BEHAVIORAL HEALTH NON PROFIT AND PRIVATE OPERATIONS Goal

BEHAVIORAL HEALTH NON PROFIT AND PRIVATE OPERATIONS

Goal for today Provide an orientation on environmental supports, threats and opportunities in our current OCBH member community based delivery system. • • • Mission Funding Workforce Compliance and requirements Basic business structures (This presentations does not focus on county governmental services or many non-Medicaid service partners)
Who are OCBH members? • Predominately non-profit and private state Medicaid letter holding organizations. • Professional experts, who have provided community based services to our most vulnerable citizens for over 30 years. • Contractors with CCO’s, counties and community stakeholders and other entities to provide care. • Provide a wide variety of care from prevention through residential and detox services and integrated care. • Agile, lean and mission driven.

A NOTE ON INTEGRATION It is a complex reorganizing of operations and system delivery. It requires culture change, resources and intention. AKA. . remodeling your house…twice as long, three times as expensive and a stress on relationship success. Why then? To improve outcomes, efficiencies, experience and care for all our diverse Oregon communities.

Education and outreach • Outpatient • Day Treatment • Supported Housing • Residential • Hospital • Prevention • Harm Reduction • Outpatient • Day Treatment • Supported Housing • Residential • Detox • Hospital level Detox Recovery and SOD • Targeted Substance use Disorder Mental Health • Prevention • Self Help • Peer run community based centers • Peers in Treatment settings • Employment services • Housing • Education • Nutrition • Fun and community
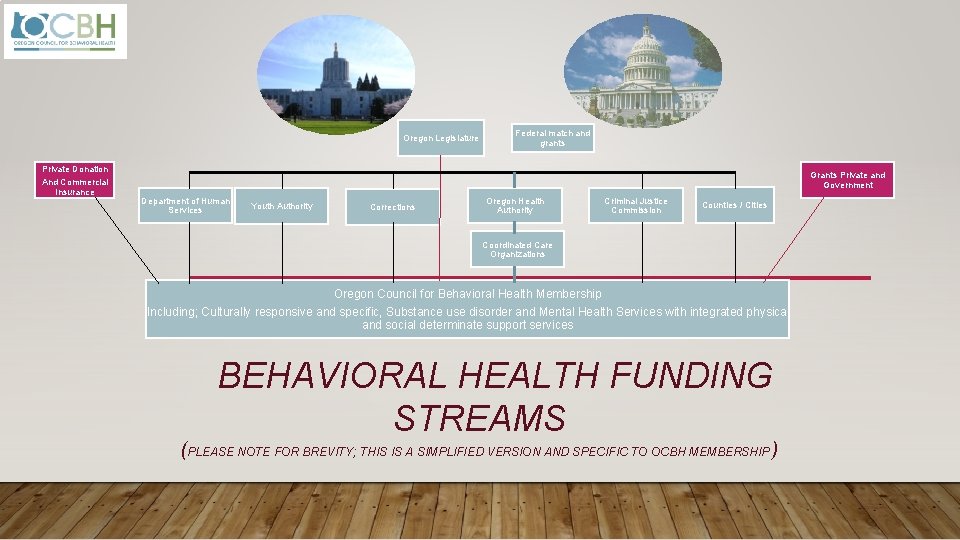
