Benign Prostatic Hyperplasia Prostate Gland Male organ 20

攝護腺肥大症 (Benign Prostatic Hyperplasia)
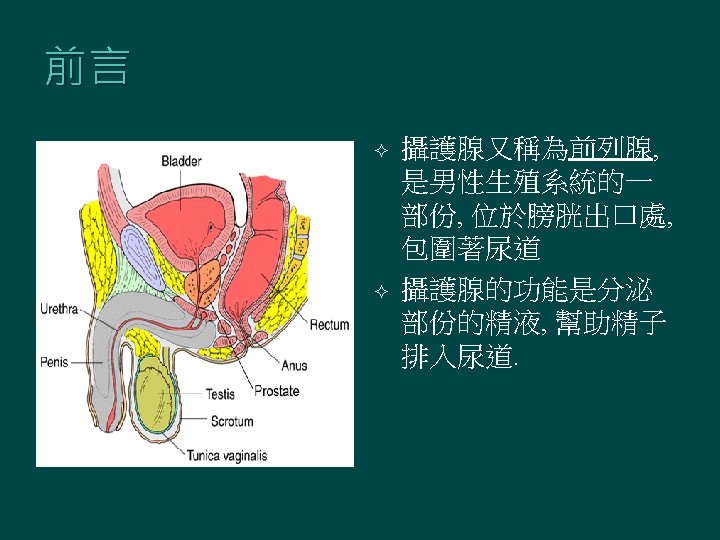
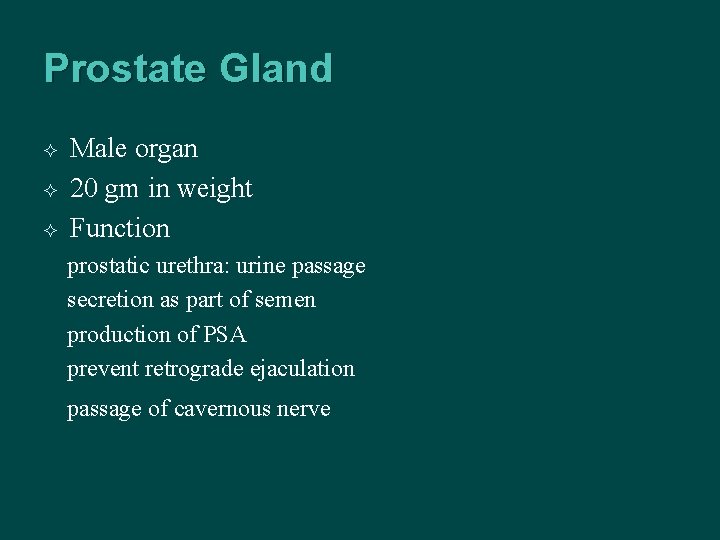
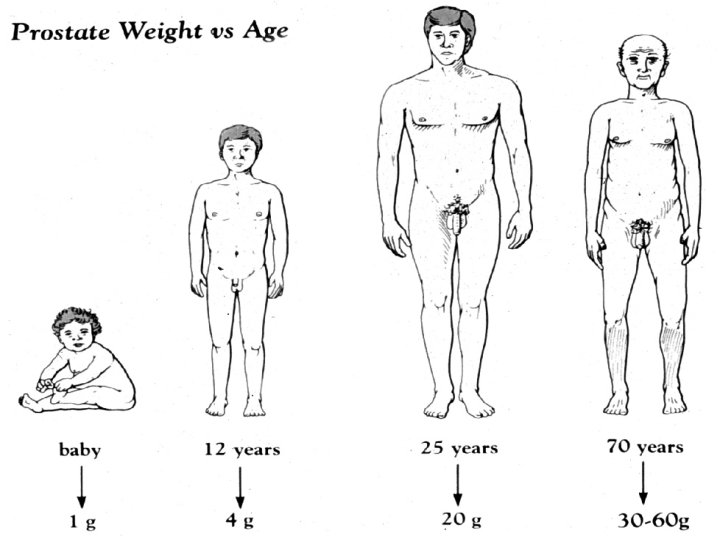
Prostate Gland Male organ 20 gm in weight Function prostatic urethra: urine passage secretion as part of semen production of PSA prevent retrograde ejaculation passage of cavernous nerve
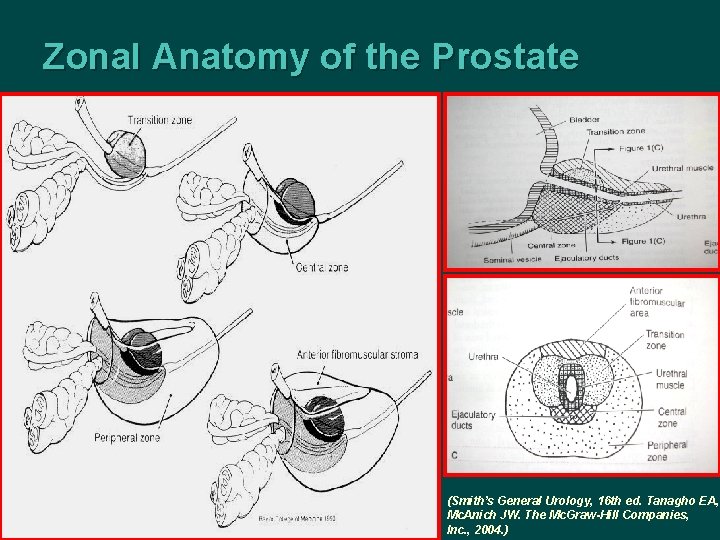
Zonal Anatomy of the Prostate (Smith’s General Urology, 16 th ed. Tanagho EA, Mc. Anich JW. The Mc. Graw-Hill Companies, Inc. , 2004. )
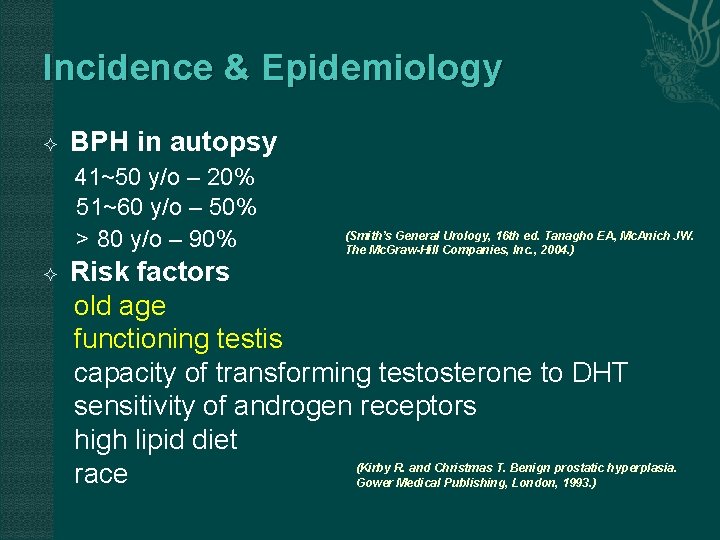
Incidence & Epidemiology BPH in autopsy 41~50 y/o – 20% 51~60 y/o – 50% > 80 y/o – 90% (Smith’s General Urology, 16 th ed. Tanagho EA, Mc. Anich JW. The Mc. Graw-Hill Companies, Inc. , 2004. ) Risk factors old age functioning testis capacity of transforming testosterone to DHT sensitivity of androgen receptors high lipid diet (Kirby R. and Christmas T. Benign prostatic hyperplasia. race Gower Medical Publishing, London, 1993. )
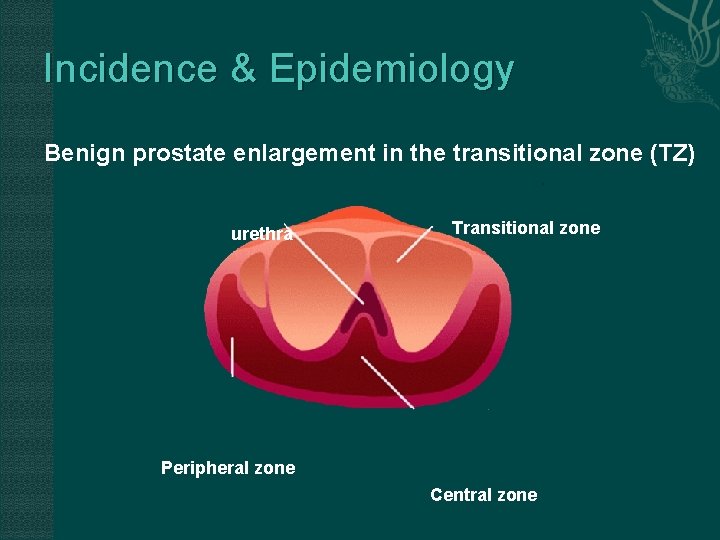
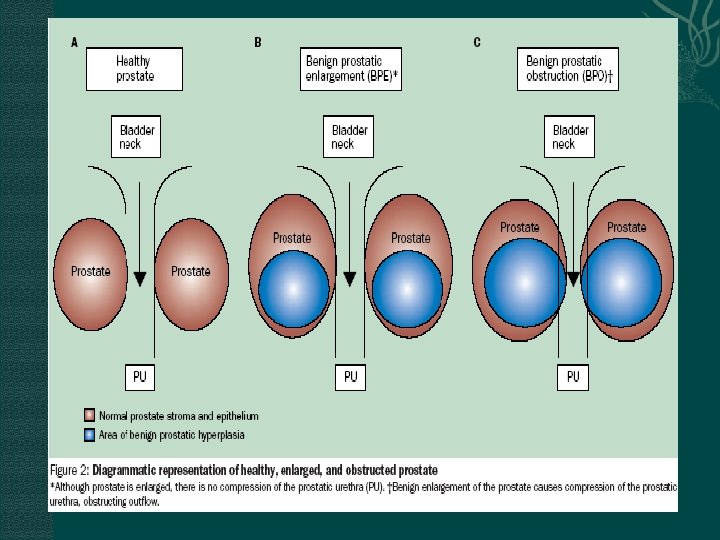
Incidence & Epidemiology Benign prostate enlargement in the transitional zone (TZ) urethra Transitional zone Peripheral zone Central zone
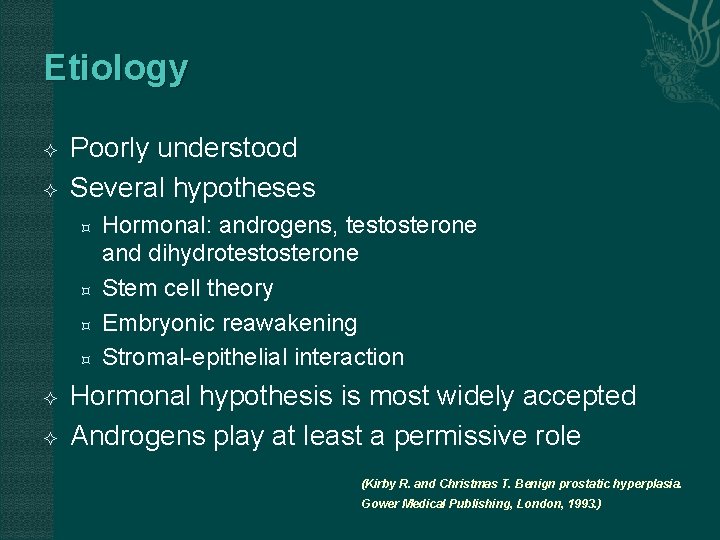
