Benign diseases of the uterus BY AMIN ALAJLOUNI
Benign diseases of the uterus BY: AMIN ALAJLOUNI
Cervix This cervix is the lower extremity of the uterus Mainly consists of collagen fibers Ectocervix Is lined by non keratinized stratified squamous epithelium. Endocervix is lined by simple columnar epithelium. There is clear demarcation between these 2 parts by : squamocolumnar junction.

Benign cervical lesions Cervical ectropion: Presence of columnar epithelium on the ectocervix How does it appear? ? Circular, red area surrounding the external cervical os.
Influences for development: 3 p’s: 1 - puberty 2 - pills (contraceptive) 3 - pregnancy Note: large cervical ectropion may predispose to intermenstrual bleeding and post coital bleeding. Some females may present with excessive clear, odorless, mucus-like vaginal discharge.
treatment We can reduce the ectropion by stopping estrogen based contraceptive pills Cervical ablation (cryocautery) We have to do cervical and lower genital tract swabs to exclude (chlamydia and sexually transmitted infections) Also cervical cytology to rule out pre-malignant and malignant cervical lesions
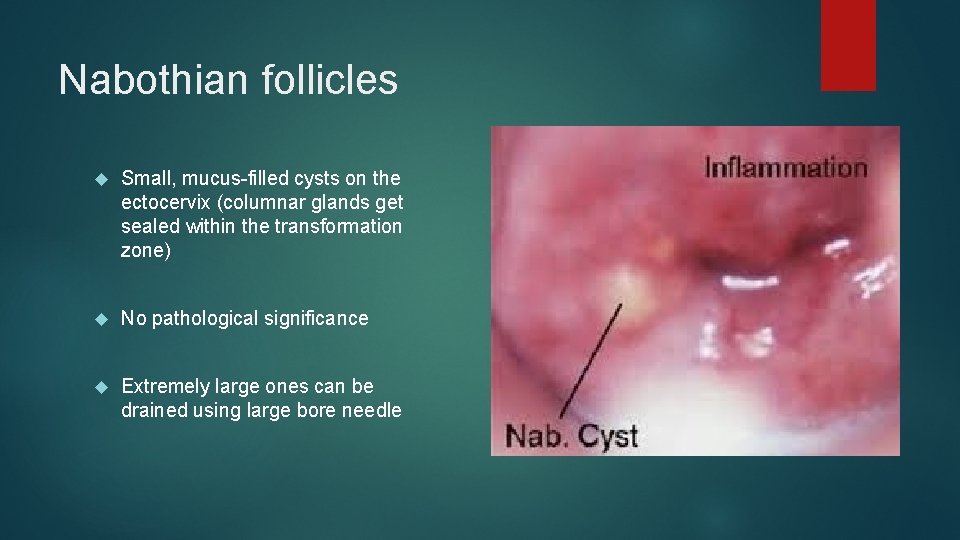
Nabothian follicles Small, mucus-filled cysts on the ectocervix (columnar glands get sealed within the transformation zone) No pathological significance Extremely large ones can be drained using large bore needle
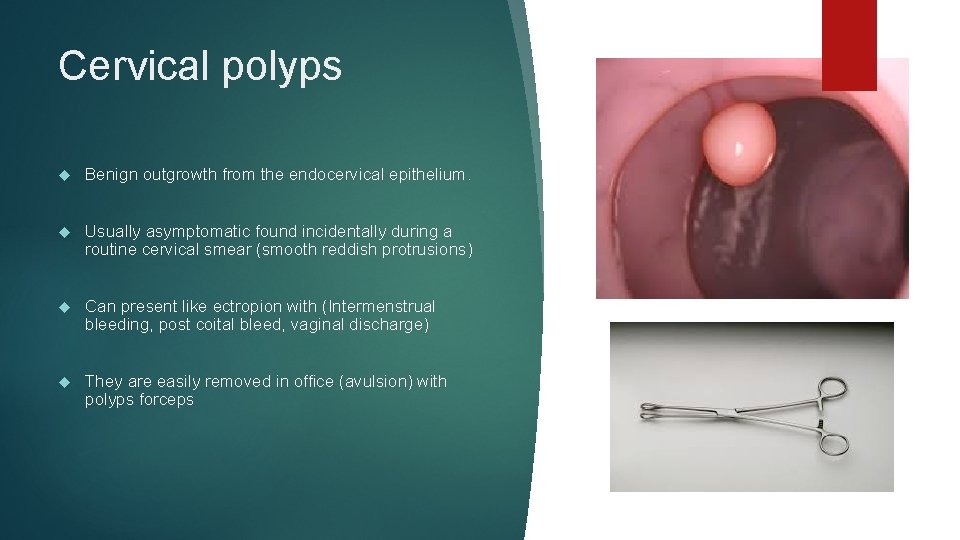
Cervical polyps Benign outgrowth from the endocervical epithelium. Usually asymptomatic found incidentally during a routine cervical smear (smooth reddish protrusions) Can present like ectropion with (Intermenstrual bleeding, post coital bleed, vaginal discharge) They are easily removed in office (avulsion) with polyps forceps
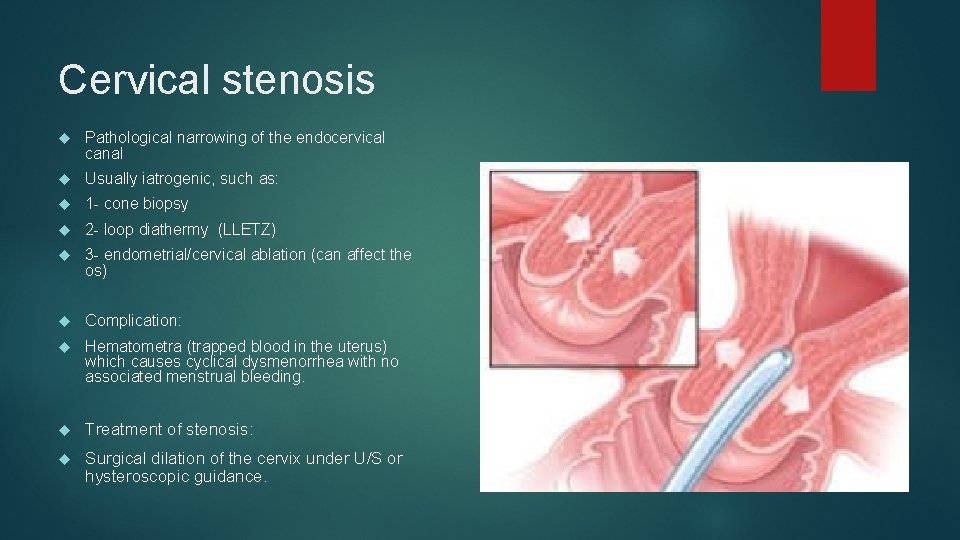
Cervical stenosis Pathological narrowing of the endocervical canal Usually iatrogenic, such as: 1 - cone biopsy 2 - loop diathermy (LLETZ) 3 - endometrial/cervical ablation (can affect the os) Complication: Hematometra (trapped blood in the uterus) which causes cyclical dysmenorrhea with no associated menstrual bleeding. Treatment of stenosis: Surgical dilation of the cervix under U/S or hysteroscopic guidance.
