Basics of Treatment of Victims of Radiation Terrorism
Basics of Treatment of Victims of Radiation Terrorism or Accidents Niel Wald, M. D. Dept. of Environmental and Occupational Health University of Pittsburgh
Medical Radiation Problems External Radiation Source: –Local Radiation Injury –Acute Radiation Syndrome Radionuclide Contamination: –External –Localized in Wound –Internal

LOCAL RADIATION INJURY: RADIODERMATITIS Type Manifestation I Erythema II Transepidermal Injury III Dermal Radionecrosis IV Chronic Radiodermatitis
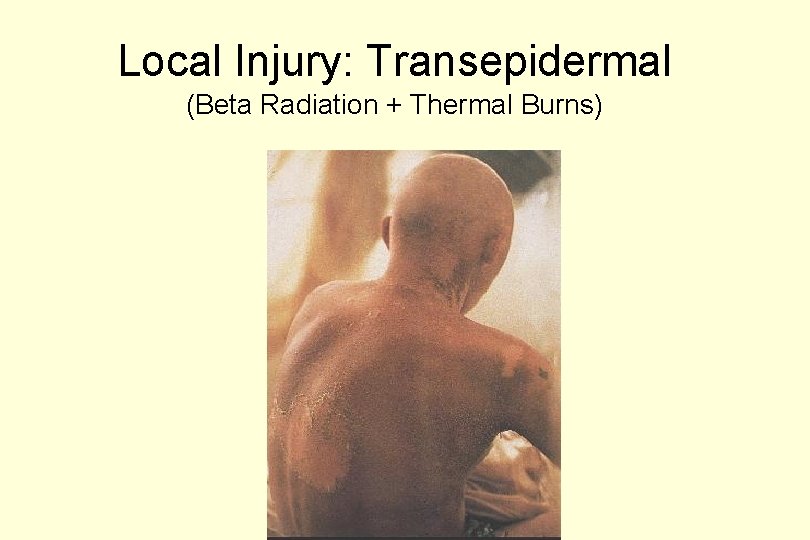
Local Injury: Transepidermal (Beta Radiation + Thermal Burns)
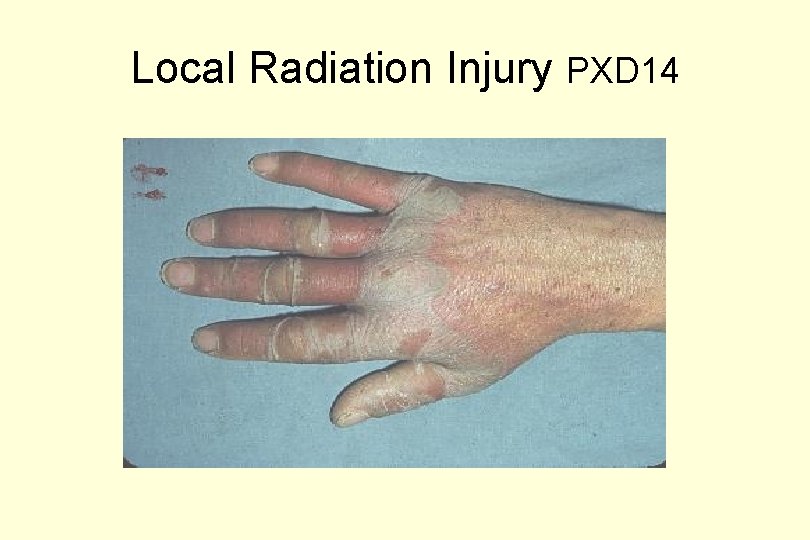
Local Radiation Injury PXD 14
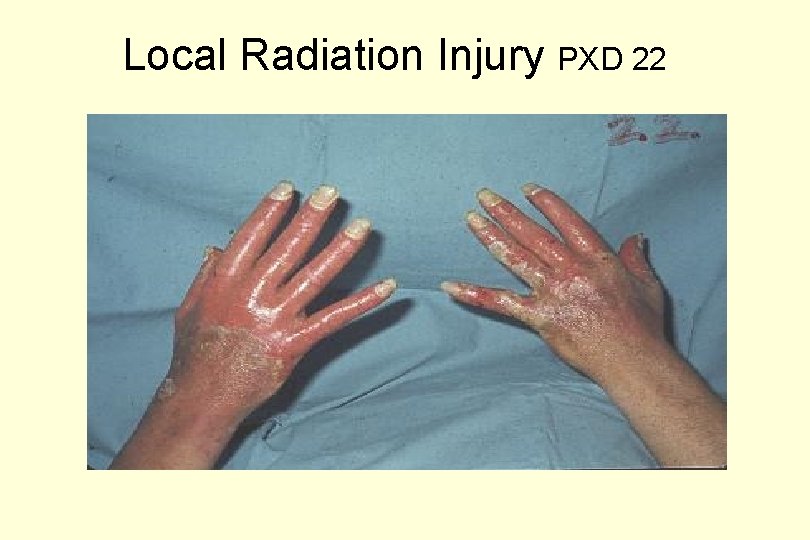
Local Radiation Injury PXD 22
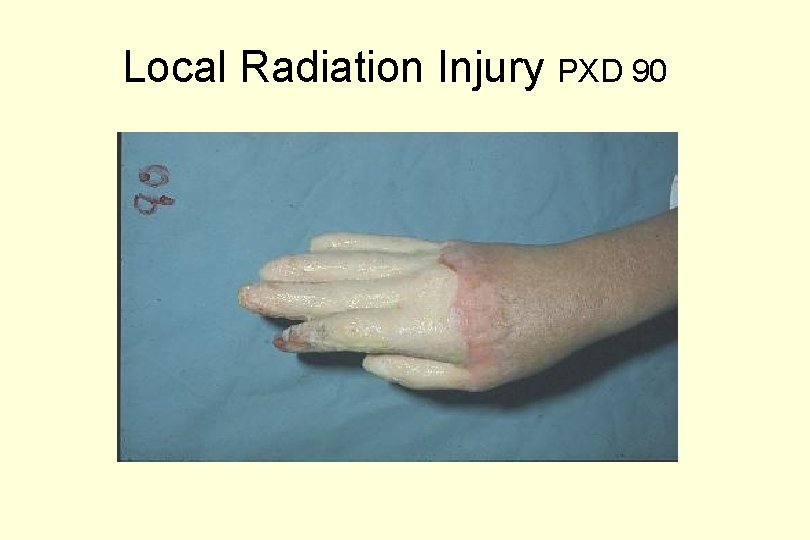
Local Radiation Injury PXD 90
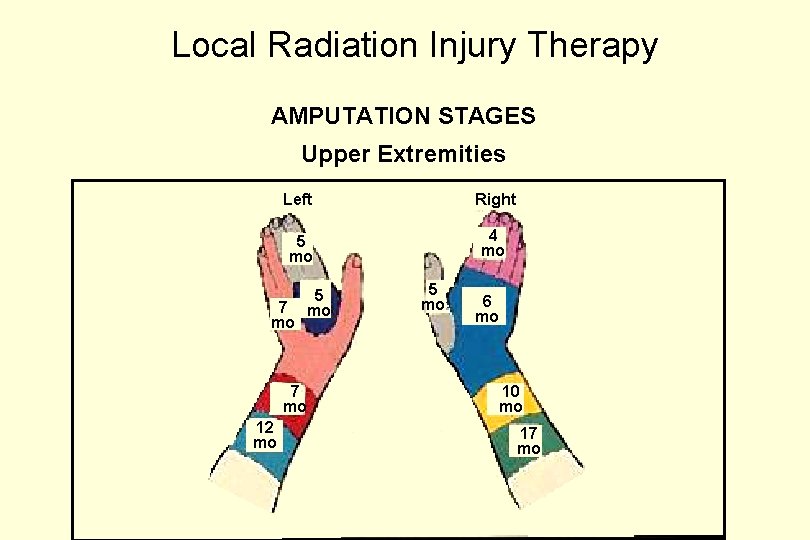
Local Radiation Injury Therapy AMPUTATION STAGES Upper Extremities Left Right 5 mo 4 mo 7 mo 12 mo 5 mo 6 mo 10 mo 17 mo
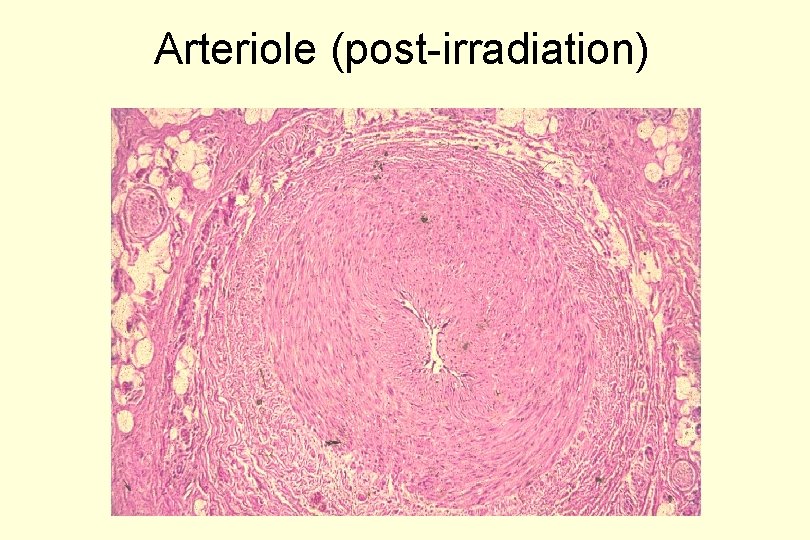
Arteriole (post-irradiation)
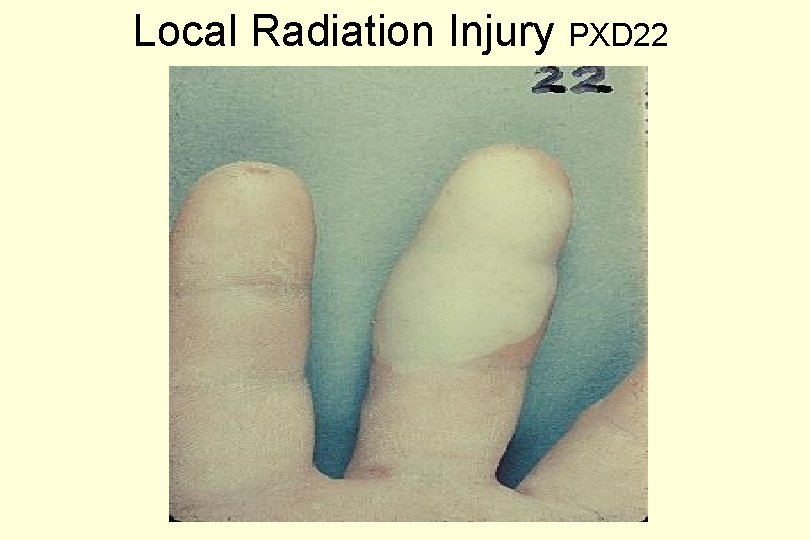
Local Radiation Injury PXD 22
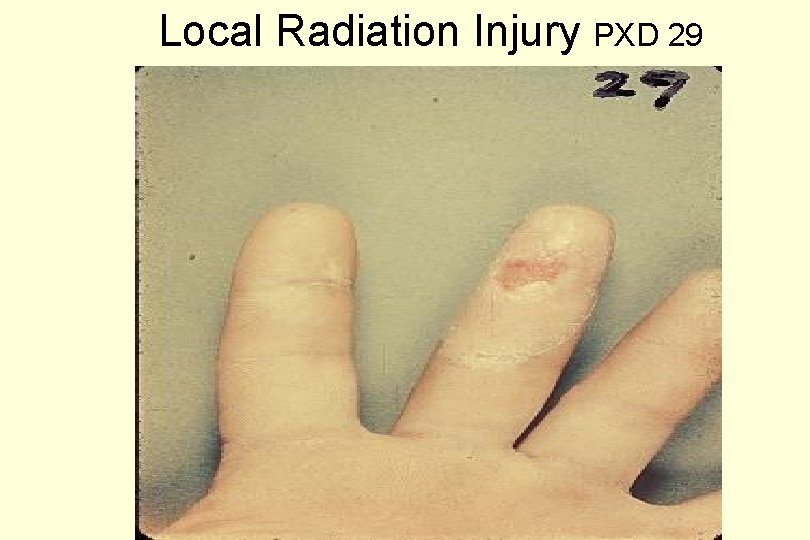
Local Radiation Injury PXD 29
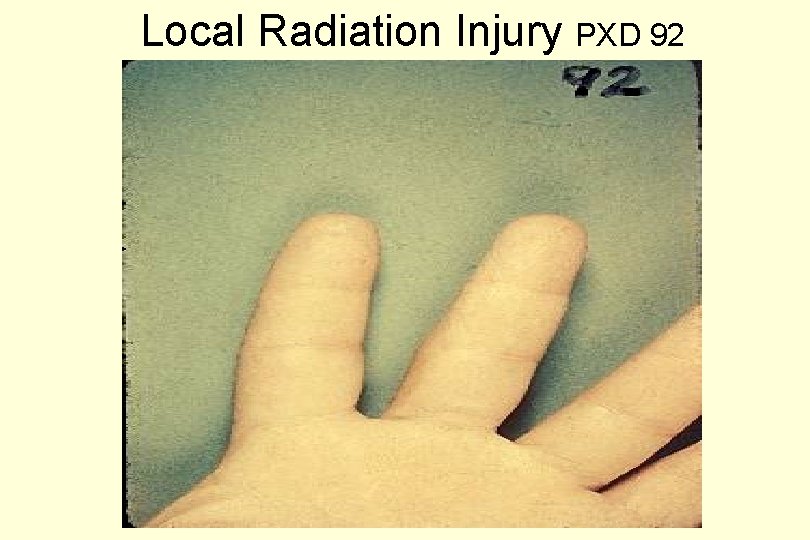
Local Radiation Injury PXD 92
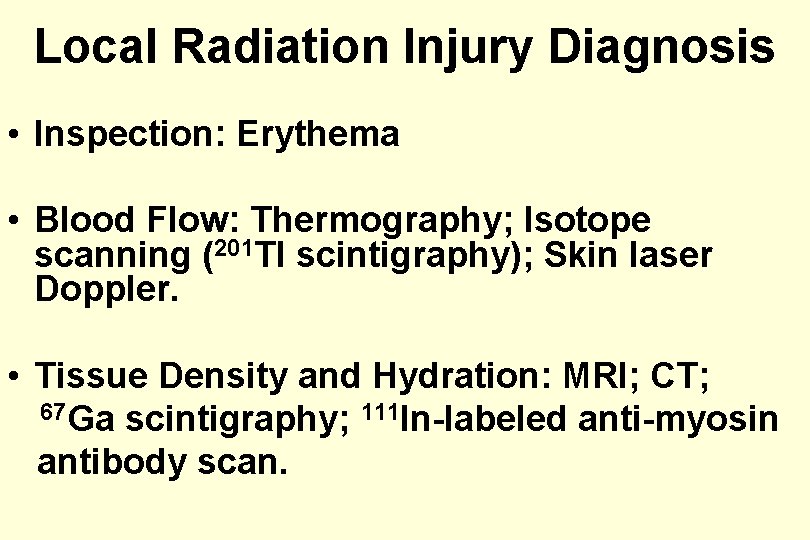
Local Radiation Injury Diagnosis • Inspection: Erythema • Blood Flow: Thermography; Isotope scanning (201 Tl scintigraphy); Skin laser Doppler. • Tissue Density and Hydration: MRI; CT; 67 Ga scintigraphy; 111 In-labeled anti-myosin antibody scan.
Useful Steps in Clinical Care of Local Radiation Injury • • • History and Physical Examination Serial Blood Counts Chromosome Analysis Re-enactment of Accident Frequent Color Photographs Baseline Extremity X-rays Ophthalmologic Slit Lamp Examination Sperm Counts Surgical Consult
