Benign and malign diseases of Stomach Prof Dr
Benign and malign diseases of Stomach Prof. Dr. Öge TAŞCILAR
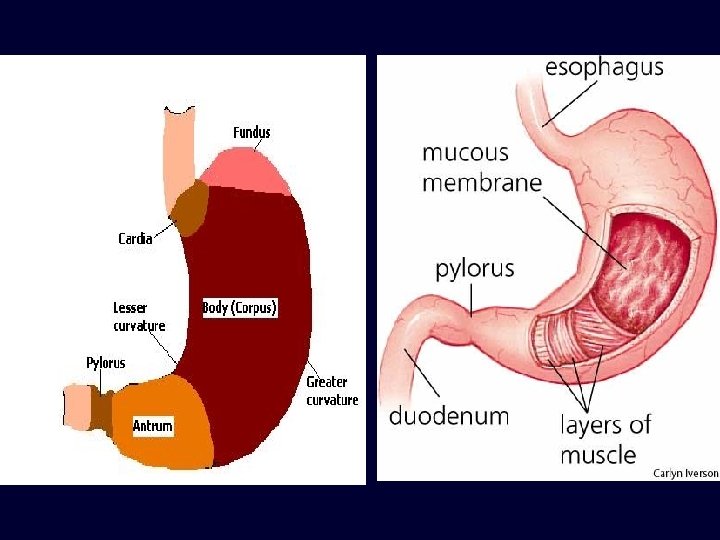
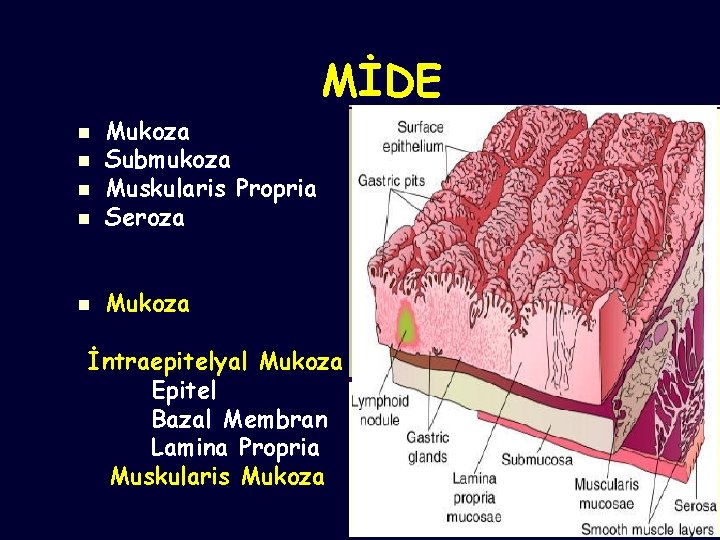
MİDE n Mukoza Submukoza Muskularis Propria Seroza n Mukoza n n n İntraepitelyal Mukoza Epitel Bazal Membran Lamina Propria Muskularis Mukoza
MİDE n Fonksiyon: Alınan gıdaların sindirimi ve emilimi n Reseptif relaksasyon ve gastrik adaptasyon n İntragastrik basınç düşer. n n 100 cc-------1500 cc
MİDE n Mallory-Weiss Sendromu n n Kusma ile ÖG bileşke mukoza submukoza yırtık ve kanama Endoskopi Alkol, diyabet, gebelik, üremi, Tam kat olursa Booerhaave sendromu
MİDE n n n n Bezoarlar Midede oluşan yabancı cisimler. Trikobezoar-fitobezoar Mide operasyonu sonrası Antrumun öğütücü işlevinin kaybolması HCL azalmasına bağlı Candida Albicans bezoar Tanı: Radyoloji-endoskopi Tedavi: Endoskopik-Cerrahi
MİDE n n n n n Menetrier Hastalığı Hipertrofik mukozal gastropati Fundus ve korpusta dev rugalar Foveolar hiperplazi Hipoklorhidri ve Hipoalbüminemi 50> erkekler Epigastrik ağrı, kilo kaybı, (özellikle protein) , kanama, diare, ödem Medikal tedavi PPI Destek tedavisi Çok ciddi olgularda rezeksiyon
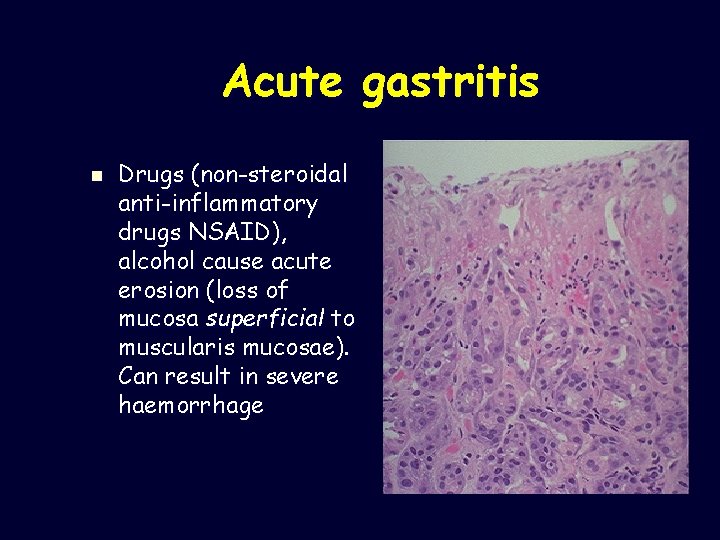
Acute gastritis n Drugs (non-steroidal anti-inflammatory drugs NSAID), alcohol cause acute erosion (loss of mucosa superficial to muscularis mucosae). Can result in severe haemorrhage
Chronic gastritis ABC n A – autoimmune(associated with vitamin B 12 malabsorption (pernicious anaemia) n B – bacterial (helicobacter) n C – chemical(bile reflux, drugs)