Etiology Poorly understood Several hypotheses Hormonal: androgens, testosterone and dihydrotestosterone Stem cell theory Embryonic reawakening Stromal-epithelial interaction Hormonal hypothesis is most widely accepted Androgens play at least a permissive role (Kirby R. and Christmas T. Benign prostatic hyperplasia. Gower Medical Publishing, London, 1993. )
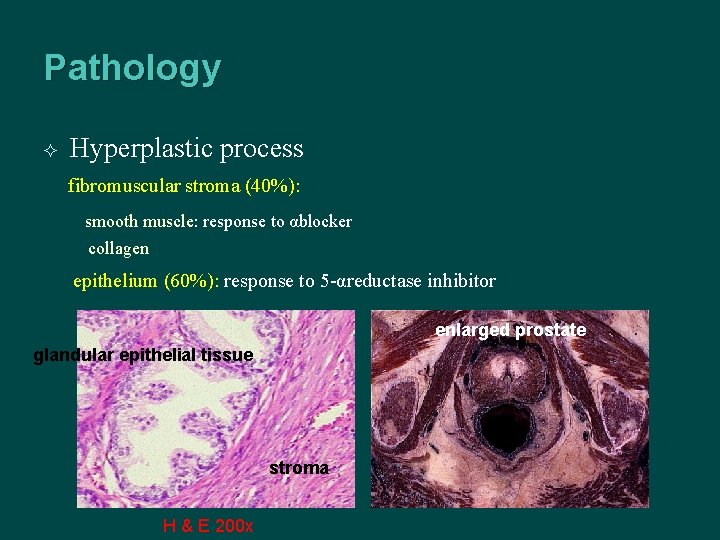
Pathology Hyperplastic process fibromuscular stroma (40%): smooth muscle: response to αblocker collagen epithelium (60%): response to 5 -αreductase inhibitor enlarged prostate glandular epithelial tissue stroma H & E 200 x
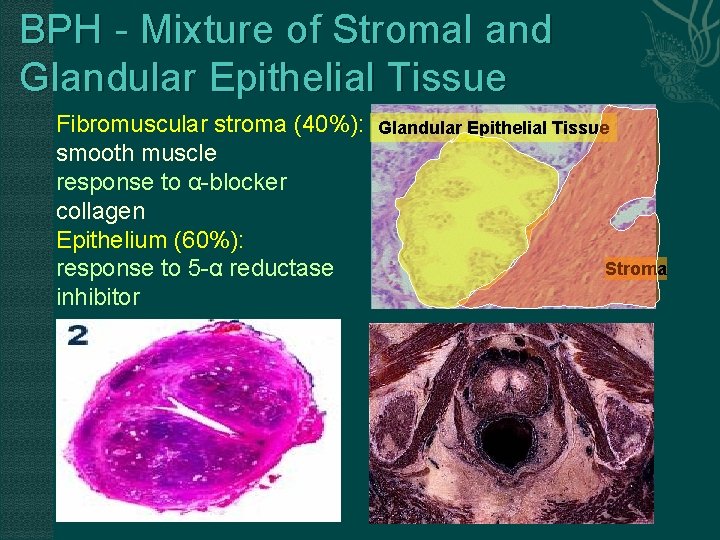
BPH - Mixture of Stromal and Glandular Epithelial Tissue Fibromuscular stroma (40%): smooth muscle response to α-blocker collagen Epithelium (60%): response to 5 -α reductase inhibitor Glandular Epithelial Tissue Stroma
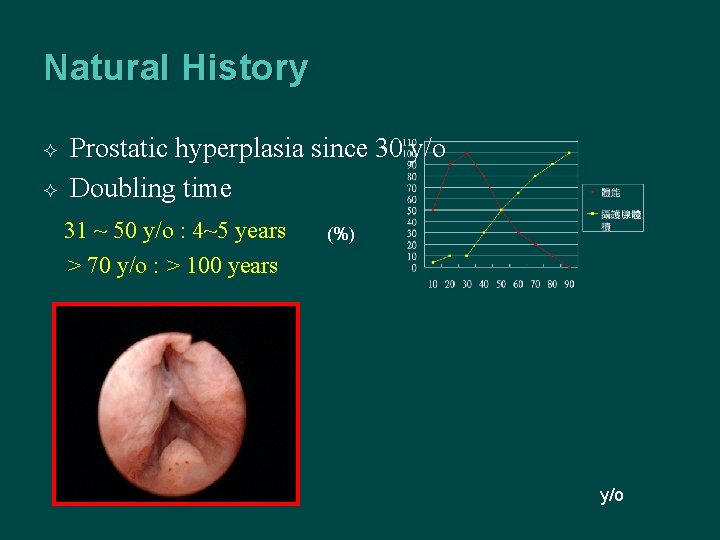
Natural History Prostatic hyperplasia since 30 y/o Doubling time 31 ~ 50 y/o : 4~5 years > 70 y/o : > 100 years (%) y/o
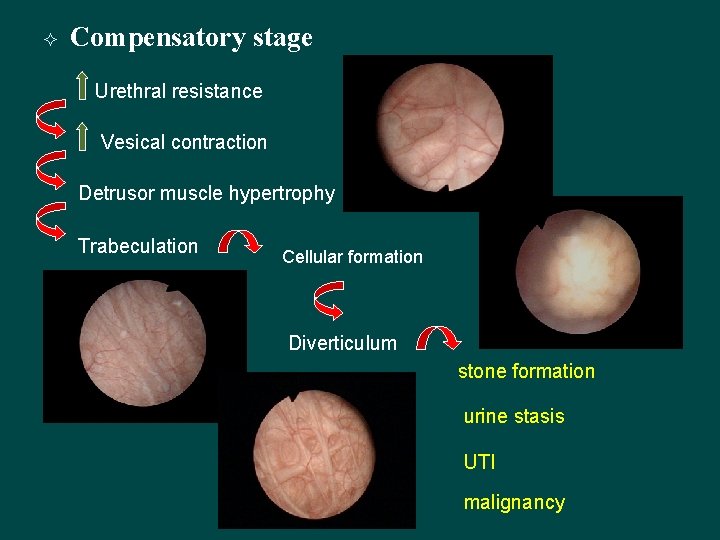
Compensatory stage Urethral resistance Vesical contraction Detrusor muscle hypertrophy Trabeculation Cellular formation Diverticulum stone formation urine stasis UTI malignancy
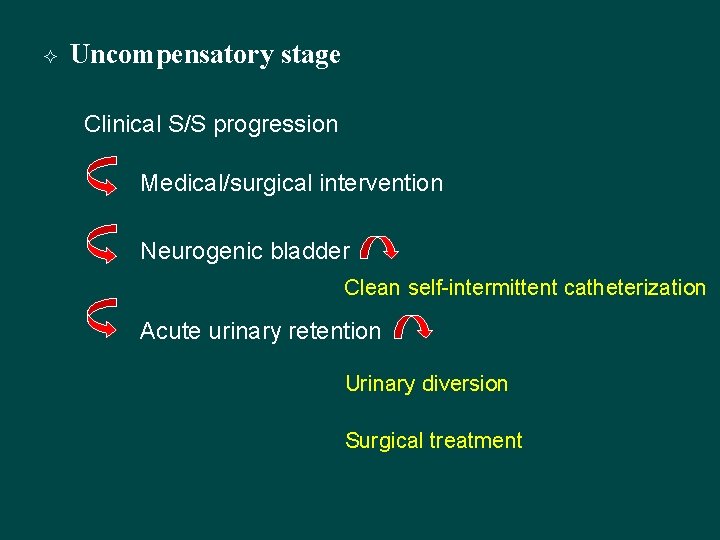
