Ben Mc Kenzie HEAD INJURY Classification Based on

Ben Mc. Kenzie HEAD INJURY
Classification Based on GCS in ATLS/EMST Mild 14 -15 Moderate 9 -13 Severe 3 -8 Many survive that wouldn’t have in past – large burden on society.

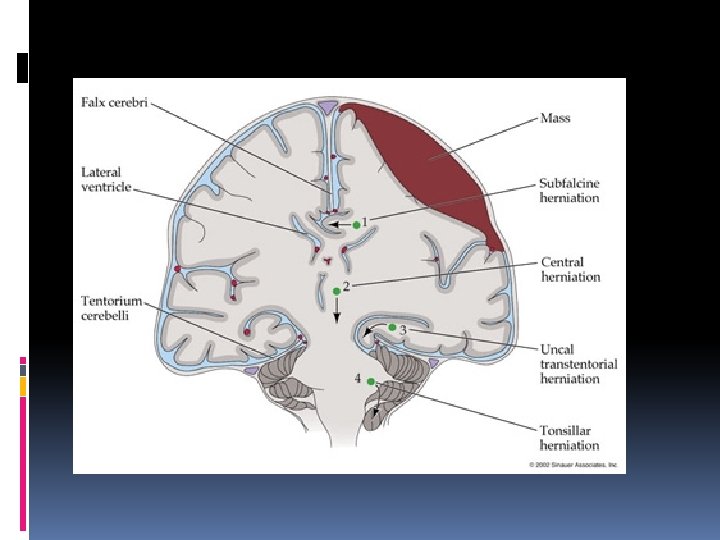
Diffuse injury Focal Injury
Physiology Intracranial volume is fixed Brain 80%, venous blood, arterial blood 10% and CSF 10% occupy this space. CSF made at 20 mls/h - 500 mls day Made by choroid plexus – absorbed by arrachnoid granulations Blood – low CO 2 causes vasoconstiction.
Cerebral Blood Flow CBF = pressure across brain / resistance CPP = MAP – ICP 20 cm CSF CPP 40 mm. Hg Autoregulation – good up to 120 mm. Hg Cushings reflex
Mild Head Injury - Why Image? For neurosurgical intervention
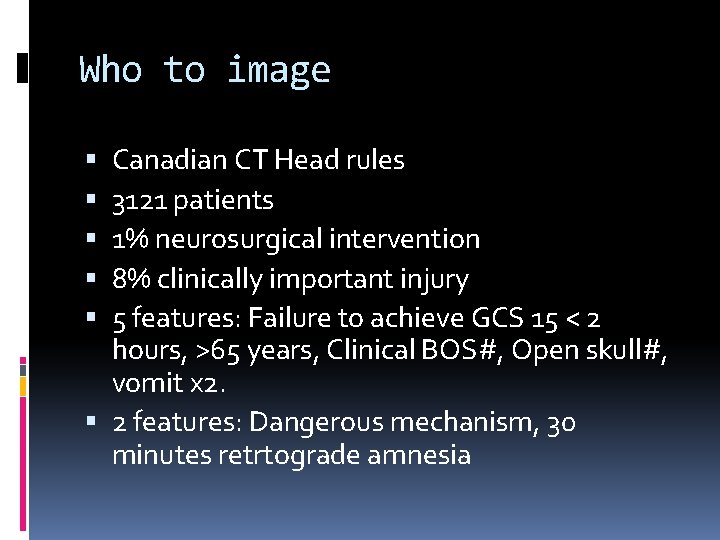
Who to image Canadian CT Head rules 3121 patients 1% neurosurgical intervention 8% clinically important injury 5 features: Failure to achieve GCS 15 < 2 hours, >65 years, Clinical BOS#, Open skull#, vomit x 2. 2 features: Dangerous mechanism, 30 minutes retrtograde amnesia
Excluded Warfarin Seizures Represents Neuro deficits
Warfarin Low threshold for CT Is there a need for observation post normal CT? Need good follow up.
