BASICS OF CARDIAC HEMODYNAMICS By Dr Sidhartha Das
BASICS OF CARDIAC HEMODYNAMICS By: Dr. Sidhartha Das
Definition of HEMODYNAMICS Ø Hemodynamics are the forces which circulate blood through the body. Ø Specifically, hemodynamics is the term used to describe the intravascular pressure and flow that occurs when the heart muscle contracts and pumps blood throughout the body. Hemodynamic monitoring refers to measurement of pressure, flow and oxygenation of blood within the cardiovascular system.
Hemodynamic Principles � Pressure measurements � Right & Left Heart catheterisation � Cardiac output & Stroke volume measurement � Vascular Resistance � Shunt detection & calculation
What is a Pressure Wave? A pressure wave is the cyclical force generated by cardiac muscle contraction. Its amplitude & duration are influenced by various mechanical and physiological parameters. The pressure waveform of a cardiac chamber is influenced by the following factors: Ø Force of the contracting chambers Ø Its surrounding structures Ø Contiguous chambers of the heart Ø The pericardium Ø The lungs Ø The vasculature Ø Heart Rate Ø The respiratory cycle
Pressure Measurement Devices For the assessment of intracardiac pressures, 2 systems are curently in use: Ø Fluid-filled catheter manometer – the pressure wave being transmitted to the pressure transducer by the fluid column within the catheter. Ø Micromanometer (catheter-tip pressure manometer) – which have miniatured pressure transducer mounted at the catheter tip.
What is Wedge Pressure? Wedge pressure is the pressure obtained when an end-hole catheter is positioned in a designated blood vessel with its open end-hole facing a capillary bed, with no connecting vessels conducting flow into or away from the designated vessel between the catheter tip and the capillary bed. Ø A True wedge pressure can be measured only in the absence of flow, allowing pressure to equilibrate across the capillary bed so that the catheter tip pressr = pressr on the other side of the capillary bed. Ø Thus, an end-hole catheter wedged in a hepatic v. measures portal ven pressr ; a catheter wedged in distal pulm artery measures pulm ven pressr ; and that in a pulm v. measures pulm artery pressr.
The Pulmonary Artery catheter The Principle: The PA catheter (also known as the Swan- Ganz catheter) is equipped with an inflatable balloon that acts like a rubber raft and allows the flow of venous blood to carry the catheter tip through the right side of the heart and out into the pulmonary circulation. This balloon floatation method makes it possible to perform a right heart catheterization at the bedside without fluoroscopic guidance.
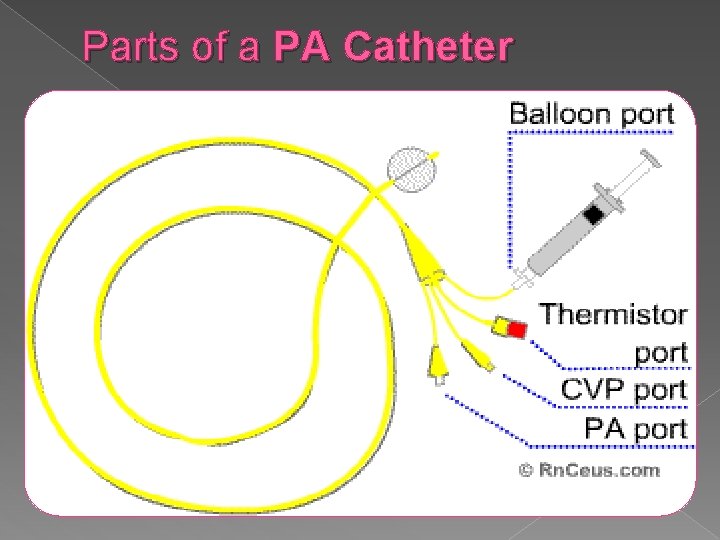
Parts of a PA Catheter
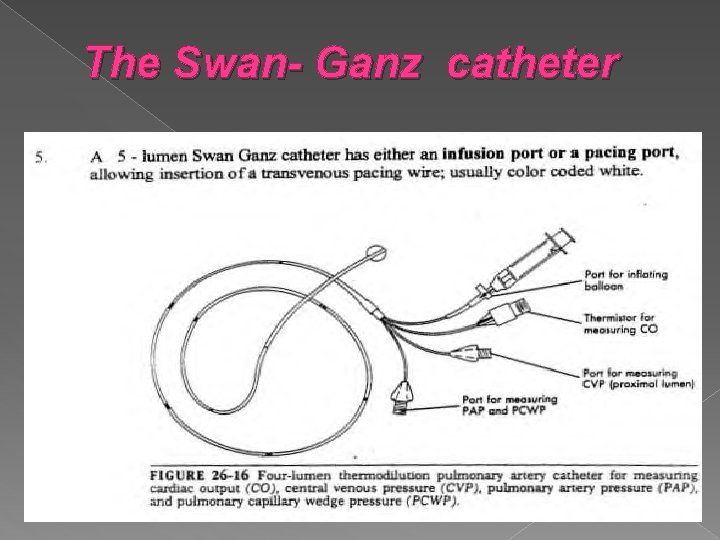
The Swan- Ganz catheter
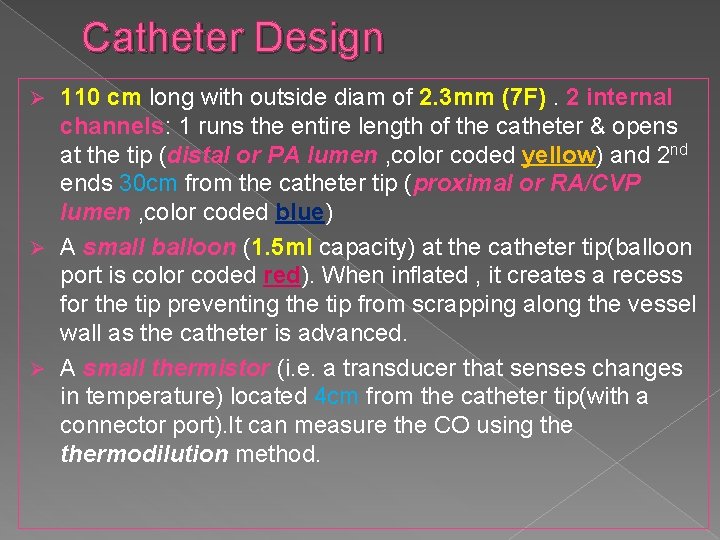