Uncompensatory stage Clinical S/S progression Medical/surgical intervention Neurogenic bladder Clean self-intermittent catheterization Acute urinary retention Urinary diversion Surgical treatment
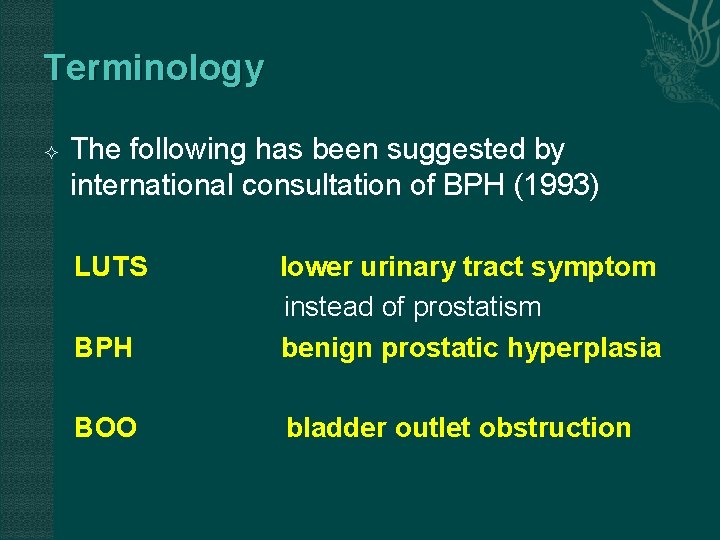
Terminology The following has been suggested by international consultation of BPH (1993) LUTS BPH lower urinary tract symptom instead of prostatism benign prostatic hyperplasia BOO bladder outlet obstruction
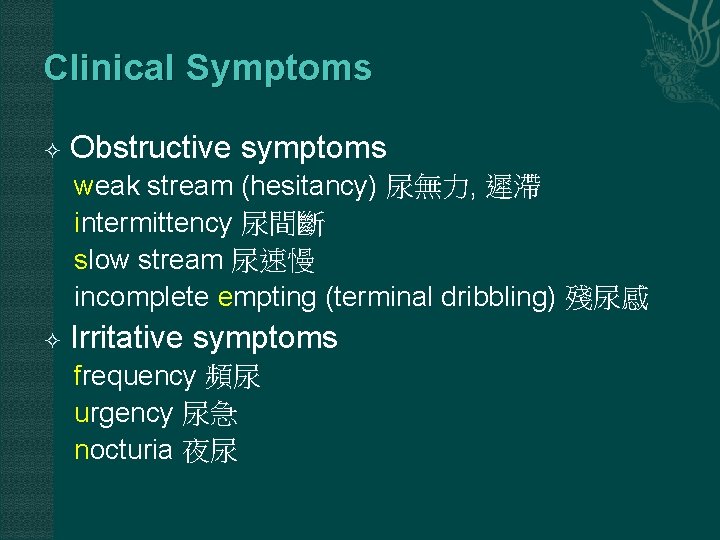
Clinical Symptoms Obstructive symptoms weak stream (hesitancy) 尿無力, 遲滯 intermittency 尿間斷 slow stream 尿速慢 incomplete empting (terminal dribbling) 殘尿感 Irritative symptoms frequency 頻尿 urgency 尿急 nocturia 夜尿
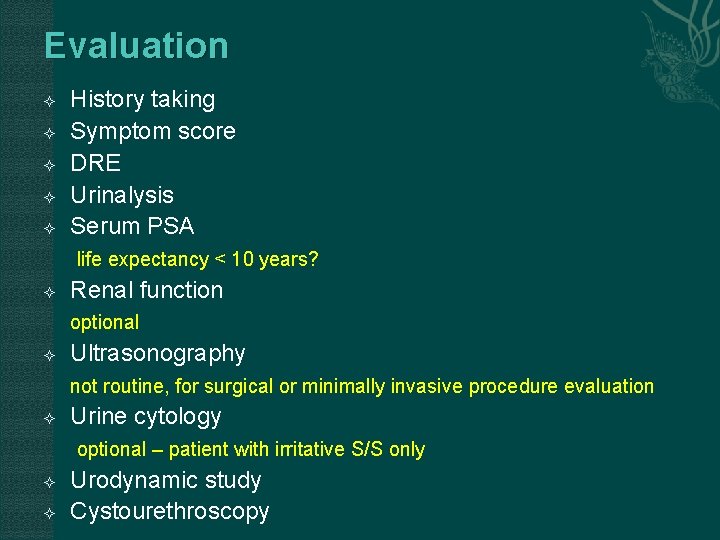
Evaluation History taking Symptom score DRE Urinalysis Serum PSA life expectancy < 10 years? Renal function optional Ultrasonography not routine, for surgical or minimally invasive procedure evaluation Urine cytology optional – patient with irritative S/S only Urodynamic study Cystourethroscopy
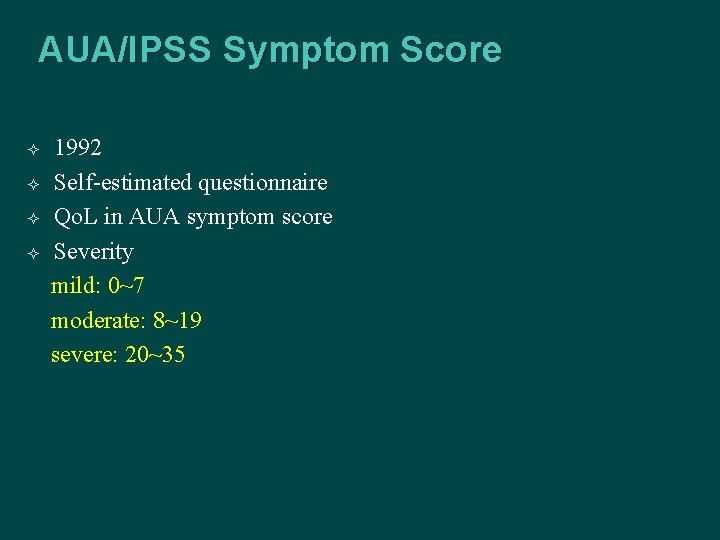
AUA/IPSS Symptom Score 1992 Self-estimated questionnaire Qo. L in AUA symptom score Severity mild: 0~7 moderate: 8~19 severe: 20~35
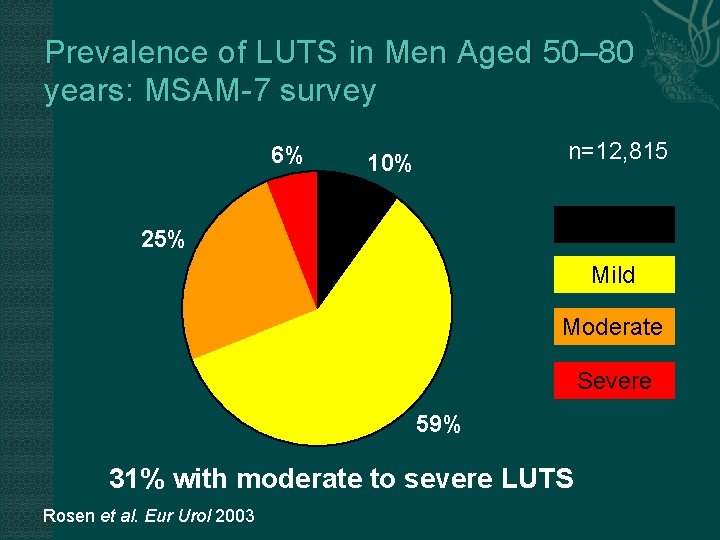
