BASICS OF PACEMAKER DN HISTORY 1958 Senning and
BASICS OF PACEMAKER DN
HISTORY • 1958 – Senning and Elmqvist – Asynchronous (VVI) pacemaker implanted by thoracotomy and functioned for 3 hours – Arne Larsson • First pacemaker patient • Used 23 pulse generators and 5 electrode systems • Died 2001 at age 86 of cancer • 1960 – First atrial triggered pacemaker • 1964 – First on demand pacemaker (DVI) • 1977 – First atrial and ventricular demand pacing (DDD) • 1981 – Rate responsive pacing by QT interval, respiration, and movement • 1994 – Cardiac resynchronization pacing
What is a Pacemaker? A Pacemaker System consists of a Pulse Generator plus Lead (s)
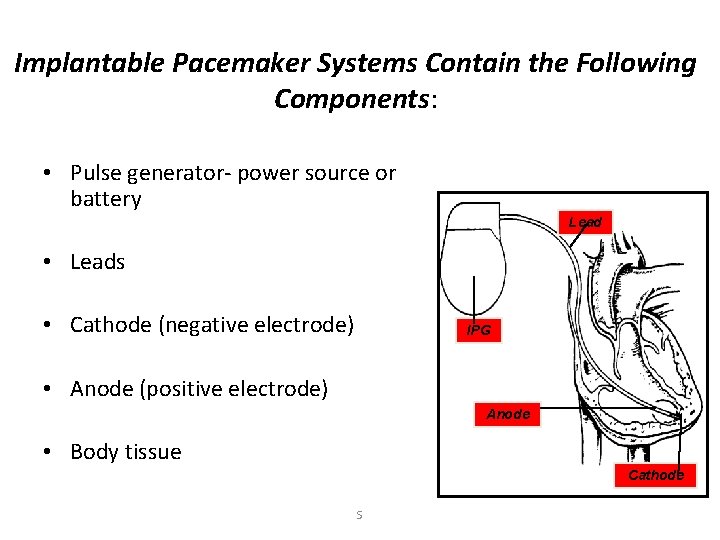
Implantable Pacemaker Systems Contain the Following Components: • Pulse generator- power source or battery Lead • Leads • Cathode (negative electrode) IPG • Anode (positive electrode) Anode • Body tissue Cathode S
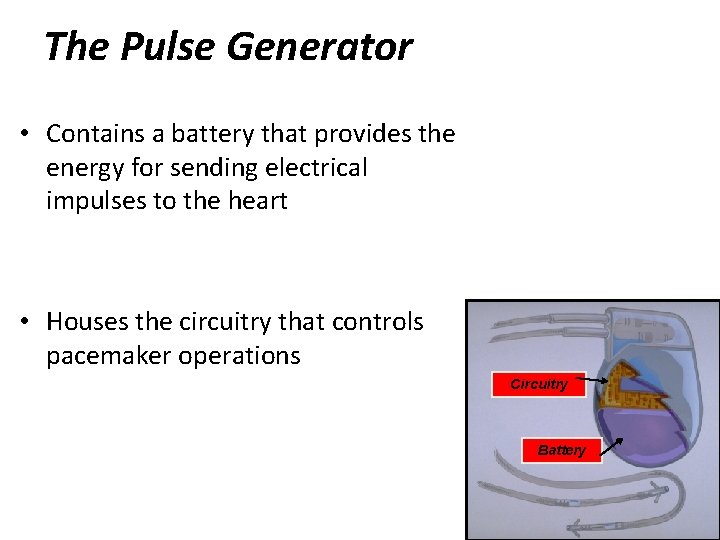
The Pulse Generator • Contains a battery that provides the energy for sending electrical impulses to the heart • Houses the circuitry that controls pacemaker operations Circuitry Battery
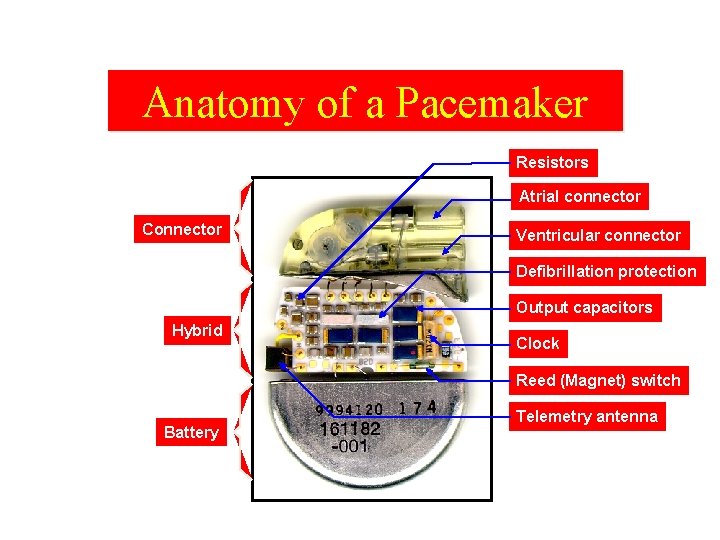
Anatomy of a Pacemaker Resistors Atrial connector Connector Ventricular connector Defibrillation protection Output capacitors Hybrid Clock Reed (Magnet) switch Battery Telemetry antenna
General Characteristics of Pacemaker Batteries • Hermeticity, as defined by the pacing industry, is an extremely low rate of helium gas leakage from the sealed pacemaker container • low rate of self-discharge • lithium iodine -a long shelf life and high energy density • DDD drains a battery more rapidly
Power source • Longevity in single chamber pacemaker is 7 to 12 years. • For dual chamber longevity is 6 to 10 years. • Most pacemakers generate 2. 8 v in the beginning of life which becomes 2. 1 to 2. 4 v towards end of life. 9
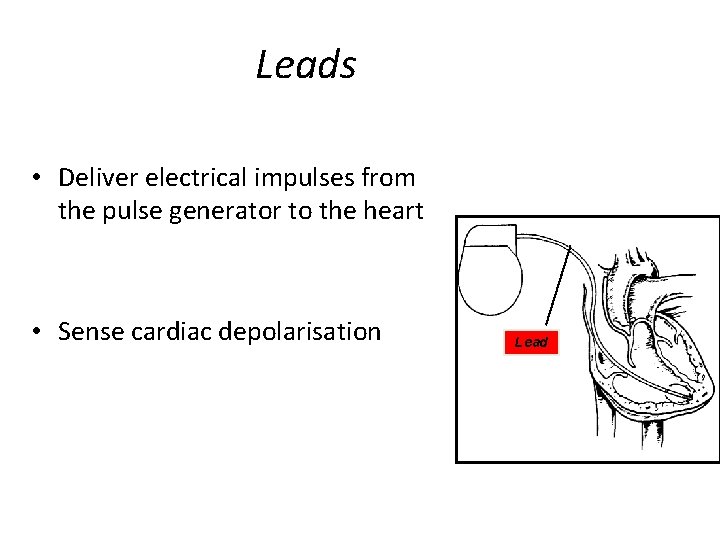
Leads • Deliver electrical impulses from the pulse generator to the heart • Sense cardiac depolarisation Lead
Lead Characterization • Position within the heart – Endocardial or transvenous leads – Epicardial leads • Polarity – Unipolar – Bipolar • Fixation mechanism – Active/Screw-in – Passive/Tined • Shape – Straight – J-shaped used in the atrium • Insulator – Silicone – Polyurethane
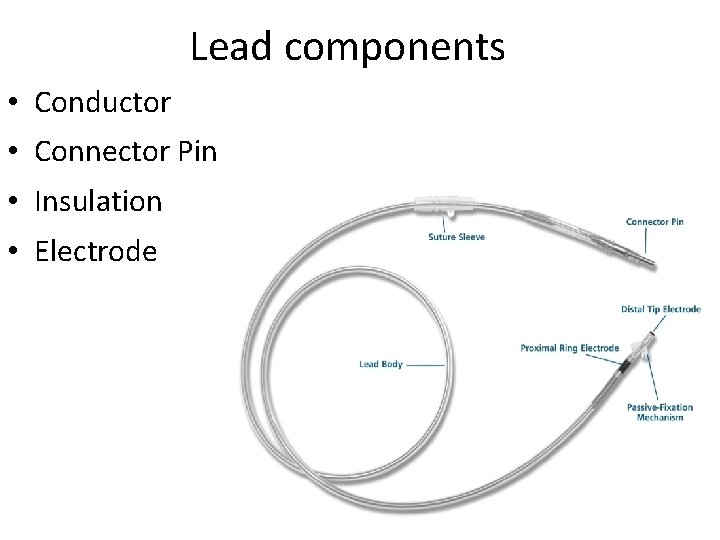
Lead components • Conductor • Connector Pin • Insulation • Electrode
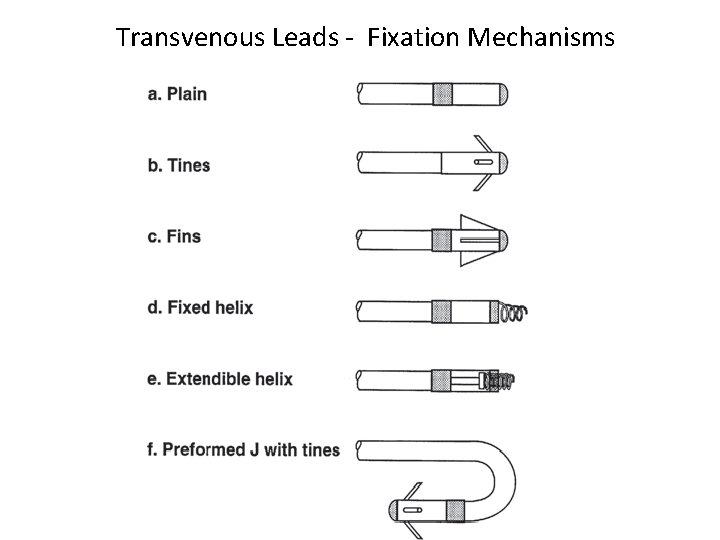
Transvenous Leads - Fixation Mechanisms
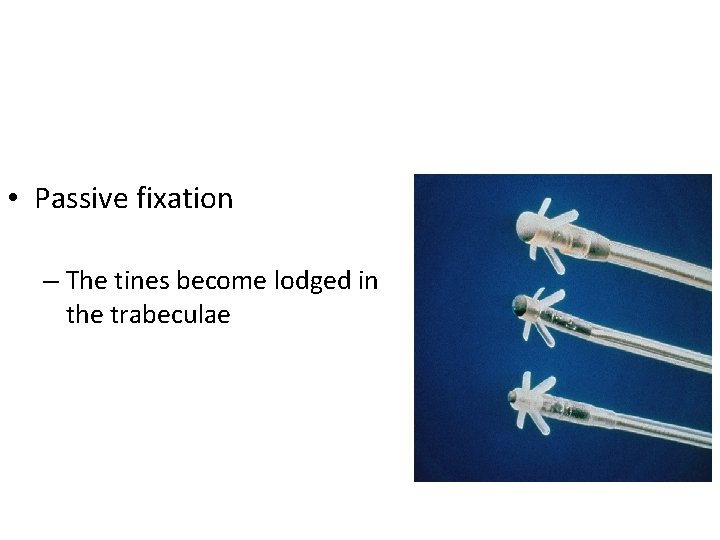
• Passive fixation – The tines become lodged in the trabeculae
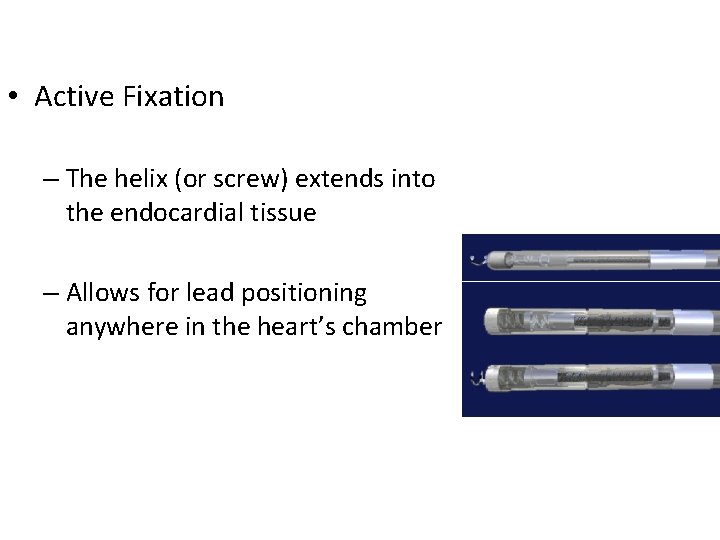
• Active Fixation – The helix (or screw) extends into the endocardial tissue – Allows for lead positioning anywhere in the heart’s chamber
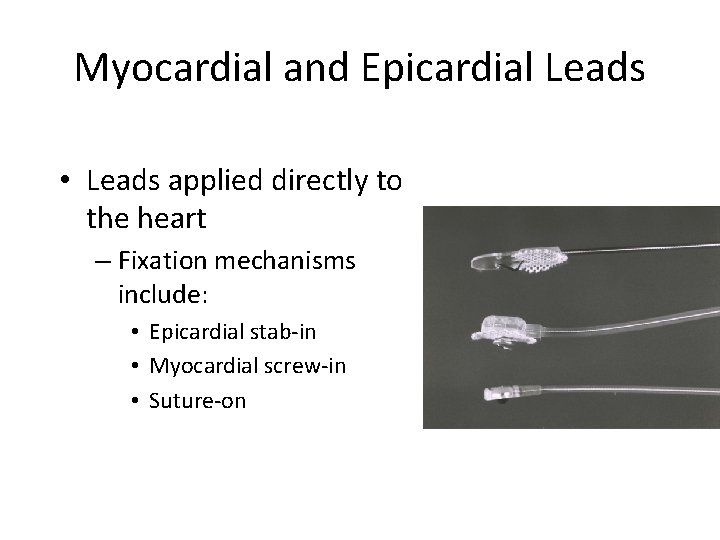
Myocardial and Epicardial Leads • Leads applied directly to the heart – Fixation mechanisms include: • Epicardial stab-in • Myocardial screw-in • Suture-on
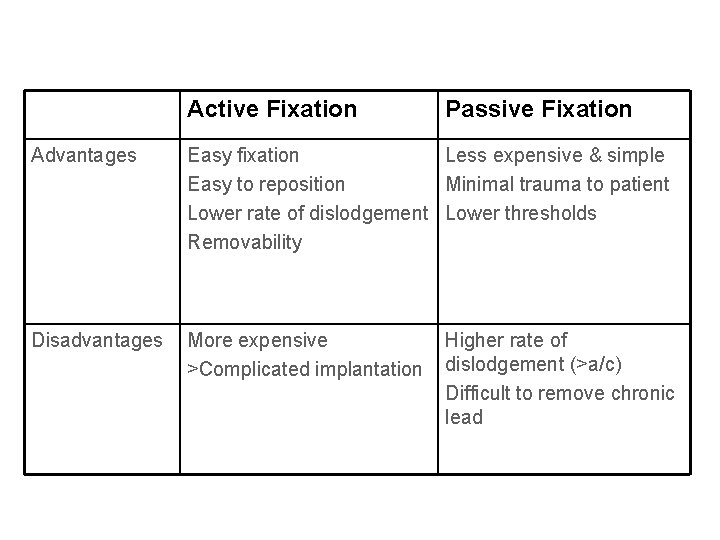
Active Fixation Passive Fixation Advantages Easy fixation Less expensive & simple Easy to reposition Minimal trauma to patient Lower rate of dislodgement Lower thresholds Removability Disadvantages More expensive >Complicated implantation Higher rate of dislodgement (>a/c) Difficult to remove chronic lead
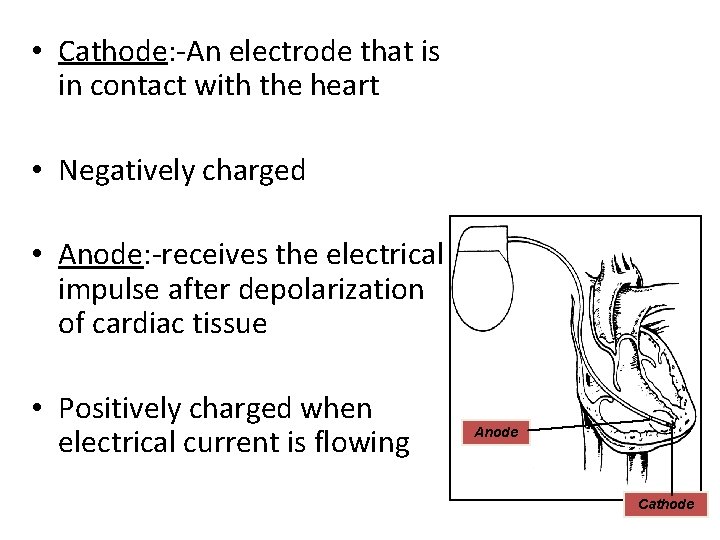
• Cathode: -An electrode that is in contact with the heart • Negatively charged • Anode: -receives the electrical impulse after depolarization of cardiac tissue • Positively charged when electrical current is flowing Anode Cathode
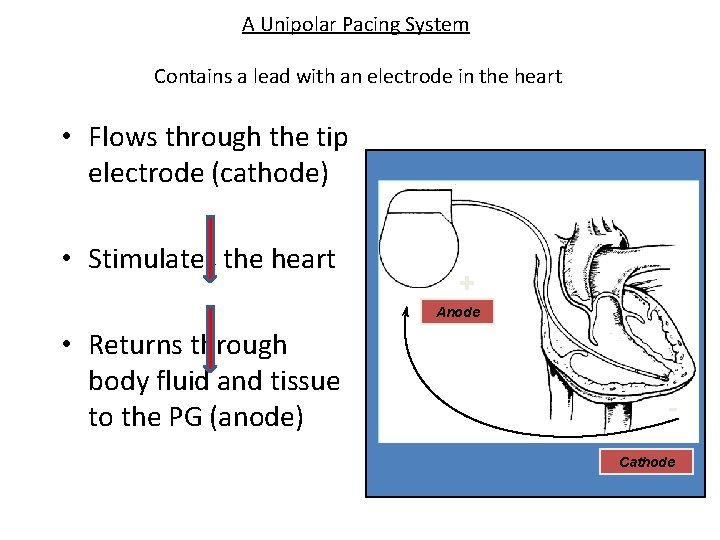
A Unipolar Pacing System Contains a lead with an electrode in the heart • Flows through the tip electrode (cathode) • Stimulates the heart + Anode • Returns through body fluid and tissue to the PG (anode) Cathode
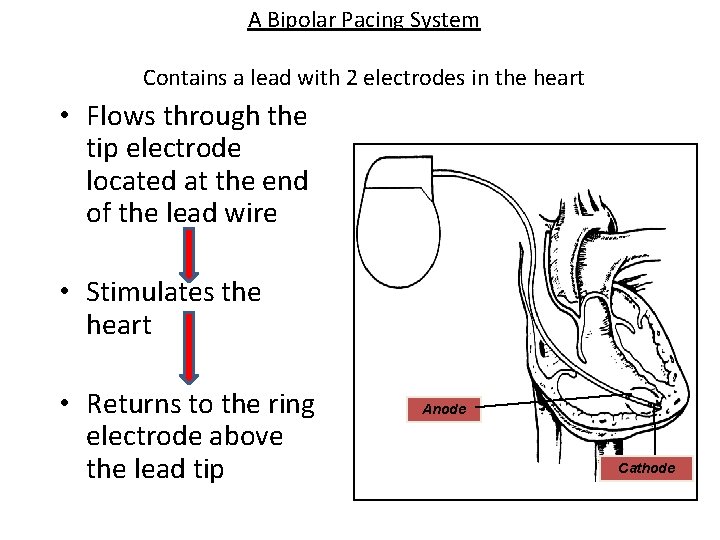