Oregon Legislature Federal match and grants Private Donation And Commercial Insurance Grants Private and Government Department of Human Services Youth Authority Corrections Oregon Health Authority Criminal Justice Commission Counties / Cities Coordinated Care Organizations Oregon Council for Behavioral Health Membership Including; Culturally responsive and specific, Substance use disorder and Mental Health Services with integrated physical and social determinate support services BEHAVIORAL HEALTH FUNDING STREAMS (PLEASE NOTE FOR BREVITY; THIS IS A SIMPLIFIED VERSION AND SPECIFIC TO OCBH MEMBERSHIP )

Mission Implementation BH is for people implemented by people Consumers and Employees Big need, ever-growing costs, diversity short falls “Non-profit penalty” A large responsibility with a small structure Compliance and data collection needs and requirements Complex funding Financial and In-Kind Vision and Mission Organizational structure
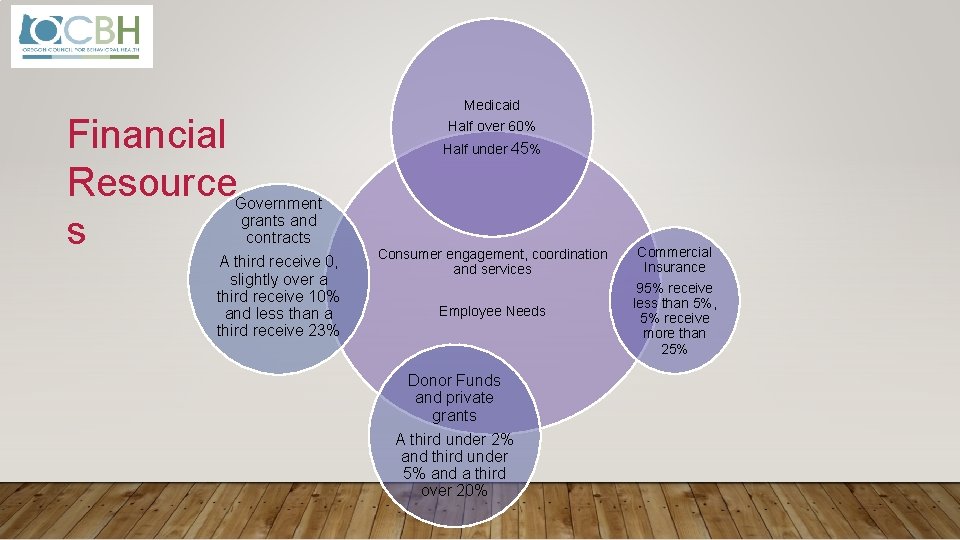
Financial Resource s Government grants and contracts A third receive 0, slightly over a third receive 10% and less than a third receive 23% Medicaid Half over 60% Half under 45% Consumer engagement, coordination and services Employee Needs Donor Funds and private grants A third under 2% and third under 5% and a third over 20% Commercial Insurance 95% receive less than 5%, 5% receive more than 25%
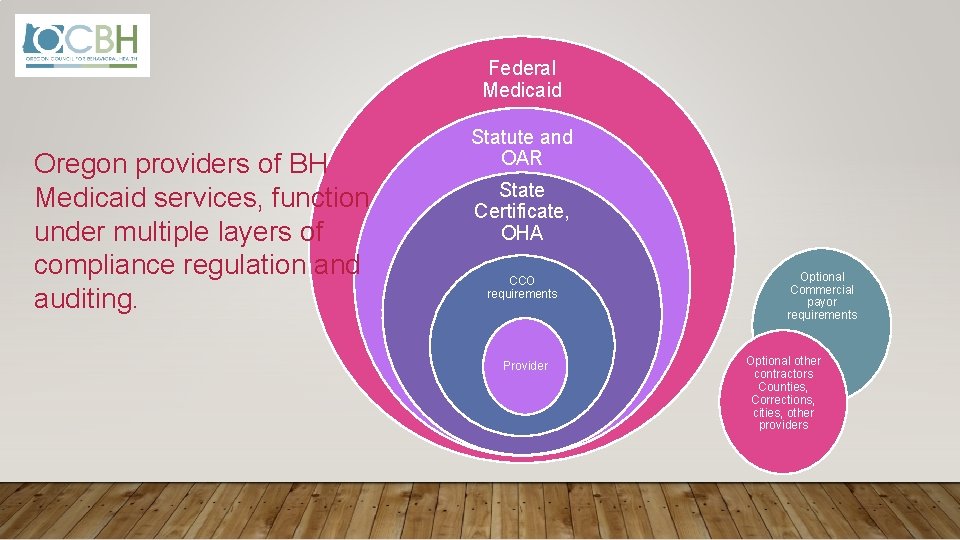
Federal Medicaid Oregon providers of BH Medicaid services, function under multiple layers of compliance regulation and auditing. Statute and OAR State Certificate, OHA CCO requirements Provider Optional Commercial payor requirements Optional other contractors Counties, Corrections, cities, other providers
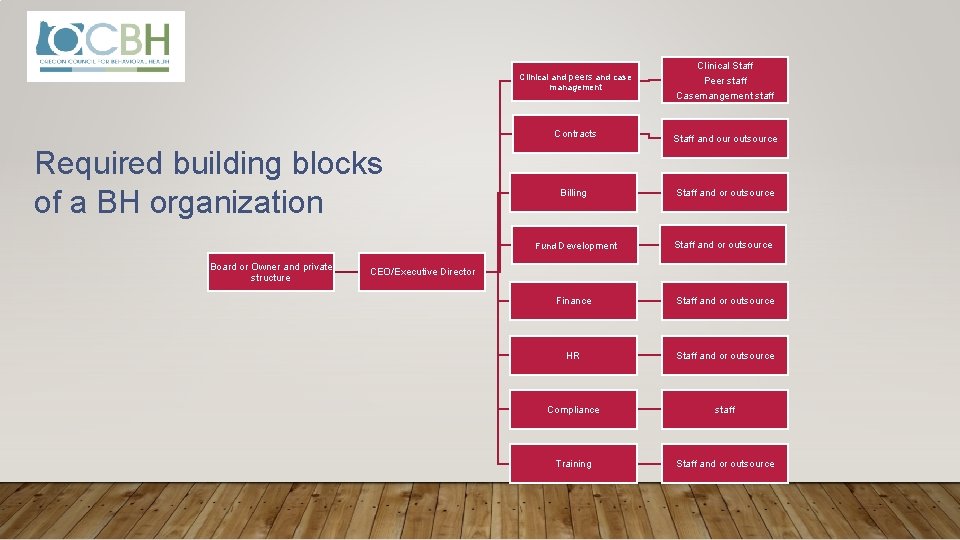