Local Radiation Injury Therapy • • • Analgesics, Antipruritics Anti-inflammatories Antibiotics as needed Skin Growth Factors Synthetic Occlusive Dressings Surgical Intervention: – Debridement – Excision and Grafting – Amputation
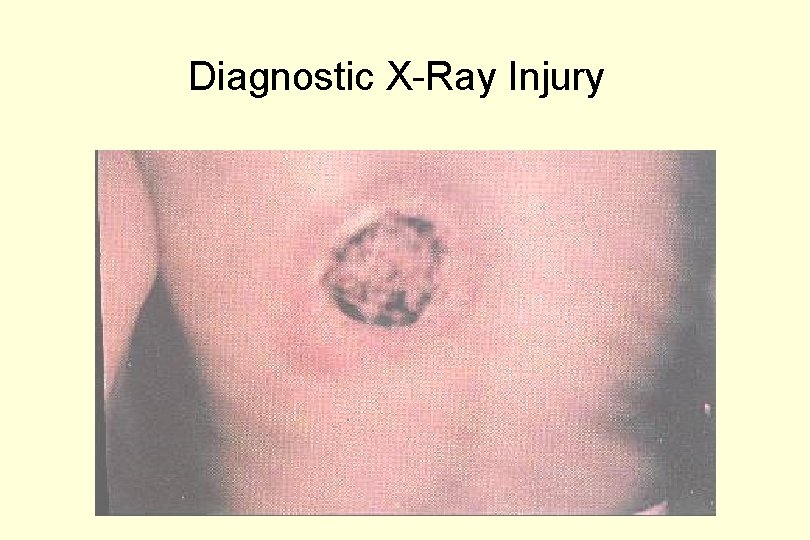
Diagnostic X-Ray Injury

Diagnostic X-ray Injury: Repaired
Acute Radiation Syndromes and Their Management • Key underlying pathophysiology at the cell and organ level • Description of syndromes • Diagnostic procedures • Clinical care 589 -1
Acute Radiation Syndromes • Underlying Cellular Radiation Effects – Mitotic inhibition – Cell killing – Organ malfunction – Vascular reactions • Clinical Manifestations – Hematological – Gastrointestinal – Neurovascular – Pulmonary
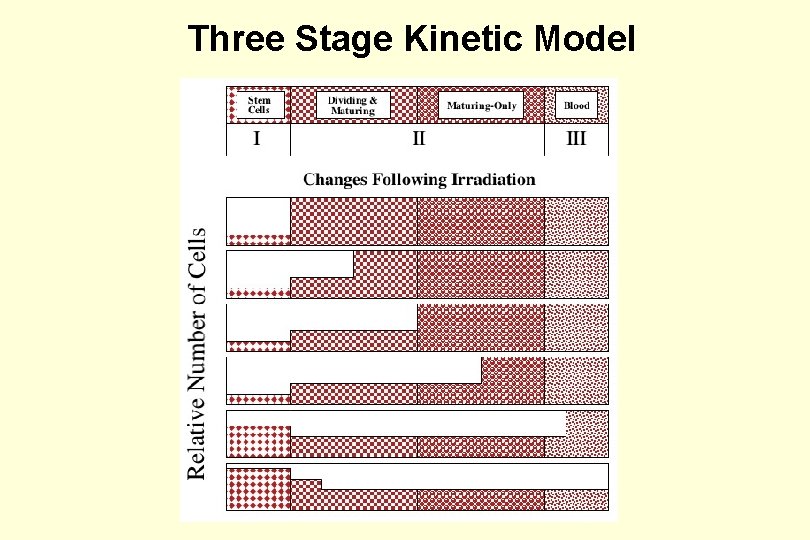
Three Stage Kinetic Model
Prodromal Symptoms & Signs Neurogenic Anorexia Nausea Vomiting Diarrhea Fever Weakness Vascular Conjunctivitis Skin Erythema

Radiation Erythema (PXD 10)
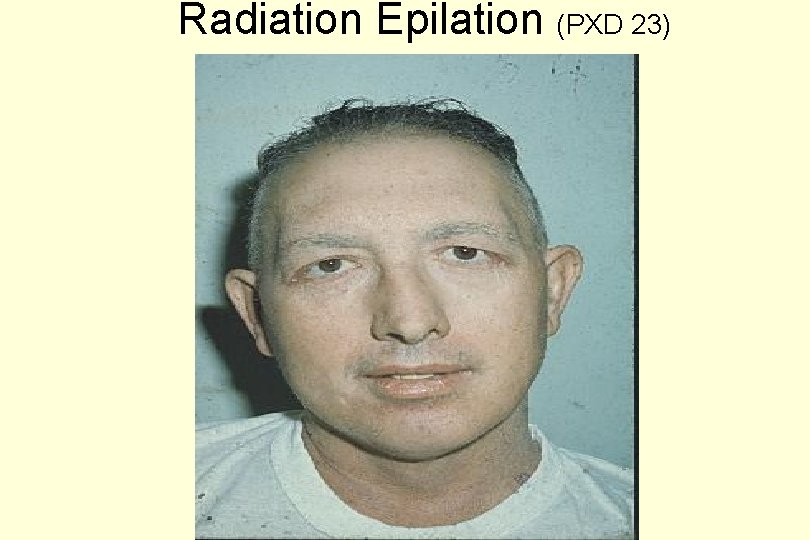
Radiation Epilation (PXD 23)
ARS: 45 Days post-Epilation
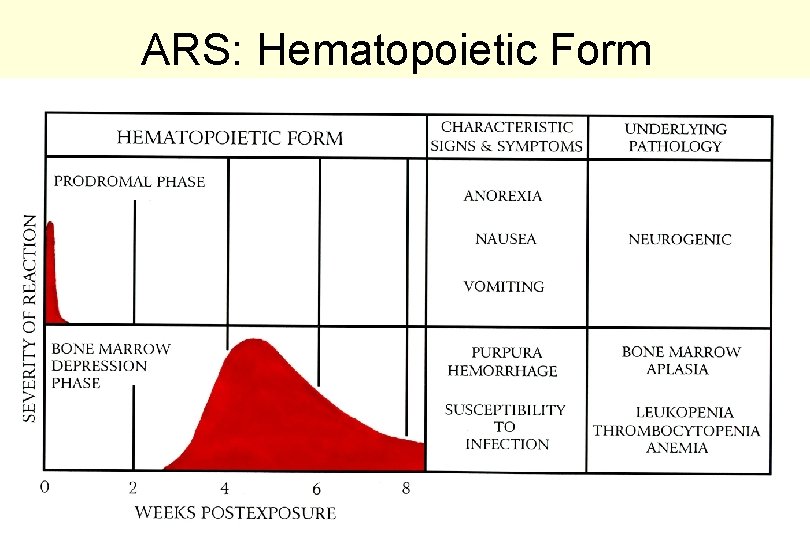
ARS: Hematopoietic Form 38 -C
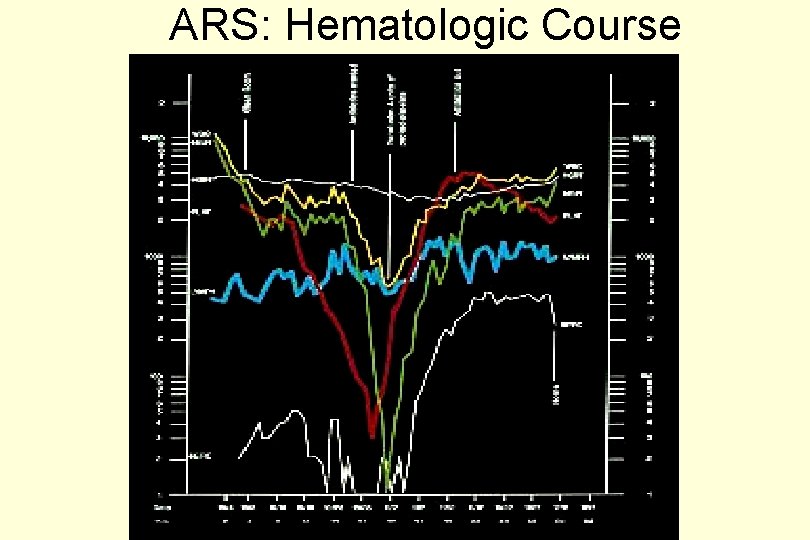
ARS: Hematologic Course
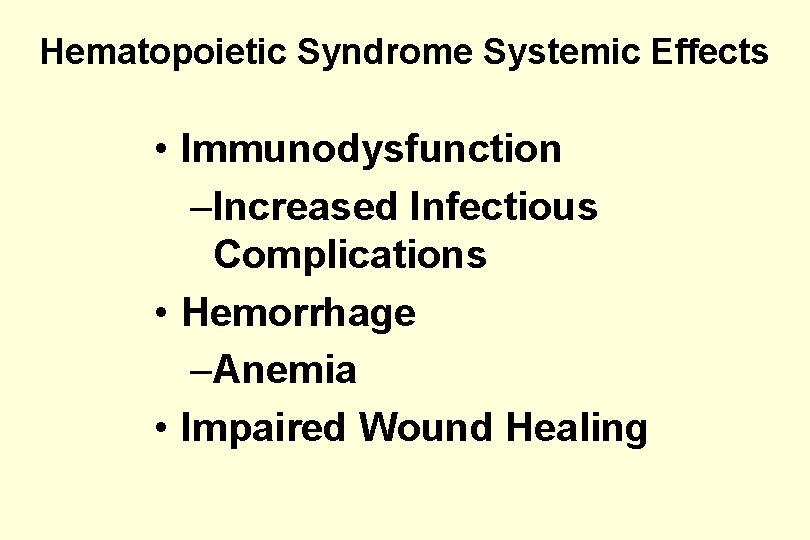
Hematopoietic Syndrome Systemic Effects • Immunodysfunction –Increased Infectious Complications • Hemorrhage –Anemia • Impaired Wound Healing
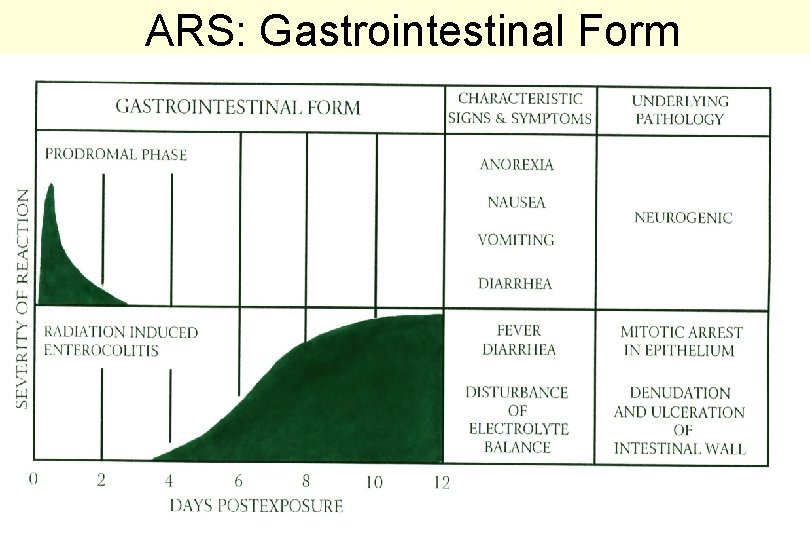
ARS: Gastrointestinal Form 38 -D
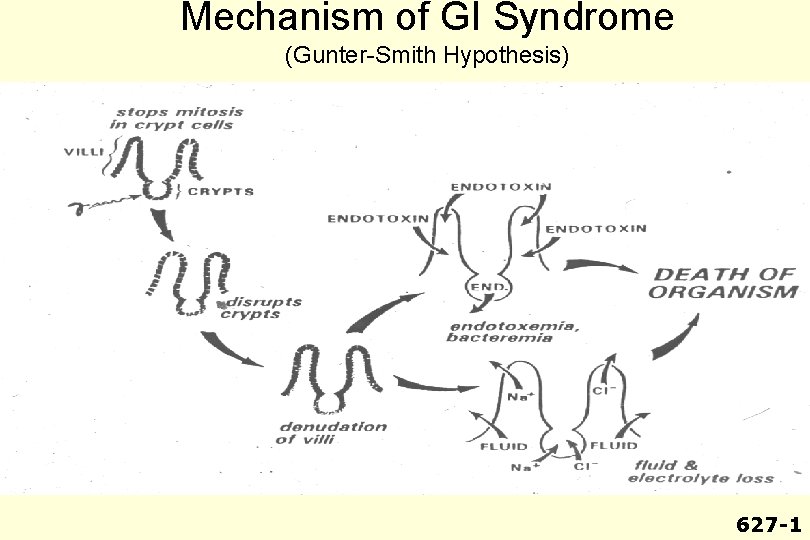
Mechanism of GI Syndrome (Gunter-Smith Hypothesis) 627 -1

GI Syndrome Systemic Effects • Malabsorption • Ileus – Vomiting – Abdominal distention • Fluid and Electrolyte Shifts – Dehydration – Acute renal failure – Cardiovascular • GI Bleeding • Sepsis