Prevalence of LUTS in Men Aged 50– 80 years: MSAM-7 survey 6% n=12, 815 10% IPSS=0 25% Mild Moderate Severe 59% 31% with moderate to severe LUTS Rosen et al. Eur Urol 2003
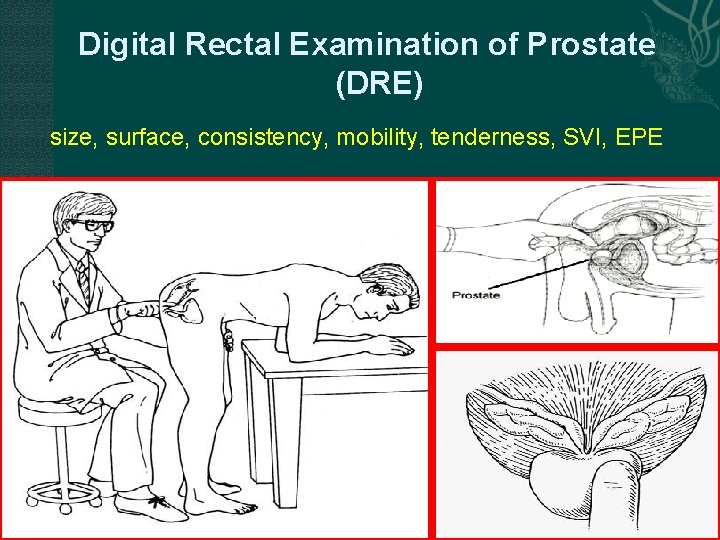
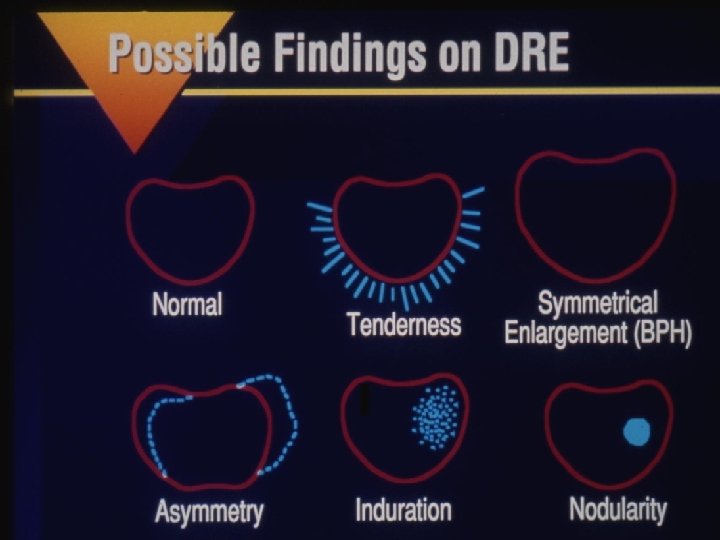
Digital Rectal Examination of Prostate (DRE) size, surface, consistency, mobility, tenderness, SVI, EPE
Physical examination – rectal examination Inspection – bulging, hairy skin or discoloration or scar in sacral area; lumps, ulcers, inflammation, rashes or excoriation in perianal areas Palpation 1. Perianal sensation, bulbocavernous reflex 2. The tonicity of the rectal sphincter 3. Prostate- size, shape and consistency- nodules induration, asymmetry, tenderness 4. Seminal vesicles 5. Peritoneal cavity- rectal shelf , tenderness
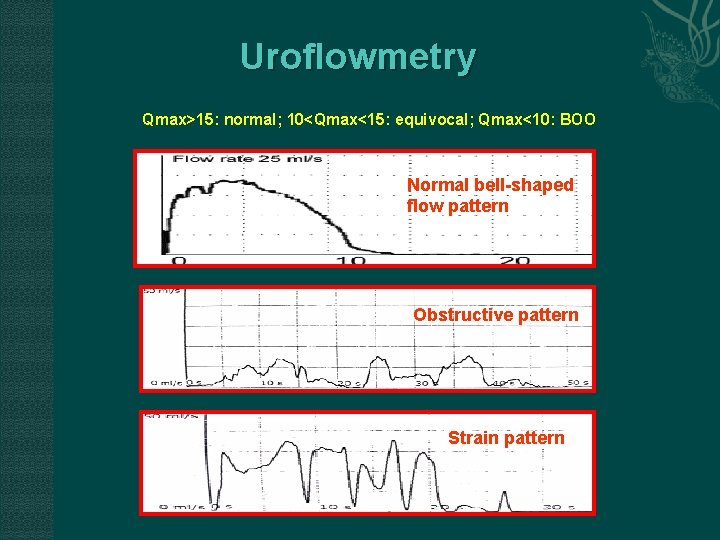
Uroflowmetry Qmax>15: normal; 10<Qmax<15: equivocal; Qmax<10: BOO Normal bell-shaped flow pattern Obstructive pattern Strain pattern
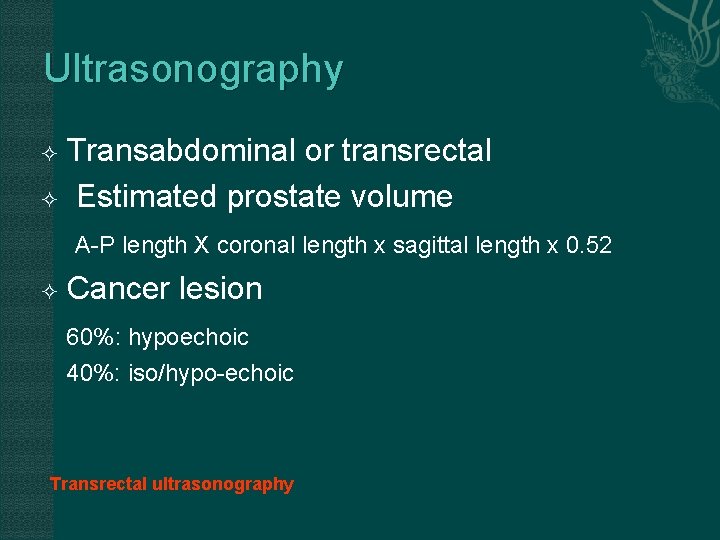
Ultrasonography Transabdominal or transrectal Estimated prostate volume A-P length X coronal length x sagittal length x 0. 52 Cancer lesion 60%: hypoechoic 40%: iso/hypo-echoic Transrectal ultrasonography
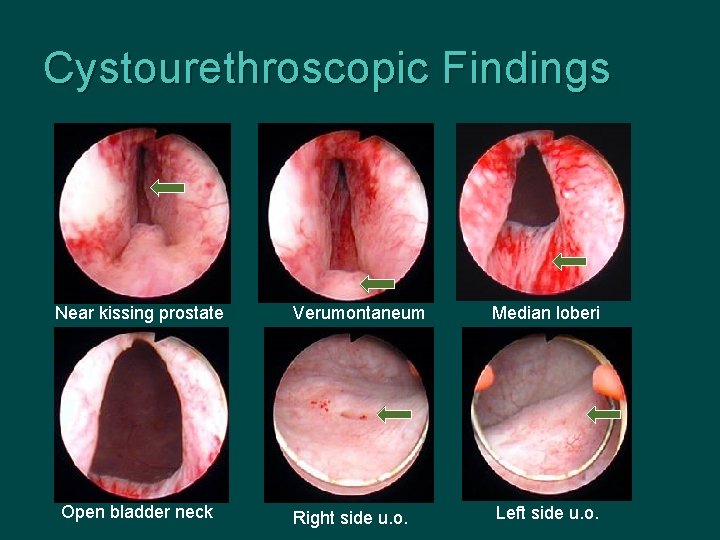
Cystourethroscopic Findings Near kissing prostate Open bladder neck Verumontaneum Median loberi Right side u. o. Left side u. o.