A Bipolar Pacing System Contains a lead with 2 electrodes in the heart • Flows through the tip electrode located at the end of the lead wire • Stimulates the heart • Returns to the ring electrode above the lead tip Anode Cathode
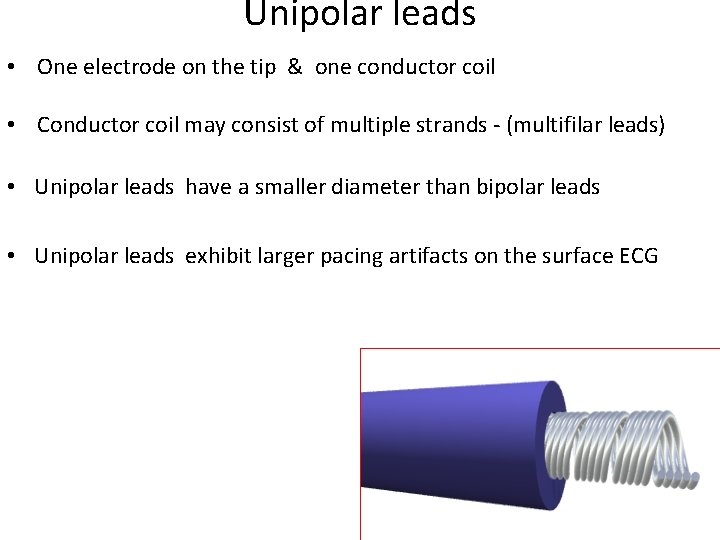
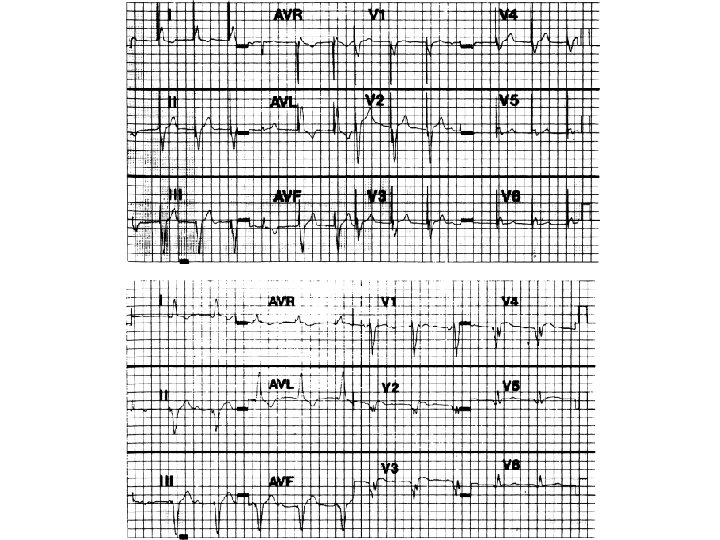
Unipolar leads • One electrode on the tip & one conductor coil • Conductor coil may consist of multiple strands - (multifilar leads) • Unipolar leads have a smaller diameter than bipolar leads • Unipolar leads exhibit larger pacing artifacts on the surface ECG
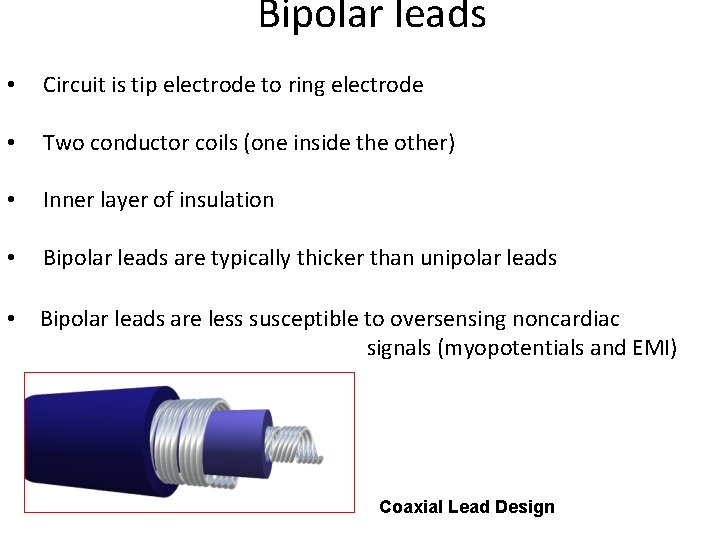
Bipolar leads • Circuit is tip electrode to ring electrode • Two conductor coils (one inside the other) • Inner layer of insulation • Bipolar leads are typically thicker than unipolar leads • Bipolar leads are less susceptible to oversensing noncardiac signals (myopotentials and EMI) Coaxial Lead Design
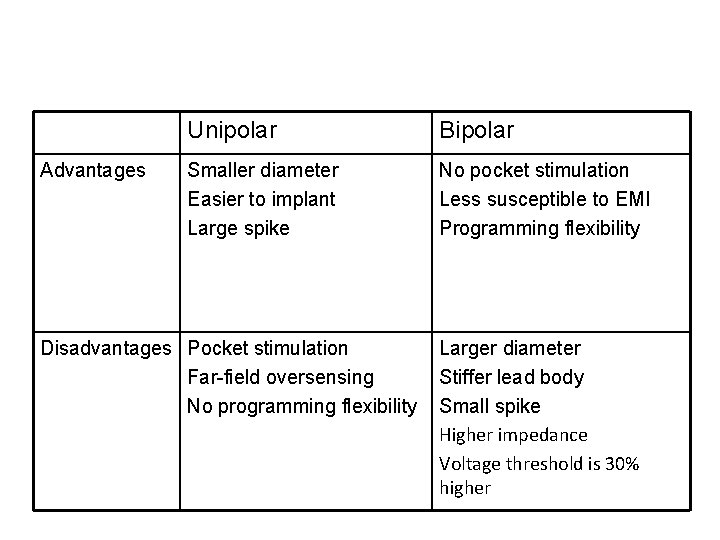
Advantages Unipolar Bipolar Smaller diameter Easier to implant Large spike No pocket stimulation Less susceptible to EMI Programming flexibility Disadvantages Pocket stimulation Far-field oversensing No programming flexibility Larger diameter Stiffer lead body Small spike Higher impedance Voltage threshold is 30% higher
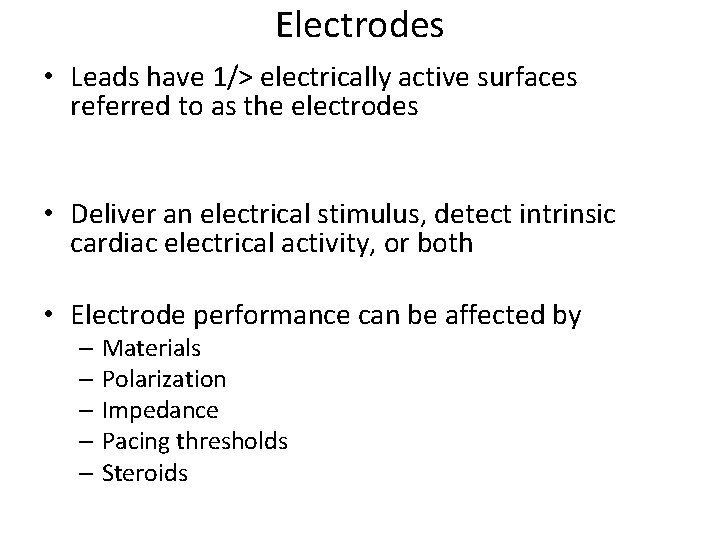
Electrodes • Leads have 1/> electrically active surfaces referred to as the electrodes • Deliver an electrical stimulus, detect intrinsic cardiac electrical activity, or both • Electrode performance can be affected by – Materials – Polarization – Impedance – Pacing thresholds – Steroids
Electrode Materials • The ideal material for an electrode – Porous (allows tissue ingrowth) – Should not corrode or degrade – Small in size but have large surface area – Common materials • Platinum and alloys (titanium-coated platinum iridium) • Vitreous carbon (pyrolytic carbon) • Stainless steel alloys such as Elgiloy
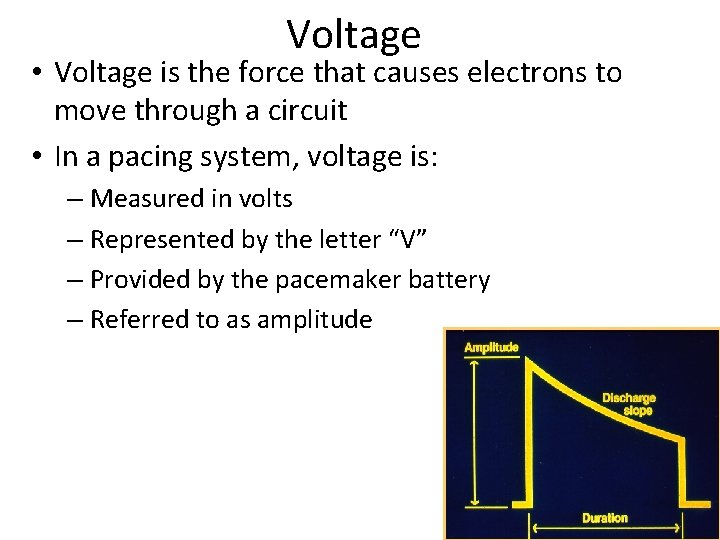
Voltage • Voltage is the force that causes electrons to move through a circuit • In a pacing system, voltage is: – Measured in volts – Represented by the letter “V” – Provided by the pacemaker battery – Referred to as amplitude
Current • The flow of electrons in a completed circuit • In a pacing system, current is: – Measured in m. A (milliamps) – Represented by the letter “I” – Determined by the amount of electrons that move through a circuit
• Constant-Voltage and Constant-Current Pacing • Most permanent pacemakers are constantvoltage pacemakers • Voltage and Current Threshold • Voltage threshold is the most commonly used measurement of pacing threshold
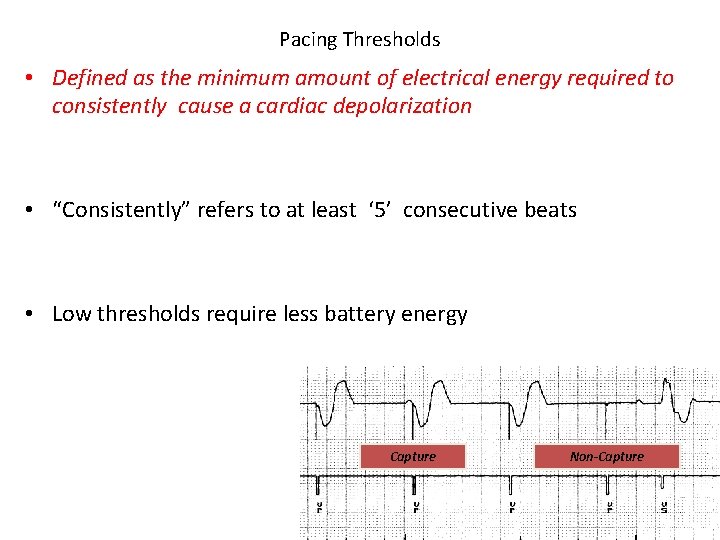
Pacing Thresholds • Defined as the minimum amount of electrical energy required to consistently cause a cardiac depolarization • “Consistently” refers to at least ‘ 5’ consecutive beats • Low thresholds require less battery energy Capture Non-Capture
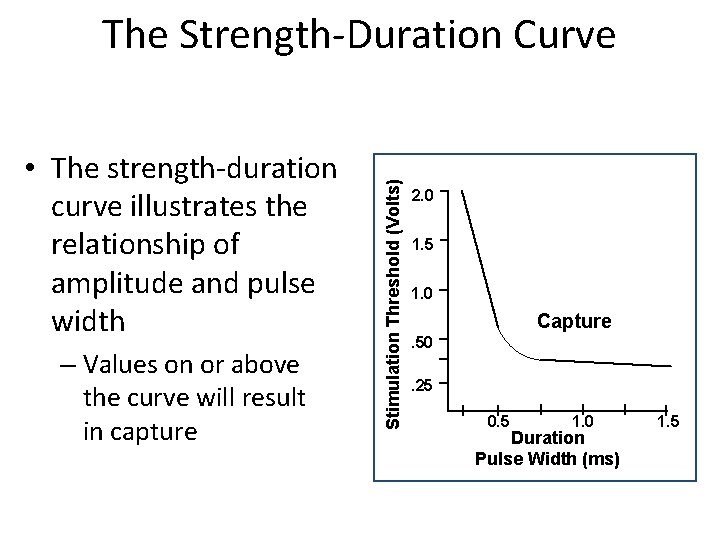
• The strength-duration curve illustrates the relationship of amplitude and pulse width – Values on or above the curve will result in capture Stimulation Threshold (Volts) The Strength-Duration Curve 2. 0 1. 5 1. 0 Capture. 50. 25 0. 5 1. 0 Duration Pulse Width (ms) 1. 5
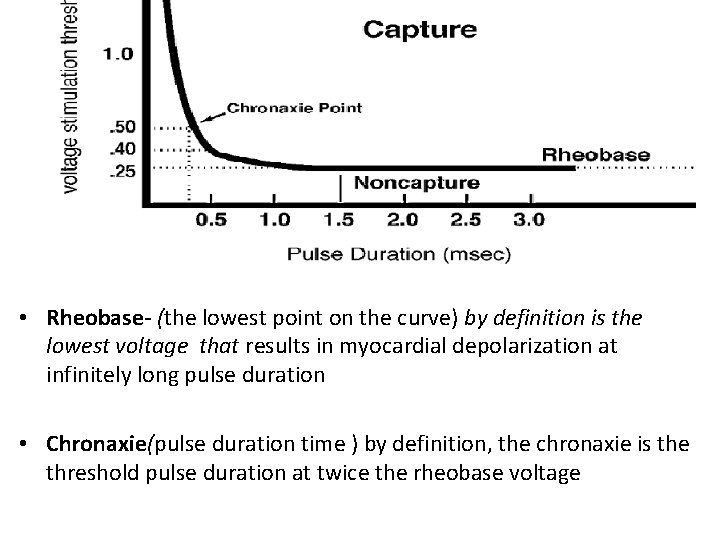
• Rheobase- (the lowest point on the curve) by definition is the lowest voltage that results in myocardial depolarization at infinitely long pulse duration • Chronaxie(pulse duration time ) by definition, the chronaxie is the threshold pulse duration at twice the rheobase voltage
Lessons from SDC • The ideal pulse duration should be greater than the chronaxie time • Cannot overcome high threshold exit block by increasing the pulse duration, If the voltage output remains less than the rheobase • Energy (μJ) = Voltage (V) × Current (m. A) × Pulse Duration (PD in ms). • Charge (μC) = Current (m. A) × Pulse Duration (ms).
