Basics of Antimicrobial Therapy 1 Selective Toxicity How
Basics of Antimicrobial Therapy 1
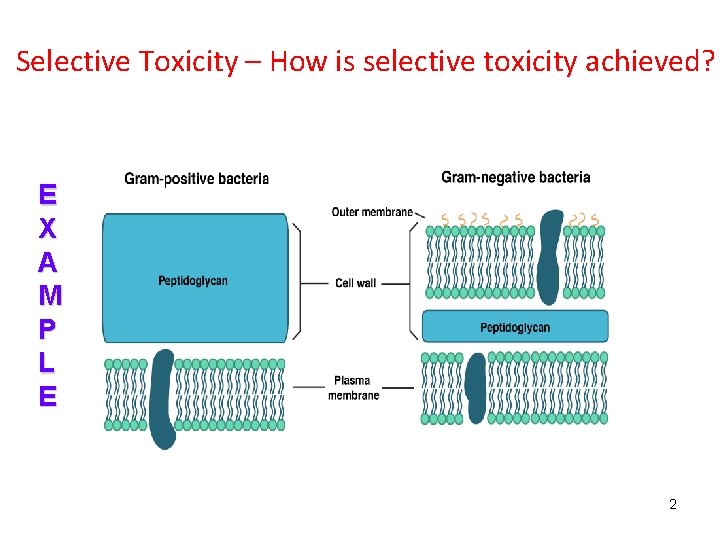
Selective Toxicity – How is selective toxicity achieved? E X A M P L E 2

Selective Toxicity – How is selective toxicity achieved? E X A M P L E https: //www. slideshare. net/shahmurad 65/folic-acid-synthesis-inhibitors Q. Why don’t sulfonamides hurt us? 3

4
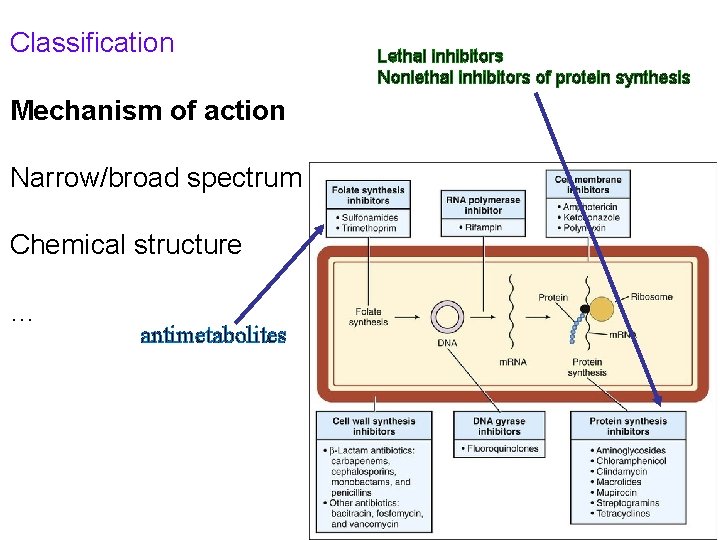
Classification Lethal inhibitors Nonlethal inhibitors of protein synthesis Mechanism of action Narrow/broad spectrum Chemical structure … antimetabolites 5
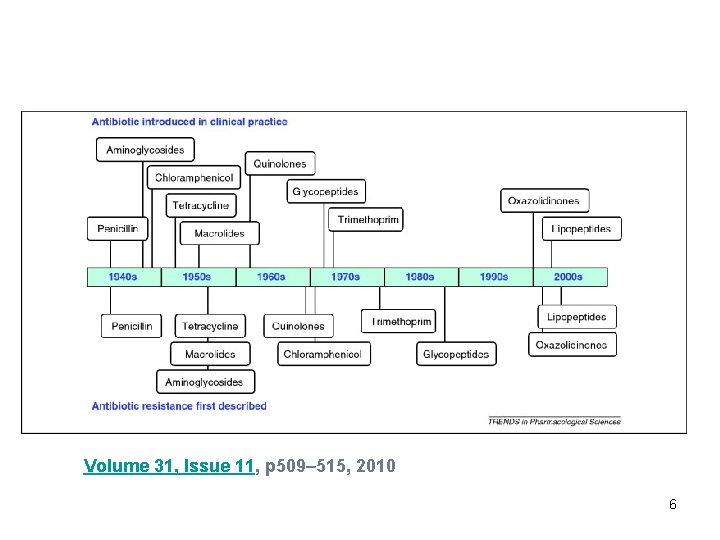
Volume 31, Issue 11, p 509– 515, 2010 6
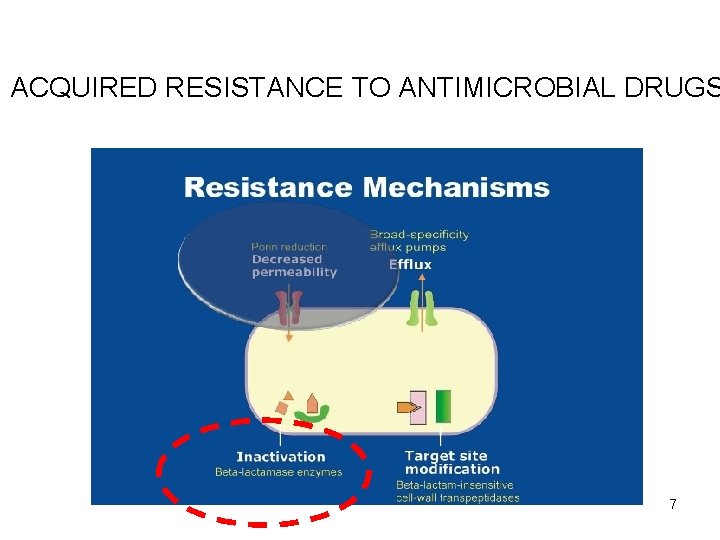
ACQUIRED RESISTANCE TO ANTIMICROBIAL DRUGS 7

8

9
NOSOCOMIAL INFECTION Nosocomial infections or healthcare associated infections occur in patients under medical care that occurre within 48 hours of hospital admission, 3 days of discharge or 30 days of an operation SUPRAINFECTION 10
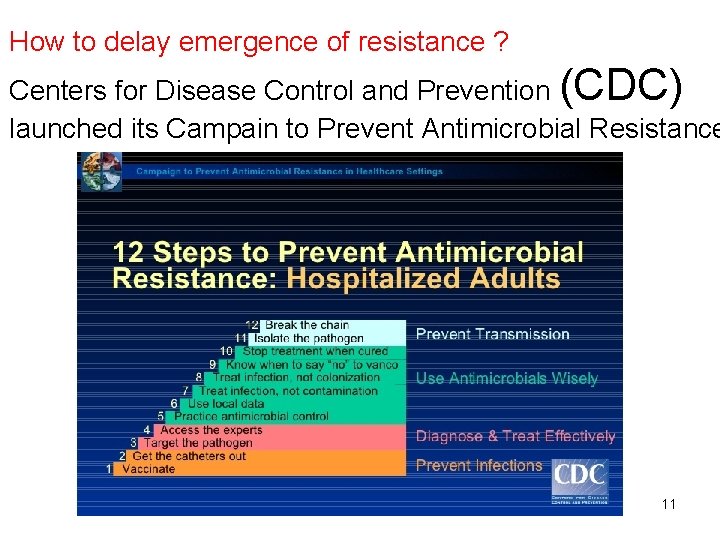
How to delay emergence of resistance ? Centers for Disease Control and Prevention (CDC) launched its Campain to Prevent Antimicrobial Resistance 11

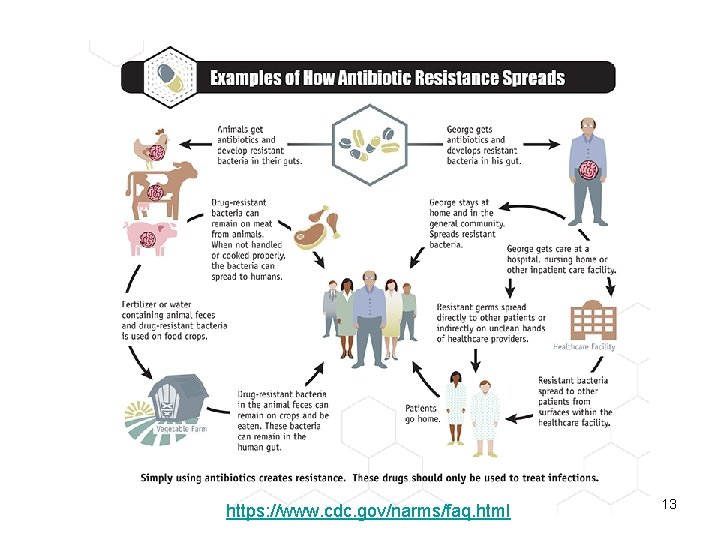
https: //www. cdc. gov/narms/faq. html 13
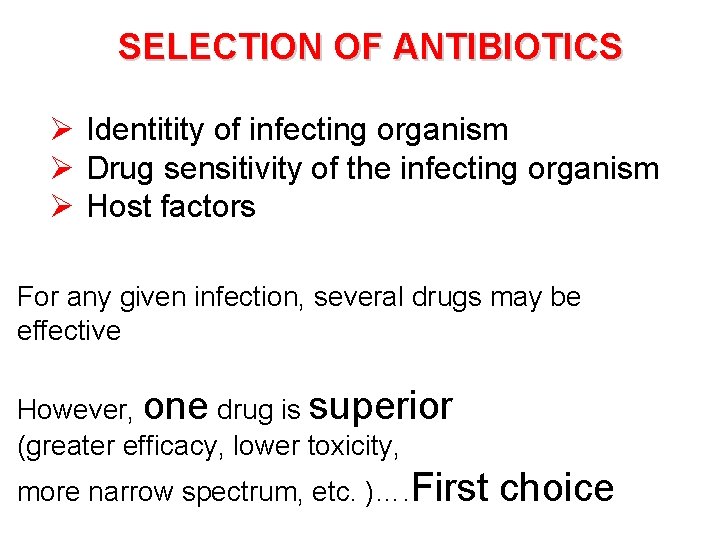
SELECTION OF ANTIBIOTICS Ø Identitity of infecting organism Ø Drug sensitivity of the infecting organism Ø Host factors For any given infection, several drugs may be effective However, one drug is superior (greater efficacy, lower toxicity, more narrow spectrum, etc. )…. First choice
