BASICS OF HIV TESTING HIV testing in a

BASICS OF HIV TESTING: HIV testing in a time-limited setting - Aleasha Hacault STI/HIV outreach RN - Ida-Lynn Gregan MD, CCFP
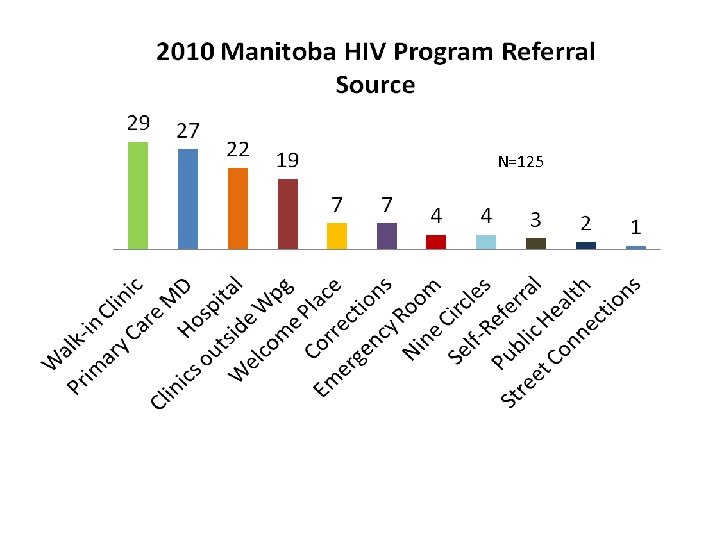
N=125

Objectives • Review current HIV testing recommendations, including HIV “indicator” conditions that should trigger testing • Perform a basic HIV risk assessment • Confidently offer HIV testing (obtaining consent and offer the variety of testing available) • Deliver an HIV +ve test result • Perform an initial assessment on a newly diagnosed HIV+ve individual
A. HIV RISK ASSESSMENT Case Study • 47 year old female (“Susan”) • Aboriginal • Recently divorced • Dating for last 6 months • Sexually active • c/o notable change in vaginal discharge & experiencing dysuria
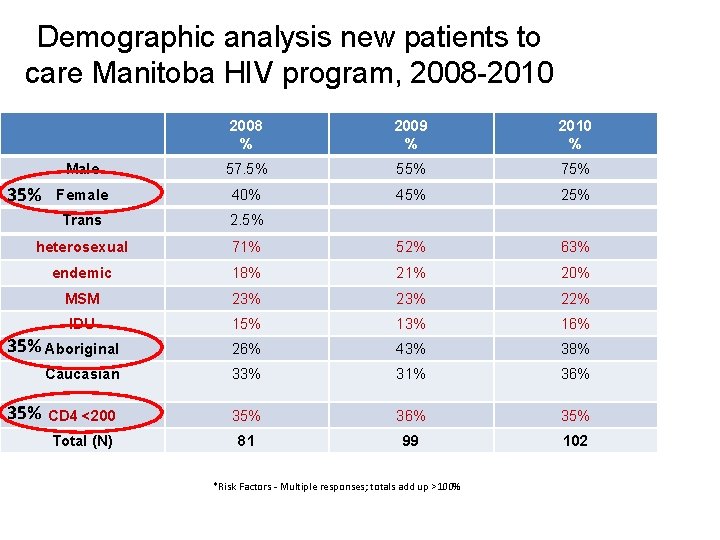
Demographic analysis new patients to care Manitoba HIV program, 2008 -2010 2008 % 2009 % 2010 % Male 57. 5% 55% 75% Female 40% 45% 25% Trans 2. 5% heterosexual 71% 52% 63% endemic 18% 21% 20% MSM 23% 22% IDU 15% 13% 16% 35% Aboriginal 26% 43% 38% Caucasian 33% 31% 36% CD 4 <200 35% 36% 35% Total (N) 81 99 102 35% *Risk Factors - Multiple responses; totals add up >100%
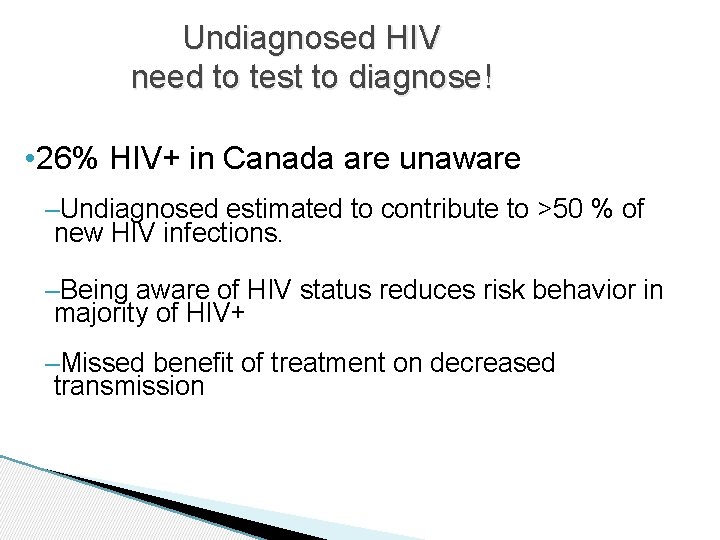
Undiagnosed HIV need to test to diagnose! • 26% HIV+ in Canada are unaware –Undiagnosed estimated to contribute to >50 % of new HIV infections. –Being aware of HIV status reduces risk behavior in majority of HIV+ –Missed benefit of treatment on decreased transmission