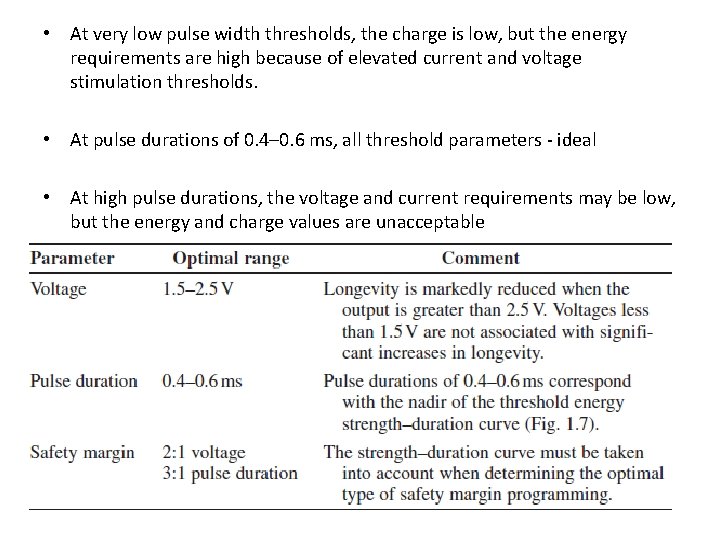
• At very low pulse width thresholds, the charge is low, but the energy requirements are high because of elevated current and voltage stimulation thresholds. • At pulse durations of 0. 4– 0. 6 ms, all threshold parameters - ideal • At high pulse durations, the voltage and current requirements may be low, but the energy and charge values are unacceptable

-Safety margins -When a threshold is determined by decrementing the pulse width at a fixed voltage • At a given voltage where the pulse width value is <. 30 ms: Tripling the pulse width will provide a two-time voltage safety margin. – Daily fluctuations in threshold that can occur due to eating, sleeping, exercise, or other factors - a/c pacing system - higher safety margin, due to the lead maturation process- occur within the first 6 -8 weeks following implant.
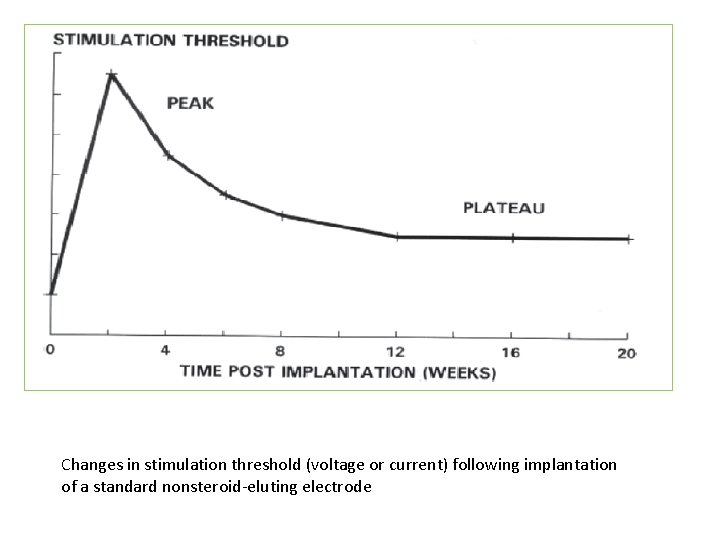
Changes in stimulation threshold (voltage or current) following implantation of a standard nonsteroid-eluting electrode
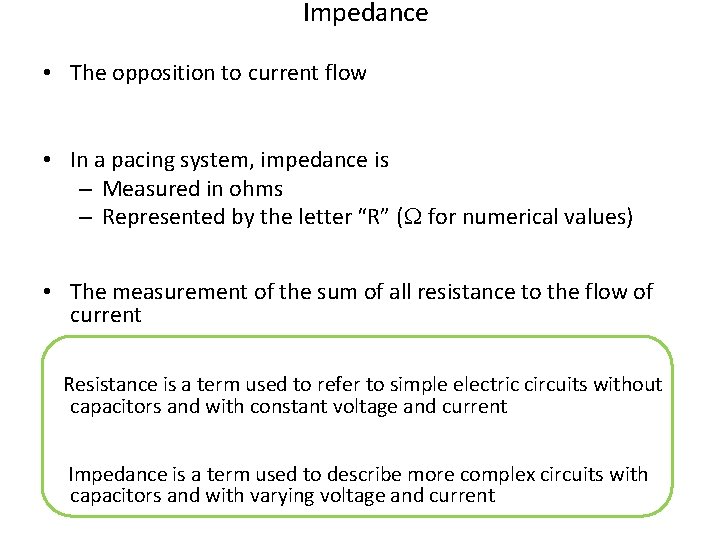
Impedance • The opposition to current flow • In a pacing system, impedance is – Measured in ohms – Represented by the letter “R” (W for numerical values) • The measurement of the sum of all resistance to the flow of current Resistance is a term used to refer to simple electric circuits without capacitors and with constant voltage and current Impedance is a term used to describe more complex circuits with capacitors and with varying voltage and current
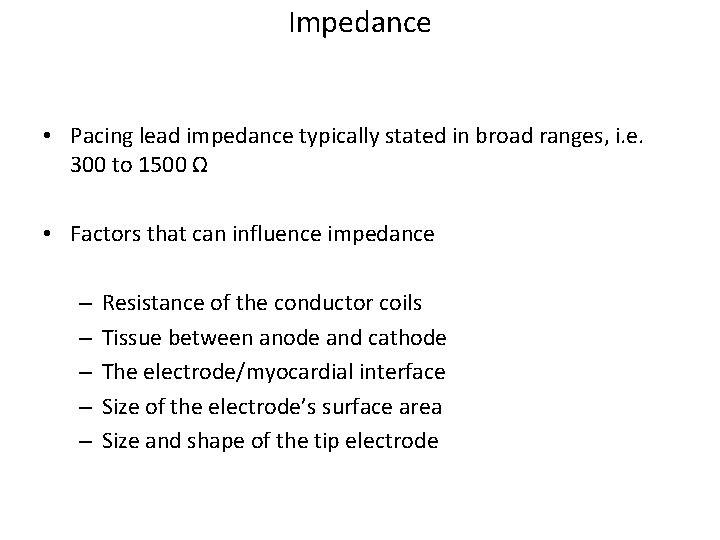
Impedance • Pacing lead impedance typically stated in broad ranges, i. e. 300 to 1500 Ω • Factors that can influence impedance – – – Resistance of the conductor coils Tissue between anode and cathode The electrode/myocardial interface Size of the electrode’s surface area Size and shape of the tip electrode
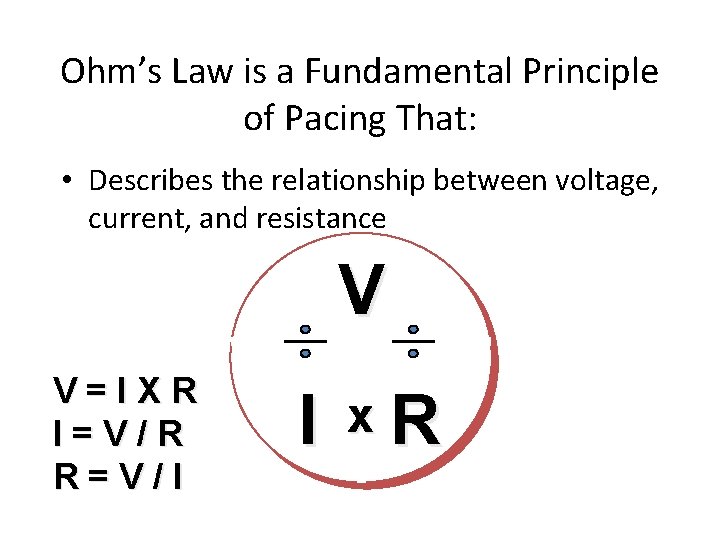
Ohm’s Law is a Fundamental Principle of Pacing That: • Describes the relationship between voltage, current, and resistance V V=IXR I=V/R R=V/I I x. R
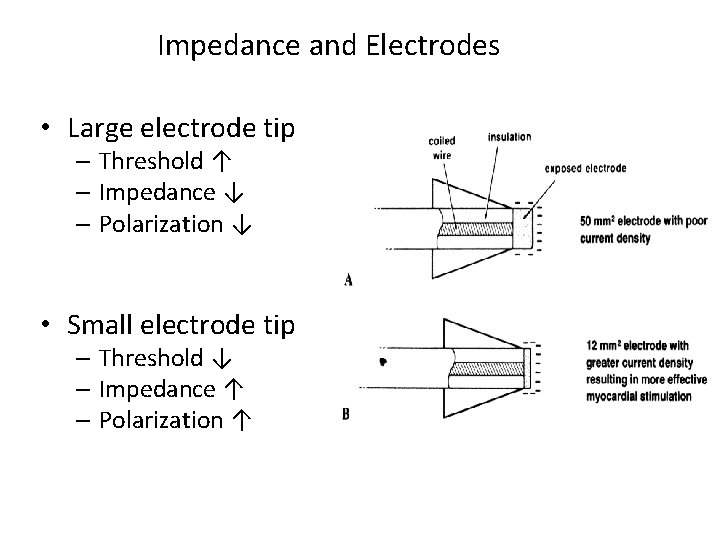
Impedance and Electrodes • Large electrode tip – Threshold ↑ – Impedance ↓ – Polarization ↓ • Small electrode tip – Threshold ↓ – Impedance ↑ – Polarization ↑
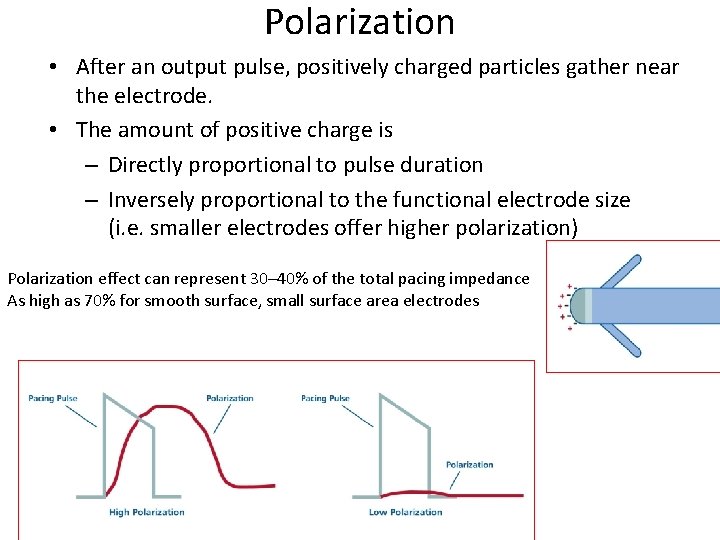
Polarization • After an output pulse, positively charged particles gather near the electrode. • The amount of positive charge is – Directly proportional to pulse duration – Inversely proportional to the functional electrode size (i. e. smaller electrodes offer higher polarization) Polarization effect can represent 30– 40% of the total pacing impedance As high as 70% for smooth surface, small surface area electrodes
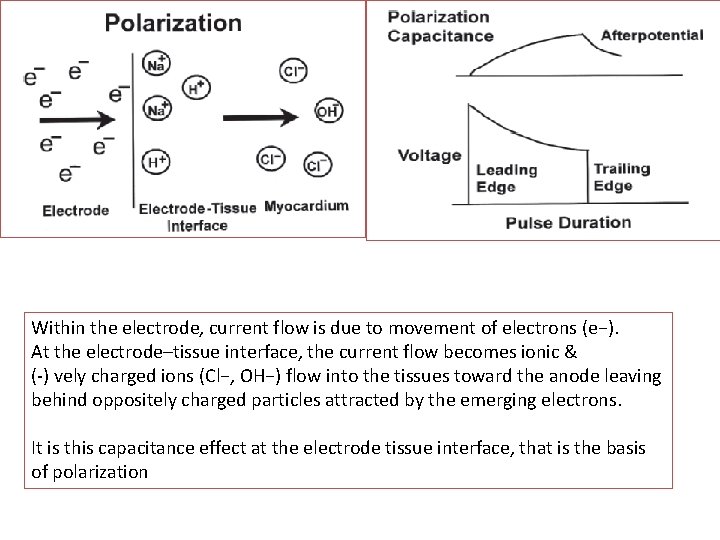
Within the electrode, current flow is due to movement of electrons (e−). At the electrode–tissue interface, the current flow becomes ionic & (-) vely charged ions (Cl−, OH−) flow into the tissues toward the anode leaving behind oppositely charged particles attracted by the emerging electrons. It is this capacitance effect at the electrode tissue interface, that is the basis of polarization
Lead Maturation Process • Fibrotic “capsule” develops around the electrode following lead implantation • 3 phases 1. A/c phase, where thresholds immediately following implant are low 2. Peaking phase- thresholds rise and reach their highest point(1 wk) , followed by a ↓ in the threshold over the next 6 to 8 wks as the tissue reaction subsides 3. C/c phase- thresholds at a level higher than that at implantation but less than the peak threshold • Trauma to cells surrounding the electrode→ edema and subsequent development of a fibrotic capsule. • Inexcitable capsule ↓ the current at the electrode interface, requiring more energy to capture the heart.
