Basics of Anatomy and Tissue Injuries Anatomical Position
Basics of Anatomy and Tissue Injuries
Anatomical Position • Anatomic Position: Refers to an erect stance with the arms at the sides and the palms of the hands facing forward • The body moves in relation to planes ▫ Frontal ▫ Sagittal ▫ Transverse • Refer back to Med Term notes/packets for help
Body Tissues • Athletic injury usually involved injury to ▫ ▫ ▫ Skin Bone Cartilage Muscle Tendons Ligaments �Basically everything
Skin • Outermost surface of the body • First line of defense against ▫ ▫ ▫ Insects Air Dirt Bacteria Blunt force • Keeps body fluids in • Senses agitators • Secretes sweat and oily substance
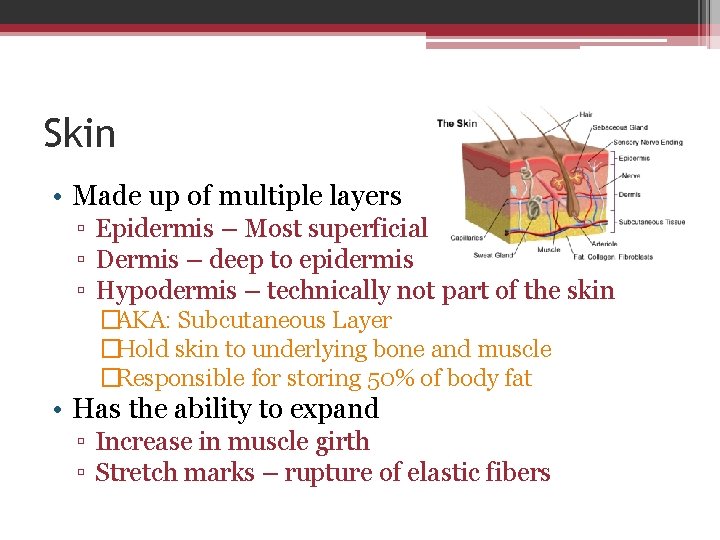
Skin • Made up of multiple layers ▫ Epidermis – Most superficial ▫ Dermis – deep to epidermis ▫ Hypodermis – technically not part of the skin �AKA: Subcutaneous Layer �Hold skin to underlying bone and muscle �Responsible for storing 50% of body fat • Has the ability to expand ▫ Increase in muscle girth ▫ Stretch marks – rupture of elastic fibers
Bones • 3 primary functions ▫ Protect vital organs ▫ Create movement ▫ Metabolically active �Produce RBC �Store minerals �Cal, Phos • Also provide a degree of protection for nerve and vessels that run length of bone
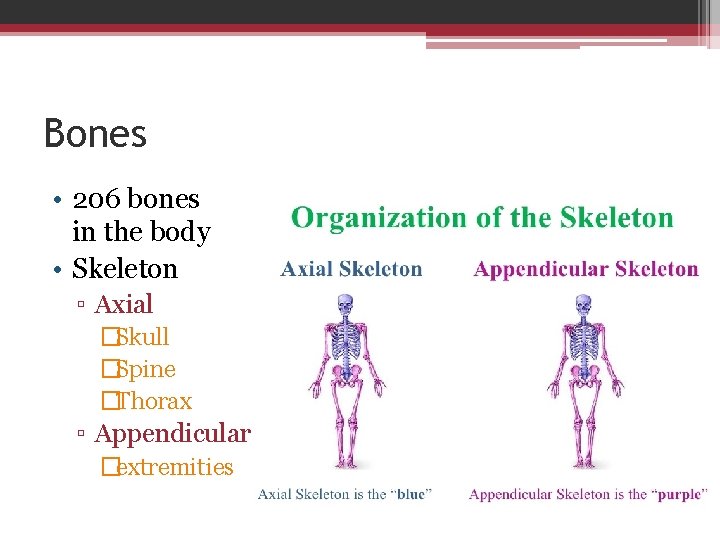
Bones • 206 bones in the body • Skeleton ▫ Axial �Skull �Spine �Thorax ▫ Appendicular �extremities
Surface Anatomy Lab • Turn to page 34 • Using figure 3. 3, place adhesive dots on various areas of the skeleton and number them • Using correct medical terminology, write now the name of the bone under the numbered adhesive and identify it’s location ▫ E. g. #3 Ulna; distal to Humerus, proximal to carpals
