Basic Concepts of Mechanical Ventilation Sang Heon Park

Basic Concepts of Mechanical Ventilation Sang. Heon Park Interdepartment of Critical Care Medicine Department of Anesthesiology and Pain management Seoul National University Bundang Hospital

Objectives of Mechanical Maintain adequate gas exchange Decrease work of breathing Avoid Complication Ventilation à Indication • During general anesthesia • Uncontrolled hyperventilation • Respiratory Failure or distress
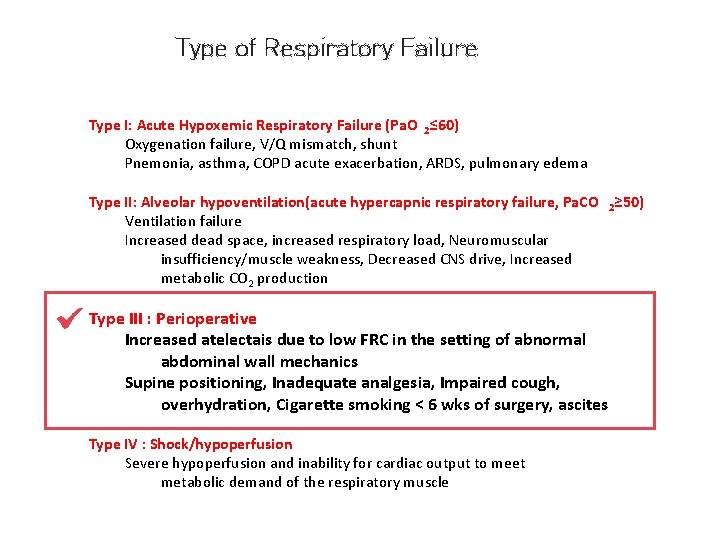
Type of Respiratory Failure Type I: Acute Hypoxemic Respiratory Failure (Pa. O 2≤ 60) Oxygenation failure, V/Q mismatch, shunt Pnemonia, asthma, COPD acute exacerbation, ARDS, pulmonary edema Type II: Alveolar hypoventilation(acute hypercapnic respiratory failure, Pa. CO 2≥ 50) Ventilation failure Increased dead space, increased respiratory load, Neuromuscular insufficiency/muscle weakness, Decreased CNS drive, Increased metabolic CO 2 production Type III : Perioperative Increased atelectais due to low FRC in the setting of abnormal abdominal wall mechanics Supine positioning, Inadequate analgesia, Impaired cough, overhydration, Cigarette smoking < 6 wks of surgery, ascites Type IV : Shock/hypoperfusion Severe hypoperfusion and inability for cardiac output to meet metabolic demand of the respiratory muscle
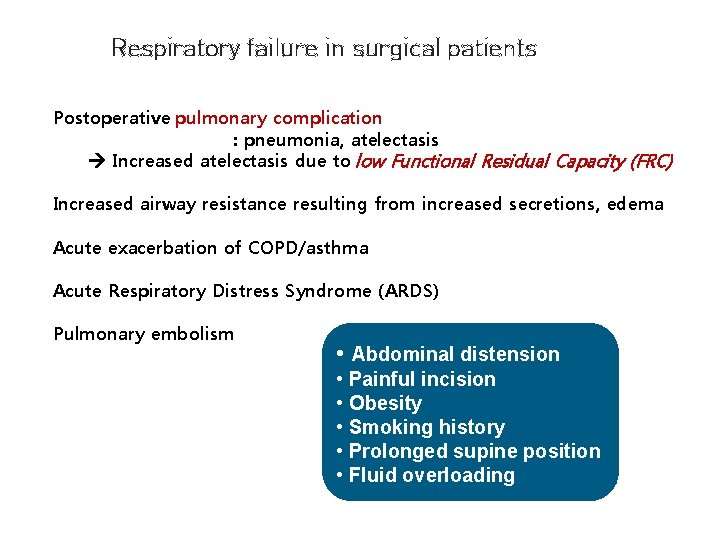
Respiratory failure in surgical patients Postoperative pulmonary complication : pneumonia, atelectasis Increased atelectasis due to low Functional Residual Capacity (FRC) Increased airway resistance resulting from increased secretions, edema Acute exacerbation of COPD/asthma Acute Respiratory Distress Syndrome (ARDS) Pulmonary embolism • Abdominal distension • Painful incision • Obesity • Smoking history • Prolonged supine position • Fluid overloading

