Benign Prostatic Hyperplasia BPH Urology Department Ain Shams
Benign Prostatic Hyperplasia BPH Urology Department Ain Shams University, 2009

BPH • Benign prostatic hyperplasia, BPH is an increase in size of the prostate gland that is so common as to be normal with advancing age. • Enlargement is due to increase in the number of glandular units, hyperplasia, with or without increase in size of muscular stroma, hypertrophy. • It is androgen dependent and BPH does not occur in castrated men. • It is unusual before the age of 45 and affects 90% of men by the age of 80. Urology Department Ain Shams University, 2009
BPH • There is little correlation between size of prostate and clinical complaints. • Although it is not life threatening, its clinical manifestation as lower urinary tract symptoms (LUTS) reduces the patient’s quality of life. • Troublesome LUTS can occur in up to 30% of men older than 60 years. • The risk of needing surgery for BPH increases with age and with the degree of clinical symptoms. Urology Department Ain Shams University, 2009
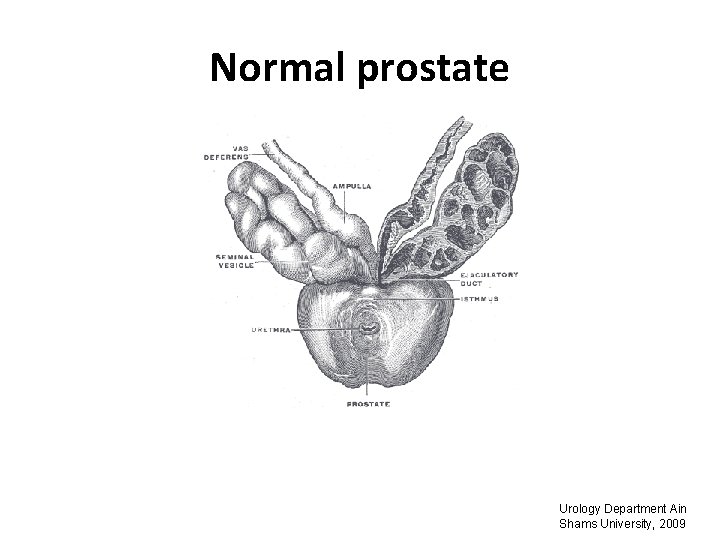
Normal prostate Urology Department Ain Shams University, 2009
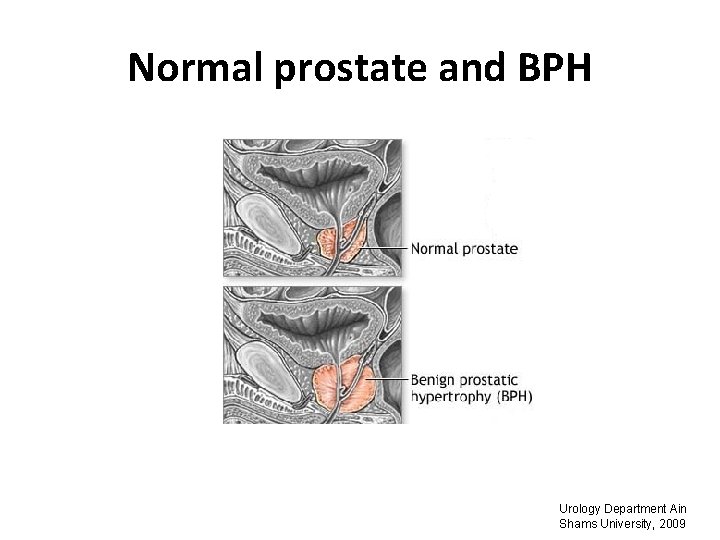
Normal prostate and BPH Urology Department Ain Shams University, 2009

BPH Gross appearance of hyperplastic prostatic tissue obstructing the prostatic urethra forming “lobes. ” A, Isolated middle lobe enlargement. B, Isolated lateral lobe enlargement. C, Lateral and middle lobe enlargement. D, Posterior commissural hyperplasia (median bar). Urology Department Ain Shams University, 2009

