Basics of Hemodynamics Christian Sonnier MD Learning Objectives
Basics of Hemodynamics Christian Sonnier MD
Learning Objectives • • Review basic cardiac anatomy Review cardiac output and its variables Discuss non-invasive and invasive monitoring Discuss strategies to manipulate cardiac output
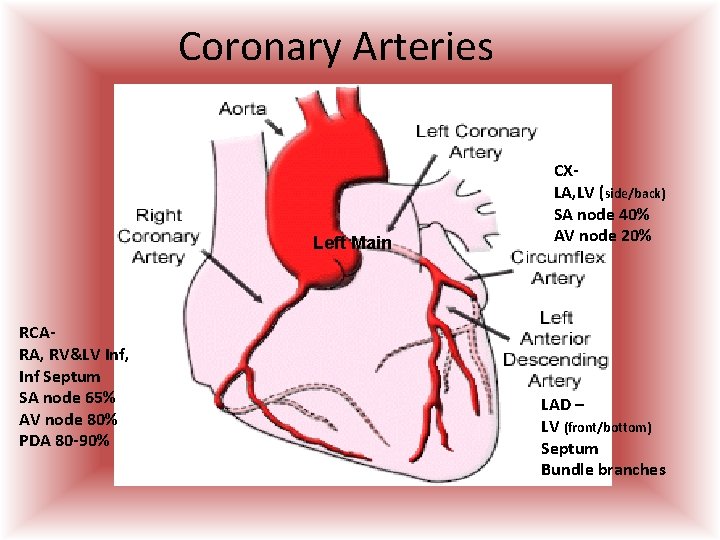
Coronary Arteries Left Main RCARA, RV&LV Inf, Inf Septum SA node 65% AV node 80% PDA 80 -90% CXLA, LV (side/back) SA node 40% AV node 20% LAD – LV (front/bottom) Septum Bundle branches
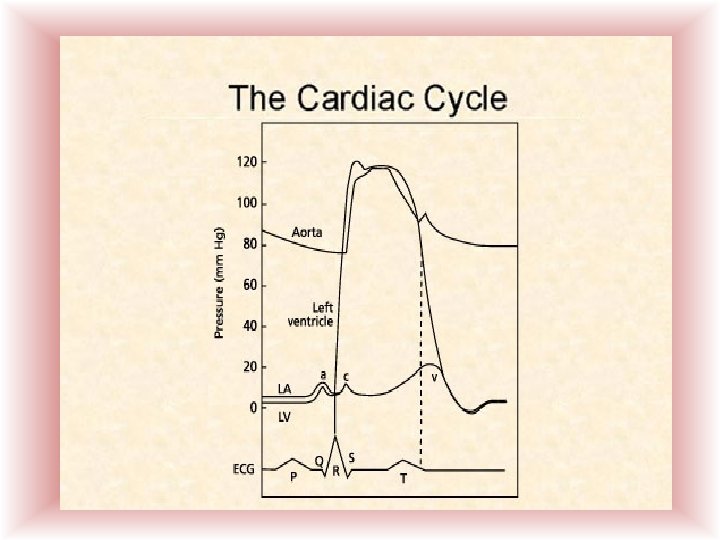
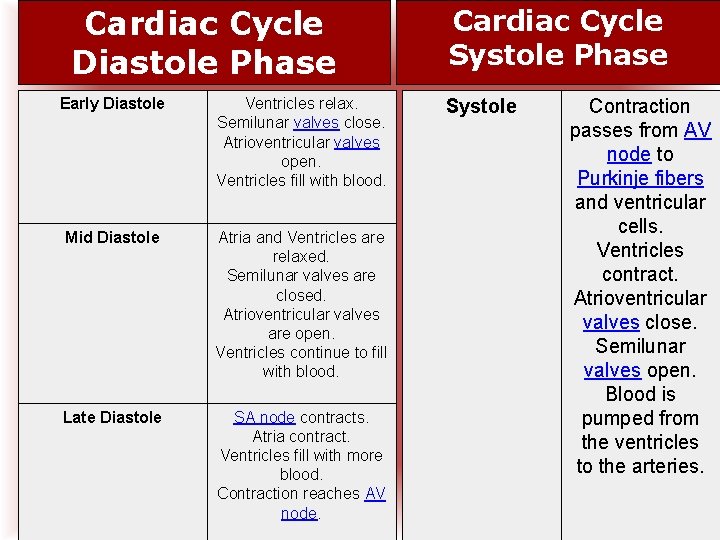
Cardiac Cycle Diastole Phase Early Diastole Ventricles relax. Semilunar valves close. Atrioventricular valves open. Ventricles fill with blood. Mid Diastole Atria and Ventricles are relaxed. Semilunar valves are closed. Atrioventricular valves are open. Ventricles continue to fill with blood. Late Diastole SA node contracts. Atria contract. Ventricles fill with more blood. Contraction reaches AV node. Cardiac Cycle Systole Phase Systole Contraction passes from AV node to Purkinje fibers and ventricular cells. Ventricles contract. Atrioventricular valves close. Semilunar valves open. Blood is pumped from the ventricles to the arteries.
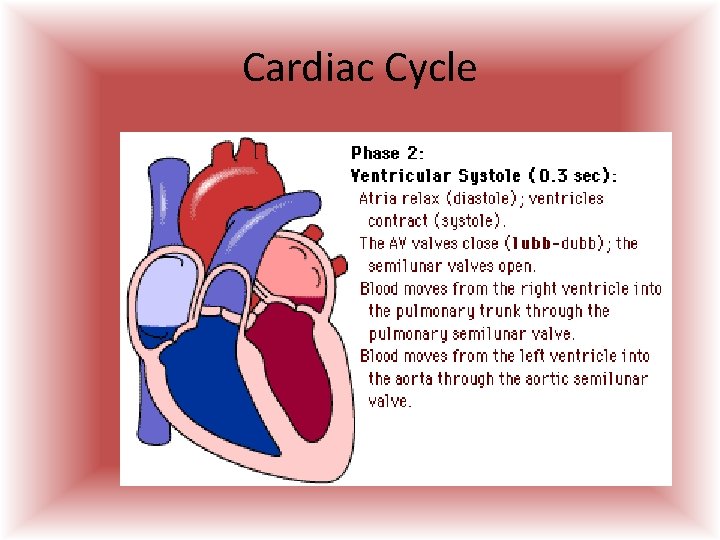
Cardiac Cycle
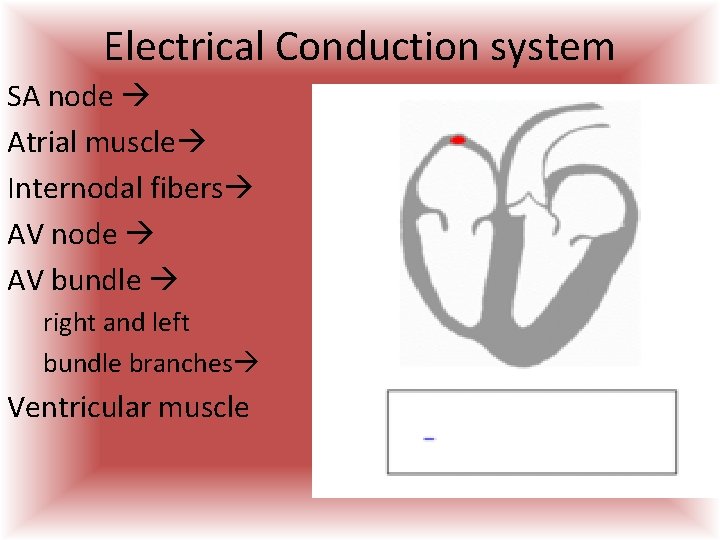
Electrical Conduction system SA node Atrial muscle Internodal fibers AV node AV bundle right and left bundle branches Ventricular muscle
