BASIC POISON MANAGEMENT John F Haynes Jr MD
BASIC POISON MANAGEMENT John F. Haynes, Jr. , MD Associate Professor Emergency Medicine/Medical Toxicology Texas Tech University HSC El Paso
History ¨ Ebers Papyrus 1500 BC ¨ Poison Arrows of Greeks, India, Masi ¨ Dioscorides (40 – 80 AD) “Materia Medica” ¨ Renaissance: Paracelsus; Borgia family; “age of the poisoner” ¨ Bonaventure Orfelia
Paracelsus ¨ Phillippus Theophrastus Aureolus Bombastus von Hohenheim (1493 -1541) ¨ “What is there that is not poison? All things are poison and nothing is without poison, only the dose permits something not to be poisonous”
Poison Control Centers ¨ Post WW II proliferation of drugs and chemicals ¨ Chicago 1953 ¨ AAPCC Certification as of 1978 ¨ Regional Poison Centers ¨ Texas Poison Center Network

Identification

Poison ¨ Any agent capable of producing a deleterious response in a biological system.

General ¨ Poisoning: to injure or kill with chemical substance. Usually unintentional ¨ Overdose: Usually implies intent

General ¨ 2 to 3 million human exposures reported to AAPCC data collection base in U. S. /year ¨ 100 to 200 fatalities ¨ 7 to 15% of all ED visits ¨ 10 to 20% of adult admissions ¨ 5% of Pediatric admissions
General ¨ 68% of Poison Center calls ¨ ¨ ¨ 0 -19 y/o 80% of these are < 6 y/o 9% of Pediatric exposures are 13 -19 y/o Of the < 6 y/o 99% are unintentional 50% of adolescent exposures are unintentional 55% of Pediatric exposures are nonpharmaceuticals

General ¨ “Toddlers” ¨ Usually accidental ¨ One substance ¨ Substance usually non- toxic ¨ Small amount ¨ Present early after ingestion ¨ Repetitive risk? 30% happens again

Outcome AGE: Minor Mod. Major Death 0 -5 93 1 0. 05 0. 003 6 -12 86 2 0. 1 0. 005 13 -19 75 7 0. 04 All children (0 -19) 91 2 0. 1 0. 006
Identification ¨ Exact name of the product ¨ Date on container ¨ When purchased ¨ Consult current reference (Poison Center, MSDS, etc) ¨ CHEMTREC 800 -424 -9300; www. cmahq. com ¨ National Poison Control Number is : ¨ 1 -800 -222 -1222 ¨ MSDS-SEARCH www. msdssearch. com/DBLinks. htm
History ¨ Often difficult (toddler, suicidal, abuse) ¨ Type of substance ¨ Amount ¨ Time since ingestion ¨ Allergies/Illnesses ¨ “Non – toxic” exposure? ?

History ¨ Number of pills missing ¨ Amount of liquid missing ¨ History remains consistent between observers ¨ Presentation is consistent with history ¨ Child’s level is consistent ¨ Any exposure < 1 THINK Abuse?
Clinical Evaluation ¨ Lab: CMB, CMP, serum osmolality, ABG? , EKG UA with drug screen ¨ CXR, KUB (free air, body packer/stuffer) ¨ CHIPES: Chloral hydrate, heavy metals, iron, psychotropics, enteric coated tabs. ) ¨ Drug levels: Digoxin, APAP, ASA, ETOH, iron, valproic acid and other anticonvulsants, lithium
Clinical Evaluation ¨ Osmolar Gap=2 Na+Glu/18+BUN/2. 8 ¨ Anion Gap=Na – (Cl+HCO 3) Widened in: Methanol, Ethylene Glycol, Salicylates, Uremia, DKA, Iron, Isoniazid, metformin ¨ Volume of Distribution A(L/kg)=D/pc
Management ¨ Treat the patient ¨ ABC’s; assess vital signs including mental status ¨ Consider use of “coma protocol” ¨ Rapid physical exam “toxidrome? ”