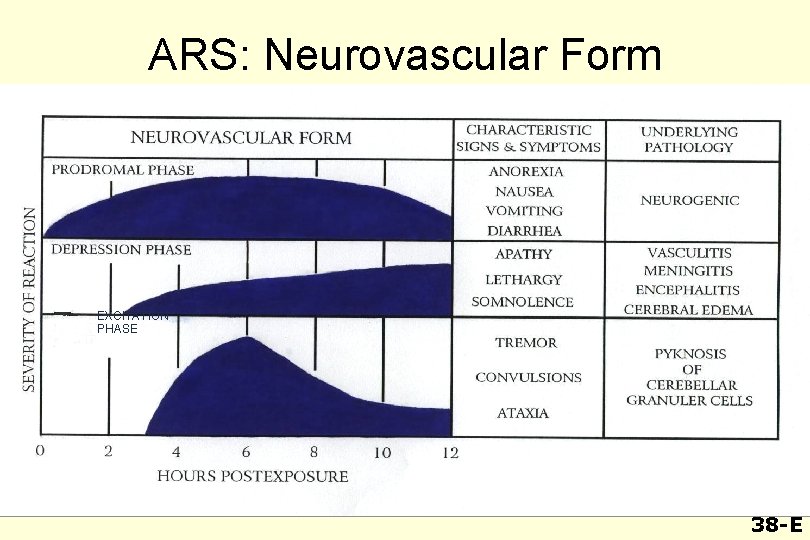
ARS: Neurovascular Form EXCITATION PHASE 38 -E
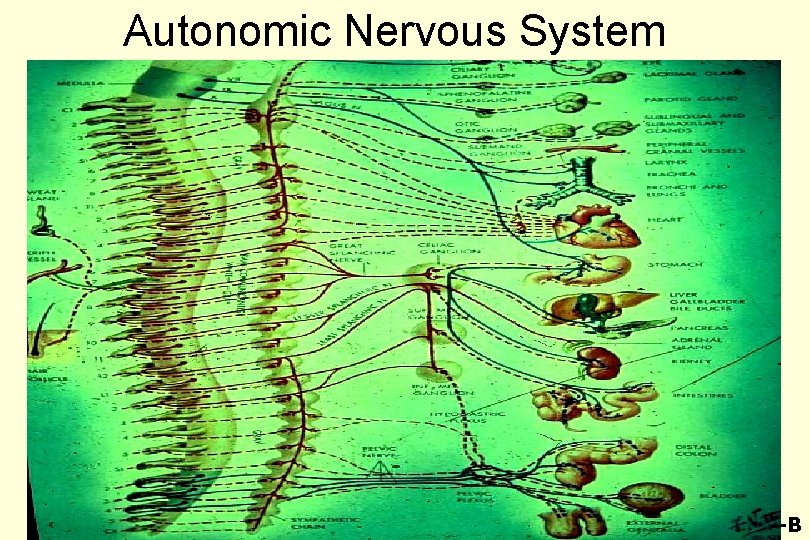
Autonomic Nervous System 49 -B
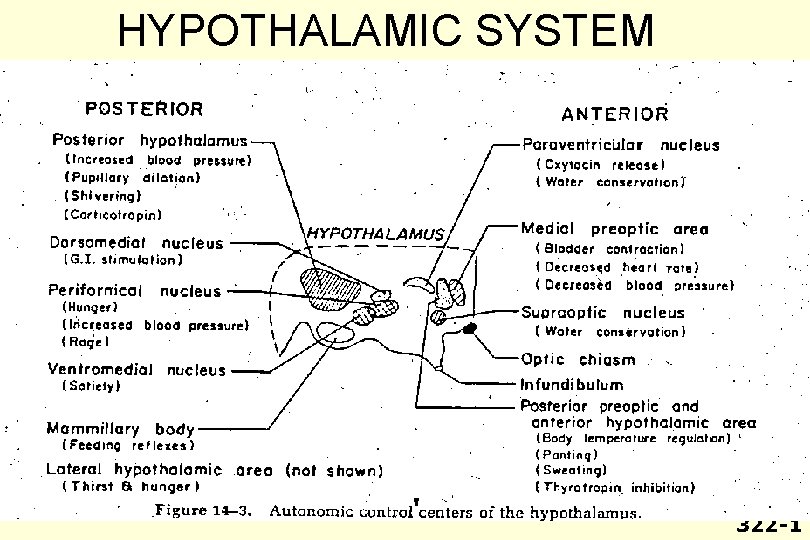
HYPOTHALAMIC SYSTEM 322 -1
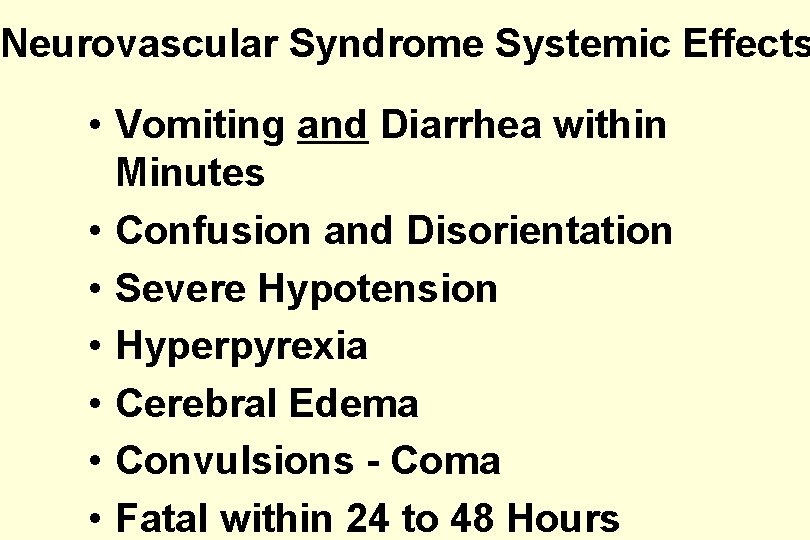
Neurovascular Syndrome Systemic Effects • Vomiting and Diarrhea within Minutes • Confusion and Disorientation • Severe Hypotension • Hyperpyrexia • Cerebral Edema • Convulsions - Coma • Fatal within 24 to 48 Hours
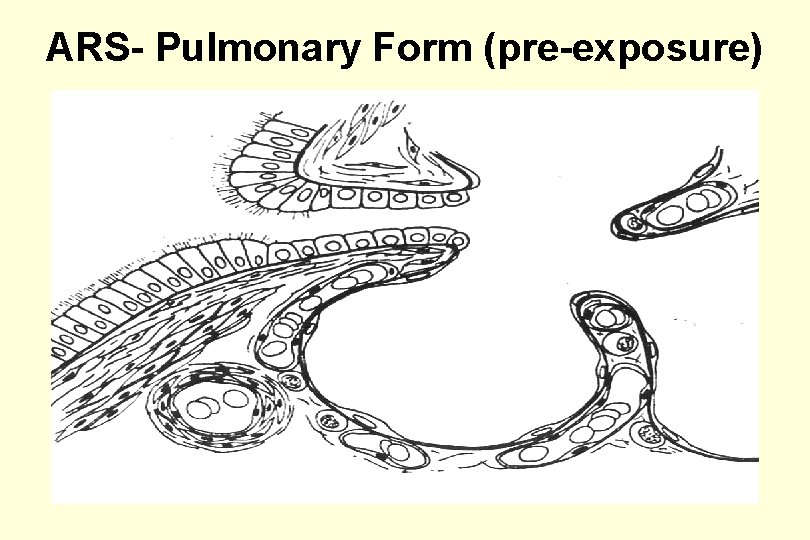
ARS- Pulmonary Form (pre-exposure)
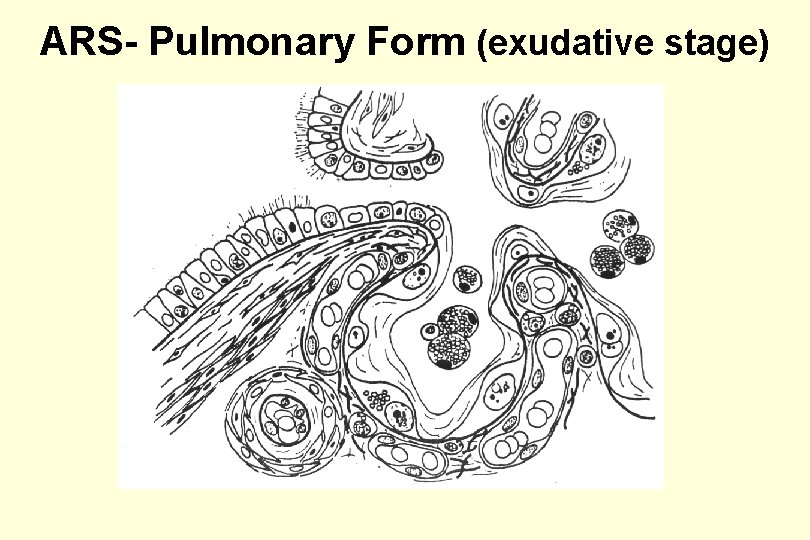
ARS- Pulmonary Form (exudative stage)
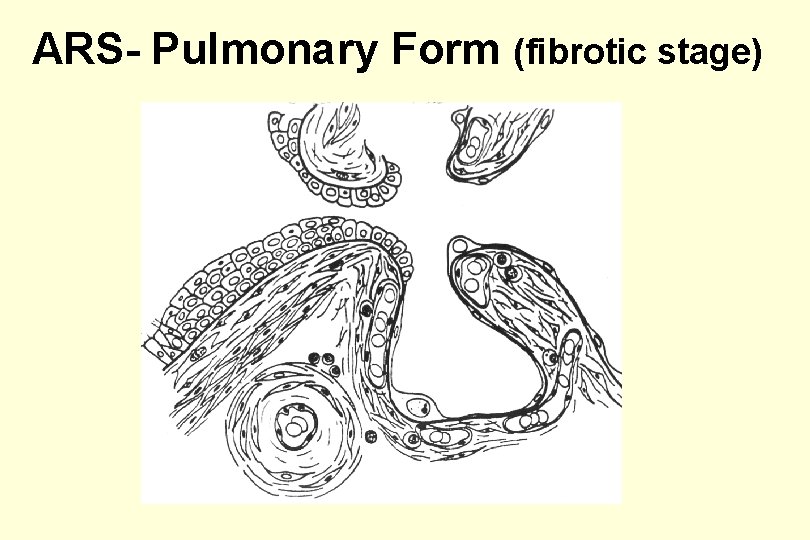
ARS- Pulmonary Form (fibrotic stage)
Pulmonary Syndrome Systemic Effects • Early Phase – Dyspnea – Cough – Pulmonary Edema – Acute Respiratory Distress Syndrome • Late Phase – Interstitial Fibrosis – Interstitial Pneumonitis – Chronic Respiratory Distress Syndrome
Acute Radiation Syndrome Clinical Management Problems • Psychological Stress • Infection – Bacterial, viral, fungal, CMV, herpes • • Hemorrhage Radiation Enterocolitis Radiation Pneumonitis Combined Injuries – Radiation plus trauma, burns, etc. 648 -4
General Treatment Plan for External Exposure • Provide Psychological Support – Professional – Family – Clergy • Use Symptomatic Treatment – Antiemetics – Analgesics • Prevent Infection and Hemorrhage – Reverse Isolation – Antibiotics – Blood Products
General Treatment Plan (cont. ) • Maintain Hydration and Nutrition – Fluids – Electrolytes – Nutrients • Encourage Cell Renewal – Growth Factors – Stem Cells • Control Inflammatory Response – Steroids – Vasodilators