Autoimmune chronic gastritis Autoantibodies to gastric parietal cells n Hypochlorhydria/achlorhydria n n Loss of gastric intrinsic factor leads to malabsorption of vitamin B 12 with macrocytic, megaloblastic anaemia
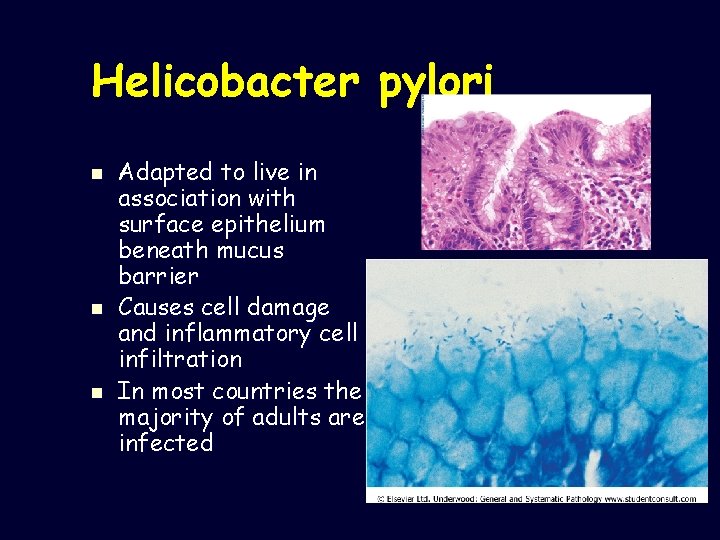
Helicobacter pylori n n n Adapted to live in association with surface epithelium beneath mucus barrier Causes cell damage and inflammatory cell infiltration In most countries the majority of adults are infected
Peptic ulcer disease n n A surface breach of mucosal lining of GI tract occurring as a result of acid and pepsin attack Sites: – – – Duodenum (DU) Stomach (GU) Oesophagus Gastro-enterostomy stoma Related to ectopic gastric mucosa (e. g. in Meckel’s diverticulum)
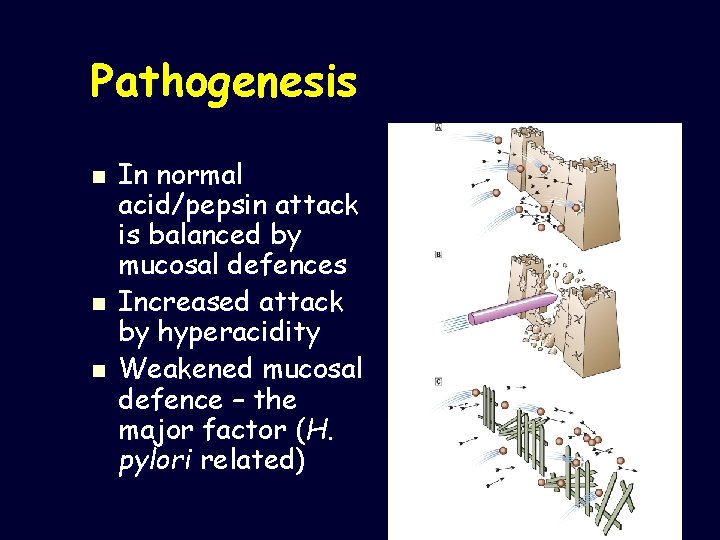
Pathogenesis n n n In normal acid/pepsin attack is balanced by mucosal defences Increased attack by hyperacidity Weakened mucosal defence – the major factor (H. pylori related)
MİDE n n n Duodenal Ülser: Duodenal HCO 3 sekresyonu azalmış Gece asit sekresyonu artmış Duodenal asit yükü artmış Bazal ve postprandial gastrin artmış Tamamına yakın HP gastrit saptanmıştır.
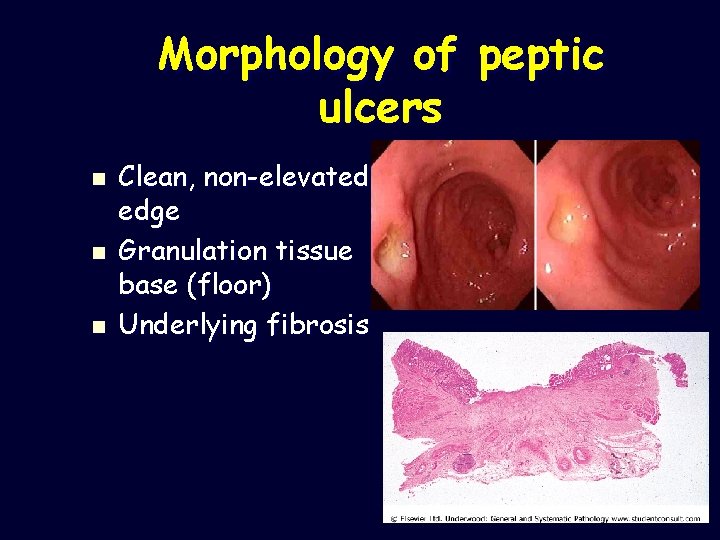
Morphology of peptic ulcers n n n Clean, non-elevated edge Granulation tissue base (floor) Underlying fibrosis
MİDE n n n n Klinik: Yanıcı, kemirici, açlık ağrısı. Epigastrium Antiasit ve gıda ile hafifler. Mevsimsel bir ağrı. İlkbahar, sonbahar, stress dönemleri Penetre olursa ağrı özellikleri değişir.
