Basic Clinician Training Module 4 Hypercoagulable States Introduction
Basic Clinician Training Module 4 Hypercoagulable States Introduction Hypercoagulable States Test Your Knowledge
Introduction • • Prothrombotic or hypercoagulable state § Hyperactive platelet function § Hyperactive coagulation cascade function Prevention of development of a thrombotic event § Proper assessment of the factors contributing to a hypercoagulable state, which is necessary to determine proper pharmacological intervention 2
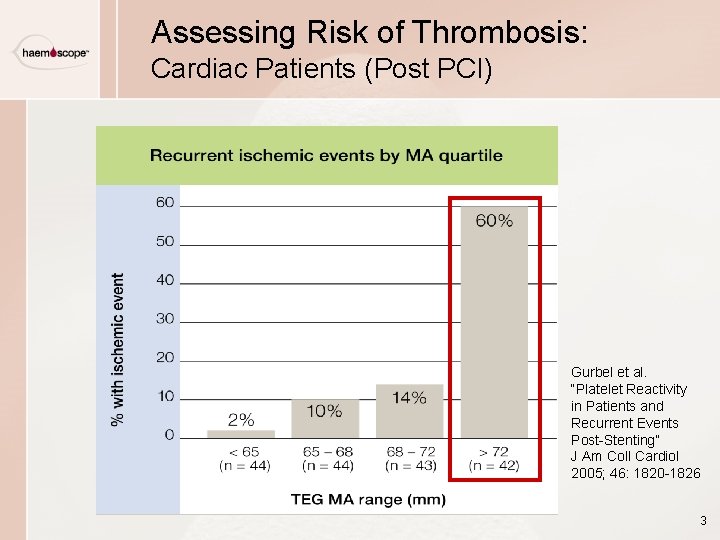
Assessing Risk of Thrombosis: Cardiac Patients (Post PCI) Gurbel et al. “Platelet Reactivity in Patients and Recurrent Events Post-Stenting” J Am Coll Cardiol 2005; 46: 1820 -1826 3
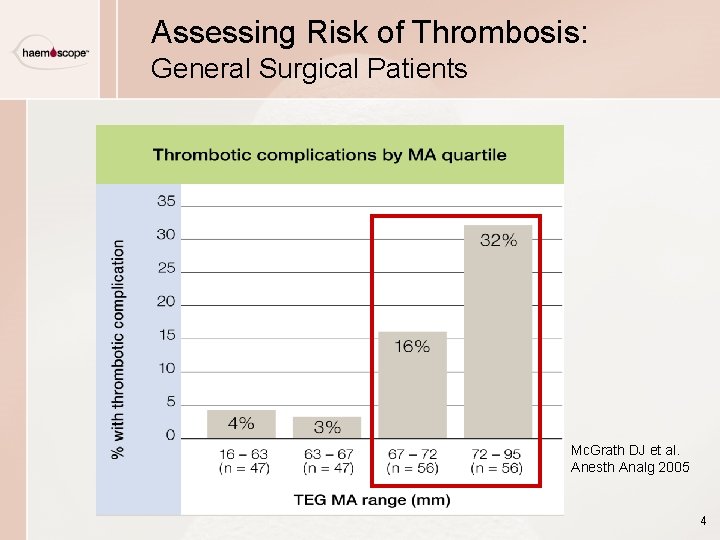
Assessing Risk of Thrombosis: General Surgical Patients Mc. Grath DJ et al. Anesth Analg 2005 4
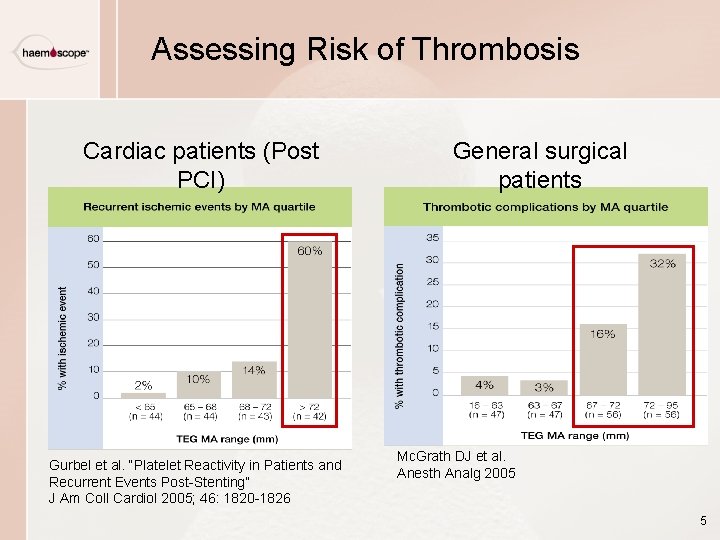
Assessing Risk of Thrombosis Cardiac patients (Post PCI) Gurbel et al. “Platelet Reactivity in Patients and Recurrent Events Post-Stenting” J Am Coll Cardiol 2005; 46: 1820 -1826 General surgical patients Mc. Grath DJ et al. Anesth Analg 2005 5