Autonomic Nervous System • The autonomic nervous system stimulates the heart through a balance of sympathetic nervous system and parasympathetic nervous system innervations. – The sympathetic nervous system plays a role in speeding up impulse formation, thus increasing the heart rate – The parasympathetic nervous system slows the heart rate.
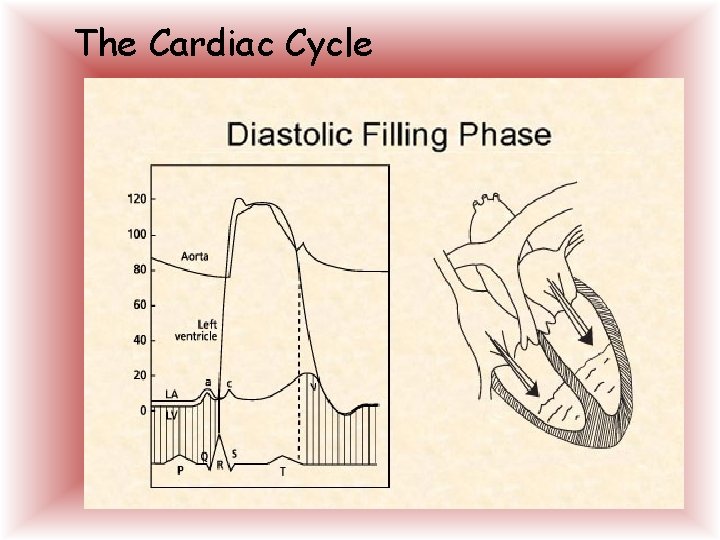
The Cardiac Cycle
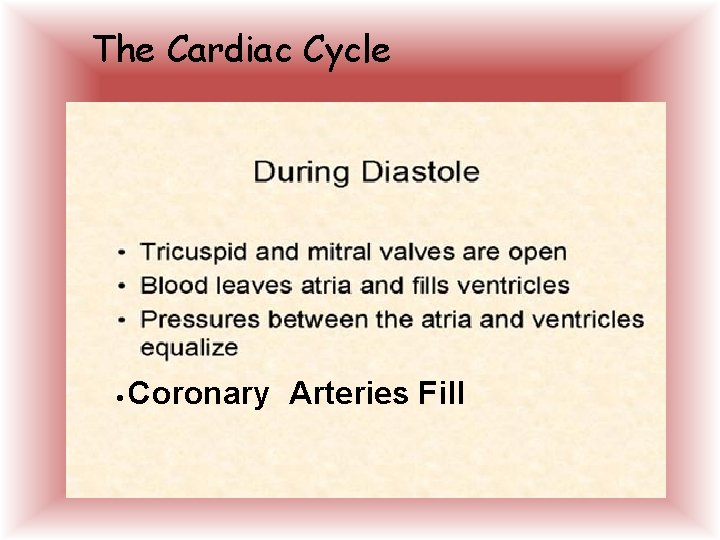
The Cardiac Cycle • Coronary Arteries Fill
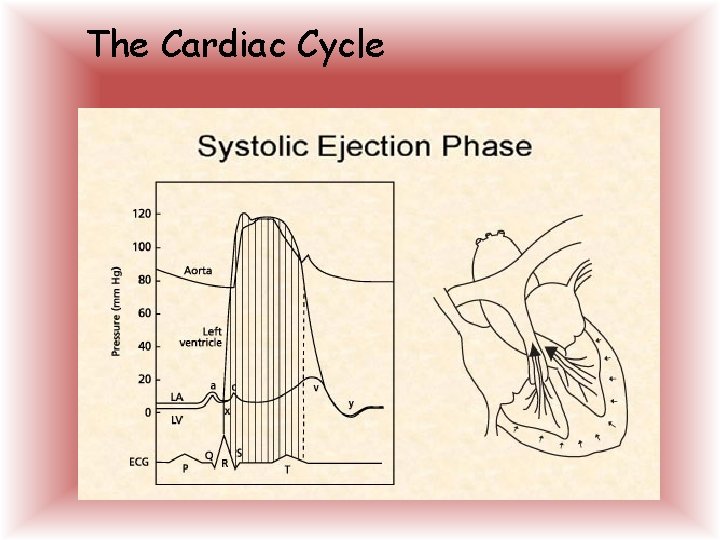
The Cardiac Cycle
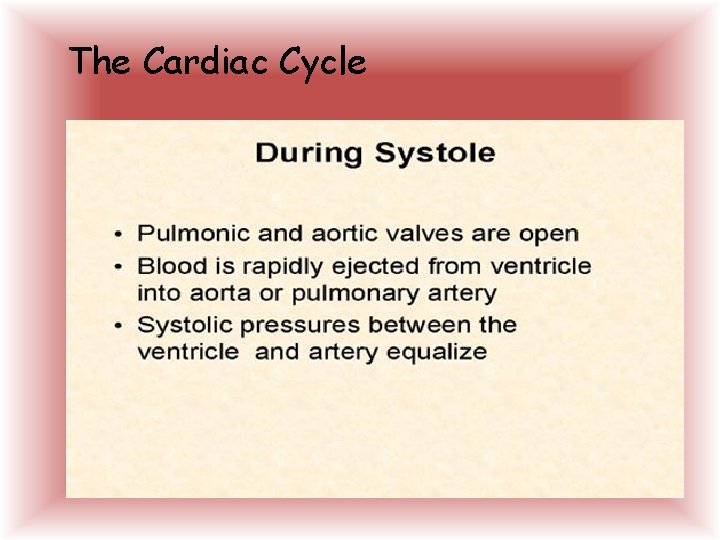
The Cardiac Cycle
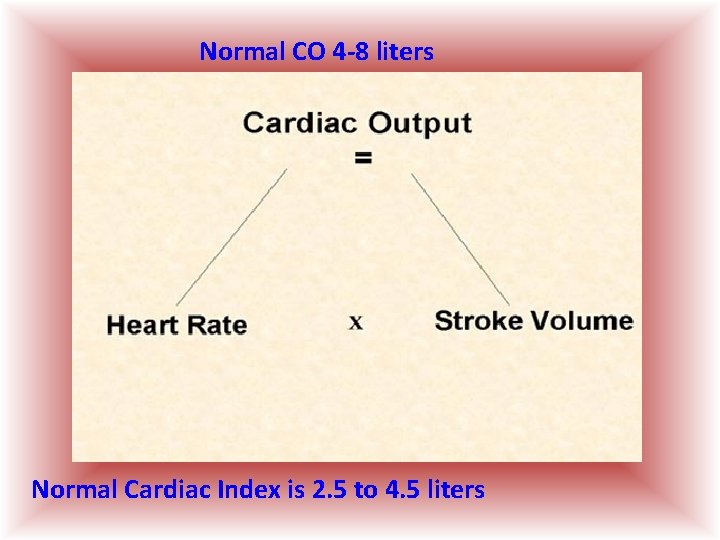
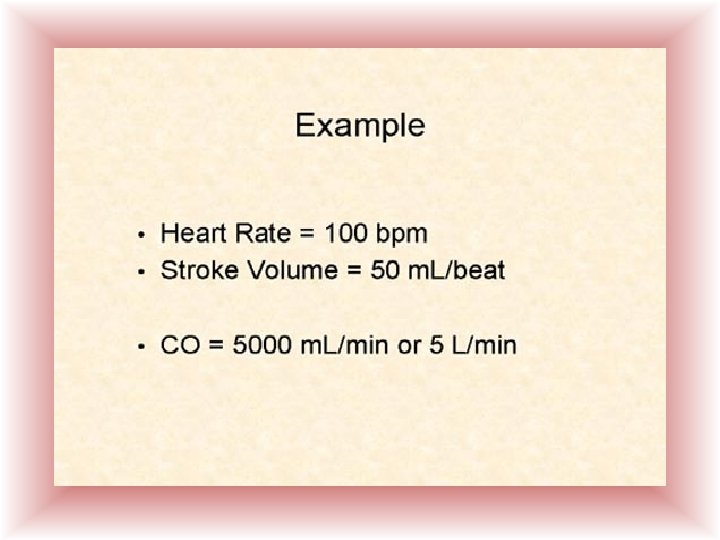
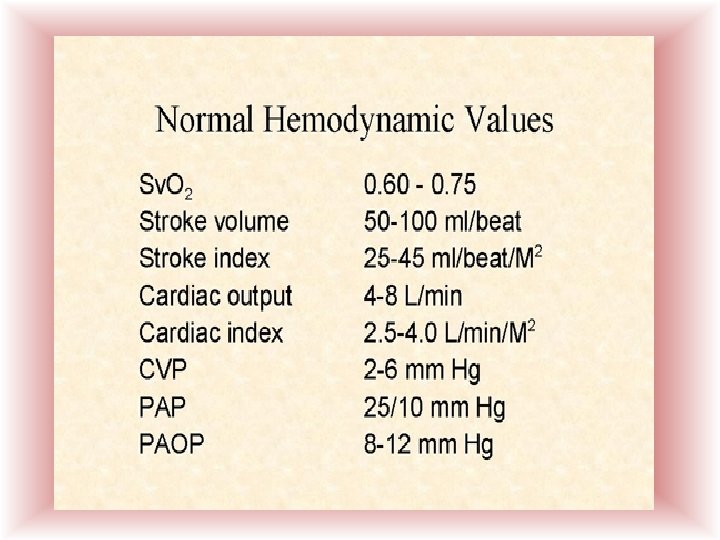
Normal CO 4 -8 liters Normal Cardiac Index is 2. 5 to 4. 5 liters
Heart Rate ØWorks with Stroke Volume ØCompensatory ØTachycardia ØBradycardia ØDysrhythmias
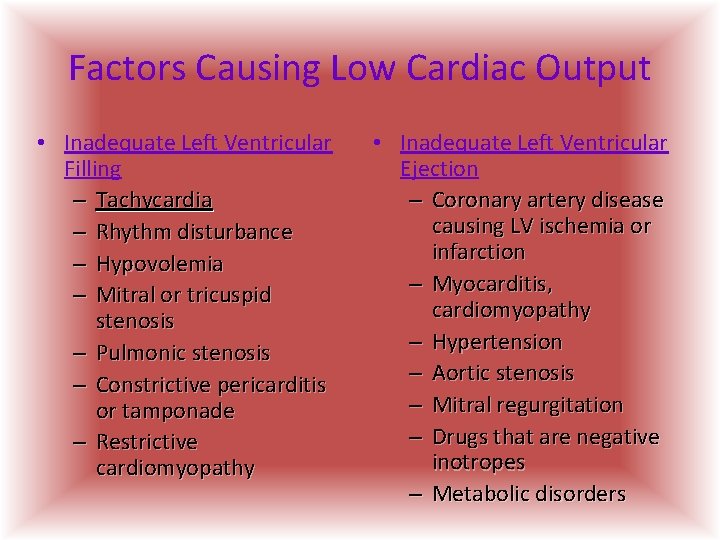
Factors Causing Low Cardiac Output • Inadequate Left Ventricular Filling – Tachycardia – Rhythm disturbance – Hypovolemia – Mitral or tricuspid stenosis – Pulmonic stenosis – Constrictive pericarditis or tamponade – Restrictive cardiomyopathy • Inadequate Left Ventricular Ejection – Coronary artery disease causing LV ischemia or infarction – Myocarditis, cardiomyopathy – Hypertension – Aortic stenosis – Mitral regurgitation – Drugs that are negative inotropes – Metabolic disorders
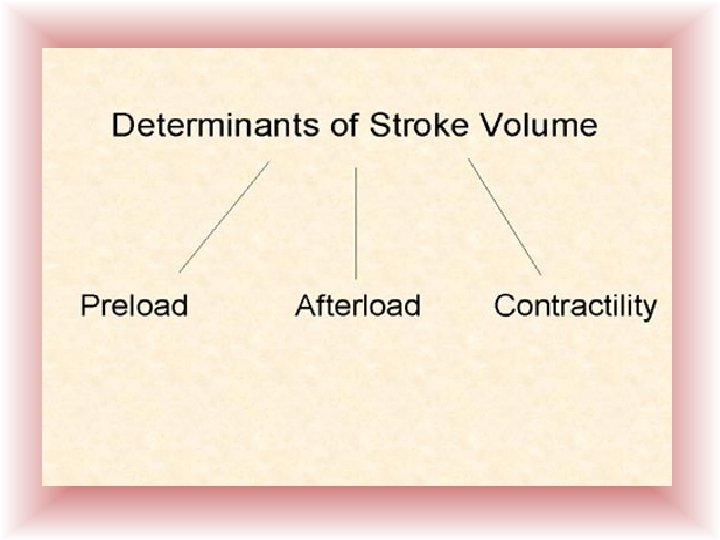
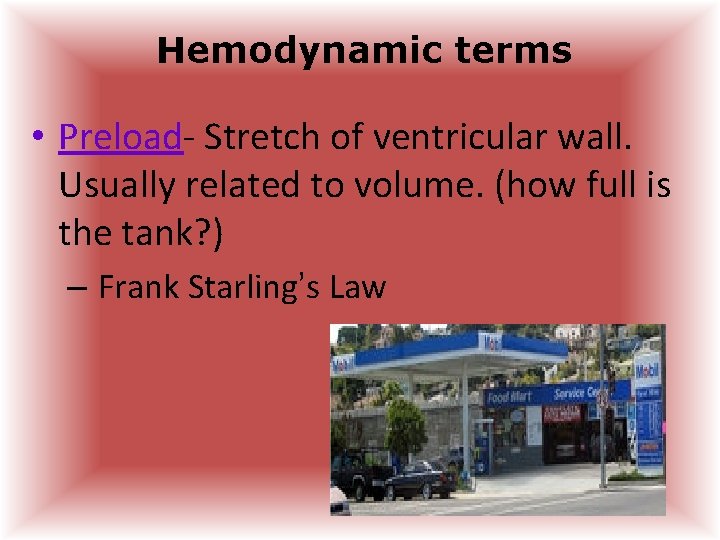
Hemodynamic terms • Preload- Stretch of ventricular wall. Usually related to volume. (how full is the tank? ) – Frank Starling’s Law