Bone categories • Bones come in several shapes and sizes ▫ ▫ Long (femur) Short (metacarpal) Flat (scapula) Irregular (vertebra) • Features ▫ Shaft - Diaphysis ▫ Epiphysis – growth plate �Spongy during adolescence

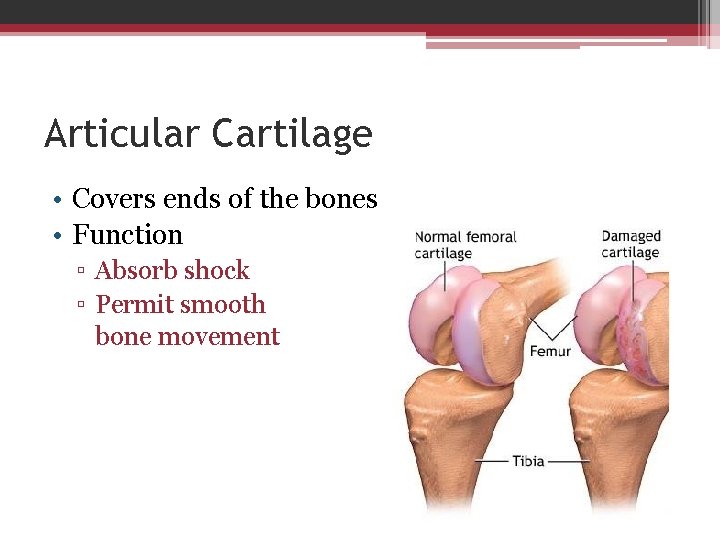
Articular Cartilage • Covers ends of the bones • Function ▫ Absorb shock ▫ Permit smooth bone movement
Muscles, Tendons, Ligaments • Muscles – contract to create ▫ ▫ ▫ Acceleration Deceleration Stop movement Maintain normal postural alignment Produce heat • Tendons – connect MUSCLE to BONE • Ligaments – connect BONE to BONE
Your Aging Body • As infants: ▫ Bones are cartilaginous • As adults ▫ Bones harden and become strong ▫ Muscles are composed of fibers with high excitability and elasticity • As elders ▫ Bones become brittle ▫ Muscle degenerates and replaced by fibrous connective tissue
Classification of Joints • 3 different classifications: ▫ Diarthrodial ▫ Amphiarthrodial ▫ Synarthrodial

Diarthrodial • AKA Synovial joints • Have excellent mobility • Components: ▫ Joint Capsule (sleeve-like ligament that surround entire joint) ▫ Synovial membrane (slick lining on the inside of the capsule) ▫ Hyaline cartilage (thin layer of cushioning at the ends of the bone) ▫ Ligaments
Diarthrodial • Divided into several types: ▫ Hinge joints �Knee and elbow – move back and forth like hindges on a door ▫ Multiaxial �Shoulder and hip (AKA ball and socket) – move alone many axes
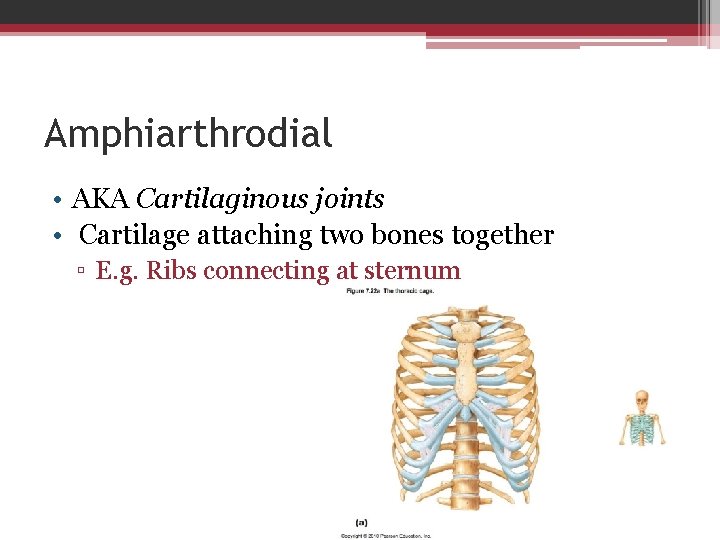
Amphiarthrodial • AKA Cartilaginous joints • Cartilage attaching two bones together ▫ E. g. Ribs connecting at sternum

Synarhtrodial • AKA Fibrous Joints • Held together by tough connective tissue • Immovable ▫ E. g. – bones of the skull; tibia/fibula