Indications for the use of mechanical ventilation Do not delay like most procedures, elective intubation is much safer than emergent intubation Not an act of personal weakness. Airway control in an unstable patient is an act of conviction and is better for the patient Not the “kiss of death. ” Being on the vent does not create vent-dependence
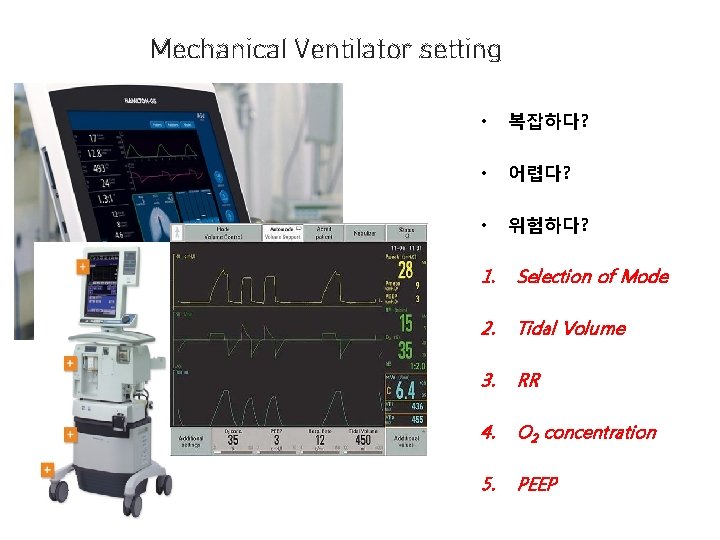
Mechanical Ventilator setting • 복잡하다? • 어렵다? • 위험하다? 1. Selection of Mode 2. Tidal Volume 3. RR 4. O 2 concentration 5. PEEP
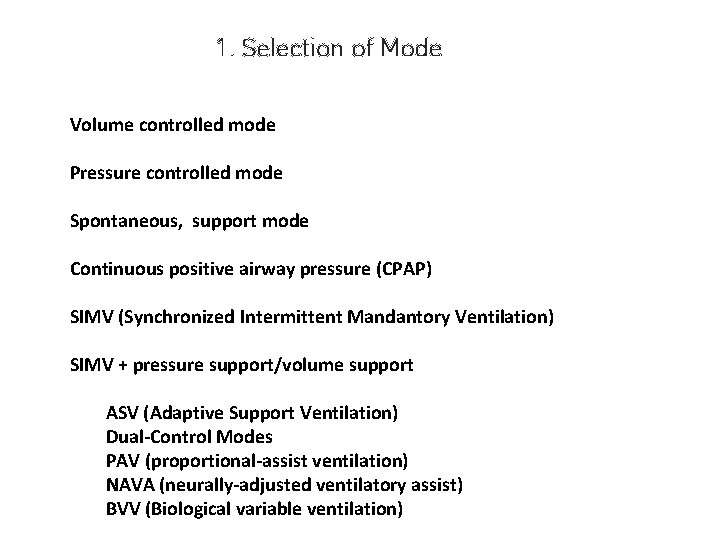
1. Selection of Mode Volume controlled mode Pressure controlled mode Spontaneous, support mode Continuous positive airway pressure (CPAP) SIMV (Synchronized Intermittent Mandantory Ventilation) SIMV + pressure support/volume support ASV (Adaptive Support Ventilation) Dual-Control Modes PAV (proportional-assist ventilation) NAVA (neurally-adjusted ventilatory assist) BVV (Biological variable ventilation)
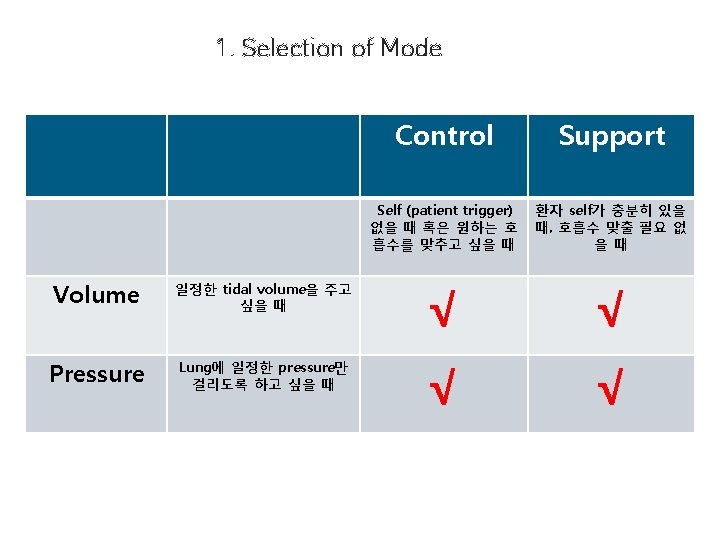
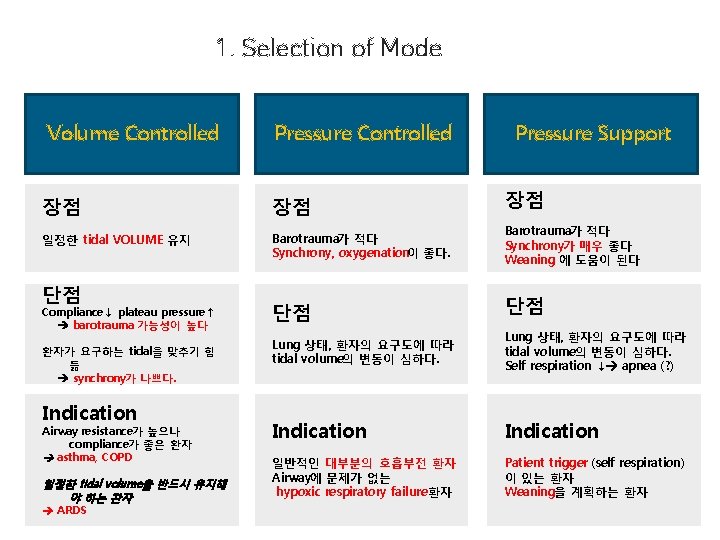
1. Selection of Mode Volume Controlled Pressure Controlled 장점 장점 일정한 tidal VOLUME 유지 Barotrauma가 적다 Synchrony, oxygenation이 좋다. 단점 Compliance↓ plateau pressure↑ barotrauma 가능성이 높다 환자가 요구하는 tidal을 맞추기 힘 듦 synchrony가 나쁘다. Indication Airway resistance가 높으나 compliance가 좋은 환자 asthma, COPD 일정한 tidal volume을 반드시 유지해 야 하는 환자 ARDS 단점 Pressure Support 장점 Barotrauma가 적다 Synchrony가 매우 좋다 Weaning 에 도움이 된다 단점 Lung 상태, 환자의 요구도에 따라 tidal volume의 변동이 심하다. Self respiration ↓ apnea (? ) Indication 일반적인 대부분의 호흡부전 환자 Airway에 문제가 없는 hypoxic respiratory failure 환자 Patient trigger (self respiration) 이 있는 환자 Weaning을 계획하는 환자

SIMV 장점 SIMV Pressure Support mode 보다 안전하다? Synchrony가 좋다? Weaning에 도움이 된다? 단점 복잡하다 Indication ?

SIMV & Weaning SIMV may lead to a longer duration of the weaning process than either T-piece or PSV Crit Care Med 1999; 27: 2331
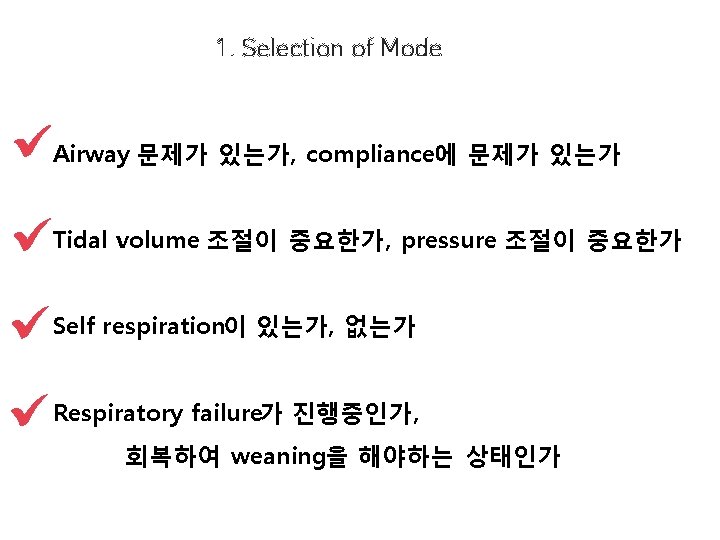
1. Selection of Mode Airway 문제가 있는가, compliance에 문제가 있는가 Tidal volume 조절이 중요한가, pressure 조절이 중요한가 Self respiration이 있는가, 없는가 Respiratory failure가 진행중인가 , 회복하여 weaning을 해야하는 상태인가