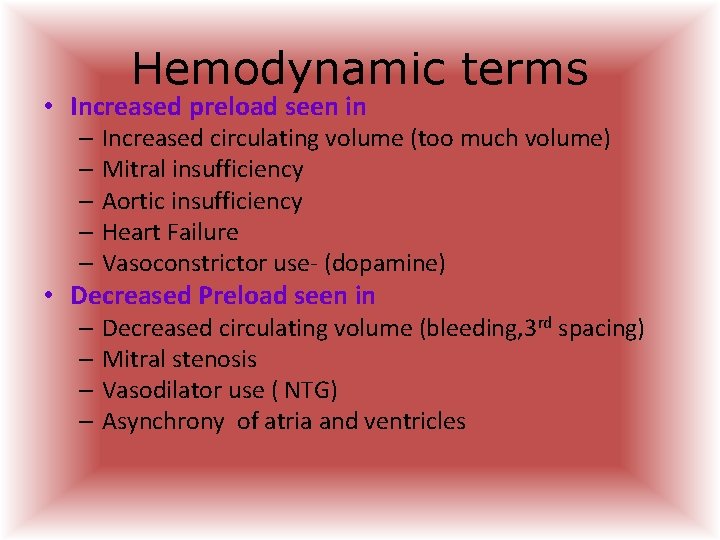
Hemodynamic terms • Increased preload seen in – Increased circulating volume (too much volume) – Mitral insufficiency – Aortic insufficiency – Heart Failure – Vasoconstrictor use- (dopamine) • Decreased Preload seen in – Decreased circulating volume (bleeding, 3 rd spacing) – Mitral stenosis – Vasodilator use ( NTG) – Asynchrony of atria and ventricles
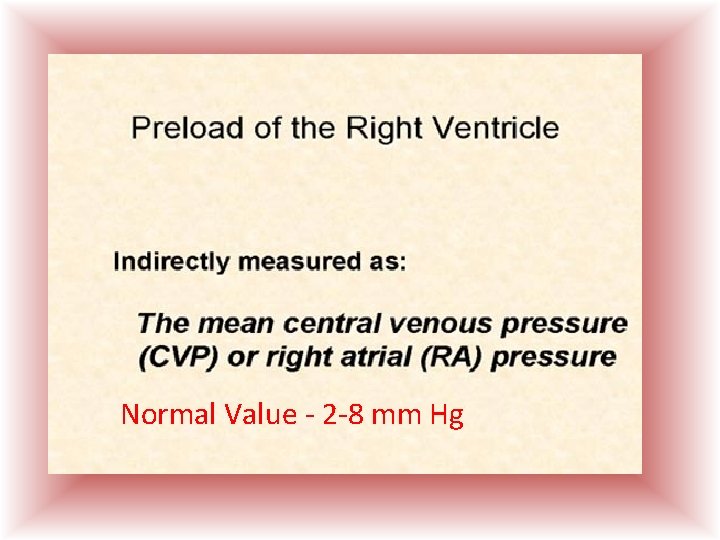
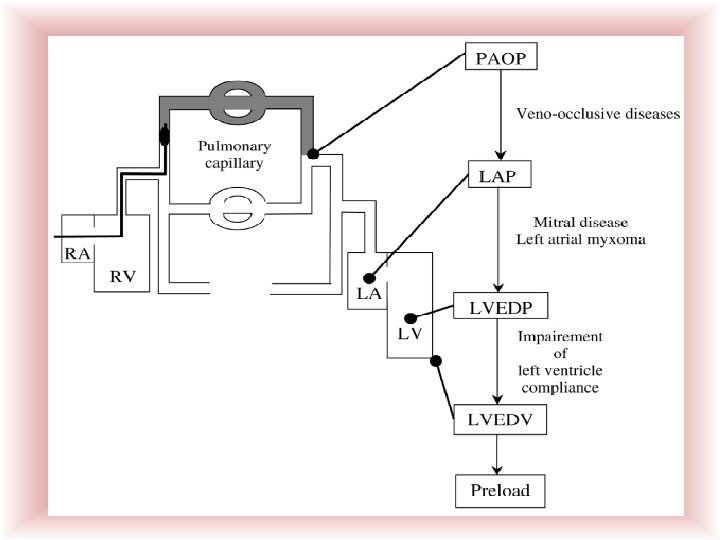
Normal Value - 2 -8 mm Hg
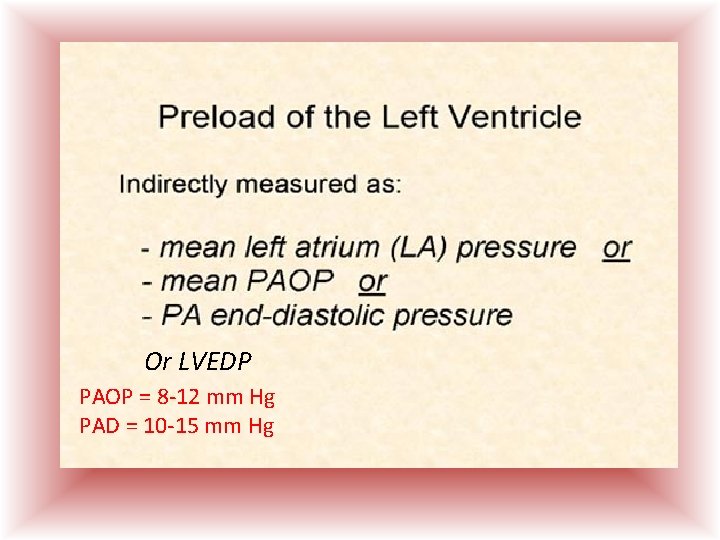
Or LVEDP PAOP = 8 -12 mm Hg PAD = 10 -15 mm Hg
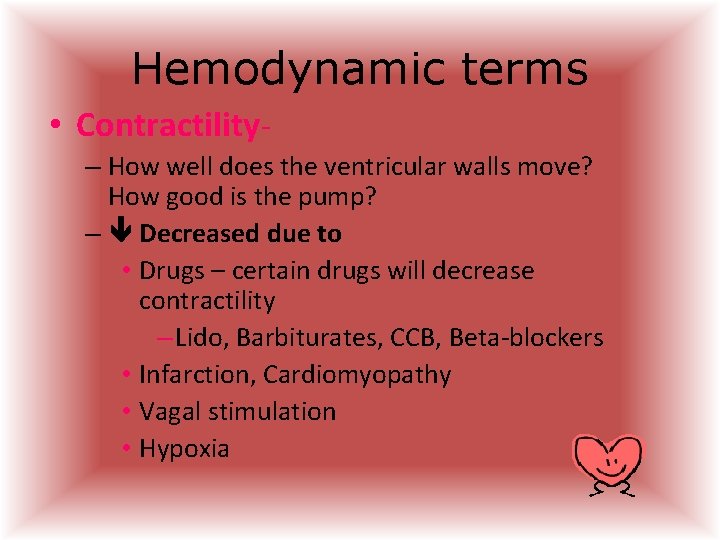
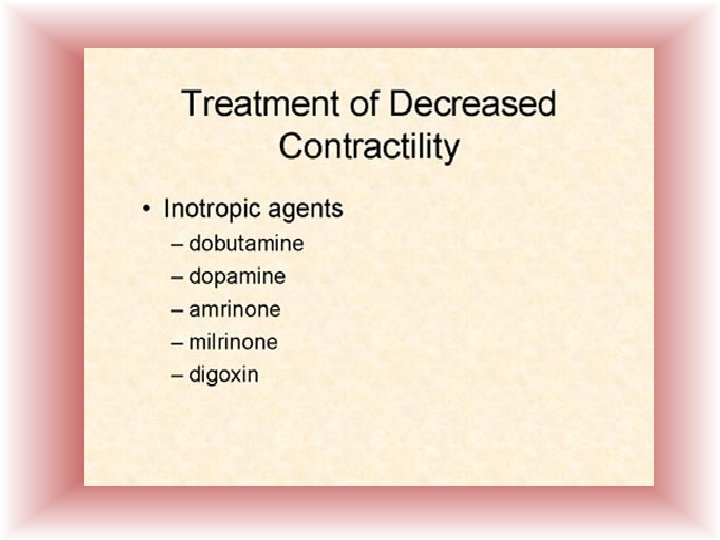
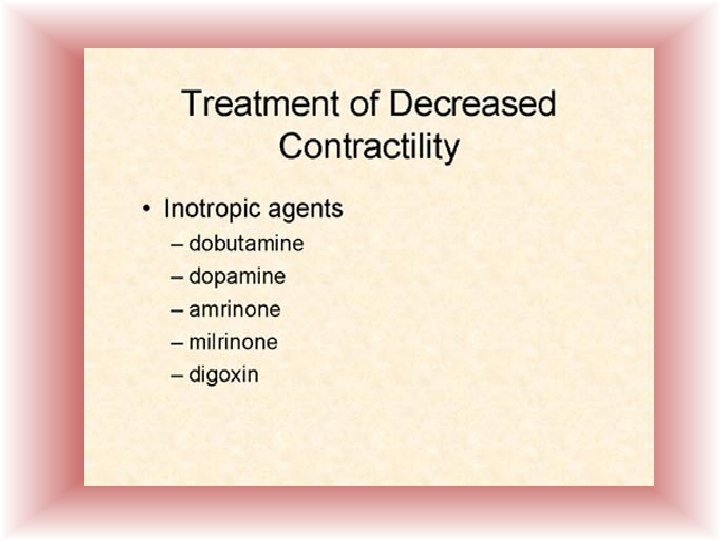
Hemodynamic terms • Contractility– How well does the ventricular walls move? How good is the pump? – Decreased due to • Drugs – certain drugs will decrease contractility – Lido, Barbiturates, CCB, Beta-blockers • Infarction, Cardiomyopathy • Vagal stimulation • Hypoxia

Hemodynamic terms • Contractility– Increased • Positive inotropic drugs – Dobutamine, Digoxin, Epinephrine • Sympathetic stimulation – Fear, anxiety • Hypercalcemia ( high calcium)
CONTRACTILITY PRECAUTIONS • Do Not use Inotropes until volume deficiency is corrected • Correct Hypoxemia and electrolyte imbalance.
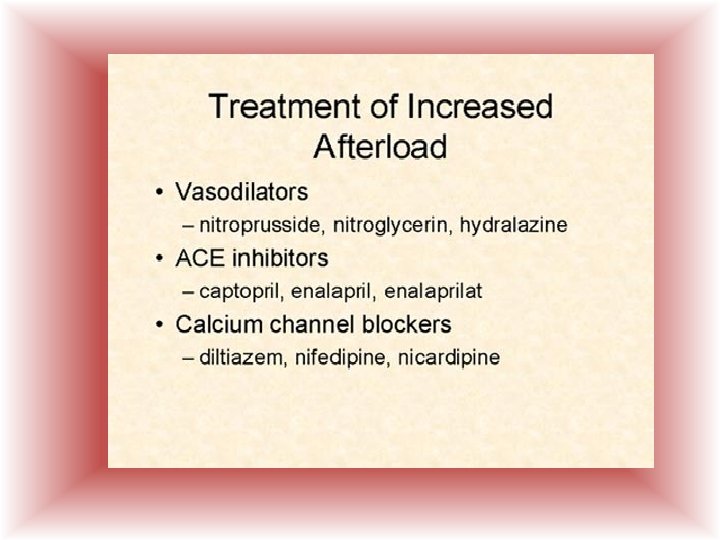
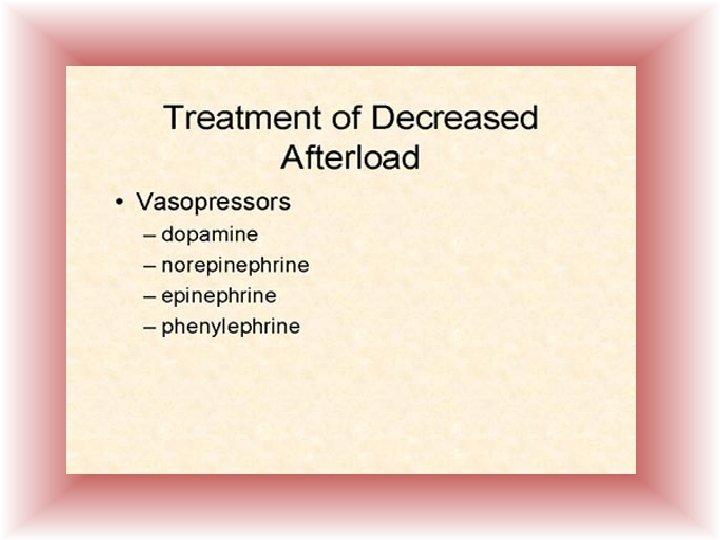
Hemodynamic terms • Afterload – resistance the blood in the ventricle must overcome to force the valves open and eject contents to circulation.