Catheter Design 110 cm long with outside diam of 2. 3 mm (7 F). 2 internal channels: 1 runs the entire length of the catheter & opens at the tip (distal or PA lumen , color coded yellow) and 2 nd ends 30 cm from the catheter tip (proximal or RA/CVP lumen , color coded blue) Ø A small balloon (1. 5 ml capacity) at the catheter tip(balloon port is color coded red). When inflated , it creates a recess for the tip preventing the tip from scrapping along the vessel wall as the catheter is advanced. Ø A small thermistor (i. e. a transducer that senses changes in temperature) located 4 cm from the catheter tip(with a connector port). It can measure the CO using thermodilution method. Ø
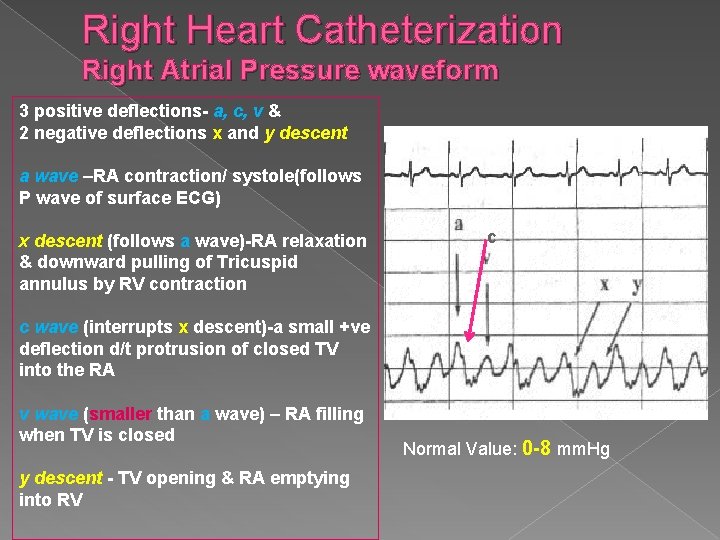
Right Heart Catheterization Right Atrial Pressure waveform 3 positive deflections- a, c, v & 2 negative deflections x and y descent a wave –RA contraction/ systole(follows P wave of surface ECG) x descent (follows a wave)-RA relaxation & downward pulling of Tricuspid annulus by RV contraction c c wave (interrupts x descent)-a small +ve deflection d/t protrusion of closed TV into the RA v wave (smaller than a wave) – RA filling when TV is closed y descent - TV opening & RA emptying into RV Normal Value: 0 -8 mm. Hg
Central Venous Pressure The proximal part of the PA catheter measures the pressure in the SVC , which is equivalent to the pressure in the RA. This pressure is commonly known as the Central venous pressure (CVP). In the absence of a TV abnormality the CVP or the Rt Atrial Pressr (RAP) is equivalent to the Rt Vent End-Diastolic pressr (RVEDP) i. e. CVP = RAP = RVEDP So CVP can be used as a measure of Rt vent filling
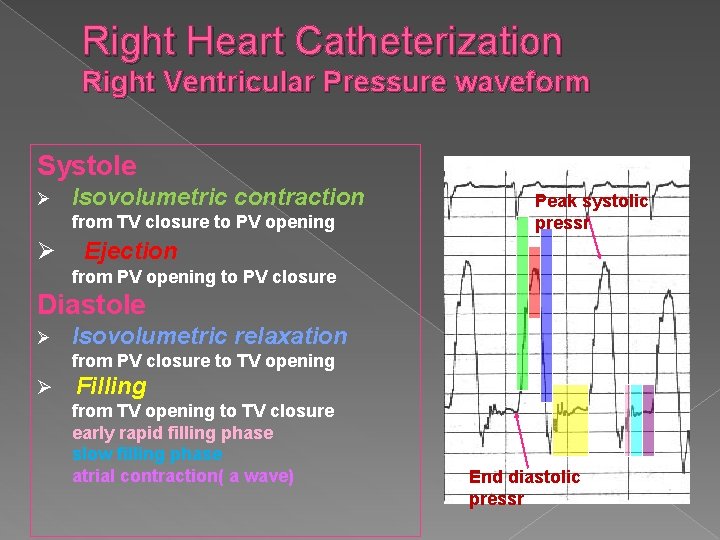
Right Heart Catheterization Right Ventricular Pressure waveform Systole Ø Isovolumetric contraction from TV closure to PV opening Ø Peak systolic pressr Ejection from PV opening to PV closure Diastole Ø Isovolumetric relaxation from PV closure to TV opening Ø Filling from TV opening to TV closure early rapid filling phase slow filling phase atrial contraction( a wave) End diastolic pressr
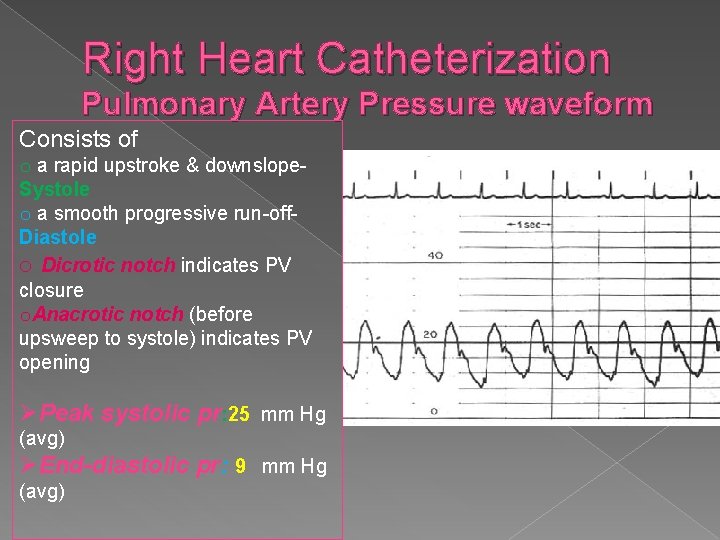
Right Heart Catheterization Pulmonary Artery Pressure waveform Consists of o a rapid upstroke & downslope. Systole o a smooth progressive run-off. Diastole o Dicrotic notch indicates PV closure o. Anacrotic notch (before upsweep to systole) indicates PV opening ØPeak systolic pr: 25 mm Hg (avg) ØEnd-diastolic pr: 9 mm Hg (avg)
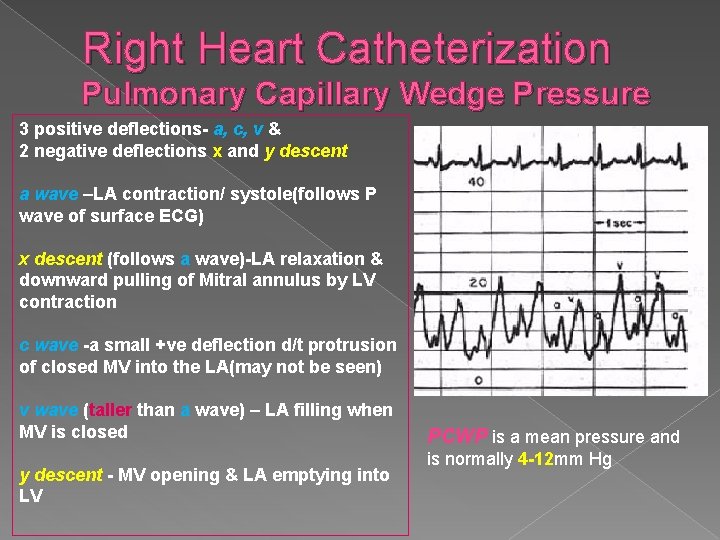
Right Heart Catheterization Pulmonary Capillary Wedge Pressure 3 positive deflections- a, c, v & 2 negative deflections x and y descent a wave –LA contraction/ systole(follows P wave of surface ECG) x descent (follows a wave)-LA relaxation & downward pulling of Mitral annulus by LV contraction c wave -a small +ve deflection d/t protrusion of closed MV into the LA(may not be seen) v wave (taller than a wave) – LA filling when MV is closed y descent - MV opening & LA emptying into LV PCWP is a mean pressure and is normally 4 -12 mm Hg
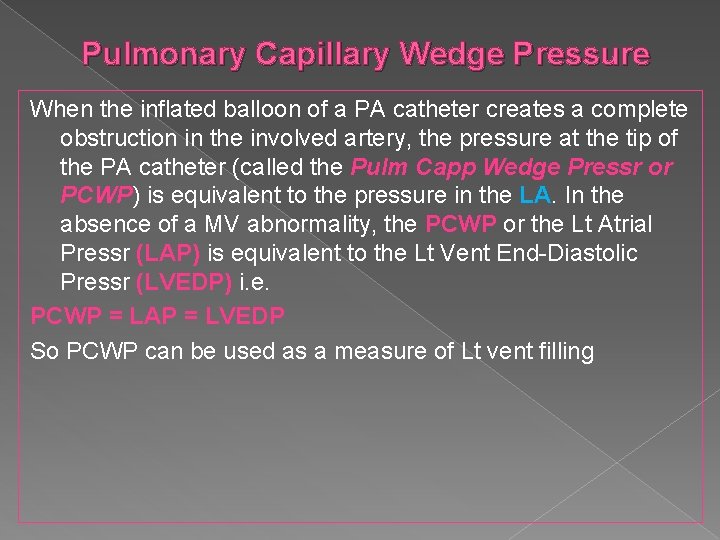