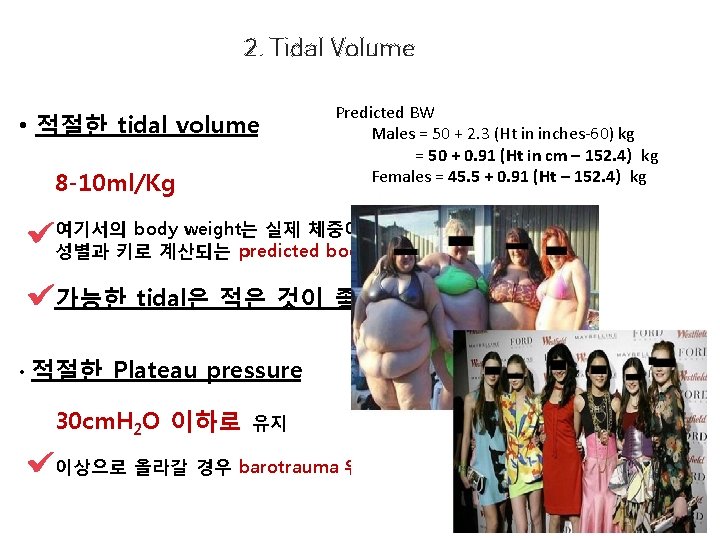
2. Tidal Volume • 적절한 tidal volume 8 -10 ml/Kg Predicted BW Males = 50 + 2. 3 (Ht in inches-60) kg = 50 + 0. 91 (Ht in cm – 152. 4) kg Females = 45. 5 + 0. 91 (Ht – 152. 4) kg 여기서의 body weight는 실제 체중이 아니고 성별과 키로 계산되는 predicted body weight임 가능한 tidal은 적은 것이 좋다. • 적절한 Plateau pressure 30 cm. H 2 O 이하로 유지 이상으로 올라갈 경우 barotrauma 위험성 증가
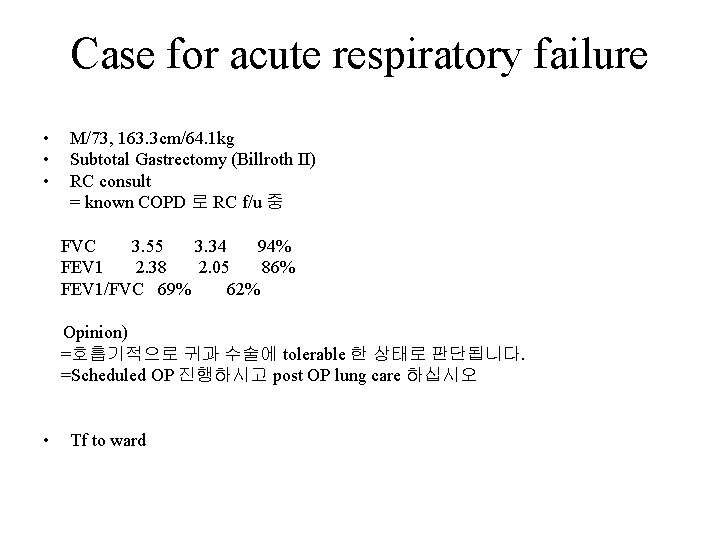
Case for acute respiratory failure • • • M/73, 163. 3 cm/64. 1 kg Subtotal Gastrectomy (Billroth II) RC consult = known COPD 로 RC f/u 중 FVC 3. 55 3. 34 94% FEV 1 2. 38 2. 05 86% FEV 1/FVC 69% 62% Opinion) =호흡기적으로 귀과 수술에 tolerable 한 상태로 판단됩니다. =Scheduled OP 진행하시고 post OP lung care 하십시오 • Tf to ward
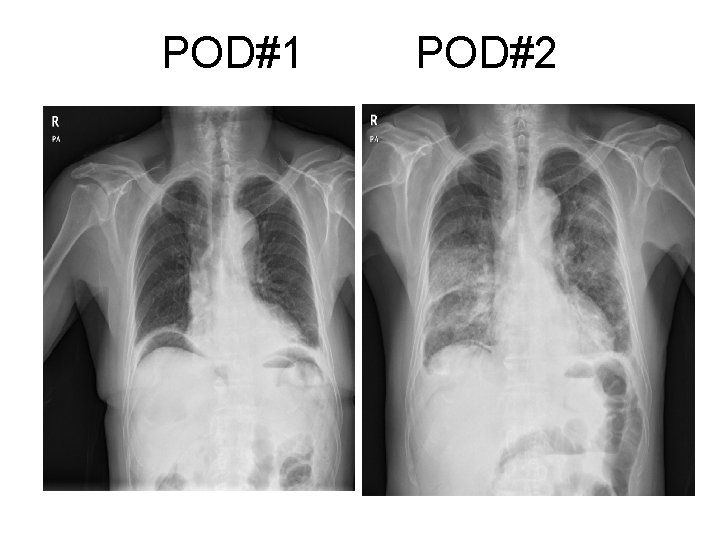
POD#1 POD#2

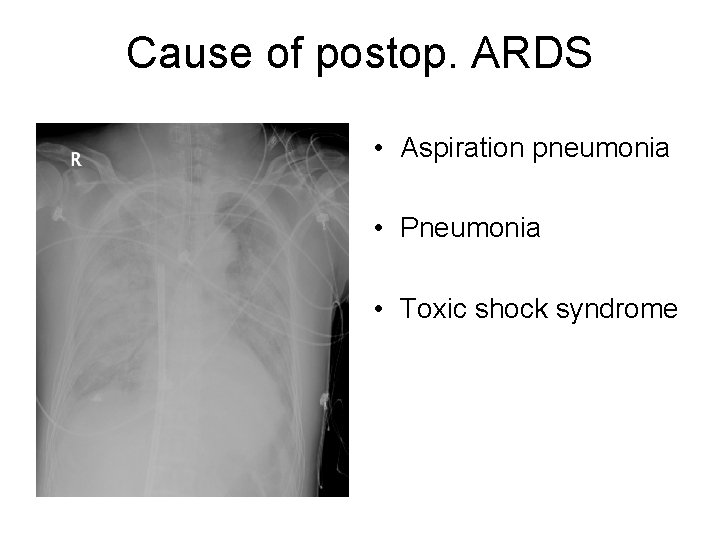
Cause of postop. ARDS • Aspiration pneumonia • Pneumonia • Toxic shock syndrome
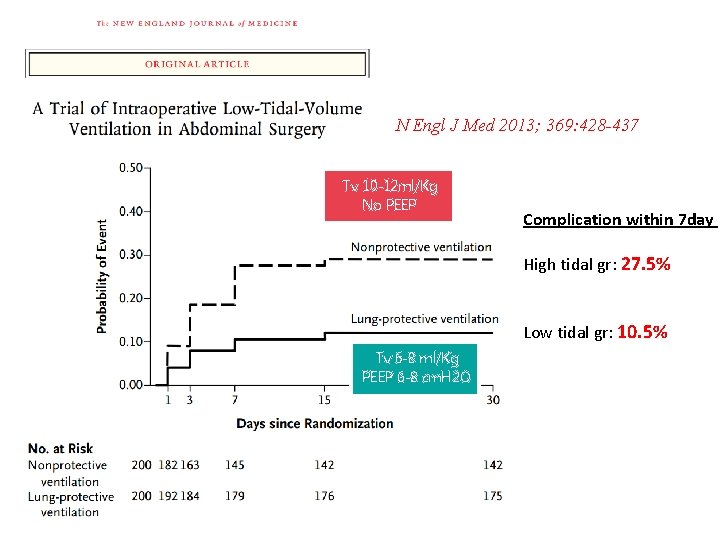
N Engl J Med 2013; 369: 428 -437 Tv 10 -12 ml/Kg No PEEP Complication within 7 day High tidal gr: 27. 5% Low tidal gr: 10. 5% Tv 6 -8 ml/Kg PEEP 6 -8 cm. H 2 O
3. Respiratory Rate • Ventilation (환기)를 유지시키는 목적 Ventilation = remove of Pa. CO 2 • Ventilation은 Minute ventilation과 비례 Minute ventilation = RR x tidal volume • Target: p. H (7. 30~7. 45), Pa. CO 2 p. H는 Pa. CO 2와 반비례 Pa. CO 2는 ventilation과 반비례 p. H는 minute ventilation (RR x TV)과 비례 • acidosis나 alkalosis가 발생하지 않을 만큼의 RR을 결정 • 보통 최대 35회 이하
4. Oxygen concentration • High concentration of oxygen àFree radical ↑ àReperfusion injury ↑ Pulmonary damage ↑ • Optimal O 2 concentration àsufficient to maintain adequate tissue oxygenation but not in excess àTarget oxygenation: Sa. O 2 >90%, Pa. O 2 between 60 – 80 mm. Hg àSevere brain injury: 80 mm. Hg Target에 도달할 정도의 제일 낮은 Fi. O 2를 공급

5. PEEP • Positive end-expiratory pressure; PEEP • Definition – airway pressure that is kept above atmospheric pressure at the end of the expiratory cycle.