Psychological Stress Reducers • One Responsible Decision-Maker • Realistic Appraisal of Problem and Clear Communication • Credible Action Plan and Adequate Resources • Pre-Emergency Education
Infection Problems Secondary to Radiation Pancytopenia • Invasion and colonization of rectal or colonic wall by normal flora • Activation of latent infections • Opportunistic infections –Gram Negative –Staphylococcus Aureus 56 -J
General Anti-Infection Measures in Radiation Pancytopenia • Control Bacterial and Fungal Flora of – Naso-Oro-Pharyngeal Tract – Gastrointestinal Tract • Avoid Disruption of Skin and Mucosa • Introduce Environmental Control • Use Optimal Regimen vs. Overt Infection
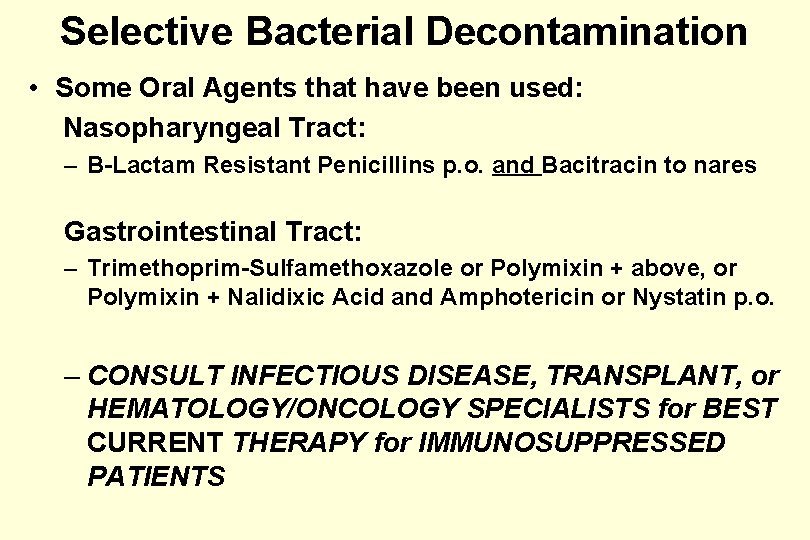
Selective Bacterial Decontamination • Some Oral Agents that have been used: Nasopharyngeal Tract: – B-Lactam Resistant Penicillins p. o. and Bacitracin to nares Gastrointestinal Tract: – Trimethoprim-Sulfamethoxazole or Polymixin + above, or Polymixin + Nalidixic Acid and Amphotericin or Nystatin p. o. – CONSULT INFECTIOUS DISEASE, TRANSPLANT, or HEMATOLOGY/ONCOLOGY SPECIALISTS for BEST CURRENT THERAPY for IMMUNOSUPPRESSED PATIENTS
Environmental Control in Radiation Pancytopenia • Air Filtration and Positive Pressure • Reverse Isolation Procedures • Dietary Considerations • Special Precautions for Skin Punctures • Limitation of Attending Personnel
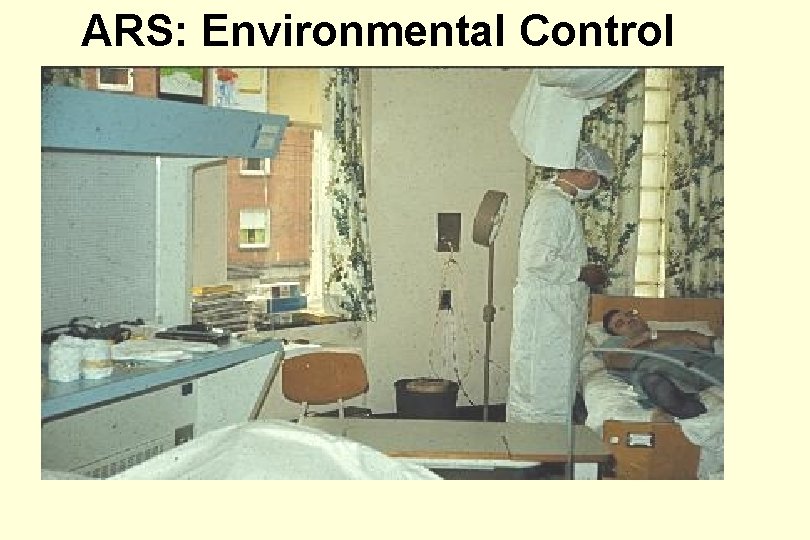
ARS: Environmental Control
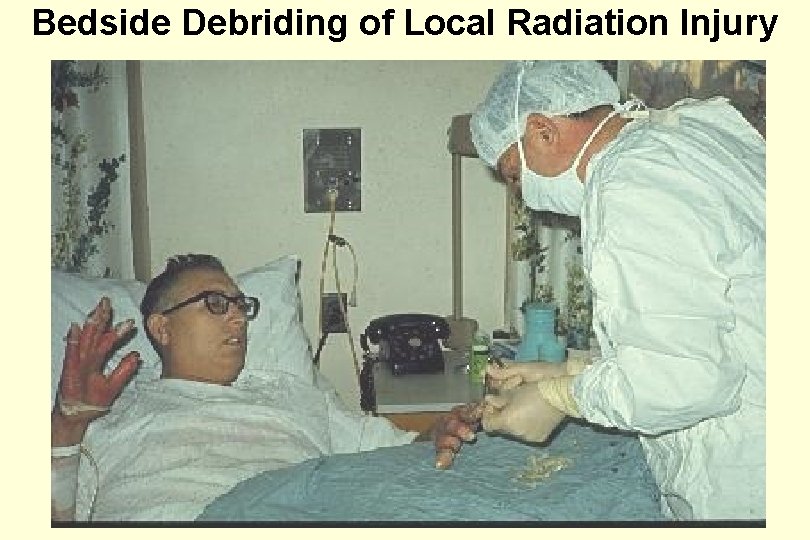
Bedside Debriding of Local Radiation Injury
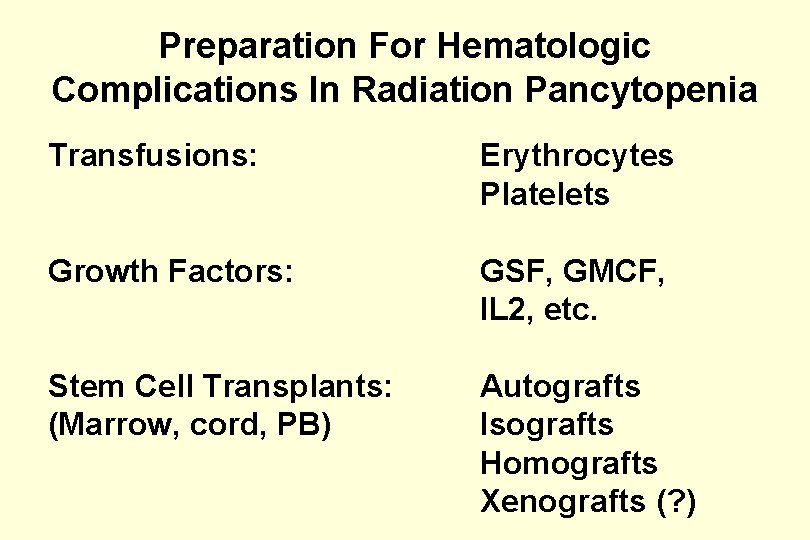
Preparation For Hematologic Complications In Radiation Pancytopenia Transfusions: Erythrocytes Platelets Growth Factors: GSF, GMCF, IL 2, etc. Stem Cell Transplants: (Marrow, cord, PB) Autografts Isografts Homografts Xenografts (? )