Pulmonary Capillary Wedge Pressure When the inflated balloon of a PA catheter creates a complete obstruction in the involved artery, the pressure at the tip of the PA catheter (called the Pulm Capp Wedge Pressr or PCWP) is equivalent to the pressure in the LA. In the absence of a MV abnormality, the PCWP or the Lt Atrial Pressr (LAP) is equivalent to the Lt Vent End-Diastolic Pressr (LVEDP) i. e. PCWP = LAP = LVEDP So PCWP can be used as a measure of Lt vent filling
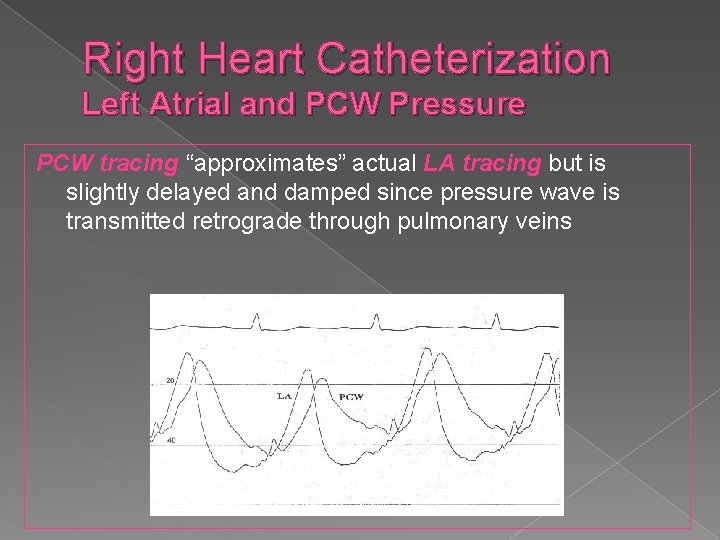
Right Heart Catheterization Left Atrial and PCW Pressure PCW tracing “approximates” actual LA tracing but is slightly delayed and damped since pressure wave is transmitted retrograde through pulmonary veins
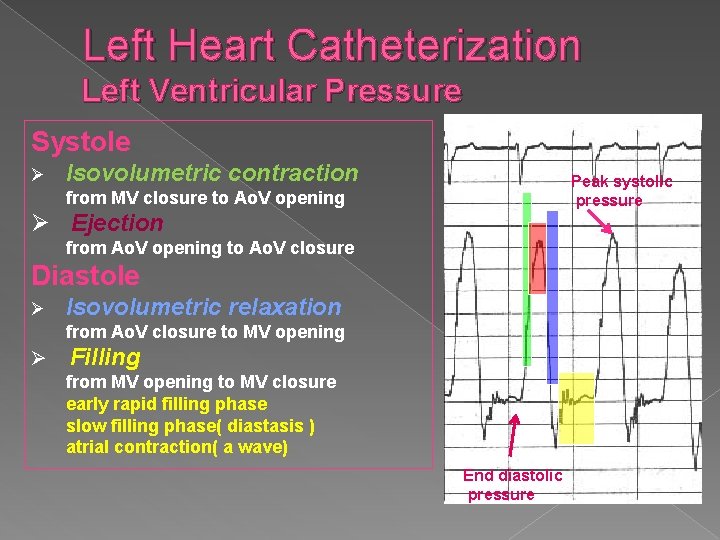
Left Heart Catheterization Left Ventricular Pressure Systole Ø Isovolumetric contraction Peak systolic pressure from MV closure to Ao. V opening Ø Ejection from Ao. V opening to Ao. V closure Diastole Ø Isovolumetric relaxation from Ao. V closure to MV opening Ø Filling from MV opening to MV closure early rapid filling phase slow filling phase( diastasis ) atrial contraction( a wave) End diastolic pressure
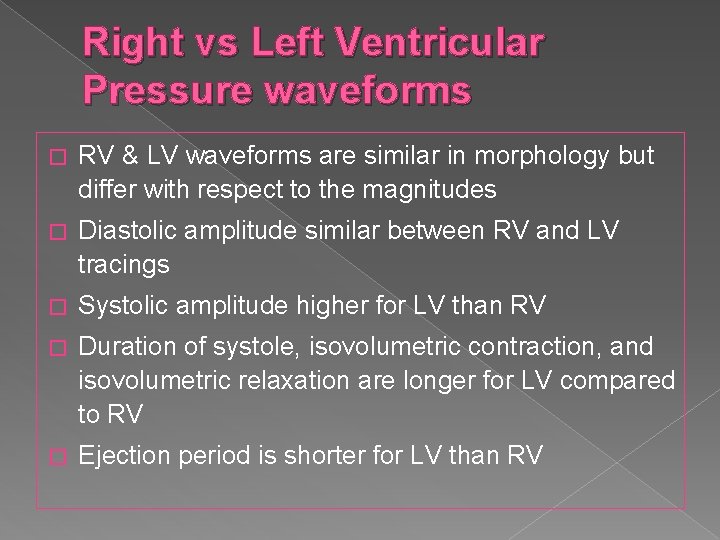
Right vs Left Ventricular Pressure waveforms � RV & LV waveforms are similar in morphology but differ with respect to the magnitudes � Diastolic amplitude similar between RV and LV tracings � Systolic amplitude higher for LV than RV � Duration of systole, isovolumetric contraction, and isovolumetric relaxation are longer for LV compared to RV � Ejection period is shorter for LV than RV
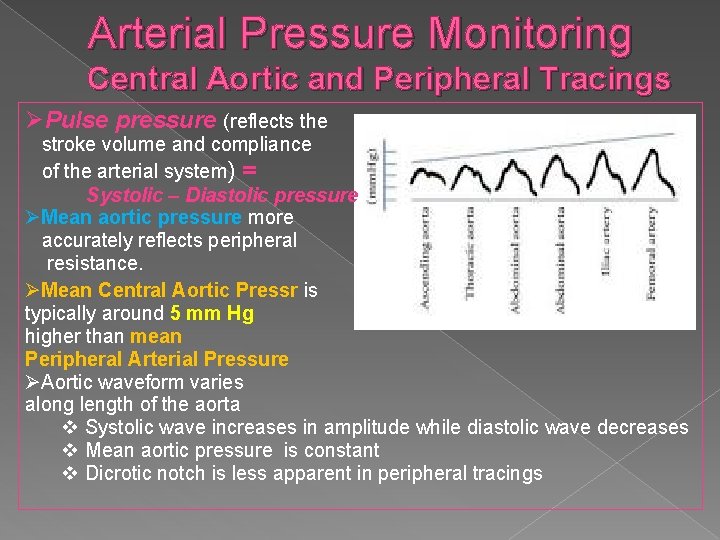
Arterial Pressure Monitoring Central Aortic and Peripheral Tracings ØPulse pressure (reflects the stroke volume and compliance of the arterial system) = Systolic – Diastolic pressure ØMean aortic pressure more accurately reflects peripheral resistance. ØMean Central Aortic Pressr is typically around 5 mm Hg higher than mean Peripheral Arterial Pressure ØAortic waveform varies along length of the aorta v Systolic wave increases in amplitude while diastolic wave decreases v Mean aortic pressure is constant v Dicrotic notch is less apparent in peripheral tracings
What is Cardiac Index ? Cardiac output is affected by several factors including age, body size, and metabolic demands. To normalize resting C. O among different body sizes, the Cardiac Index is used: Cardiac Index = Cardiac output/Body Surface Area ( N- 2. 4 -4. 4 L/min/m 2) Eg : CO for a 4 yr old (BSA- 0. 5) is 1. 5 L/min CI= 1. 5/0. 5 =3. 0 L/min/m 2 CO for a 50 yr old (BSA- 2. 0) is 6. 0 L/min CI= 6. 0/2. 0 =3. 0 L/min/m 2
Cardiac Output Measurement Ficks Oxygen Method � Ficks Principle: The total uptake or release of any substance by an organ is the product of blood flow to the organ and the arteriovenous concentration difference of the substance. � As applied to lungs, the substance released to the blood is oxygen, oxygen consumption is the product of arteriovenous difference of oxygen across the lungs and pulmonary blood flow (Qp). Qp (L/min) = Oxygen consumption (VO 2) Arteriovenous O 2 difference � In the absence of a shunt, systemic blood flow (Qs) is equal to pulmonary blood flow (Qp).