Assessing Hypercoagulability with the TEG Analyzer TEG analysis • • Demonstrates hypercoagulable and hypocoagulable states § Platelets § Coagulation pathways § Enzymatic pathways Aids in identifying § Type and magnitude of imbalance § Specific hemostatic interpretation 6
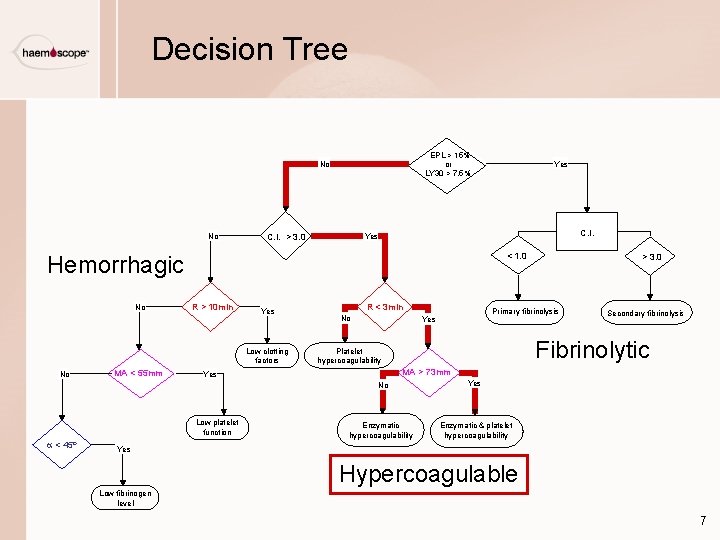
Decision Tree EPL > 15% or LY 30 > 7. 5% No No C. I. > 3. 0 C. I. Yes < 1. 0 Hemorrhagic No R > 10 min Yes Low clotting factors No MA < 55 mm R < 3 min No Secondary fibrinolysis Fibrinolytic Platelet hypercoagulability MA > 73 mm Yes Low platelet function > 3. 0 Primary fibrinolysis Yes No a < 45º Yes Enzymatic hypercoagulability Yes Enzymatic & platelet hypercoagulability Yes Hypercoagulable Low fibrinogen level 7
Hypercoagulable States: Platelet vs. Enzymatic • • Hyperactive platelet function § Characterized by rapid clot development and abnormally high clot strength Enzymatic pathway hypercoagulability § Characterized by rapid fibrin formation, with subsequent clot formation 8
Platelet Hypercoagulability • • Rapid clot development, with higher than normal clot strength § Hyperactive platelet function Probable causes § § Diminished endogenous platelet inhibitory mechanisms High platelet numbers Abnormal generation of platelet activators Inflammatory mediators 9