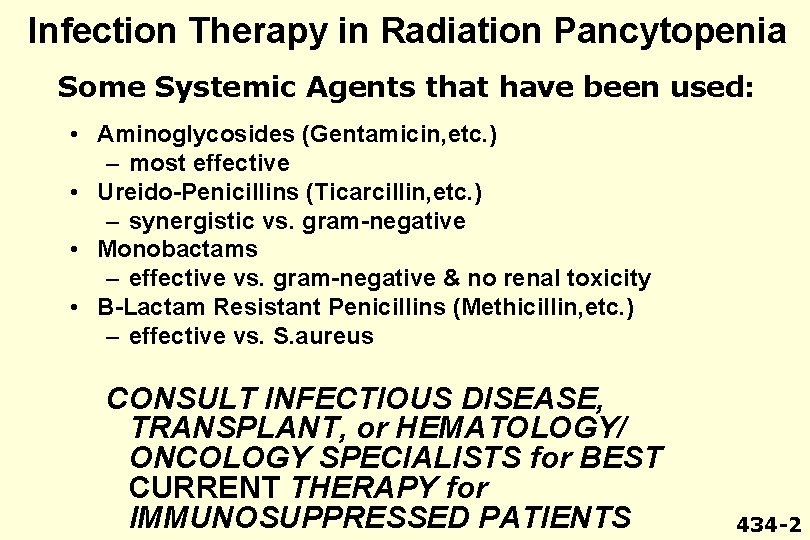
Infection Therapy in Radiation Pancytopenia Some Systemic Agents that have been used: • Aminoglycosides (Gentamicin, etc. ) – most effective • Ureido-Penicillins (Ticarcillin, etc. ) – synergistic vs. gram-negative • Monobactams – effective vs. gram-negative & no renal toxicity • B-Lactam Resistant Penicillins (Methicillin, etc. ) – effective vs. S. aureus CONSULT INFECTIOUS DISEASE, TRANSPLANT, or HEMATOLOGY/ ONCOLOGY SPECIALISTS for BEST CURRENT THERAPY for IMMUNOSUPPRESSED PATIENTS 434 -2
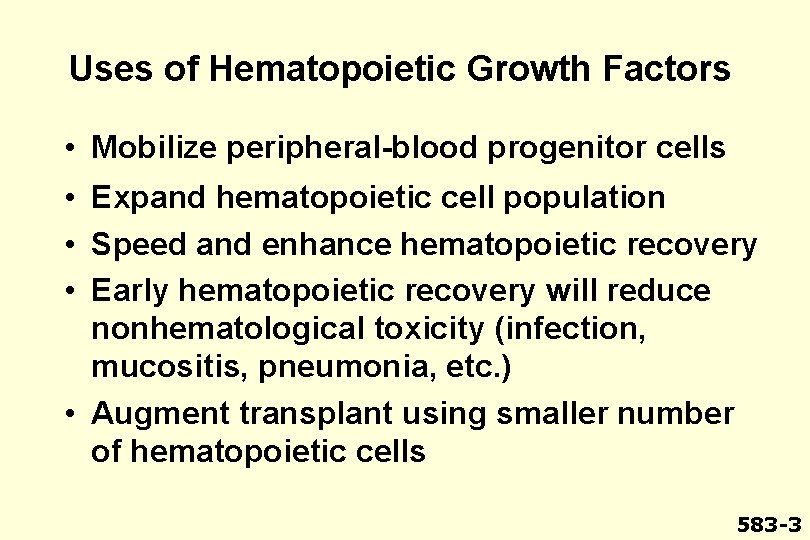
Uses of Hematopoietic Growth Factors • Mobilize peripheral-blood progenitor cells • Expand hematopoietic cell population • Speed and enhance hematopoietic recovery • Early hematopoietic recovery will reduce nonhematological toxicity (infection, mucositis, pneumonia, etc. ) • Augment transplant using smaller number of hematopoietic cells 583 -3
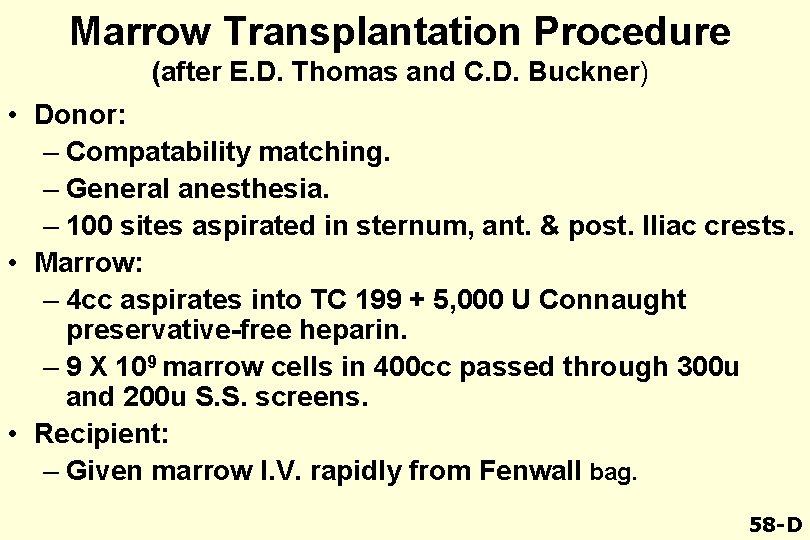
Marrow Transplantation Procedure (after E. D. Thomas and C. D. Buckner) • Donor: – Compatability matching. – General anesthesia. – 100 sites aspirated in sternum, ant. & post. Iliac crests. • Marrow: – 4 cc aspirates into TC 199 + 5, 000 U Connaught preservative-free heparin. – 9 X 109 marrow cells in 400 cc passed through 300 u and 200 u S. S. screens. • Recipient: – Given marrow I. V. rapidly from Fenwall bag. 58 -D
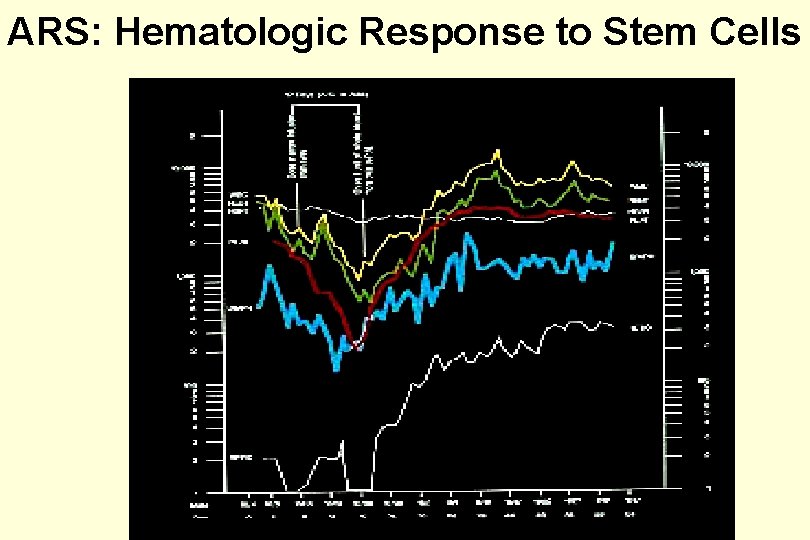
ARS: Hematologic Response to Stem Cells
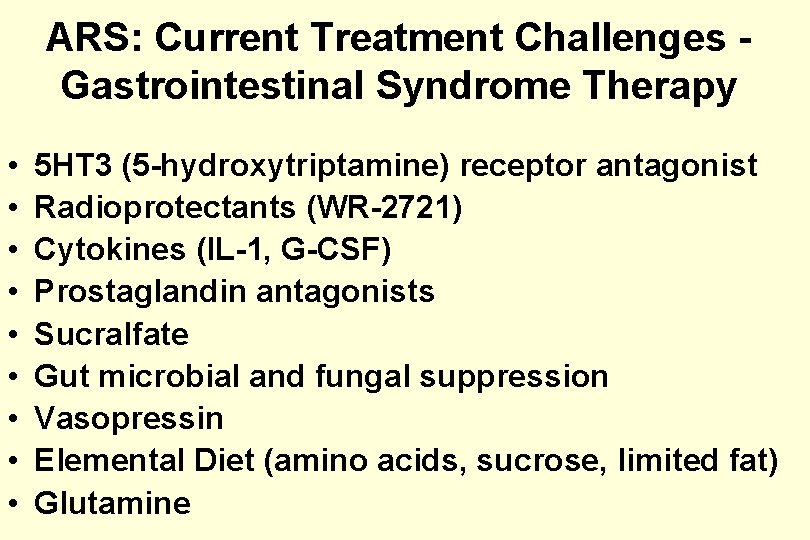
ARS: Current Treatment Challenges Gastrointestinal Syndrome Therapy • • • 5 HT 3 (5 -hydroxytriptamine) receptor antagonist Radioprotectants (WR-2721) Cytokines (IL-1, G-CSF) Prostaglandin antagonists Sucralfate Gut microbial and fungal suppression Vasopressin Elemental Diet (amino acids, sucrose, limited fat) Glutamine