Inability of the drug to penetrate to the site of infection Unusual susceptibility of the patient to the toxic effects of first choice drug 15
General Guidelines Do not treat colonization or contamination (S. epidermidis from a single blood culture should be carefully examined) Use the most narrow-spectrum agent for the infection Use proper dose Use the shortest effective duration 16
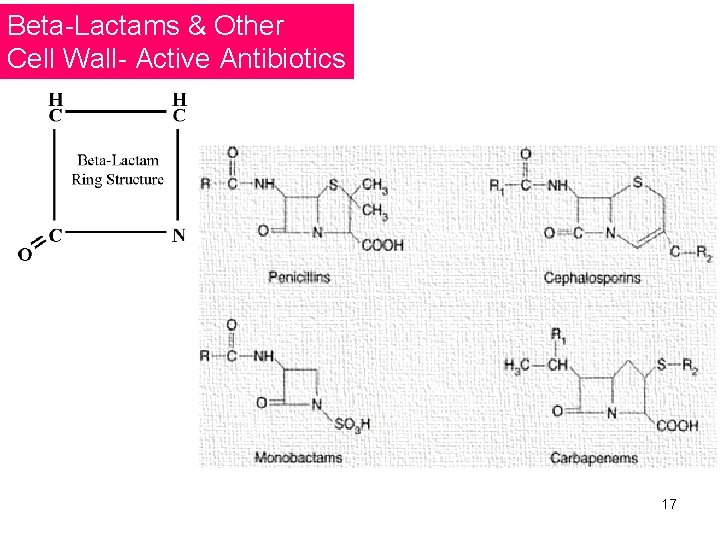
Beta-Lactams & Other Cell Wall- Active Antibiotics 17
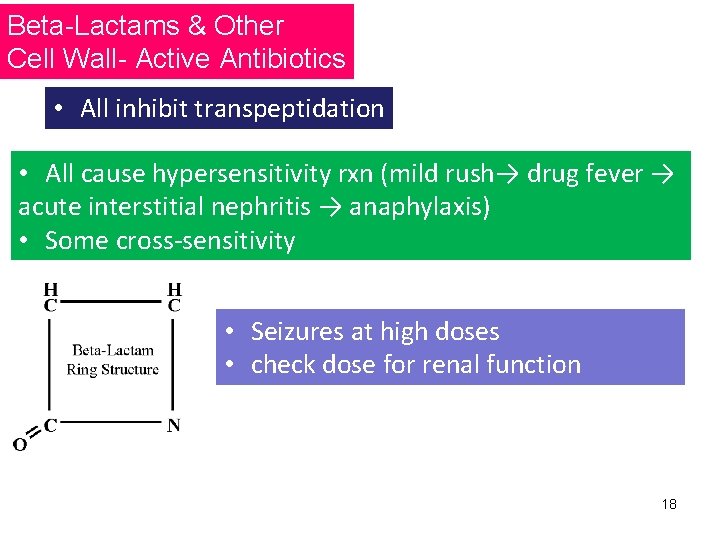
Beta-Lactams & Other Cell Wall- Active Antibiotics • All inhibit transpeptidation • All cause hypersensitivity rxn (mild rush→ drug fever → acute interstitial nephritis → anaphylaxis) • Some cross-sensitivity • Seizures at high doses • check dose for renal function 18
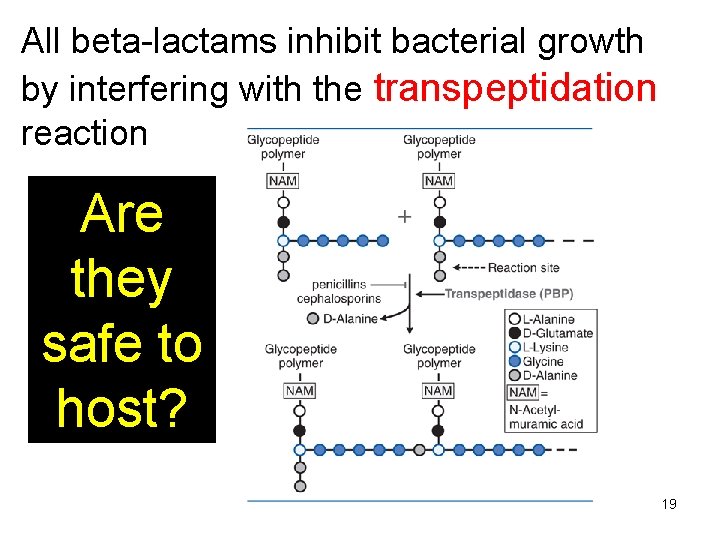
All beta-lactams inhibit bacterial growth by interfering with the transpeptidation reaction Are they safe to host? 19
![f. T>MIC Time-dependent killing • [AB] > MIC for a spesific time during dosing f. T>MIC Time-dependent killing • [AB] > MIC for a spesific time during dosing](http://slidetodoc.com/presentation_image_h2/ea8999abceb98d7c39233e0c861d4b0d/image-20.jpg)
f. T>MIC Time-dependent killing • [AB] > MIC for a spesific time during dosing interval • Prototype β-lactams f. T>MIC Penicillins Cephalosporins Carbapenems 50% 60 -70* % 40% 20
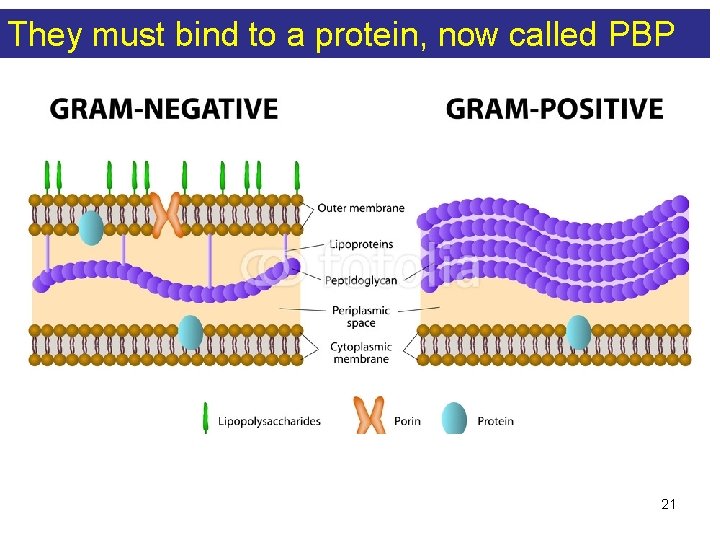
They must bind to a protein, now called PBP 21
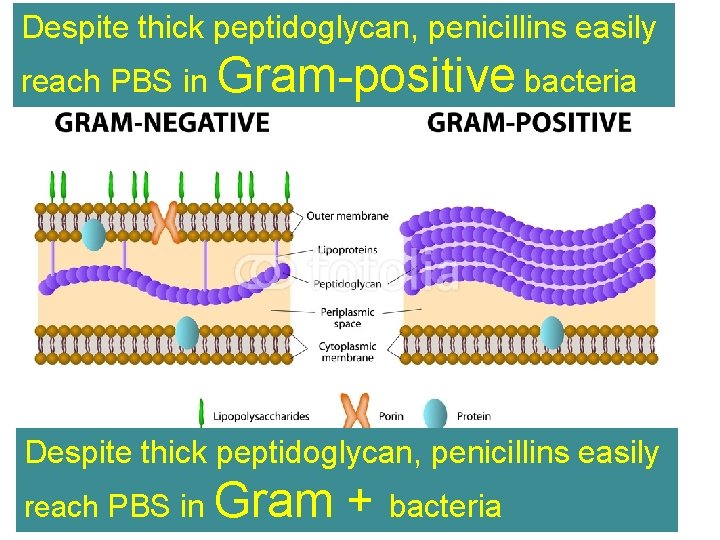
Despite thick peptidoglycan, penicillins easily reach PBS in Gram-positive bacteria Despite thick peptidoglycan, penicillins easily reach PBS in Gram + bacteria 22