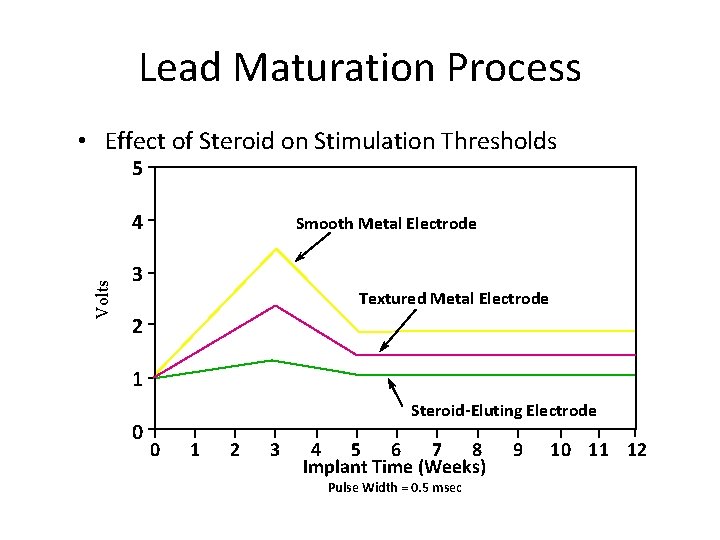
Lead Maturation Process • Effect of Steroid on Stimulation Thresholds 5 Volts 4 Smooth Metal Electrode 3 Textured Metal Electrode 2 1 0 Steroid-Eluting Electrode 0 1 2 3 4 5 6 7 8 Implant Time (Weeks) Pulse Width = 0. 5 msec 9 10 11 12
Sensing • Sensing is the ability of the pacemaker to detect an intrinsic depolarization – Pacemakers sense cardiac depolarization by measuring changes in electrical potential of myocardial cells between the anode and cathode
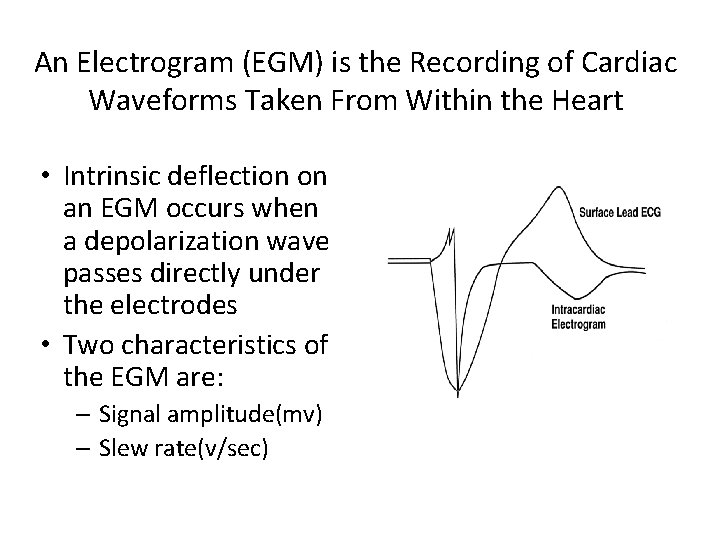
An Electrogram (EGM) is the Recording of Cardiac Waveforms Taken From Within the Heart • Intrinsic deflection on an EGM occurs when a depolarization wave passes directly under the electrodes • Two characteristics of the EGM are: – Signal amplitude(mv) – Slew rate(v/sec)
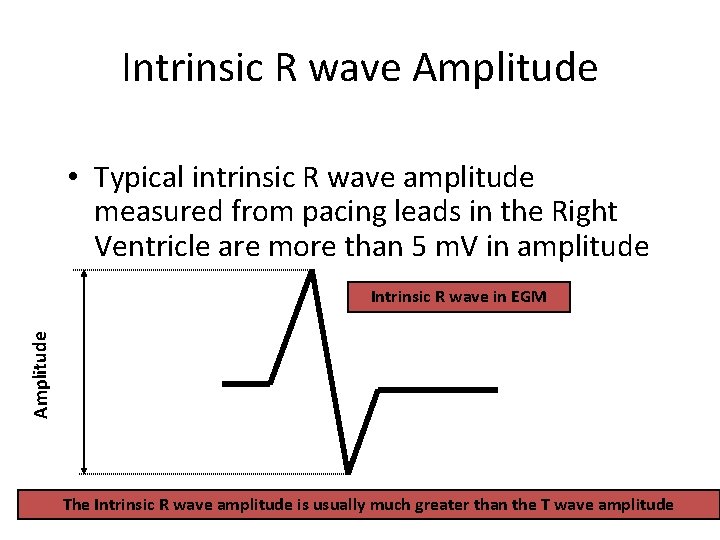
Intrinsic R wave Amplitude • Typical intrinsic R wave amplitude measured from pacing leads in the Right Ventricle are more than 5 m. V in amplitude Amplitude Intrinsic R wave in EGM The Intrinsic R wave amplitude is usually much greater than the T wave amplitude
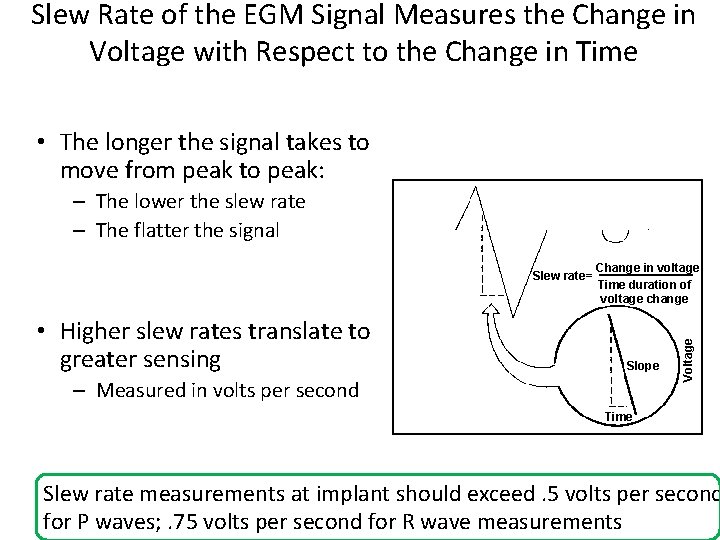
Slew Rate of the EGM Signal Measures the Change in Voltage with Respect to the Change in Time • The longer the signal takes to move from peak to peak: – The lower the slew rate – The flatter the signal • Higher slew rates translate to greater sensing Change in voltage Time duration of voltage change Slope – Measured in volts per second Voltage Slew rate= Time Slew rate measurements at implant should exceed. 5 volts per second for P waves; . 75 volts per second for R wave measurements
Factors That May Affect Sensing Are: • Lead polarity (unipolar vs. bipolar) • Lead integrity – Insulation break – Wire fracture • EMI – Electromagnetic Interference
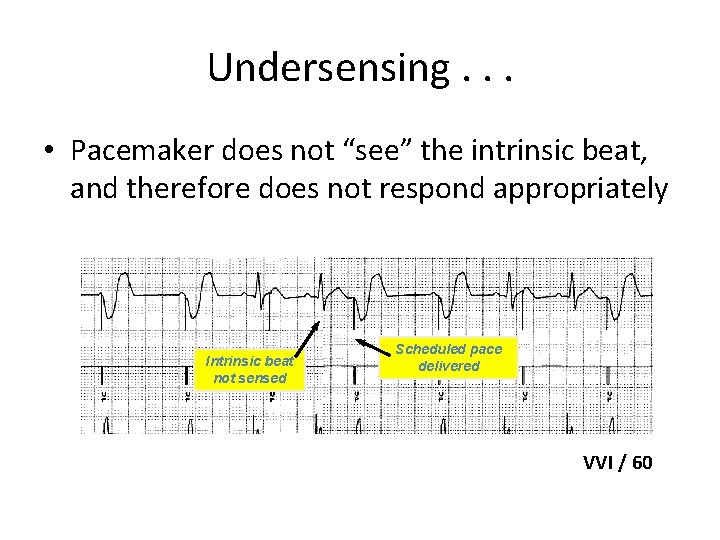
Undersensing. . . • Pacemaker does not “see” the intrinsic beat, and therefore does not respond appropriately Intrinsic beat not sensed Scheduled pace delivered VVI / 60
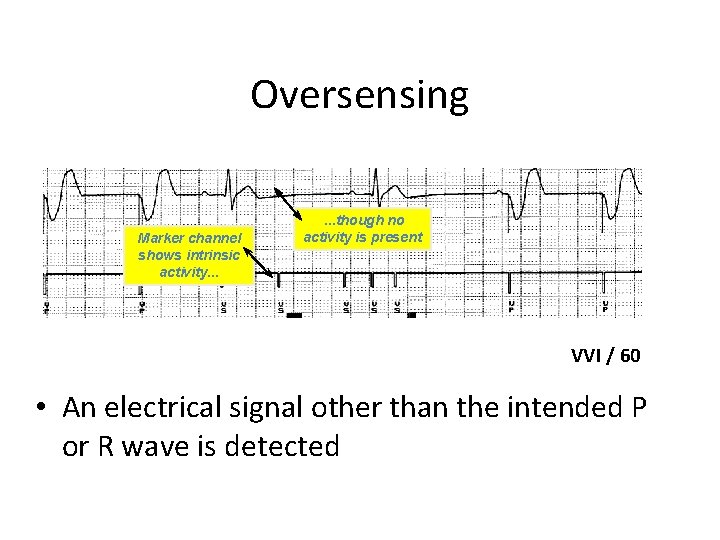
Oversensing Marker channel shows intrinsic activity. . . though no activity is present VVI / 60 • An electrical signal other than the intended P or R wave is detected
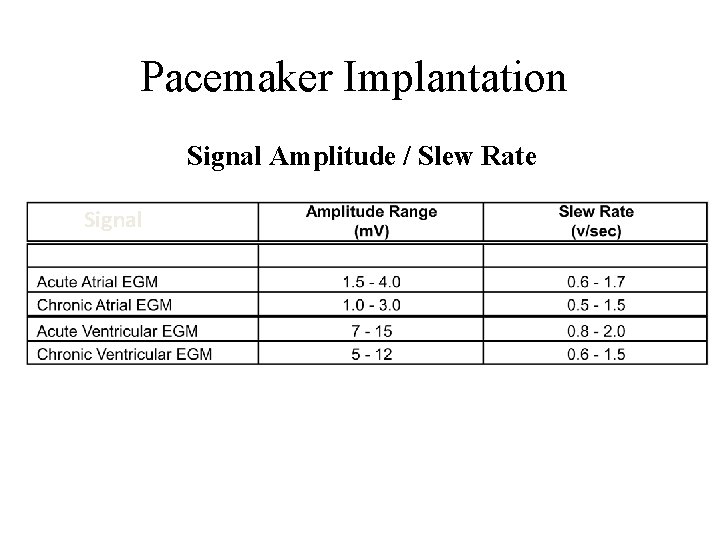
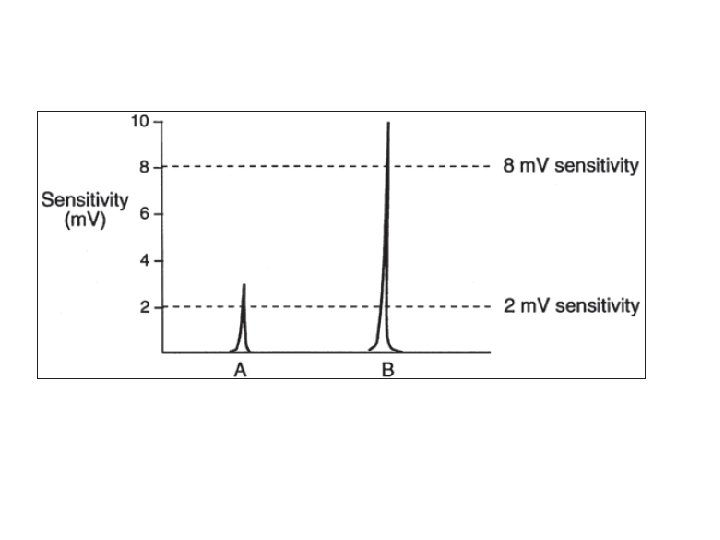
Pacemaker Implantation Signal Amplitude / Slew Rate Signal
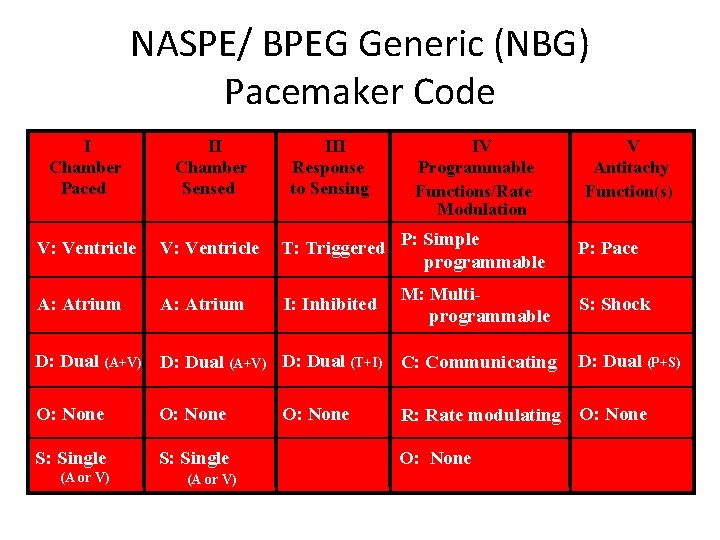
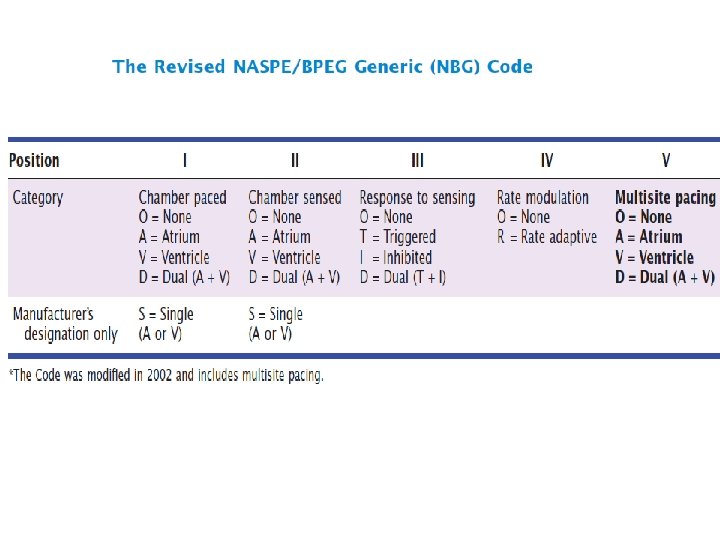
NASPE/ BPEG Generic (NBG) Pacemaker Code I Chamber Paced II Chamber Sensed III Response to Sensing IV Programmable Functions/Rate Modulation V: Ventricle T: Triggered P: Simple programmable A: Atrium I: Inhibited M: Multiprogrammable D: Dual (A+V) D: Dual (T+I) C: Communicating O: None S: Single (A or V) O: None V Antitachy Function(s) P: Pace S: Shock D: Dual (P+S) R: Rate modulating O: None
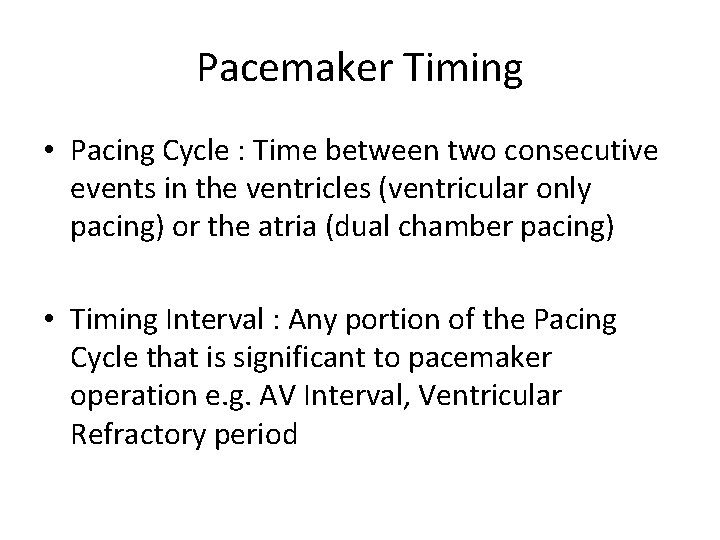
Pacemaker Timing • Pacing Cycle : Time between two consecutive events in the ventricles (ventricular only pacing) or the atria (dual chamber pacing) • Timing Interval : Any portion of the Pacing Cycle that is significant to pacemaker operation e. g. AV Interval, Ventricular Refractory period
Single-Chamber Timing
Single Chamber Timing Terminology • • Lower rate Refractory period Blanking period Upper rate
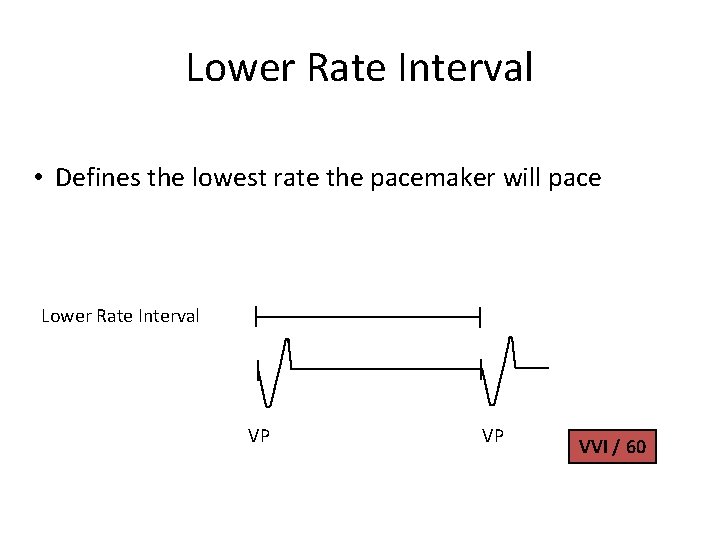
Lower Rate Interval • Defines the lowest rate the pacemaker will pace Lower Rate Interval VP VP VVI / 60
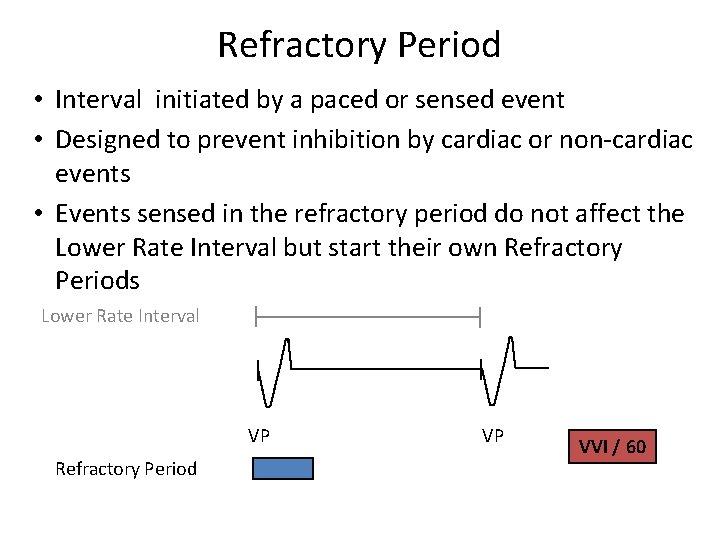
Refractory Period • Interval initiated by a paced or sensed event • Designed to prevent inhibition by cardiac or non-cardiac events • Events sensed in the refractory period do not affect the Lower Rate Interval but start their own Refractory Periods Lower Rate Interval VP Refractory Period VP VVI / 60