Soft Tissue Injuries • Wounds, Strains, Sprains ▫ Bleed, become infected, produced extra fluid • Classification: Acute ▫ Occurs suddenly as a result of a high amount of force applied to the tissue over a short time (milliseconds-seconds)
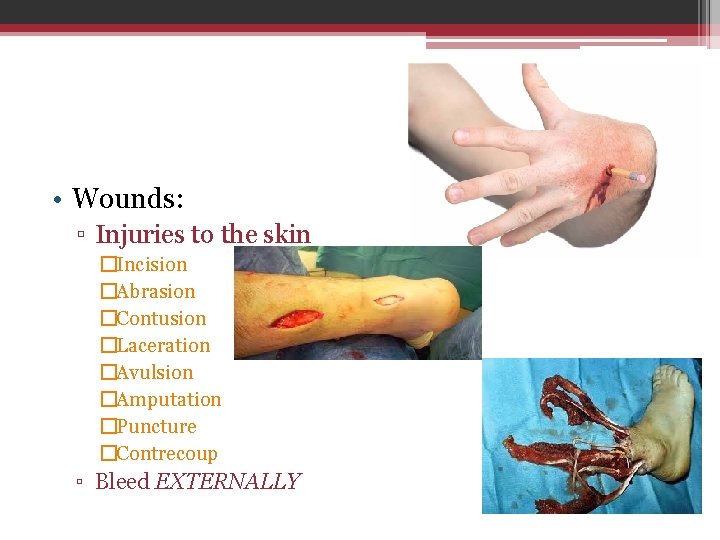
• Wounds: ▫ Injuries to the skin �Incision �Abrasion �Contusion �Laceration �Avulsion �Amputation �Puncture �Contrecoup ▫ Bleed EXTERNALLY
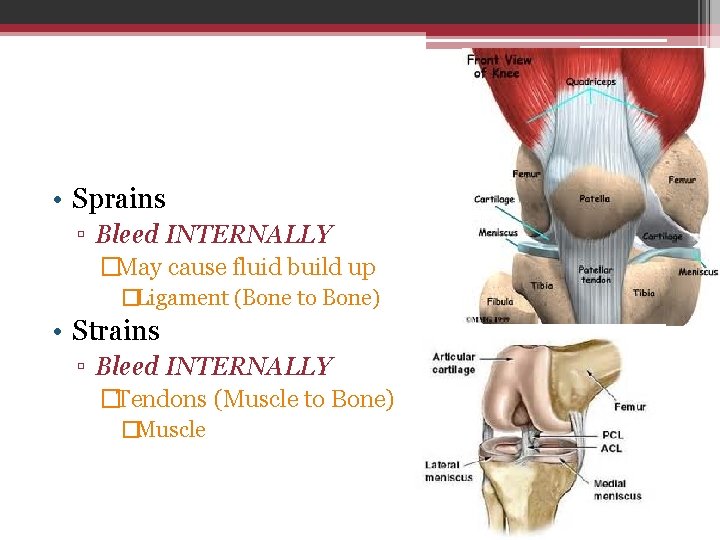
• Sprains ▫ Bleed INTERNALLY �May cause fluid build up �Ligament (Bone to Bone) • Strains ▫ Bleed INTERNALLY �Tendons (Muscle to Bone) �Muscle
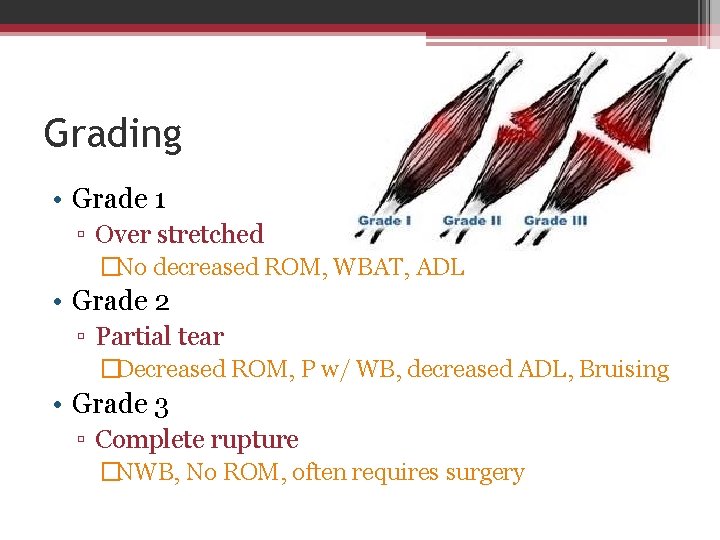
Grading • Grade 1 ▫ Over stretched �No decreased ROM, WBAT, ADL • Grade 2 ▫ Partial tear �Decreased ROM, P w/ WB, decreased ADL, Bruising • Grade 3 ▫ Complete rupture �NWB, No ROM, often requires surgery
Chronic Soft Tissue Injury • Chronic is the result of lesser forces being applied over a long period of time (weeks to months) ▫ Often the product of overuse • Types: ▫ ▫ Synovitis Bursitis Myositis Fasciitis
• Synovitis ▫ Inflammation of the synovial joint lining �Acute injury that never healed or from repeated join injury • Bursitis ▫ Inflammation of the bursa sac �Tends to swell
• Myositis ▫ Chronic Inflammation of the muscle (Myo= Muscle) �Sore, tender, mild swelling, excessively sore • Fasciitis ▫ Inflammation of the Thick, rough connective tissue that surrounds the muscles �Thicken, swollen, painful
Stages of Soft-Tissue Healing • Stage 1: Acute Inflammatory ▫ Cells die from being ripped apart & from being cut off from food and oxygen supply �Fresh blood bring chemicals to begin healing process �Phagocytes, Leukocytes, Platelets (Vocab) ▫ Acute stage lasts 48 hrs
