Basic Pathology Basic Pathology Phase 2 a Revision
Basic Pathology
Basic Pathology Phase 2 a Revision Session Sara Howells & Katie Edwards 6 th march The Peer Teaching Society is not liable for false or misleading information…
What is inflammation? • Inflammation is the local physiological response to tissue injury. Why does inflammation occur? Occurs to bring all the essential cells for healing to the area of tissue damage.
Effects of inflammation Benefits: • Destruction if invading microbes • Can also have harmful effects – Digestion of normal tissues – Swelling – Inappropriate inflammatory response
2 main types of inflammation • Acute v Chronic • What is the difference? – Duration – Cells involved – Cause
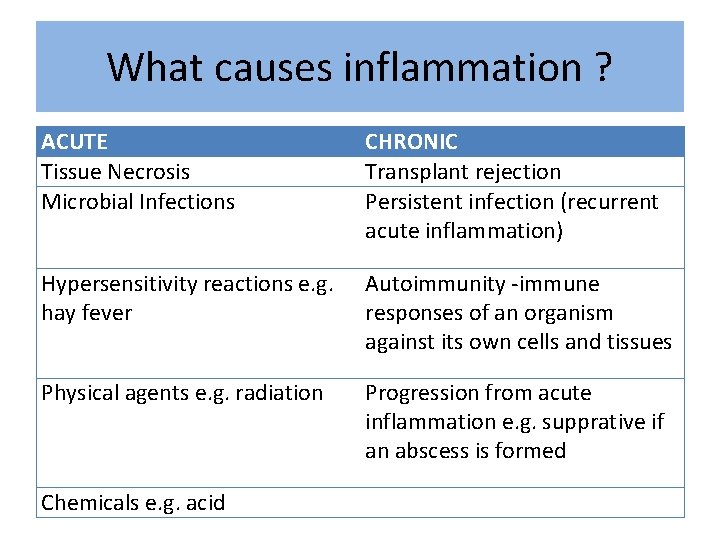
What causes inflammation ? ACUTE Tissue Necrosis Microbial Infections CHRONIC Transplant rejection Persistent infection (recurrent acute inflammation) Hypersensitivity reactions e. g. hay fever Autoimmunity -immune responses of an organism against its own cells and tissues Physical agents e. g. radiation Progression from acute inflammation e. g. supprative if an abscess is formed Chemicals e. g. acid
5 cardinal sign of Acute Inflammation – Swelling • Due to oedema – accumulation of fluid in the extravascular space – Redness • Due to dilation of small blood vessels within the damaged area – Heat • Due to increased blood flow (hyperaemia) – Pain • Due to stretching and distribution of the tissues to inflammatory oedema – Loss of function
Examples of inflammation • • • Septic Arthritis Cellulitis Appendicitis Acne Asthma
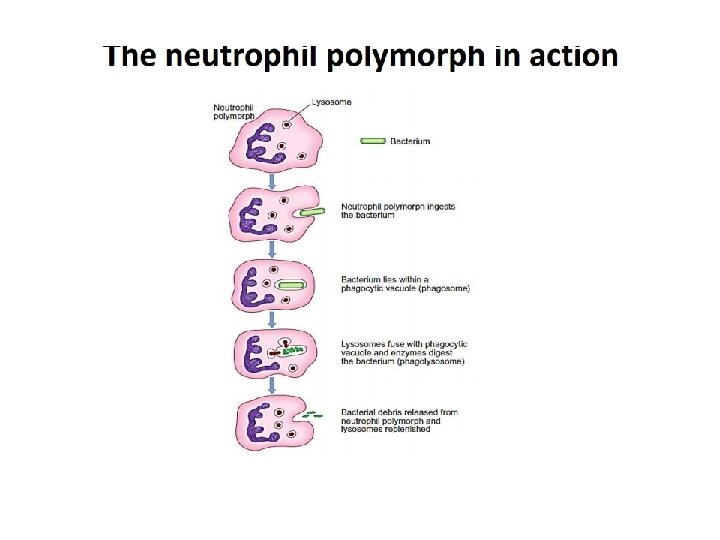
What are the key cells involved in acute inflammation? • Neutrophil polymorphs = hallmark of inflammation – Phagocytose pathogens • Phagocytosis: pathogens ingested to form phagosome, lysosomes released from neutrophils to kill pathogens, and then expelled from phagolysosome • Macrophages – secrete chemical mediators essential for chemotaxis
Chemical Mediators of Acute Inflammation • Spread the acute inflammatory response following the injury of a small area • Histamine and Thrombin – cause neutrophil adhesion to endothelial surface
What are the 3 main stages of acute inflammation? 1. Changes in vessel calibre – vasodilation brings blood and cells into the site of inflammation 2. Fluid exudate - the vasodilation and chemical mediators (e. g. histamine, bradykinin, NO, C 5 a) make vessels more permeable.