Cardiac Output Measurement Ficks Oxygen Method: O 2 Consumption Measurement of O 2 Consumption : Douglas Bag method Ø Polarographic method Ø Oxygen Consumption Charts(O 2 Consumption Ø per BSA based on La. Farge & Miettinen charts)
Cardiac Output Measurement Ficks Oxygen Method: AV O 2 Difference Sampling technique › Mixed venous sample �Collect from pulmonary artery(true mixed venous blood) �Because of streaming and incomplete mixing, collection from more proximal sites such as RA or vena cavae may result in error with left-right shunts �RV blood is closer to true mixed venous blood and may be substituted for PA blood if necessary › Arterial sample �Ideal source: pulmonary vein �Alternative sites: LV, LA, peripheral arterial �If arterial dessaturation (Sa. O 2 < 95%) is present , a central right -to-left shunt must be excluded before accepting systemic arterial oxygen content as representative of pulmonary venous blood
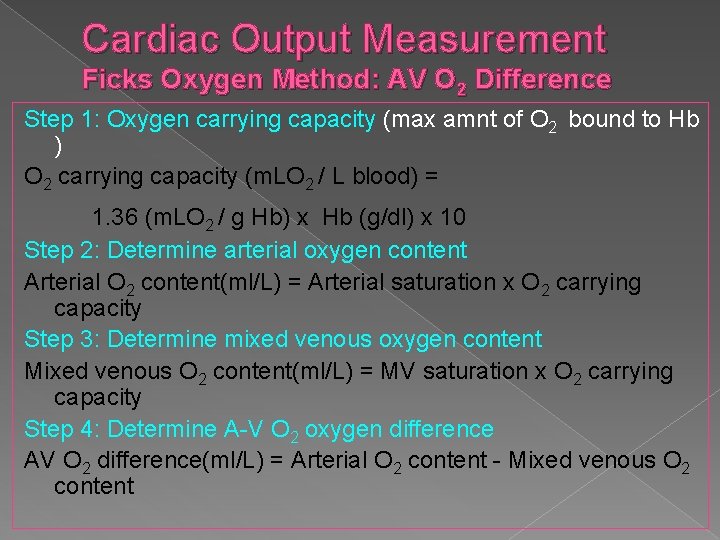
Cardiac Output Measurement Ficks Oxygen Method: AV O 2 Difference Step 1: Oxygen carrying capacity (max amnt of O 2 bound to Hb ) O 2 carrying capacity (m. LO 2 / L blood) = 1. 36 (m. LO 2 / g Hb) x Hb (g/dl) x 10 Step 2: Determine arterial oxygen content Arterial O 2 content(ml/L) = Arterial saturation x O 2 carrying capacity Step 3: Determine mixed venous oxygen content Mixed venous O 2 content(ml/L) = MV saturation x O 2 carrying capacity Step 4: Determine A-V O 2 oxygen difference AV O 2 difference(ml/L) = Arterial O 2 content - Mixed venous O 2 content
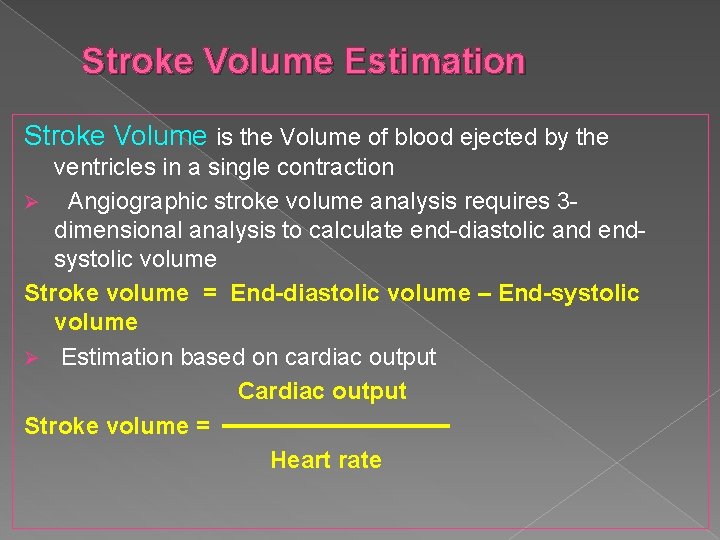
Stroke Volume Estimation Stroke Volume is the Volume of blood ejected by the ventricles in a single contraction Ø Angiographic stroke volume analysis requires 3 dimensional analysis to calculate end-diastolic and endsystolic volume Stroke volume = End-diastolic volume – End-systolic volume Ø Estimation based on cardiac output Cardiac output Stroke volume = Heart rate
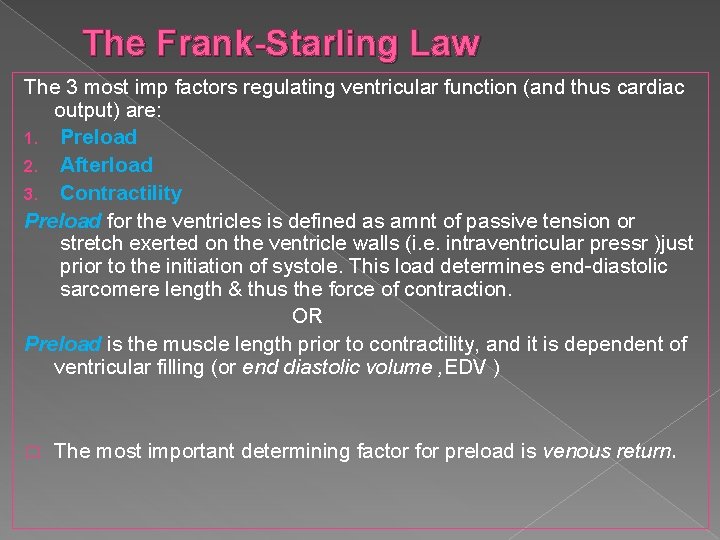
The Frank-Starling Law The 3 most imp factors regulating ventricular function (and thus cardiac output) are: 1. Preload 2. Afterload 3. Contractility Preload for the ventricles is defined as amnt of passive tension or stretch exerted on the ventricle walls (i. e. intraventricular pressr )just prior to the initiation of systole. This load determines end-diastolic sarcomere length & thus the force of contraction. OR Preload is the muscle length prior to contractility, and it is dependent of ventricular filling (or end diastolic volume , EDV ) � The most important determining factor for preload is venous return.