Positive Effects of PEEP • • • Recruits collapsed alveoli and/or keeps recruited units open Decrease shunt, improves gas exchange & lung compliance Shift lung water from the alveoli to the perivascular interstitial space May reduces ventilator-induced lung injury Improves triggering in spontaneously breathing patients with auto- PEEP (COPD or asthma)
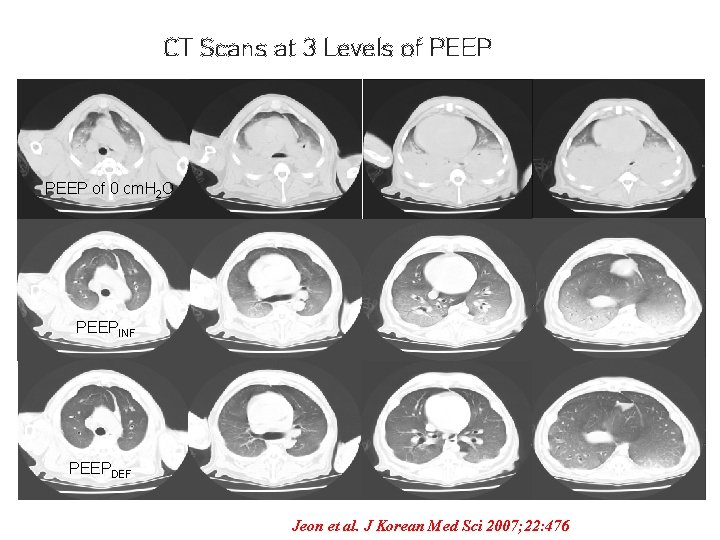
CT Scans at 3 Levels of PEEP of 0 cm. H 2 O PEEPINF PEEPDEF Jeon et al. J Korean Med Sci 2007; 22: 476
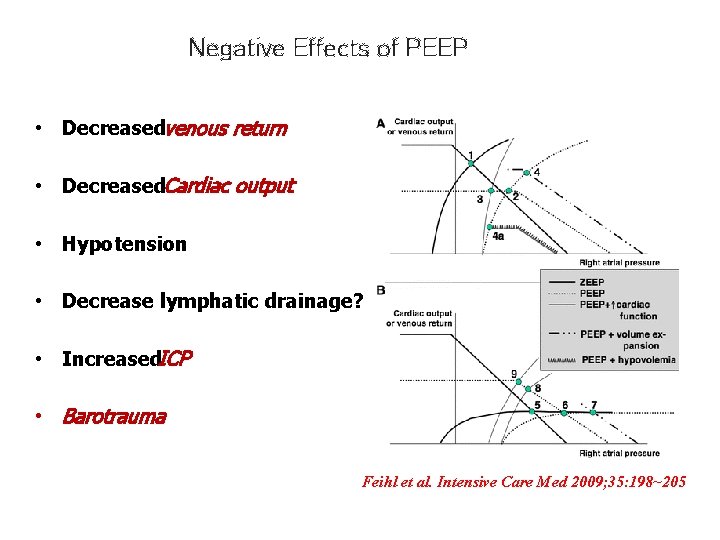
Negative Effects of PEEP • Decreased venous return • Decreased Cardiac output • Hypotension • Decrease lymphatic drainage? • Increased ICP • Barotrauma Feihl et al. Intensive Care Med 2009; 35: 198~205
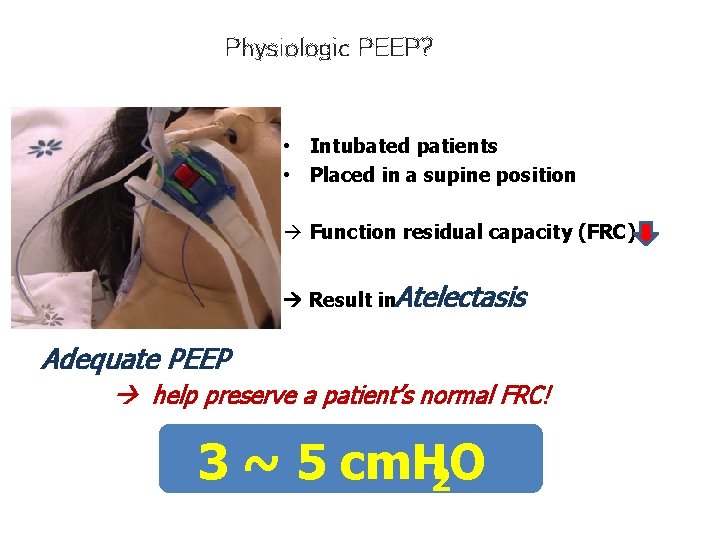
Physiologic PEEP? • Intubated patients • Placed in a supine position à Function residual capacity (FRC) Result in Atelectasis Adequate PEEP help preserve a patient’s normal FRC! 3 ~ 5 cm. H 2 O
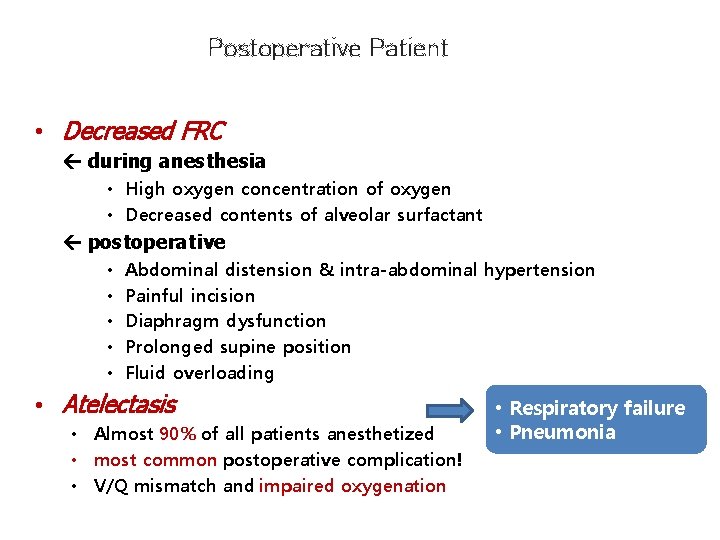
Postoperative Patient • Decreased FRC during anesthesia • High oxygen concentration of oxygen • Decreased contents of alveolar surfactant postoperative • • • Abdominal distension & intra-abdominal hypertension Painful incision Diaphragm dysfunction Prolonged supine position Fluid overloading • Atelectasis • Almost 90% of all patients anesthetized • most common postoperative complication! • V/Q mismatch and impaired oxygenation • Respiratory failure • Pneumonia
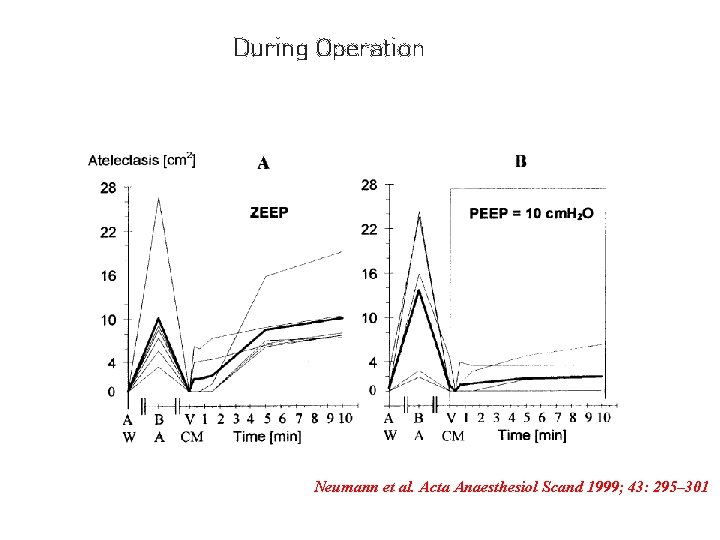