Platelet Hypercoagulability Common conditions • • • Sepsis Disseminated Intravascular Coagulation (DIC) Malignancy Thrombomodulin-Protein C dysfunction Activated protein C (APC) resistance Antithrombin III deficiency Diminished nitric oxide synthesis/release Dysplasminogenemia High plasminogen activator inhibitor Hyperhomocysteinemia 10
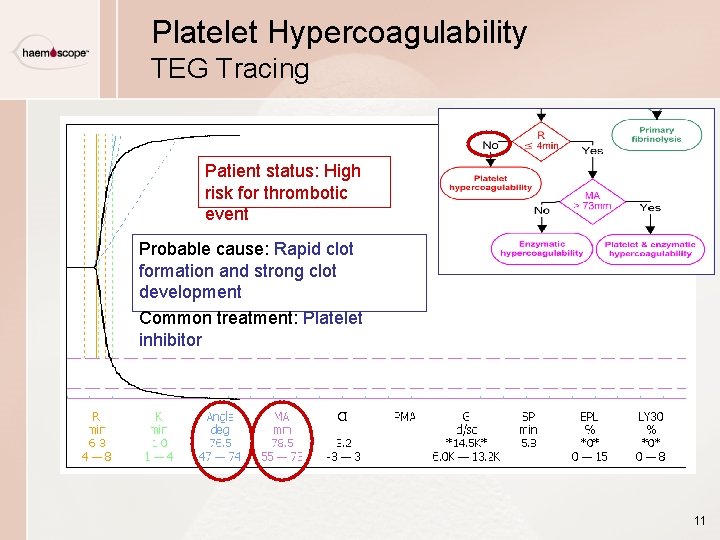
Platelet Hypercoagulability TEG Tracing Patient status: High risk for thrombotic event Probable cause: Rapid clot formation and strong clot development Common treatment: Platelet inhibitor 11
Platelet Hypercoagulability Treatment Considerations Best Treatment • • Step 1: Identify and quantify prothrombotic state Step 2: Determine therapeutic response to antiplatelet therapy § WHY? : Resistance to aspirin and clopidogrel § HOW? : TEG analysis with Platelet. Mapping assay • Assess platelet inhibition against maximum platelet function • Provide personalized treatment regimen 12
Enzymatic Hypercoagulability • • Rapid thrombin generation, leading to clot formation Probable causes: § Loss of antithrombotic protective mechanisms • APC resistance (Factor V Leiden) • ATIII deficiency § Dysfibrinogenemia § Hyperactive platelets 13
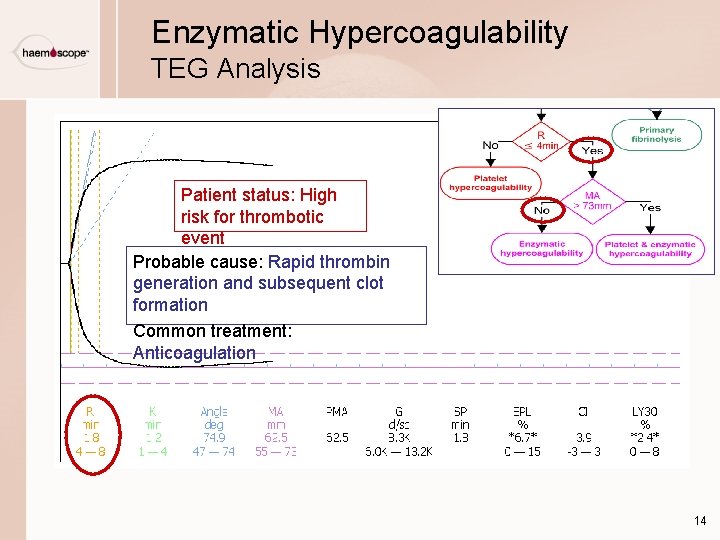