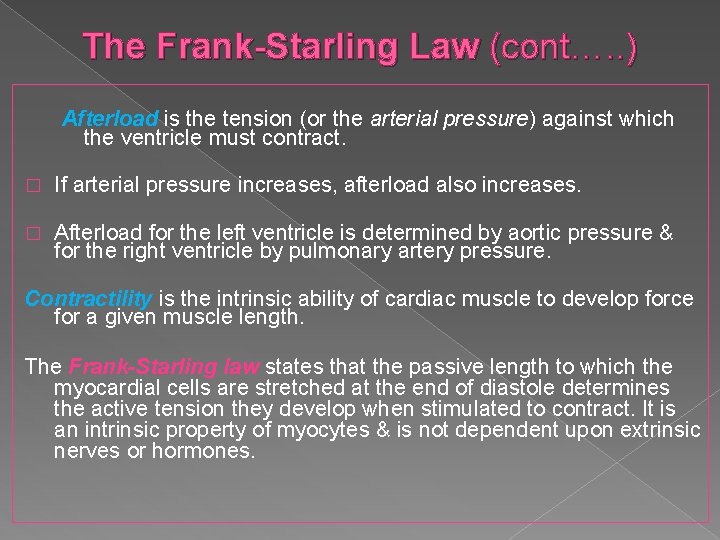
The Frank-Starling Law (cont…. . ) Afterload is the tension (or the arterial pressure) against which the ventricle must contract. � If arterial pressure increases, afterload also increases. � Afterload for the left ventricle is determined by aortic pressure & for the right ventricle by pulmonary artery pressure. Contractility is the intrinsic ability of cardiac muscle to develop force for a given muscle length. The Frank-Starling law states that the passive length to which the myocardial cells are stretched at the end of diastole determines the active tension they develop when stimulated to contract. It is an intrinsic property of myocytes & is not dependent upon extrinsic nerves or hormones.
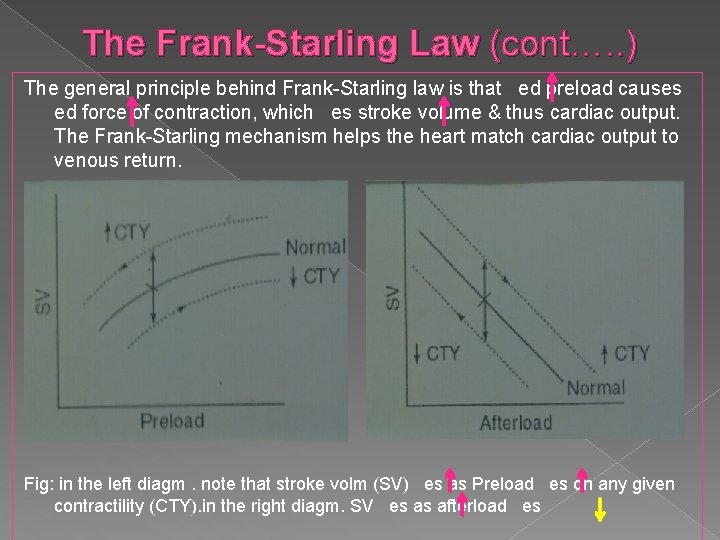
The Frank-Starling Law (cont…. . ) The general principle behind Frank-Starling law is that ed preload causes ed force of contraction, which es stroke volume & thus cardiac output. The Frank-Starling mechanism helps the heart match cardiac output to venous return. Fig: in the left diagm. note that stroke volm (SV) es as Preload es on any given contractility (CTY). in the right diagm. SV es as afterload es
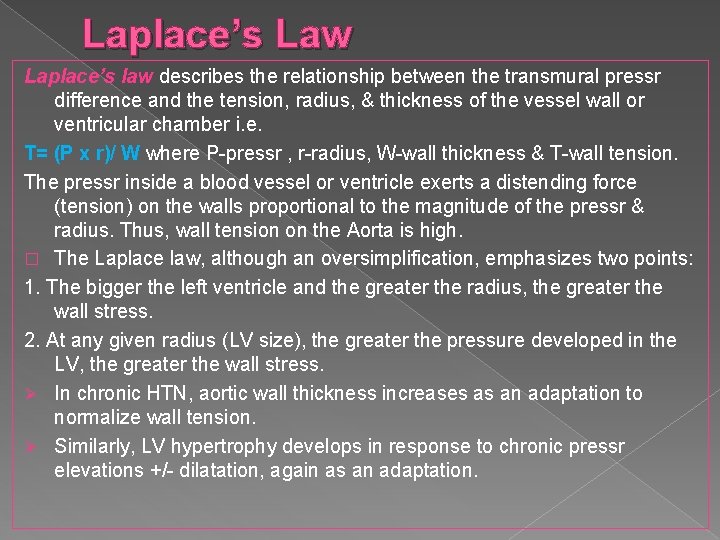
Laplace’s Law Laplace’s law describes the relationship between the transmural pressr difference and the tension, radius, & thickness of the vessel wall or ventricular chamber i. e. T= (P x r)/ W where P-pressr , r-radius, W-wall thickness & T-wall tension. The pressr inside a blood vessel or ventricle exerts a distending force (tension) on the walls proportional to the magnitude of the pressr & radius. Thus, wall tension on the Aorta is high. � The Laplace law, although an oversimplification, emphasizes two points: 1. The bigger the left ventricle and the greater the radius, the greater the wall stress. 2. At any given radius (LV size), the greater the pressure developed in the LV, the greater the wall stress. Ø In chronic HTN, aortic wall thickness increases as an adaptation to normalize wall tension. Ø Similarly, LV hypertrophy develops in response to chronic pressr elevations +/- dilatation, again as an adaptation.
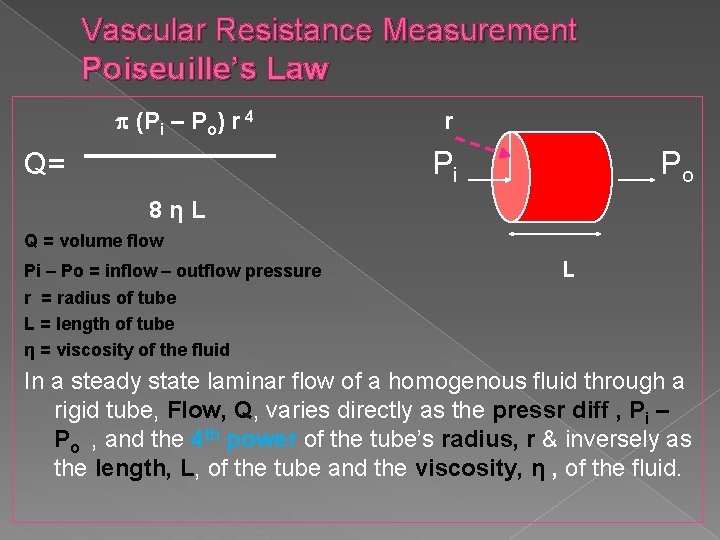
Vascular Resistance Measurement Poiseuille’s Law (Pi – Po) r 4 r Pi Q= Po 8ηL Q = volume flow Pi – Po = inflow – outflow pressure r = radius of tube L = length of tube η = viscosity of the fluid L In a steady state laminar flow of a homogenous fluid through a rigid tube, Flow, Q, varies directly as the pressr diff , Pi – Po , and the 4 th power of the tube’s radius, r & inversely as the length, L, of the tube and the viscosity, η , of the fluid.