During Operation Neumann et al. Acta Anaesthesiol Scand 1999; 43: 295– 301

Optimal PEEP? • PEEP is beneficial? Definitely “YES”, but double edge sword • What is “optimal” PEEP? Debatable, “No body knows”, “case by case” • Physiologic PEEP 3 ~ 5 cm. H 2 O • Hypoxic respiratory failure lowest PEEP with acceptable oxygenation with Fi. O 2 <0. 6 • in ARDS sufficient PEEP to recruit and keep the collapsed alveoli
Mechanical Ventilation ARDS
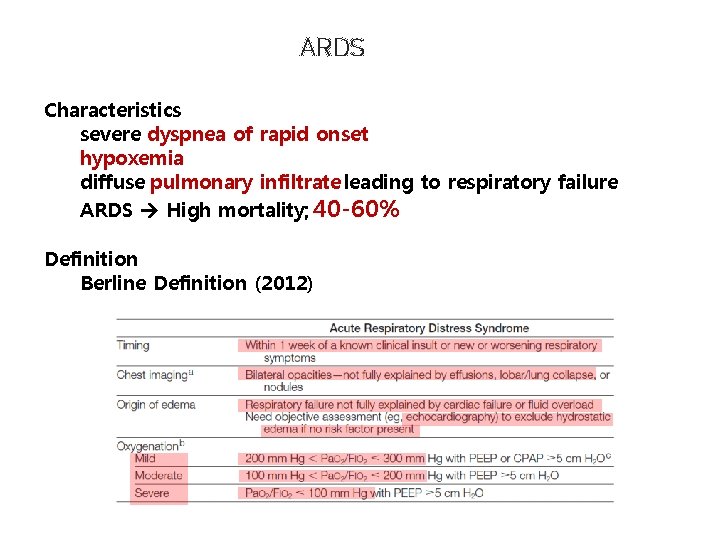
ARDS Characteristics severe dyspnea of rapid onset hypoxemia diffuse pulmonary infiltrate leading to respiratory failure ARDS High mortality; 40 -60% Definition Berline Definition (2012)
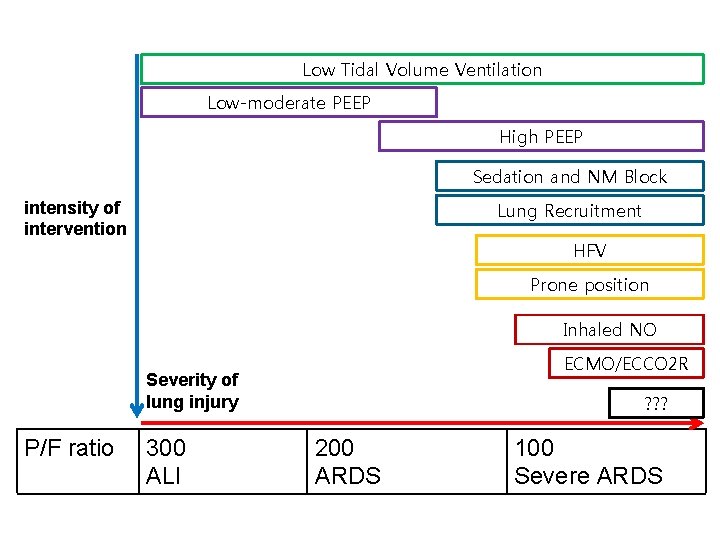
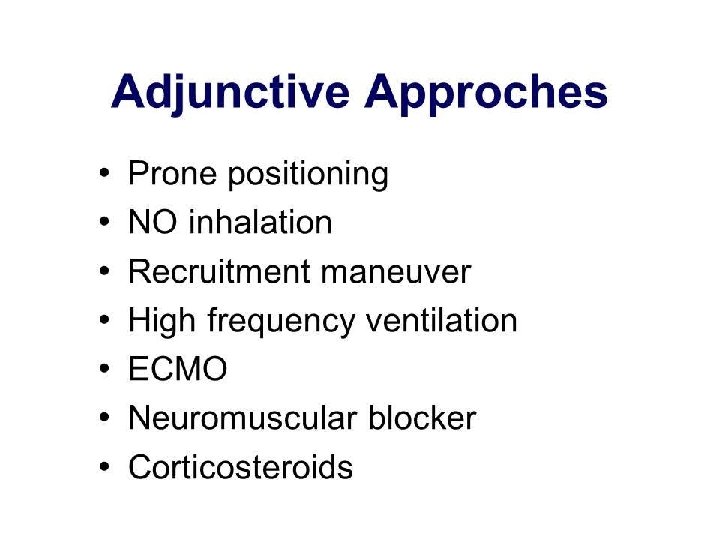
Low Tidal Volume Ventilation Low-moderate PEEP High PEEP Sedation and NM Block Lung Recruitment intensity of intervention HFV Prone position Inhaled NO ECMO/ECCO 2 R Severity of lung injury P/F ratio 300 ALI ? ? ? 200 ARDS 100 Severe ARDS
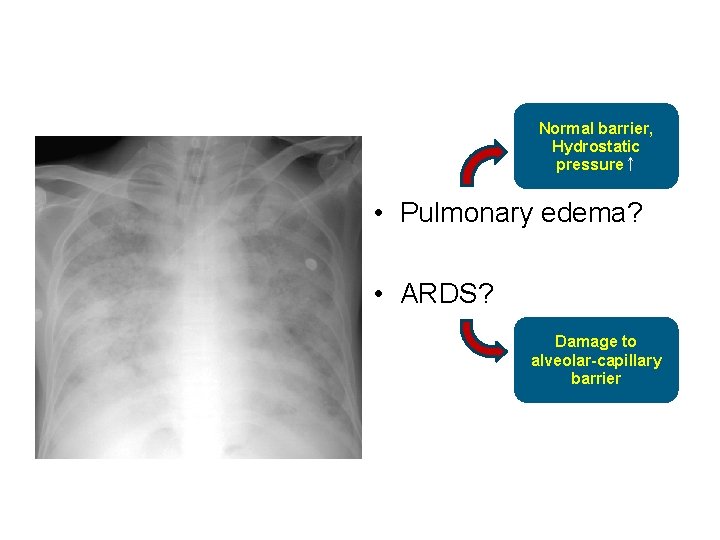
Normal barrier, Hydrostatic pressure↑ • Pulmonary edema? • ARDS? Damage to alveolar-capillary barrier
Treatments • Intrapulmonary shunt and ventilation-perfusion imbalances – Life-threatening hypoxemia • High work of breathing from increased alveolar dead space and reduced respiratory system compliance – Ventilatory failure • The mainstay of supportive care – Time for administration of treatment for theunderlying cause – Time for the evolution of natural healing processes – Arterial oxygenation (Fi. O 2, PEEP) Mechanical ventilation!!