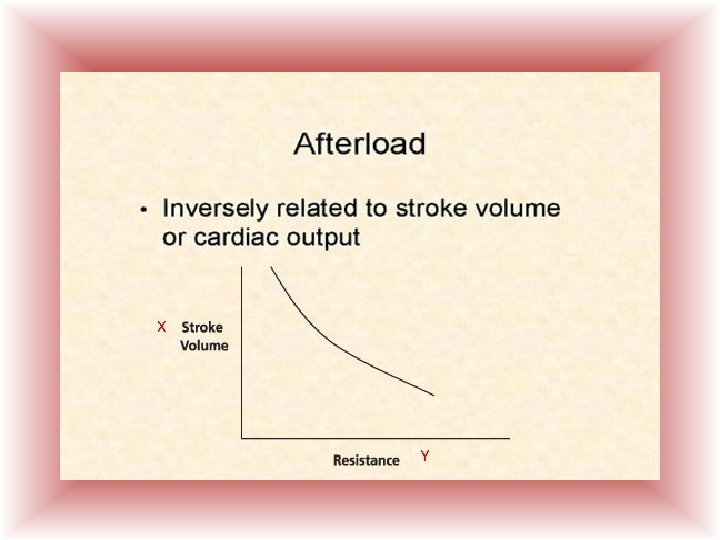
X Y
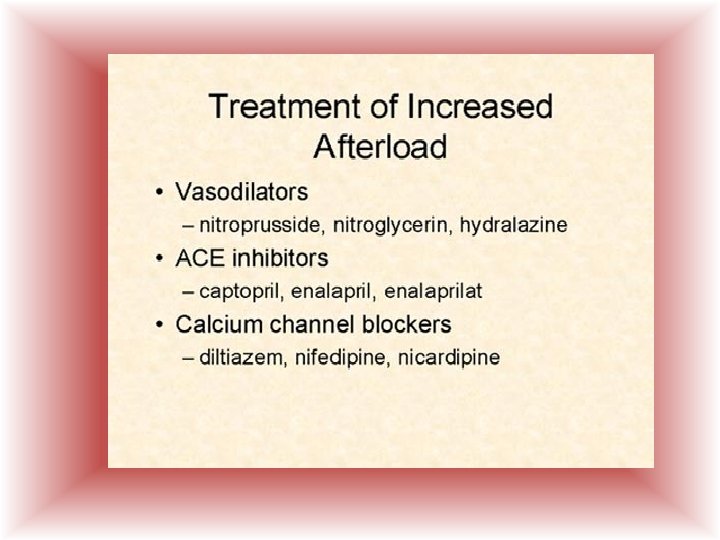
Hemodynamic terms • Factors that increase afterload are – Systemic resistance or High Blood pressure – Aortic stenosis – Myocardial Infarcts / Cardiomyopathy – Polycythemia – Increased blood viscosity
Hemodynamic terms • Factors that decrease Afterload – Decreased volume – Septic shock- warm phase – End stage cirrhosis – Vasodilators
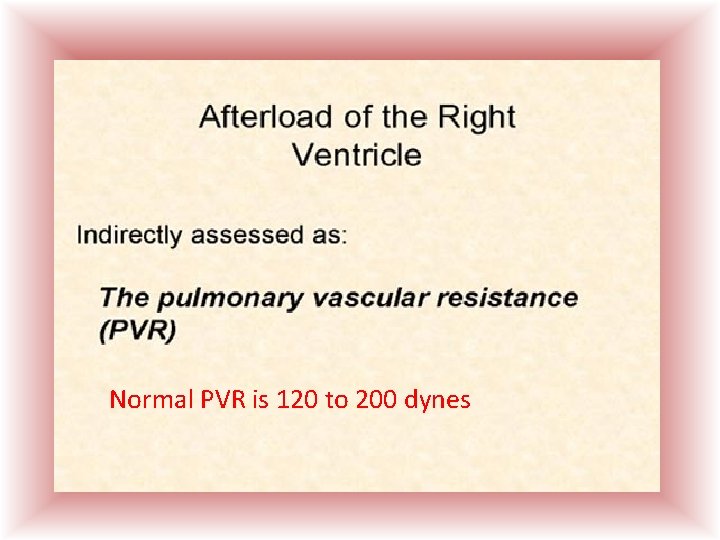
Normal PVR is 120 to 200 dynes
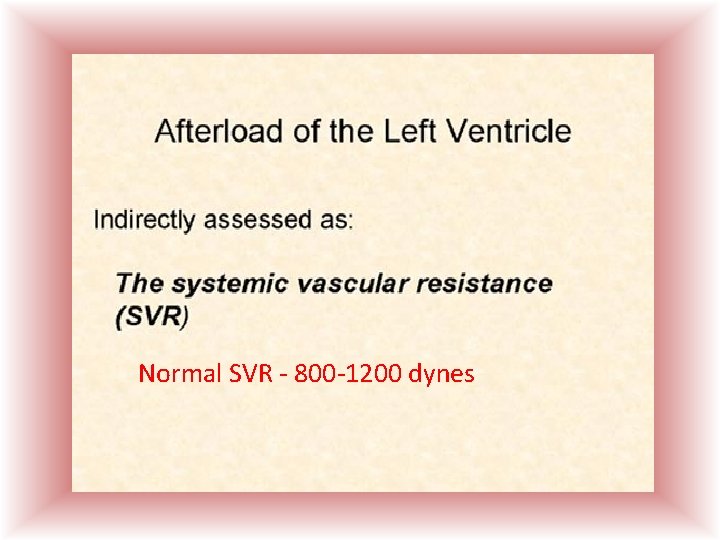
Normal SVR - 800 -1200 dynes
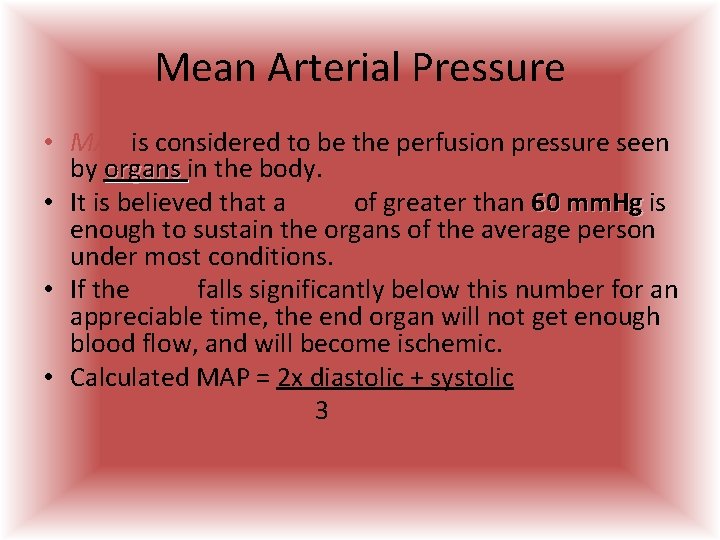
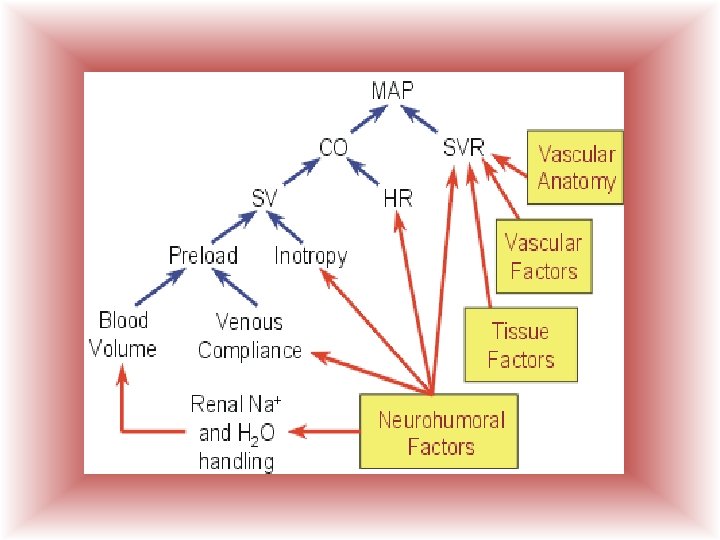
Mean Arterial Pressure • MAP is considered to be the perfusion pressure seen by organs in the body. • It is believed that a MAP of greater than 60 mm. Hg is enough to sustain the organs of the average person under most conditions. • If the MAP falls significantly below this number for an appreciable time, the end organ will not get enough blood flow, and will become ischemic. • Calculated MAP = 2 x diastolic + systolic 3
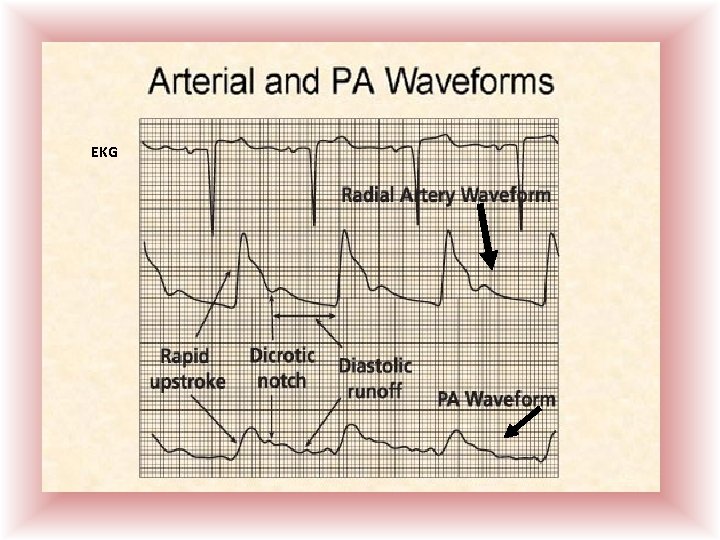
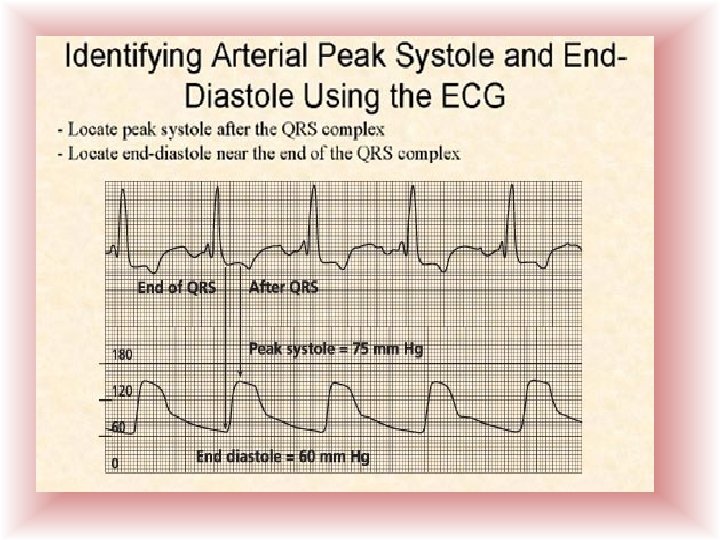
EKG
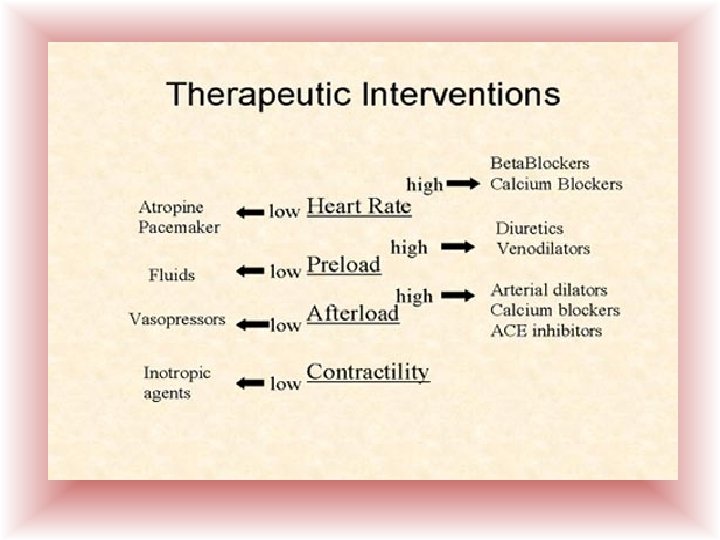
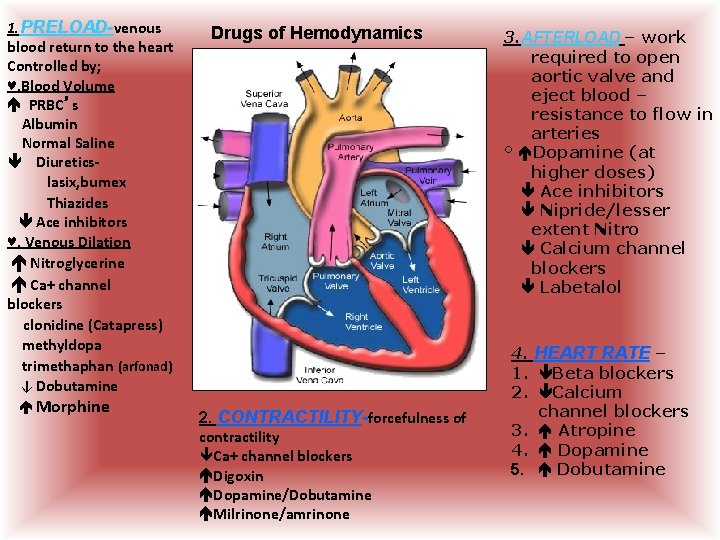
1. PRELOAD-venous blood return to the heart Controlled by; ♥. Blood Volume PRBC’s Albumin Normal Saline Diureticslasix, bumex Thiazides Ace inhibitors ♥. Venous Dilation Nitroglycerine Ca+ channel blockers clonidine (Catapress) methyldopa trimethaphan (arfonad) ↓ Dobutamine Morphine Drugs of Hemodynamics 2. CONTRACTILITY-forcefulness of contractility Ca+ channel blockers Digoxin Dopamine/Dobutamine