Basics of Oxygen delivery Adjusting FIO 2 equation
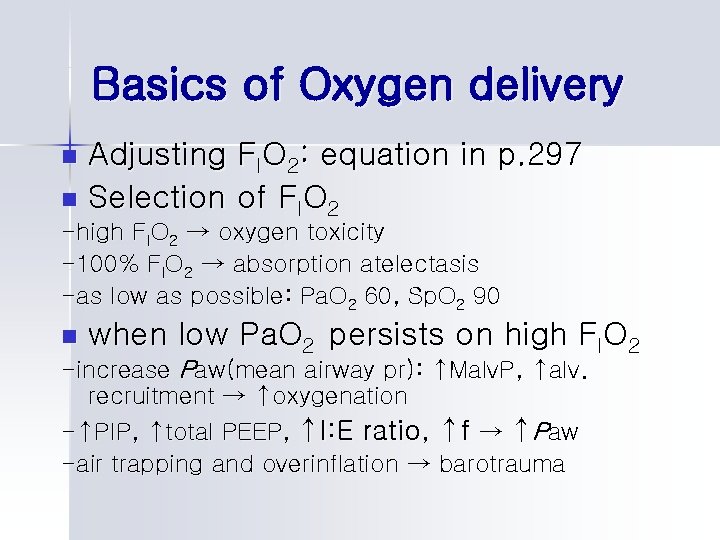
Basics of Oxygen delivery Adjusting FIO 2: equation in p. 297 n Selection of FIO 2 n -high FIO 2 → oxygen toxicity -100% FIO 2 → absorption atelectasis -as low as possible: Pa. O 2 60, Sp. O 2 90 n when low Pa. O 2 persists on high FIO 2 -increase Paw(mean airway pr): ↑Malv. P, ↑alv. recruitment → ↑oxygenation -↑PIP, ↑total PEEP, ↑I: E ratio, ↑f → ↑Paw -air trapping and overinflation → barotrauma
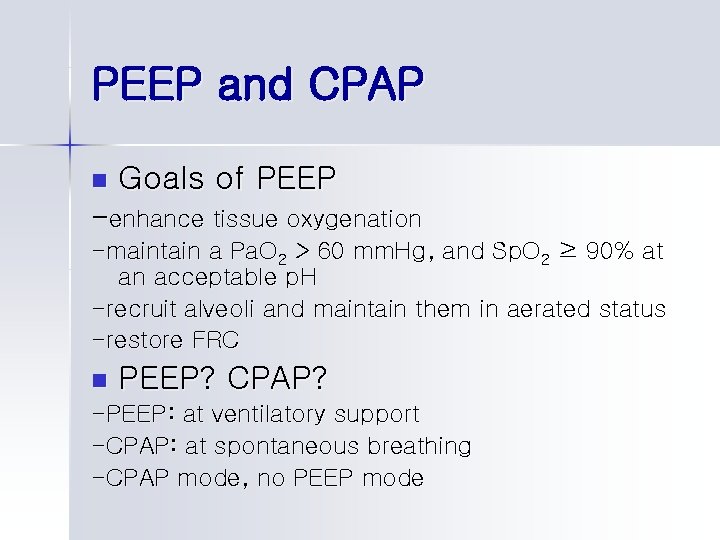
PEEP and CPAP n Goals of PEEP -enhance tissue oxygenation -maintain a Pa. O 2 > 60 mm. Hg, and Sp. O 2 ≥ 90% at an acceptable p. H -recruit alveoli and maintain them in aerated status -restore FRC n PEEP? CPAP? -PEEP: at ventilatory support -CPAP: at spontaneous breathing -CPAP mode, no PEEP mode
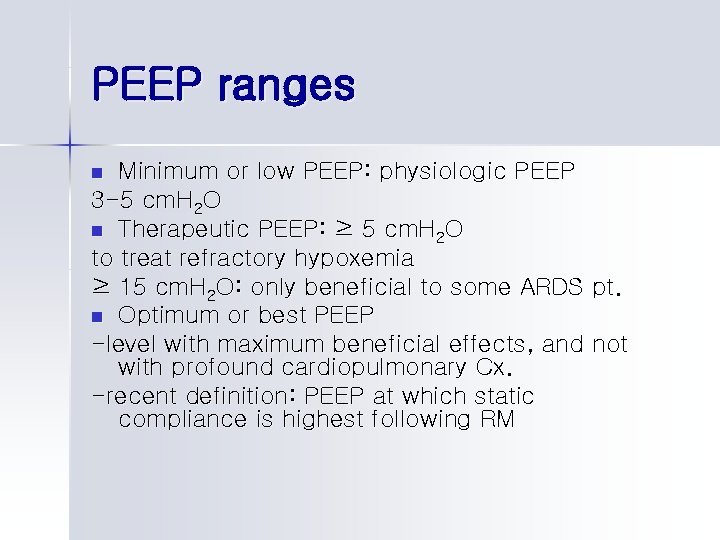
PEEP ranges Minimum or low PEEP: physiologic PEEP 3 -5 cm. H 2 O n Therapeutic PEEP: ≥ 5 cm. H 2 O to treat refractory hypoxemia ≥ 15 cm. H 2 O: only beneficial to some ARDS pt. n Optimum or best PEEP -level with maximum beneficial effects, and not with profound cardiopulmonary Cx. -recent definition: PEEP at which static compliance is highest following RM n