MECHANISMS OF RESISTANCE • inability to reach PBPs • inactivation of penicillins (β- lactam ring) by bacterial enzymes • beta-lactamases that selectively act on penicillins are penicillinases 23
β-lactamases are enzymes that open the beta-lactam ring, inactivating the antibiotic The first plasmid-mediated β-lactamase in gramnegative bacteria was discovered in Greece in the 1960 s It was named TEM after the patient from whom it was isolated (Temoniera ) Subsequently, a closely related enzyme was discovered and named TEM-2 24
Microorganisms with β-lactamase activity hundreds of β -lactamases!! … Some are narrow in specificity. . prefer penicillins Amp. C and ESBLs hydrolyse almost all antibiotics 25
https: //www. uptodate. com/contents/overview-of-carbapenemaseproducing-gram-negative-bacilli 26
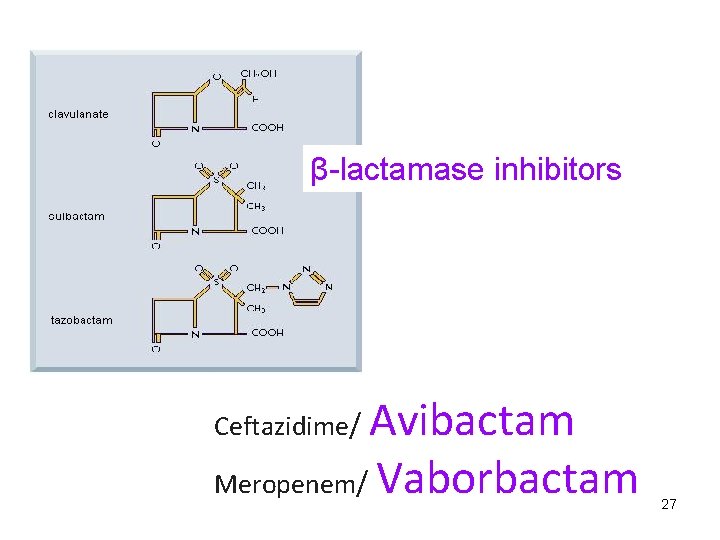
β-lactamase inhibitors Avibactam Meropenem/ Vaborbactam Ceftazidime/ 27
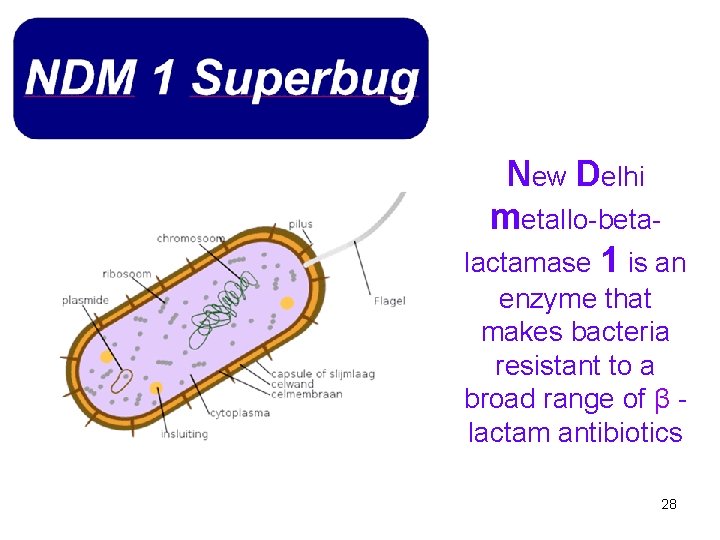
New Delhi metallo-betalactamase 1 is an enzyme that makes bacteria resistant to a broad range of β lactam antibiotics 28
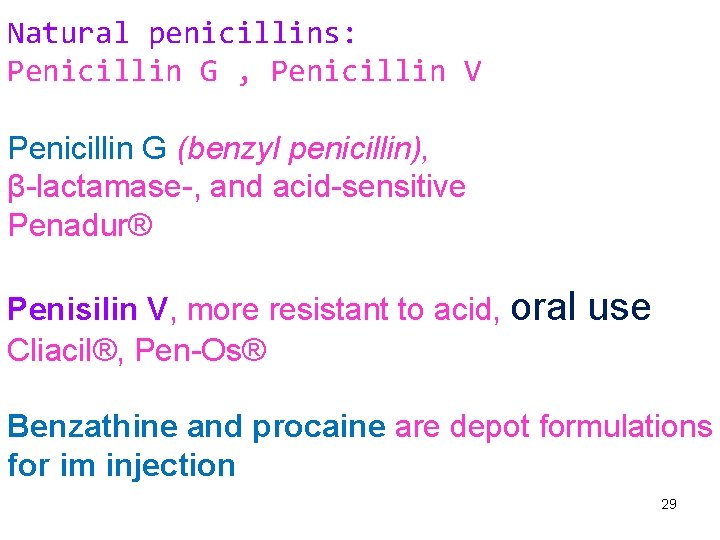
Natural penicillins: Penicillin G , Penicillin V Penicillin G (benzyl penicillin), β-lactamase-, and acid-sensitive Penadur® Penisilin V, more resistant to acid, oral Cliacil®, Pen-Os® use Benzathine and procaine are depot formulations for im injection 29
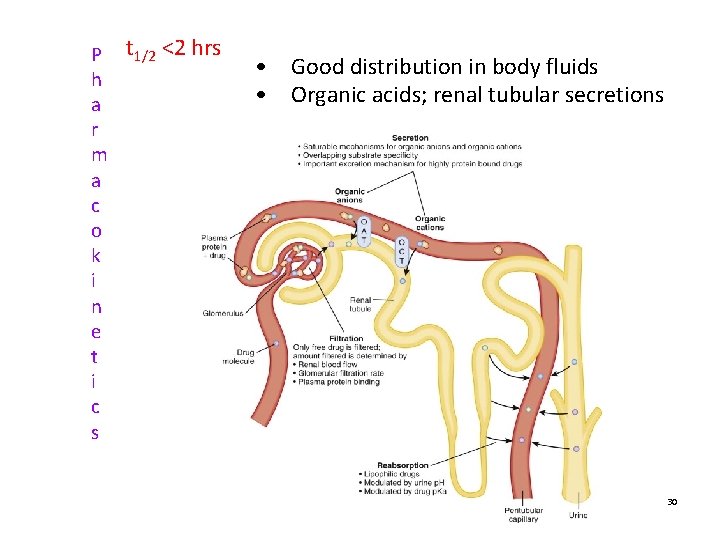
P t 1/2 <2 hrs h a r m a c o k i n e t i c s • Good distribution in body fluids • Organic acids; renal tubular secretions 30
