BASICS OF ULTRASONOGRAPHY 1 ULTRASONOGRAPHY VS RADIOGRAPHY They
BASICS OF ULTRASONOGRAPHY 1
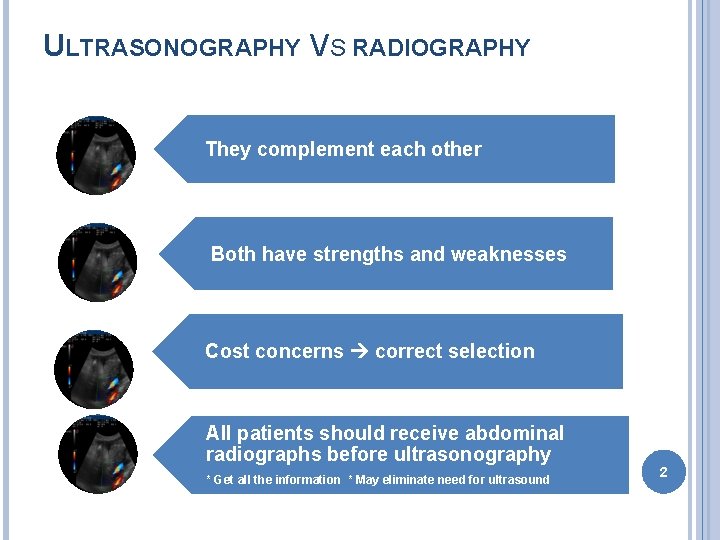
ULTRASONOGRAPHY VS RADIOGRAPHY They complement each other Both have strengths and weaknesses Cost concerns correct selection All patients should receive abdominal radiographs before ultrasonography * Get all the information * May eliminate need for ultrasound 2
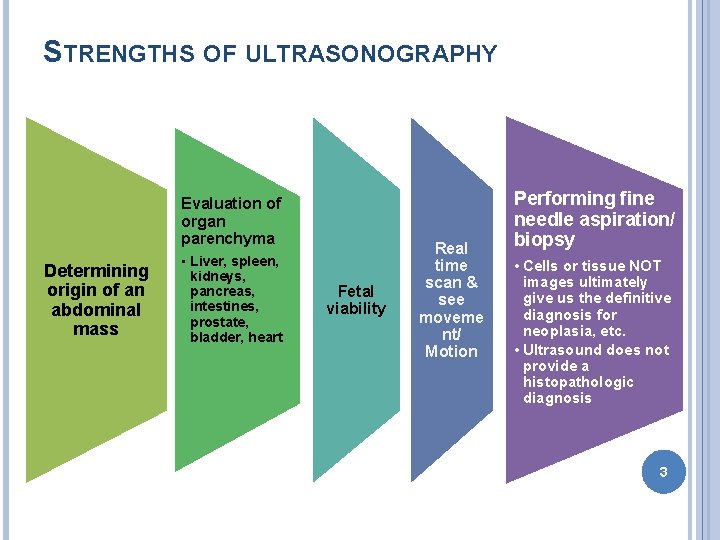
STRENGTHS OF ULTRASONOGRAPHY Evaluation of organ parenchyma Determining origin of an abdominal mass • Liver, spleen, kidneys, pancreas, intestines, prostate, bladder, heart Fetal viability Real time scan & see moveme nt/ Motion Performing fine needle aspiration/ biopsy • Cells or tissue NOT images ultimately give us the definitive diagnosis for neoplasia, etc. • Ultrasound does not provide a histopathologic diagnosis 3