Toxidromes ¨ Anticholinergic ¨ Sympathomimetic ¨ Opioid ¨ Cholinergic (Anticholinesterase) ¨ Sedative – Hypnotic ¨ Withdrawal
Anticholinergic “Hot as a hare, blind as a bat, dry as a bone, red as a beet, mad as a hatter, bloated as a bladder” ¨ Seizures and coma may occur ¨ Antihistamines, Atropine, antispasmotics, muscle relaxants, tricyclic antidepressants, antiparkinson meds. , plants
Sympathomimetic ¨ Diaphoresis, tachycardia, tachypnea, hyperthermia, hypertension, mydriasis, restlessness, tremors, insomnia ¨ Dysrhythmias and seizures may occur ¨ Difficult to distinguish from anticholinergic ¨ Cocaine, amphetamines, caffeine, OTC’s, plants (ma huang)
Opioid ¨ Clasic triad: Mental status depression, respiratory depression, pinpoint pupils ¨ Morphine, heroin, fentayl, other synthetics ¨ Meperidine, propoxyphene, Tramadol, Dextromethorphan ¨ Central alpha 2 receptor agonists: clonidine

Cholinergic ¨ “SLUDGE” salivation, lacrimation, urination, diarrhea, GI distress, emesis ¨ Miosis, bronchorrhea, bronchoconstriction, vagal tone, are muscarinic effects ¨ Nicotinic: fasciculations, pallor, weakness, hypertension, mydriasis, tachycardia ¨ CNS: ataxia, headache, aggitation, delirium, seizures
Sedative-Hypnotic ¨ Mental status depression, hypotension, respiratory depression, hypothermia, ataxia, slurred speech ¨ Includes Barbiturates, benzodiazepines, etc. ¨ Ethanol “fits” into this class, Many other drugs have similar effects
GI Emptying ¨ Ipecac was used for home management of mild possibly toxic ingestions ¨ Gastric lavage: early, selectively, properly ¨ Whole bowel irrigation ¨ Activated charcoal
Toxin Elimination ¨ Manipulation of p. H ¨ Dialysis - VD= A/SL; protein binding; MW ¨ Exchange transfusion ¨ Multiple dose activated charcoal ¨ Chelation ¨ “Antidotes” ¨ Toxin specific FAB Fragment

Danger in Small Quantities ¨ Codeine 15 mg/Kg ¨ Benadryl 25 mg/Kg ¨ Chloroquine 20 mg/Kg ¨ Methanol 0. 6 ml/Kg ¨ Imiparamine 15 mg/Kg ¨ Meth Salicylate 200 mg/Kg ¨ Benzocaine 10 mg/Kg 5 tablets 1 tablet 1 tsp 1 tablet <1 tsp