Treatment Modalities for BPH Watchful waiting Medical therapy Phytotherapy -adrenergic blockers 5 -reductase inhibitors Combination therapy Office-based treatment TUMT TUNA WIT Surgicenter/Hospital-based treatment TURP (gold standard) TUIP Open surgery (prostatectomy) TUVP ILC VLAP Prostatic stents Chatelain C et al. In: Chatelain C et al, eds. Benign Prostatic Hyperplasia. Plymouth, UK: Health Publication Ltd; 2001; 519 -534. Mc. Connell JD et al. Benign Prostatic Hyperplasia: Diagnosis and Treatment. Clinical Practice Guideline, Number 8.
Treatment Modalities for BPH Watchful waiting Medical therapy Phytotherapy -adrenergic blockers 5 -reductase inhibitors Combination therapy Office-based treatment TUMT TUNA WIT Surgicenter/Hospital-based treatment TURP (gold standard) TUIP Open surgery (prostatectomy) TUVP ILC VLAP Prostatic stents Chatelain C et al. In: Chatelain C et al, eds. Benign Prostatic Hyperplasia. Plymouth, UK: Health Publication Ltd; 2001; 519 -534. Mc. Connell JD et al. Benign Prostatic Hyperplasia: Diagnosis and Treatment. Clinical Practice Guideline, Number 8.
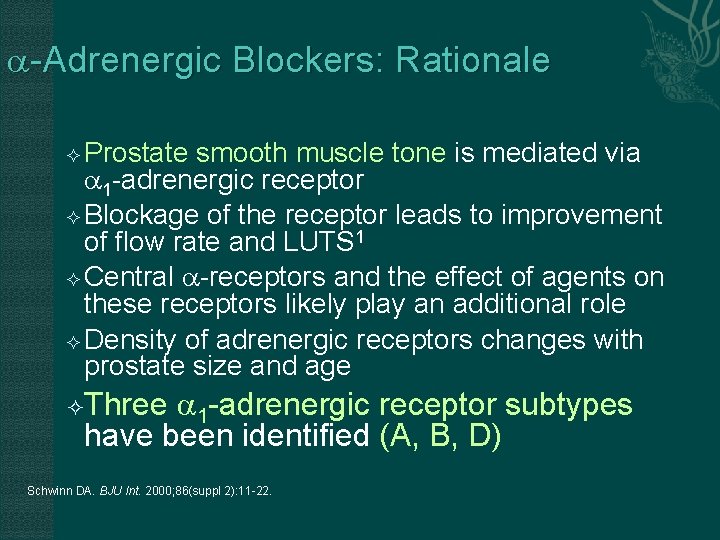
-Adrenergic Blockers: Rationale Prostate smooth muscle tone is mediated via 1 -adrenergic receptor Blockage of the receptor leads to improvement of flow rate and LUTS 1 Central -receptors and the effect of agents on these receptors likely play an additional role Density of adrenergic receptors changes with prostate size and age Three 1 -adrenergic receptor subtypes have been identified (A, B, D) Schwinn DA. BJU Int. 2000; 86(suppl 2): 11 -22.
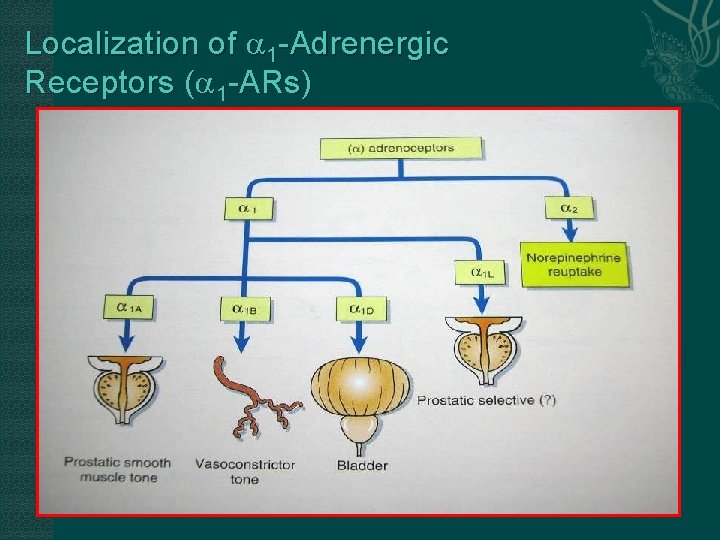
Localization of 1 -Adrenergic Receptors ( 1 -ARs)
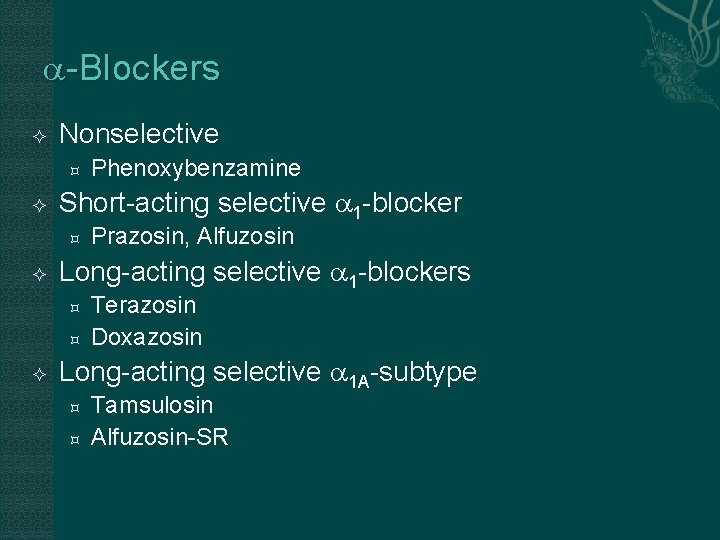
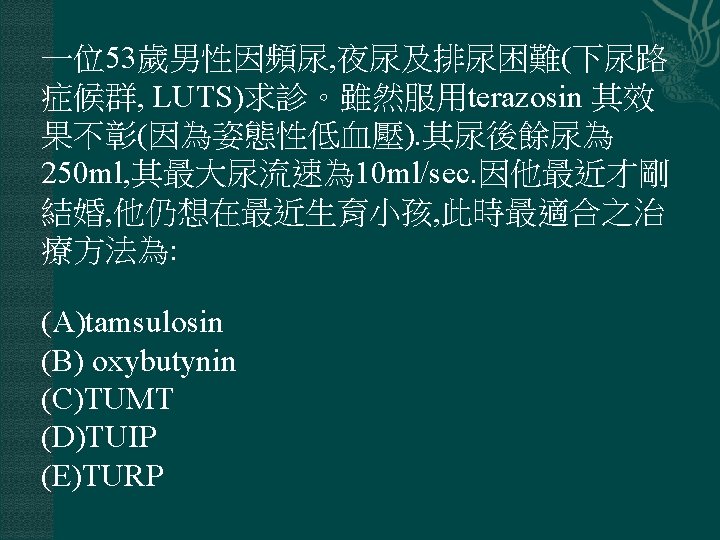
-Blockers Nonselective Short-acting selective 1 -blocker Prazosin, Alfuzosin Long-acting selective 1 -blockers Phenoxybenzamine Terazosin Doxazosin Long-acting selective 1 A-subtype Tamsulosin Alfuzosin-SR
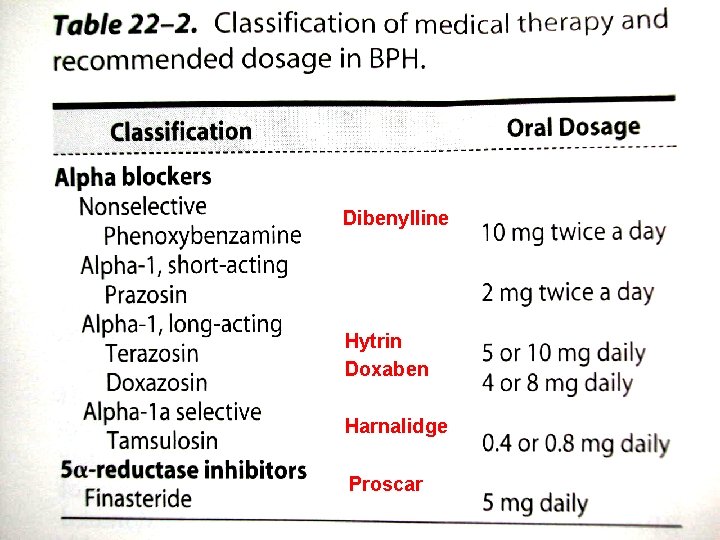
Dibenylline Hytrin Doxaben Harnalidge Proscar
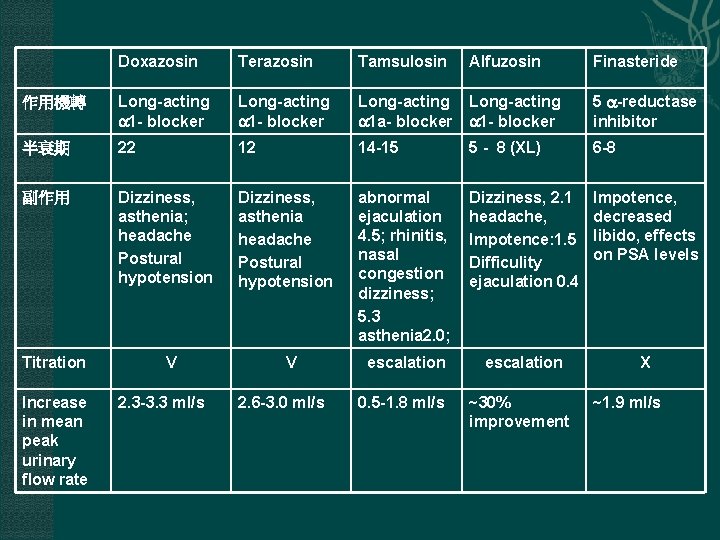