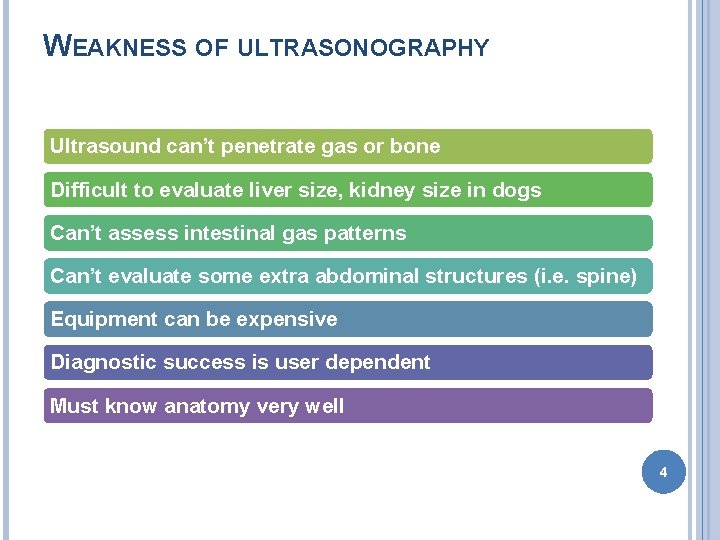
WEAKNESS OF ULTRASONOGRAPHY Ultrasound can’t penetrate gas or bone Difficult to evaluate liver size, kidney size in dogs Can’t assess intestinal gas patterns Can’t evaluate some extra abdominal structures (i. e. spine) Equipment can be expensive Diagnostic success is user dependent Must know anatomy very well 4
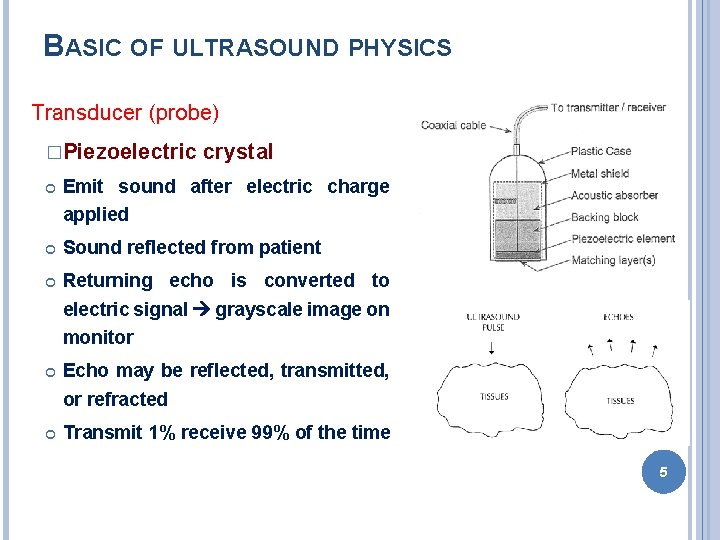
BASIC OF ULTRASOUND PHYSICS Transducer (probe) �Piezoelectric crystal Emit sound after electric charge applied Sound reflected from patient Returning echo is converted to electric signal grayscale image on monitor Echo may be reflected, transmitted, or refracted Transmit 1% receive 99% of the time 5
ACOUSTIC IMPEDANCE The velocity of sound in a tissue and tissue density = determine acoustic impedance Most soft tissues = 1400 -1600 m/sec � Bone = 4080 � Air � Sound will not penetrate – gets reflected or absorbed = 330 Travel time – dot depth 6
