy Continence Nurs, 33(2), 140‐ 4. • Wilde, M. H. (1986). Living with a Foley. American Journal of Nursing , 86(10), 1121‐ 3. • Wilde, M. H. , Brasch, J. , Getliffe, K. , Brown, K. A. , Mc. Mahon, J. M. , Smith, J. A. , . . . Tu, X. (2010). Study on the use of long‐term urinary catheters in community‐dwelling individuals. Journal of Wound, Ostomy, and Continence Nursing, 37(3), 301‐ 310. doi: 10. 1097/WON. 0 b 013 e 3181 d 73 ac 4 • Wilde, M. H. , Fader, M. , Ostaszkiewicz, J. , Prieto, J. , & Moore, K. (2013). Urinary bag decontamination for long‐term use: A systematic review. Journal of Wound, Ostomy, and Continence Nursing, 40(3), 299‐ 308. doi: 10. 1097/WON. 0 b 013 e 3182800305 [doi] Teaching Module

• Wilde, M. H. , Mc. Donald, M. V. , Brasch, J. , Mc. Mahon, J. M. , Fairbanks, E. , Shah, S. , . . . Scheid, E. (2013). Long‐term urinary catheter users self‐care practices and problems. Journal of Clinical Nursing, 22(3‐ 4), 356‐ 367. • Wilde, M. H. , & Zhang, F. (2013). Best practices in managing the indwelling urinary catheter for the homecare patient. Perspectives, 10, 1‐ 7‐ 12. • Wilde, M. H. , Zhang, F. , Fairbanks, E. , Shah, S. , Mc. Donald, M. V. , & Brasch, J. , (2013). Perceived value of a urinary catheter self‐ management program in the home. Home Healthcare Nurse, 31 (9), 465 -473. doi: 10. 1097/NHH. 0 b 013 e 3182 a 89791 • WOCN Society Clinical Practice Continence subcommittee. (2009). Indwelling urinary catheters: Best practice for clinicians Wound Ostomy and Continence Nursing Society. Teaching Module
- Slides: 27