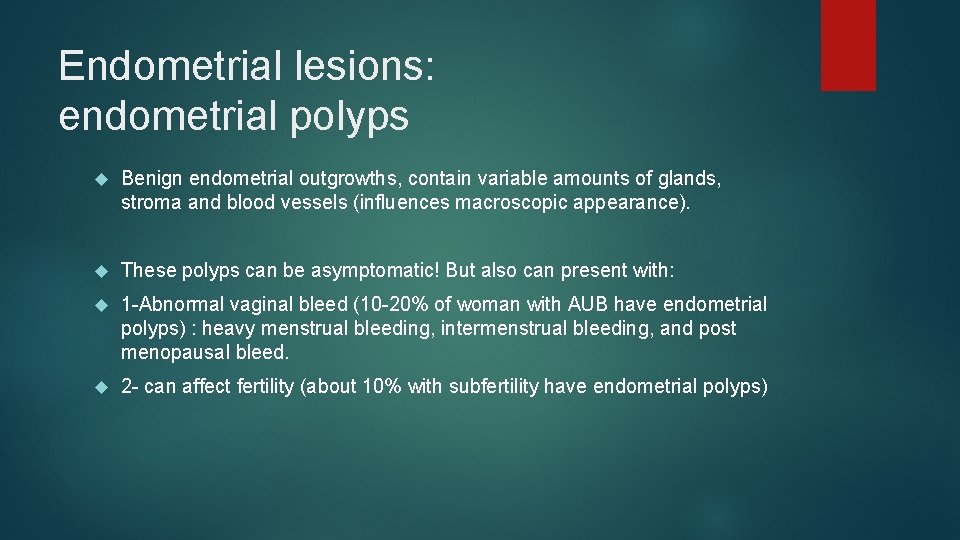
Endometrial lesions: endometrial polyps Benign endometrial outgrowths, contain variable amounts of glands, stroma and blood vessels (influences macroscopic appearance). These polyps can be asymptomatic! But also can present with: 1 -Abnormal vaginal bleed (10 -20% of woman with AUB have endometrial polyps) : heavy menstrual bleeding, intermenstrual bleeding, and post menopausal bleed. 2 - can affect fertility (about 10% with subfertility have endometrial polyps)
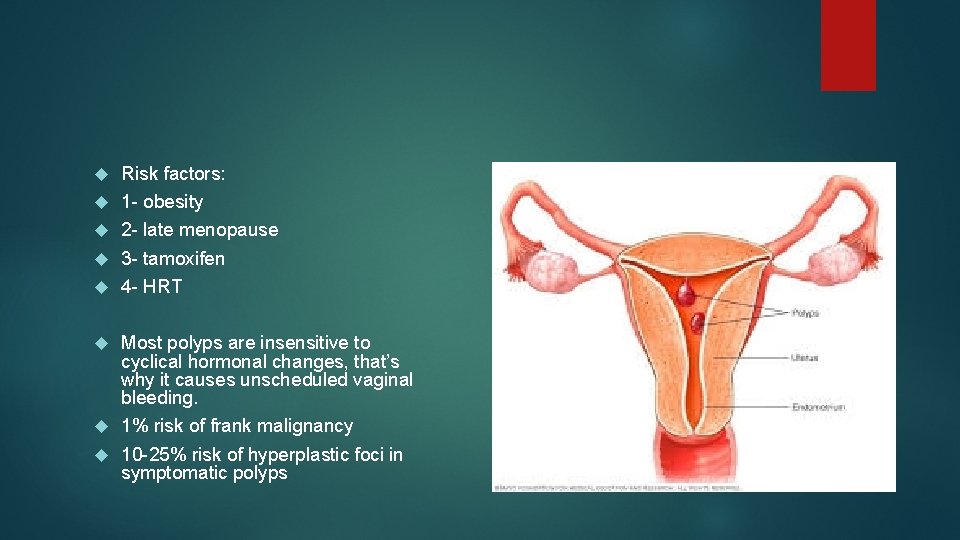
Risk factors: 1 - obesity 2 - late menopause 3 - tamoxifen 4 - HRT Most polyps are insensitive to cyclical hormonal changes, that’s why it causes unscheduled vaginal bleeding. 1% risk of frank malignancy 10 -25% risk of hyperplastic foci in symptomatic polyps
The risk of causing serious disease is increased after menopause and patients on tamoxifen Polyps can be: Pedunculated or sessile Single or multiple (. 5 -4 cm) in size
diagnosis Transvaginal ultrasound can be used Most accurate is hysteroscopy with saline infusion sonography (SIS) Once diagnosis is certain: Endometrial polyps removal is indicated! (polypectomy), why? 1 - to alleviate AUB symptoms 2 - optimize fertility 3 - exclude endometrial cancer and hyperplasia
Asherman syndrome Irreversible damage to the endometrial basal layer (single layer), which ruins the ability of normal endometrial regeneration. The uterus this undergoes fibrosis and adhesion formation. What causes this to happen? Usually it occurs after pregnancy if uterine infection occurs (endometritis), or after traumatic curettage of uterine cavity during management of miscarriage or PPH How to prevent? Adoption conservative surgical approaches for RPOC management, and preventing endometritis when we could.
Symptoms: 1 - reduced or absent menstrual shedding 2 - subfertility treatment? : Adhesiolysis hysteroscopically Note: treatment can be difficult and risks further uterine trauma
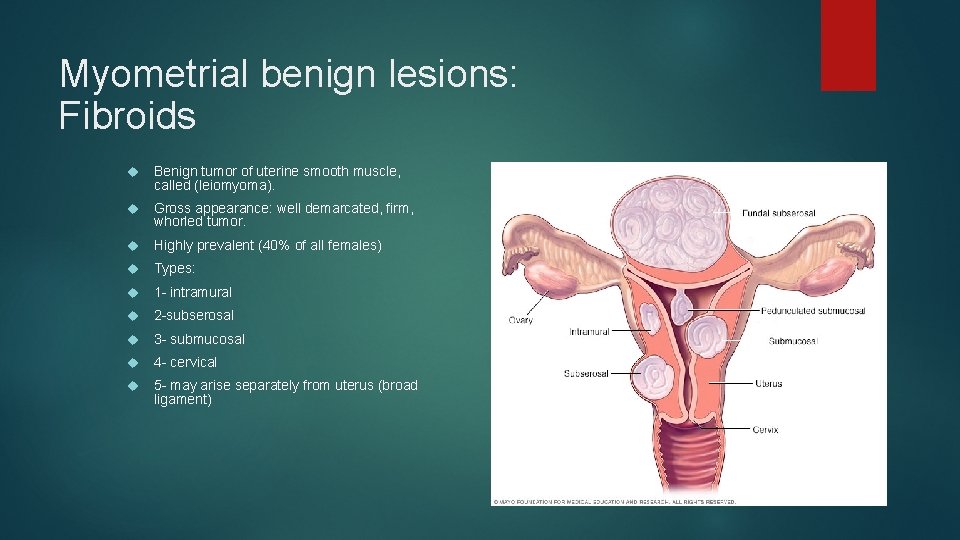