BASIC OF ULTRASOUND PHYSICS Sound waves are measured in Hertz (Hz) Diagnostic ultrasound typically 1 -20 MHz As frequency increases, resolution improves As frequency increases, depth of penetration decreases 7
ULTRASOUND TERMINOLOGY Never use dense, opaque, lucent Anechoic � Echogenic � No returning echoes= black (acellular fluid) Regarding fluid--some shade of grey d/t returning echoes Relative terms � Comparison to normal echogenicity of the same organ or other structure � Hypoechoic, isoechoic, hyperechoic Spleen should be hyperechoic to liver 8

ULTRASOUND PROBE A B C D A B C 9
MODES OF DISPLAY A mode � Spikes – where precise length and depth measurements are needed – ophtho B mode (brightness) – used most often � M mode – motion mode � o 2 D reconstruction of the image slice Moving 1 D image – cardiac mainly CFM : Color Flow Monitory : showed blood circulation to tissue � Doppler : Live sound produced by tissue or organ used for fetal viability and echocardiography 10
ARTIFACTS Improper machine settings – gain Reverberation � Mirror image – liver GB � Comet tail – gas bubble � Ring down – skin transducer surface Acoustic shadowing Acoustic enhancement Edge enhancement � Border of kidney 11
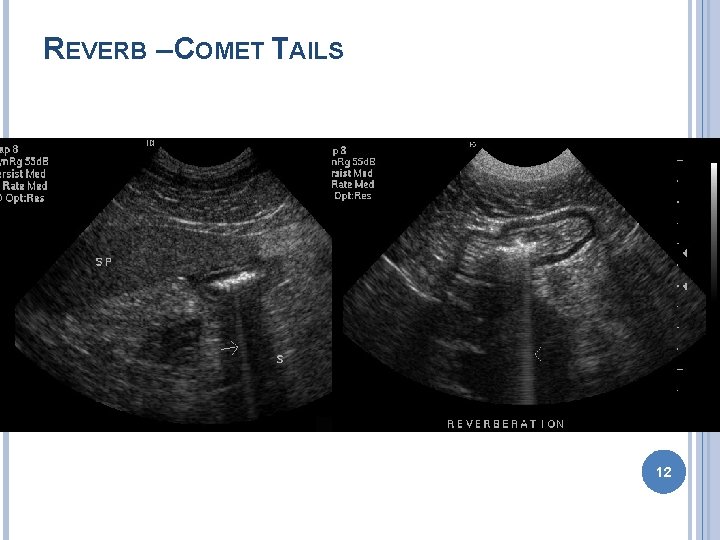
REVERB – COMET TAILS 12
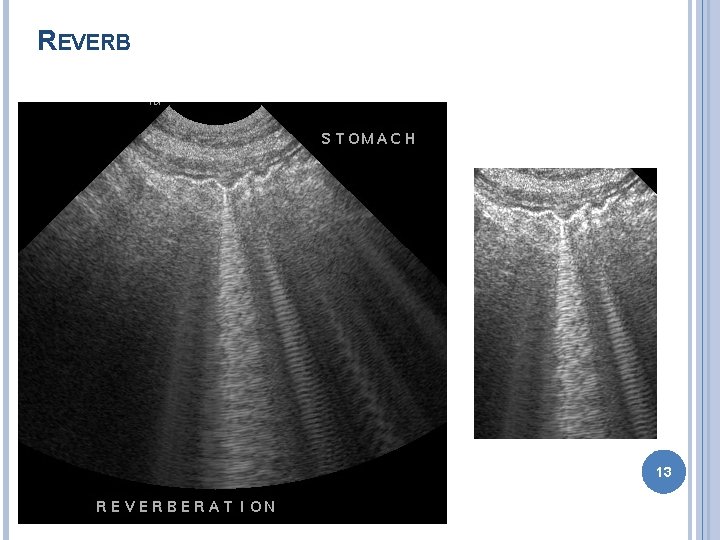
REVERB 13
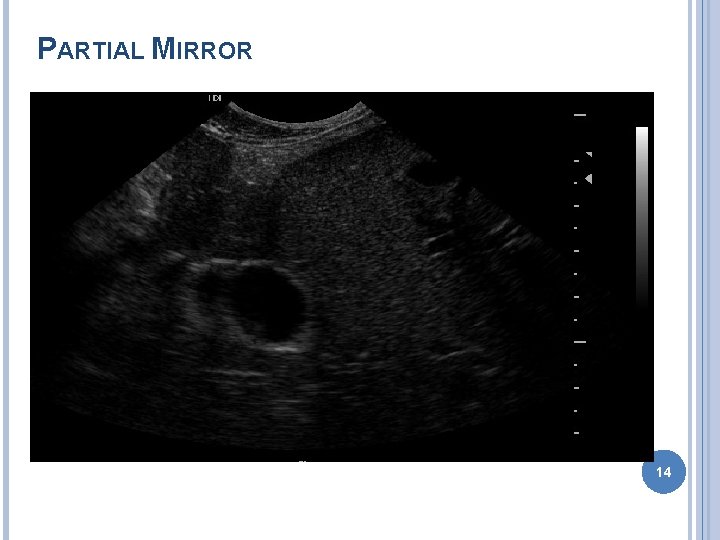
PARTIAL MIRROR 14
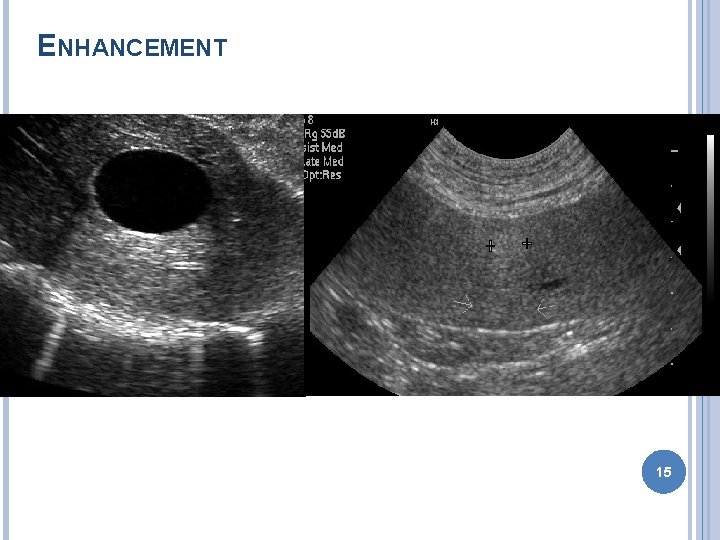
ENHANCEMENT 15
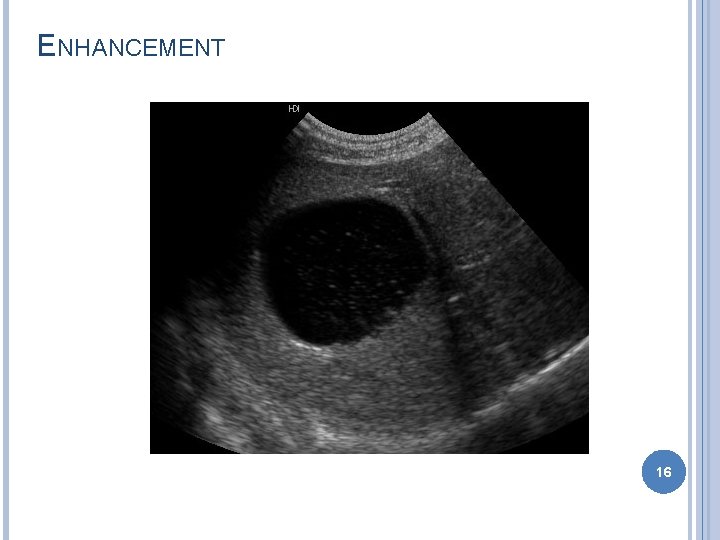
ENHANCEMENT 16
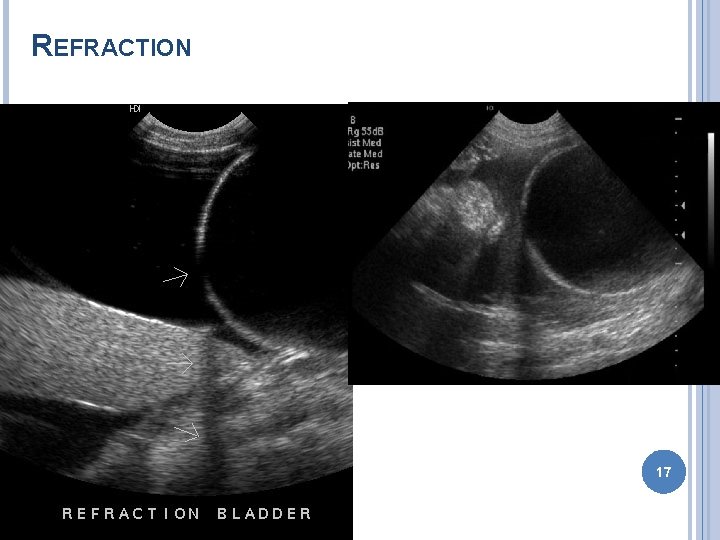
REFRACTION 17
PATIENT POSITIONING - PREPARATION Dorsal recumbency Lateral recumbency Standing Clip hair � Be sure to check with owners Apply ultrasound gel Alcohol can be used – esp. in horses 18