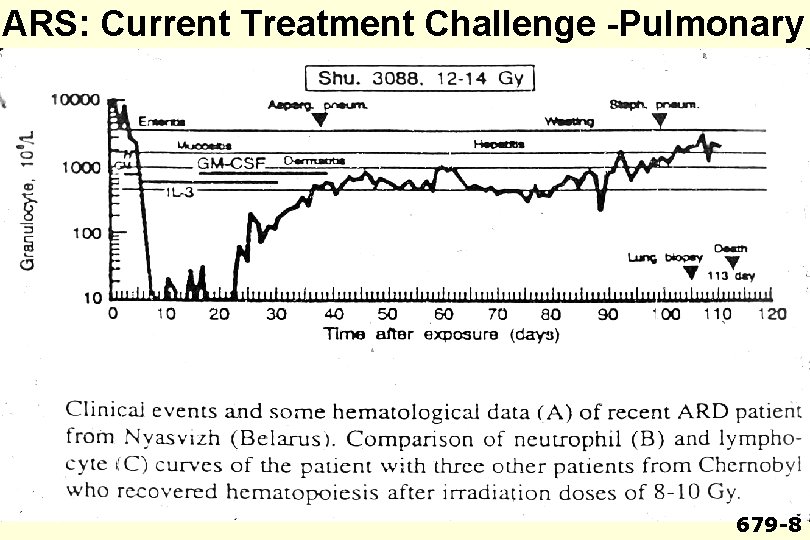
ARS: Current Treatment Challenge -Pulmonary 679 -8
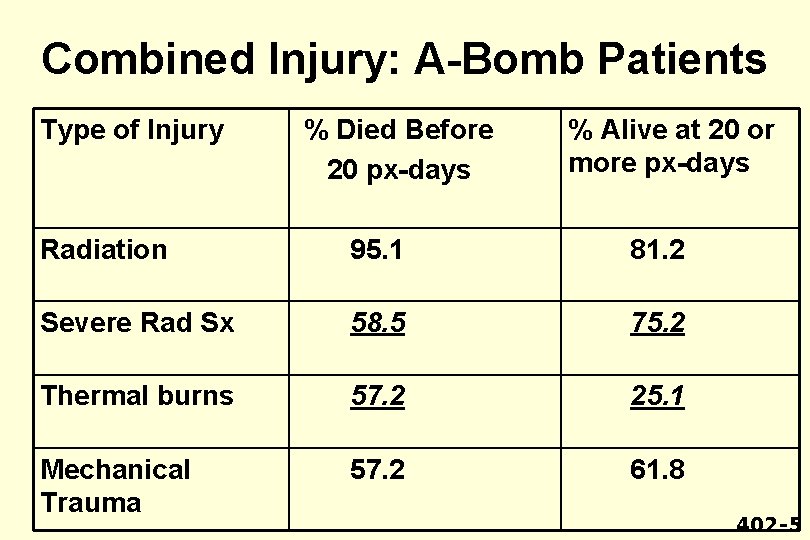
Combined Injury: A-Bomb Patients Type of Injury % Died Before 20 px-days % Alive at 20 or more px-days Radiation 95. 1 81. 2 Severe Rad Sx 58. 5 75. 2 Thermal burns 57. 2 25. 1 Mechanical Trauma 57. 2 61. 8 402 -5
ARS: General Therapeutic Approach • • • Provide Psychological Support Use Symptomatic Treatment Prevent Infection and Hemorrhage Maintain Hydration and Nutrition Encourage Cell Renewal Control Inflammatory Response
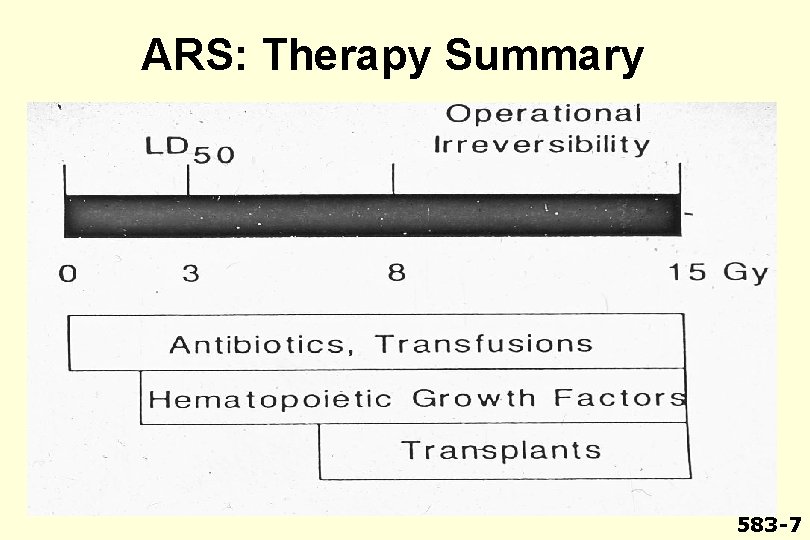
ARS: Therapy Summary 583 -7
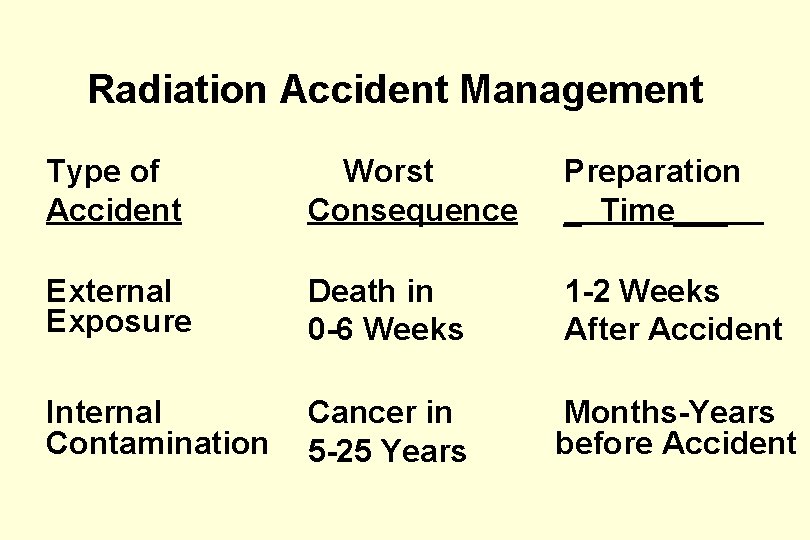
Radiation Accident Management Type of Accident Worst Consequence Preparation _ Time___ External Exposure Death in 0 -6 Weeks 1 -2 Weeks After Accident Internal Contamination Cancer in 5 -25 Years Months-Years before Accident
Internal Exposure Variables Routes of Entry: – Inhalation, Ingestion, Injection and Absorption Decay Rates and energies Chemical Compounds, Solubility, Particle Size, etc. Time and Duration Radionuclides and Forms Metabolic Behavior – Deposition, Retention, Elimination and Critical Organs
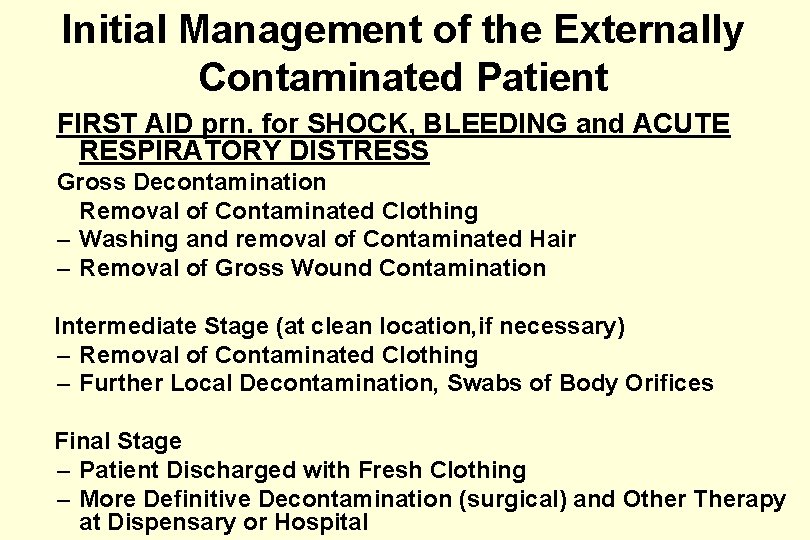
Initial Management of the Externally Contaminated Patient FIRST AID prn. for SHOCK, BLEEDING and ACUTE RESPIRATORY DISTRESS Gross Decontamination Removal of Contaminated Clothing – Washing and removal of Contaminated Hair – Removal of Gross Wound Contamination Intermediate Stage (at clean location, if necessary) – Removal of Contaminated Clothing – Further Local Decontamination, Swabs of Body Orifices Final Stage – Patient Discharged with Fresh Clothing – More Definitive Decontamination (surgical) and Other Therapy at Dispensary or Hospital