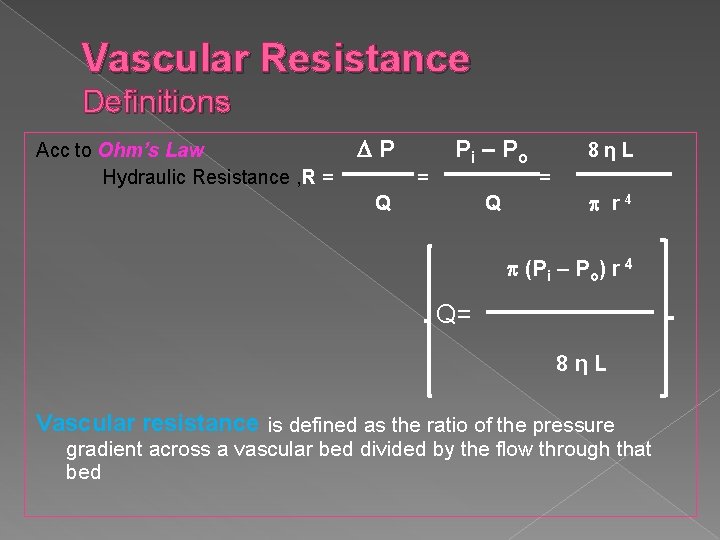
Vascular Resistance Definitions Acc to Ohm’s Law Hydraulic Resistance , R = P = P i – Po Q Q 8ηL = r 4 (Pi – Po) r 4 Q= 8ηL Vascular resistance is defined as the ratio of the pressure gradient across a vascular bed divided by the flow through that bed
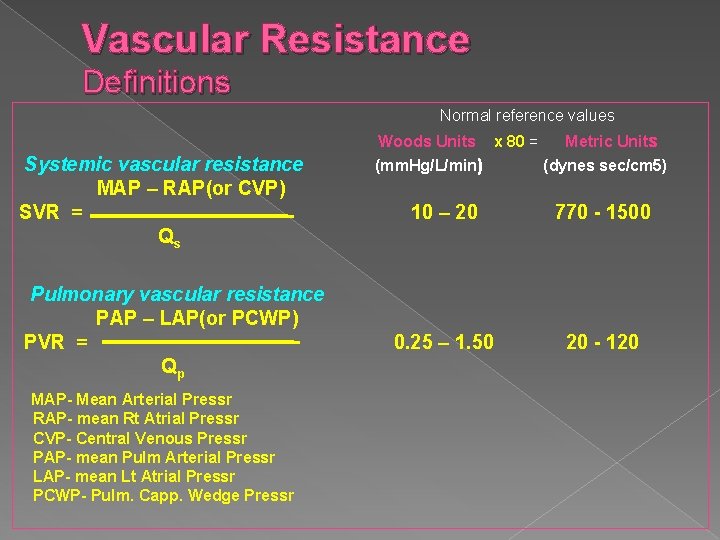
Vascular Resistance Definitions Normal reference values Woods Units Systemic vascular resistance MAP – RAP(or CVP) SVR = Qs Pulmonary vascular resistance PAP – LAP(or PCWP) PVR = Qp MAP- Mean Arterial Pressr RAP- mean Rt Atrial Pressr CVP- Central Venous Pressr PAP- mean Pulm Arterial Pressr LAP- mean Lt Atrial Pressr PCWP- Pulm. Capp. Wedge Pressr (mm. Hg/L/min) x 80 = Metric Units (dynes sec/cm 5) 10 – 20 770 - 1500 0. 25 – 1. 50 20 - 120
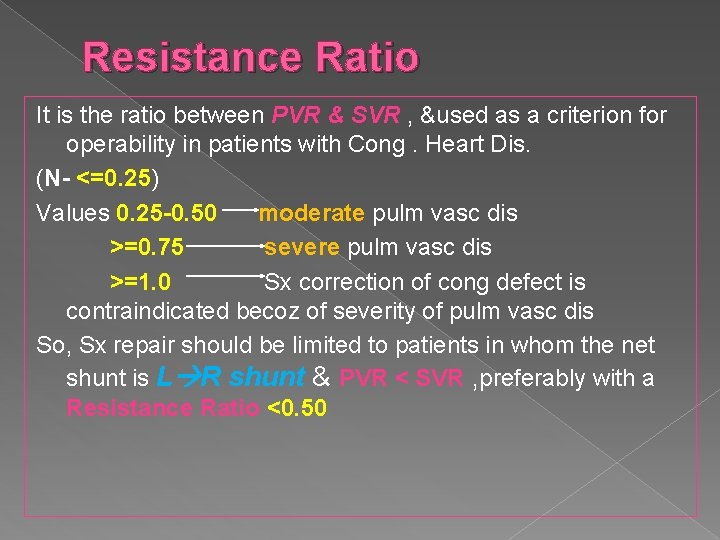
Resistance Ratio It is the ratio between PVR & SVR , &used as a criterion for operability in patients with Cong. Heart Dis. (N- <=0. 25) Values 0. 25 -0. 50 moderate pulm vasc dis >=0. 75 severe pulm vasc dis >=1. 0 Sx correction of cong defect is contraindicated becoz of severity of pulm vasc dis So, Sx repair should be limited to patients in whom the net shunt is L R shunt & PVR < SVR , preferably with a Resistance Ratio <0. 50
Shunt Detection & Measurement Normally, pulmonary blood flow & systemic blood flow are equal. With an abnormal communication between intracardiac chambers or great vessels, blood flow is shunted from systemic circulation to pulmonary circulation (L R shunt) , from pulmonary circulation to systemic circulation (R L shunt) , or in both directions (Bidirectional shunt)
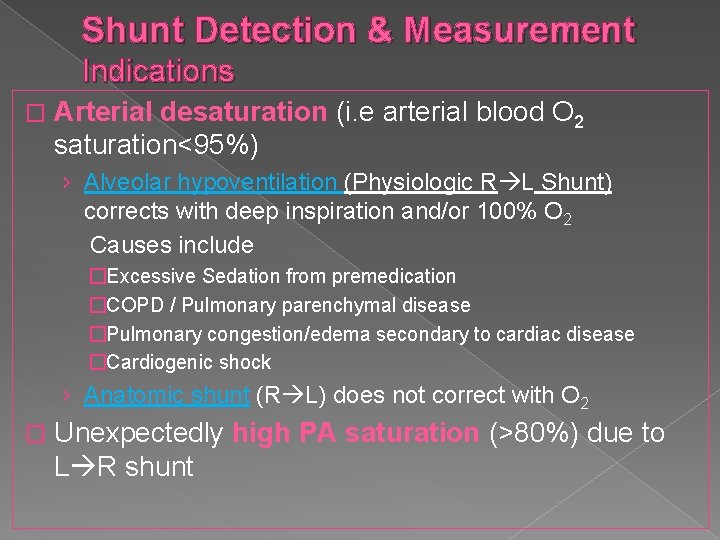
Shunt Detection & Measurement Indications � Arterial desaturation (i. e arterial blood O 2 saturation<95%) › Alveolar hypoventilation (Physiologic R L Shunt) corrects with deep inspiration and/or 100% O 2 Causes include �Excessive Sedation from premedication �COPD / Pulmonary parenchymal disease �Pulmonary congestion/edema secondary to cardiac disease �Cardiogenic shock › Anatomic shunt (R L) does not correct with O 2 � Unexpectedly high PA saturation (>80%) due to L R shunt
Shunt Detection & Measurement Methods � Shunt Detection › Oximetric method (most commonly used) › Indocyanine green method › Angiography � Shunt Measurement › Left-to-Right Shunt › Right-to-Left Shunt › Bidirectional Shunt
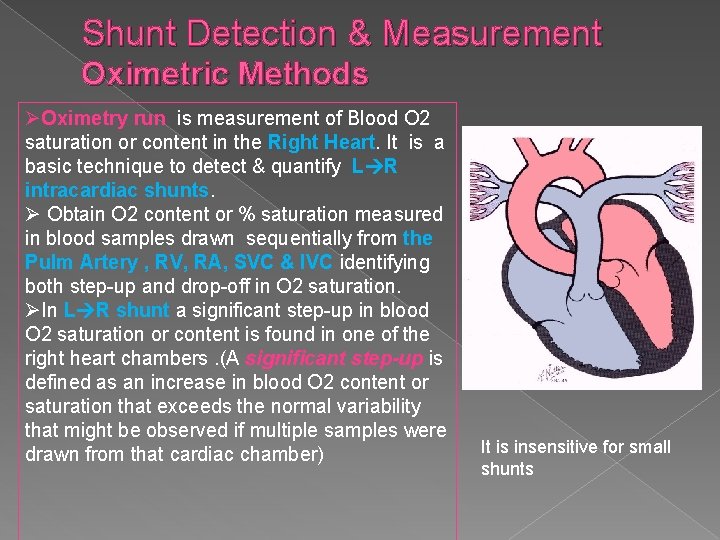