Enzymatic Hypercoagulability TEG Analysis Patient status: High risk for thrombotic event Probable cause: Rapid thrombin generation and subsequent clot formation Common treatment: Anticoagulation 14
Enzymatic Hypercoagulability Special Considerations Treatment depends on clinical situation • • Goal is to prevent clot formation § Common inpatient treatment: heparin, LMWH, APC (activated protein C) § Common outpatient treatment: LMWH or warfarin to maintain INR > 2. 0, slightly higher R (10 -14 minutes) Patient may require fibrinolytic agent before anticoagulation if clots have already formed. 15
Platelet and Enzymatic Hypercoagulability Common conditions • • Sepsis Trauma Pregnancy Cancer Orthopedic surgery Burns Lupus anticoagulant Heart assist device 16
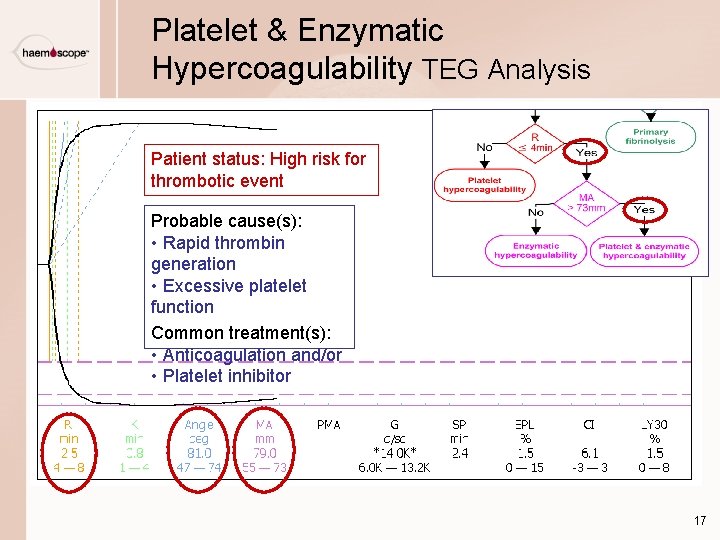
Platelet & Enzymatic Hypercoagulability TEG Analysis Patient status: High risk for thrombotic event Probable cause(s): • Rapid thrombin generation • Excessive platelet function Common treatment(s): • Anticoagulation and/or • Platelet inhibitor 17
Basic Clinician Training Interpretation Exercises Prothrombotic States
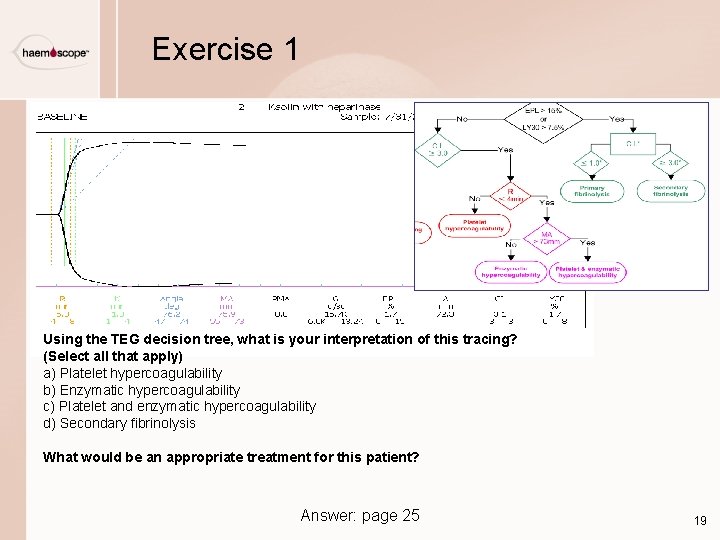
Exercise 1 Using the TEG decision tree, what is your interpretation of this tracing? (Select all that apply) a) Platelet hypercoagulability b) Enzymatic hypercoagulability c) Platelet and enzymatic hypercoagulability d) Secondary fibrinolysis What would be an appropriate treatment for this patient? Answer: page 25 19