Indications for PEEP/CPAP Box 14 -3 n Examples of specific clinical disorder that may benefit from PEEP n -ALI or ARDS -Cardiogenic pulmonary edema -Bilateral diffuse pneumonia n Initiating PEEP therapy: if indicated, as soon as possible

Selection of appropriate PEEP/CPAP level(optimum PEEP) n Allow adequate tissue oxygenation at a safe FIO 2 with an acceptable Pa. O 2/ FIO 2 ratio (Key point 14 -3) Optimum PEEP study. Box 14 -4 n -pt. appearance -BP -breath sounds -ventilator parameters -static compliance -Pa. O 2, FIO 2, Pa. O 2/ FIO 2, P(A-a)DO 2 -Pa. CO 2 and p. H, P(a-et)CO 2 -hemodynamic data: C(a-v)O 2, Pv. O 2 or Sv. O 2, cardiac output

P-V loops in setting PEEP n n n Lower inflection point(LIP); PPLEX Upper inflection point(UIP). Fig 14 -10 2 -4 cm. H 2 O above LIP Ventilating pressure; not exceed UIP during deflation: deflection point. Fig 14 -17 2 -4 cm. H 2 O above deflection point

How to get static P-V loop Super syringe technique. Fig. 14 -11, 14 -12, 14 -13 n
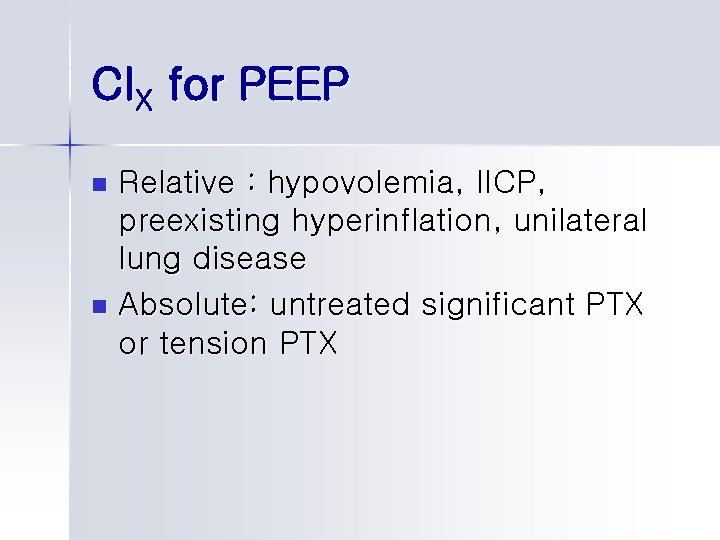
CIX for PEEP Relative : hypovolemia, IICP, preexisting hyperinflation, unilateral lung disease n Absolute: untreated significant PTX or tension PTX n
Pulmonary effects of PEEP Varies with areas of lung: dependent, middle, independent n Upper limit of PEEP beyond which no benefit to lung volume exists; about 15 cm. H 2 O n
Weaning from PEEP n Box 14 -8
ARDS: acute respiratory distress syndrome ALI and ARDS: Pa. O 2/FIO 2 200 vs. 300 n Increased permeability; leakage of protein-rich plasma→ pulmonary edema n Pulmonary vs. nonpulmonary ARDS: -pulmonary; pneumonia, aspiration -nonpulmonary; sepsis, trauma, massive Tf, pancreatitis n ARDS itself can induce multiple organ dysfunction n Shunt, atelectasis n Stiff lung(↓CL), ↓lung vol(↓FRC) n 2 phases: acute exudative and subacute fibroproliferative phase n
ARDS lung is heterogenous Normal/atelectatic but inflatable/completely collapsed → regional overdistention of normal alveoli n Gravitational effect and weight of wet lung tissue → more collapse in dependent region n
Lung protective strategy 1. 2. 3. 4. 5. 6. 7. Small tidal vol. 4 -6 m. L/kg: saves lives!! PEEP: protective effect against lung damage, helps to keep the lung open Pa. O 2: not a good indicator of appropriate PEEP Early application of PEEP. kept above UIP on the deflation limb High pr. with VV → PV. To improve Pa. O 2 ↑Paw with ↑TI Pplat < 30 cm. H 2 O: to avoid overinflation of normal alv Permissive hypercapnia