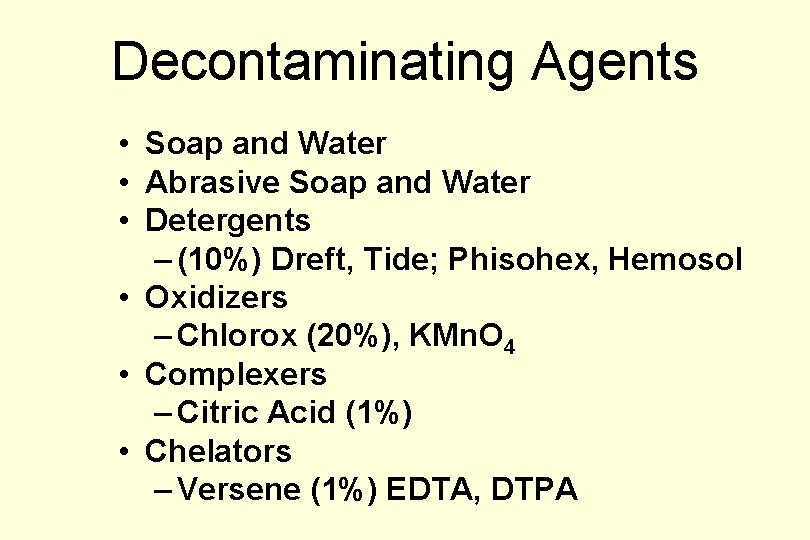
Decontaminating Agents • Soap and Water • Abrasive Soap and Water • Detergents – (10%) Dreft, Tide; Phisohex, Hemosol • Oxidizers – Chlorox (20%), KMn. O 4 • Complexers – Citric Acid (1%) • Chelators – Versene (1%) EDTA, DTPA
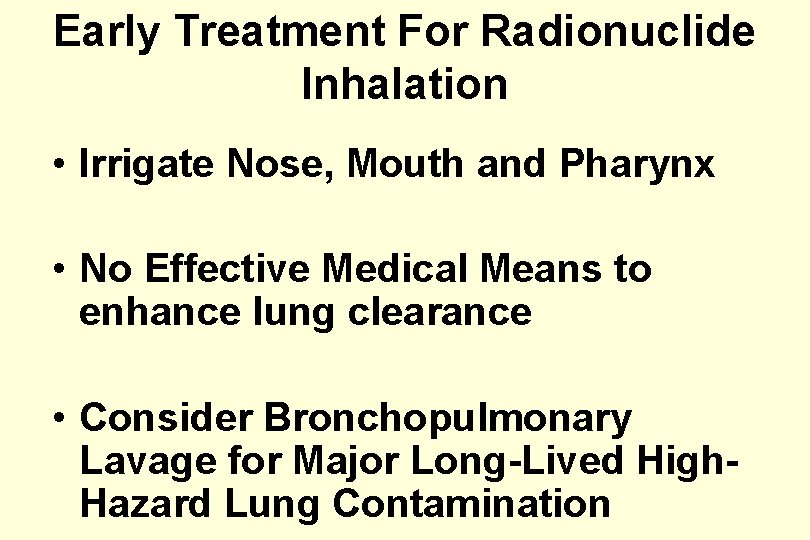
Early Treatment For Radionuclide Inhalation • Irrigate Nose, Mouth and Pharynx • No Effective Medical Means to enhance lung clearance • Consider Bronchopulmonary Lavage for Major Long-Lived High. Hazard Lung Contamination
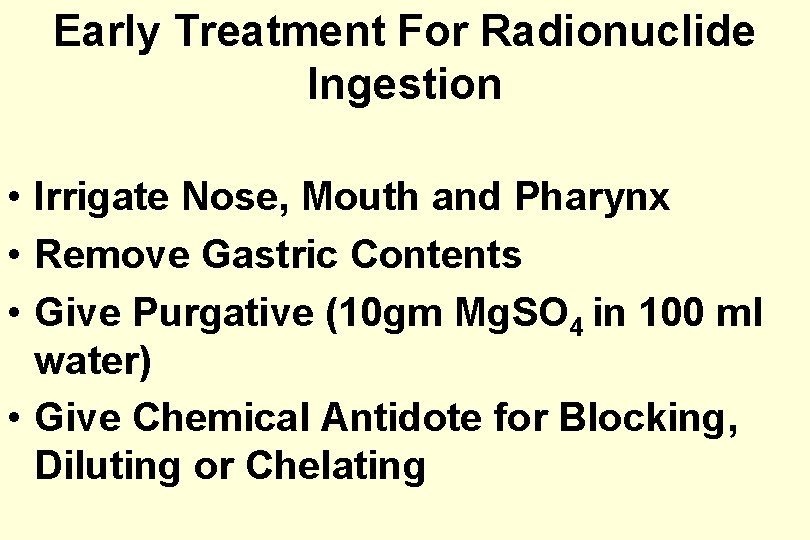
Early Treatment For Radionuclide Ingestion • Irrigate Nose, Mouth and Pharynx • Remove Gastric Contents • Give Purgative (10 gm Mg. SO 4 in 100 ml water) • Give Chemical Antidote for Blocking, Diluting or Chelating
Early Treatment For Contaminated Wounds • Irrigate Wound – Saline – Water • Decontaminate Skin (But Do Not Injure) – Detergent • Continue Wound Irrigation Until Radiation Level Is Zero or Constant • Treat Wound as Usual – Consider Excision of Embedded Long. Lived High-Hazard Contaminants
Pu-Contaminated Lacerations
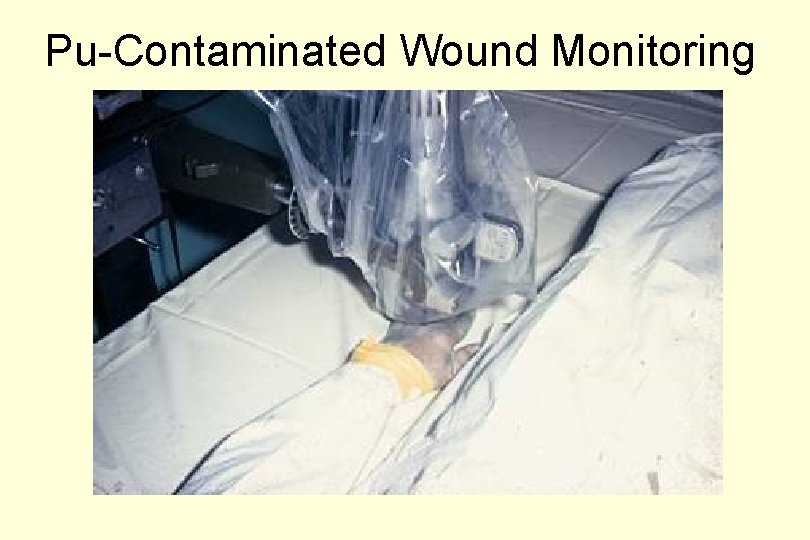
Pu-Contaminated Wound Monitoring
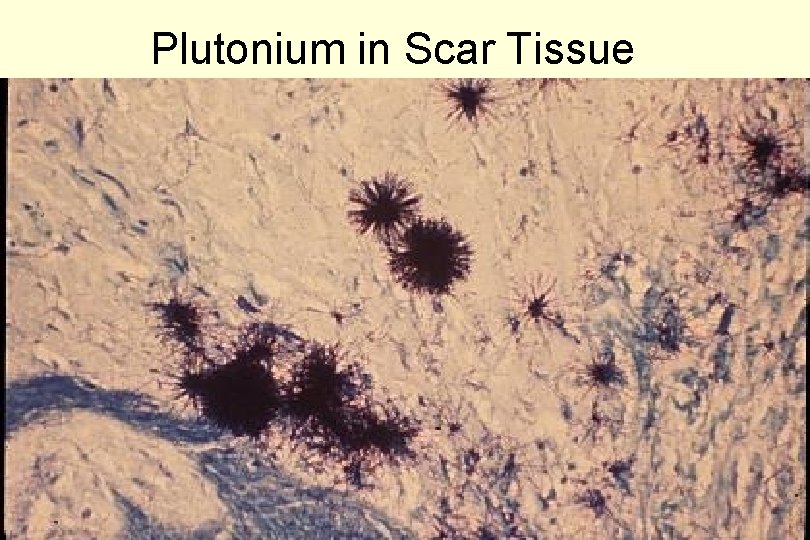
Plutonium in Scar Tissue
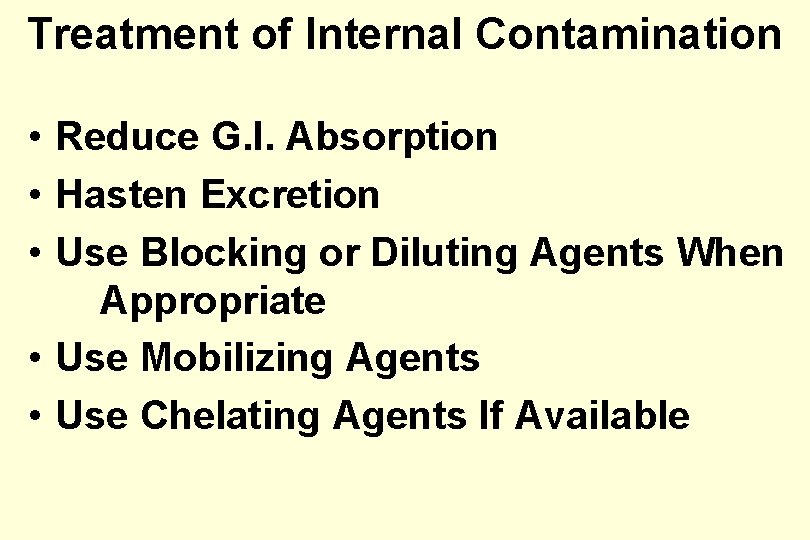
Treatment of Internal Contamination • Reduce G. I. Absorption • Hasten Excretion • Use Blocking or Diluting Agents When Appropriate • Use Mobilizing Agents • Use Chelating Agents If Available
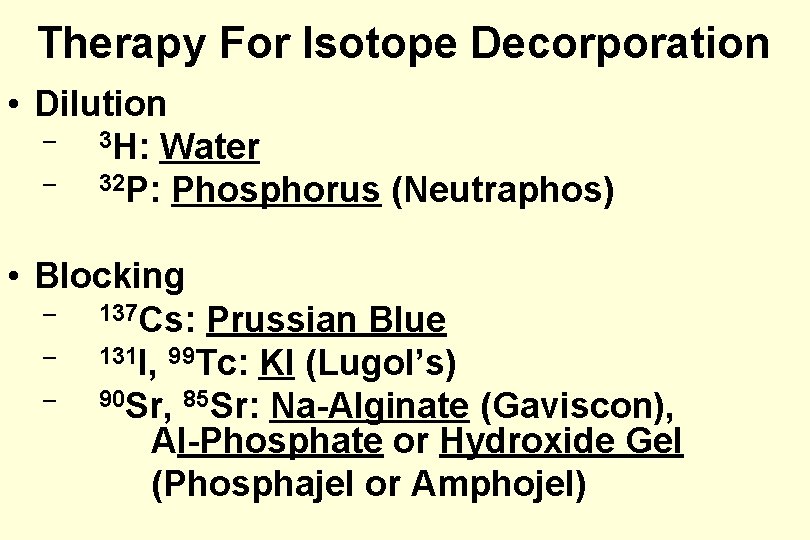