Shunt Detection & Measurement Oximetric Methods ØOximetry run is measurement of Blood O 2 saturation or content in the Right Heart. It is a basic technique to detect & quantify L R intracardiac shunts. Ø Obtain O 2 content or % saturation measured in blood samples drawn sequentially from the Pulm Artery , RV, RA, SVC & IVC identifying both step-up and drop-off in O 2 saturation. ØIn L R shunt a significant step-up in blood O 2 saturation or content is found in one of the right heart chambers. (A significant step-up is defined as an increase in blood O 2 content or saturation that exceeds the normal variability that might be observed if multiple samples were drawn from that cardiac chamber) It is insensitive for small shunts
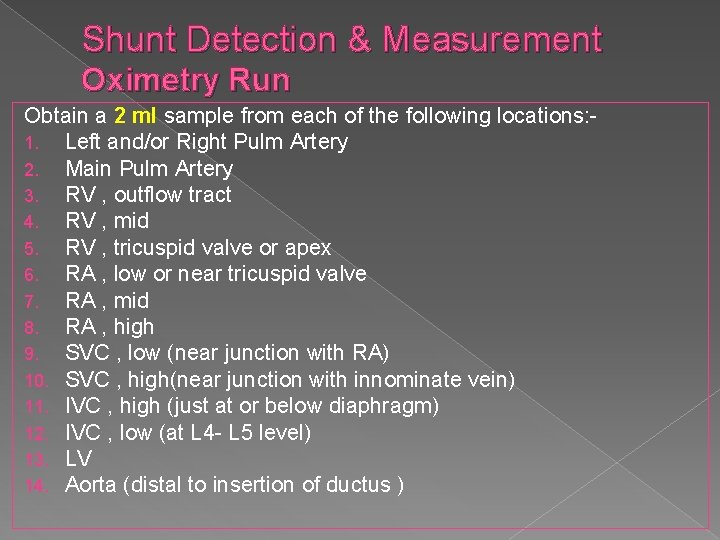
Shunt Detection & Measurement Oximetry Run Obtain a 2 ml sample from each of the following locations: 1. Left and/or Right Pulm Artery 2. Main Pulm Artery 3. RV , outflow tract 4. RV , mid 5. RV , tricuspid valve or apex 6. RA , low or near tricuspid valve 7. RA , mid 8. RA , high 9. SVC , low (near junction with RA) 10. SVC , high(near junction with innominate vein) 11. IVC , high (just at or below diaphragm) 12. IVC , low (at L 4 - L 5 level) 13. LV 14. Aorta (distal to insertion of ductus )
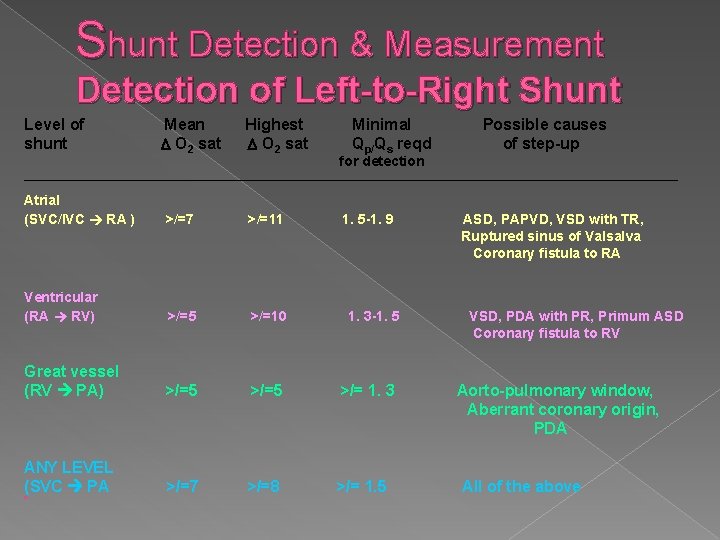
Shunt Detection & Measurement Detection of Left-to-Right Shunt Level of shunt Mean O 2 sat Highest O 2 sat Minimal Qp/Qs reqd for detection Atrial (SVC/IVC RA ) >/=7 >/=11 Ventricular (RA RV) >/=5 >/=10 Great vessel (RV PA) >/=5 >/= 1. 3 ANY LEVEL (SVC PA >/=7 >/=8 >/= 1. 5 � , Possible causes of step-up 1. 5 -1. 9 1. 3 -1. 5 ASD, PAPVD, VSD with TR, Ruptured sinus of Valsalva Coronary fistula to RA VSD, PDA with PR, Primum ASD Coronary fistula to RV Aorto-pulmonary window, Aberrant coronary origin, PDA All of the above
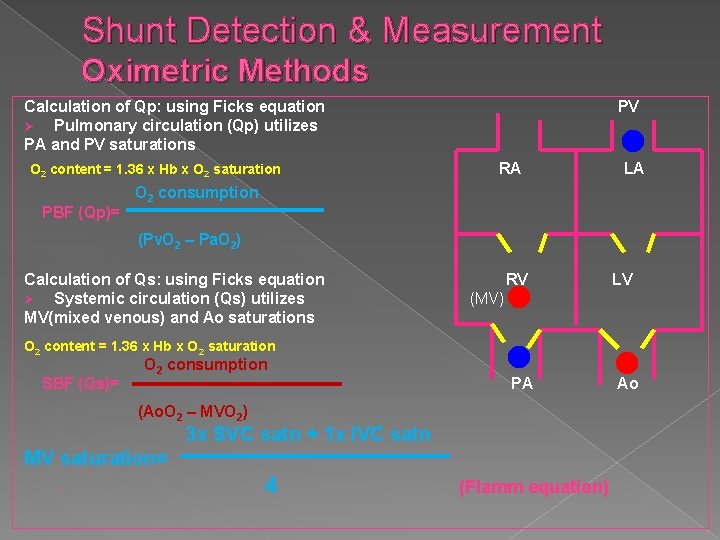
Shunt Detection & Measurement Oximetric Methods Calculation of Qp: using Ficks equation Ø Pulmonary circulation (Qp) utilizes PA and PV saturations O 2 content = 1. 36 x Hb x O 2 saturation PBF (Qp)= PV RA LA O 2 consumption (Pv. O 2 – Pa. O 2) Calculation of Qs: using Ficks equation Ø Systemic circulation (Qs) utilizes MV(mixed venous) and Ao saturations RV LV (MV) O 2 content = 1. 36 x Hb x O 2 saturation SBF (Qs)= O 2 consumption PA (Ao. O 2 – MVO 2) 3 x SVC satn + 1 x IVC satn MV saturation= › 4 (Flamm equation) Ao
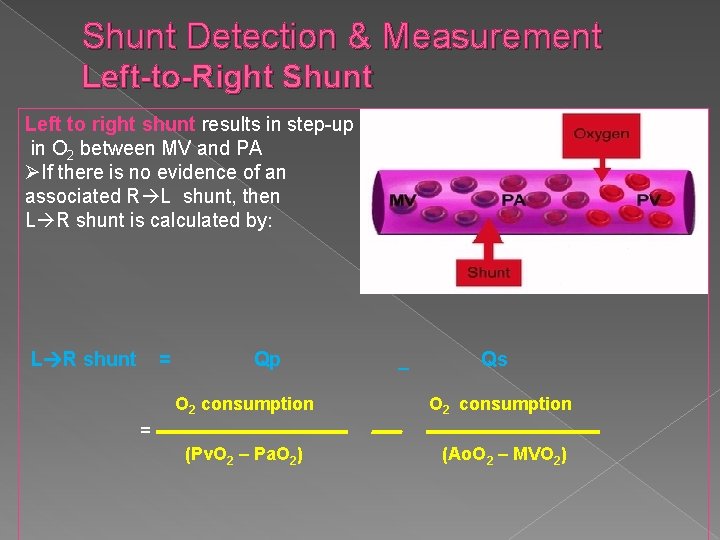