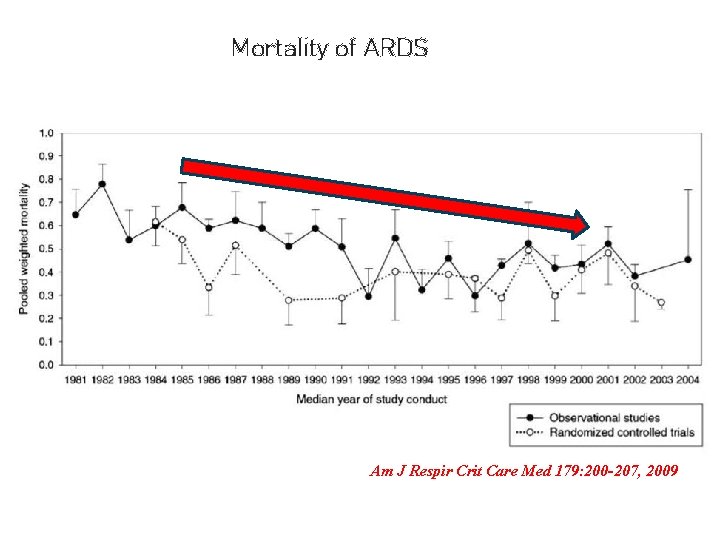
Mortality of ARDS Am J Respir Crit Care Med 179: 200 -207, 2009
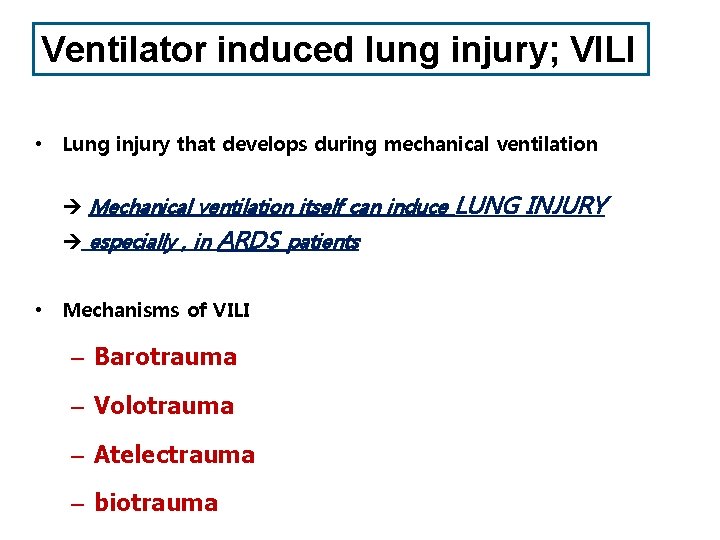
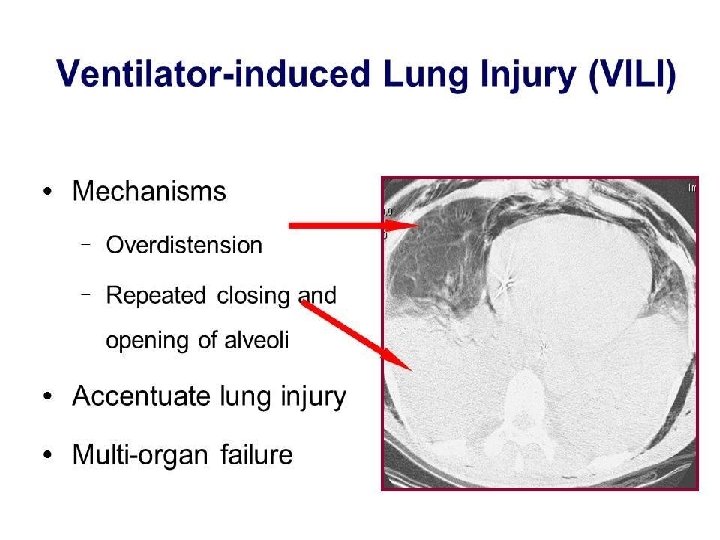
Ventilator induced lung injury; VILI • Lung injury that develops during mechanical ventilation Mechanical ventilation itself can induce especially , in ARDS patients • Mechanisms of VILI – Barotrauma – Volotrauma – Atelectrauma – biotrauma LUNG INJURY
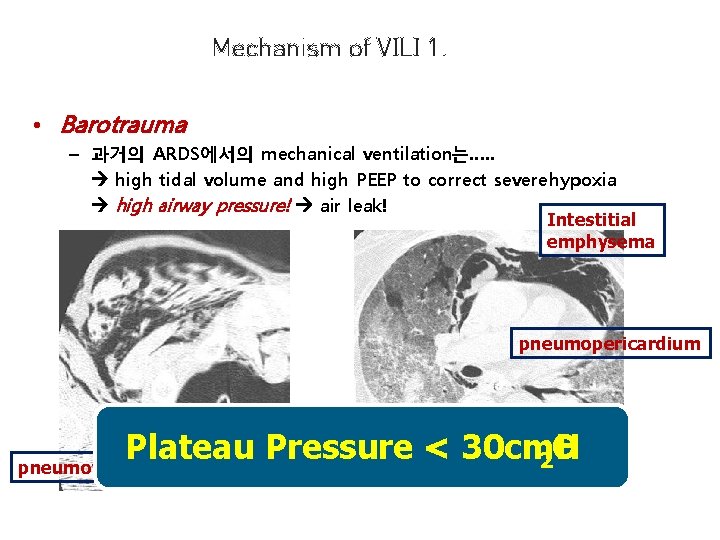
Mechanism of VILI 1. • Barotrauma – 과거의 ARDS에서의 mechanical ventilation는…. . high tidal volume and high PEEP to correct severe hypoxia high airway pressure! air leak! Intestitial emphysema pneumopericardium pneumomediastinum Plateau Pressure < 30 cm. H O 2 pneumothorax
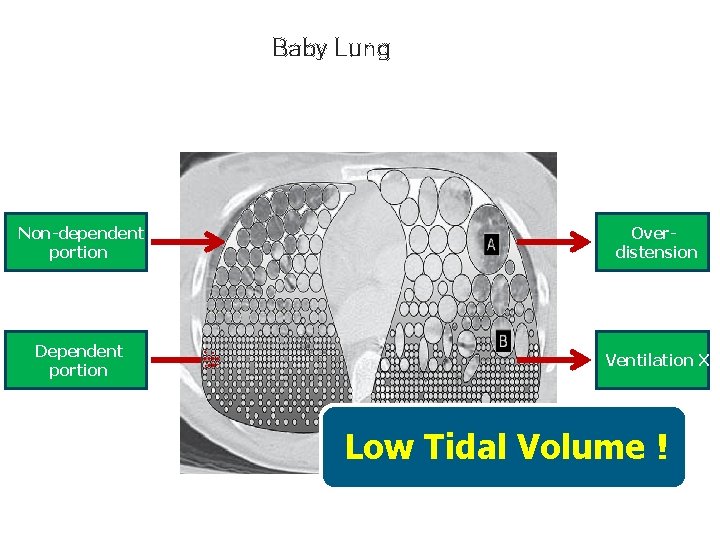
Baby Lung Non-dependent portion Overdistension Dependent portion Ventilation X Low Tidal Volume !