Milrinone/amrinone 3. AFTERLOAD – work required to open aortic valve and eject blood – resistance to flow in arteries ° Dopamine (at higher doses) Ace inhibitors Nipride/lesser extent Nitro Calcium channel blockers Labetalol 4. HEART RATE – 1. Beta blockers 2. Calcium channel blockers 3. Atropine 4. Dopamine 5. Dobutamine
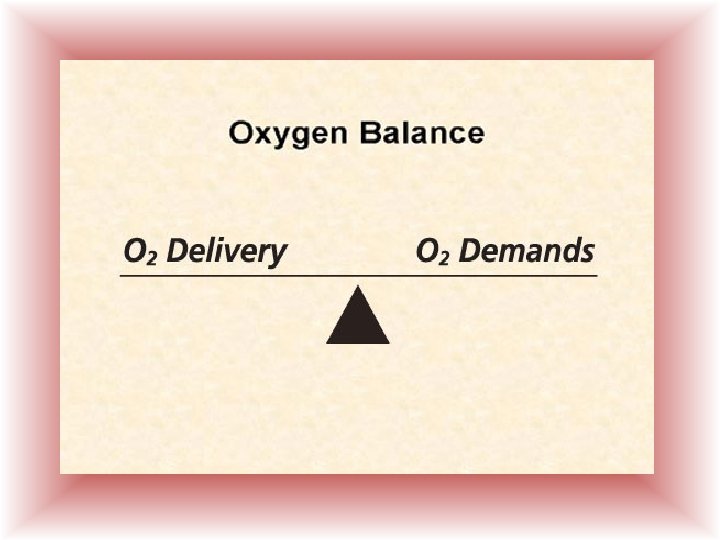
O 2 To O 2 BODY O 2 O 2 dy From Bo
O 2 O 2
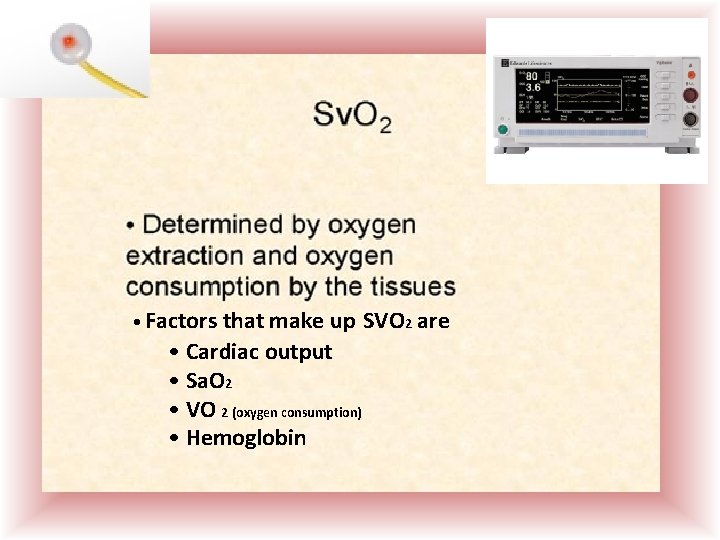
• Factors that make up • Cardiac output • Sa. O 2 • VO 2 (oxygen consumption) • Hemoglobin SVO 2 are
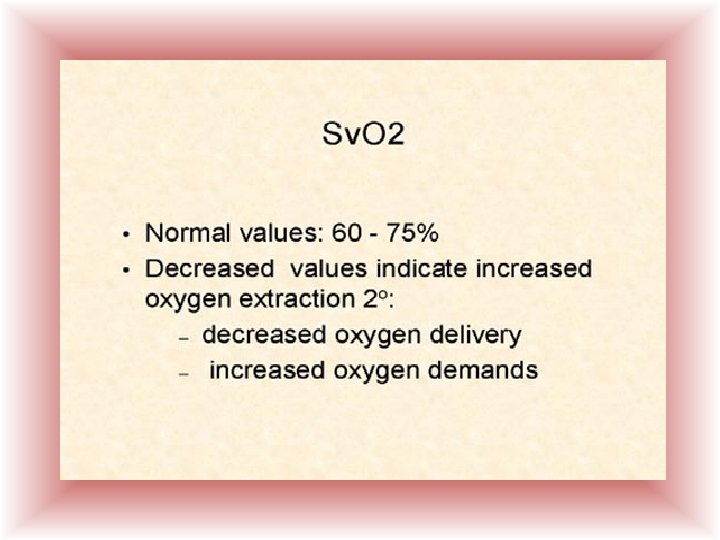
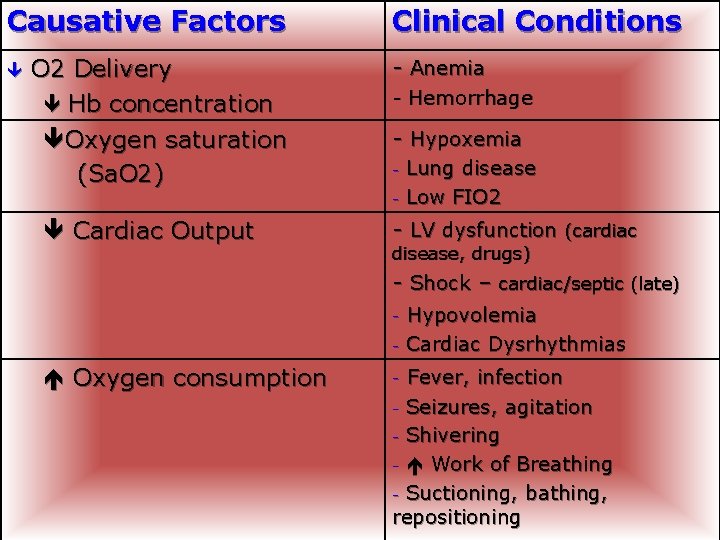
Causative Factors O 2 Delivery Hb concentration Oxygen saturation (Sa. O 2) Clinical Conditions - Anemia - Hemorrhage - Hypoxemia - Cardiac Output Lung disease Low FIO 2 - LV dysfunction (cardiac disease, drugs) - Shock – cardiac/septic (late) - Oxygen consumption Hypovolemia Cardiac Dysrhythmias Fever, infection - Seizures, agitation - Shivering - Work of Breathing - Suctioning, bathing, repositioning -
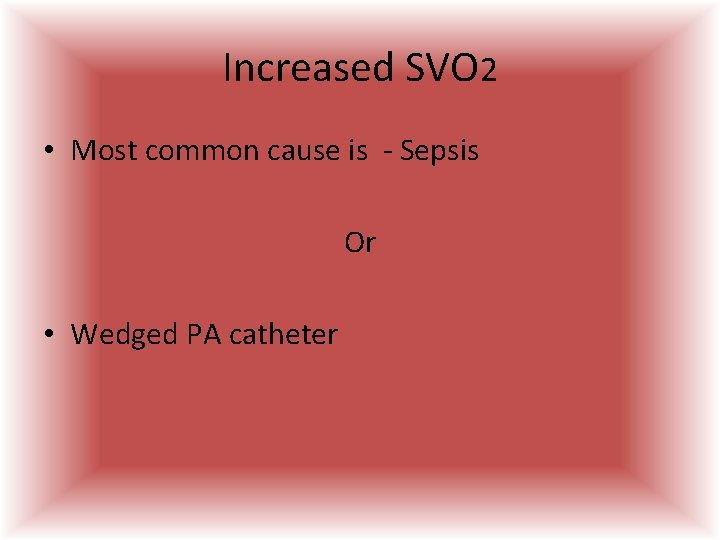
Increased SVO 2 • Most common cause is - Sepsis Or • Wedged PA catheter
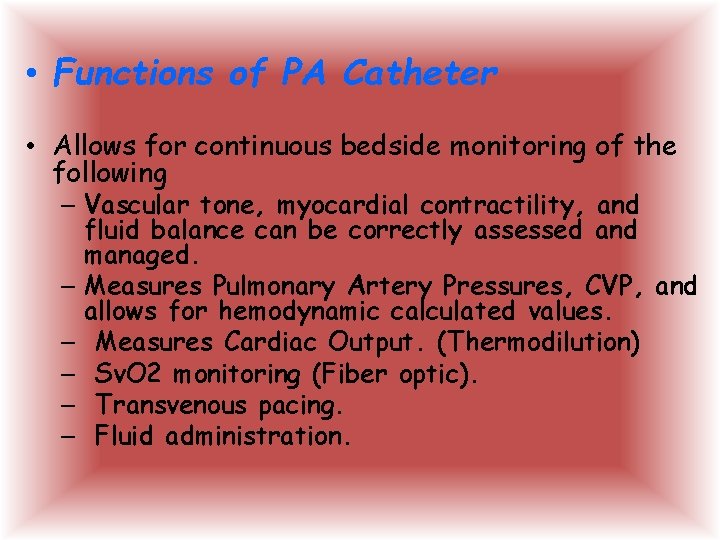
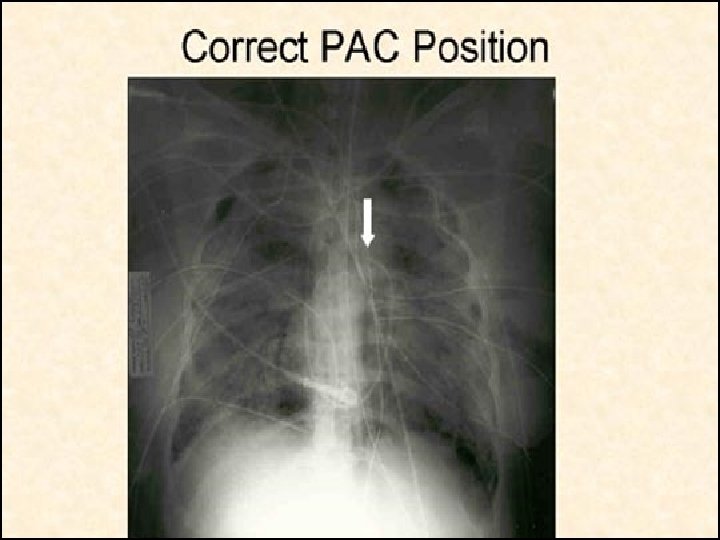
• Functions of PA Catheter • Allows for continuous bedside monitoring of the following – Vascular tone, myocardial contractility, and fluid balance can be correctly assessed and managed. – Measures Pulmonary Artery Pressures, CVP, and allows for hemodynamic calculated values. – Measures Cardiac Output. (Thermodilution) – Sv. O 2 monitoring (Fiber optic). – Transvenous pacing. – Fluid administration.