MİDE n n n Anamnez, Radyoloji Endoskopi, biyopsi n Tedavi: n Medikal tedavi Antiasit Sükralfat H 2 blokör PPI Prostoglandin analogları
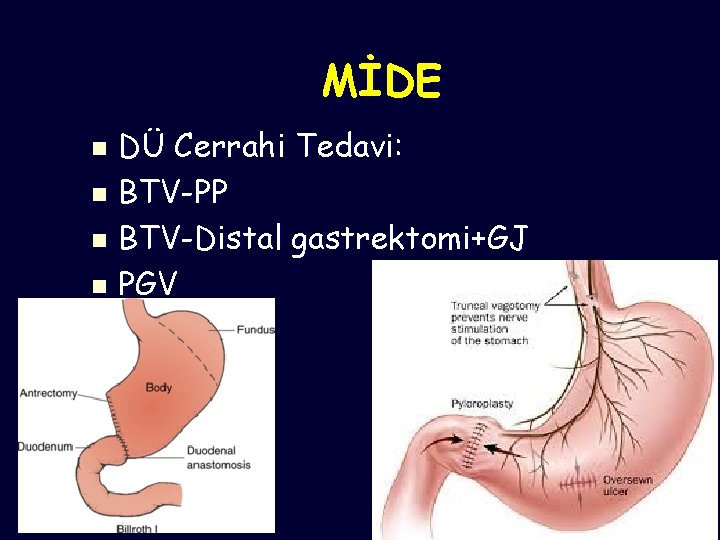
MİDE DÜ Cerrahi Tedavi: n BTV-PP n BTV-Distal gastrektomi+GJ n PGV n
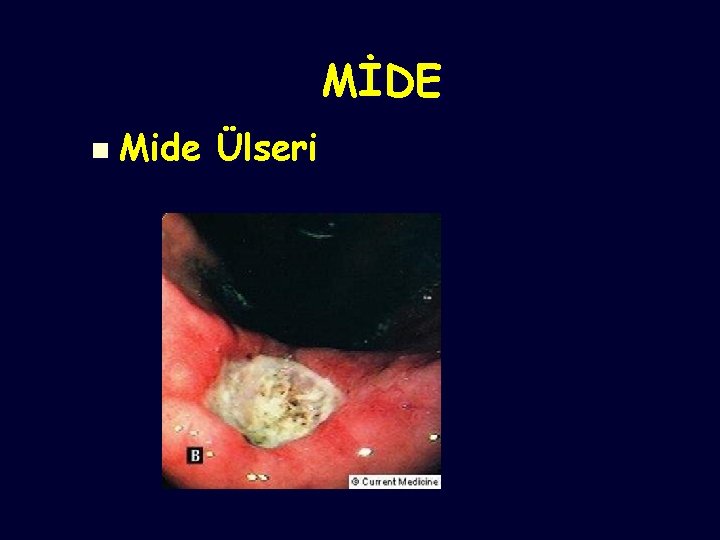
MİDE n Mide Ülseri
Complications of peptic ulcer n n n Perforation leading to peritonitis Haemorrhage by erosion of vessel in base Penetration of surrounding organ (liver/pancreas) Obstruction (by scarring) – pyloric stenosis (Cancer – rare event in true peptic ulcer)

NEOPLASMS OF STOMACH n. BENIGN__ 10% n. MALIGNANT__90% n. BENIGN n. Polyps n. Lipomas n. Leiomyomas
NEOPLASMS OF STOMACH MALIGNANT Adenocarcinoma 95% Lymphoma 4% Others 1% (sq. cell ca, angiosarcoma, carcinosarcoma, Gist)
Less common gastric neoplasms Gastrointestinal stromal tumour (GIST) n Lymphoma n Neuroendocrine (carcinoid) tumours n
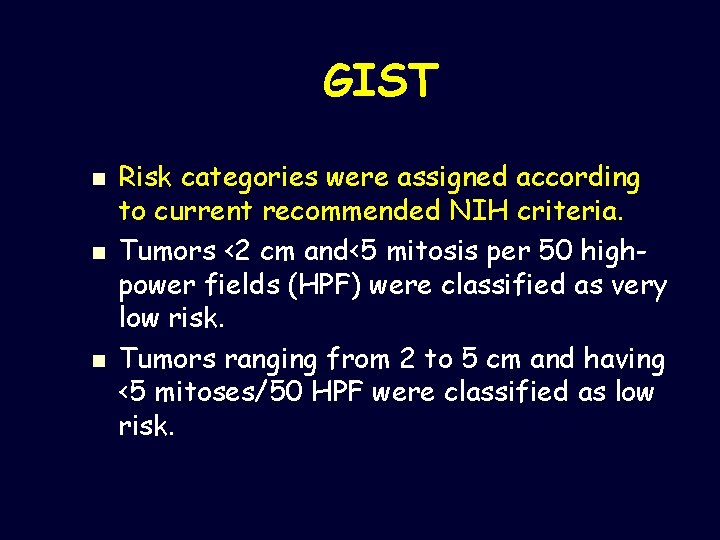
GIST n n n Risk categories were assigned according to current recommended NIH criteria. Tumors <2 cm and<5 mitosis per 50 highpower fields (HPF) were classified as very low risk. Tumors ranging from 2 to 5 cm and having <5 mitoses/50 HPF were classified as low risk.
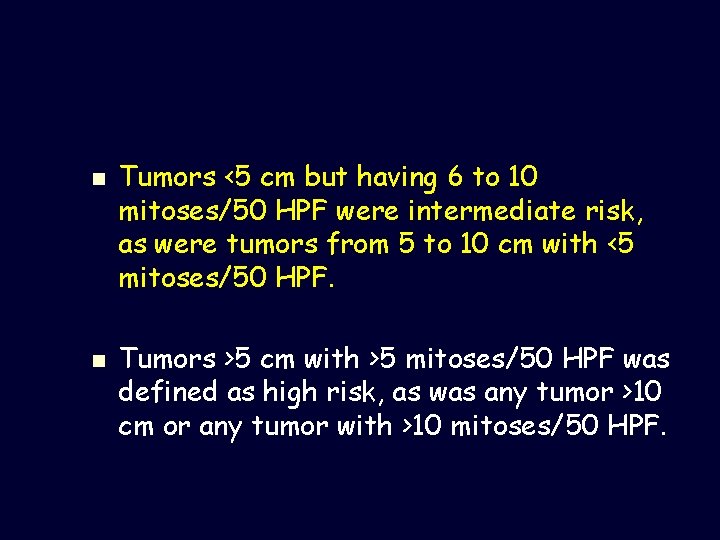
n n Tumors <5 cm but having 6 to 10 mitoses/50 HPF were intermediate risk, as were tumors from 5 to 10 cm with <5 mitoses/50 HPF. Tumors >5 cm with >5 mitoses/50 HPF was defined as high risk, as was any tumor >10 cm or any tumor with >10 mitoses/50 HPF.
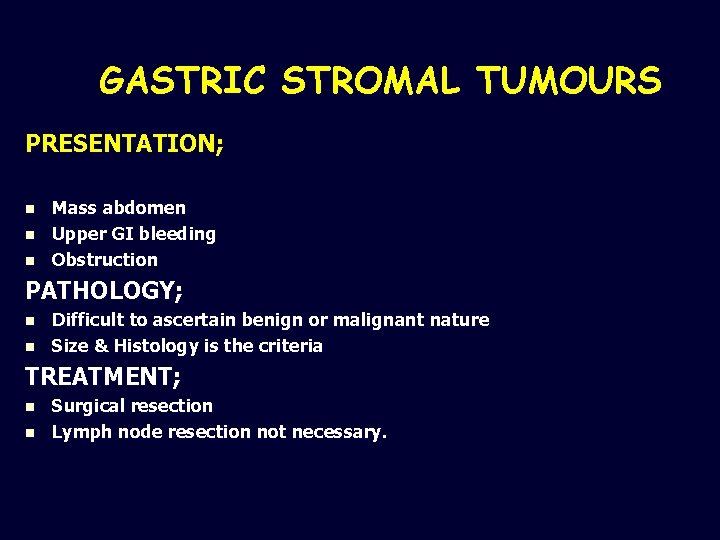
GASTRIC STROMAL TUMOURS PRESENTATION; n n n Mass abdomen Upper GI bleeding Obstruction PATHOLOGY; n n Difficult to ascertain benign or malignant nature Size & Histology is the criteria TREATMENT; n n Surgical resection Lymph node resection not necessary.