Clinical assessment of BPH Symptoms Storage symptoms: • Urinary frequency • Nocturia • Urinary urgency • Urge incontinence Voiding symptoms: • Hesitancy • Straining • Weak urinary stream • Interrupted or intermittent stream • Incomplete bladder emptying • Urinary retention. Urology Department Ain Shams University, 2009

Clinical assessment of BPH • Symptoms should be converted into score. • The International Prostate Symptoms Score (IPPS) is a quantitative and validated technique based on 7 questions. The results are summated to give a figure for the degree of trouble caused by the condition over the preceding month. Urology Department Ain Shams University, 2009

International Prostate Symptom Score, IPSS Incomplete emptying Over the last month, how often have you had a sensation of not emptying your bladder completely after you finished urinating? 0 point – Not at all 1 point – less than one time in 5 2 points - less than half the time 3 points - about half the time 4 points – more than half the time 5 points – almost always Frequency Over the past month, how often have you had the urge to urinate again less than two hours after you finished urinating? As above Intermittency Over the past month, how often have you found you stopped and started again several times when you urinated? As above Urgency Over the past month, how often have you found it difficult to postpone urination? As above Weak stream Over the past month, how often have you had a weak urinary stream? As above Straining Over the past month, how often have you had to push or strain to begin urination? As above Nocturia Over the past month, how many times did you most typically get up to urinate from the time you went to bed at night until the time you got up in the morning? 0 point - None 1 point - Once 2 points - Twice 3 points - Three times 4 points - Four times 5 points - Five or more times Quality of life due to urinary symptoms If you were to spend the rest of your life with your urinary condition the way it is now, how would you feel about that? 0 point – Delighted 1 point - pleased 2 points - mostly satisfied 3 points – about equqlly satisfied and unsatisfied 4 points – mostly dissatisfied 5 points – unhappy 6 points - terrible

Clinical assessment of BPH q. Three categories of symptom severity were described: • Mild (0 -7) • Moderate (8 -19) • Severe (20 -35) q. Evaluating symptom severity with a symptom score is important in selecting treatment and in monitoring the response to therapy. Urology Department Ain Shams University, 2009

Examination • Examination of the abdomen looking for a palpable (full) bladder. This may indicate chronic retention of urine. • Digital rectal examination (DRE) is an important examination in men with LUTS for two reasons. Firstly, it can determine the coexistence of prostatic carcinoma, and Secondly, the prostate size. Urology Department Ain Shams University, 2009
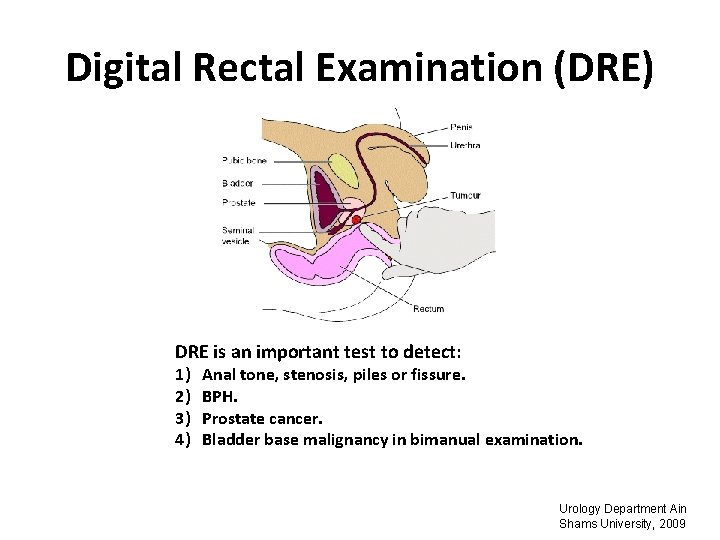