Doxazosin Terazosin Tamsulosin 作用機轉 Long-acting 1 - blocker Long-acting 1 a- blocker 1 - blocker 5 -reductase inhibitor 半衰期 22 12 14 -15 5 - 8 (XL) 6 -8 副作用 Dizziness, asthenia; headache Postural hypotension Dizziness, asthenia headache Postural hypotension abnormal ejaculation 4. 5; rhinitis, nasal congestion dizziness; 5. 3 asthenia 2. 0; Dizziness, 2. 1 headache, Impotence: 1. 5 Difficulity ejaculation 0. 4 Impotence, decreased libido, effects on PSA levels escalation X Titration Increase in mean peak urinary flow rate V 2. 3 -3. 3 ml/s V 2. 6 -3. 0 ml/s 0. 5 -1. 8 ml/s Alfuzosin ~30% improvement Finasteride ~1. 9 ml/s
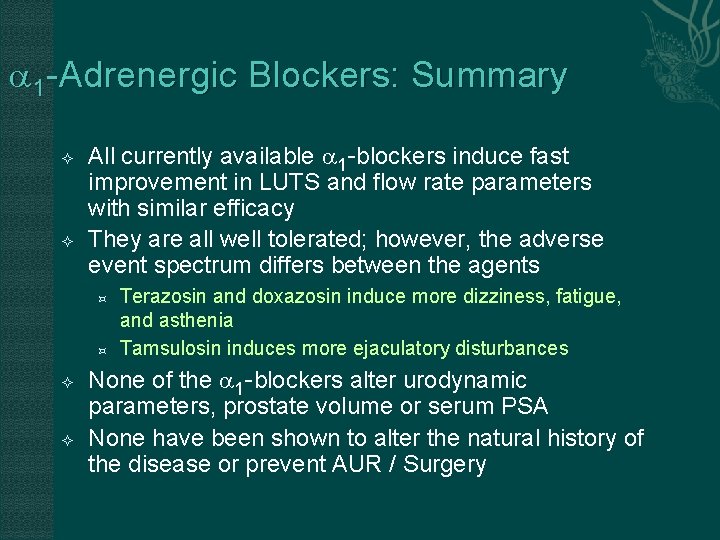
1 -Adrenergic Blockers: Summary All currently available 1 -blockers induce fast improvement in LUTS and flow rate parameters with similar efficacy They are all well tolerated; however, the adverse event spectrum differs between the agents Terazosin and doxazosin induce more dizziness, fatigue, and asthenia Tamsulosin induces more ejaculatory disturbances None of the 1 -blockers alter urodynamic parameters, prostate volume or serum PSA None have been shown to alter the natural history of the disease or prevent AUR / Surgery
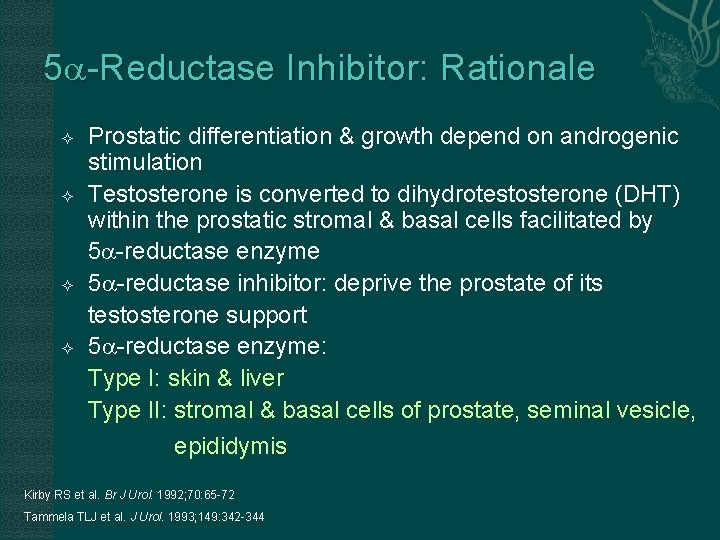
5 -Reductase Inhibitor: Rationale Prostatic differentiation & growth depend on androgenic stimulation Testosterone is converted to dihydrotestosterone (DHT) within the prostatic stromal & basal cells facilitated by 5 -reductase enzyme 5 -reductase inhibitor: deprive the prostate of its testosterone support 5 -reductase enzyme: Type I: skin & liver Type II: stromal & basal cells of prostate, seminal vesicle, epididymis Kirby RS et al. Br J Urol. 1992; 70: 65 -72 Tammela TLJ et al. J Urol. 1993; 149: 342 -344
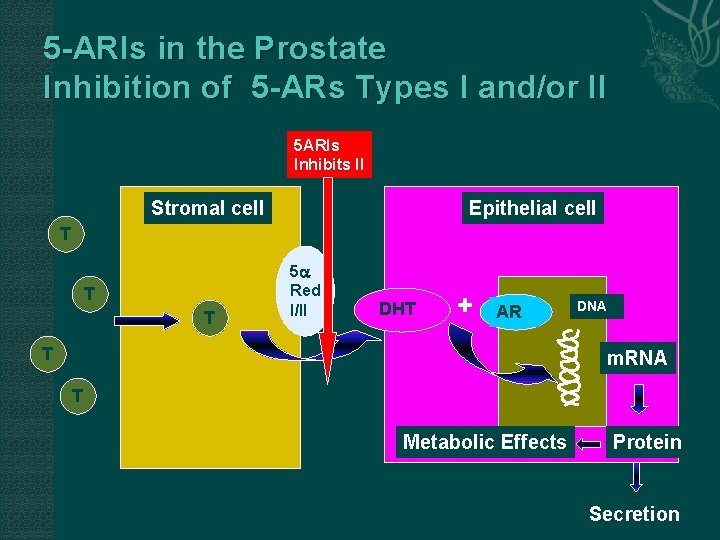
5 -ARIs in the Prostate Inhibition of 5 -ARs Types I and/or II 5 ARIs Inhibits II Stromal cell Epithelial cell T T T 5 Red I/II DHT + AR T DNA m. RNA T Metabolic Effects Protein Secretion
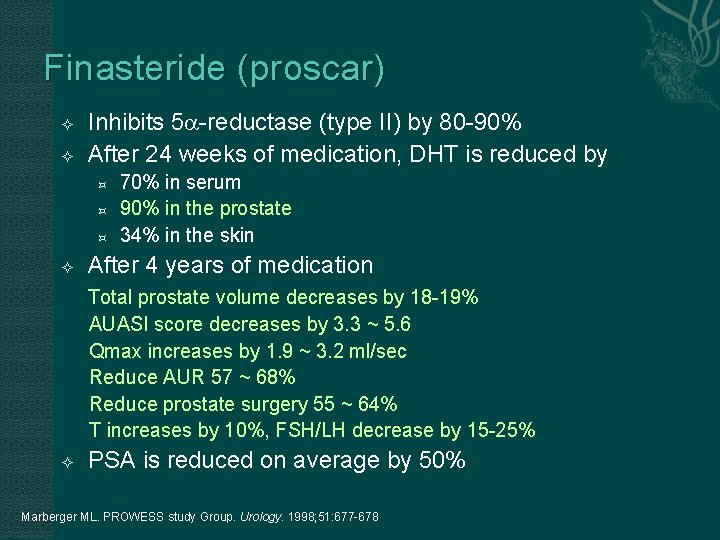