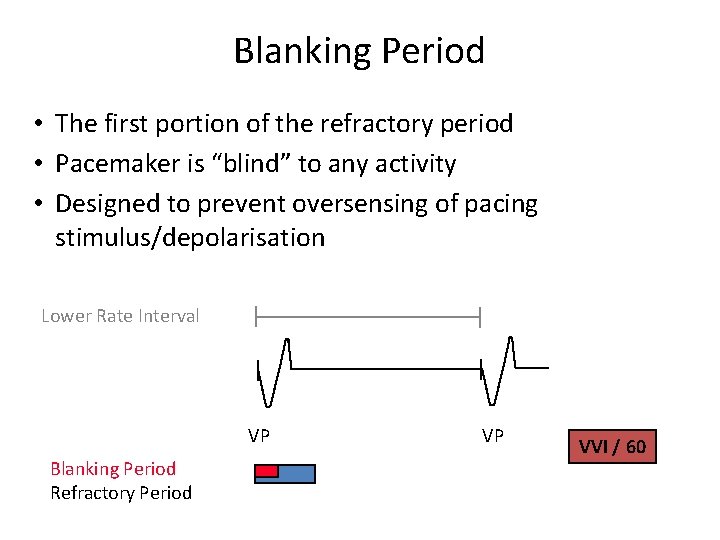
Blanking Period • The first portion of the refractory period • Pacemaker is “blind” to any activity • Designed to prevent oversensing of pacing stimulus/depolarisation Lower Rate Interval VP Blanking Period Refractory Period VP VVI / 60
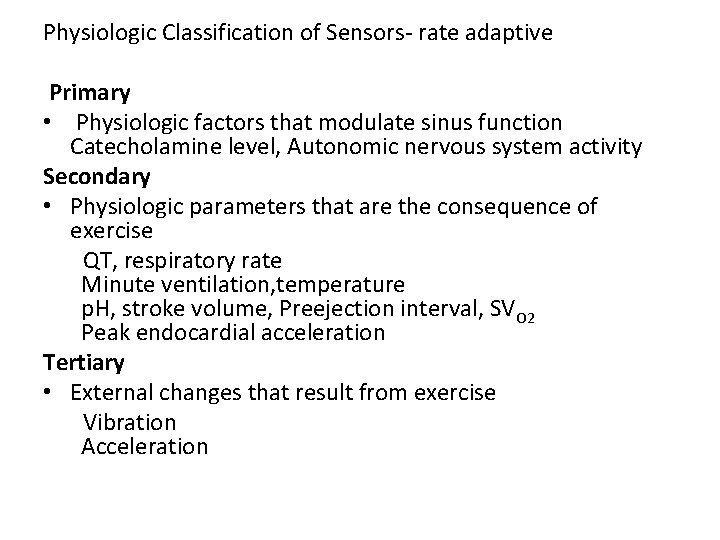
Physiologic Classification of Sensors- rate adaptive Primary • Physiologic factors that modulate sinus function Catecholamine level, Autonomic nervous system activity Secondary • Physiologic parameters that are the consequence of exercise QT, respiratory rate Minute ventilation, temperature p. H, stroke volume, Preejection interval, SVO 2 Peak endocardial acceleration Tertiary • External changes that result from exercise Vibration Acceleration
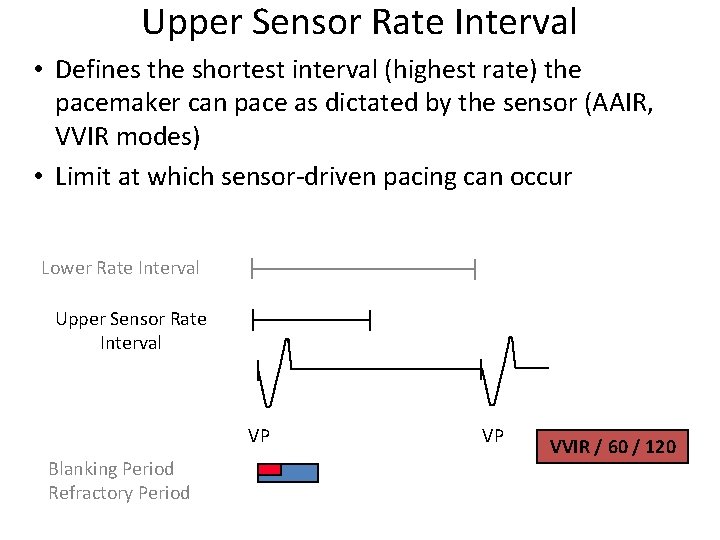
Upper Sensor Rate Interval • Defines the shortest interval (highest rate) the pacemaker can pace as dictated by the sensor (AAIR, VVIR modes) • Limit at which sensor-driven pacing can occur Lower Rate Interval Upper Sensor Rate Interval VP Blanking Period Refractory Period VP VVIR / 60 / 120
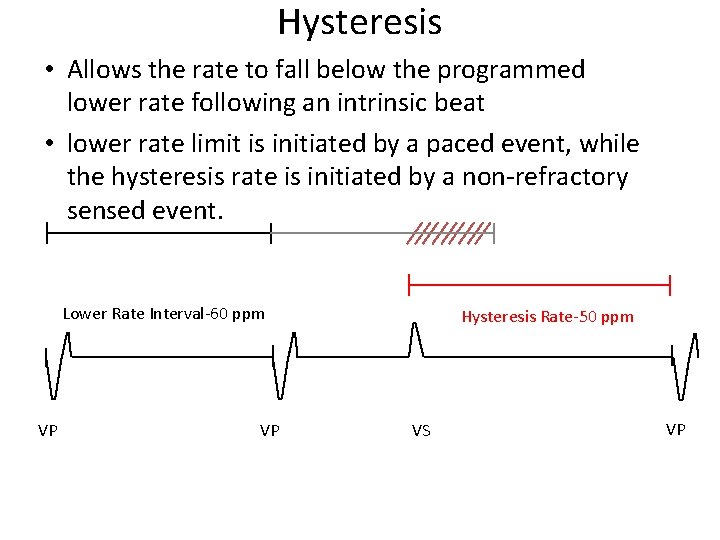
Hysteresis • Allows the rate to fall below the programmed lower rate following an intrinsic beat • lower rate limit is initiated by a paced event, while the hysteresis rate is initiated by a non-refractory sensed event. Lower Rate Interval-60 ppm VP VP Hysteresis Rate-50 ppm VS VP

Noise Reversion • Continuous refractory sensing will cause pacing at the lower rate Lower Rate Interval Noise Sensed VP VVI/60 SR SR VP
Modes-SINGLE CHAMBER
AOO & VOO-asynchronous modes • By application of magnet • Useful in diagnosing pacemaker dysfunction • During surgery to prevent interference from electrocautery
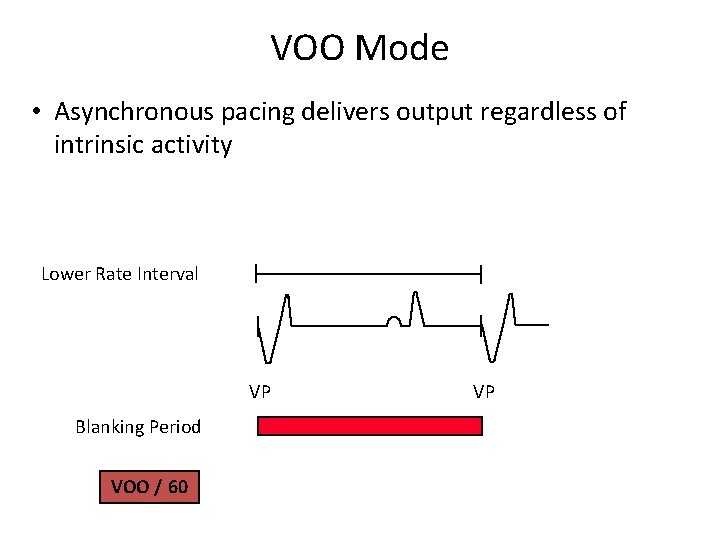
VOO Mode • Asynchronous pacing delivers output regardless of intrinsic activity Lower Rate Interval VP Blanking Period VOO / 60 VP
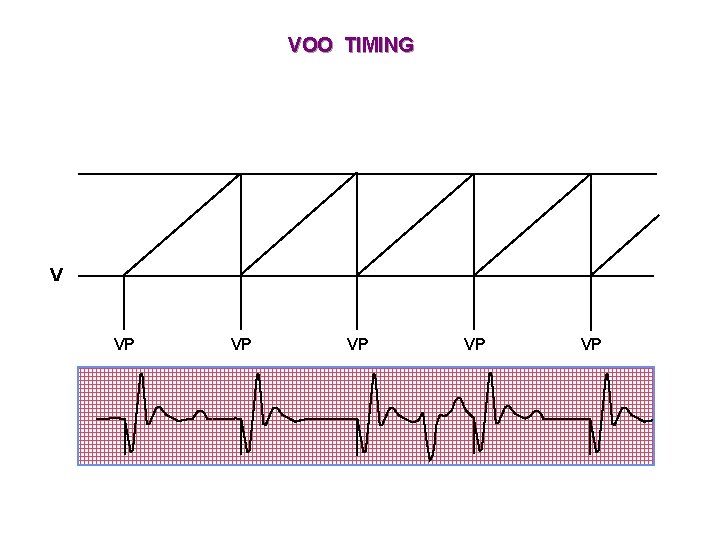
VOO TIMING V VP VP VP
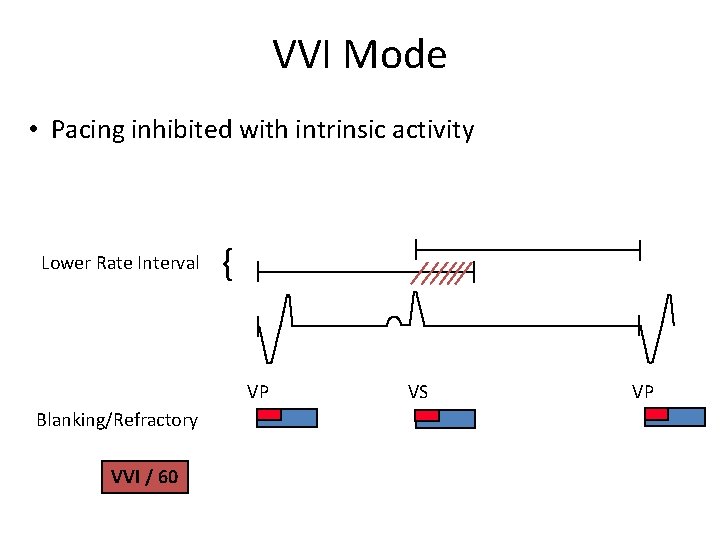
VVI Mode • Pacing inhibited with intrinsic activity Lower Rate Interval { VP Blanking/Refractory VVI / 60 VS VP
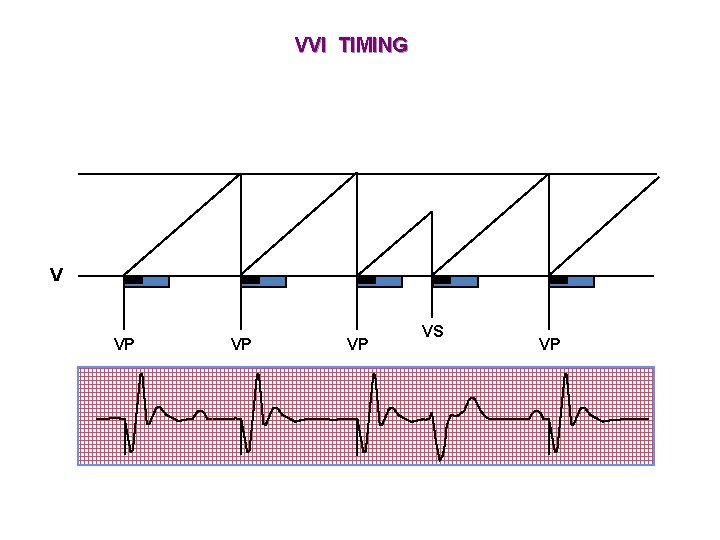
VVI TIMING V VP VP VP VS VP
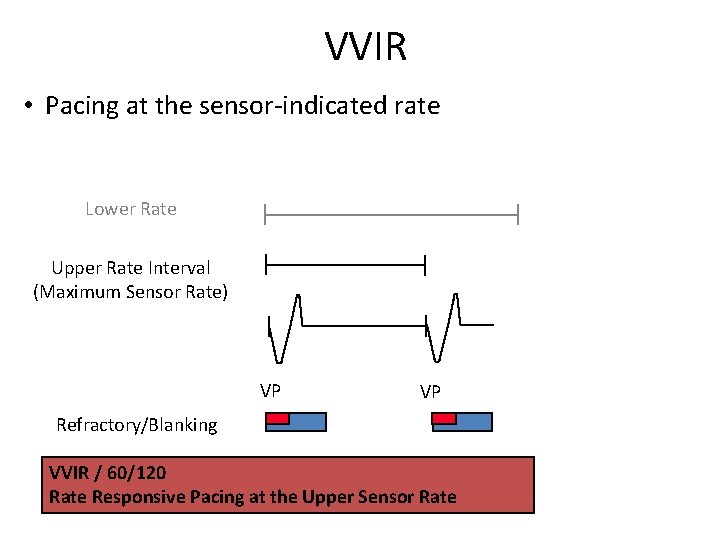
VVIR • Pacing at the sensor-indicated rate Lower Rate Upper Rate Interval (Maximum Sensor Rate) VP VP Refractory/Blanking VVIR / 60/120 Rate Responsive Pacing at the Upper Sensor Rate
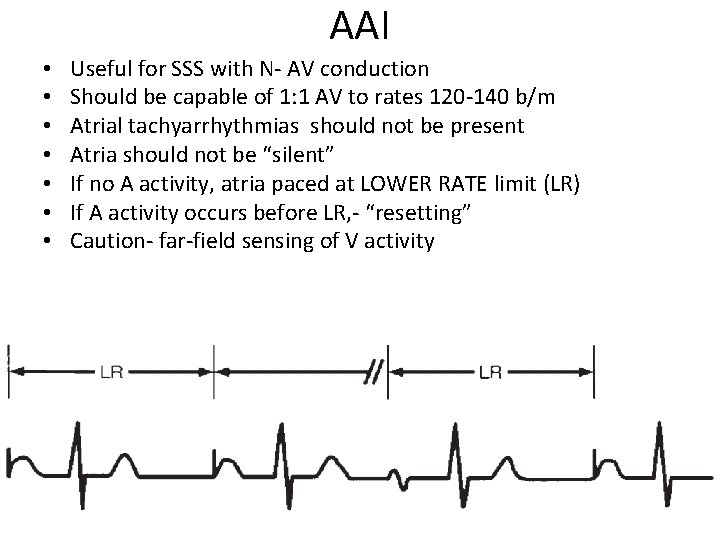
AAI • • Useful for SSS with N- AV conduction Should be capable of 1: 1 AV to rates 120 -140 b/m Atrial tachyarrhythmias should not be present Atria should not be “silent” If no A activity, atria paced at LOWER RATE limit (LR) If A activity occurs before LR, - “resetting” Caution- far-field sensing of V activity
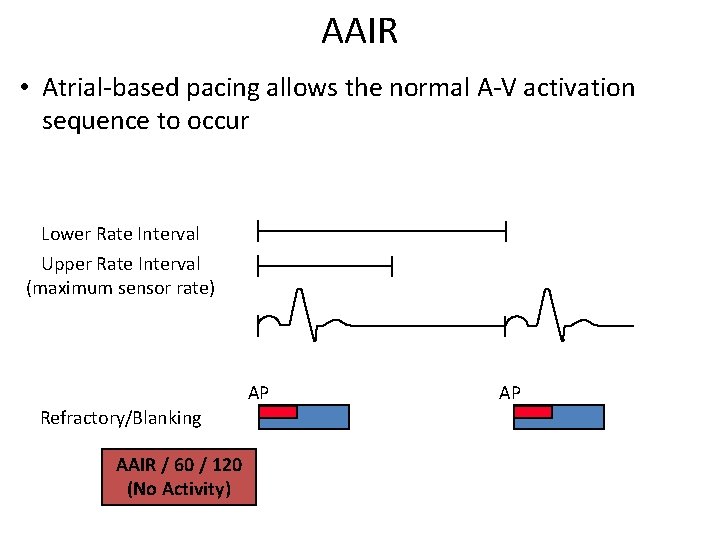
AAIR • Atrial-based pacing allows the normal A-V activation sequence to occur Lower Rate Interval Upper Rate Interval (maximum sensor rate) AP Refractory/Blanking AAIR / 60 / 120 (No Activity) AP
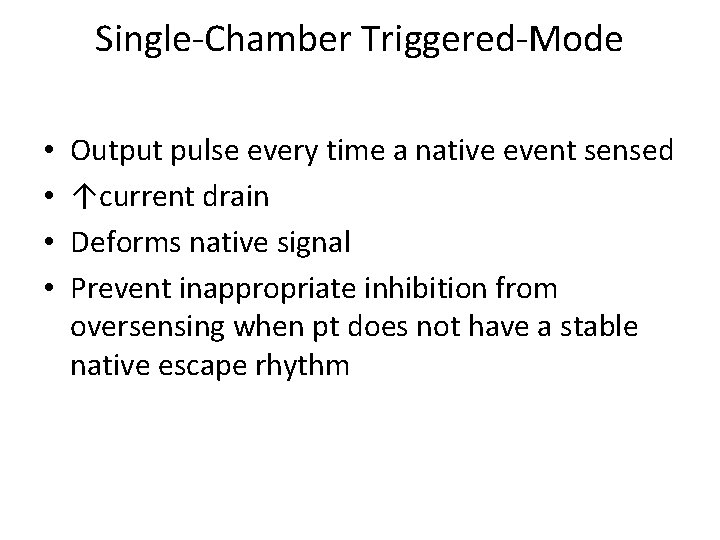
Single-Chamber Triggered-Mode • • Output pulse every time a native event sensed ↑current drain Deforms native signal Prevent inappropriate inhibition from oversensing when pt does not have a stable native escape rhythm
Benefits of Dual Chamber Pacing • Provides AV synchrony • Lower incidence of atrial fibrillation • Lower risk of systemic embolism and stroke • Lower incidence of new congestive heart failure • Lower mortality and higher survival rates