MİDE LENFOMA Non-Hodgkin Lenfoma(NHL) klasik olarak lenf nodlarından gelişir. n Ama NHL %30 olguda ekstranodal(Solid organ kaynaklı) olarak gelişebilir. n GI sistem tüm NHL %20 n
MİDE LENFOMA n GI lenfoma; oral kaviteden rektuma En sık; Mide n Sonra ince barsak n Kolon n Pankreas n
MİDE LENFOMA NHL, ekstranodal lenfoma ve GI lenfomanın en sık görülen tipi diffüz B hücre lenfoması. n MALT lenfoma n Burkitt lenfoma n T- hücre lenfoma n
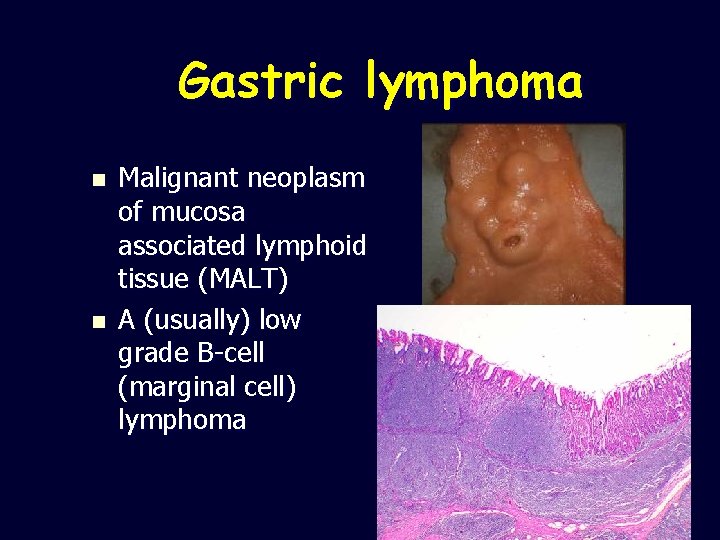
Gastric lymphoma n n Malignant neoplasm of mucosa associated lymphoid tissue (MALT) A (usually) low grade B-cell (marginal cell) lymphoma
MİDE LENFOMA n n n Antrum ve distal mide Proksimal yerleşebilir. Karın ağrısı, erken doyma Bulantı, kusma, halsizlik Abdominal dolgunluk Kronik kan kaybı, anemi melena
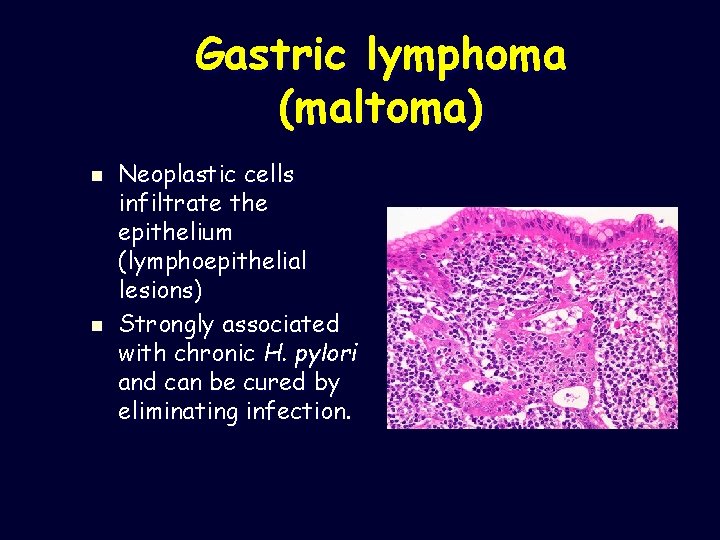
Gastric lymphoma (maltoma) n n Neoplastic cells infiltrate the epithelium (lymphoepithelial lesions) Strongly associated with chronic H. pylori and can be cured by eliminating infection.
MİDE LENFOMA n n n n n Tedavi HP tedavi edilmeli. Bir zamanlar cerrahi Şimdi Konservatif, bazı olgularda cerrahi Low grade lenfoma(MALT) HP eradikasyonu, KRT, High Grade: Antihelikobakter tedaviye cevap vermeyen erken evre PGL, ileri evre lenfoma, diffüz büyük hücreli lenfoma ise cerrahi tedavi KT-RT Residual hastalık: KT-cerrahi
Neuroendocrine tumours Carcinoids are tumours of resident neuroendocrine cells in gastric glands n Usually seen in context of chronic atrophic gastritis (driven by gastrin) n Clinical behaviour variable n