What are they good for? Treponema pallidum (T. pallidum) Syphilis Benzathin penicillin, 2. 4 x 106 U im, once a week, 1 -3 weeks 31
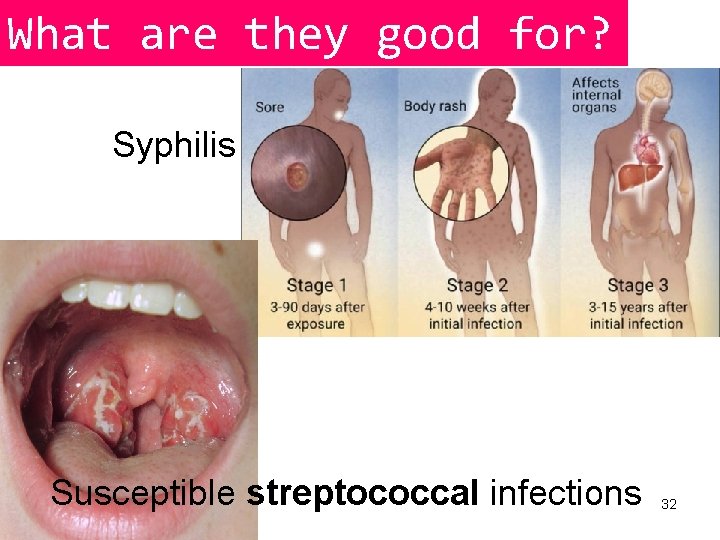
What are they good for? Syphilis Susceptible streptococcal infections 32
Antistaphylococcal Penicillin(s): nafcillin, oxacillin, dicloxacillin, methicillin, cloxacillin flucloxacillin • Short half-life (30 -60’) 33
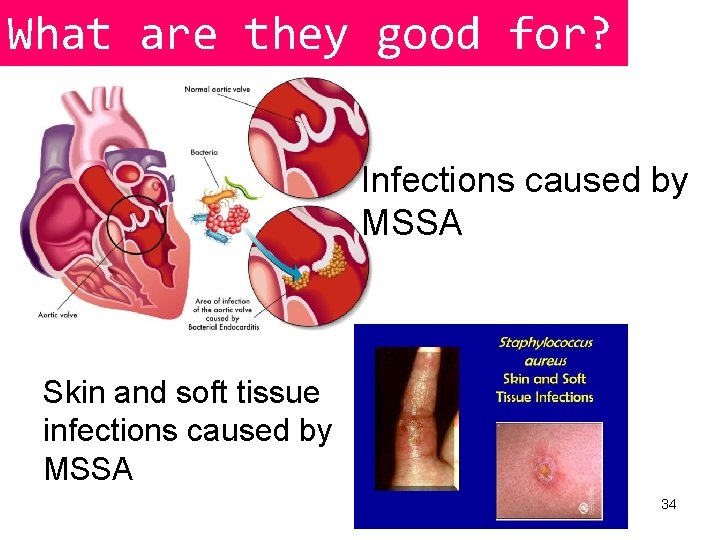
What are they good for? Infections caused by MSSA Skin and soft tissue infections caused by MSSA 34
Aminopenicillins: (Broad-Spectrum Penicillins) Ampicillin, Amoxicillin • More water-soluble and pass through porin channels of some Gram - • SUSCEPTIBLE to beta-lactamases • Usually combined with beta-lactamase inhibitors • High incidence of diarrhea when given orally • (in US, ampicillin iv, amoxicillin per os) 35
Except for amoxicillin, absorption of penicillins is impaired by food 36

Co-amoxiclav (amoxicillin+clavulanic acid) Sultamicillin (ampicillin+sulbactam) 37
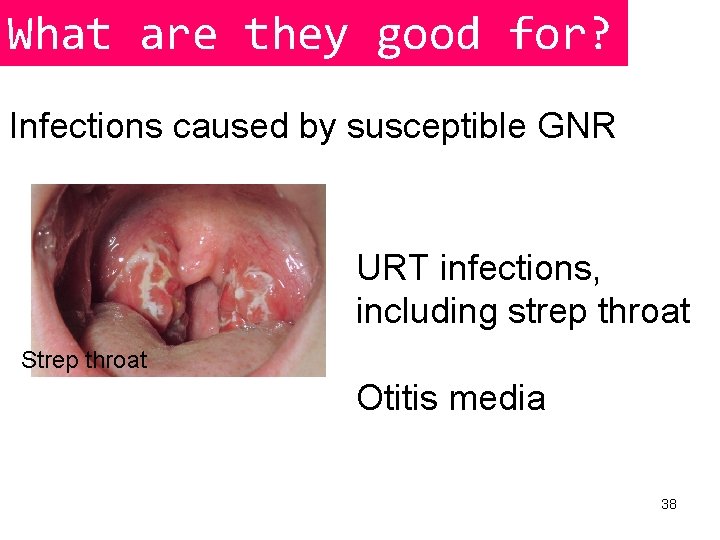
What are they good for? Infections caused by susceptible GNR URT infections, including strep throat Strep throat Otitis media 38
Centers for Disease Control and Prevention https: //www. cdc. gov/antibioticuse/community/for-hcp/outpatienthcp/adult-treatment-rec. html The Infectious Diseases Society of America (IDSA) http: //www. idsociety. org/ Practice. Guidelines/? q= 39
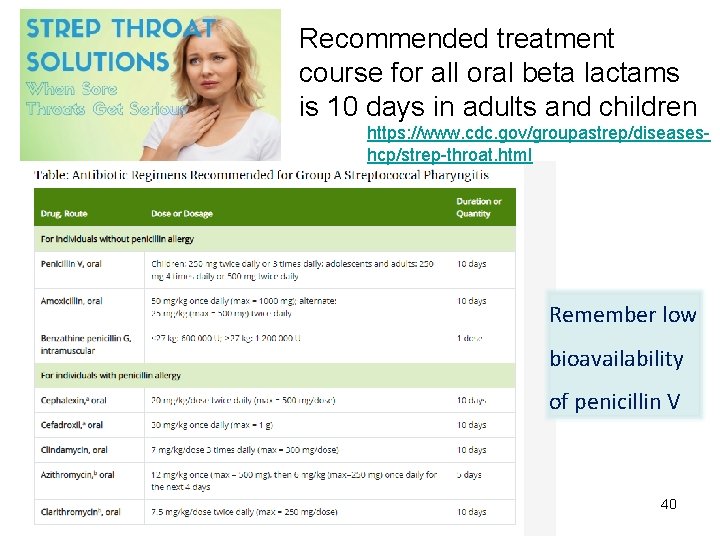
Recommended treatment course for all oral beta lactams is 10 days in adults and children https: //www. cdc. gov/groupastrep/diseaseshcp/strep-throat. html Remember low bioavailability of penicillin V 40
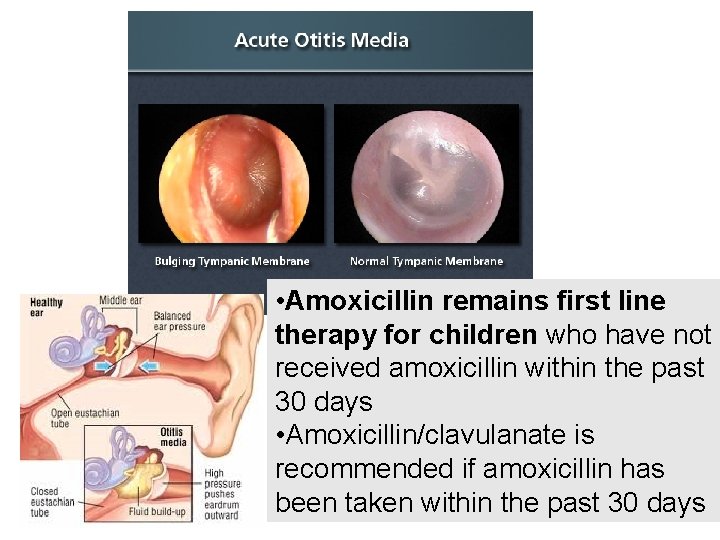
