Basics of Healthcare Financing and Reimbursement PTH 511
Basics of Healthcare Financing and Reimbursement PTH 511 LAMP I
Assigned Reading � Kettenbach, Chapter 4
Reimbursement � Three Essentials � Documentation � Therapy services must be skilled, reasonable, and neccessary � Charge Capture � Coding
�History of Healthcare financing
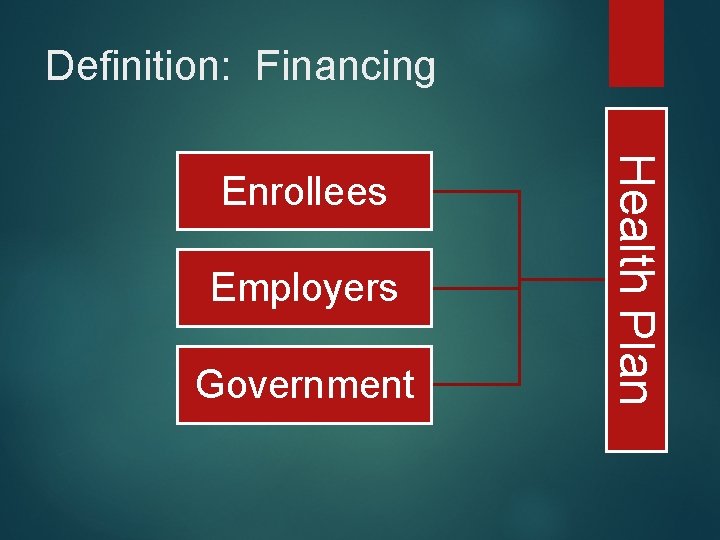
Definition: Financing Employers Government Health Plan Enrollees
Health Care Financing � Out of pocket or Fee For Service (FFS) � Government: Medicare or Medicaid (CMS) � Individual private insurance � Deductible � Copayment � coinsurance � Indemnity clause � Uncovered services
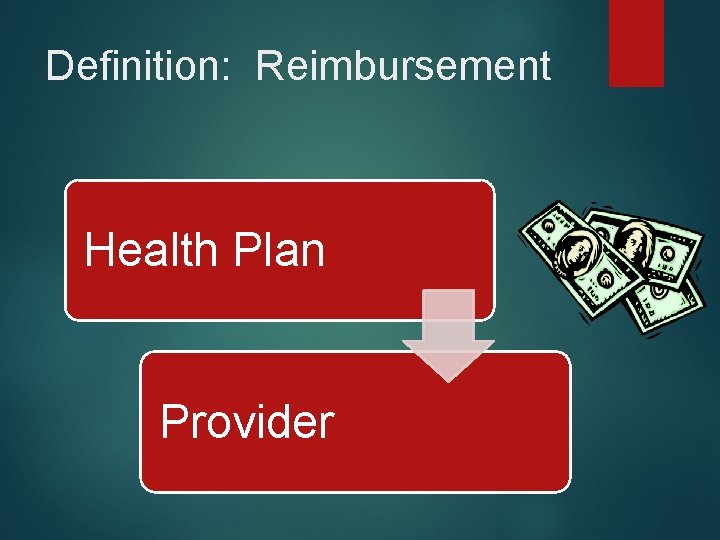
Definition: Reimbursement Health Plan Provider
Definition: Third Party Payment System � 1 st Patient/client (beneficiary) � 2 nd Provider � 3 rd insurance provider
Definitions � Subscriber: Individual who purchases policy from insurance provider � Premium: Cost of insurance � Claims: Submission by Provider (2 nd Party) to Insurance Provider (3 rd Party) for payment for health care services rendered � Denials � Appeals
Medicare � Federally funded � Qualification Criteria: � Over 65 years old AND � Paid in to Social Security through an employer for at least 10 years � Under 65 years old AND � Considered medically disabled OR � Have end-stage renal disease
Medicare � Part A � � � Includes inpatient (acute) care, hospice, and some health care Part B � Physician services � Outpatient care, including PT & OT Part D � Provides prescription drug coverage
Medicare Part A � Entitled � Part A is funded by social security taxes from employers/employees (Federal Insurance Contributions Act or FICA) � Hospital, Skilled Nursing Facilities (SNF), Hospice, Home Health Care (HH), Inpatient Rehabilitation (IRF) � Paid under Prospective Payment System � Method of Payment (vs. Reimbursement) � Service Period=Episode � Medicare-Severity Diagnostic Related Groups (MS-DRGs)
Medicare Part A � Benefit Period � Admission � Skilled until 60 days after discharge Nursing Facility: � Care must me skilled � Three night/4 day hospital stay before admission, must document neccessity � Home Health Care � Skilled � Homebound � Agency must be Medicare provider � Hospice � Physician provider certified, patient chooses, Medicare
Medicare Part A: Inpatient Hospital � Medicare-Severity Diagnostic Related Groups (MSDRGs) � Rehabilitation services are not billed separately � Hospital acquired conditions (HACs) paid for by hospital
Medicare Part A: SNF � RUGS* (changes in payment system) � Assessment tool: MDS 3. 0 � 66 categories/14 rehab categories � 4 day/3 night hospital admission � Physician certification for skilled need and/or orders for therapy � Patient needs daily skilled services � Nursing 7 d/week and/or � Therapy at least 5 d/week
Medicare A: Inpatient Rehab Facility � Assessment tool = Patient assessment instrument (PAI) � Uses Functional Independence Measure � Outcome Measure which tracks progress � Payment covers entire stay � 25% reduction in payment if discharged to SNF vs outpatient or HHC
Medicare A: Home Health Services � Assessment tool = OASIS � Payment dependent upon # of visits* � Payment based on 60 day episodes � Functional reassessments must be completed by therapy regularly
Medicare Part B � Voluntary– Person doesn’t need to sign up � Provides payment for outpatient, physician services, and some durable medical equipment (DME) � Paid through federal taxes and monthly premiums � Paid through a fee schedule � Resource-Based Relative Value Scale (RBRVS) 1. Work Involved (Knowledge needed to perform) 2. Practice Expense (How much does the service cost? 3. Malpractice associated with the procedure (Risk) � Includes a geographic adjustment
Variations to Medicare Part B � Outpatient Services provided in inpatient settings: � Hospital based outpatient department � Rehab agency with outpatient department � SNF services to people who come in from community � HHC services to people who are no longer “homebound” but want therapy in the home