Low V T vs High V T • Amato et al. NEJM 1998; 338: 347 -54 • Tidal volume <6 ml/Kg, PEEP 15 -20, Plateau Pr < 30 • Tidal volume 12 ml/Kg, PEEP 6 -8, Plateau Pr 46 40%
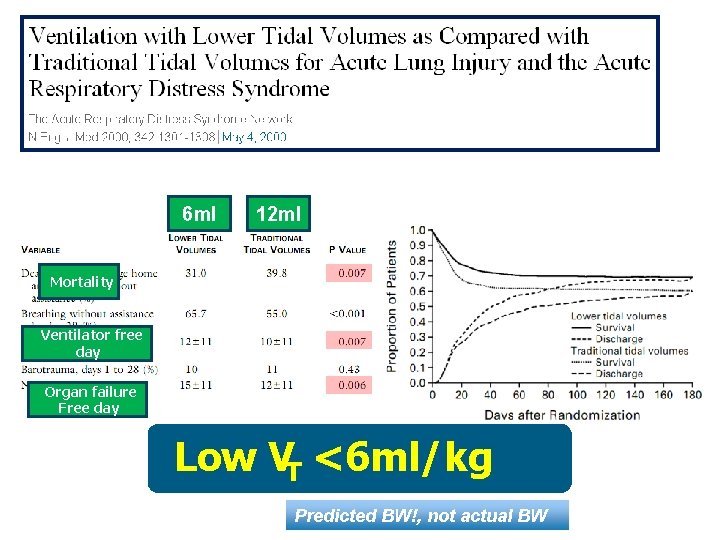
` 6 ml 12 ml Mortality Ventilator free day Organ failure Free day Low VT <6 ml/kg Predicted BW!, not actual BW
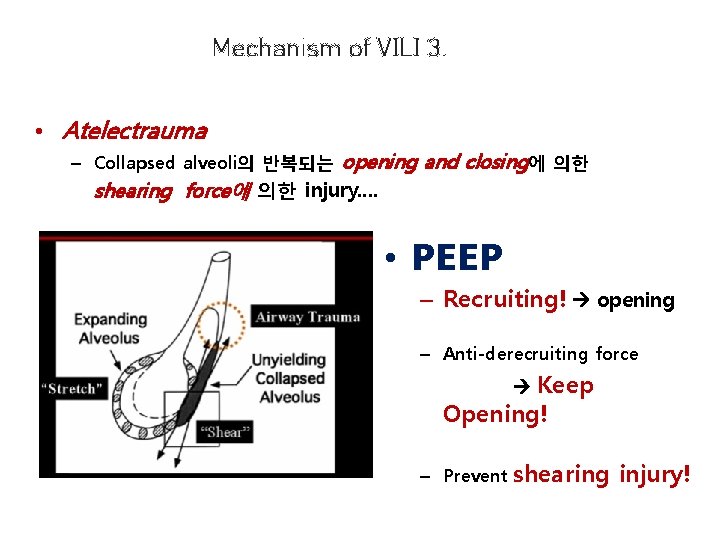
Mechanism of VILI 3. • Atelectrauma – Collapsed alveoli의 반복되는 opening and closing에 의한 shearing force에 의한 injury…. • PEEP – Recruiting! opening – Anti-derecruiting force Keep Opening! – Prevent shearing injury!
