BARIUM MEAL ENEMA STUDY PATHOLOGY Dr Vasudha Agarwal
BARIUM MEAL, ENEMA STUDY & PATHOLOGY Dr. Vasudha Agarwal Senior Resident Under the guidance of Dr. Sachin Bagale Sir
Source & Chemical nature Barium Sulphate (Ba. So 4) is used. Naturally occurring Ba. So 4 is toxic. Medically used Ba. So 4 is precipitated from other compounds. An inert substance. Atomic number-56 Specific gravity - 4. 5
DENSITY & VISCOCITY : Density depends on the particle size Thick and Thin barium depending on the viscosity of the suspension not on the density.
ADVANTAGES: • EXCELLENT COATING allowing good demonstration of anatomical details. • Cost effective. DISADVANTAGES • High morbidity if barium enters peritoneal cavity • Subsequent CTand ultrasound exams are rendered difficult as it may take a few days for the barium to clear up
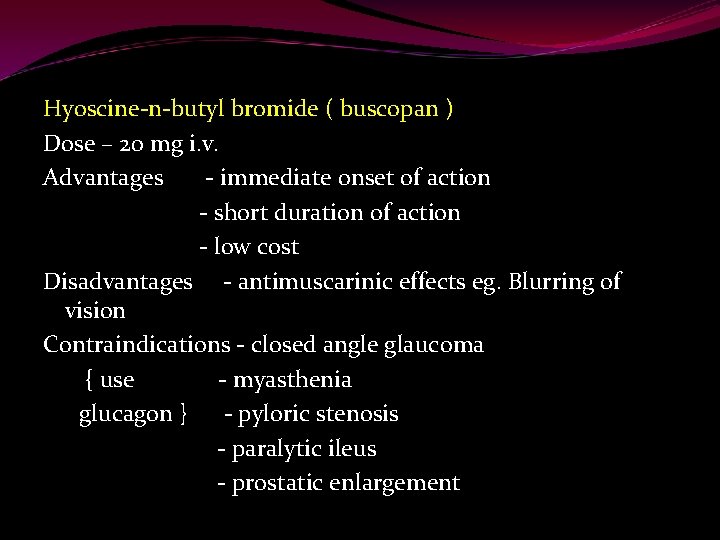
Hyoscine-n-butyl bromide ( buscopan ) Dose – 20 mg i. v. Advantages - immediate onset of action - short duration of action - low cost Disadvantages - antimuscarinic effects eg. Blurring of vision Contraindications - closed angle glaucoma { use - myasthenia glucagon } - pyloric stenosis - paralytic ileus - prostatic enlargement
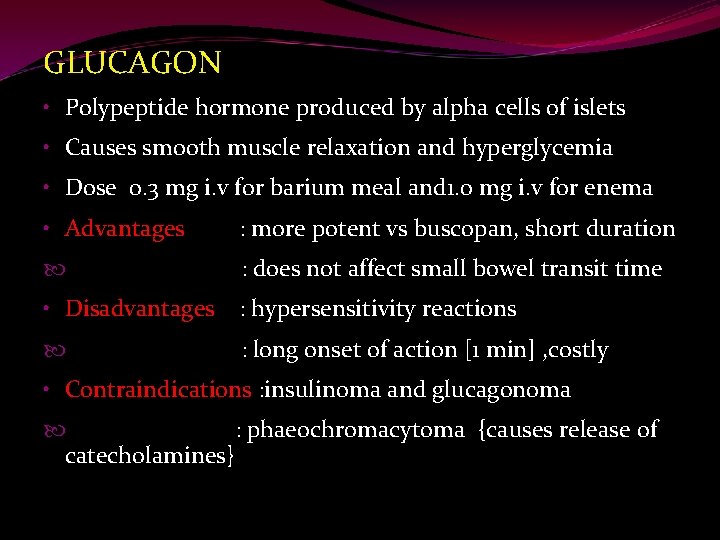
GLUCAGON • Polypeptide hormone produced by alpha cells of islets • Causes smooth muscle relaxation and hyperglycemia • Dose 0. 3 mg i. v for barium meal and 1. 0 mg i. v for enema • Advantages : more potent vs buscopan, short duration : does not affect small bowel transit time • Disadvantages : hypersensitivity reactions : long onset of action [1 min] , costly • Contraindications : insulinoma and glucagonoma : phaeochromacytoma {causes release of catecholamines}
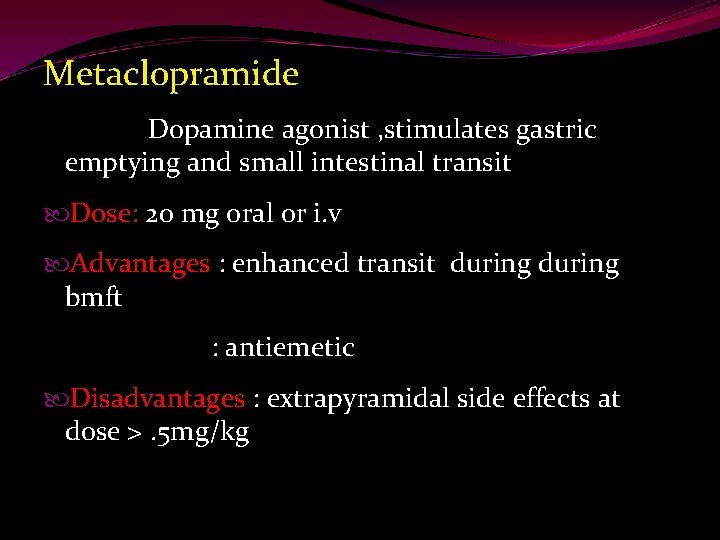
Metaclopramide Dopamine agonist , stimulates gastric emptying and small intestinal transit Dose: 20 mg oral or i. v Advantages : enhanced transit during bmft : antiemetic Disadvantages : extrapyramidal side effects at dose >. 5 mg/kg

Double Vs single contrast studies In a double contrast study a negative contrast agent like air is used in addition to Ba. So 4 to distend and help in coating the mucosa. A very high density and low viscosity Ba. So 4 suspension used. Gives a better mucosal detail. Technically demanding.