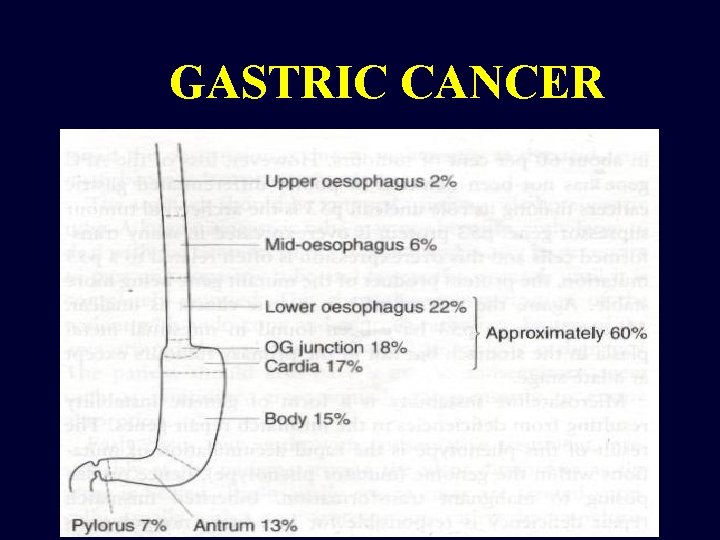
GASTRIC CANCER
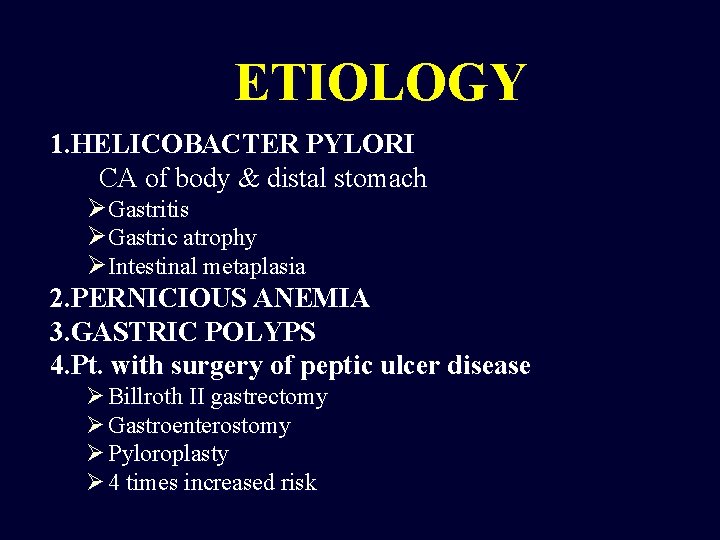
ETIOLOGY 1. HELICOBACTER PYLORI CA of body & distal stomach Ø Gastritis Ø Gastric atrophy Ø Intestinal metaplasia 2. PERNICIOUS ANEMIA 3. GASTRIC POLYPS 4. Pt. with surgery of peptic ulcer disease Ø Billroth II gastrectomy Ø Gastroenterostomy Ø Pyloroplasty Ø 4 times increased risk
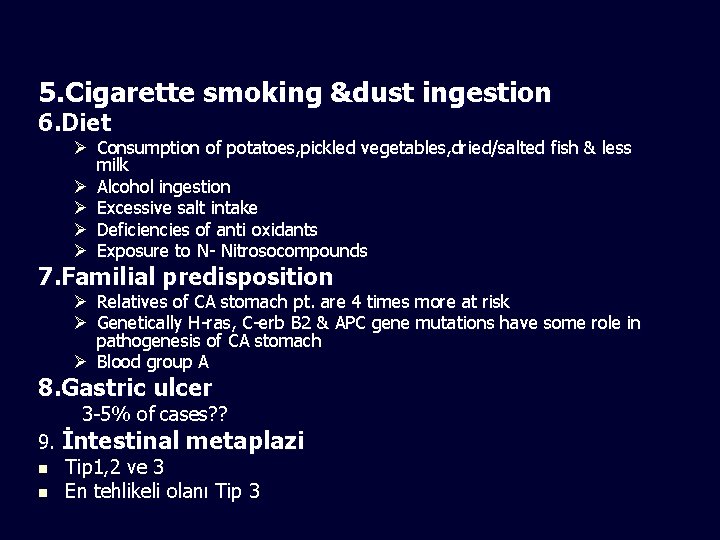
5. Cigarette smoking &dust ingestion 6. Diet Ø Consumption of potatoes, pickled vegetables, dried/salted fish & less milk Ø Alcohol ingestion Ø Excessive salt intake Ø Deficiencies of anti oxidants Ø Exposure to N- Nitrosocompounds 7. Familial predisposition Ø Relatives of CA stomach pt. are 4 times more at risk Ø Genetically H-ras, C-erb B 2 & APC gene mutations have some role in pathogenesis of CA stomach Ø Blood group A 8. Gastric ulcer 3 -5% of cases? ? 9. İntestinal metaplazi n Tip 1, 2 ve 3 n En tehlikeli olanı Tip 3
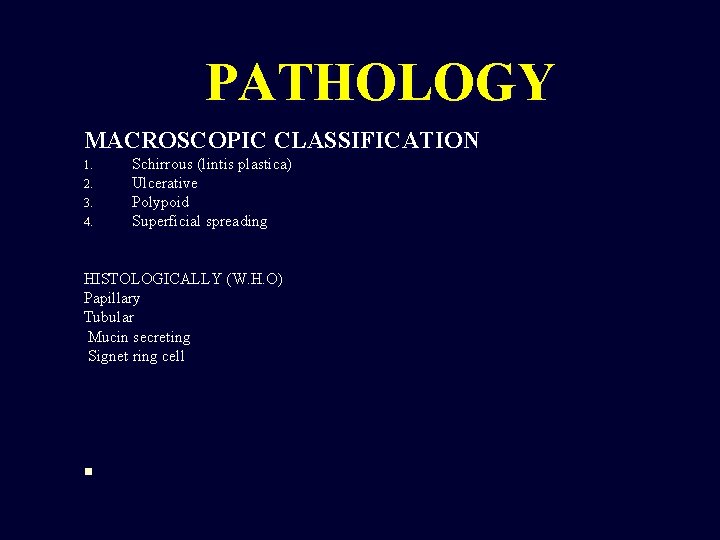
PATHOLOGY MACROSCOPIC CLASSIFICATION 1. 2. 3. 4. Schirrous (lintis plastica) Ulcerative Polypoid Superficial spreading HISTOLOGICALLY (W. H. O) Papillary Tubular Mucin secreting Signet ring cell n
Clinical Features GASTRIC CANCER n n n n Early feeling of fullness after meal Bloating , distention Vomiting Pallor – iron deficiency anemia due to tumour bleed Dysphygia –epigastric fullness or vomiting due to obstrution of gastric outlet Epigastric mass – ¼ of cases Non metastatic effects ; thrombophlebitis Deep venous thrombosis ( by affecting thrombotic & haemostatic mechanism)