• Amoxicillin remains first line therapy for children who have not received amoxicillin within the past 30 days • Amoxicillin/clavulanate is recommended if amoxicillin has 41 been taken within the past 30 days
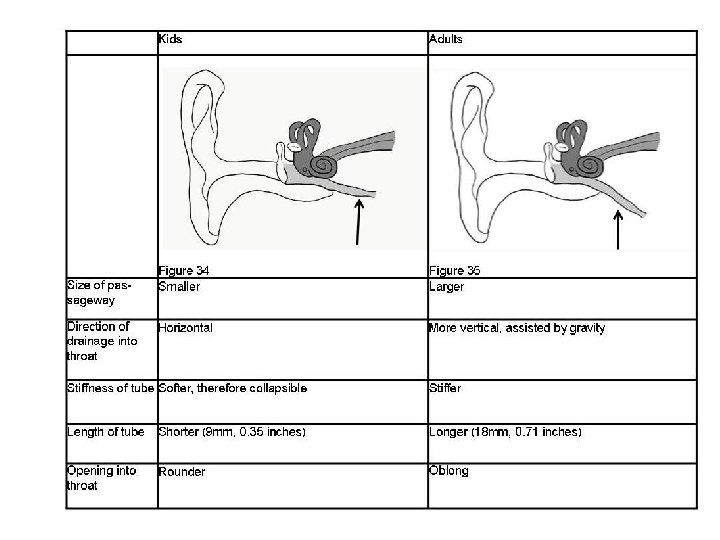
42
Acute rhinosinusitis • Amoxicillin or amoxicillin/clavulanate is the recommended first-line therapy 43
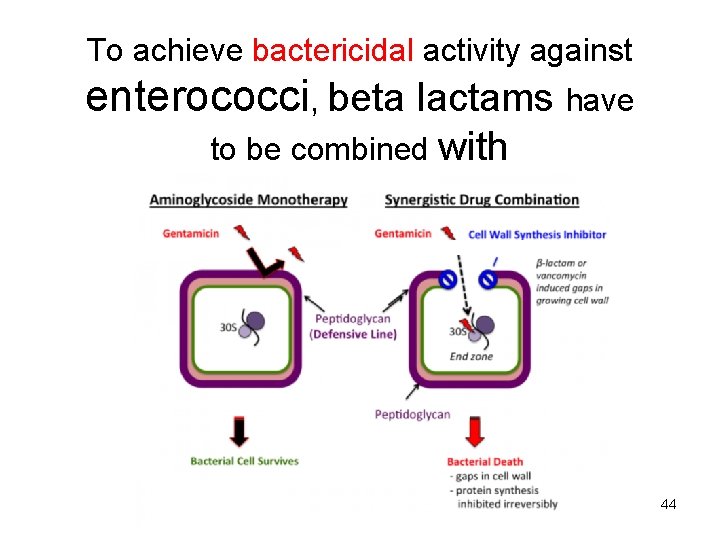
To achieve bactericidal activity against enterococci, beta lactams have to be combined with aminoglycosides 44
Antipseudomonal Penicillins: piperacillin, mezlocillin*, carbenicillin*, ticarcillin* *no longer produced in Turkey 45
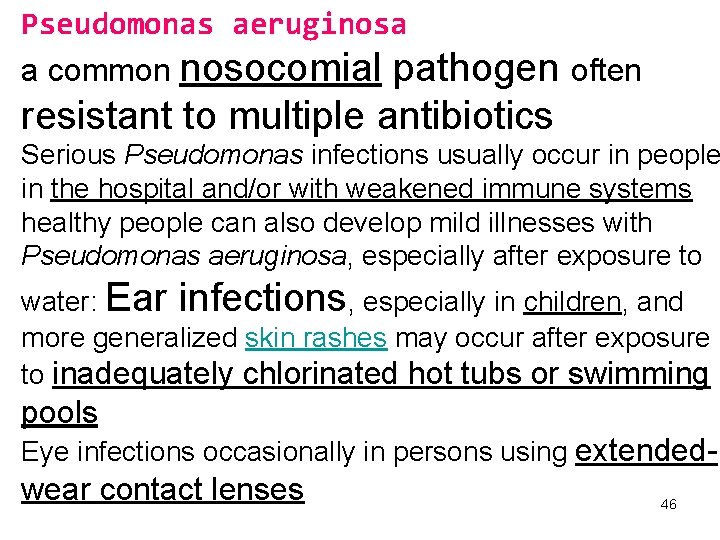
Pseudomonas aeruginosa a common nosocomial pathogen often resistant to multiple antibiotics Serious Pseudomonas infections usually occur in people in the hospital and/or with weakened immune systems healthy people can also develop mild illnesses with Pseudomonas aeruginosa, especially after exposure to water: Ear infections, especially in children, and more generalized skin rashes may occur after exposure to inadequately chlorinated hot tubs or swimming pools Eye infections occasionally in persons using extended- wear contact lenses 46
Piperacillin ve tazobactam: Tazeracin® • Susceptible to beta-lactamases 47
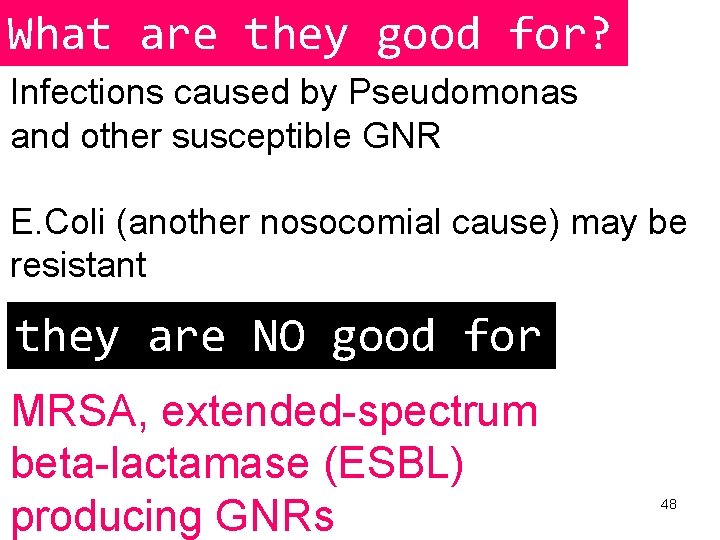
What are they good for? Infections caused by Pseudomonas and other susceptible GNR E. Coli (another nosocomial cause) may be resistant they are NO good for MRSA, extended-spectrum beta-lactamase (ESBL) producing GNRs 48
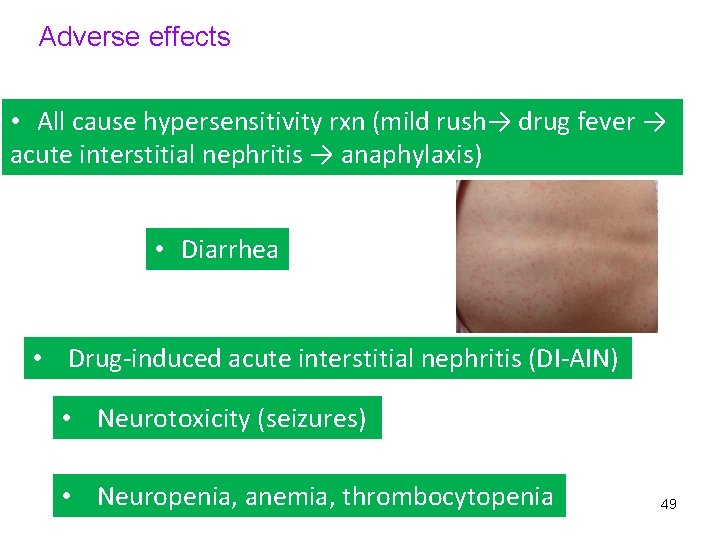