Post Traumatic Amnesia
Post Traumatic Amnesia Is a stage of recovery of the brain from an injury. Onset once patient regains consciousness and lasts for a variable time. Affects orientation and memory for ongoing events
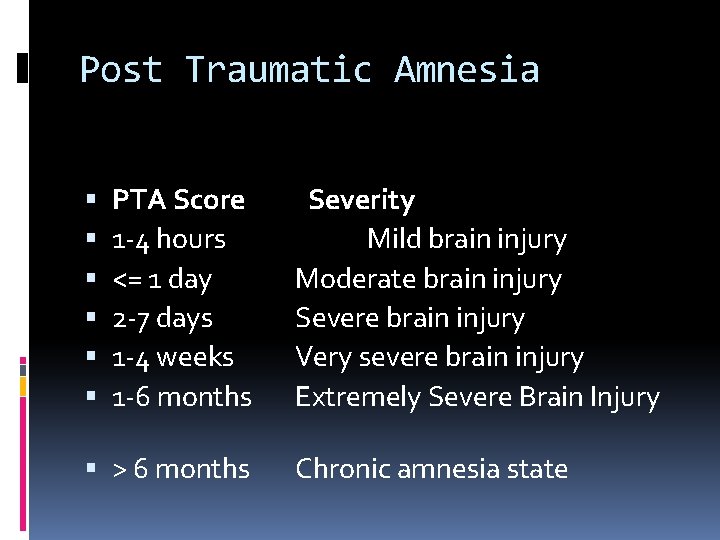
Post Traumatic Amnesia PTA Score 1 -4 hours <= 1 day 2 -7 days 1 -4 weeks 1 -6 months > 6 months Severity Mild brain injury Moderate brain injury Severe brain injury Very severe brain injury Extremely Severe Brain Injury Chronic amnesia state
Westmead PTA Scale Shores EA. , Marosszeky JE. , Sandanam J. , Batchelor J. Preliminary validation of a clinical scale for measuring the duration of post-traumatic amnesia. Medical Journal of Australia. 144(11): 569 -72, 1986 May 26. Patient said to be recovered when scores perfectly on three consecutive days. More sensitive than GCS alone Abbreviated version considered in emergency departments
Revised Westmead Use of the Westmead PTA Scale to Monitor Recovery of Memory after Mild Head Injury. Brain Injury. 18(6): 603 -614, June 2004. Several studies suggest can be used in ED and is more sensitive.
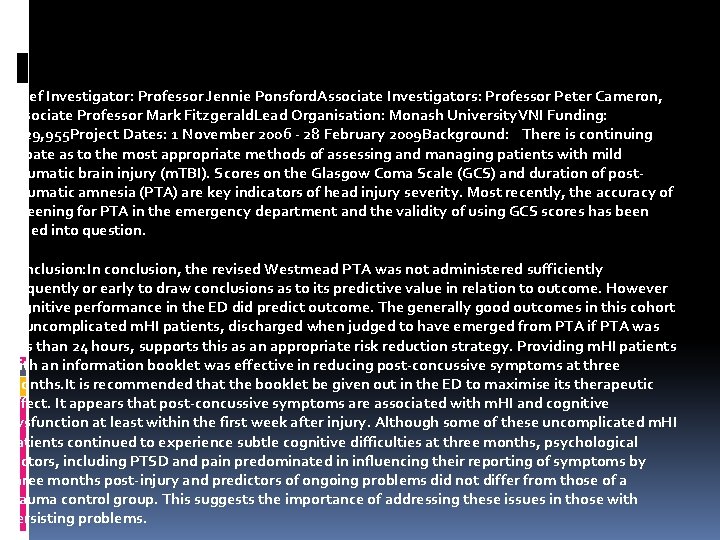
Chief Investigator: Professor Jennie Ponsford. Associate Investigators: Professor Peter Cameron, Associate Professor Mark Fitzgerald. Lead Organisation: Monash University. VNI Funding: $229, 955 Project Dates: 1 November 2006 - 28 February 2009 Background: There is continuing debate as to the most appropriate methods of assessing and managing patients with mild traumatic brain injury (m. TBI). Scores on the Glasgow Coma Scale (GCS) and duration of posttraumatic amnesia (PTA) are key indicators of head injury severity. Most recently, the accuracy of screening for PTA in the emergency department and the validity of using GCS scores has been called into question. Conclusion: In conclusion, the revised Westmead PTA was not administered sufficiently frequently or early to draw conclusions as to its predictive value in relation to outcome. However cognitive performance in the ED did predict outcome. The generally good outcomes in this cohort of uncomplicated m. HI patients, discharged when judged to have emerged from PTA if PTA was less than 24 hours, supports this as an appropriate risk reduction strategy. Providing m. HI patients with an information booklet was effective in reducing post-concussive symptoms at three months. It is recommended that the booklet be given out in the ED to maximise its therapeutic effect. It appears that post-concussive symptoms are associated with m. HI and cognitive dysfunction at least within the first week after injury. Although some of these uncomplicated m. HI patients continued to experience subtle cognitive difficulties at three months, psychological factors, including PTSD and pain predominated in influencing their reporting of symptoms by three months post-injury and predictors of ongoing problems did not differ from those of a trauma control group. This suggests the importance of addressing these issues in those with persisting problems.