n Ascites n Jaundice n Trosier sign(virchows node) n Sister mary joseph nodule n krukenberg tumour n Blummer Shelf
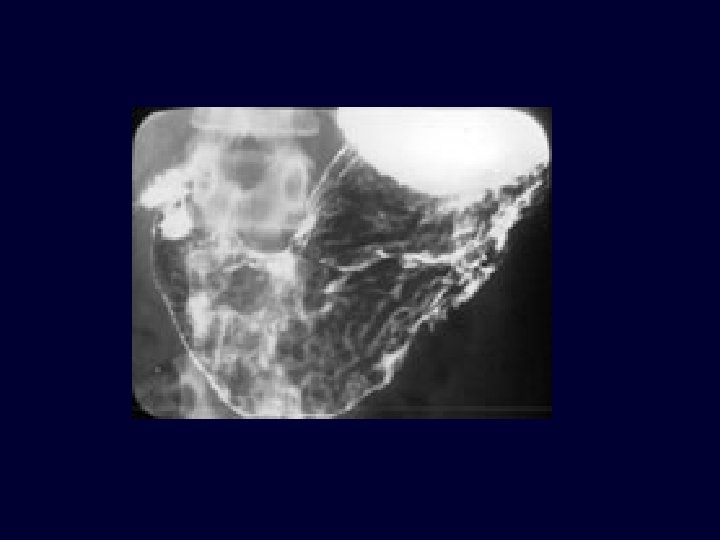
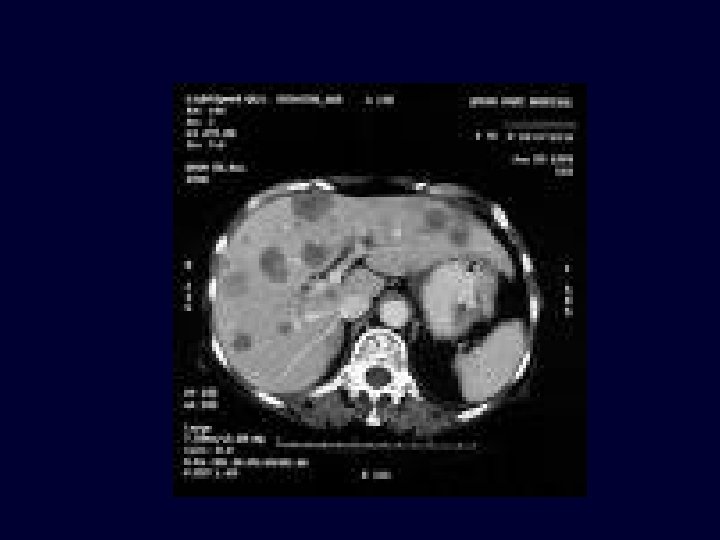
INVESTIGATIONS 1. 2. 3. 4. 5. 6. 7. 8. 9. BLOOD COMPLETE EXAM. ------ Anemia STOOL EXAM. --- for occult blood in ½ of pts. CARCINOEMBRYONIC (CEA) LEVEL--- elevated in 65% of cases GASTRIC JUICE ANALYSIS--- 20% are achlorhydric after maximal stimulation DOUBLE CONTRAST BARIUM MEAL--- mucosal irregularities and to assess the size , shape, margins of lesions GASTROSCOPY & BIOPSY---minimum of 6 biopsies for accuracy --- brush cytology C. T. SCAN ENDOSCOPIC USG LAPAROSCOPY
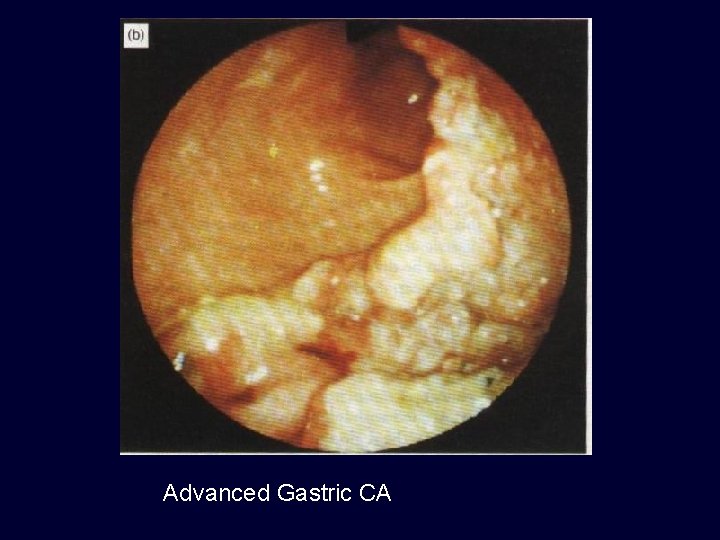
Advanced Gastric CA

Advanced Gastric CA
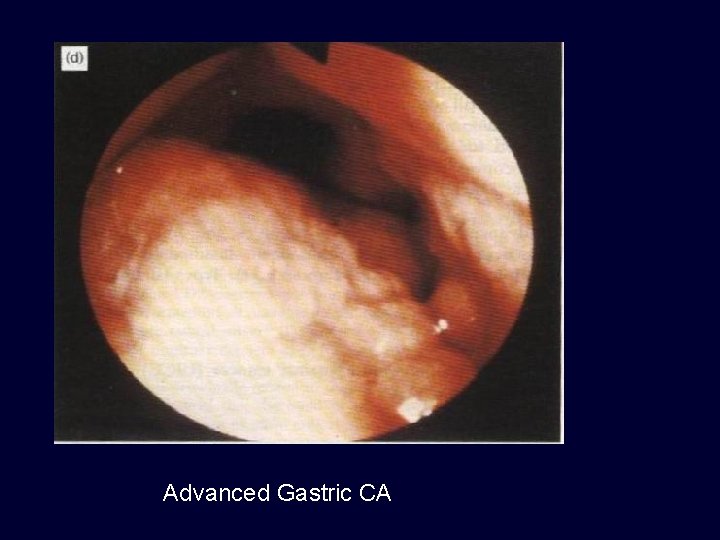
Advanced Gastric CA

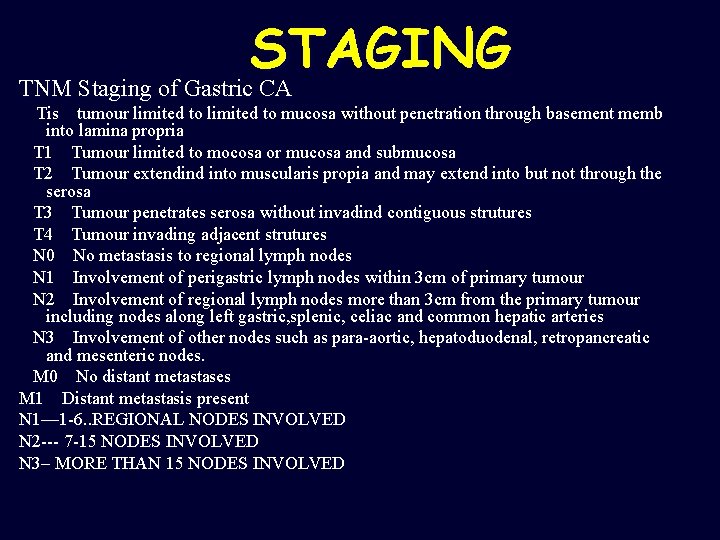
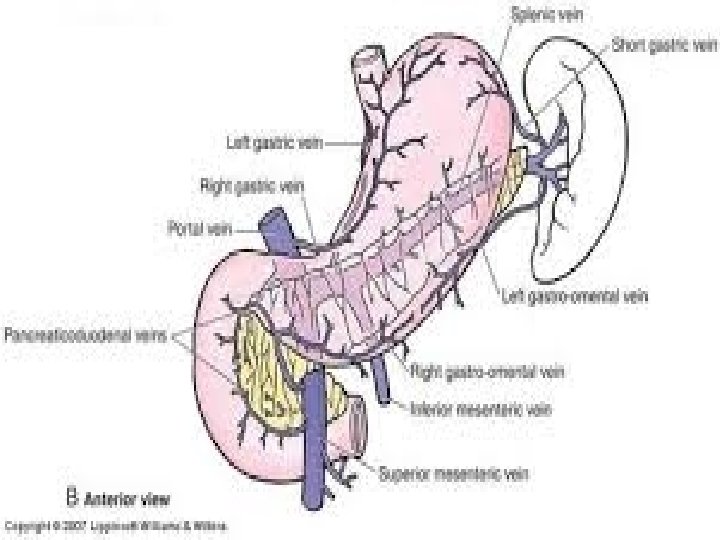
STAGING TNM Staging of Gastric CA Tis tumour limited to mucosa without penetration through basement memb into lamina propria T 1 Tumour limited to mocosa or mucosa and submucosa T 2 Tumour extendind into muscularis propia and may extend into but not through the serosa T 3 Tumour penetrates serosa without invadind contiguous strutures T 4 Tumour invading adjacent strutures N 0 No metastasis to regional lymph nodes N 1 Involvement of perigastric