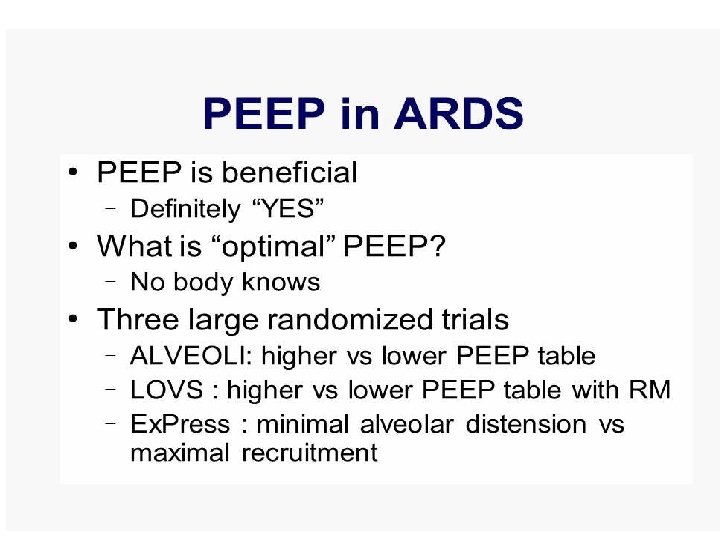
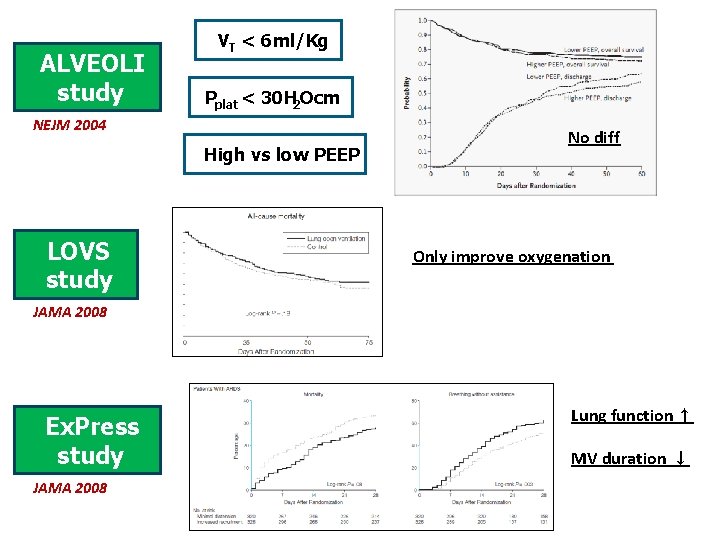
ALVEOLI study VT < 6 ml/Kg Pplat < 30 H 2 Ocm NEJM 2004 High vs low PEEP LOVS study No diff Only improve oxygenation JAMA 2008 Ex. Press study JAMA 2008 Lung function ↑ MV duration ↓
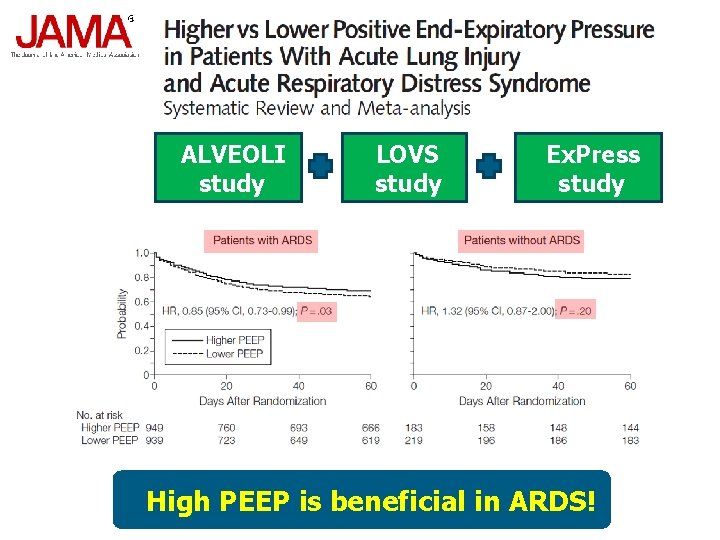
ALVEOLI study LOVS study Ex. Press study High PEEP is beneficial in ARDS!
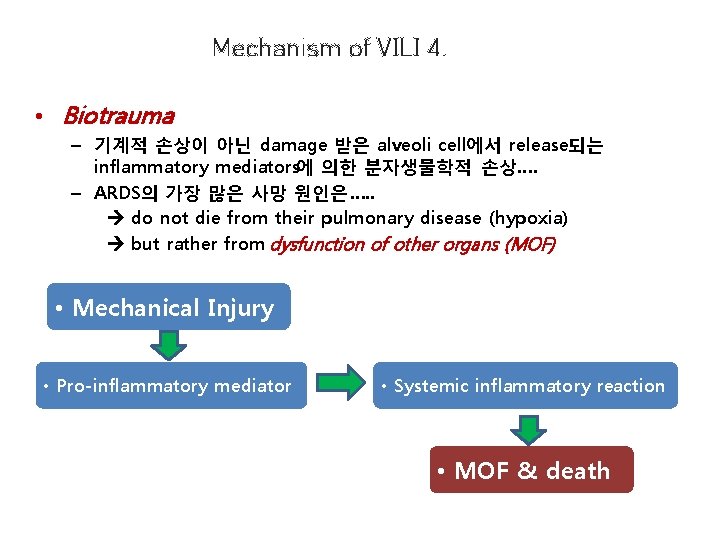
Mechanism of VILI 4. • Biotrauma – 기계적 손상이 아닌 damage 받은 alveoli cell에서 release되는 inflammatory mediators에 의한 분자생물학적 손상…. – ARDS의 가장 많은 사망 원인은…. . do not die from their pulmonary disease (hypoxia) but rather from dysfunction of other organs (MOF) • Mechanical Injury • Pro-inflammatory mediator • Systemic inflammatory reaction • MOF & death
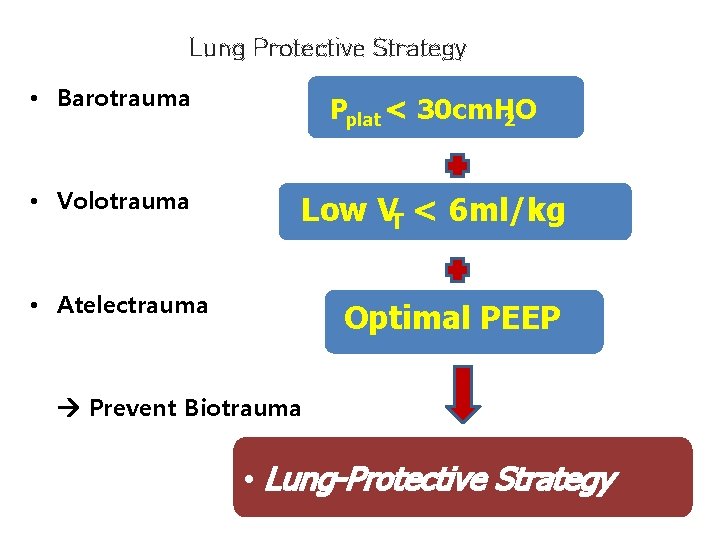
Lung Protective Strategy • Barotrauma Pplat < 30 cm. H 2 O • Volotrauma Low VT < 6 ml/kg • Atelectrauma Optimal PEEP Prevent Biotrauma • Lung-Protective Strategy
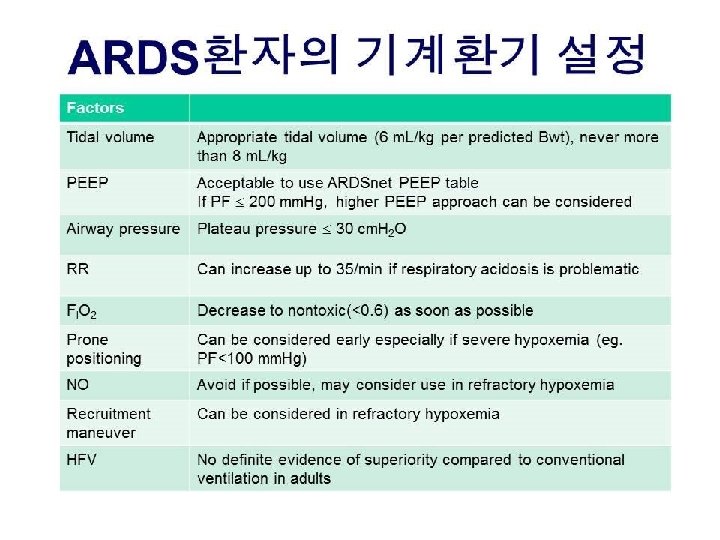
Lung Protective Ventilation
- Slides: 50