Clinical and peers and case management Required building blocks of a BH organization Board or Owner and private structure Clinical Staff Peer staff Casemangement staff Contracts Staff and our outsource Billing Staff and or outsource Fund Development Staff and or outsource Finance Staff and or outsource HR Staff and or outsource Compliance staff Training Staff and or outsource CEO/Executive Director
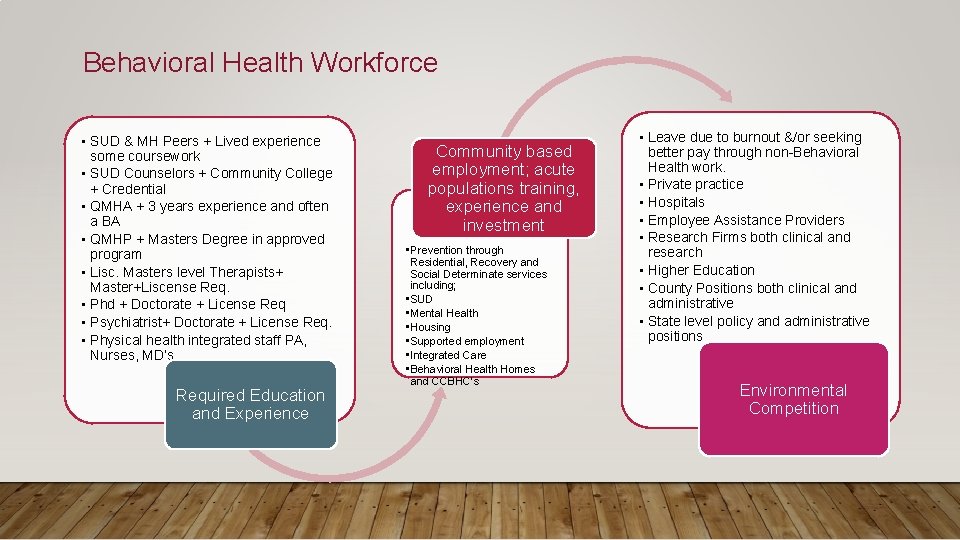
Behavioral Health Workforce • SUD & MH Peers + Lived experience some coursework • SUD Counselors + Community College + Credential • QMHA + 3 years experience and often a BA • QMHP + Masters Degree in approved program • Lisc. Masters level Therapists+ Master+Liscense Req. • Phd + Doctorate + License Req • Psychiatrist+ Doctorate + License Req. • Physical health integrated staff PA, Nurses, MD’s Required Education and Experience Community based employment; acute populations training, experience and investment • Prevention through Residential, Recovery and Social Determinate services including; • SUD • Mental Health • Housing • Supported employment • Integrated Care • Behavioral Health Homes and CCBHC’s • Leave due to burnout &/or seeking better pay through non-Behavioral Health work. • Private practice • Hospitals • Employee Assistance Providers • Research Firms both clinical and research • Higher Education • County Positions both clinical and administrative • State level policy and administrative positions Environmental Competition
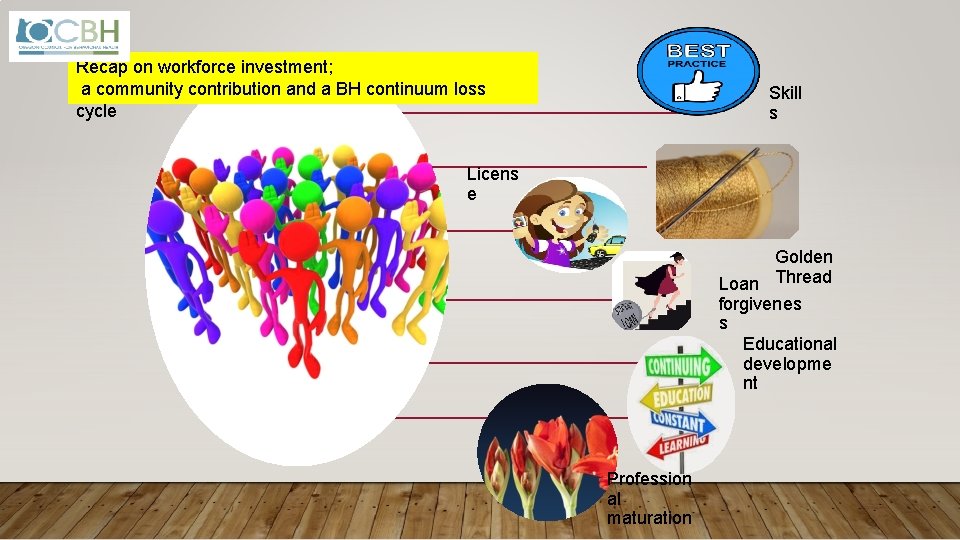
Recap on workforce investment; a community contribution and a BH continuum loss cycle Skill s Licens e Golden Loan Thread forgivenes s Educational developme nt Profession al maturation