Adverse effects • All cause hypersensitivity rxn (mild rush→ drug fever → acute interstitial nephritis → anaphylaxis) • Diarrhea • Drug-induced acute interstitial nephritis (DI-AIN) • Neurotoxicity (seizures) • Neuropenia, anemia, thrombocytopenia 49
Cephalosporins cephalosporin penicillin • Grouped into generations that largely correlate with their spectrum of activity • All have some cross-allergenity with penicillins • Usually more resistant to β-lactamases • None of the current have useful activity against enterococci
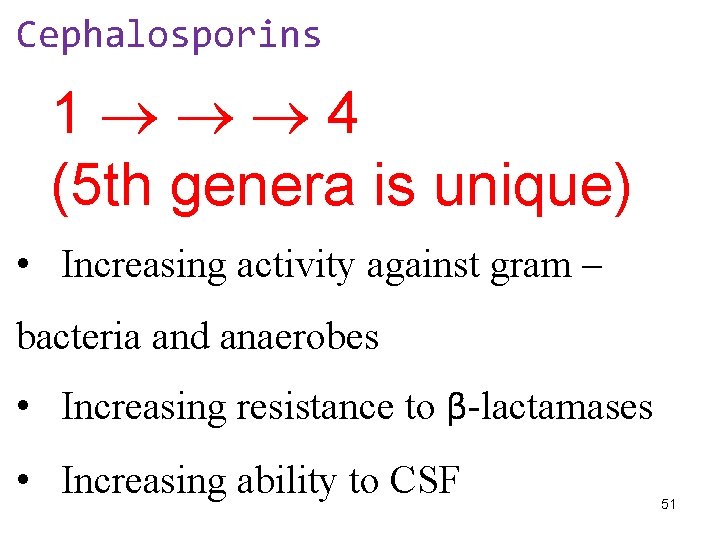
Cephalosporins 1 4 (5 th genera is unique) • Increasing activity against gram – bacteria and anaerobes • Increasing resistance to β-lactamases • Increasing ability to CSF 51
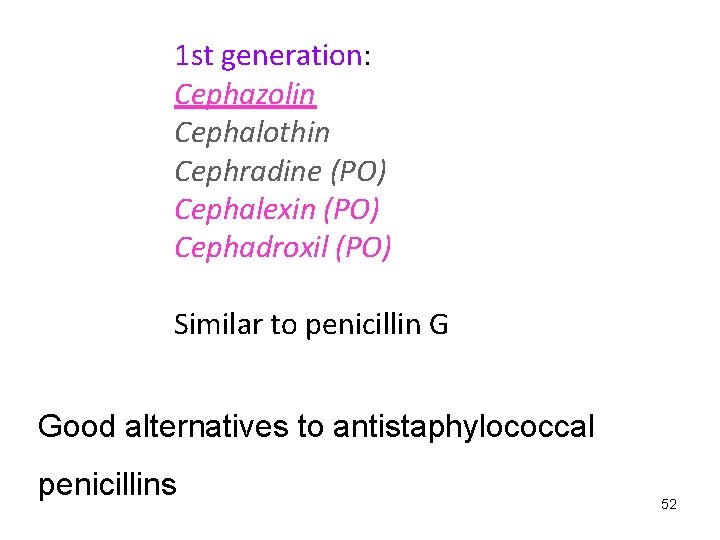
1 st generation: Cephazolin Cephalothin Cephradine (PO) Cephalexin (PO) Cephadroxil (PO) Similar to penicillin G Good alternatives to antistaphylococcal penicillins 52
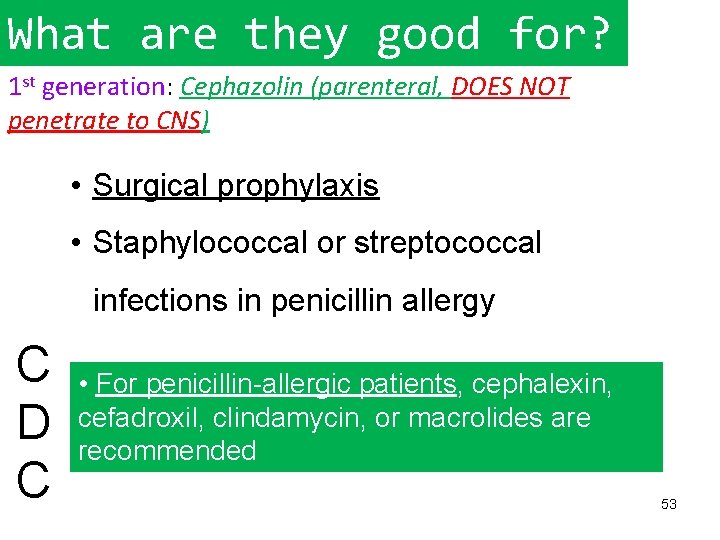
What are they good for? 1 st generation: Cephazolin (parenteral, DOES NOT penetrate to CNS) • Surgical prophylaxis • Staphylococcal or streptococcal infections in penicillin allergy C D C • For penicillin-allergic patients, cephalexin, cefadroxil, clindamycin, or macrolides are recommended 53
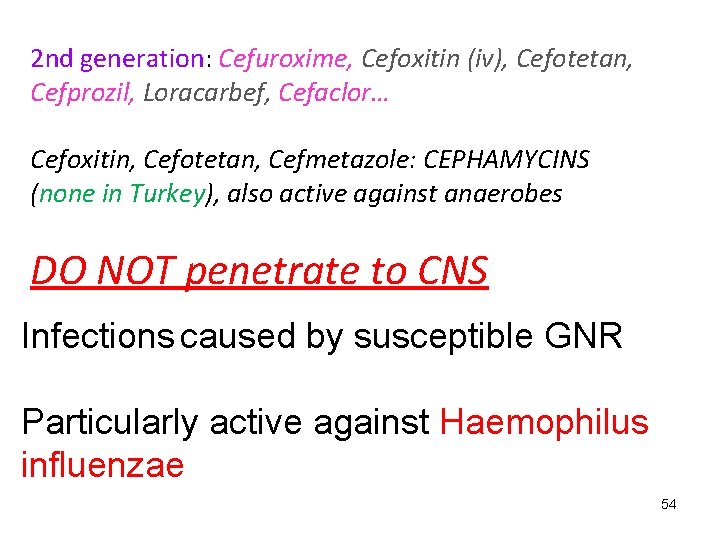
2 nd generation: Cefuroxime, Cefoxitin (iv), Cefotetan, Cefprozil, Loracarbef, Cefaclor… Cefoxitin, Cefotetan, Cefmetazole: CEPHAMYCINS (none in Turkey), also active against anaerobes DO NOT penetrate to CNS Infections caused by susceptible GNR Particularly active against Haemophilus influenzae 54