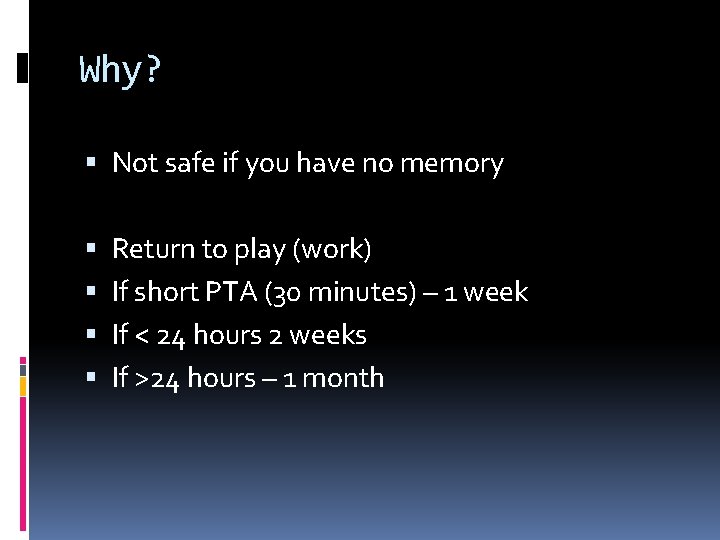
Why? Not safe if you have no memory Return to play (work) If short PTA (30 minutes) – 1 week If < 24 hours 2 weeks If >24 hours – 1 month
Post Concussion Syndrome
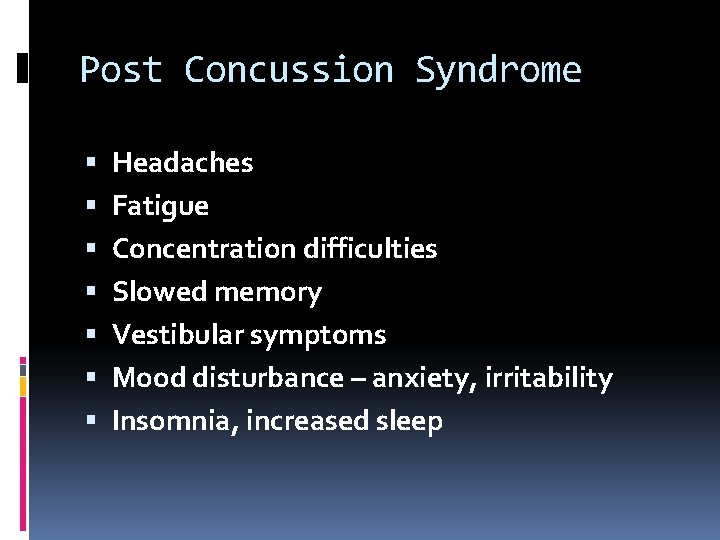
Post Concussion Syndrome Headaches Fatigue Concentration difficulties Slowed memory Vestibular symptoms Mood disturbance – anxiety, irritability Insomnia, increased sleep
Post concussion syndrome Most brief – days Most/All resolve within 3 months EDUCATION, EXPLANATION, INFORMATION Multiple studies show that this reduces duration of symptoms
Bendigo Anyone with amnesia for an hour or so can probably managed by GP with good advice. They will have a good outcome Anyone with amnesia for some hours should go to short stay under the head injury pathway with detailed follow up with GP/OT Anyone with persisting amnesia needs admission for rehabilitation.