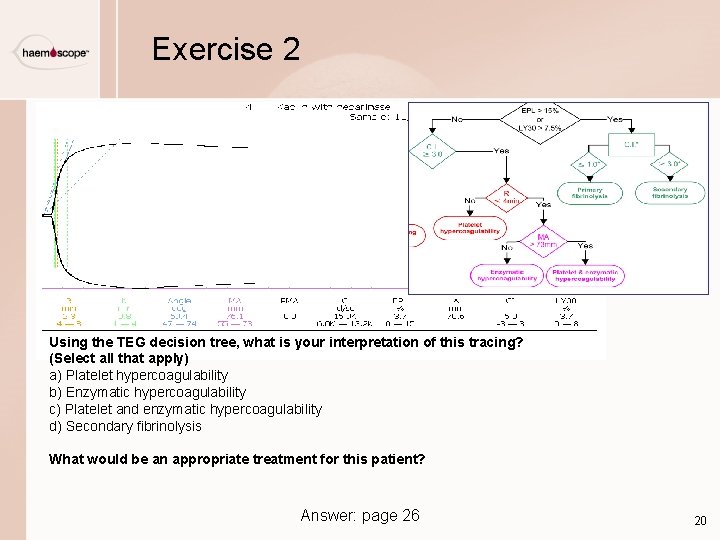
Exercise 2 Using the TEG decision tree, what is your interpretation of this tracing? (Select all that apply) a) Platelet hypercoagulability b) Enzymatic hypercoagulability c) Platelet and enzymatic hypercoagulability d) Secondary fibrinolysis What would be an appropriate treatment for this patient? Answer: page 26 20
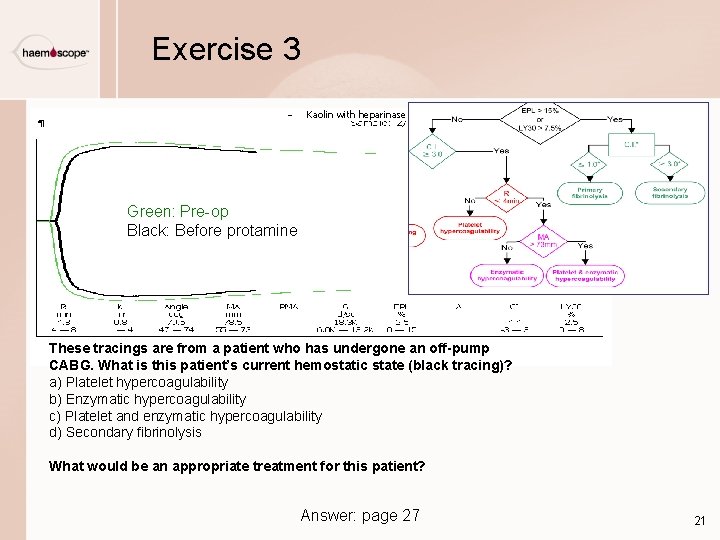
Exercise 3 Kaolin with heparinase Green: Pre-op Black: Before protamine These tracings are from a patient who has undergone an off-pump CABG. What is this patient’s current hemostatic state (black tracing)? a) Platelet hypercoagulability b) Enzymatic hypercoagulability c) Platelet and enzymatic hypercoagulability d) Secondary fibrinolysis What would be an appropriate treatment for this patient? Answer: page 27 21
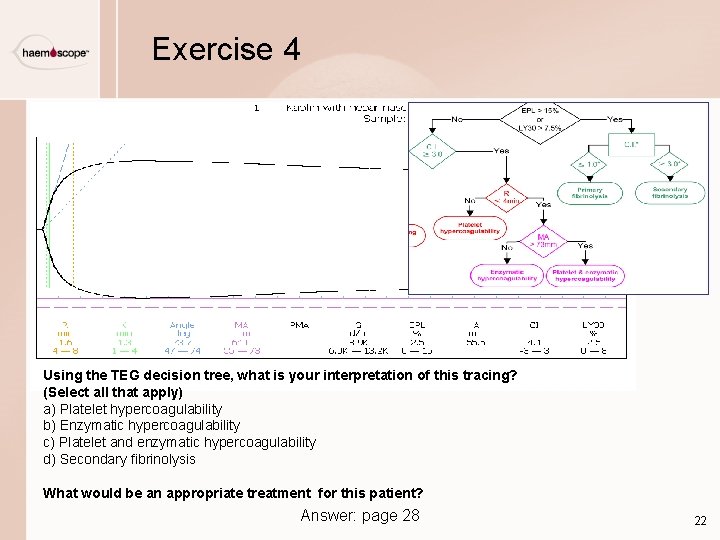
Exercise 4 Using the TEG decision tree, what is your interpretation of this tracing? (Select all that apply) a) Platelet hypercoagulability b) Enzymatic hypercoagulability c) Platelet and enzymatic hypercoagulability d) Secondary fibrinolysis What would be an appropriate treatment for this patient? Answer: page 28 22