ULTRASOUND-GUIDED FNA/ BIOPSIES NORMAL ABD U/S FINDINGS DO NOT MEAN ORGANS ARE NORMAL!!! � ***Do FNA if suspect disease Abnormal u/s findings nonspecific � Benign and malignant masses identical � Bright liver may be secondary to Cushing’s disease or lymphoma Aspirate abnormal structures (with few exceptions)!!! � Obtain owner approval prior to exam � Warn owner of risks � +/- Clotting profile 19
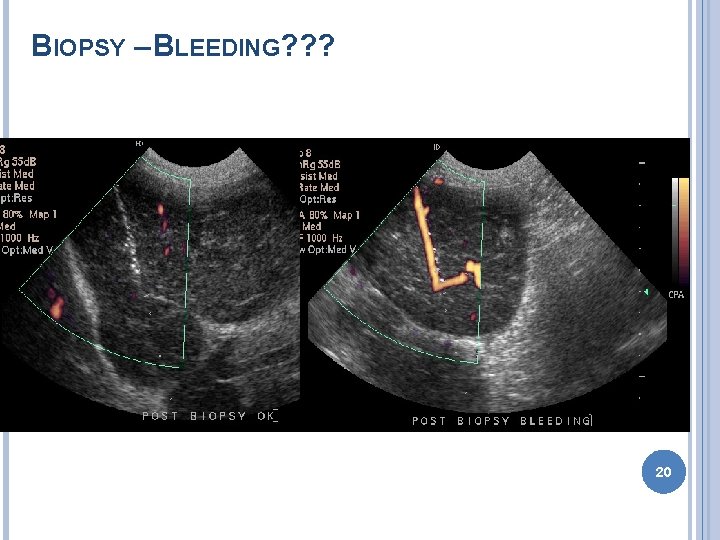
BIOPSY – BLEEDING? ? ? 20
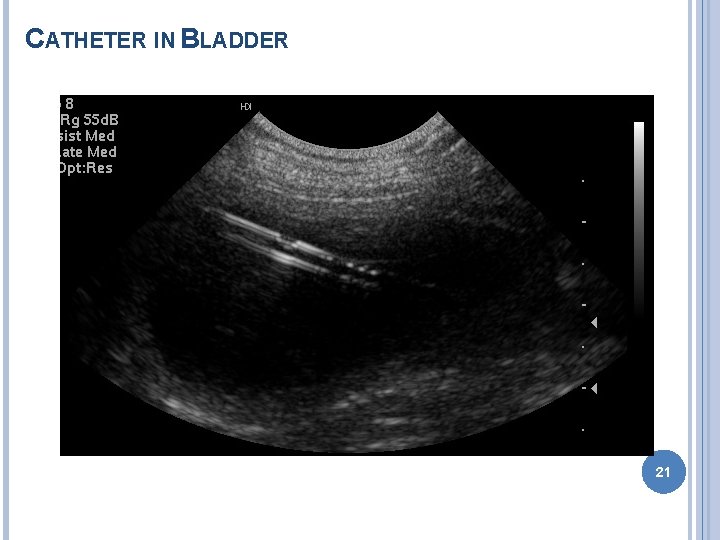
CATHETER IN BLADDER 21
NOTE: • See the images by using the given software. • No need to separate print and fix in manual. • Images given in presentation is only to understand, no need to print. • Write only text in manual and draw a figure of probe only with name. 22
- Slides: 22