Digital Rectal Examination (DRE) DRE is an important test to detect: 1) 2) 3) 4) Anal tone, stenosis, piles or fissure. BPH. Prostate cancer. Bladder base malignancy in bimanual examination. Urology Department Ain Shams University, 2009

Laboratory investigations • Urinalysis: mandatory. • Creatinine measurement: BPH might cause hydronephrosis and renal Failure, so the measurement of creatinine is highly recommended. • Prostate-specific antigen (PSA) measurement: If DRE is suspicious for cancer. Urology Department Ain Shams University, 2009
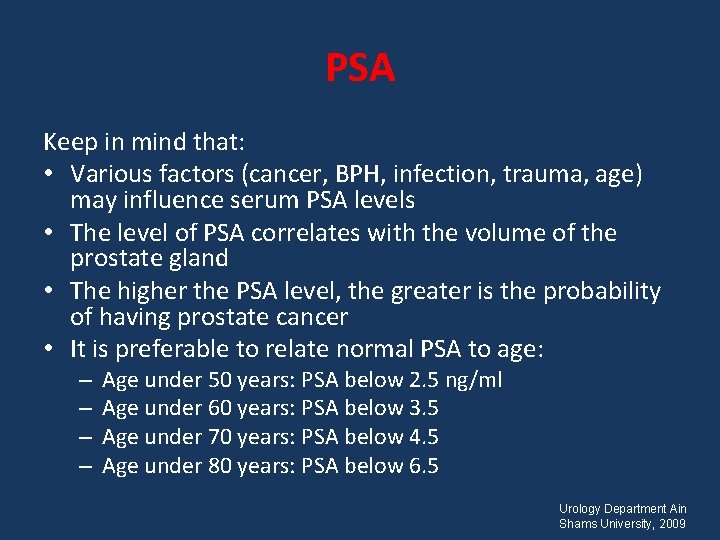
PSA Keep in mind that: • Various factors (cancer, BPH, infection, trauma, age) may influence serum PSA levels • The level of PSA correlates with the volume of the prostate gland • The higher the PSA level, the greater is the probability of having prostate cancer • It is preferable to relate normal PSA to age: – – Age under 50 years: PSA below 2. 5 ng/ml Age under 60 years: PSA below 3. 5 Age under 70 years: PSA below 4. 5 Age under 80 years: PSA below 6. 5 Urology Department Ain Shams University, 2009
Differential diagnosis • • • Carcinoma of prostate Bladder calculi Bladder tumors Urinary tract infection Detrusor muscle weakness and/or instability Chronic prostatitis Urology Department Ain Shams University, 2009
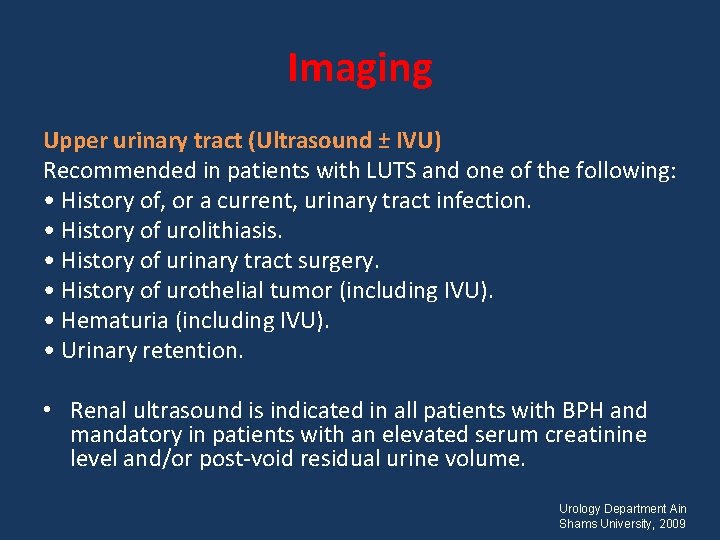
Imaging Upper urinary tract (Ultrasound ± IVU) Recommended in patients with LUTS and one of the following: • History of, or a current, urinary tract infection. • History of urolithiasis. • History of urinary tract surgery. • History of urothelial tumor (including