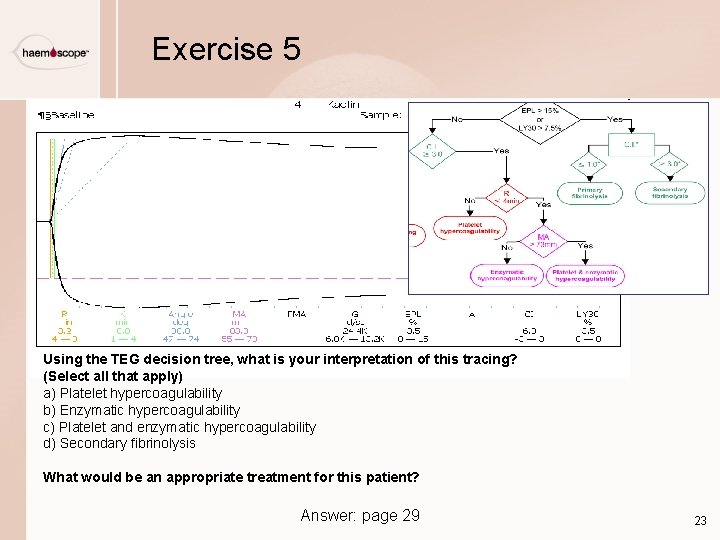
Exercise 5 Using the TEG decision tree, what is your interpretation of this tracing? (Select all that apply) a) Platelet hypercoagulability b) Enzymatic hypercoagulability c) Platelet and enzymatic hypercoagulability d) Secondary fibrinolysis What would be an appropriate treatment for this patient? Answer: page 29 23
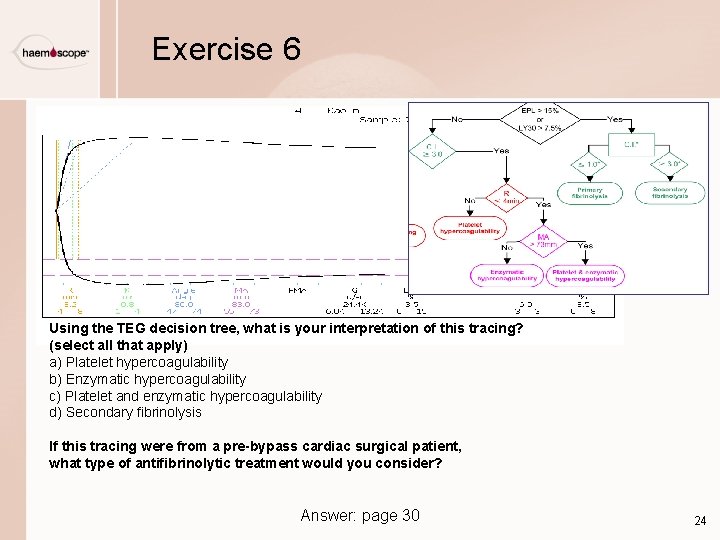
Exercise 6 Using the TEG decision tree, what is your interpretation of this tracing? (select all that apply) a) Platelet hypercoagulability b) Enzymatic hypercoagulability c) Platelet and enzymatic hypercoagulability d) Secondary fibrinolysis If this tracing were from a pre-bypass cardiac surgical patient, what type of antifibrinolytic treatment would you consider? Answer: page 30 24
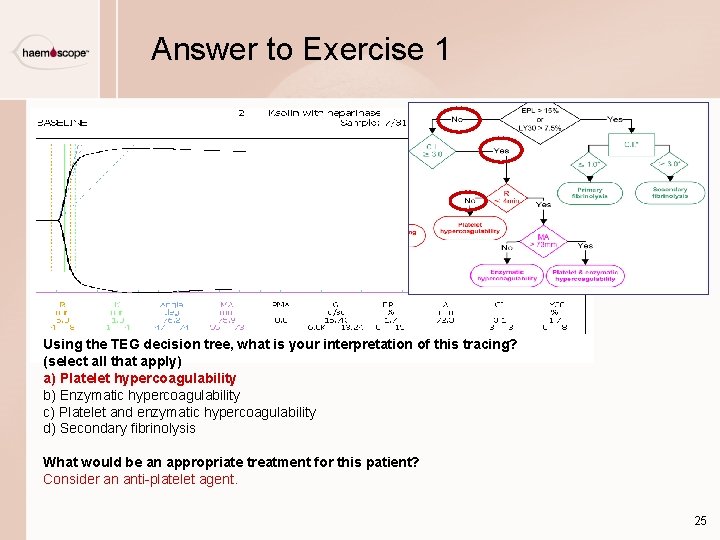
Answer to Exercise 1 Using the TEG decision tree, what is your interpretation of this tracing? (select all that apply) a) Platelet hypercoagulability b) Enzymatic hypercoagulability c) Platelet and enzymatic hypercoagulability d) Secondary fibrinolysis What would be an appropriate treatment for this patient? Consider an anti-platelet agent. 25
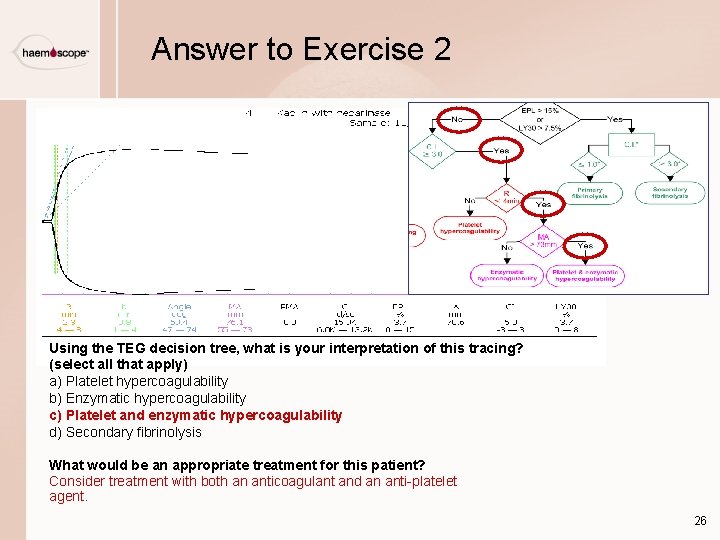