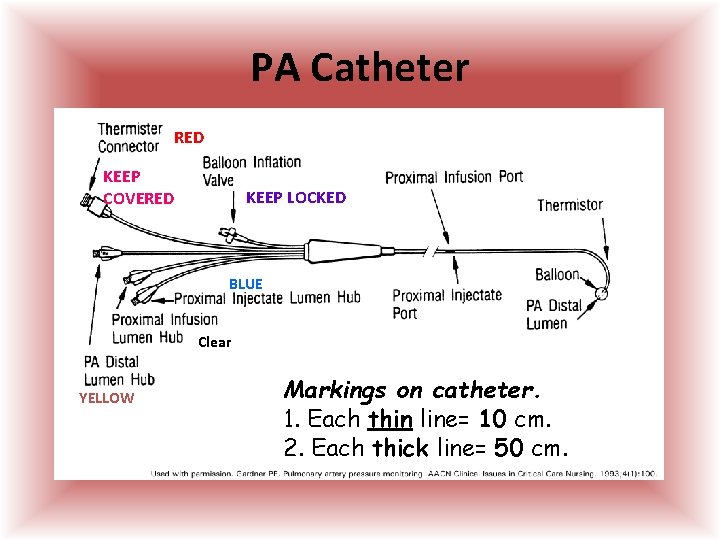
PA Catheter RED KEEP COVERED KEEP LOCKED BLUE Clear YELLOW Markings on catheter. 1. Each thin line= 10 cm. 2. Each thick line= 50 cm.
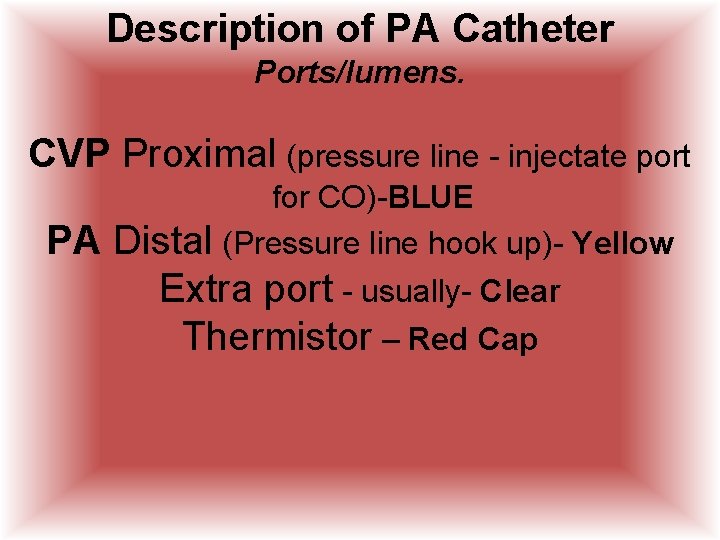
Description of PA Catheter Ports/lumens. CVP Proximal (pressure line - injectate port PA for CO)-BLUE Distal (Pressure line hook up)- Yellow Extra port - usually- Clear Thermistor – Red Cap
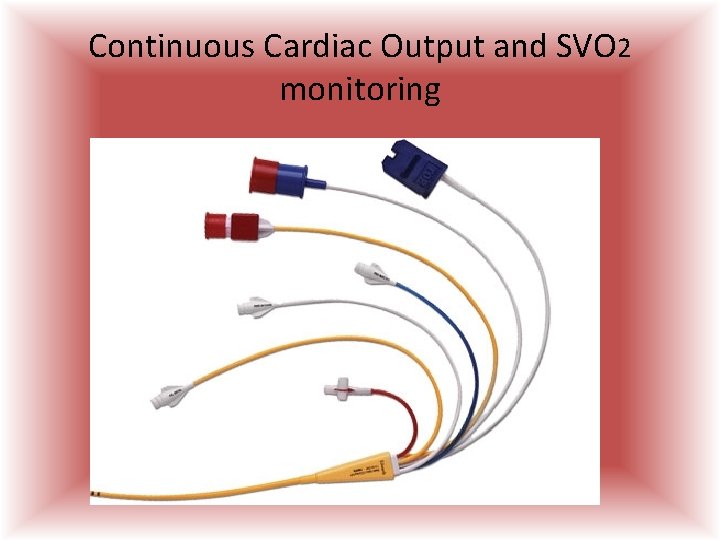
Continuous Cardiac Output and SVO 2 monitoring
Indications for PA catheter • The pulmonary artery catheter is indicated in patients whose cardiopulmonary pressures, flows, and circulating volume require precise, intensive management. • MI – cardiogenic shock - CHF • Shock - all types • Valvular dysfunction • Preoperative, Intraoperative, and Postoperative Monitoring • ARDS, Burns, Trauma, Renal Failure
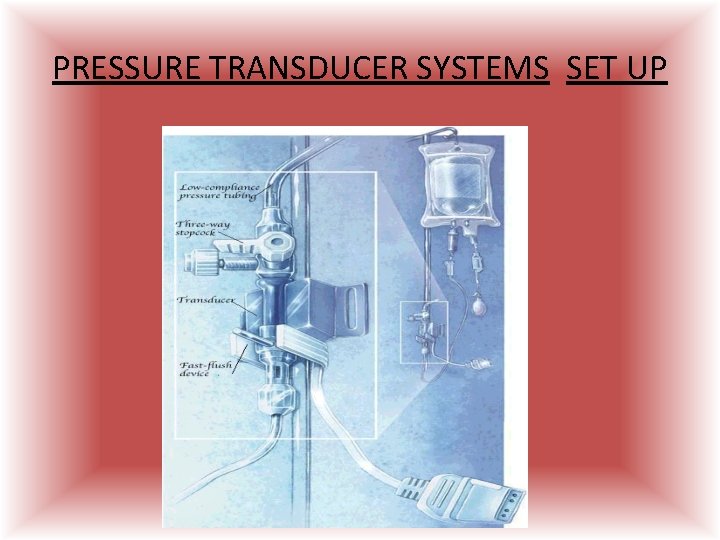
PRESSURE TRANSDUCER SYSTEMS SET UP
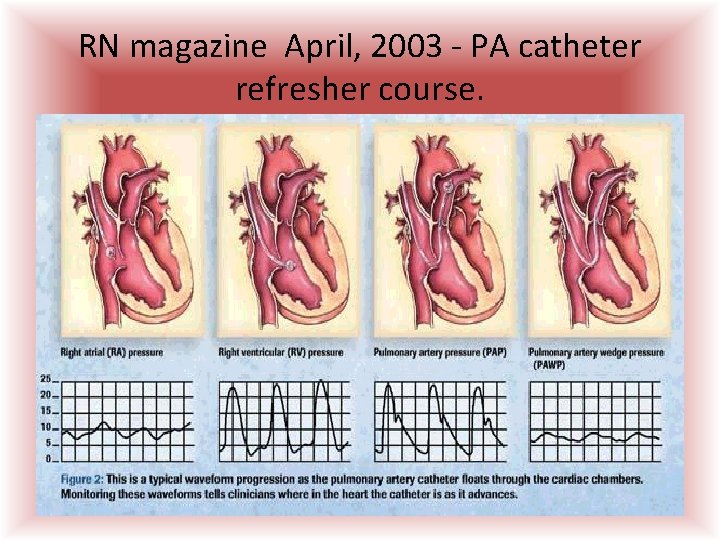
RN magazine April, 2003 - PA catheter refresher course.
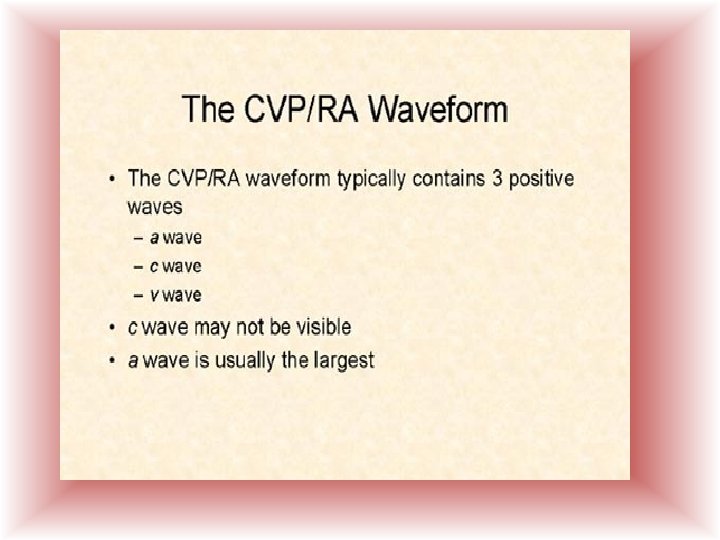
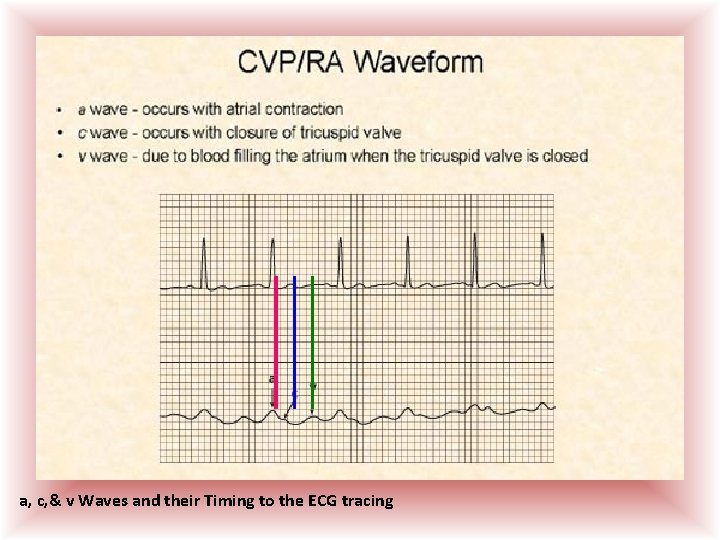
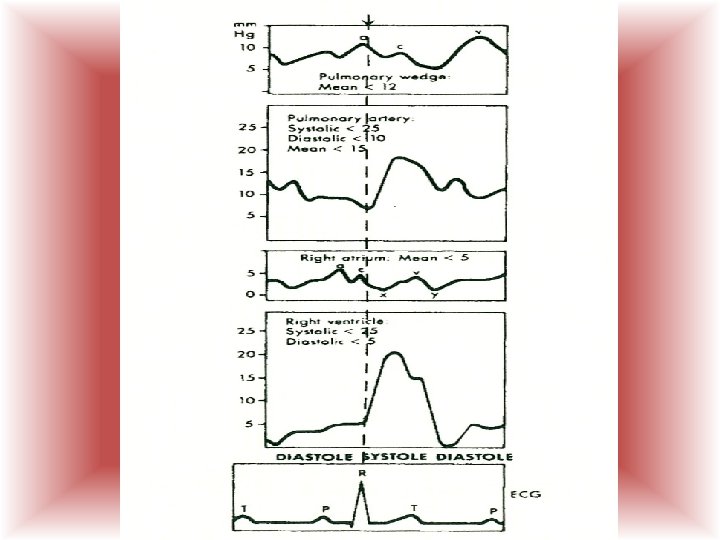
a, c, & v Waves and their Timing to the ECG tracing
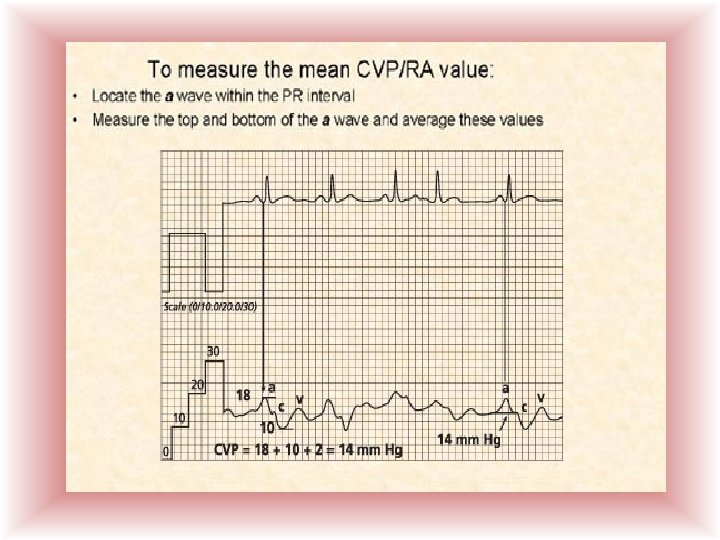
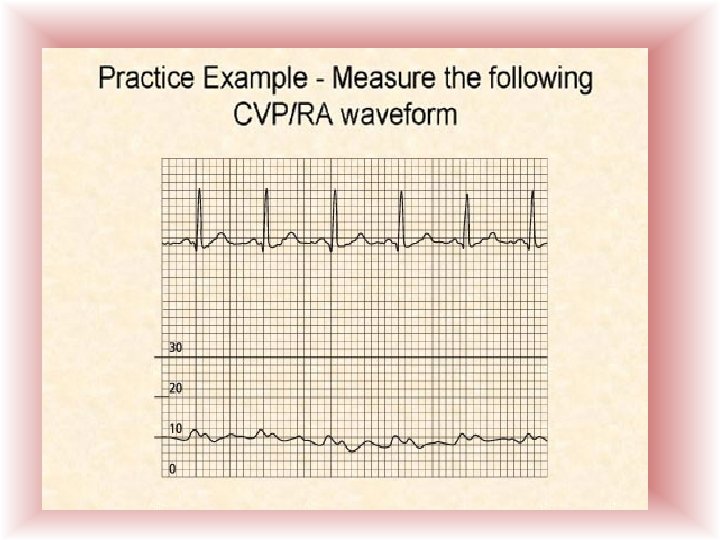
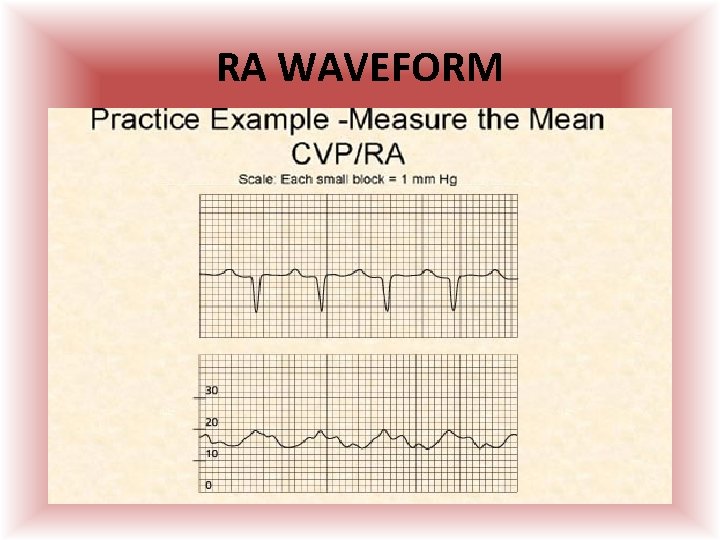
RA WAVEFORM
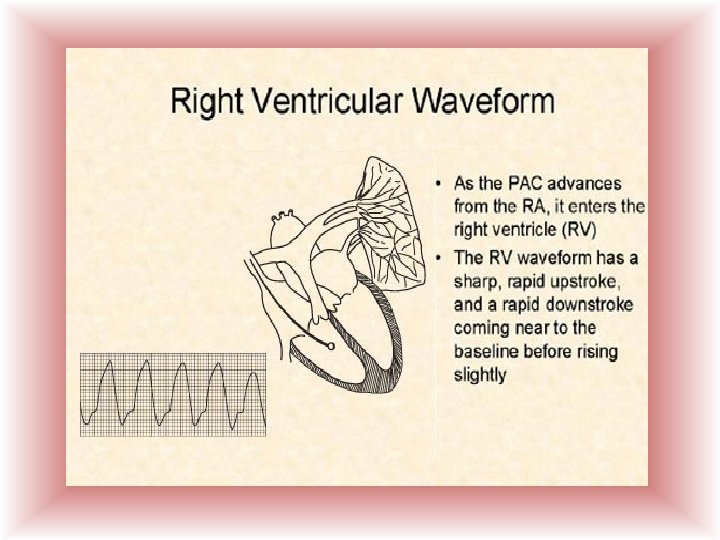
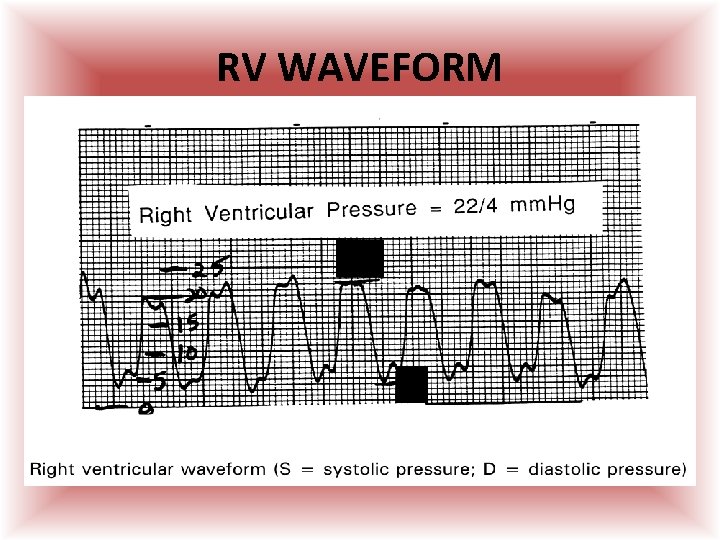
RV WAVEFORM 22 4
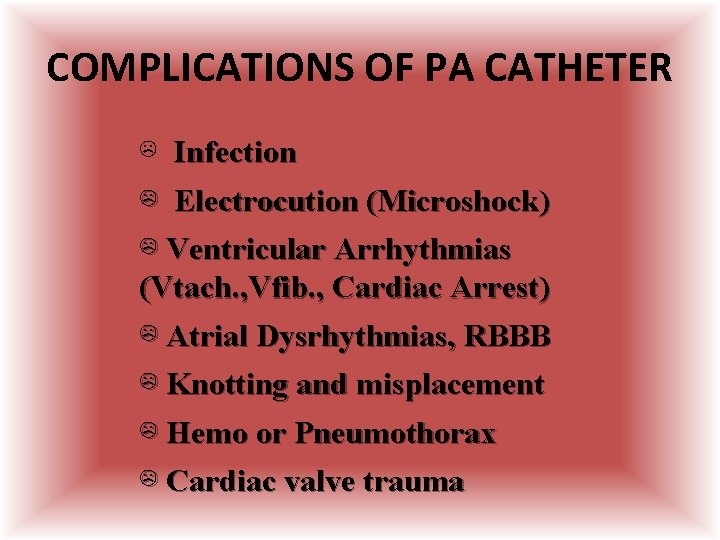