Changing demographics � Boom in aging population � Increase in life expectancy � Trend toward independent living � More people eligible for services � Affordable Care Act
Medicaid � Funded federally AND by each state � Offers medical assistance to those with low incomes � Qualification guidelines vary by state � Exact coverage varies, but some services included are: � Inpatient, hospital care � Outpatient care � Screenings for children � Some PT & OT
Medicaid: Children’s Health Insurance Program � CHIP � Joint funding by federal government and individual states � Provide the standard Medicaid benefit package, including Early and Periodic Screening, Diagnostic, and Treatment (EPSDT) services, which includes all medically necessary services like mental health and dental services. � Serves uninsured children who do not qualify for Medicaid (up to 200% above the poverty level).
Reimbursement � Retrospective (pre-1980 s) � Prospective (PPS) � 4 Basic Reimbursement Methods � FFS (fee schedule based on usual, customary, reasonable UCR) � Per visit � Case or Episode � (ex. DRG) SSA 1983 � Capitation (PMPM) � Greatest risk? ? � Bundling
Payment by Commercial Insurance � Negotiated Rate � � � Per Case � Cases identified by diagnostic coding (ICD-10) � Payment is based on ICD-10 diagnosis code Per Diem � � Usual, Customary, Reasonable Reimbursement occurs at a cost per day Per Visit � Common in rehabilitation � Insurer will pay for X number of visits
Managed Care � Predetermined Payment schedule (discounted fee schedule) � Provider network (providers who contract with insurance company and agree to schedule)
Managed Care Types � � Health Maintenance Organization (HMO) � Staff model (providers are employed by HMO that operates facilities where services provided i. e. Kaiser-Permanente) � Independent practice association (IPA) model (Dr. or groups form to contract services) Preferred Provider Organization (PPO) � � Open managed care model. Health insurer or employer negotiates discounted fees with networks of providers in exchange for guaranteeing volume (indemnity clause) Point-of-Service (POS) � In-network and out-of-network benefits � Greatest coverage with in-network benefits
Healthcare Common Procedure Coding System � � Level 1 CPT � Most common � >8000 codes � Comprised of 5 numbers Level 2 HCPCS � Supplies/procedures/DME � One alphabetical character (A-V) and 4 numbers
Therapy Cap � 2014 � $1, 920 for PT/SLP and $1920 for OT � Not applied to hospital OP depts � Exceptions process (KX modifier)
How to Manage under Managed Care? � Increase volume of patients � Reduce costs – increase efficiency � Negotiate contracts � Create “payer mix” that meets needs � Be proactive � Create new levels of care � Evidence needed!
Reimbursement Issues � Growth in CPT codes � Medicare Physician Fee Schedule � Proposed rule changes 2012 � Multiple procedure payment reduction � Projected reduction of 29. 5% � Differentiation of practice settings � Reduction in payment for multiple codes � Review group therapy
Test Your Skills � Worksheet review
Protect Thy Patients and Thyself Kornblau, B. , and Starling, S. Ethics in � P – Put a copy of licensure law on desk 2000, Slack: Rehabilitation: A Clinical Perspective. � R – Report Thorofare, NJ. ethical violations � O – open your eyes � T – Tell them you want it in writing � E – encourage ethical behavior � C – Cover yourself with documentation � T - Think
�T – Take the patient’s interest above all � H – handle situations as they arise � Y – Yearn to learn �P – Plug into professional assoc. � A – Ask a lot of questions � T – Train and supervise properly � I – Invest in newspaper subscription � E – Establish relationship with mentor � N – never fall behind � T – take a good look at professional lit. � S – surf internet for changes in regulations
�T – Take time to read code and standards � H – hand over patients to those with more expertise � Y – Yield to dictates of insurance regs. �S – Save copy of all written correspondence � E – Explore all alternatives � L – Look at professional assoc. home pgs. � F – Fill out all forms accurately and truthfully
- Slides: 34