Finasteride (proscar) Inhibits 5 -reductase (type II) by 80 -90% After 24 weeks of medication, DHT is reduced by 70% in serum 90% in the prostate 34% in the skin After 4 years of medication Total prostate volume decreases by 18 -19% AUASI score decreases by 3. 3 ~ 5. 6 Qmax increases by 1. 9 ~ 3. 2 ml/sec Reduce AUR 57 ~ 68% Reduce prostate surgery 55 ~ 64% T increases by 10%, FSH/LH decrease by 15 -25% PSA is reduced on average by 50% Marberger ML. PROWESS study Group. Urology. 1998; 51: 677 -678
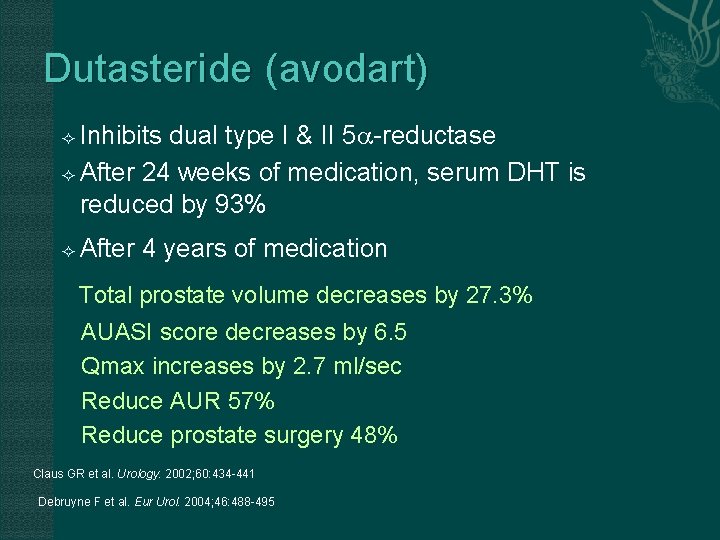
Dutasteride (avodart) Inhibits dual type I & II 5 -reductase After 24 weeks of medication, serum DHT is reduced by 93% After 4 years of medication Total prostate volume decreases by 27. 3% AUASI score decreases by 6. 5 Qmax increases by 2. 7 ml/sec Reduce AUR 57% Reduce prostate surgery 48% Claus GR et al. Urology. 2002; 60: 434 -441 Debruyne F et al. Eur Urol. 2004; 46: 488 -495
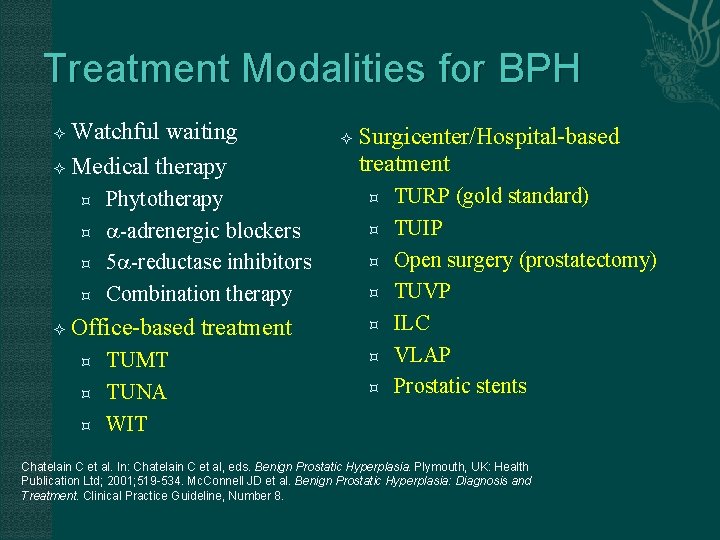
Treatment Modalities for BPH Watchful waiting Medical therapy Phytotherapy -adrenergic blockers 5 -reductase inhibitors Combination therapy Office-based treatment TUMT TUNA WIT Surgicenter/Hospital-based treatment TURP (gold standard) TUIP Open surgery (prostatectomy) TUVP ILC VLAP Prostatic stents Chatelain C et al. In: Chatelain C et al, eds. Benign Prostatic Hyperplasia. Plymouth, UK: Health Publication Ltd; 2001; 519 -534. Mc. Connell JD et al. Benign Prostatic Hyperplasia: Diagnosis and Treatment. Clinical Practice Guideline, Number 8.
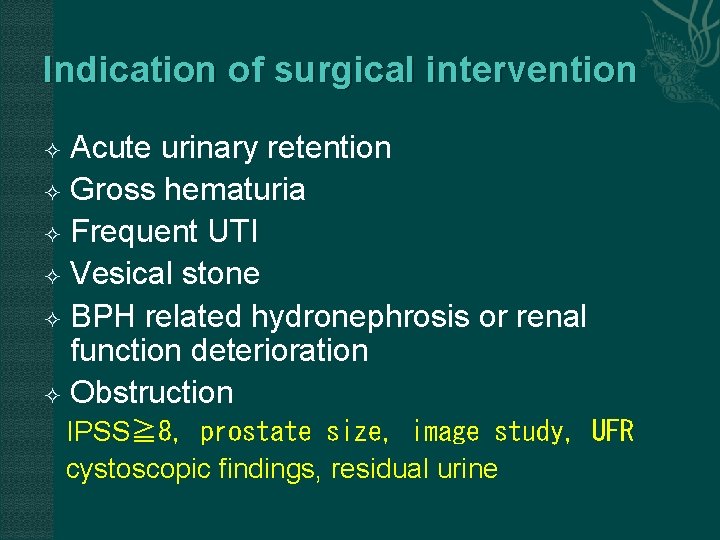
Indication of surgical intervention Acute urinary retention Gross hematuria Frequent UTI Vesical stone BPH related hydronephrosis or renal function deterioration Obstruction IPSS≧ 8, prostate size, image study, UFR cystoscopic findings, residual urine
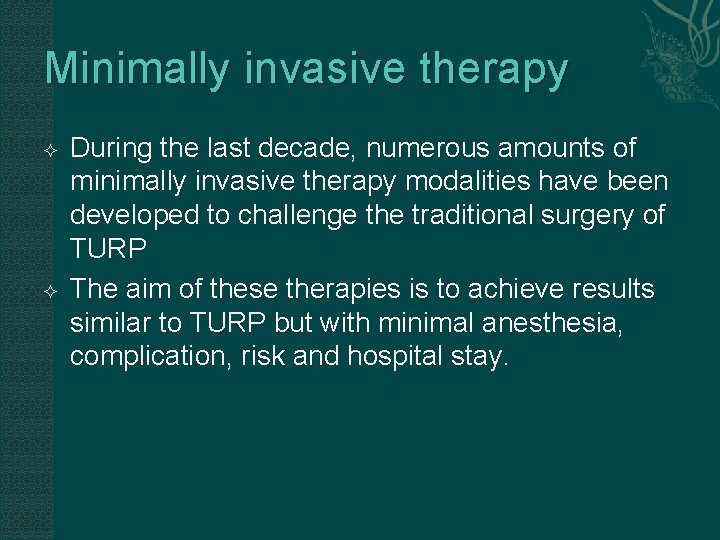
Minimally invasive therapy During the last decade, numerous amounts of minimally invasive therapy modalities have been developed to challenge the traditional surgery of TURP The aim of these therapies is to achieve results similar to TURP but with minimal anesthesia, complication, risk and hospital stay.