COMPLICATIONS OF PA CATHETER ☹ Infection ☹ Electrocution (Microshock) ☹ Ventricular Arrhythmias (Vtach. , Vfib. , Cardiac Arrest) ☹ Atrial Dysrhythmias, RBBB ☹ Knotting and misplacement ☹ Hemo or Pneumothorax ☹ Cardiac valve trauma
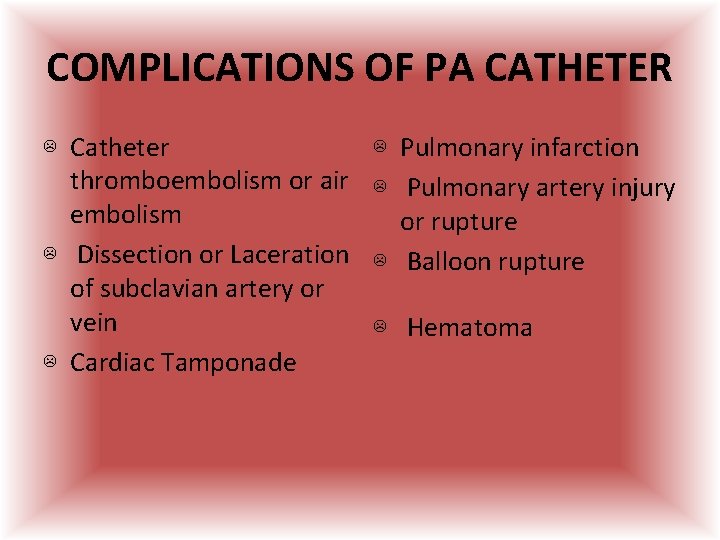
COMPLICATIONS OF PA CATHETER ☹ Catheter thromboembolism or air embolism ☹ Dissection or Laceration of subclavian artery or vein ☹ Cardiac Tamponade ☹ Pulmonary infarction ☹ Pulmonary artery injury or rupture ☹ Balloon rupture ☹ Hematoma
Arterial line • Indicated in patient’s with – Hypotension – Pressors – Need for recurrent/frequent abg’s – LHC
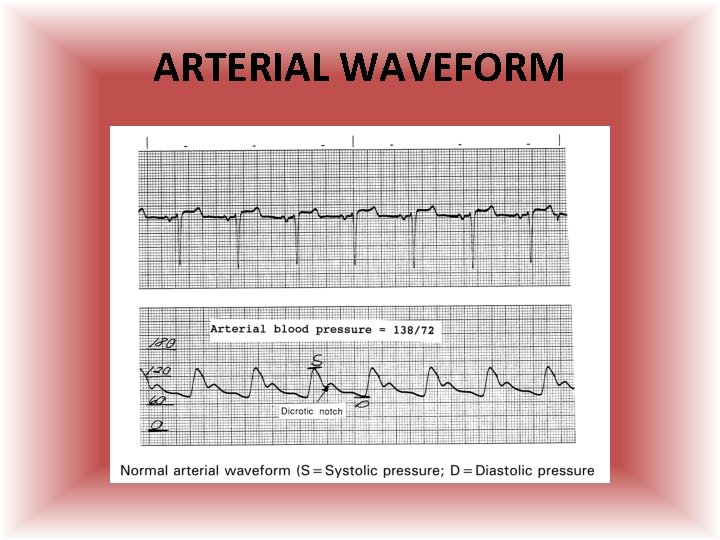
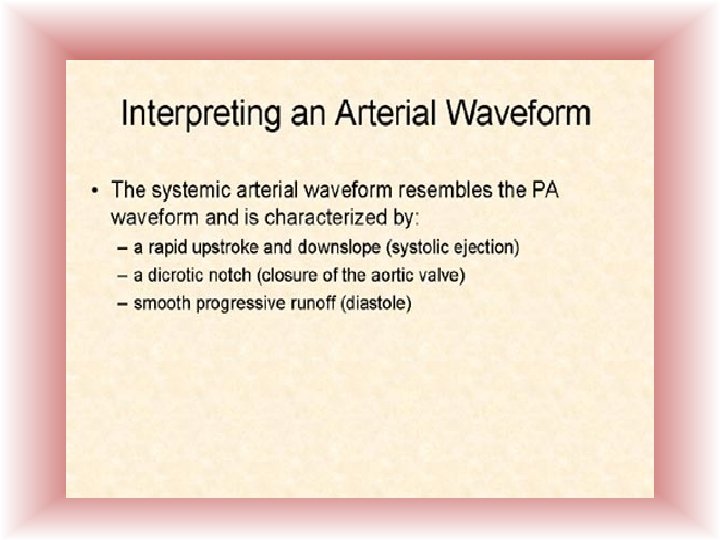
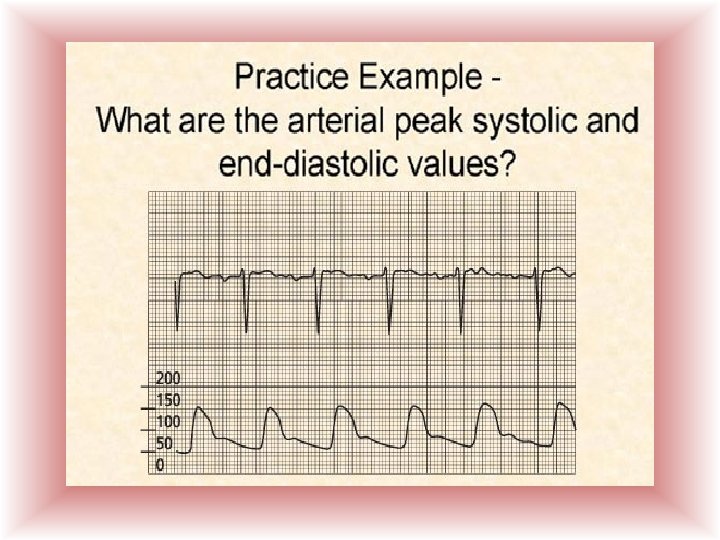
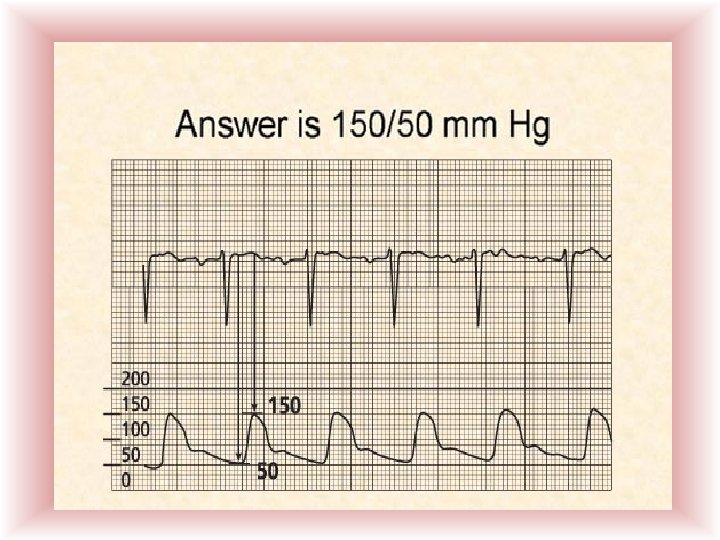
ARTERIAL WAVEFORM
Strategies to manipulate cardiac output
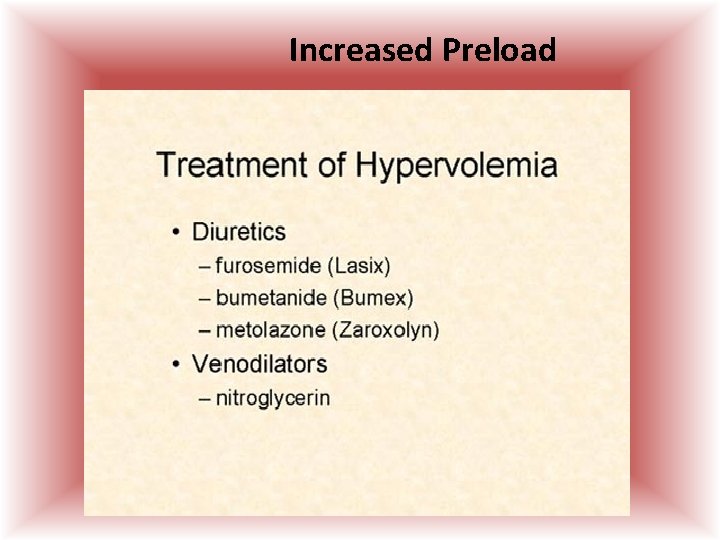
Increased Preload
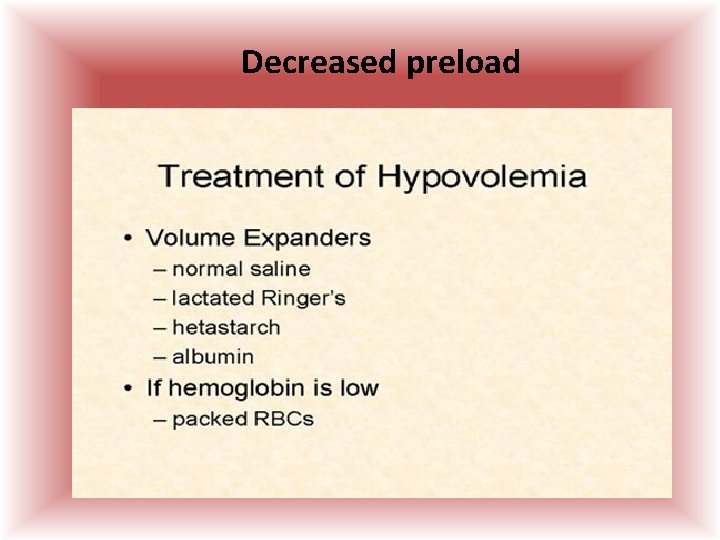
Decreased preload
Hemodynamic terms • Contractility– Increased • Positive inotropic drugs – Dobutamine, Digoxin, Epinephrine
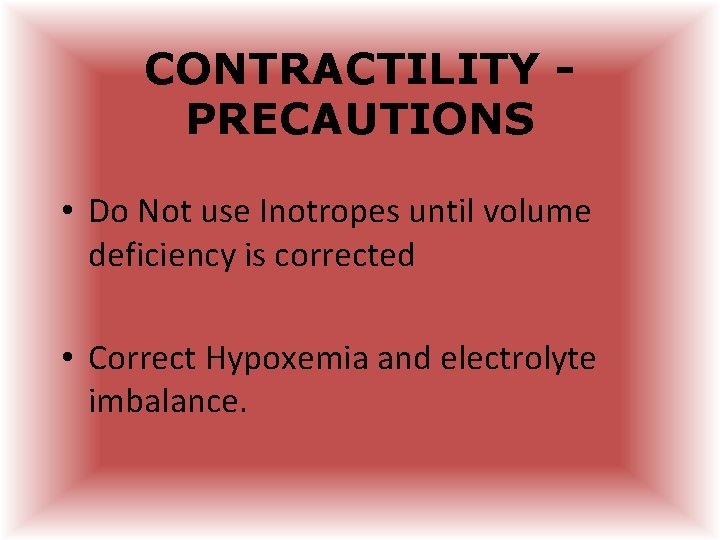
CONTRACTILITY PRECAUTIONS • Do Not use Inotropes until volume deficiency is corrected • Correct Hypoxemia and electrolyte imbalance.
Hemodynamic terms • Afterload – resistance the blood in the ventricle must overcome to force the valves open and eject contents to circulation.
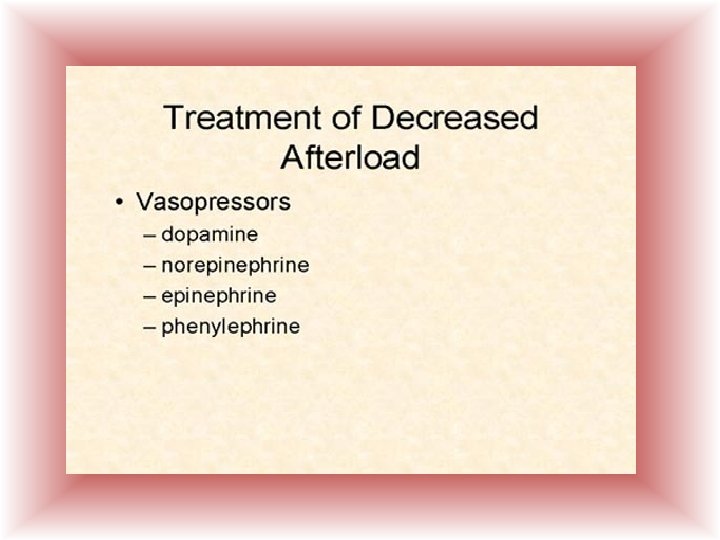
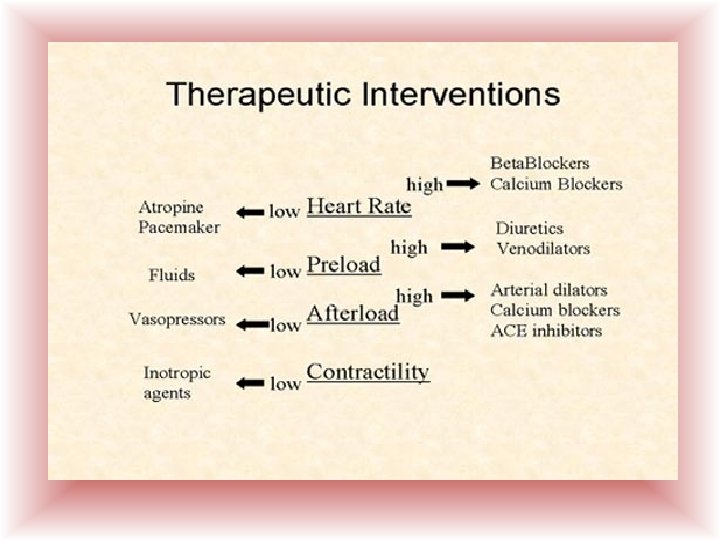