Other Medications ¨ Oral hypoglycemics ¨ Calcium channel blockers ¨ Beta adrenergic blockers ¨ Ethanol ¨ Tylenol
Case # 1 ¨ 13 year old female presents, tearful, labile BIB her parents after argument parent’s keeping her home from going out with her 23 year old boyfriend. ¨ Threatened to “kill herself” ¨ Locked herself in bathroom, brought in after father broke the door of bathroom to remove her.
Case # 1 ¨ What do you want to do 1 st? ¨ Initial management? ¨ Testing? ¨ What are the possibilities?
Acetaminophen ¨ Over 100, 000 calls per year ¨ Most common hospitalization from OTC’s ¨ Toxicity less common in children (< 5 y/o) ¨ Adults: APAP glucuronidation exceeds sulfation ( 60% to 30%) children may have reverse ratio ¨ Increased glutathione capability of children
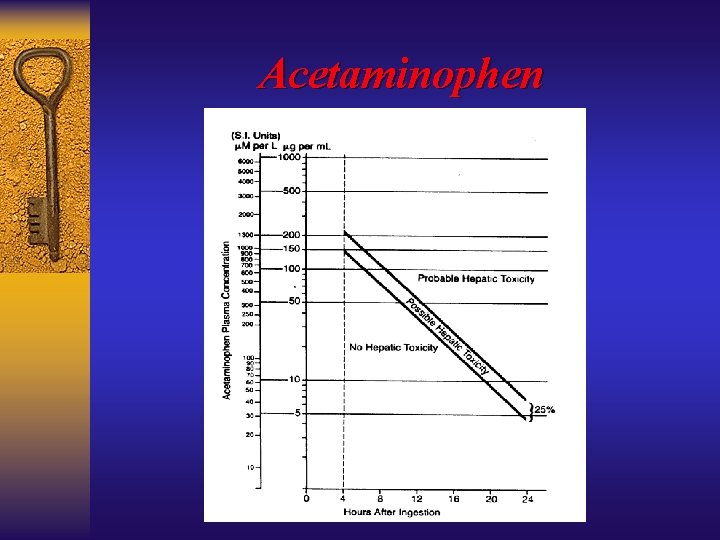
Acetaminophen
Acetaminophen ¨ Acute ingestion: ¨ > 7. 5 g in adult or > 150 mg/Kg in child ¨ 4 hour level > 150 micg/m. L ¨ If AST is elevates ¨ If time of ingestion unknown and level is >10 micg/m. L
Acetaminophen ¨ Chronic ingestion: ¨ Hepatotoxicity from repeated dose is rare ¨ Occurs in infants (febrile) receive excessive dose; chronic alcohol users; those on P-450 inducing medications ¨ Get APAP and AST levels ¨ More likely to be symptomatic on presentation ¨ > 75 mg/Kg in 24 hour period
Acetaminophen ¨ Clinical Presentation: ¨ Phase I: (0. 5 -24 hrs) Malase, anorexia, N/V, palor, diaphoresis ¨ Phase II: (24 -72 hrs) URQ abd. Pain, elevation of enzymes. ¨ Phase III: (72 -96 hrs) Coagulopathy, jaundice, renal failure, encephalopathy ¨ Phase IV: (4 d-2 wks) Resolution