Dual Chamber Timing Parameters • • • Lower rate AV and VA intervals Upper rate intervals Refractory periods Blanking periods
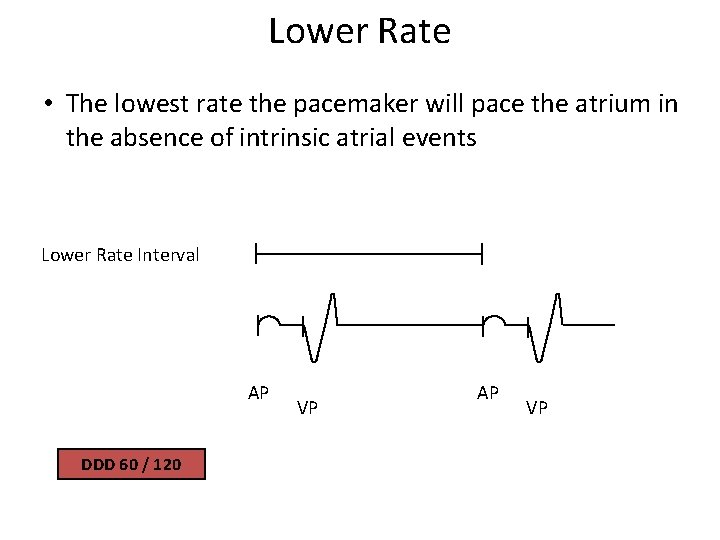
Lower Rate • The lowest rate the pacemaker will pace the atrium in the absence of intrinsic atrial events Lower Rate Interval AP DDD 60 / 120 VP AP VP
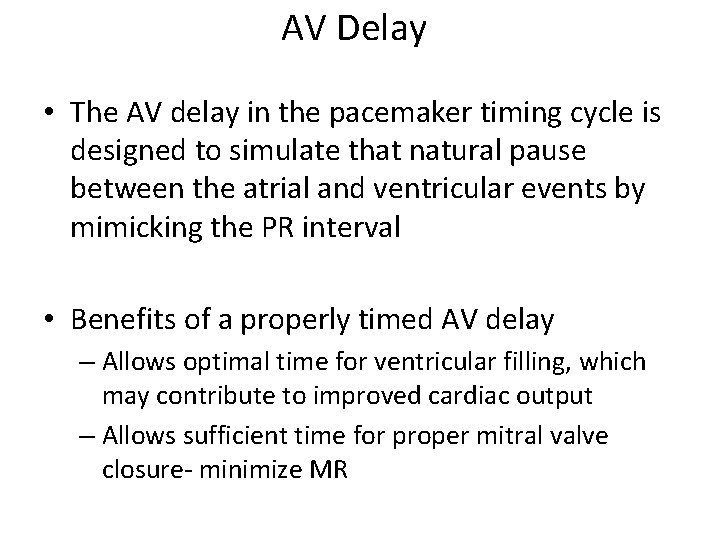
AV Delay • The AV delay in the pacemaker timing cycle is designed to simulate that natural pause between the atrial and ventricular events by mimicking the PR interval • Benefits of a properly timed AV delay – Allows optimal time for ventricular filling, which may contribute to improved cardiac output – Allows sufficient time for proper mitral valve closure- minimize MR
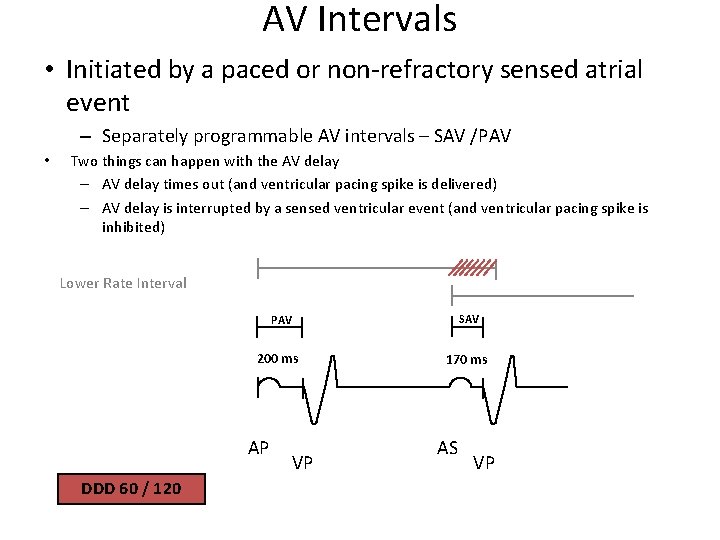
AV Intervals • Initiated by a paced or non-refractory sensed atrial event – Separately programmable AV intervals – SAV /PAV • Two things can happen with the AV delay – AV delay times out (and ventricular pacing spike is delivered) – AV delay is interrupted by a sensed ventricular event (and ventricular pacing spike is inhibited) Lower Rate Interval SAV PAV 200 ms AP DDD 60 / 120 VP 170 ms AS VP
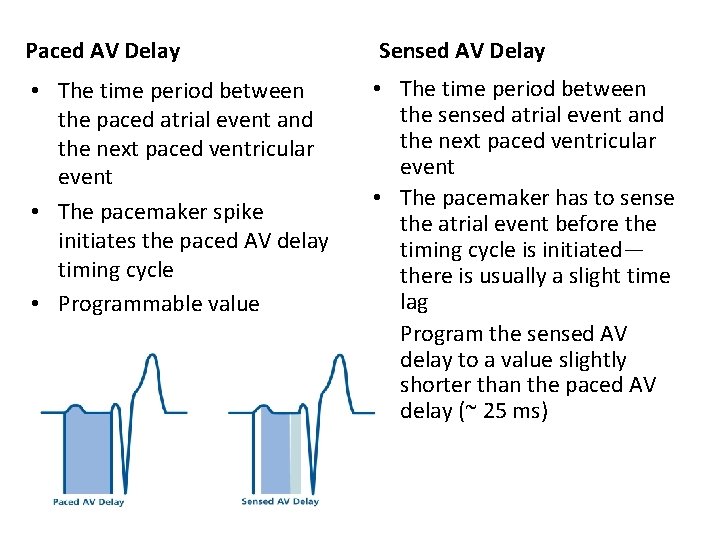
Paced AV Delay Sensed AV Delay • The time period between the paced atrial event and the next paced ventricular event • The pacemaker spike initiates the paced AV delay timing cycle • Programmable value • The time period between the sensed atrial event and the next paced ventricular event • The pacemaker has to sense the atrial event before the timing cycle is initiated— there is usually a slight time lag • Program the sensed AV delay to a value slightly shorter than the paced AV delay (~ 25 ms)
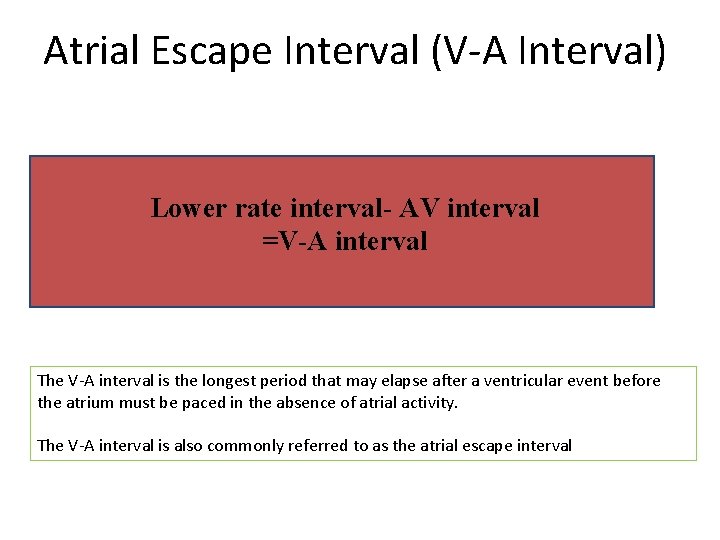
Atrial Escape Interval (V-A Interval) Lower rate interval- AV interval =V-A interval The V-A interval is the longest period that may elapse after a ventricular event before the atrium must be paced in the absence of atrial activity. The V-A interval is also commonly referred to as the atrial escape interval
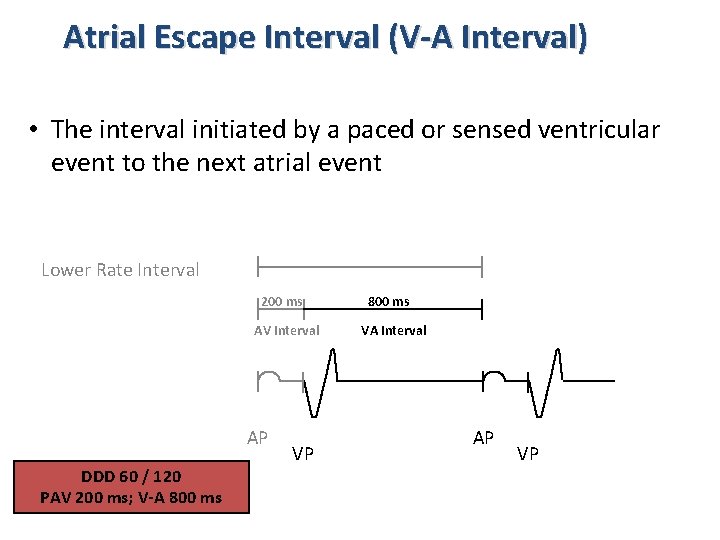
Atrial Escape Interval (V-A Interval) • The interval initiated by a paced or sensed ventricular event to the next atrial event Lower Rate Interval 200 ms AV Interval AP DDD 60 / 120 PAV 200 ms; V-A 800 ms VP 800 ms VA Interval AP VP
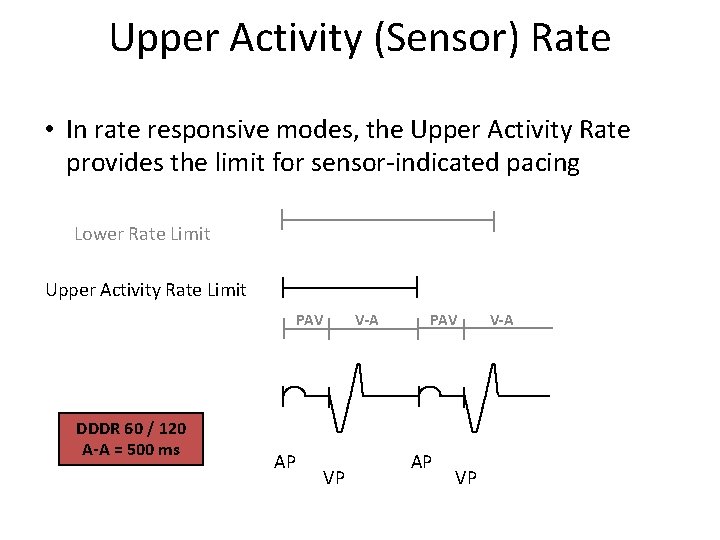
Upper Activity (Sensor) Rate • In rate responsive modes, the Upper Activity Rate provides the limit for sensor-indicated pacing Lower Rate Limit Upper Activity Rate Limit PAV DDDR 60 / 120 A-A = 500 ms AP V-A VP PAV AP VP V-A
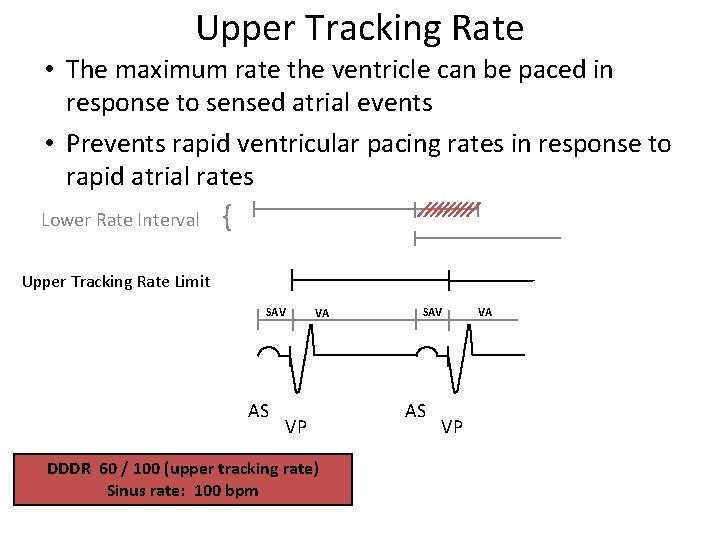
Upper Tracking Rate • The maximum rate the ventricle can be paced in response to sensed atrial events • Prevents rapid ventricular pacing rates in response to rapid atrial rates Lower Rate Interval { Upper Tracking Rate Limit SAV AS VA VP DDDR 60 / 100 (upper tracking rate) Sinus rate: 100 bpm SAV AS VP VA
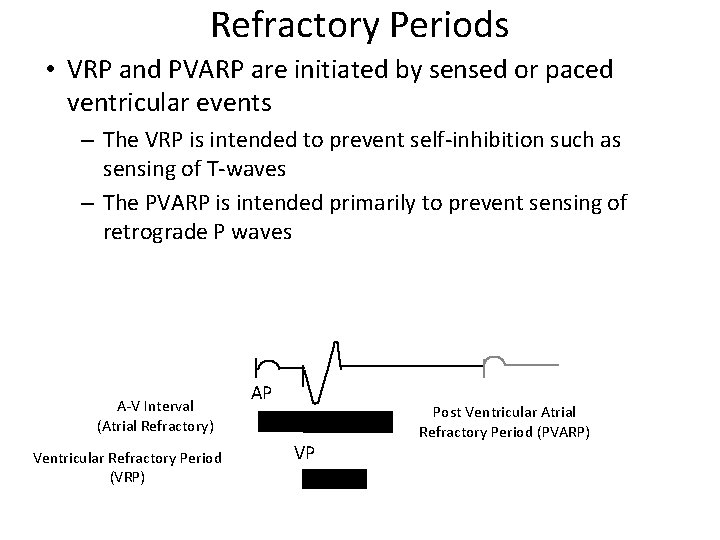
Refractory Periods • VRP and PVARP are initiated by sensed or paced ventricular events – The VRP is intended to prevent self-inhibition such as sensing of T-waves – The PVARP is intended primarily to prevent sensing of retrograde P waves A-V Interval (Atrial Refractory) Ventricular Refractory Period (VRP) AP VP Post Ventricular Atrial Refractory Period (PVARP)
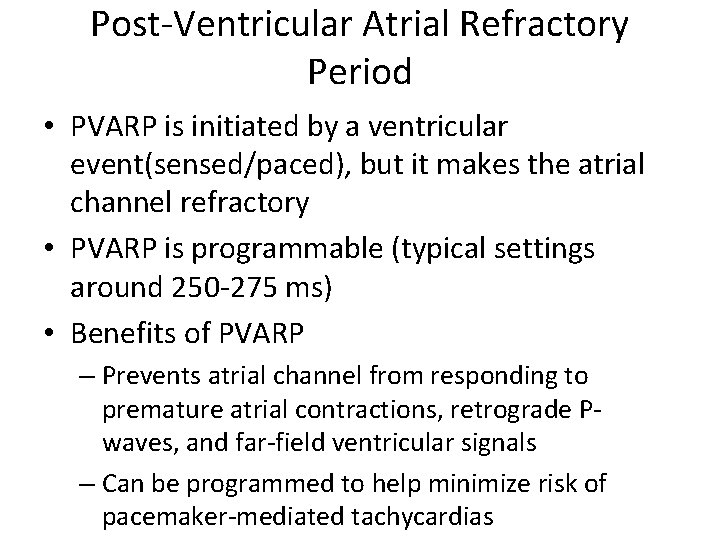
Post-Ventricular Atrial Refractory Period • PVARP is initiated by a ventricular event(sensed/paced), but it makes the atrial channel refractory • PVARP is programmable (typical settings around 250 -275 ms) • Benefits of PVARP – Prevents atrial channel from responding to premature atrial contractions, retrograde Pwaves, and far-field ventricular signals – Can be programmed to help minimize risk of pacemaker-mediated tachycardias