Answer to Exercise 2 Using the TEG decision tree, what is your interpretation of this tracing? (select all that apply) a) Platelet hypercoagulability b) Enzymatic hypercoagulability c) Platelet and enzymatic hypercoagulability d) Secondary fibrinolysis What would be an appropriate treatment for this patient? Consider treatment with both an anticoagulant and an anti-platelet agent. 26
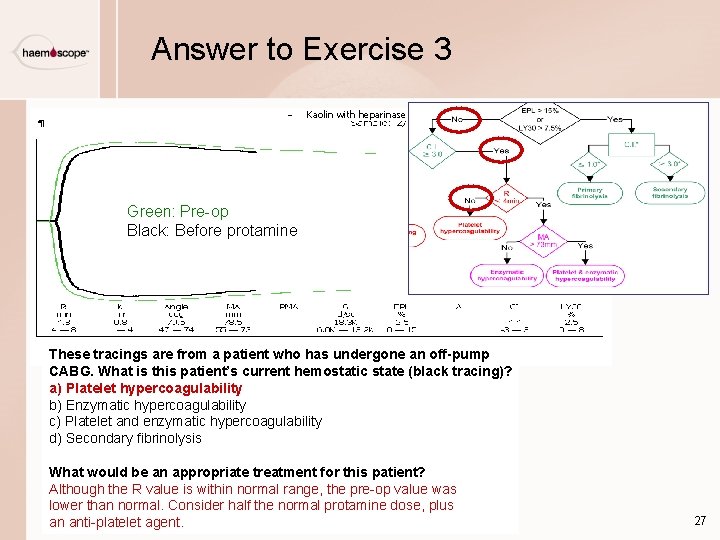
Answer to Exercise 3 Kaolin with heparinase Green: Pre-op Black: Before protamine These tracings are from a patient who has undergone an off-pump CABG. What is this patient’s current hemostatic state (black tracing)? a) Platelet hypercoagulability b) Enzymatic hypercoagulability c) Platelet and enzymatic hypercoagulability d) Secondary fibrinolysis What would be an appropriate treatment for this patient? Although the R value is within normal range, the pre-op value was lower than normal. Consider half the normal protamine dose, plus an anti-platelet agent. 27
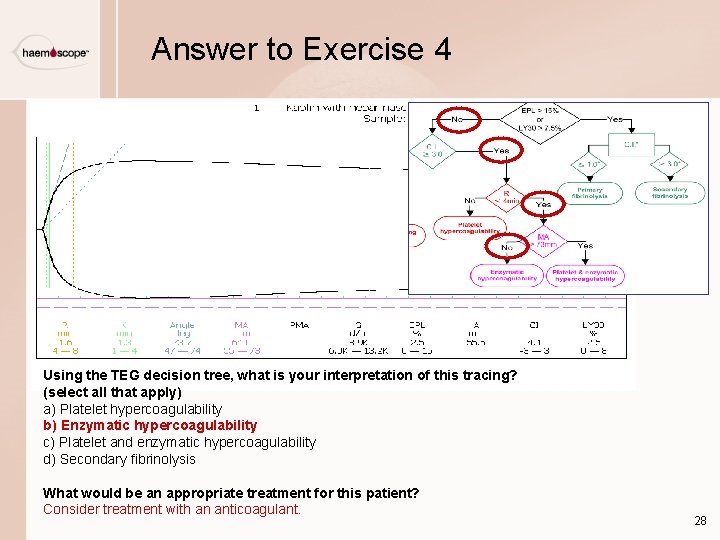
Answer to Exercise 4 Using the TEG decision tree, what is your interpretation of this tracing? (select all that apply) a) Platelet hypercoagulability b) Enzymatic hypercoagulability c) Platelet and enzymatic hypercoagulability d) Secondary fibrinolysis What would be an appropriate treatment for this patient? Consider treatment with an anticoagulant. 28