Benefits of early HIV diagnosis • Benefits to the infected individual – Antiretroviral therapy (ART) Reduced mortality & morbidity (near normal life expectancy) • Benefits to the public health – Reduced onward transmission - Reduction in unsafe sexual behaviour (68%) - ART-reduced infectiousness ( x 96% in HPTN 0523) – Reduced health care costs
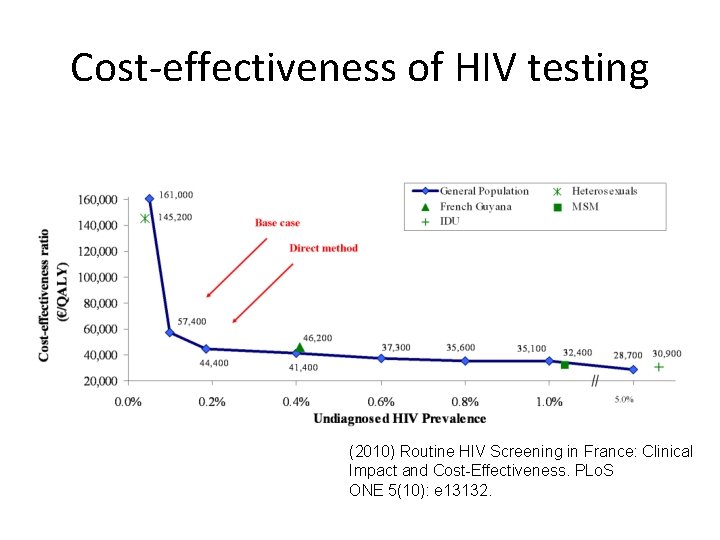
Cost-effectiveness of HIV testing (2010) Routine HIV Screening in France: Clinical Impact and Cost-Effectiveness. PLo. S ONE 5(10): e 13132.
September 22, 2006 US guidelines OPT-OUT • Routine voluntary testing for patients ages 13 -64 in all health care settings • Persons at high risk should be screened annually • No separate consent for HIV • Prevention counseling should not be required • Objectives – Increase screening – Foster early detection – Identify and counsel persons with unrecognized HIV infection and link them to clinical and preventative services – Reduce perinatal transmission
Test for HIV • • • Unprotected sex (anal or vaginal w/o barrier) Sex under the influence of ETOH or drugs Tested +ve for an STI (GC, CT, Hep, syphilis) Shared needles/drug equipment Tatooing, piercing, or accupuncture (unsterile) Blood or blood products prior to Nov 1986 PHAC April 2012
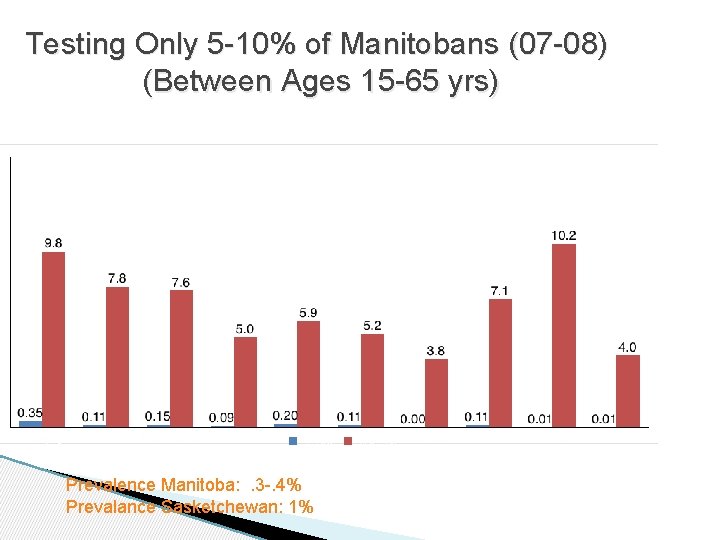