… continued 3. Cellular exudate – accumulation of neutrophil polymorphs into the extracellular space Later stages of Acute inflammation: Chemotaxis – attraction of cells to site through release of chemicals: process by which neutrophils move to inflammation site, attracted to inflammatory mediators released - Chemotaxis
Outcomes of Acute inflammation • Resolution – complete restoration of the tissues to normal • Suppuration – formation of pus • Organisation – When tissue is replaced with granulation tissue as part of the healing process • Progression to chronic inflammation
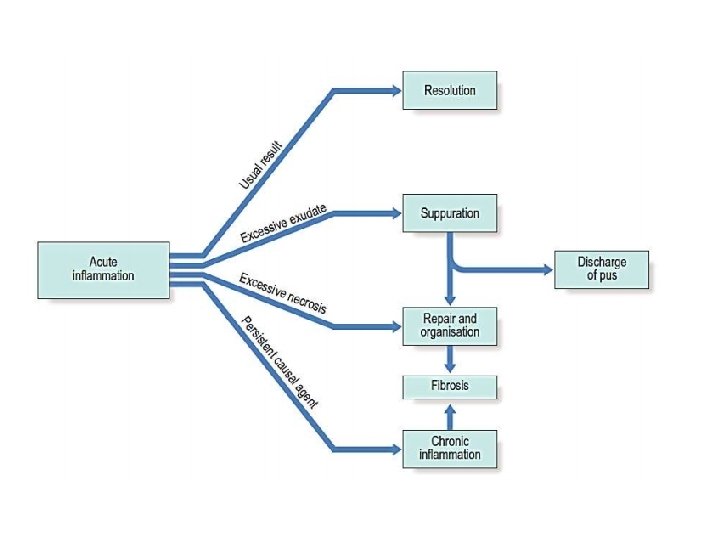
Chronic Inflammation • Not ideal – it’s an unnecessary when your body cannot turn of the immune response. • Unresolved acute inflammation = chronic inflammation e. g. ulcers, pulmonary fibrosis etc
What causes chronic inflammation? • Primary: – Agent resistant to phagocytosis, e. g. TB, leprosy – Agent indigestible, i. e. fat, bone, asbestos, silica – Autoimmune diseases – Crohn’s disease/ulcerative colitis – Transplant rejection •
What cells are involved? • Lymphocytes, plasma cells and macrophages • Less swelling than acute (less exudate formation) • Inflammation and repair is occurring at the same time • Fibrosis (scar tissue formation) = key feature.
What are the role of each of these cells? • Plasma Cells: What do they do and where are they derived from? – derive from B lymphocytes, produce antibodies • B-lymphocytes – differentiate into plasma cells to make antibodies • T-lymphocytes – cell-mediated immunity
Define Granuloma? • AGGREGATE OF EPITHELIOID HISTIOCYTES These cells excrete ACE, which therefore is a blood marker if someone has systemic granulomatosis disease Can you name 4 examples.
THROMBOSIS AND INFARCTION
What is a thrombus? • Solid mass of blood constituents • Not necessarily a bad things – essential part of healing and repair. • Physiological - as part of haemostasis (to prevent bleeding outside vessels) • Pathological - when there is an imbalance in the blood coagulation system
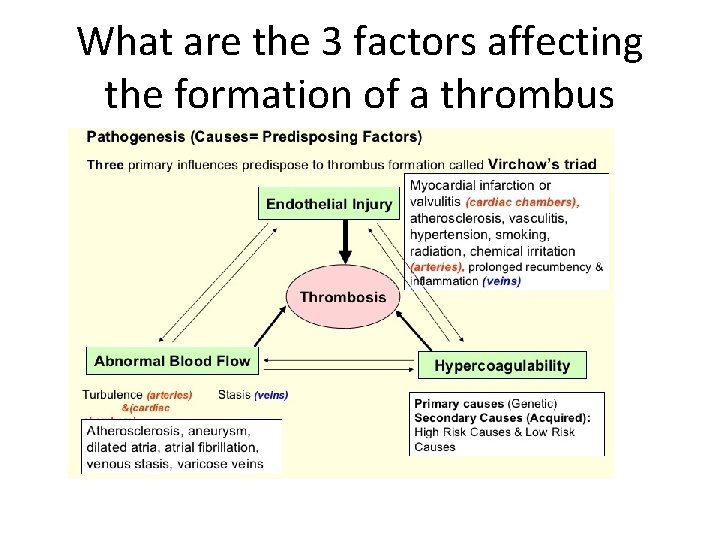