IVU). • Hematuria (including IVU). • Urinary retention. • Renal ultrasound is indicated in all patients with BPH and mandatory in patients with an elevated serum creatinine level and/or post-void residual urine volume. Urology Department Ain Shams University, 2009
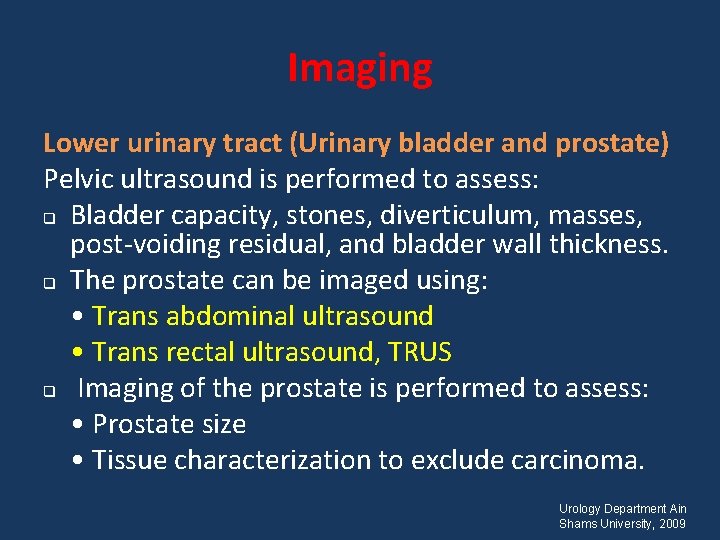
Imaging Lower urinary tract (Urinary bladder and prostate) Pelvic ultrasound is performed to assess: q Bladder capacity, stones, diverticulum, masses, post-voiding residual, and bladder wall thickness. q The prostate can be imaged using: • Trans abdominal ultrasound • Trans rectal ultrasound, TRUS q Imaging of the prostate is performed to assess: • Prostate size • Tissue characterization to exclude carcinoma. Urology Department Ain Shams University, 2009
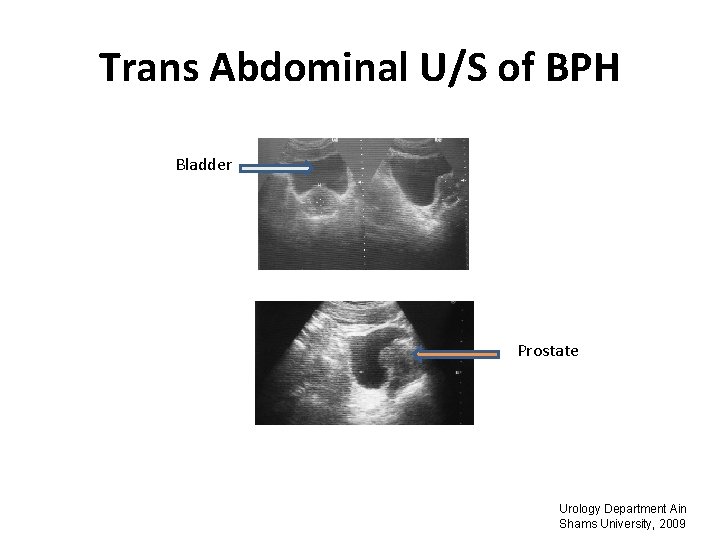
Trans Abdominal U/S of BPH Bladder Prostate Urology Department Ain Shams University, 2009
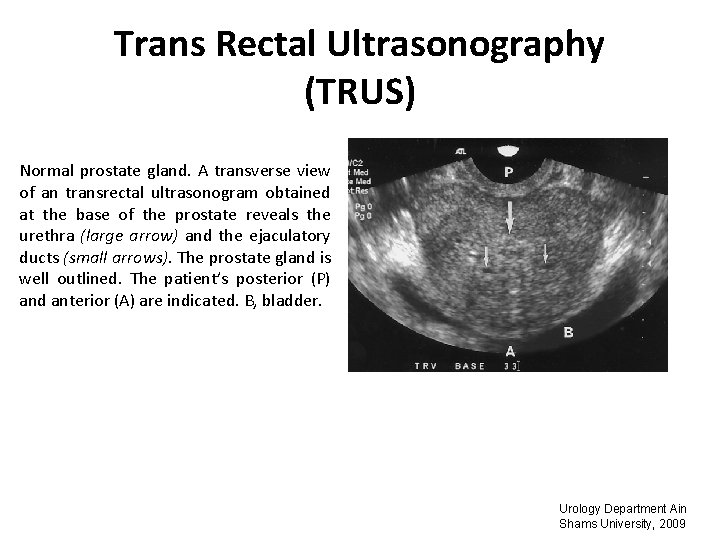
Trans Rectal Ultrasonography (TRUS) Normal prostate gland. A transverse view of an transrectal ultrasonogram obtained at the base of the prostate reveals the urethra (large arrow) and the ejaculatory ducts (small arrows). The prostate gland is well outlined. The patient’s posterior (P) and anterior (A) are indicated. B, bladder. Urology Department Ain Shams University, 2009
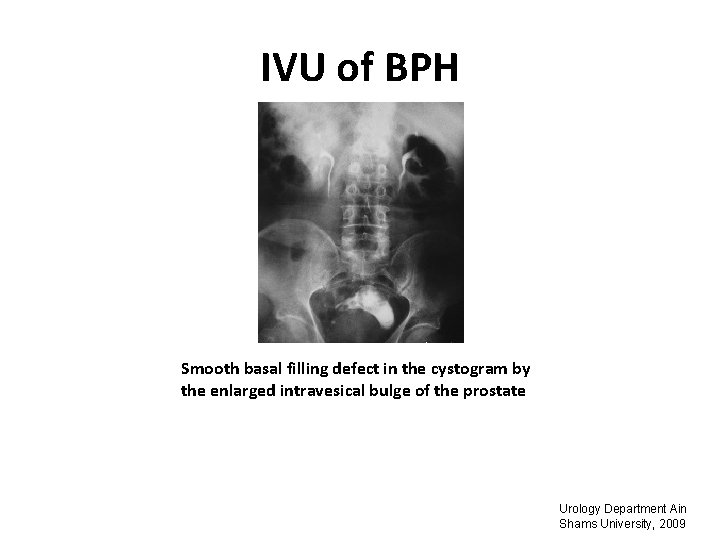
IVU of BPH Smooth basal filling defect in the cystogram by the enlarged intravesical bulge of the prostate Urology Department Ain Shams University, 2009
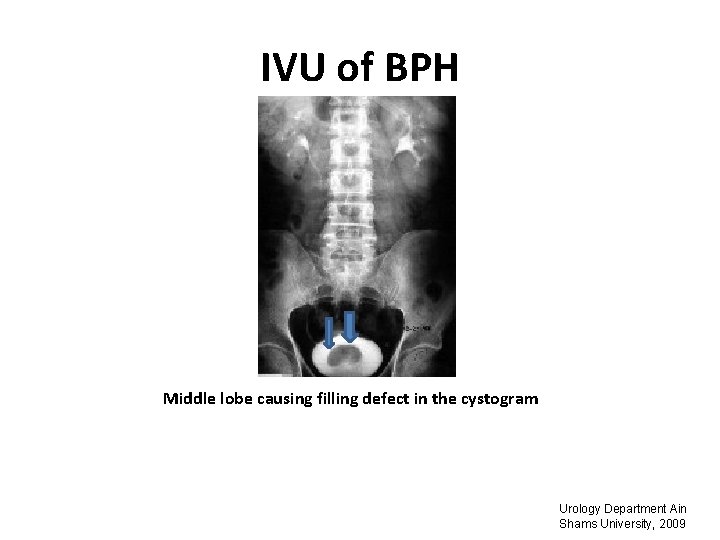