• Stage 2: Repair ▫ Injured area filled with fresh blood, cells, and chemicals to rebuild the damage. �Fibroblasts for scar tissue 6 wks-3 mo depending on severity • Stage 3: Remodeling ▫ Takes up to 1 year+
Factors That Slow Healing • Poor Blood Supply • Poor nutrition • Illness/disease ▫ Diabetes • Medications ▫ Corticosteriods �Chems made in the body to help reduce inflammation �Synthetic versions are available (i. e. Advil) • Infection

Bone Injuries • Dislocation ▫ Force displaces two ends of articulating bone causes them to separate ▫ Disloc also causes: �Avulsion fx �Strains/sprains �Disruptions of blood flow �Disruption of nerve conduction ▫ Present w/ obvious deformity, P, NO ROM
• Fractures ▫ Failure point �Vary with age, bone structure, medical predisposition ▫ (osteoporosis) ▫ Name according to type of impact/how failure occurs �Broken/cracked/chipped/hairline fx ▫ 13 types of fractures – pg 46 to 49

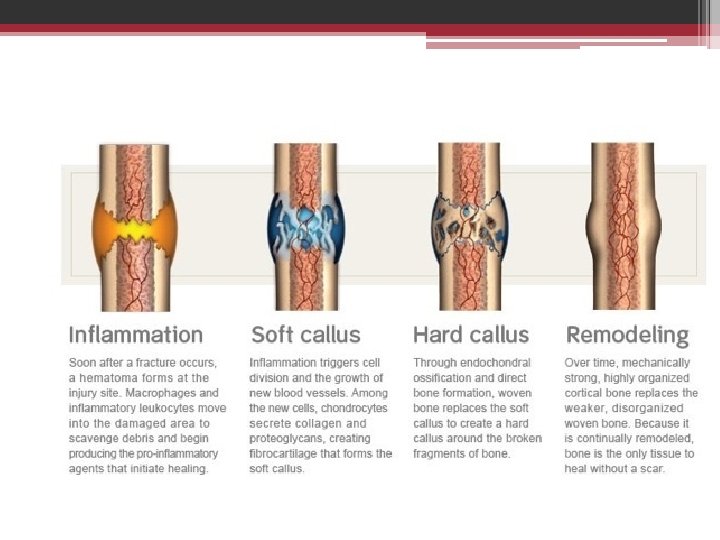
Stages of Bone Healing • Stage 1: Acute ▫ injury causes break which causes bleeding at site �Osteoclasts begin to eat the debris to absorb back in the body �Osteoblasts begin to add new layers to outside of bone �Lasts 4 days
• Stage 2: Repair ▫ Soft Callus forms internally and externally to hold fractured ends together ▫ Eventually turns to hard callus ▫ Process turning callus to bone begins at 3 weeks and last approx 3 mo
• Stage 3: Remodeling ▫ Takes several years to complete �Callus is reabsorbed and replaced with bone �Electrical stimulation can be applied to fx that are not healing ▫ Due to minerals in bone ▫ Fractures can be nonunion �Only in WB bones (leg, foot, scaphoid most common sites) �Painful, loss of ROM, necrosis
• Define terms found on pages 42 and 43 • Create a summary of each of the 13 fractures • Chapter 4 worksheet
- Slides: 38