Contusions Swelling and oedema around greatest at 48 hours. Rarely need any surgical intervention Often multiple of complicate management of other traumatic lesions
Extradural Bound by dural reflection of skull bones Therefore lentiform and over single skull bone Usually arterial but can be venous Often reach their maximum size within minutes but can rebleed/keep expanding
Subdural Bridging veins between cortex and venous sinus tear and bleed. Separate arachnoid and dura and can extend anywhere in the cranium in this plane – falx, tentorium, around calvarium. Can spontaneously happen in people with atrophic brains
Subdural Treatment Often conservative in older asymptomatic people. A true neurosurgical emergency if symptoms and time critical if conscious state deteriorating.
Mannitol 1 gram/kg Give: If dilated pupil If GCS deteriorating persistently leading to intubation.
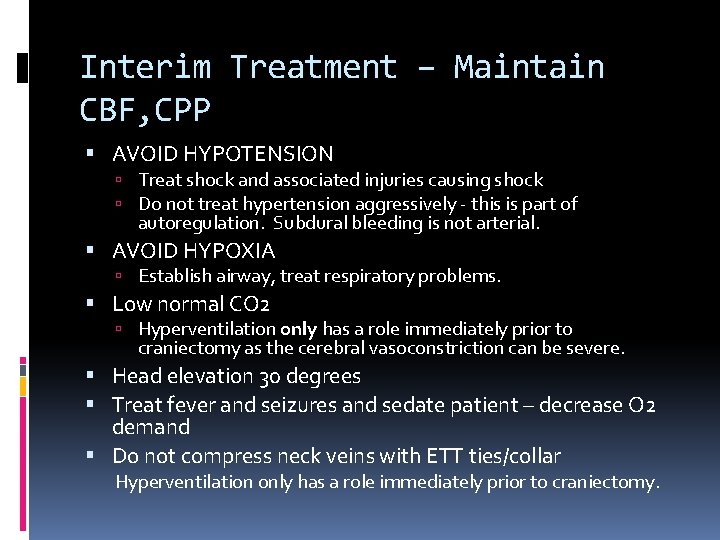
Interim Treatment – Maintain CBF, CPP AVOID HYPOTENSION Treat shock and associated injuries causing shock Do not treat hypertension aggressively - this is part of autoregulation. Subdural bleeding is not arterial. AVOID HYPOXIA Establish airway, treat respiratory problems. Low normal CO 2 Hyperventilation only has a role immediately prior to craniectomy as the cerebral vasoconstriction can be severe. Head elevation 30 degrees Treat fever and seizures and sedate patient – decrease O 2 demand Do not compress neck veins with ETT ties/collar Hyperventilation only has a role immediately prior to craniectomy.
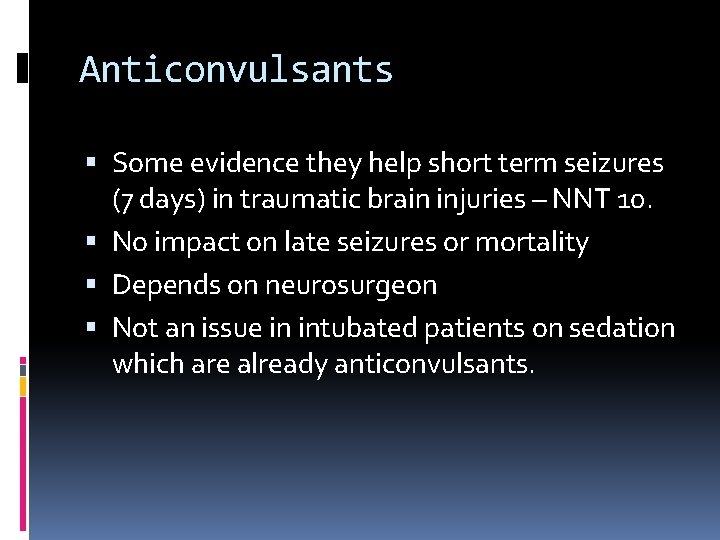
Anticonvulsants Some evidence they help short term seizures (7 days) in traumatic brain injuries – NNT 10. No impact on late seizures or mortality Depends on neurosurgeon Not an issue in intubated patients on sedation which are already anticonvulsants.