Testing Only 5 -10% of Manitobans (07 -08) (Between Ages 15 -65 yrs) Prevalence Manitoba: . 3 -. 4% Prevalance Sasketchewan: 1%
HIDES (HIV Indicator Diseases in Europe Study) Indicator conditions: 1. AIDS-defining conditions (ADC) 2. Conditions associated with increased HIV prevalence (>0. 1%) 3. Conditions where failure to diagnose HIV infection may have severe consequences for person’s health - Dr. Keith Radcliffe, HIV Europe March 2012, Copenhagen
AIDS-defining conditions (ADC) • Opportunistic infections – Fungal e. g. Pneumocystis jiroveci, cryptococcosis, histoplasmosis, candidiasis (oesophageal, tracheal, pulmonary) – Bacterial e. g. Tuberculosis (TB), disseminated Mycobacterium avium, recurrent pneumonia or salmonella septicaemia
AIDS-defining conditions (cont’d): • Opportunistic (cont’d): – Parasitic e. g. cerebral toxoplasmosis, cryptospridiosis, microsporidiosis – Viral e. g. CMV retinitis, PML, persistent HSV • Neoplasms – Non-Hodgkin’s lymphoma, Kaposi’s sarcoma, cervical carcinoma
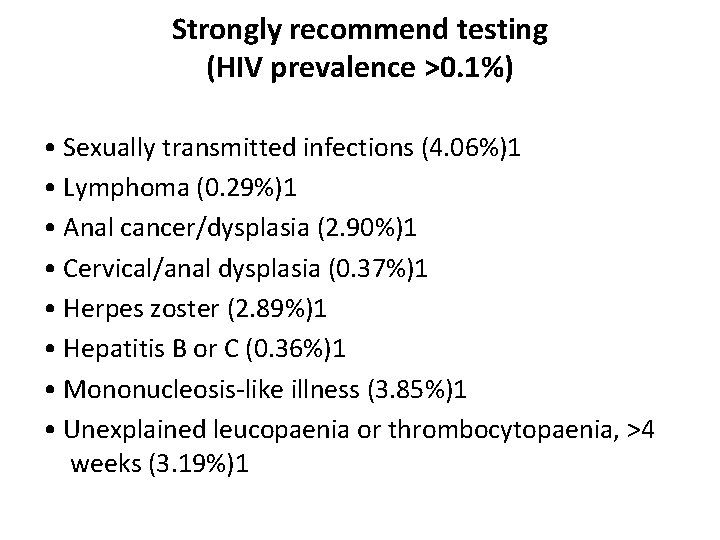
Strongly recommend testing (HIV prevalence >0. 1%) • Sexually transmitted infections (4. 06%)1 • Lymphoma (0. 29%)1 • Anal cancer/dysplasia (2. 90%)1 • Cervical/anal dysplasia (0. 37%)1 • Herpes zoster (2. 89%)1 • Hepatitis B or C (0. 36%)1 • Mononucleosis-like illness (3. 85%)1 • Unexplained leucopaenia or thrombocytopaenia, >4 weeks (3. 19%)1