What are the 3 factors affecting the formation of a thrombus
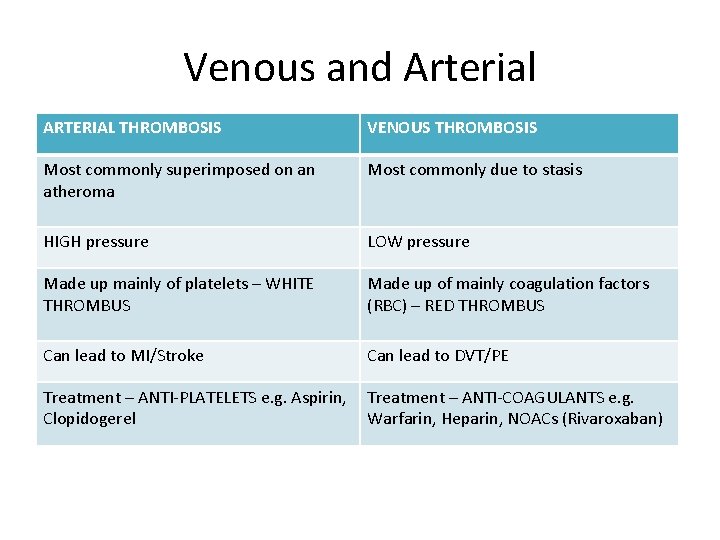
Venous and Arterial ARTERIAL THROMBOSIS VENOUS THROMBOSIS Most commonly superimposed on an atheroma Most commonly due to stasis HIGH pressure LOW pressure Made up mainly of platelets – WHITE THROMBUS Made up of mainly coagulation factors (RBC) – RED THROMBUS Can lead to MI/Stroke Can lead to DVT/PE Treatment – ANTI-PLATELETS e. g. Aspirin, Clopidogerel Treatment – ANTI-COAGULANTS e. g. Warfarin, Heparin, NOACs (Rivaroxaban)
Atherosclerosis • What vessels does it effect? • Name 5 Risk factors for atherosclerosis – try to split them into non modifiable and modifiable • Large and Medium • Risk factors: Modifiable - Smoking, hypertension, hyperlipidaemia, diabetes Non-Modifiable - Age, male sex, post menopausal, family history
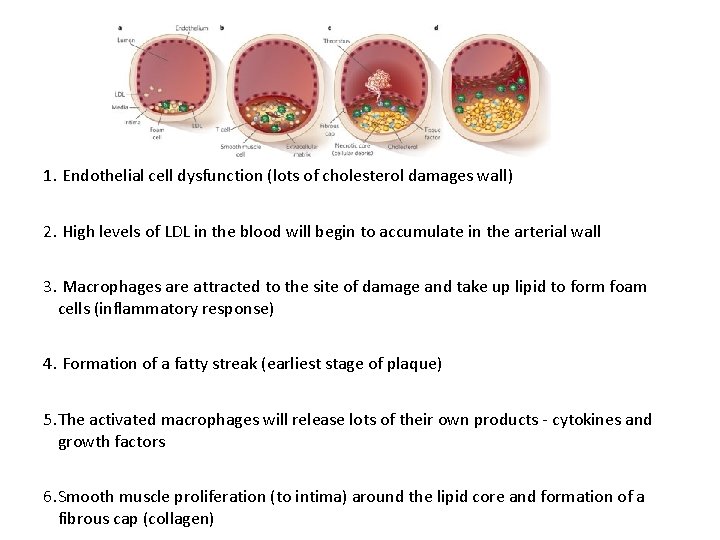
1. Endothelial cell dysfunction (lots of cholesterol damages wall) 2. High levels of LDL in the blood will begin to accumulate in the arterial wall 3. Macrophages are attracted to the site of damage and take up lipid to form foam cells (inflammatory response) 4. Formation of a fatty streak (earliest stage of plaque) 5. The activated macrophages will release lots of their own products - cytokines and growth factors 6. Smooth muscle proliferation (to intima) around the lipid core and formation of a fibrous cap (collagen)
Complications • Thrombus formation if the unstable cap of the plaque ruptures and partially occludes the vessel. Causing ischaemia of tissue • Embolism: – If the thrombus is dislodged • Plaques can weaken wall of arteries and lead to aneurysm – AAA – DD central abdominal pain esp in Males >55
What is infarction? • Tissue death due to lack of blood supply to the affected area. • Normally due to a disruption in the blood flow e. g fibrous plaque
What is an embolism? • Process of a mass in the blood being carried through the circulation to the place where it gets stuck • Can also include air, fat or foreign body e. g. vegetations of bacteria

- Slides: 30