Therapy For Isotope Decorporation • Dilution – 3 H: Water – 32 P: Phosphorus (Neutraphos) • Blocking – 137 Cs: Prussian Blue – 131 I, 99 Tc: KI (Lugol’s) – 90 Sr, 85 Sr: Na-Alginate (Gaviscon), Al-Phosphate or Hydroxide Gel (Phosphajel or Amphojel)
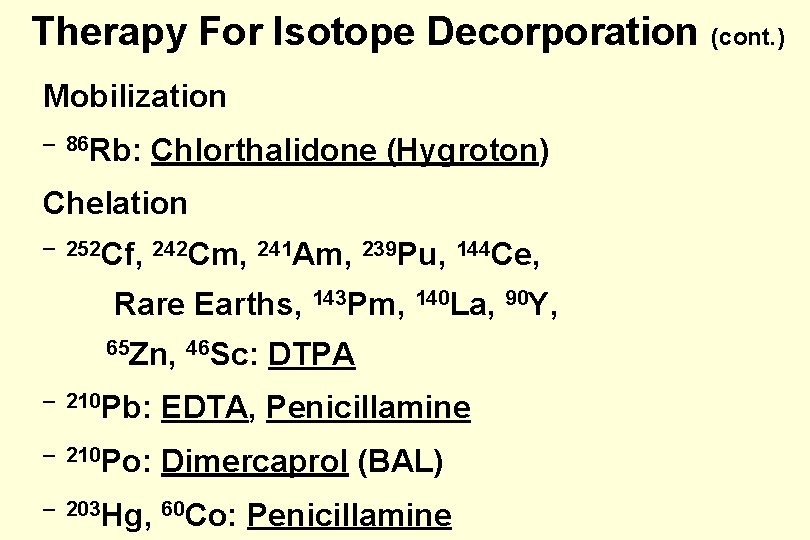
Therapy For Isotope Decorporation (cont. ) Mobilization – 86 Rb: Chlorthalidone (Hygroton) Chelation – 252 Cf, 242 Cm, 241 Am, 239 Pu, 144 Ce, Rare Earths, 143 Pm, 140 La, 90 Y, 65 Zn, 46 Sc: DTPA – 210 Pb: EDTA, Penicillamine – 210 Po: Dimercaprol (BAL) – 203 Hg, 60 Co: Penicillamine
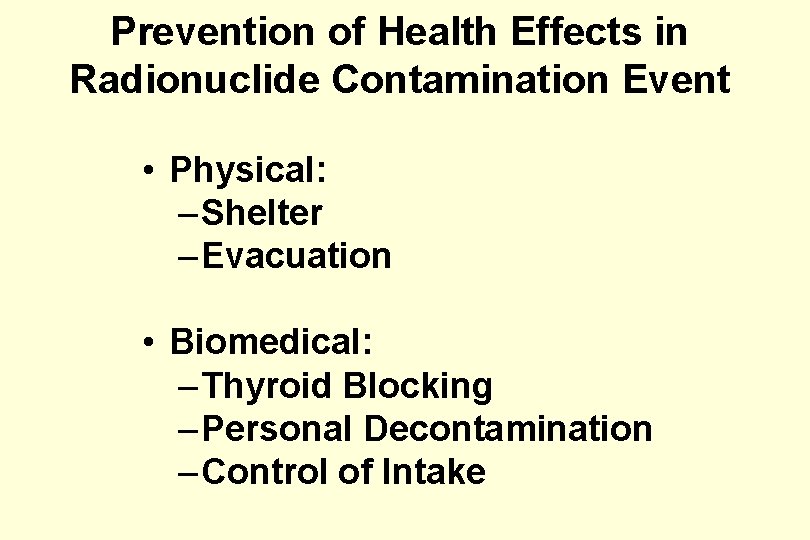
Prevention of Health Effects in Radionuclide Contamination Event • Physical: – Shelter – Evacuation • Biomedical: – Thyroid Blocking – Personal Decontamination – Control of Intake
Bibliography • The Medical Basis for Radiation-Accident Preparedness: The Clinical Care of Victims. Ricks, R. C. , Berger, M. E. and O’Hara, Jr. , F. M. , Editors. Parthenon Publishing Group, New York, 2002. • Medical Management of Radiation Accidents. Gusev, I. A. , Guskova, A. K. and Mettler Jr. , F. A. , Editors, CRC Press, Boca Raton, FL, 2001. • NCRP Report No. 138. Management of Terrorist Events Involving Radioactivity. National Council on Radiation Protection and Measurements Committee 46 -14, John W. Poston, Sr. Chairman; NCRP, Washington, DC, 2001.
• Advances in the Biosciences: Advances in the Treatment of Radiation Injuries. Mac. Vittie, T. J. , Weiss, J. F. , and Browne, D. , Pergamon Press, New York, 1996. • Medical Effects of Ionizing Radiation. 2 nd Edition. Mettler, F. A. Jr, and Upton, A. C. , W. B. Saunders, Philadelphia, PA, 1995. • NCRP Report No. 65, Management of Persons Accidentally Contaminated with Radionuclides. National Council on Radiation Protection and Measurements Committee, George L. Voelz, Chairman; NCRP, Washington, DC, 1980.
- Slides: 74