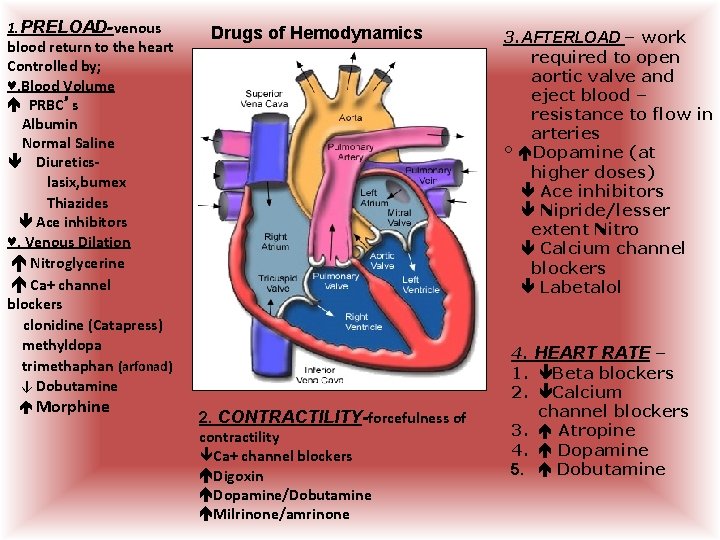
1. PRELOAD-venous blood return to the heart Controlled by; ♥. Blood Volume PRBC’s Albumin Normal Saline Diureticslasix, bumex Thiazides Ace inhibitors ♥. Venous Dilation Nitroglycerine Ca+ channel blockers clonidine (Catapress) methyldopa trimethaphan (arfonad) ↓ Dobutamine Morphine Drugs of Hemodynamics 2. CONTRACTILITY-forcefulness of contractility Ca+ channel blockers Digoxin Dopamine/Dobutamine Milrinone/amrinone 3. AFTERLOAD – work required to open aortic valve and eject blood – resistance to flow in arteries ° Dopamine (at higher doses) Ace inhibitors Nipride/lesser extent Nitro Calcium channel blockers Labetalol 4. HEART RATE – 1. Beta blockers 2. Calcium channel blockers 3. Atropine 4. Dopamine 5. Dobutamine
References • Pulmonary Artery Catheter Education Project @ www. pacep. org sponsored by – American Association of Critical Care Nurses American Association of Nurse Anesthetists American College of Chest Physicians American Society of Anesthesiologists American Thoracic Society National Heart Lung Blood Institute Society of Cardiovascular Anesthesiologists Society of Critical Care Medicine • Hemodynamics Made Incredibly Visual – LWW publishing 2007 • AACN practice alert – Pulmonary Artery Pressure Monitoring - Issued 5/2004 • Handbook of Hemodynamic Monitoring – G Darovic 2 nd ed. • TCHP Education Consortium 2005 – A Primer for Cardiovascular Surgery and Hemodynamic Monitoring • Uptodate. com
- Slides: 93