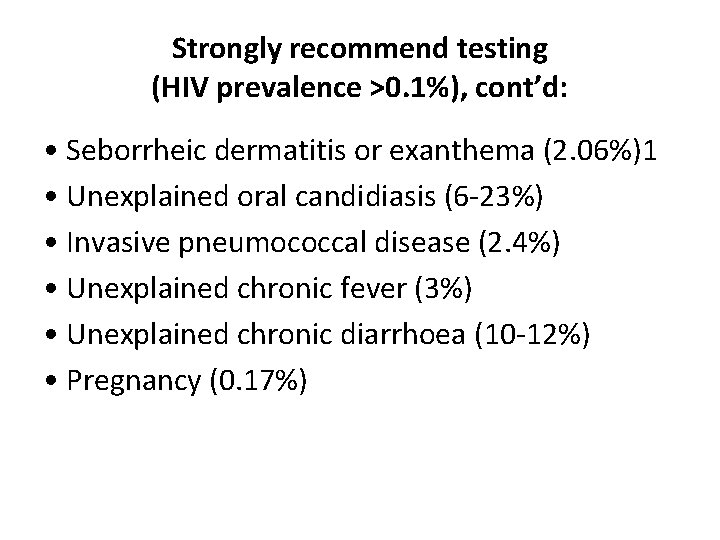
Strongly recommend testing (HIV prevalence >0. 1%), cont’d: • Seborrheic dermatitis or exanthema (2. 06%)1 • Unexplained oral candidiasis (6 -23%) • Invasive pneumococcal disease (2. 4%) • Unexplained chronic fever (3%) • Unexplained chronic diarrhoea (10 -12%) • Pregnancy (0. 17%)
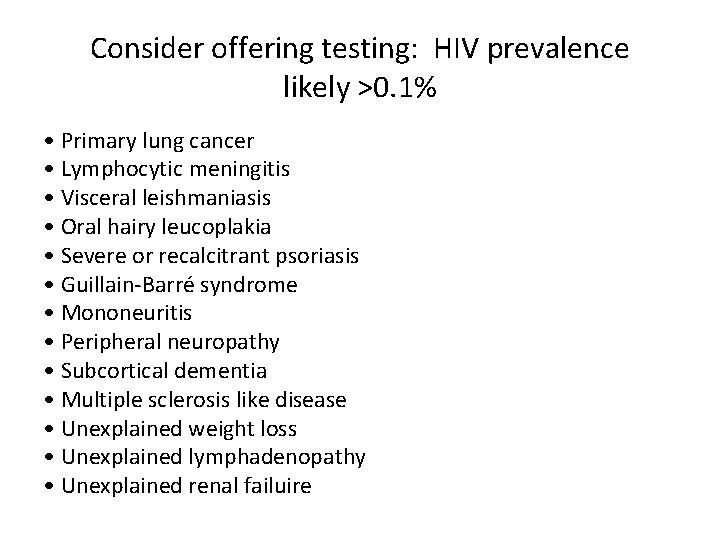
Consider offering testing: HIV prevalence likely >0. 1% • Primary lung cancer • Lymphocytic meningitis • Visceral leishmaniasis • Oral hairy leucoplakia • Severe or recalcitrant psoriasis • Guillain-Barré syndrome • Mononeuritis • Peripheral neuropathy • Subcortical dementia • Multiple sclerosis like disease • Unexplained weight loss • Unexplained lymphadenopathy • Unexplained renal failuire
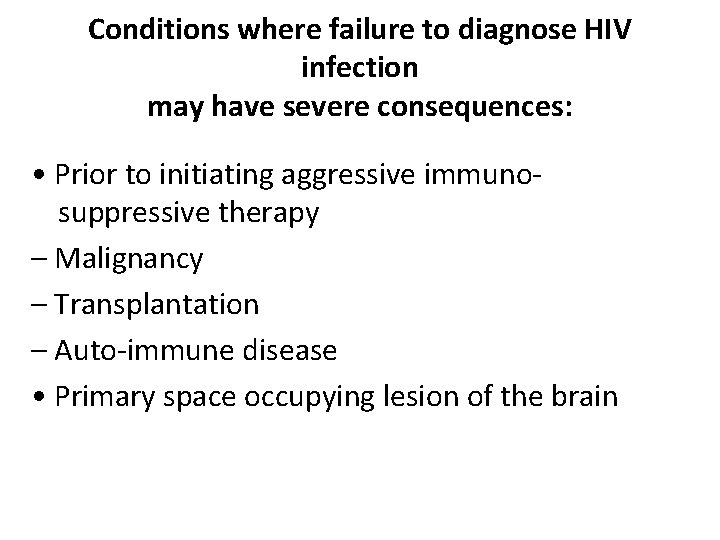
Conditions where failure to diagnose HIV infection may have severe consequences: • Prior to initiating aggressive immunosuppressive therapy – Malignancy – Transplantation – Auto-immune disease • Primary space occupying lesion of the brain
A. HIV RISK ASSESSMENT Case Study • 47 year old female (“Susan”) • Aboriginal • Recently divorced • Dating for last 6 months • Sexually active • c/o notable change in vaginal discharge & experiencing dysuria
A. HIV RISK ASSESSMENT Type of partners (relationship) Drug/ETOH as a part of sexual experience Use of barriers # of partners Priority Assessment Type of sex