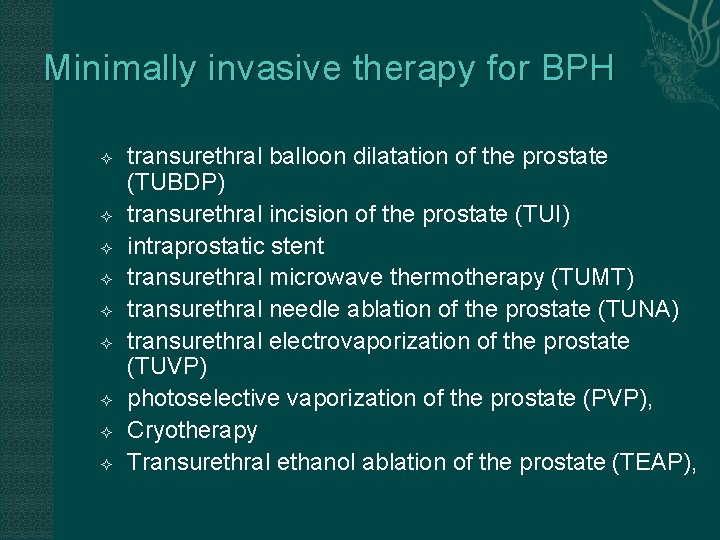
Minimally invasive therapy for BPH transurethral balloon dilatation of the prostate (TUBDP) transurethral incision of the prostate (TUI) intraprostatic stent transurethral microwave thermotherapy (TUMT) transurethral needle ablation of the prostate (TUNA) transurethral electrovaporization of the prostate (TUVP) photoselective vaporization of the prostate (PVP), Cryotherapy Transurethral ethanol ablation of the prostate (TEAP),
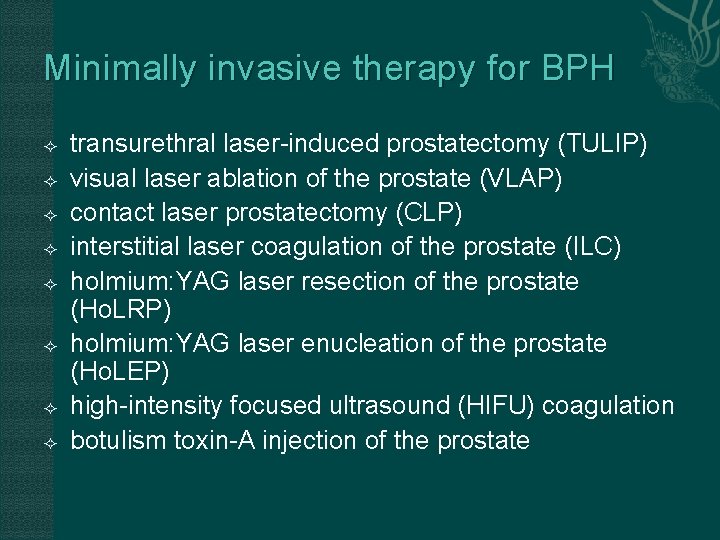
Minimally invasive therapy for BPH transurethral laser-induced prostatectomy (TULIP) visual laser ablation of the prostate (VLAP) contact laser prostatectomy (CLP) interstitial laser coagulation of the prostate (ILC) holmium: YAG laser resection of the prostate (Ho. LRP) holmium: YAG laser enucleation of the prostate (Ho. LEP) high-intensity focused ultrasound (HIFU) coagulation botulism toxin-A injection of the prostate
Conventional Surgical Therapy Transurethral resection of the prostate (TURP) Transurethral incision of the prostate Open simple prostatectomy
TURP “Gold standard” of surgical treatment for BPH 80~90% obstructive symptom improved 30% irritative symptom improved Low mortality rate 0. 2%
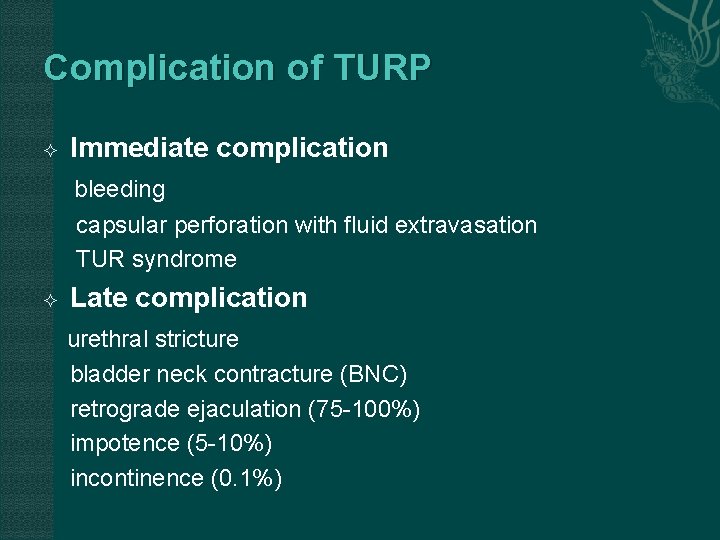
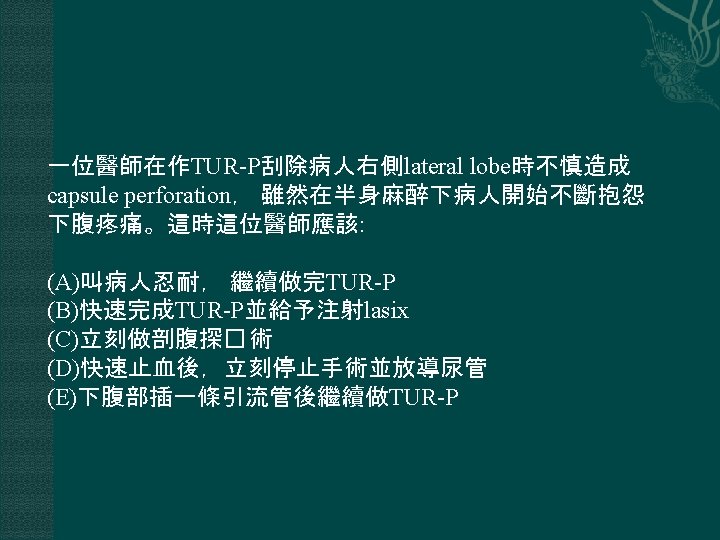
Complication of TURP Immediate complication bleeding capsular perforation with fluid extravasation TUR syndrome Late complication urethral stricture bladder neck contracture (BNC) retrograde ejaculation (75 -100%) impotence (5 -10%) incontinence (0. 1%)
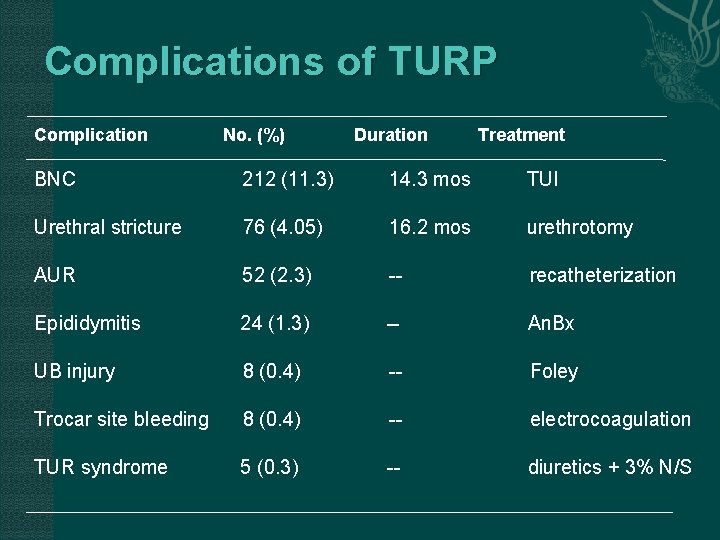
Complications of TURP Complication No. (%) Duration Treatment BNC 212 (11. 3) 14. 3 mos TUI Urethral stricture 76 (4. 05) 16. 2 mos urethrotomy AUR 52 (2. 3) -- recatheterization Epididymitis 24 (1. 3) -- An. Bx UB injury 8 (0. 4) -- Foley Trocar site bleeding 8 (0. 4) -- electrocoagulation TUR syndrome 5 (0. 3) -- diuretics + 3% N/S
Open Simple Prostatectomy “too large prostate” -- >100 gm Combined with bladder diverticulum or vesical stone surgery Suprapubic or retropubic method
Thank you
- Slides: 50