PEEP/FIO 2 algorithm
Recruitment maneuver in ARDS n Sustained increase in pr. in the lungs with the goal of opening as many collapsed lung units as possible n Once the lungs are recruited, kept open by adequate PEEP above LIP of inflation or preferably UIP of deflation
Types of RM; p. 325 Sustained inflation n PCV with a high PEEP level n PCV with increased PEEP n Sighs n Summary of RM in ARDS. p. 326 n
Pharmacological agents in ventilated patients n Sedatives: to reduce anxiety and agitation, to promote sleep, during nonconventional modes of ventilation n Analgesics: to lessen pain n Paralytics: to facilitate invasive procedure, to prevent movement and ensure the stability of artificial airway, to decrease mean airway pressures during uncoordinated and uncontrolled MV n Primary goal: maintain optimal level of patient comfort and safety
Pharmacological agents in ventilated patients n Sedatives -benzodiazepines: diazepam, midazolam, lorazepam -opioids*: morphine, fentanyl -neuroleptics: haloperidol -anesthetics*: profopol *: also analgesics n Paralytics -depolarizing agents: succinylcholine -nondepolarizing agents: pancuronium, vecuronium
Sedatives and analgesics Level of sedation: Box 15 -1 n Oversedation hinders weaning process n Assess the need for sedation and analgesia -regularly assess pt: relaxed, no pain -Ramsay scale: score 2 -4, adequate sedation n
Benzodiazepines n n n n Drug of choice for treatment of anxiety in critical care Relatively low cost Anxiolytic, hypnotic, muscle relaxant, anticonvulsant, antegrade amnesic Mechanism of action: nonspecific depression of CNS by binding GABA receptor complex→hyperpolarization of neuron Vary in potency, onset of action, elimination half-life(Table 15 -2) Pt-specific factors: age, pathology, concurrent drug Tx Minimal cardiovascular and respiratory effects Reversed by flumazenil
Diazepam(ValiumⓇ) n Rapid onset: 3 -5 min -High lipid solubility -Traverse BBB quickly n Relatively long half-life: 40 -100 hr -active metabolite n Continuous infusion: not recommended
Midazolam(DormicumⓇ) n n Rapid onset of action, short half-life: ideal sedative for acutely agitated pt Prolonged sedation can occur due to accumulation of the drug and metabolites in the peipheral tissues when administered longer than 48 hrs
Lorazepam(AtivanⓇ) The most potent benzodiazepine n Dug of choice for sedating MV pt in the ICU for longer than 24 hrs n Slower onset, longer duration n Potential adverse drug interaction less likely: inactive metabolite n
Opioids Primary analgesic effect n Secondary sedative and anxiolytic effects n Can cause many side effects. Box 15 -2 -dose, pt illness extent, inetgrity of organ function -opioid antagonist; naloxone n
Morphine Potent natural opioid n Preferred agent for intermittent therapy: d/t longer duration of action n Significant CNS and respiratory effects even in healthy individual -depression of brainstem respiratory center -drowsiness and lethergy n GI effect n Decrease sympathetic tone and increase vagal tone: hypotension n Increase in serum histamin level: periph. vasoconstriction, hypotension, pruritus, bronchospasm n Bolus or continuous infusion n Slower onset of action n
Fentanyl n n n n Synthetic opioid More potent than morphine(100 -150 times) Rapid onset Longer half-life than morphine Continuous infusion Minimal cardiovascular effect No histamine release Opioid of choice for hemodynamically unstable pt. or pt. with renal insufficiency
Neuroleptics: haloperidol For Tx of extreme agitation and delirium n CNS depression n Potential side effects -Antidopaminergic and anticholinergic effects -alpha-blockade, evoke Parkinson-like sx -cardiac dysrhythmia; QT prolongation, Td. P -5 mg bolus n
Anesthetic agent: Propofol General anesthetic agent n Sedative, amnesic, hypnotic n No analgesic n Initial bolus(1 -2 mg/kg) followed by continuous infusion(3 -6 mg/kg/hr) n Hemodynamic effect -↓SVR, ↓BP n
Paralytics: neuromuscular blocking agents Depolarizing agents: act like Ach → prolonged depolarization n Depolarizing agents: act as competitive inhibitor n No sedative or analgesic effect n Monitoring neuromuscular blockade -observation skeletal muscle movement and resp. effort -electronic technique: train-of-four n
Vecuronium(NorcuronⓇ) n n Intermediate duration No vagolytic property Loading dose 0. 1 mg/kg → 0. 05 -0. 1 mg/kg/hr Hepatic and biliary elimination: can be used in renal insufficiency
- Slides: 30