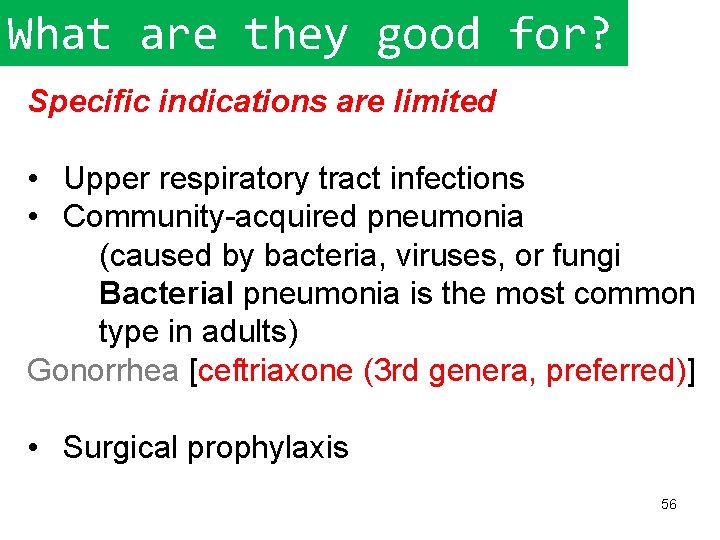
What are they good for? Specific indications are limited • Upper respiratory tract infections • Community-acquired pneumonia (caused by bacteria, viruses, or fungi Bacterial pneumonia is the most common type in adults) Gonorrhea [ceftriaxone (3 rd genera, preferred)] • Surgical prophylaxis 56
3 rd generation Cefdinir (PO) Cefdiroten(PO) Cefixime (PO) Cefdibuten (PO) Ceftazidime (parenteral) Cefaperazone (parenteral) Ceftriaxone (parenteral) Ceftizoxime (parenteral) Cefotaxime (parenteral). . . 57
Gonorrhea can be cured with the right treatment CDC recommends dual therapy, or using two drugs, to treat gonorrhea – a single dose of 250 mg of intramuscular ceftriaxone AND 1 g of oral azithromycin Antibiotic-Resistant Gonorrhea https: //www. cdc. gov/std/gonorrhea/arg/default. htm 58
BROAD SPECTRUM OF ACTIVITY More stable to common beta-lactamases of gram-negative bacilli, and these compounds are highly active against Enterobacteriaceae They are therapy of choice for gram-negative meningitis due to susceptible Enterobacteriaceae Drugs of choice for meningitis caused by enteric gram- bacilli Ceftazidime for meningitis caused by P. aeruginosa 59
NOSOCOMIAL infections caused by Gram – bacilli are indications for 3 rd genera… CAUTION for resistance! D E S U E B T O N ! Y D L L E U N I O T U SH O R 60
61
62
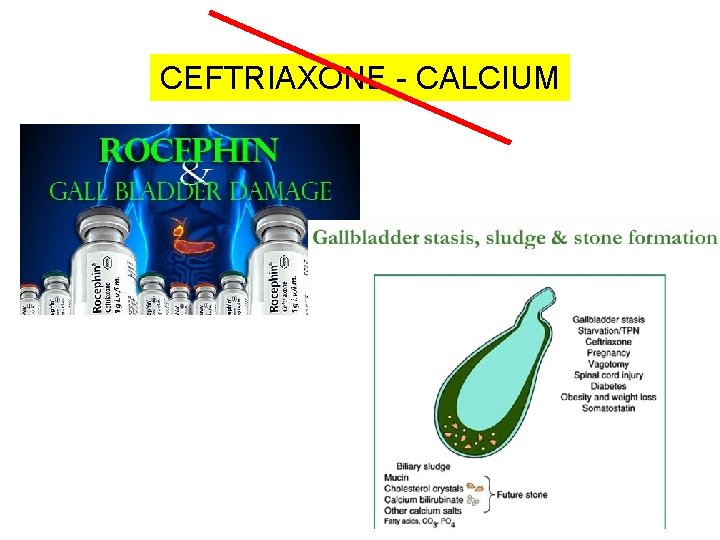
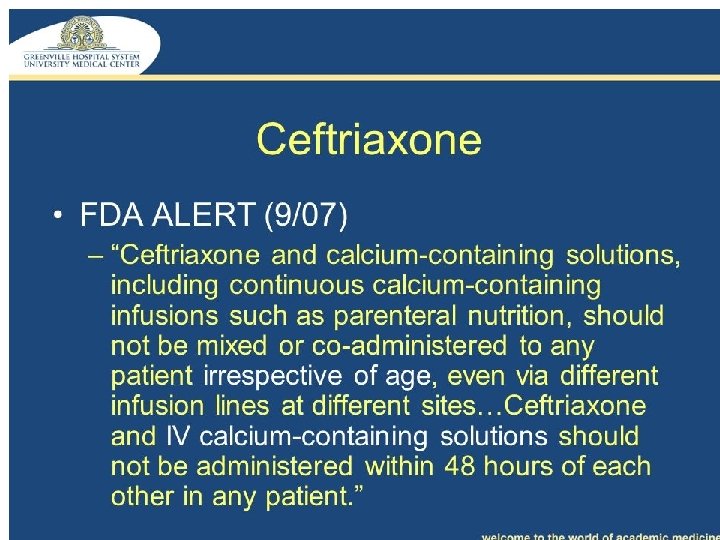
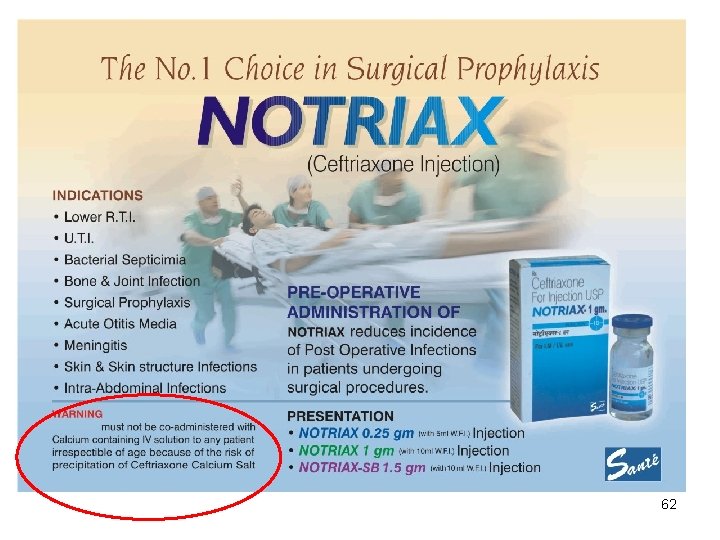
CEFTRIAXONE - CALCIUM 63
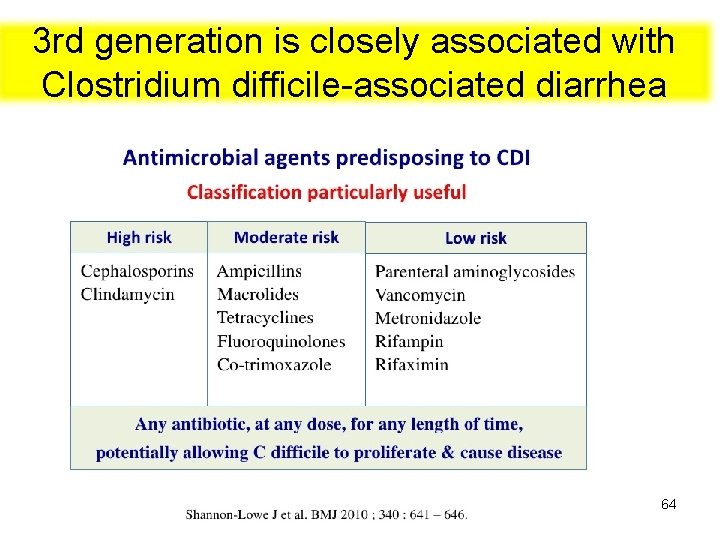
3 rd generation is closely associated with Clostridium difficile-associated diarrhea 64