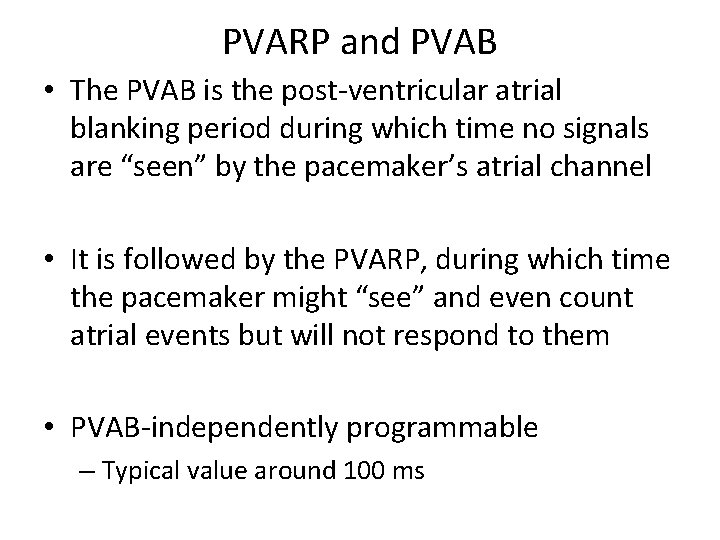
PVARP and PVAB • The PVAB is the post-ventricular atrial blanking period during which time no signals are “seen” by the pacemaker’s atrial channel • It is followed by the PVARP, during which time the pacemaker might “see” and even count atrial events but will not respond to them • PVAB-independently programmable – Typical value around 100 ms
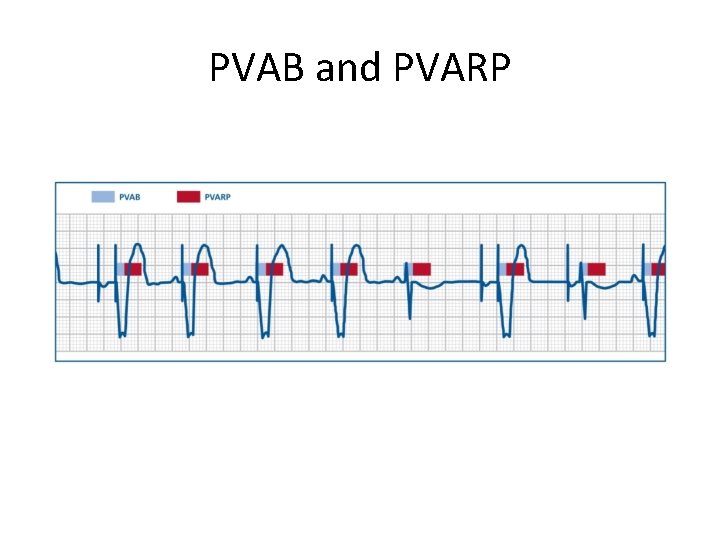
PVAB and PVARP
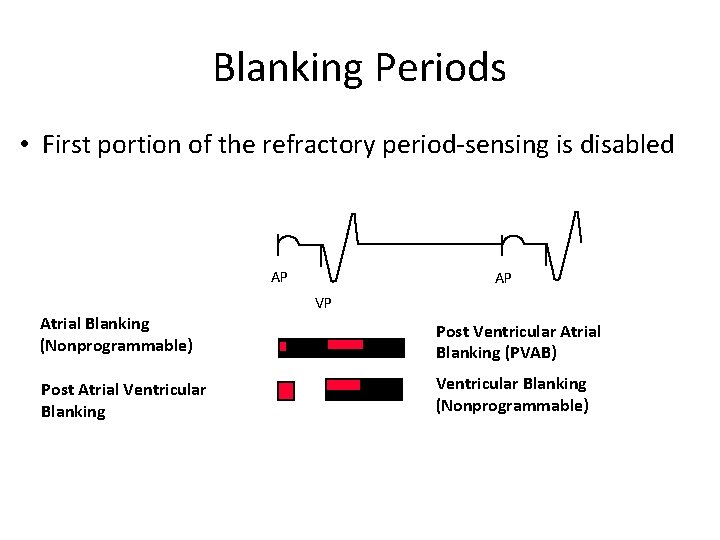
Blanking Periods • First portion of the refractory period-sensing is disabled AP Atrial Blanking (Nonprogrammable) Post Atrial Ventricular Blanking AP VP Post Ventricular Atrial Blanking (PVAB) Ventricular Blanking (Nonprogrammable)
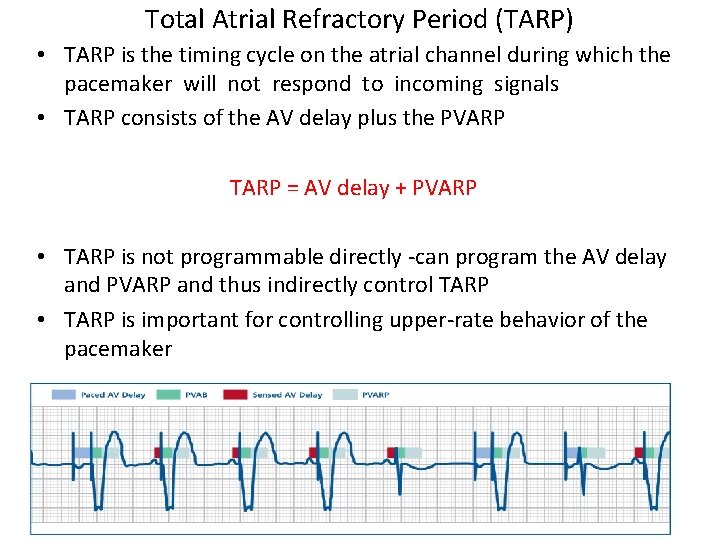
Total Atrial Refractory Period (TARP) • TARP is the timing cycle on the atrial channel during which the pacemaker will not respond to incoming signals • TARP consists of the AV delay plus the PVARP TARP = AV delay + PVARP • TARP is not programmable directly -can program the AV delay and PVARP and thus indirectly control TARP • TARP is important for controlling upper-rate behavior of the pacemaker
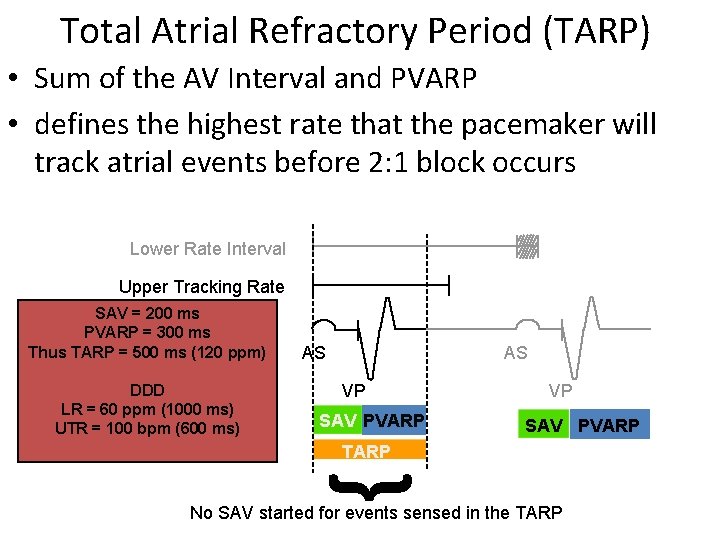
Total Atrial Refractory Period (TARP) • Sum of the AV Interval and PVARP • defines the highest rate that the pacemaker will track atrial events before 2: 1 block occurs Lower Rate Interval Upper Tracking Rate SAV = 200 ms PVARP = 300 ms Thus TARP = 500 ms (120 ppm) DDD LR = 60 ppm (1000 ms) UTR = 100 bpm (600 ms) AS AS VP SAV PVARP { TARP No SAV started for events sensed in the TARP
Wenckebach • Occurs when the intrinsic atrial rate lies between the UTR and the TARP rate • Results in gradual prolonging of the AV interval until one atrial intrinsic event occurs during the TARP and is not tracked
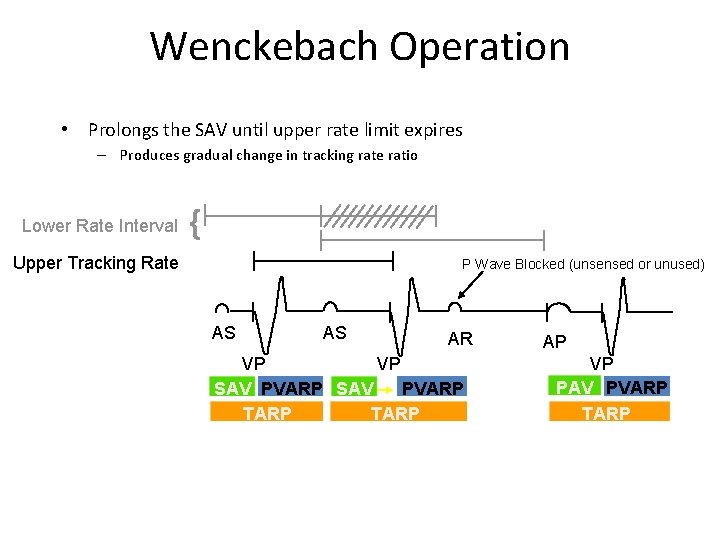
Wenckebach Operation • Prolongs the SAV until upper rate limit expires – Produces gradual change in tracking rate ratio Lower Rate Interval { Upper Tracking Rate P Wave Blocked (unsensed or unused) AS AS AR VP VP PVARP SAV TARP AP VP PAV PVARP TARP
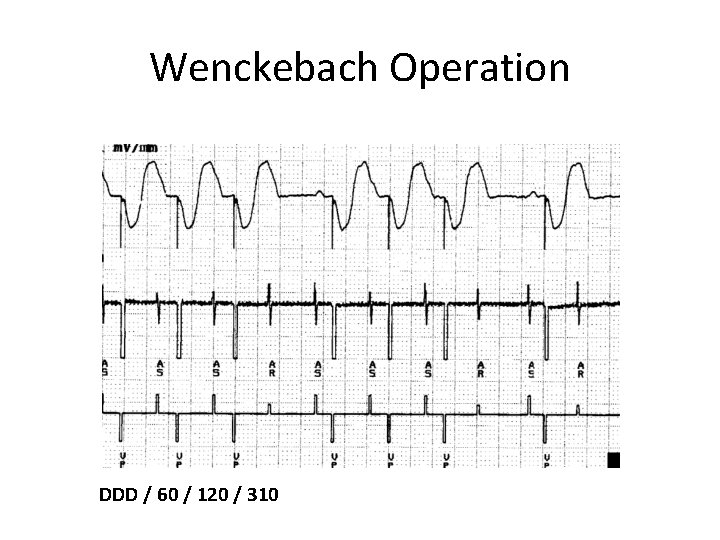
Wenckebach Operation DDD / 60 / 120 / 310
Fixed Block or 2: 1 Block • Occurs whenever the intrinsic atrial rate exceeds the TARP rate • Every other atrial event falls in the TARP when the atrial rate exceeds the TARP rate • Results in block of atrial intrinsic events in fixed ratios
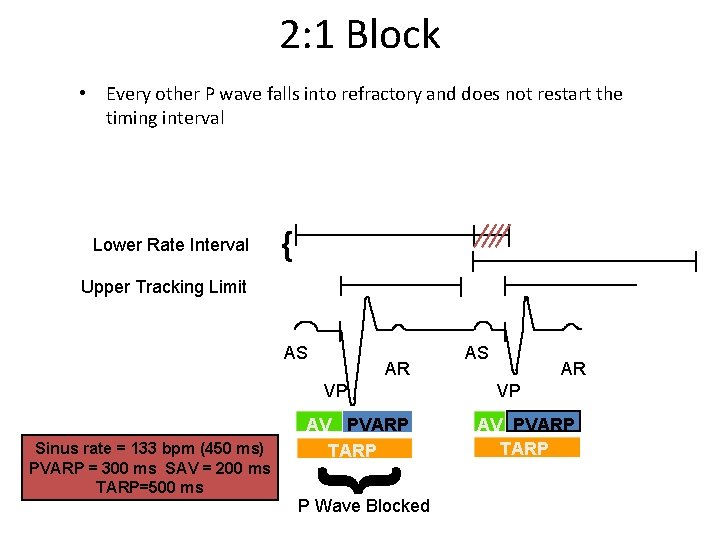
2: 1 Block • Every other P wave falls into refractory and does not restart the timing interval Lower Rate Interval { Upper Tracking Limit AS AR VP { Sinus rate = 133 bpm (450 ms) PVARP = 300 ms SAV = 200 ms TARP=500 ms AV PVARP TARP P Wave Blocked AS AR VP AV PVARP TARP
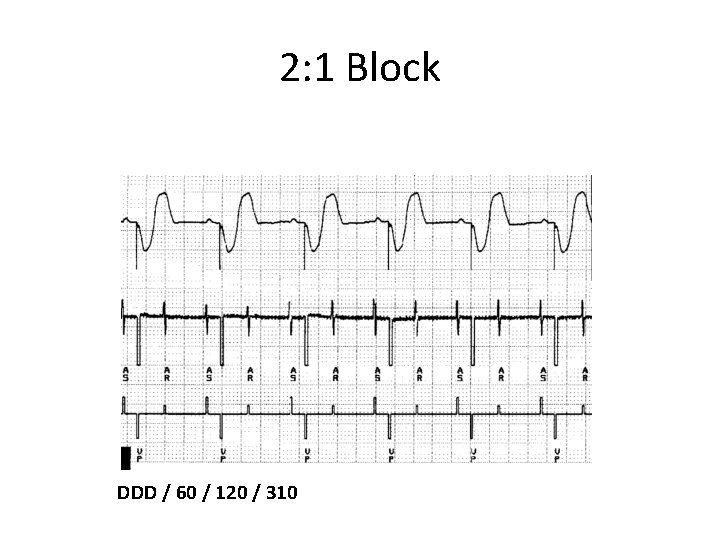
2: 1 Block DDD / 60 / 120 / 310
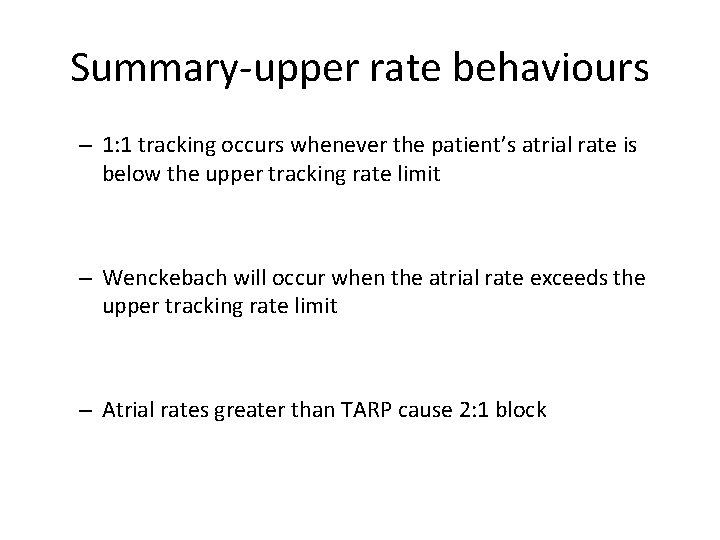
Summary-upper rate behaviours – 1: 1 tracking occurs whenever the patient’s atrial rate is below the upper tracking rate limit – Wenckebach will occur when the atrial rate exceeds the upper tracking rate limit – Atrial rates greater than TARP cause 2: 1 block
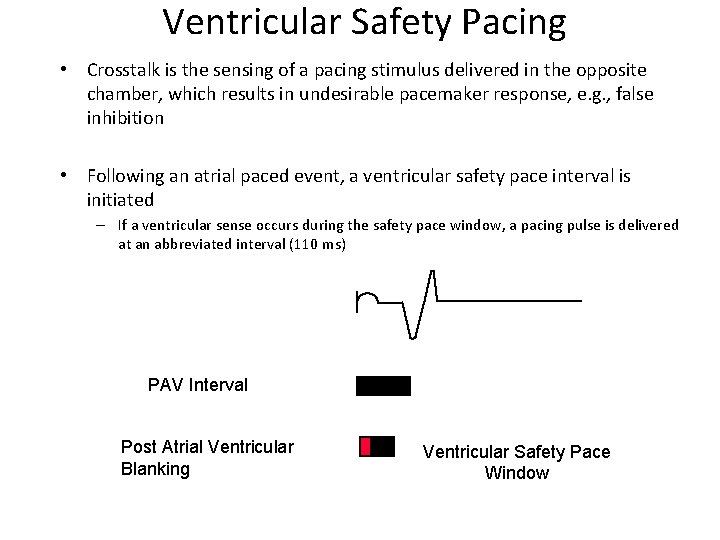
Ventricular Safety Pacing • Crosstalk is the sensing of a pacing stimulus delivered in the opposite chamber, which results in undesirable pacemaker response, e. g. , false inhibition • Following an atrial paced event, a ventricular safety pace interval is initiated – If a ventricular sense occurs during the safety pace window, a pacing pulse is delivered at an abbreviated interval (110 ms) PAV Interval Post Atrial Ventricular Blanking Ventricular Safety Pace Window