Acetaminophen ¨ Management: ¨ Measure AST during treatment, if elevates, follow PT, if > 1000 IU/L, follow BUN and Creatinine ¨ If liver failure suspected follow acid base status and glucose. ¨ p. H <7. 3, PT>100 (1. 8 Xcontrol), Cr. >3. 3, and grade III or IV encephalopathy = TRANSPLANT?
Acetaminophen ¨ Treatment: ¨ GI Decontamination if < one hour ¨ Activated charcoal? ¨ N-Acetylcysteine ¨ Control N/V ¨ Supportive care ¨ Watch for bleeding and hypoglycemia ¨ Short course NAC?
Acetaminophen ¨ USE of IV NAC? ¨ Unable to keep down oral dose ¨ Liver Failure ¨ Use with in-line 0. 22 micg filter ¨ Actadose ¨ 150 mg/kg in 200 cc D 5 W x 20 min ¨ 50 mg/kg in 500 cc x 4 hours ¨ 100 mg/kg x 16 hours
Case # 2 ¨ 17 y/o male with schizophrenia presented with thirst. Was tachycardic, diaphoretic, tachypneic, with temp. 100. 3. Complains of “hearing strange noises” ¨ He is taking Prozac and risperidone ¨ What initial steps in management? ¨ Any lab?
Case # 2 ¨ Lab: ¨ Ph: 7. 44; Pco 2 28 mm Hg; Po 2 70 mm Hg ¨ Urine ph of 5. 0 ¨ Anion gap of 17 ¨ Cr. Of 1. 5 mg/d. L ¨ CXR patchy infiltrates with nl cardiac silhouette ¨ Salicylate level 78 mg/d. L
Salicylates ¨ Toxic effects: ¨ Central stimulation of respiratory centers ¨ Dehydration, uncoupling of oxidative path. ¨ Interruption of glucose and fatty acid metab. ¨ Alter platelet function
Salicylates
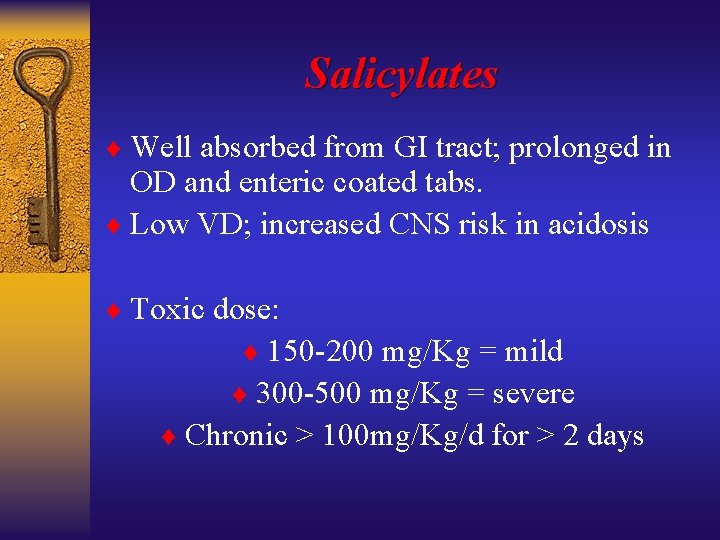
Salicylates ¨ Well absorbed from GI tract; prolonged in OD and enteric coated tabs. ¨ Low VD; increased CNS risk in acidosis ¨ Toxic dose: ¨ 150 -200 mg/Kg = mild ¨ 300 -500 mg/Kg = severe ¨ Chronic > 100 mg/Kg/d for > 2 days
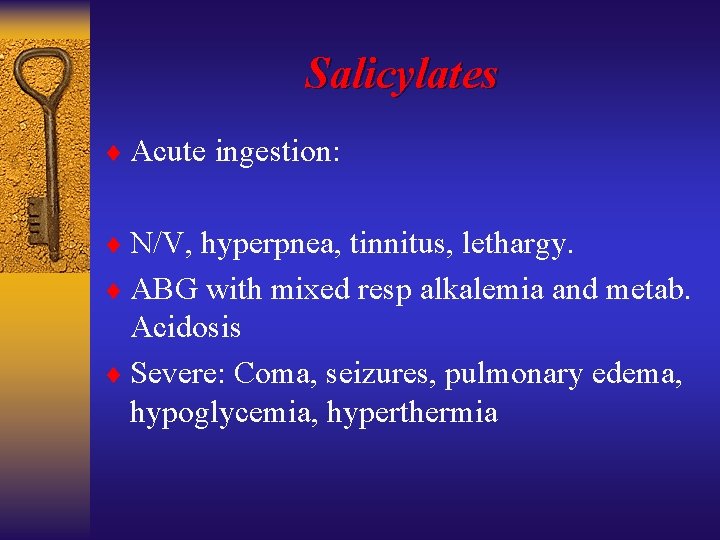