IVU of BPH Middle lobe causing filling defect in the cystogram Urology Department Ain Shams University, 2009
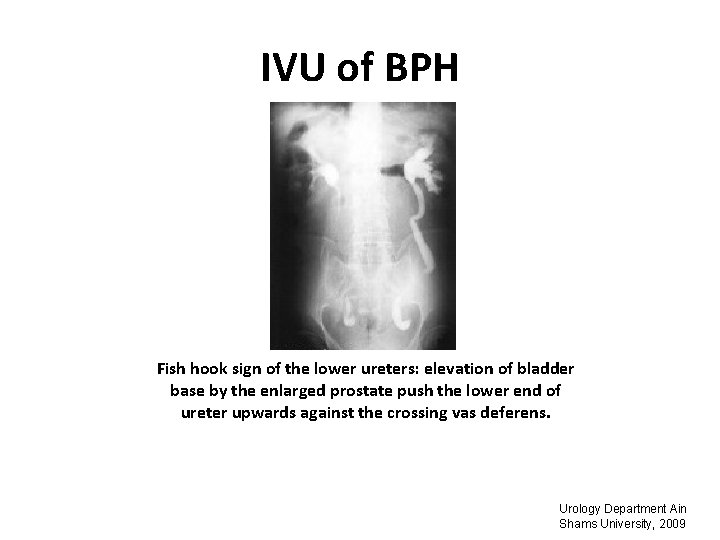
IVU of BPH Fish hook sign of the lower ureters: elevation of bladder base by the enlarged prostate push the lower end of ureter upwards against the crossing vas deferens. Urology Department Ain Shams University, 2009
Complications Bladder outlet obstruction can result in: • Recurrent UTI. • Impaired renal function. • Bladder calculi. • Hematuria. • Urinary retention. Urology Department Ain Shams University, 2009
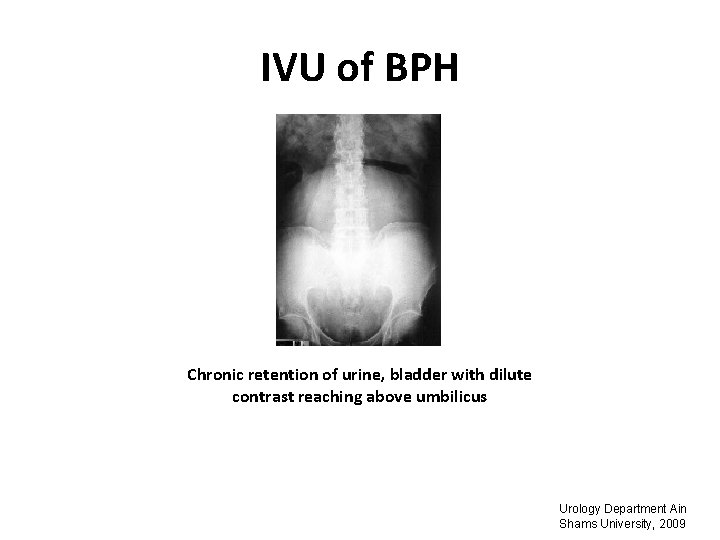
IVU of BPH Chronic retention of urine, bladder with dilute contrast reaching above umbilicus Urology Department Ain Shams University, 2009
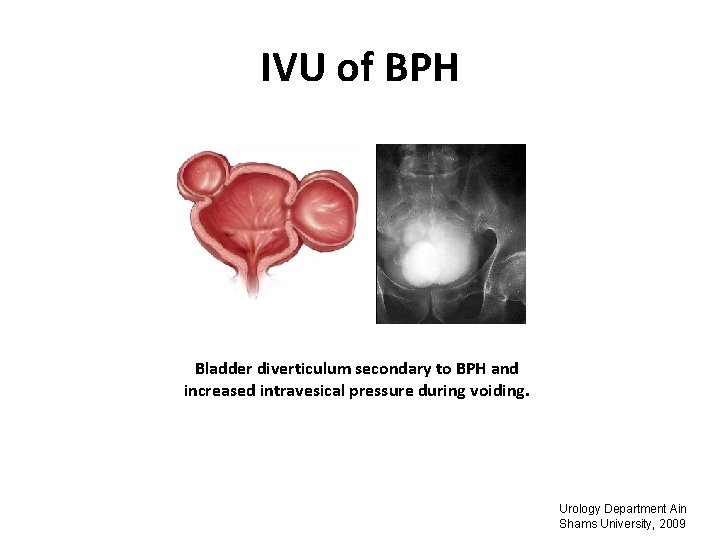
IVU of BPH Bladder diverticulum secondary to BPH and increased intravesical pressure during voiding. Urology Department Ain Shams University, 2009
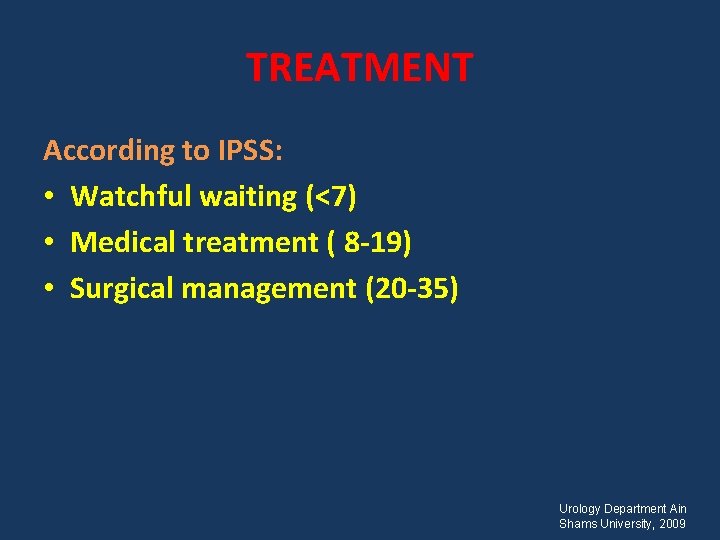
TREATMENT According to IPSS: • Watchful waiting (<7) • Medical treatment ( 8 -19) • Surgical management (20 -35) Urology Department Ain Shams University, 2009
Watchful waiting • Reassurance, periodic monitoring and lifestyle modifications can be used to optimize WW. • Increasing symptom score and post-void residual volumes are predictors of failure. Urology Department Ain Shams University, 2009

Medical treatment • 5 -alpha reductase inhibitors • Alpha-Adrenergic Blockers • Phytotherapeutic agents Urology Department Ain Shams University, 2009