Shift the operations pyramid improving sustainability and population health Mission Implementation Consumers and employees Big need, evergrowing costs “Non-profit penalty” Complex funding Financial and In. Kind Compliance and data collection needs and requirements Vision and Mission Organizational structure
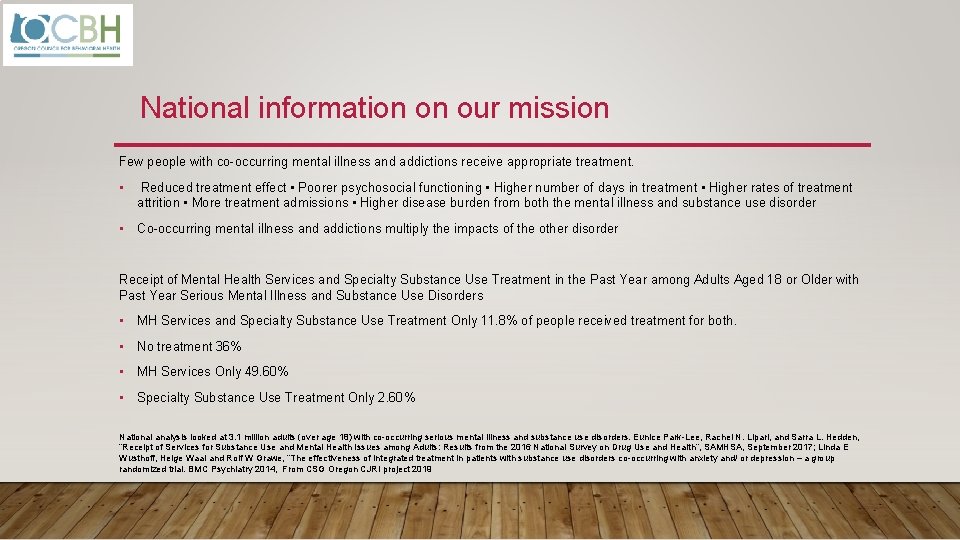
National information on our mission Few people with co-occurring mental illness and addictions receive appropriate treatment. • Reduced treatment effect • Poorer psychosocial functioning • Higher number of days in treatment • Higher rates of treatment attrition • More treatment admissions • Higher disease burden from both the mental illness and substance use disorder • Co-occurring mental illness and addictions multiply the impacts of the other disorder Receipt of Mental Health Services and Specialty Substance Use Treatment in the Past Year among Adults Aged 18 or Older with Past Year Serious Mental Illness and Substance Use Disorders • MH Services and Specialty Substance Use Treatment Only 11. 8% of people received treatment for both. • No treatment 36% • MH Services Only 49. 60% • Specialty Substance Use Treatment Only 2. 60% National analysis looked at 3. 1 million adults (over age 18) with co-occurring serious mental illness and substance use disorders. Eunice Park-Lee, Rachel N. Lipari, and Sarra L. Hedden, “Receipt of Services for Substance Use and Mental Health Issues among Adults: Results from the 2016 National Survey on Drug Use and Health”, SAMHSA, September 2017; Linda E Wusthoff, Helge Waal and Rolf W Grawe, “The effectiveness of integrated treatment in patients with substance use disorders co-occurring with anxiety and/ or depression – a group randomized trial. BMC Psychiatry 2014, From CSG Oregon CJRI project 2019
- Slides: 14