Salicylates ¨ Acute ingestion: ¨ N/V, hyperpnea, tinnitus, lethargy. ¨ ABG with mixed resp alkalemia and metab. Acidosis ¨ Severe: Coma, seizures, pulmonary edema, hypoglycemia, hyperthermia
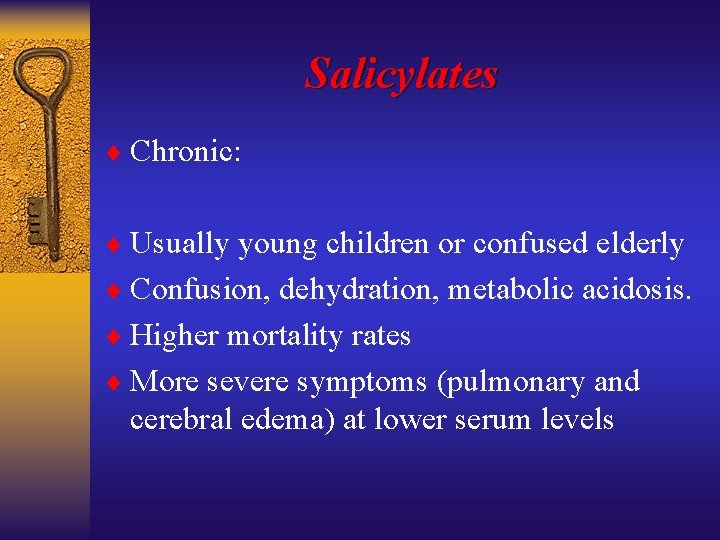
Salicylates ¨ Chronic: ¨ Usually young children or confused elderly ¨ Confusion, dehydration, metabolic acidosis. ¨ Higher mortality rates ¨ More severe symptoms (pulmonary and cerebral edema) at lower serum levels
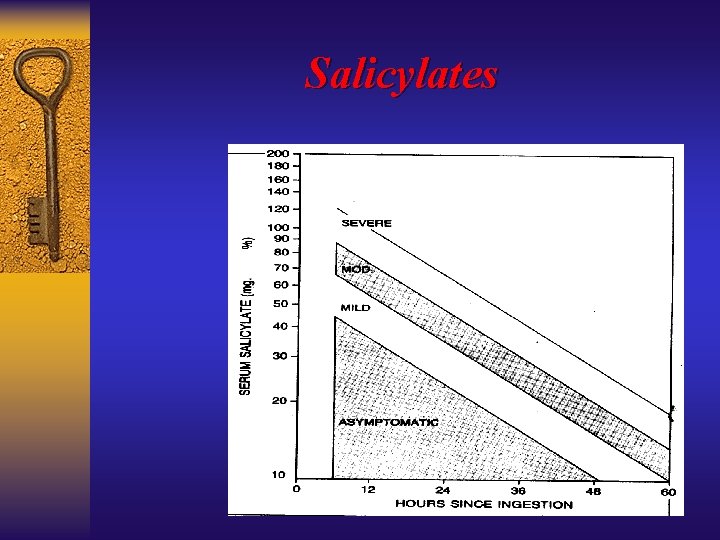
Salicylates ¨ Levels > 900 -1000 mg/L ( 90 -100 mg/d. L)= severe toxicity (Done nomogram not helpful) ¨ Chronic? > 600 mg/L ( 60 mg/d. L) + metabolic acidosis and altered mental status ¨ Look for anion gap, check glucose, BUN, creatinine, PT, CXR, ABG’s
Salicylates ¨ Treatment: ¨ ABC’s; avoid respiratory acidosis, treat coma, seizures, hyperthermia, pulmonary edema as they occur. ¨ Treat acidosis with bicarb. (> 7. 4) ¨ Fluids (carefully); Charcoal? ¨ Lavage?
Salicylates ¨ Treatment (Continued): ¨ “Urinary Alkalinization” ¨ Add 100 m. Eq Na. Bicarb to 1 L od 5%W infuse at 3 -4 m. L/Kg/h ¨ Add potassium (20 – 30 m. Eq) ¨ Maintain serum p. H between 7. 45 to 7. 55
Salicylates ¨ Hemodialysis: ¨ Serum levels > 1200 mg/L (120 mg/d. L) ¨ Renal Failure ¨ Pulmonary edema ¨ Progressive deterioration in vital signs ¨ CHF ¨ Severe acid base problem despite tx
Others ¨ Iron: ¨ Elemental Fe level (eg: Ferrous sulfate=20%) ¨ > 10 -20 mg/Kg ¨ 300 -500 micg/d. L = toxic ¨ > 1000 micg/d. L = motality ¨ Glucose and WBC count? ¨ Watch for 6 hours ¨ Deferoxamine IV 15 -20 mg/Kg/h
Others ¨ Carbon Monoxide ¨ Carboxyhemoglobin level may be deceptive ¨ Look for “cluster” ¨ 100% oxygen ¨ Hyperbarric treatment?
Others
- Slides: 51