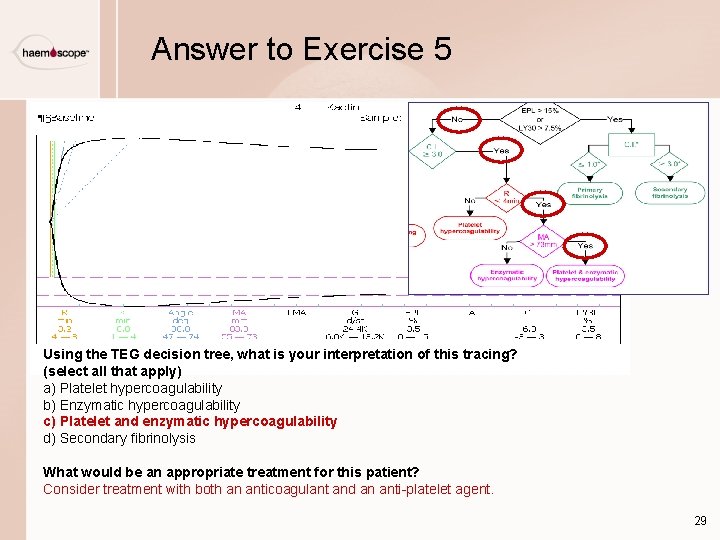
Answer to Exercise 5 Using the TEG decision tree, what is your interpretation of this tracing? (select all that apply) a) Platelet hypercoagulability b) Enzymatic hypercoagulability c) Platelet and enzymatic hypercoagulability d) Secondary fibrinolysis What would be an appropriate treatment for this patient? Consider treatment with both an anticoagulant and an anti-platelet agent. 29
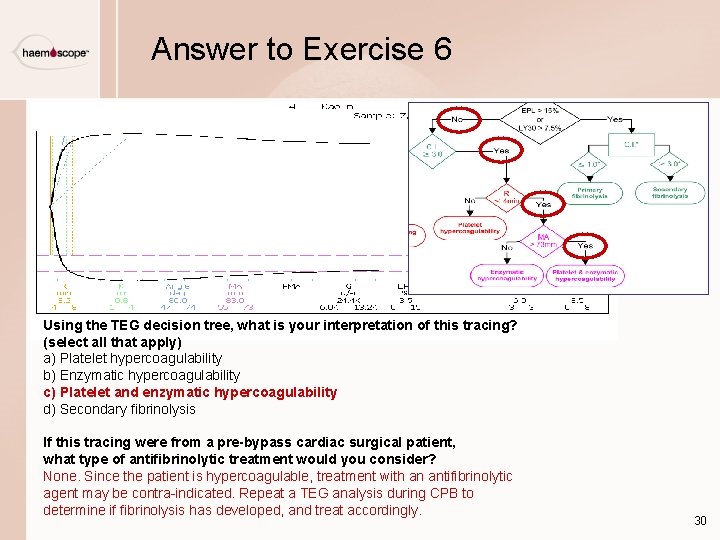
Answer to Exercise 6 Using the TEG decision tree, what is your interpretation of this tracing? (select all that apply) a) Platelet hypercoagulability b) Enzymatic hypercoagulability c) Platelet and enzymatic hypercoagulability d) Secondary fibrinolysis If this tracing were from a pre-bypass cardiac surgical patient, what type of antifibrinolytic treatment would you consider? None. Since the patient is hypercoagulable, treatment with an antifibrinolytic agent may be contra-indicated. Repeat a TEG analysis during CPB to determine if fibrinolysis has developed, and treat accordingly. 30
Basic Clinician Training End of Module 4
- Slides: 31