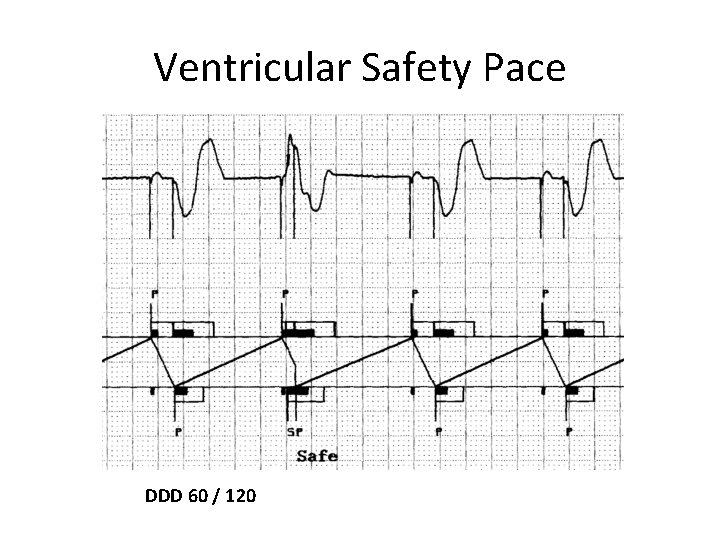
Ventricular Safety Pace DDD 60 / 120
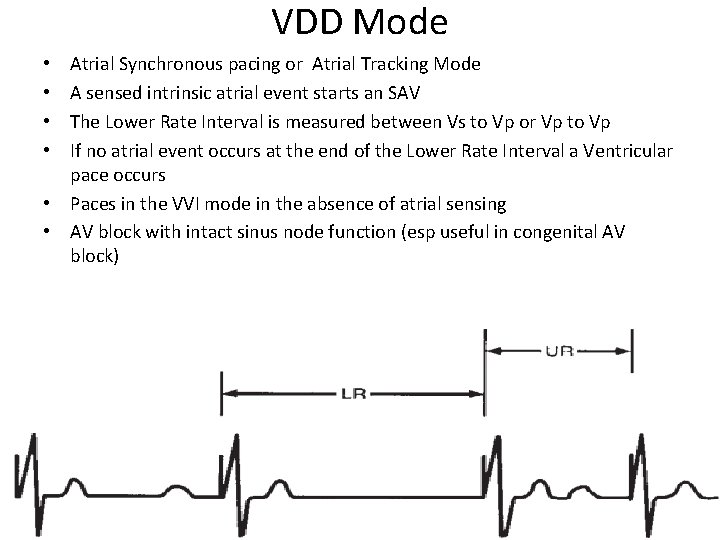
VDD Mode Atrial Synchronous pacing or Atrial Tracking Mode A sensed intrinsic atrial event starts an SAV The Lower Rate Interval is measured between Vs to Vp or Vp to Vp If no atrial event occurs at the end of the Lower Rate Interval a Ventricular pace occurs • Paces in the VVI mode in the absence of atrial sensing • AV block with intact sinus node function (esp useful in congenital AV block) • •
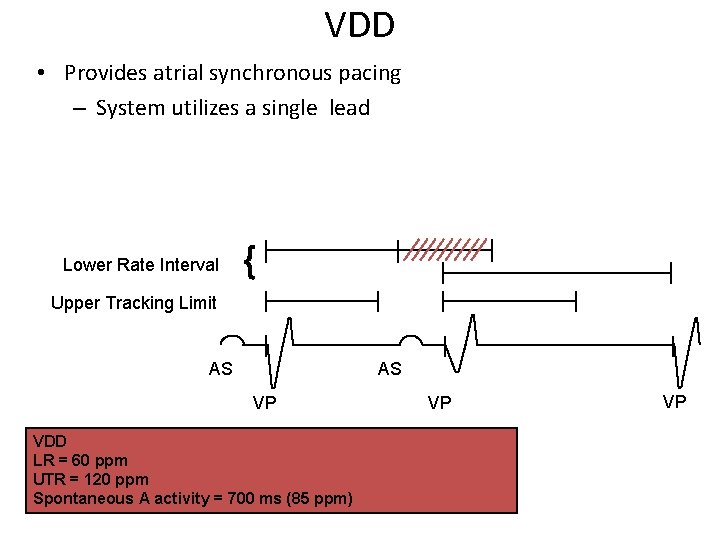
VDD • Provides atrial synchronous pacing – System utilizes a single lead Lower Rate Interval { Upper Tracking Limit AS AS VP VDD LR = 60 ppm UTR = 120 ppm Spontaneous A activity = 700 ms (85 ppm) VP VP
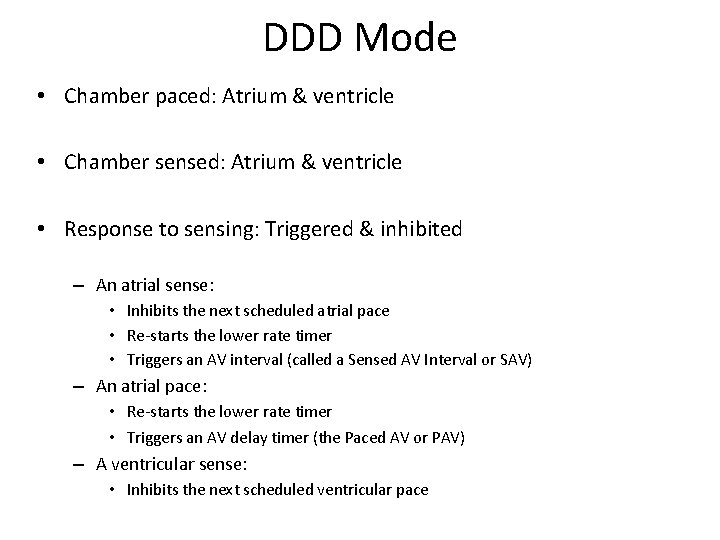
DDD Mode • Chamber paced: Atrium & ventricle • Chamber sensed: Atrium & ventricle • Response to sensing: Triggered & inhibited – An atrial sense: • Inhibits the next scheduled atrial pace • Re-starts the lower rate timer • Triggers an AV interval (called a Sensed AV Interval or SAV) – An atrial pace: • Re-starts the lower rate timer • Triggers an AV delay timer (the Paced AV or PAV) – A ventricular sense: • Inhibits the next scheduled ventricular pace
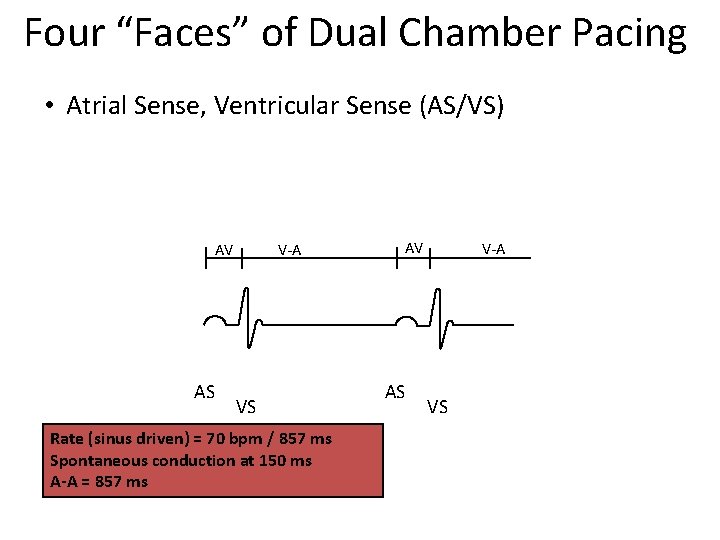
Four “Faces” of Dual Chamber Pacing • Atrial Sense, Ventricular Sense (AS/VS) AV AS V-A VS Rate (sinus driven) = 70 bpm / 857 ms Spontaneous conduction at 150 ms A-A = 857 ms AV AS V-A VS
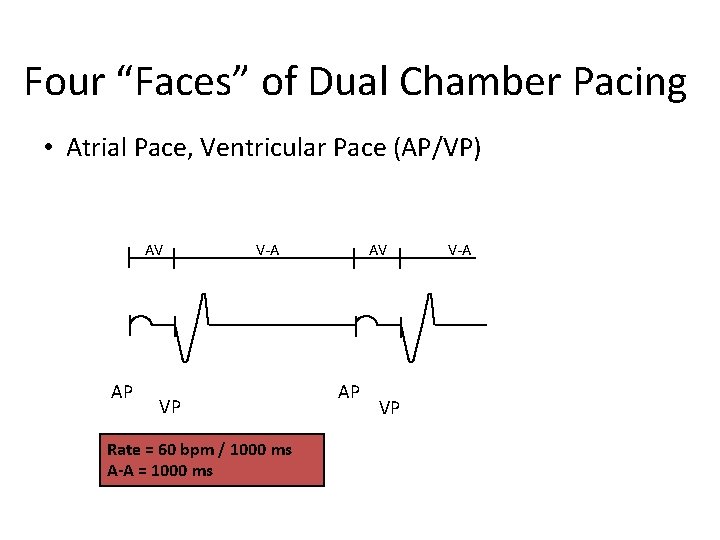
Four “Faces” of Dual Chamber Pacing • Atrial Pace, Ventricular Pace (AP/VP) AV AP V-A VP Rate = 60 bpm / 1000 ms A-A = 1000 ms AV AP VP V-A
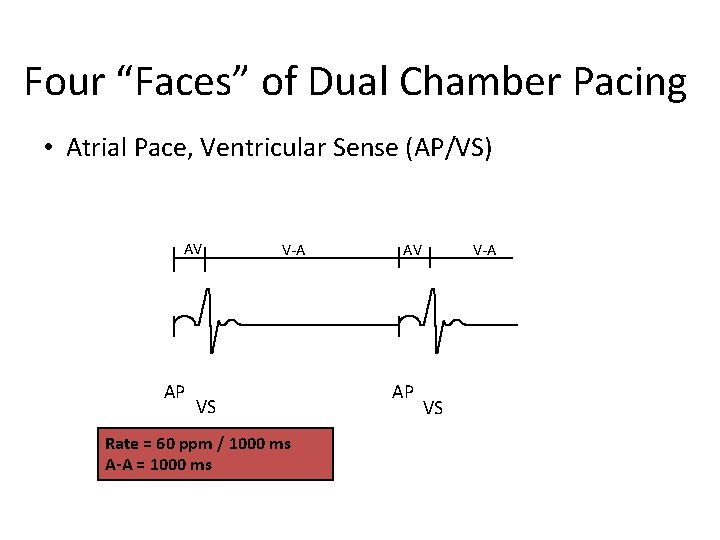
Four “Faces” of Dual Chamber Pacing • Atrial Pace, Ventricular Sense (AP/VS) AV AP V-A VS Rate = 60 ppm / 1000 ms A-A = 1000 ms AV AP V-A VS
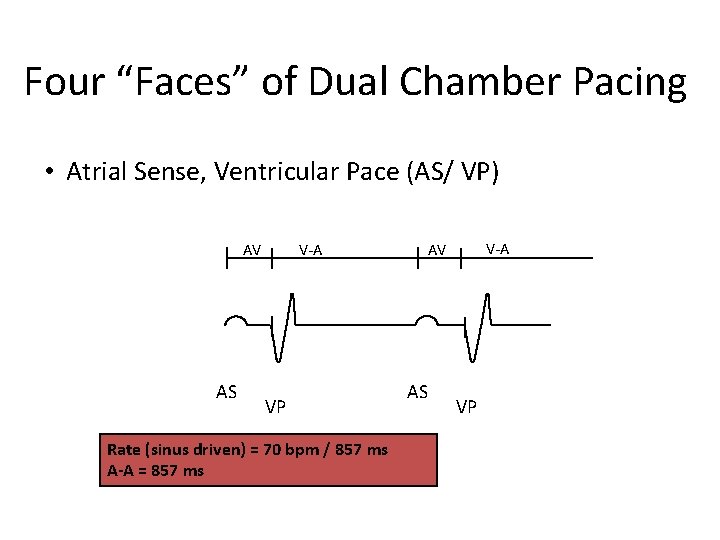
Four “Faces” of Dual Chamber Pacing • Atrial Sense, Ventricular Pace (AS/ VP) AV AS V-A VP Rate (sinus driven) = 70 bpm / 857 ms A-A = 857 ms V-A AV AS VP
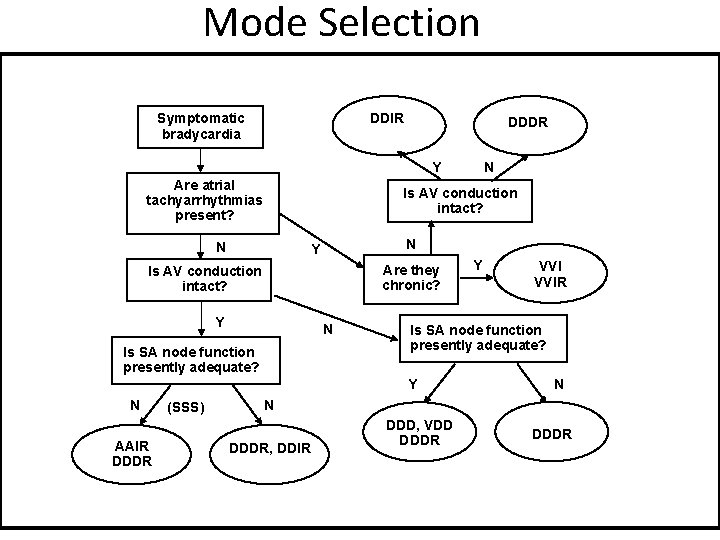
Mode Selection DDIR Symptomatic bradycardia DDDR Y Are atrial tachyarrhythmias present? Is AV conduction intact? N N Y Are they chronic? Is AV conduction intact? Y N Is SA node function presently adequate? AAIR DDDR (SSS) Y VVIR Is SA node function presently adequate? Y N N DDDR, DDIR DDD, VDD DDDR
Optimal Pacing Mode (BPEG) • • Sinus Node Disease AVB SND + AVB Chronic AF + AVB - AAI (R) DDDR + DDIR VVI
Thank u
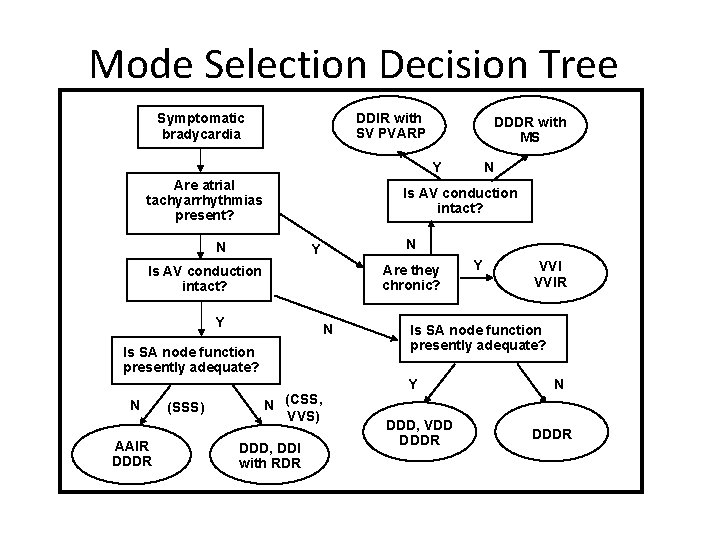
Mode Selection Decision Tree DDIR with SV PVARP Symptomatic bradycardia DDDR with MS Y Are atrial tachyarrhythmias present? Is AV conduction intact? N N Y Are they chronic? Is AV conduction intact? Y N Is SA node function presently adequate? N AAIR DDDR (SSS) N N (CSS, VVS) DDD, DDI with RDR Y VVIR Is SA node function presently adequate? Y DDD, VDD DDDR N DDDR
Pacing Modes Stuart Allen 06
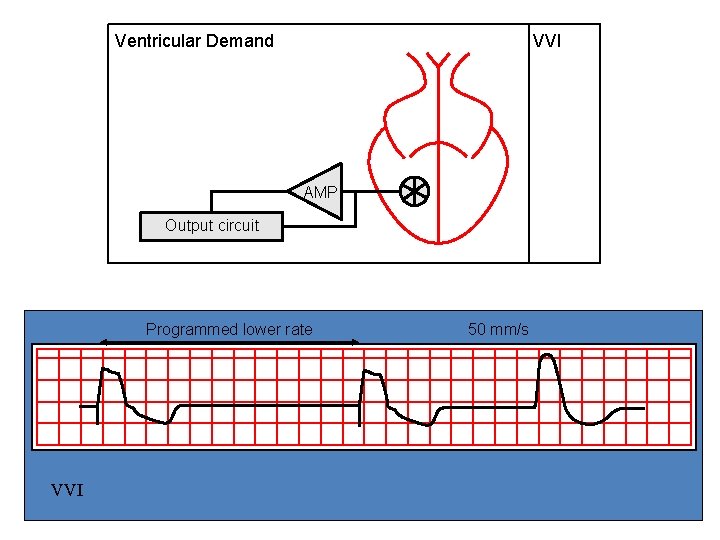
Ventricular Demand VVI AMP Output circuit Programmed lower rate VVI 50 mm/s
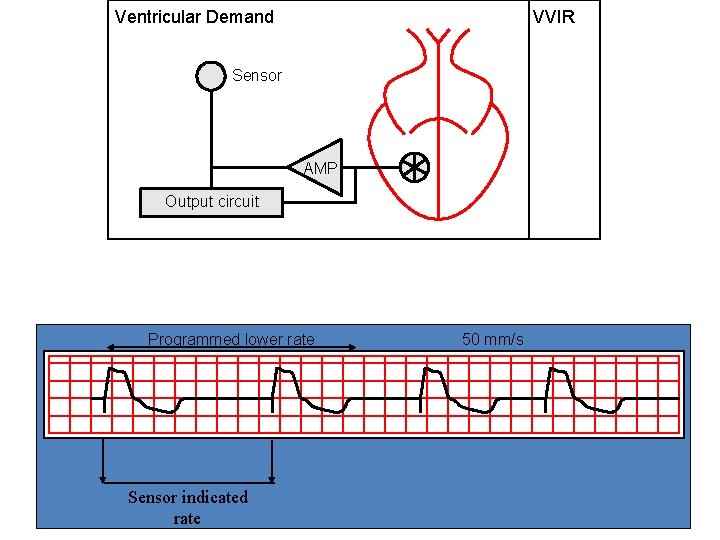
Ventricular Demand VVIR Sensor AMP Output circuit Programmed lower rate Sensor indicated rate 50 mm/s Stuart Allen 06

Atrial Demand AAI AMP Output circuit Programmed lower rate 50 mm/s AAI Stuart Allen 06
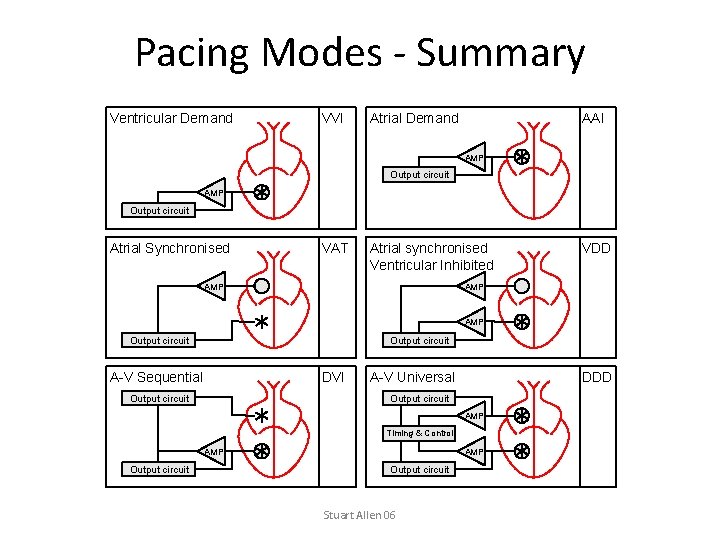
Pacing Modes - Summary Ventricular Demand VVI Atrial Demand AAI AMP Output circuit Atrial Synchronised VAT Atrial synchronised Ventricular Inhibited AMP VDD AMP Output circuit A-V Sequential DVI Output circuit A-V Universal DDD Output circuit AMP Timing & Control AMP Output circuit Stuart Allen 06
- Slides: 120