Myometrial benign lesions: Fibroids Benign tumor of uterine smooth muscle, called (leiomyoma). Gross appearance: well demarcated, firm, whorled tumor. Highly prevalent (40% of all females) Types: 1 - intramural 2 -subserosal 3 - submucosal 4 - cervical 5 - may arise separately from uterus (broad ligament)
Risk factors: 1 -nulliparity 2 -obesity 3 -positive family history 4 - African descent They usually INCREASE uterine sizeeeee and usually are multiple
Remember most fibroids are small and asymptomatic but some symptoms: 1 - AUB (HMB, IMB) 2 - Subfertility and reproductive failure 3 - Bulk effect on adjacent structures (like frequency) 4 - pressure and pain (when? ) 5 - abdominal distension 6 - bladder and bowel dysfunction
What to know about fibroids: 1 - estrogen dependent (increase in size in pregnancy, and shrink after menopause) 2 - more common with advanced reproductive age 3 - they can undergo degenerative changes (in response to outgrowing their blood supply) 4 - one of the commonest indications for hysterectomy 5 - most of them are asymptomatic 6 - on abdominal exam: a firm mass arising from the pelvis may be present. 7 - no treatment needed unless: symptomatic or proven, unexplained infertility.
Forms of fibroid degeneration: 1 - red: Hemorrhage and necrosis, usually presenting in mid 2 nd trimmest with acute pain! 2 - Hyaline: Asymptomatic softening and liquification of fibroid 3 - cystic: Asymptomatic central necrosis causing cystic spaces. Can initiate calcium deposition leading to calcification. 4 -malignant or sarcomatous: Rare (1: 350) incidence. High suspicion in (post menopausal, or rapidly increasing size of fibroid)
Why does subfertility occur? Mechanical distortion and fallopian tube occlusion by submucous fibroids Also they may prevent the implantation of a fertilized ovum. That’s why removal of submucous fibroids can enhance fertility and improve IVF outcomes.
Pregnancy Once pregnancy is established, the risk of miscarriage is not increased. In late pregnancy: Fibroids located in cervix or lower uterine segment may cause and abnormal lie. After delivery: Risk of PPH goes up due to inefficient uterine contractions
Examination findings suggestive of fibroids Anemia Palpable or visible abdominal mass First enlarged smooth uterus on bimanual examination.