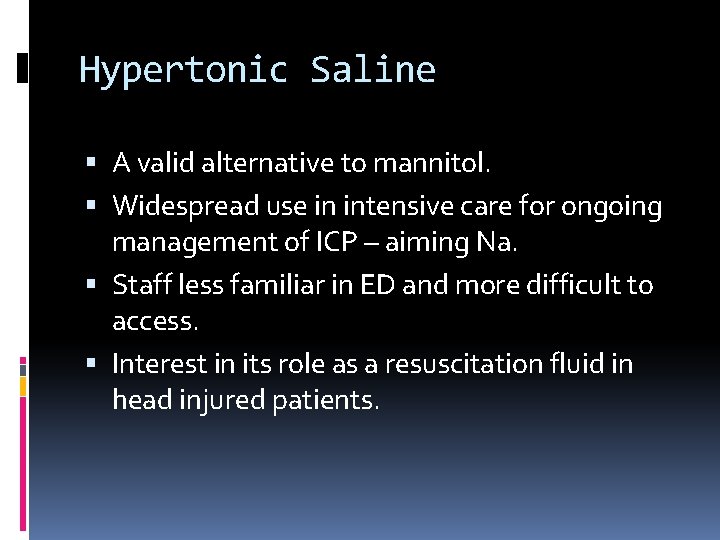
Hypertonic Saline A valid alternative to mannitol. Widespread use in intensive care for ongoing management of ICP – aiming Na. Staff less familiar in ED and more difficult to access. Interest in its role as a resuscitation fluid in head injured patients.
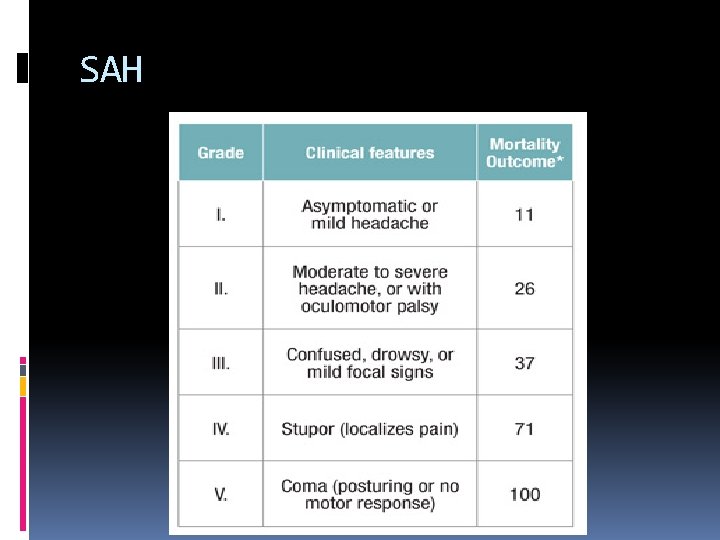
SAH
SAH 4% rebleed in 48 hours 20% rebleed in 2 weeks 60% mortality with rebleed.
SAH - Sudden Death/Global Ischaemia Presumably due to sudden rise in ICP for minutes leading to brain death. Can easily be intubated by MICA paramedics and come to your ED before body dies with last gasp.
SAH Vasospasm Peak at day 7 Manifests as strokes Nimodipine – single centre trial. Via NGT. Some neurosurgeons ask for it – ignore them and focus on BP and getting patient to neurosurgical centre. Once aneurysm clipped/coiled patients made hypervolaemic and can have low dose norad to ensure cerebral vessels are full.
SAH - Hydrocephalus 15 % of patients Seizures – treat as they arise Anticonvulsant controversial – give phenytoin if accepting neurosurgical service asks,
- Slides: 34