Shunt Detection & Measurement Left-to-Right Shunt Left to right shunt results in step-up in O 2 between MV and PA ØIf there is no evidence of an associated R L shunt, then L R shunt is calculated by: L R shunt = Qp _ Qs O 2 consumption (Pv. O 2 – Pa. O 2) (Ao. O 2 – MVO 2) =
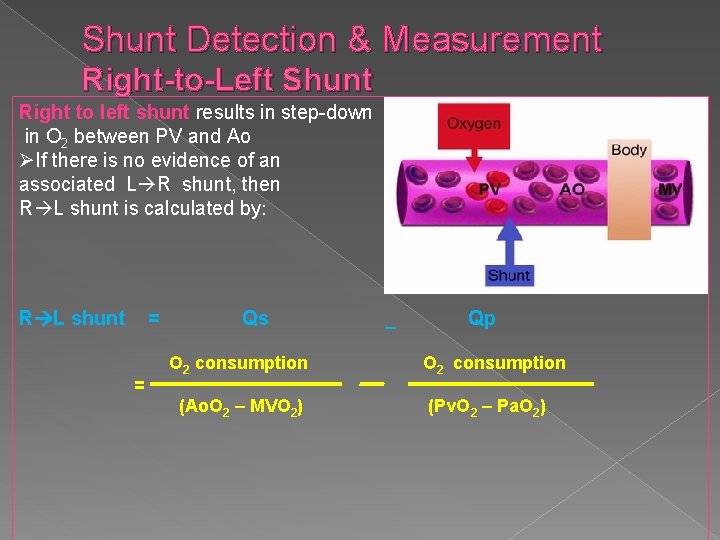
Shunt Detection & Measurement Right-to-Left Shunt Right to left shunt results in step-down in O 2 between PV and Ao ØIf there is no evidence of an associated L R shunt, then R L shunt is calculated by: R L shunt = = Qs O 2 consumption (Ao. O 2 – MVO 2) _ Qp O 2 consumption (Pv. O 2 – Pa. O 2)
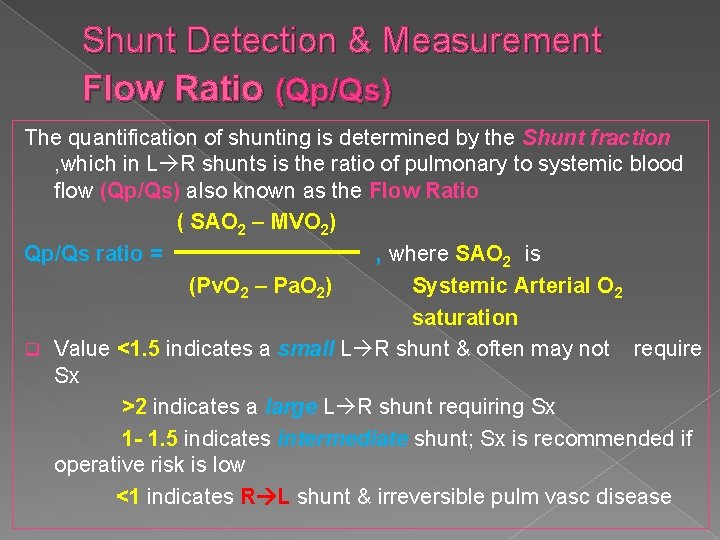
Shunt Detection & Measurement Flow Ratio (Qp/Qs) The quantification of shunting is determined by the Shunt fraction , which in L R shunts is the ratio of pulmonary to systemic blood flow (Qp/Qs) also known as the Flow Ratio ( SAO 2 – MVO 2) Qp/Qs ratio = , where SAO 2 is (Pv. O 2 – Pa. O 2) Systemic Arterial O 2 saturation q Value <1. 5 indicates a small L R shunt & often may not require Sx >2 indicates a large L R shunt requiring Sx 1 - 1. 5 indicates intermediate shunt; Sx is recommended if operative risk is low <1 indicates R L shunt & irreversible pulm vasc disease
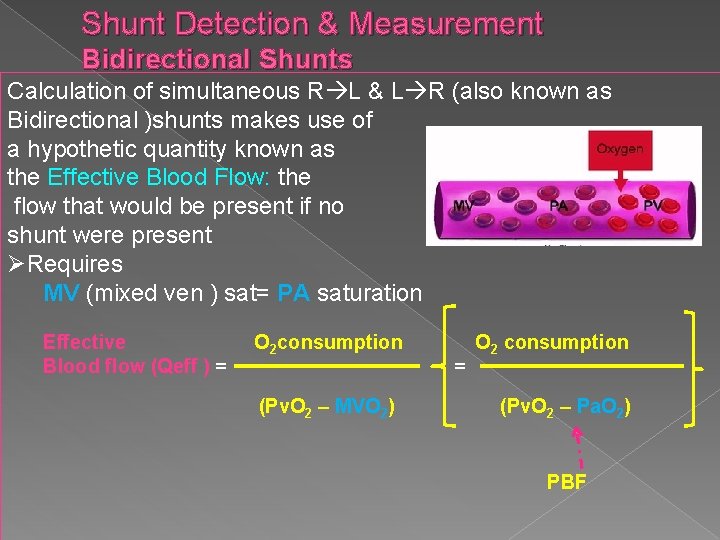
Shunt Detection & Measurement Bidirectional Shunts Calculation of simultaneous R L & L R (also known as Bidirectional )shunts makes use of a hypothetic quantity known as the Effective Blood Flow: the flow that would be present if no shunt were present ØRequires MV (mixed ven ) sat= PA saturation Effective Blood flow (Qeff ) = O 2 consumption (Pv. O 2 – MVO 2) = O 2 consumption (Pv. O 2 – Pa. O 2) PBF
Shunt Detection & Measurement Bidirectional Shunts The approximate L R shunt = Qp & The approximate R L shunt = Qs Qeff
Conclusion Hemodynamic monitoring started with the estimation of heart rate using the simple skill of 'finger on the pulse' and then moved on to more and more sophisticated techniques like stethoscope, sphygmomanometer, ECG, ECHO , catheterization etc. The status of critically ill patients can be assessed either from non-invasive single parameter indicators or various invasive techniques that provide multiparameter hemodynamic measurements. As a result, comprehensive data can be provided for the clinician to proactively address hemodynamic crisis and safely manage the patient instead of reacting to late indicators of hemodynamic instability
- Slides: 48