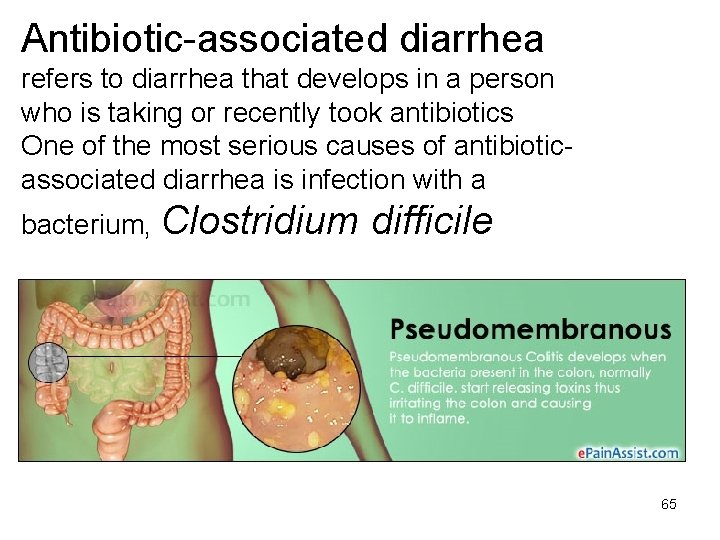
Antibiotic-associated diarrhea refers to diarrhea that develops in a person who is taking or recently took antibiotics One of the most serious causes of antibioticassociated diarrhea is infection with a bacterium, Clostridium difficile 65
Antibiotic treatment — Usually an oral antibiotic (most often vancomycin or fidaxomicin) is used to treat people who are infected with C. difficile. It is important to take each dose of the antibiotic on time and to finish the entire course of treatment (usually 10 to 14 days) Probiotics — Probiotics are "healthy" microorganisms (bacteria, yeast) that can be taken by mouth. These probiotics do not by themselves cure C. difficile infection, but they may be beneficial in selected situations. 66
4 th generation: Cefepime • Good empiric choice for many nosocomial infections • De-escalate therapy if possible • Better Gram + activity compared to 3 rd genera • MAY INDUCE LESS RESISTANCE in GNRs than 3 rd genera 67
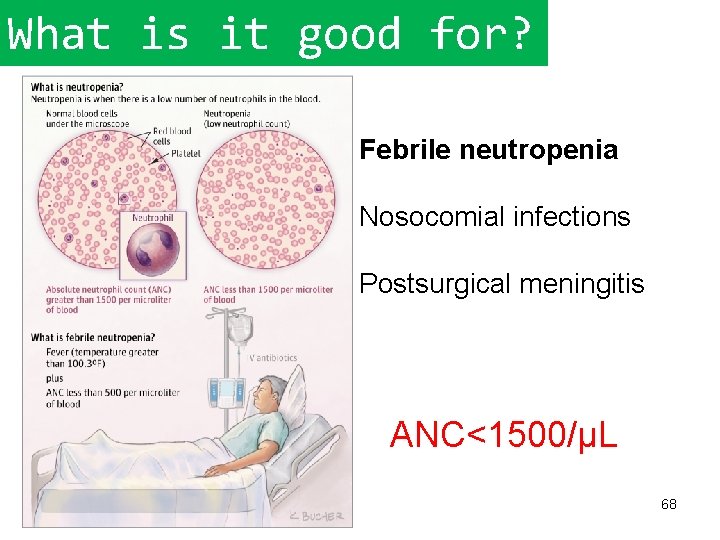
What is it good for? Febrile neutropenia Nosocomial infections Postsurgical meningitis ANC<1500/µL 68
5 th generation: Ceftaroline, Ceftolozane Complicated skin and soft tissue infections and community-acquired pneumonia Gram – activity is LESS THAN 4 th genera 69
Ceftolozan + Tazobactam Ceftolozane is a novel cephalosporin antibiotic, developed for the treatment of infections with gramnegative bacteria that have become resistant to conventional antibiotics. It was studied for urinary tract infections, intra-abdominal infections and ventilator 70 associated bacterial pneumonia
- Slides: 70