lymph nodes within 3 cm of primary tumour N 2 Involvement of regional lymph nodes more than 3 cm from the primary tumour including nodes along left gastric, splenic, celiac and common hepatic arteries N 3 Involvement of other nodes such as para-aortic, hepatoduodenal, retropancreatic and mesenteric nodes. M 0 No distant metastases M 1 Distant metastasis present N 1— 1 -6. . REGIONAL NODES INVOLVED N 2 --- 7 -15 NODES INVOLVED N 3– MORE THAN 15 NODES INVOLVED
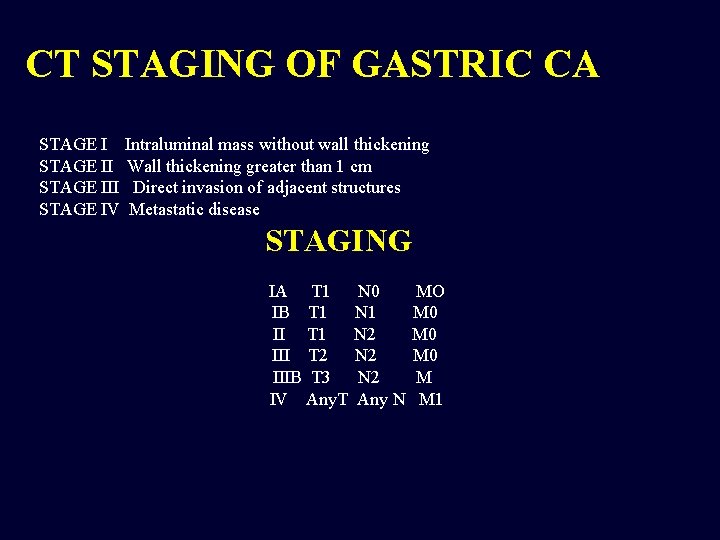
CT STAGING OF GASTRIC CA STAGE I Intraluminal mass without wall thickening STAGE II Wall thickening greater than 1 cm STAGE III Direct invasion of adjacent structures STAGE IV Metastatic disease STAGING IA T 1 N 0 MO IB T 1 N 1 M 0 II T 1 N 2 M 0 III T 2 N 2 M 0 IIIB T 3 N 2 M IV Any. T Any N M 1
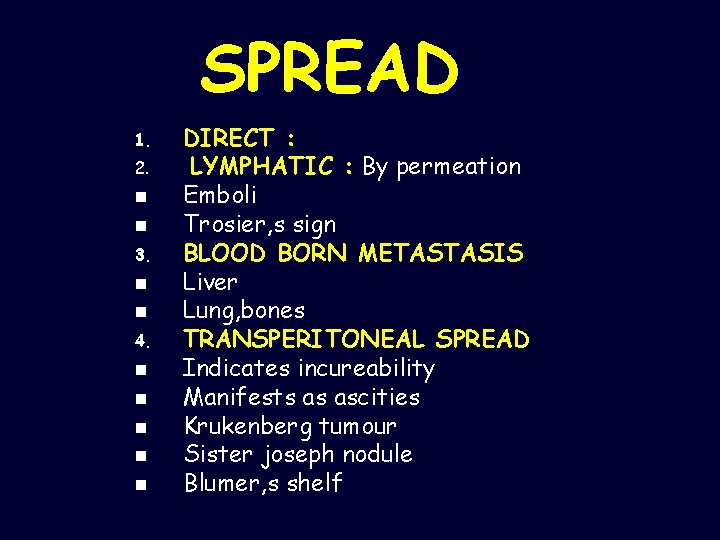
SPREAD 1. 2. n n 3. n n 4. n n n DIRECT : LYMPHATIC : By permeation Emboli Trosier, s sign BLOOD BORN METASTASIS Liver Lung, bones TRANSPERITONEAL SPREAD Indicates incureability Manifests as ascities Krukenberg tumour Sister joseph nodule Blumer, s shelf

TREATMENT 1. SURGERY; --curative --palliative 2. RADIOTHERAPY 3. CHEMOTHERAPY SURGICAL TREATMENT n n n Incurable disease is not subjected to radical surgery Evidence of incureability are; --Haematogenous spread --Distant peritoneal involvement --N 4 nodal disease & disease beyond N 4 nodes --Fixation to structures that can not be removed Cure resection should be considered in remaining pts.