Surgical management Indications for surgery • Bothersome LUTS refractory to medical management. • Refractory or recurrent urinary retention. • Recurrent hematuria refractory to medical treatment. • Renal insufficiency. • Bladder stones. • Increasing post-void residual volume despite medical treatment. Urology Department Ain Shams University, 2009
Surgical management q Transurethral resection of the prostate (TURP), transurethral incision of the prostate (TUIP) and open prostatectomy are the conventional surgical options. q Choice of surgical treatment • TURP comprises 95% of all surgical procedures and is the treatment of choice for prostates sized 30 -60 m. L. Intra- and postoperative complications are correlated with the size of the prostate and the length of the procedure. • Open prostatectomy is the treatment of choice for large glands (> 60 m. L), associated complications such as large bladder stones, or if excision of bladder diverticula is indicated. • TUIP is the surgical therapy of choice for men with prostates < 30 m. L without middle lobe enlargement. Urology Department Ain Shams University, 2009
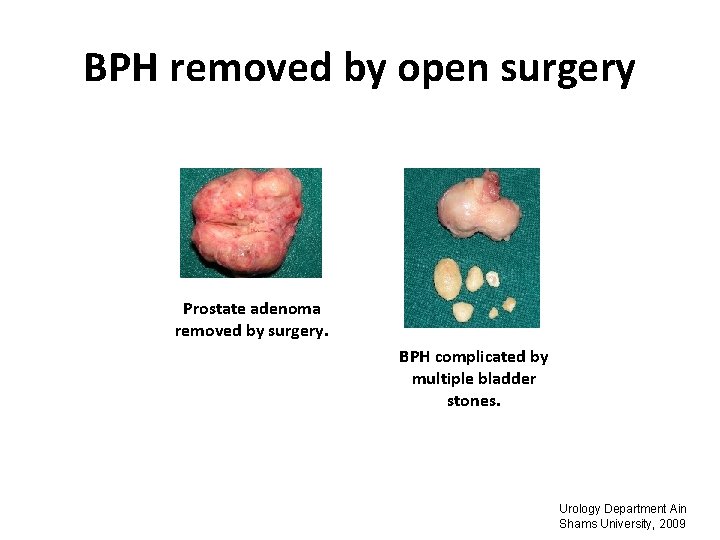
BPH removed by open surgery Prostate adenoma removed by surgery. BPH complicated by multiple bladder stones. Urology Department Ain Shams University, 2009
Non conventional modalities • Lasers • Transrectal high-intensity focused ultrasound (HIFU) • Trans Urethral Needle Ablation (TUNA) • Trans Urethral Microwave Therapy (TUMT) Urology Department Ain Shams University, 2009

Thank You
- Slides: 33