diagnosis History and physical examination are important in diagnosis CBC should be done. Abdominopelvic ultrasound (transvaginal and abdominal u/s) MRI (to demarcate morphology, size and location prior to radiological or surgical intervention)
treatment Medical: The main types for HMB are: 1 -levonorgestrel IUS 2 -tranexamic acid 3 - mefenamic acid 4 - combined oral contraceptives These 4 tend to be ineffective in the presence of submucous fibroids and enlarged uterus palpated abdominally (more than 12 wks gestation)
The only effective medical treatments in that case are: Injectable Gn. RH or ulipristal acetate (oral SPRM) SPRM do not cause menopausal symptoms However neither of these 2 is a viable long-term treatment option, because when u stop the drug ovarian function returns and the fibroid regrows.
Surgical treatment: We use hysteroscopic approaches to cut submucous fibroids. In bulky fibroids with pressure symptoms or in refractory HMB are options will be: 1 - laparoscopic or open myomectomy (preserves fertility): A small risk of uncontrolled bleeding is present, which could lead to hysterectomy. 2 - hysterectomy
In both of these surgical procedures we can use Gn. RH agonist for 3 months prior to surgery, to reduce size and vascularity of the fibroid. This will enable us to: 1 - do a low transverse incision rather than midline 2 - do a vaginal rather than abdominal hysterectomy 3 - faster recovery 4 - lower risk of bleeding and complications The only down side it’ll make the surgery harder by obscuring tissue planes around the fibroid
Radiological treatment: Uterine artery embolization: A-Entering through the femoral artery then embolizing particles into the uterine arteries, which induces infarction and degeneration of fibroids B- patient should be admitted overnight because of severe pain and should be given opiate analgesia. C- this can be complicated with potential ovarian failure!!!! So you have to counsel the patient on that especially if patient wishes to retain her fertility D- one third of females will require further medical, radiological or surgical intervention within 5 years.
- Slides: 28