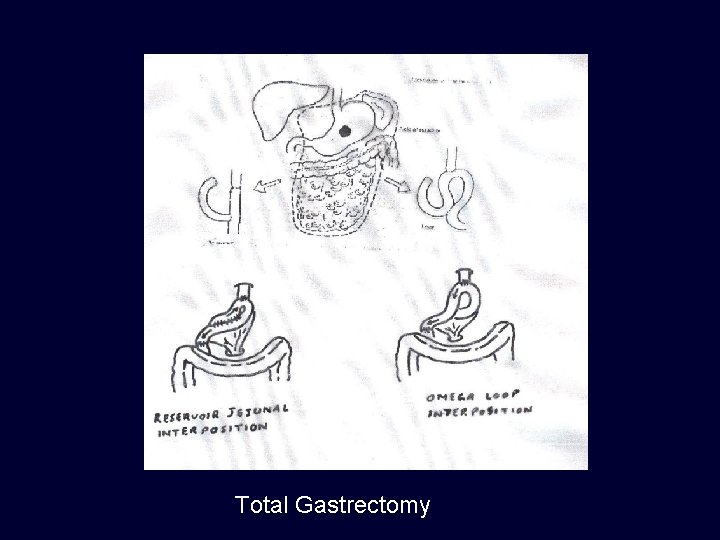
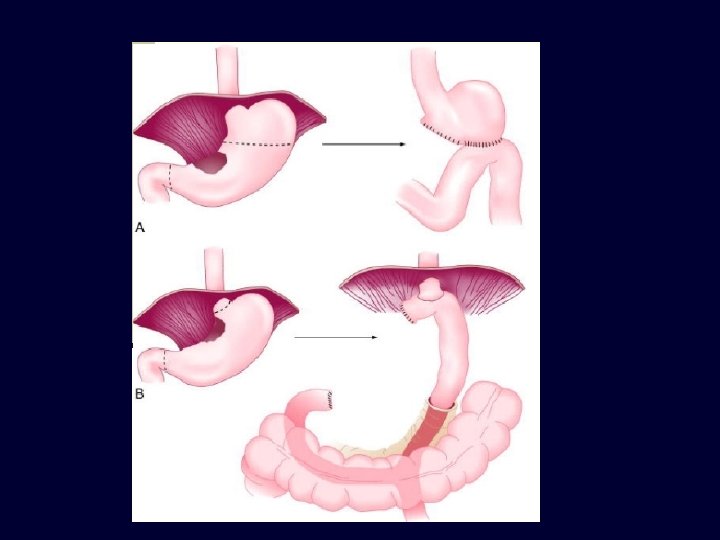
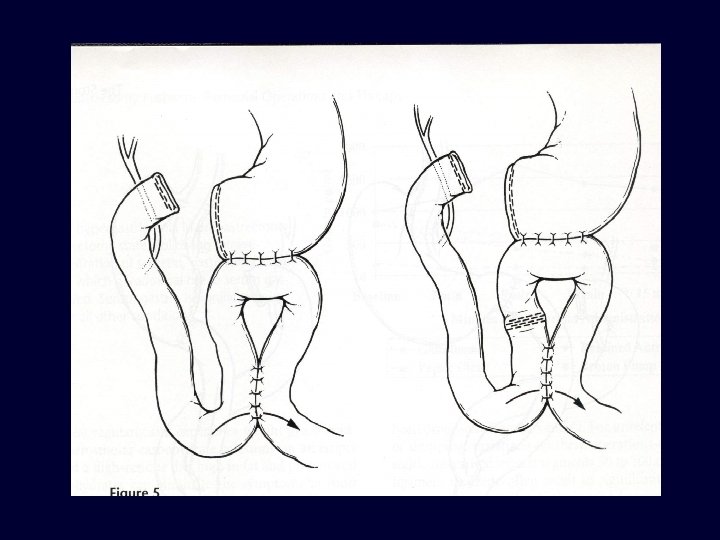
Total Gastrectomy
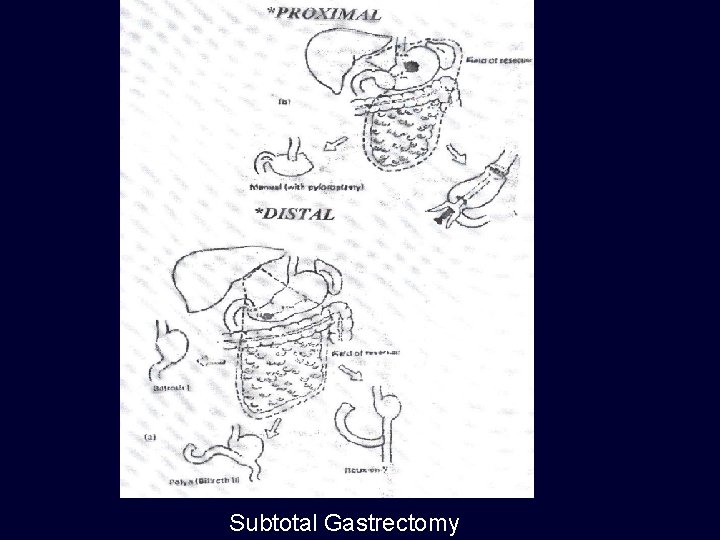
Subtotal Gastrectomy
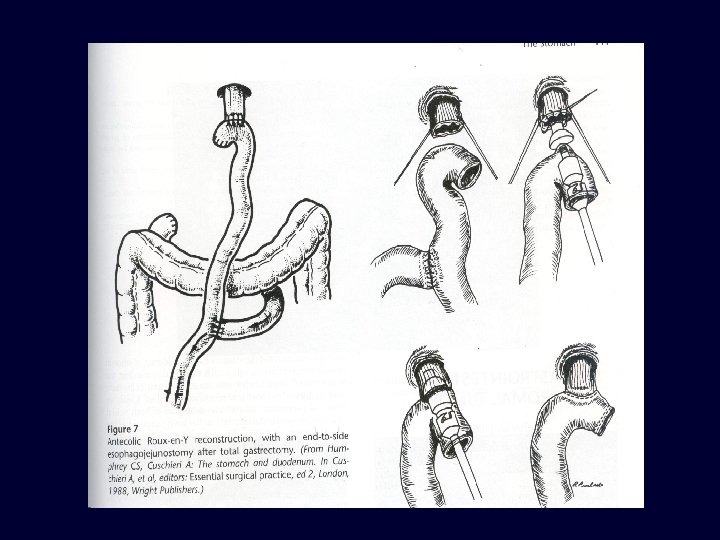
3. PALLIATIVE SURGERY; n n In symptoms of obstruction & bleeding Only tumour is removed &GIT continuity is restored by ROUX LOOP Gastric exclusion & oesophagojejunostomy Palliative intubation & stenting (for inoperable cardia tumours) RADIOTHERAPY; n n Results are disappoiting in CA stomach But have benefits in painful bony metastasis CHEMOTHERAPY; n n Epirubacin + cispltinium+5 -FU Mitomycin C– impregnated charcoal in intraperitoneal route ( in Japan) RELAPSE & METASTASIS; n n Common site of relapse is Gastric bed Metastasis occur in –intra peritoneal & distal LNs -- liver -- lungs & bones
- Slides: 60