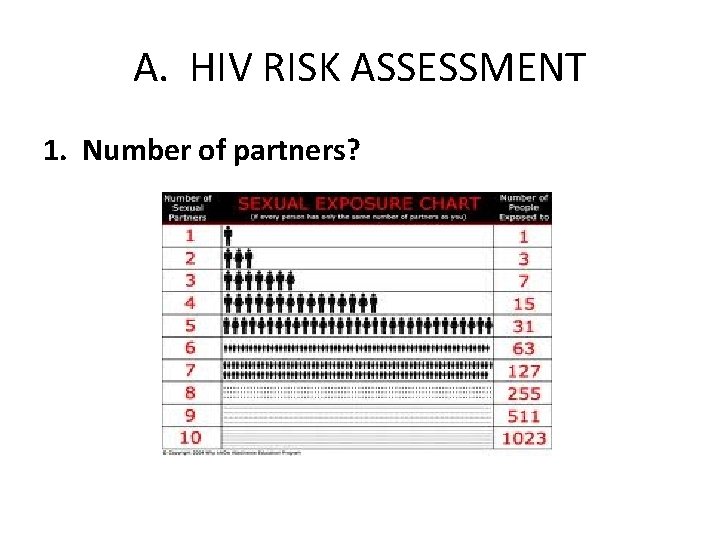
A. HIV RISK ASSESSMENT 1. Number of partners?
A. HIV RISK ASSESSMENT 2. Type of partners/relationship? Known Unknown
A. HIV RISK ASSESSMENT 3. Use of barriers? Consistent/inconsistent use
A. HIV RISK ASSESSMENT 4. Type of sex? Vaginal Anal Oral Sex toys BDSM Non-penetrative
A. HIV RISK ASSESSMENT 5. Drug-use as a part of sexual experience? Drugs: legal/illegal drugs, alcohol
A. HIV RISK ASSESSMENT SUSAN’S RISK FACTORS: • Sexually active with multiple partners in past year (6 mos. ) with unknown sexual histories • Vaginal, oral • High and low risk sexual activities • Known and anonymous partners • Alcohol use as part of sexual experience
PERFORMING AN HIV TEST… 1. 2. 3. 4. Point of Care Testing (POCT, “rapid testing”) Nominal Non-nominal Anonymous
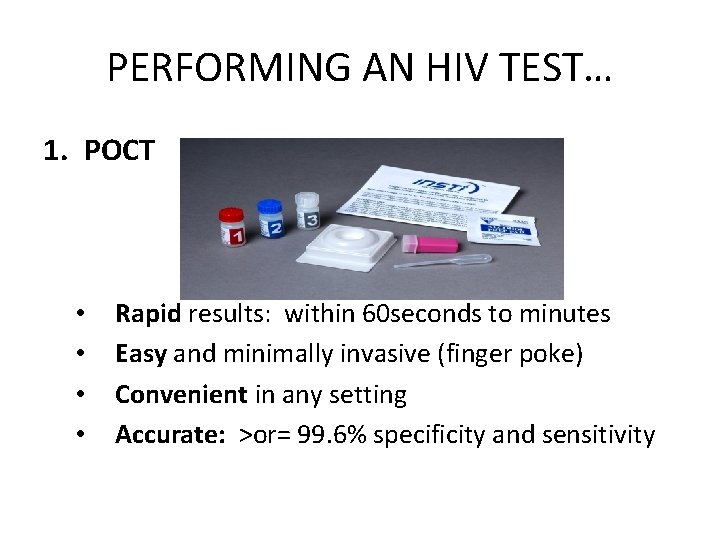
PERFORMING AN HIV TEST… 1. POCT • • Rapid results: within 60 seconds to minutes Easy and minimally invasive (finger poke) Convenient in any setting Accurate: >or= 99. 6% specificity and sensitivity
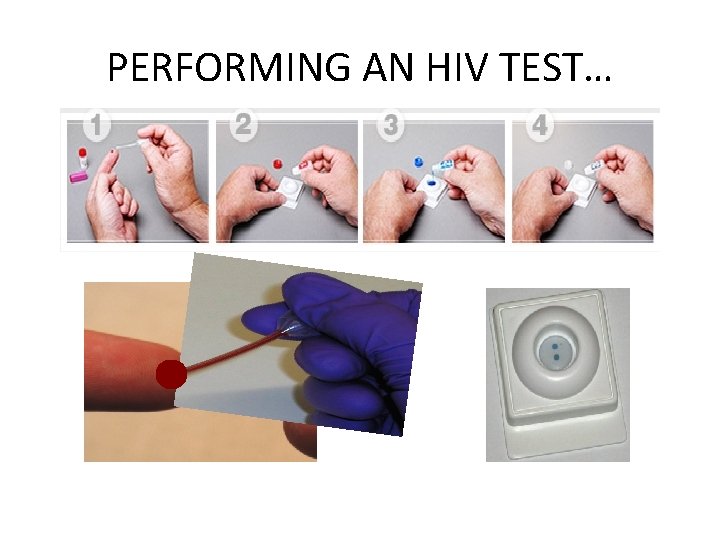
PERFORMING AN HIV TEST…
PERFORMING AN HIV TEST… 2. Nominal • • • Test is ordered using full name of patient Known identity of person being tested Health Care Practitioner ordering test obligated to report positive results to Manitoba Health
PERFORMING AN HIV TEST… 3. Non-nominal • • Test is ordered using patients initials or code Only the person ordering the test knows the person being tested Health care provider ordering the test is responsible for notifying Manitoba Health of positive results Test results is linked and entered in patient’s chart
B. PERFORMING AN HIV TEST 4. Anonymous • Test is ordered using a bar code • Practitioner performing the test and lab do not know the identity of the person being tested • Client returns to clinic to receive results with bar code ID card
B. PERFORMING AN HIV TEST Anonymous… • If client loses card, no results can be given • Anyone can return with found card and access results • Paper copies of results are not provided
PERFORMING AN HIV TEST… Informed consent is required Verbal consent is required BUT Written consent is not required
C. OBTAINING CONSENT 1. 2. 3. 4. 5. Inform that you are performing test Rationale/Indicators for test Limitations Consequences Opportunity for patient to decline
CASE STUDY • • • Nominal testing Indication: complete STI screen Limitation: window period Consequences explained Opportunity to decline • Plan for follow-up
D. Delivering a positive result A. Negative Result • • Review Safer Sex Practices/Harm Reduction Window period
D. Delivering a positive result B. • • • Positive Result Meaning of positive result Natural course of illness Management & treatment – Life expectancy – Quality of life
D. Delivering a positive result • Coping • Supports • Prevention • • Universal precautions Safer sex Issues of disclosure Birth control • Partner notification • Public health
D. Delivering a positive result • Safety • Acute suicidality • Threats of violence to self or others
D. Delivering a positive result • Linkage to care • Manitoba HIV program: P: 940 -6089; 1 -866 -4490165 Fax: 940 -6003 -HIV care and treatment -Counselling services -Social work; outreach -pharmacist --Dietician -Occupational Therapy
Initial Assessment of the HIV +ve individual: • Dr. R. Barrios/ BC Centre for Excellence in HIV/AIDS: http: //www. cfenet. ubc. ca/sites/default/files/up loads/Final%203%20 R. Barrios%20 Initial. Assessment_1. pdf
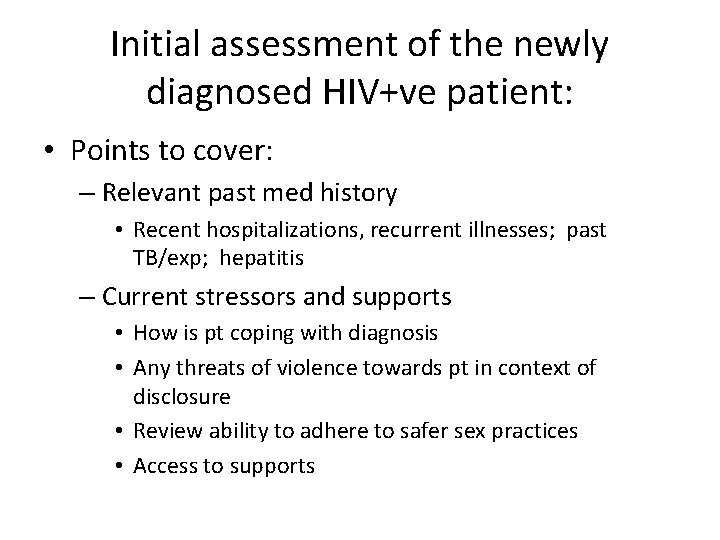
Initial assessment of the newly diagnosed HIV+ve patient: • Points to cover: – Relevant past med history • Recent hospitalizations, recurrent illnesses; past TB/exp; hepatitis – Current stressors and supports • How is pt coping with diagnosis • Any threats of violence towards pt in context of disclosure • Review ability to adhere to safer sex practices • Access to supports
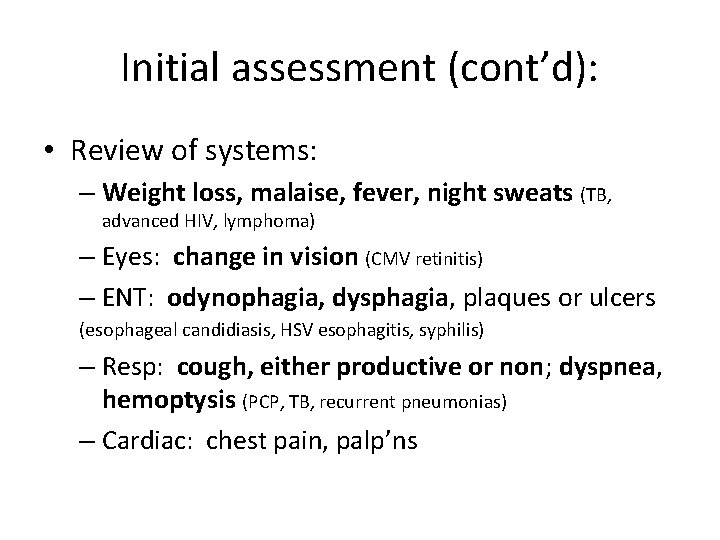
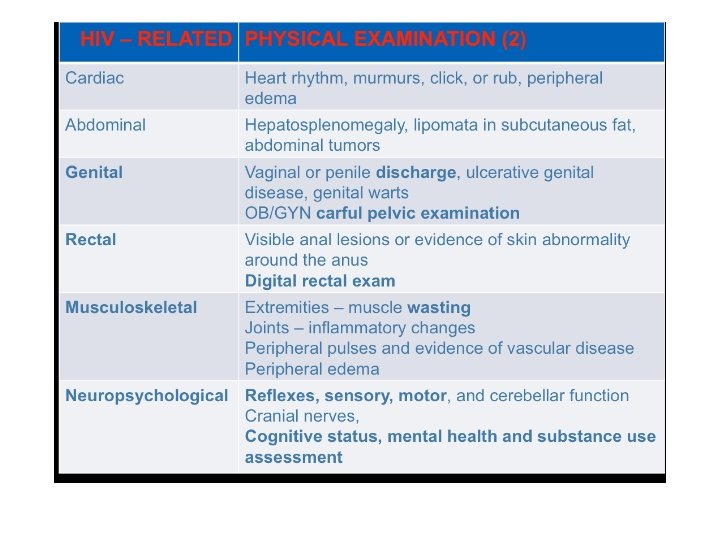
Initial assessment (cont’d): • Review of systems: – Weight loss, malaise, fever, night sweats (TB, advanced HIV, lymphoma) – Eyes: change in vision (CMV retinitis) – ENT: odynophagia, dysphagia, plaques or ulcers (esophageal candidiasis, HSV esophagitis, syphilis) – Resp: cough, either productive or non; dyspnea, hemoptysis (PCP, TB, recurrent pneumonias) – Cardiac: chest pain, palp’ns
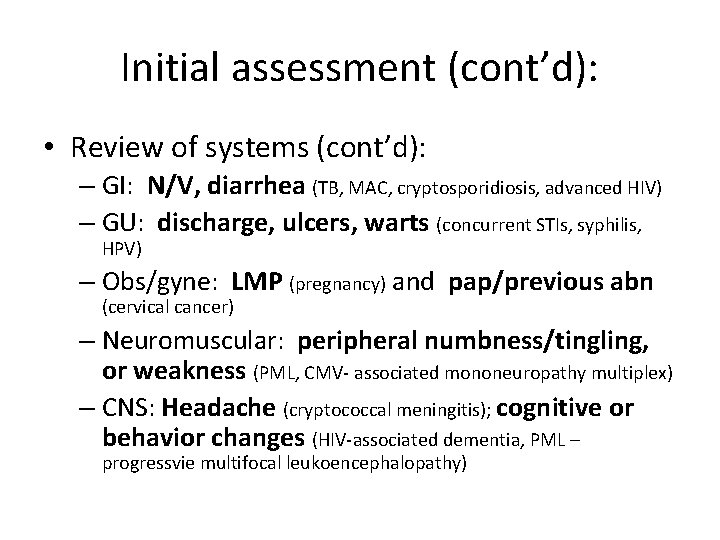
Initial assessment (cont’d): • Review of systems (cont’d): – GI: N/V, diarrhea (TB, MAC, cryptosporidiosis, advanced HIV) – GU: discharge, ulcers, warts (concurrent STIs, syphilis, HPV) – Obs/gyne: LMP (pregnancy) and pap/previous abn (cervical cancer) – Neuromuscular: peripheral numbness/tingling, or weakness (PML, CMV- associated mononeuropathy multiplex) – CNS: Headache (cryptococcal meningitis); cognitive or behavior changes (HIV-associated dementia, PML – progressvie multifocal leukoencephalopathy)
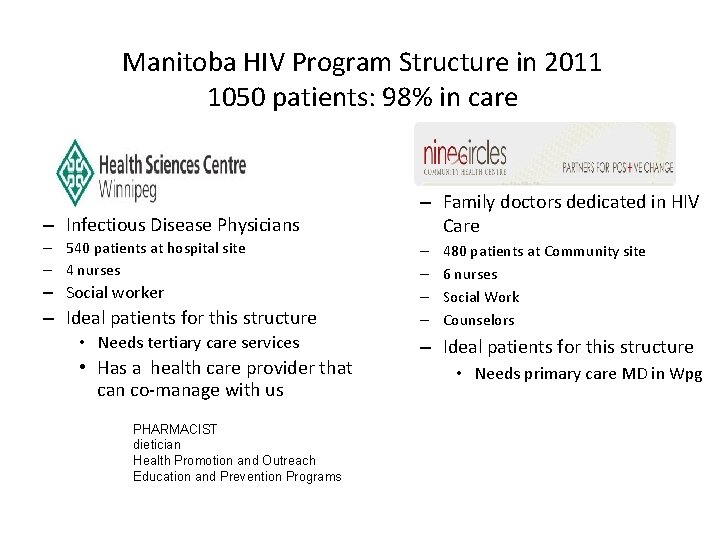
Manitoba HIV Program Structure in 2011 1050 patients: 98% in care – Infectious Disease Physicians – 540 patients at hospital site – 4 nurses – Social worker – Ideal patients for this structure • Needs tertiary care services • Has a health care provider that can co-manage with us PHARMACIST dietician Health Promotion and Outreach Education and Prevention Programs – Family doctors dedicated in HIV Care – – 480 patients at Community site 6 nurses Social Work Counselors – Ideal patients for this structure • Needs primary care MD in Wpg
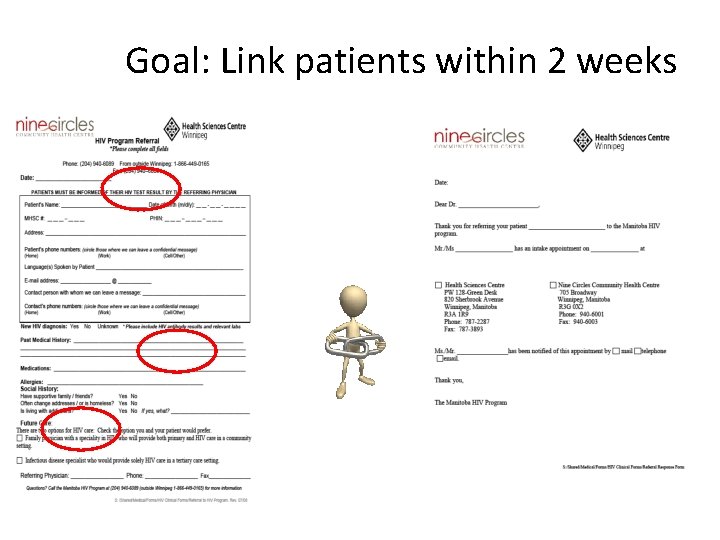
Goal: Link patients within 2 weeks
• Questions? ? ?
- Slides: 50