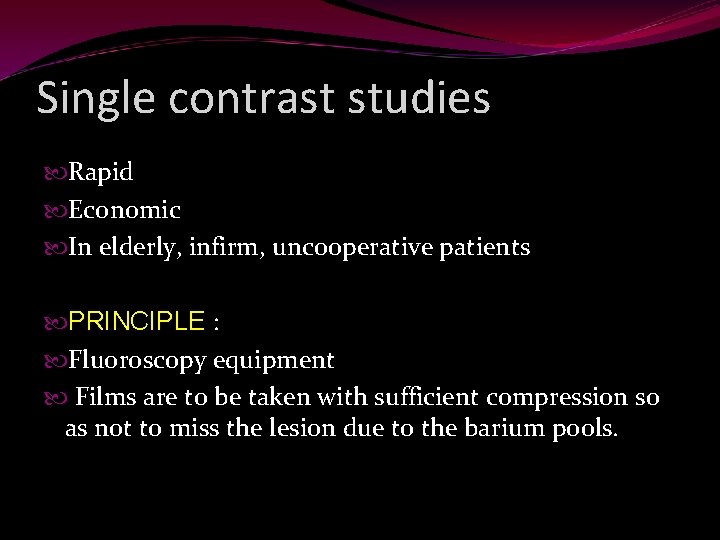
Single contrast studies Rapid Economic In elderly, infirm, uncooperative patients PRINCIPLE : Fluoroscopy equipment Films are to be taken with sufficient compression so as not to miss the lesion due to the barium pools.
Suspensions used are: Oesophagus- 50 to 100% w/v Upper GI series – 50 t 100% w/v Enteroclysis – 15 to 20 % w/v Enema – 15 to 20%
Quality control: Operated at 90 to 120 kvp. Skeletal shadows should be visible through the barium column. The bowel loops should be visible through the overlapped loops.
BARIUM MEAL To evaluate stomach and the duodenum ØPRINCIPLES Fluoroscopy Careful compression Controlled filling of each portion
INDICATIONS • Epigastric pain , anorexia, weight loss , vomiting , anemia , heart burn , dyspepsia • Upper abdominal mass • GI haemorrhage • Gastric or duodenal obstruction • Malignancies of OG junction , stomach or duodenum • Motility disorders of GIT • In children to identify causes of vomiting - reflux - pyloric obstruction - malrotation • Systemic disease like TB of GIT
CONTRAINDICATIONS • Suspected gastro duodenal perforation • History or suspicion of aspiration • Large bowel obstruction {barium inspissation may occur in these cases } • Fistulous communication with any other organ other than GIT • Recent biopsy from GIT { barium granuloma may form at biopsy site}
PREPARATION 1. NPO for at least 6 hours before examinations. For routine studies keep the patient fasting overnight. 2. Patient should restrain from smoking as it interfers with mucosal coating 3. In patients with gastric outlet obstruction , prolonged fasting , IV metaclopramide CONTRAST MEDIA • • Single contrast – lower density contrast (80 -100%w/v) is used. 30% w/v suspension in used for high kv technique Double contrast – high density (250% w/v ) low viscosity barium is best for mucosal coating
METHOD Patient drinks barium lying on the left side with elbow support Patient then lies supine and slightly to the right to check the GO junction for reflux. Take a spot film if any reflux is noted Give iv muscle relaxant Roll patient in a complete circle clockwise to finish in RAO Spot films ahould be taken in both distended and empty states
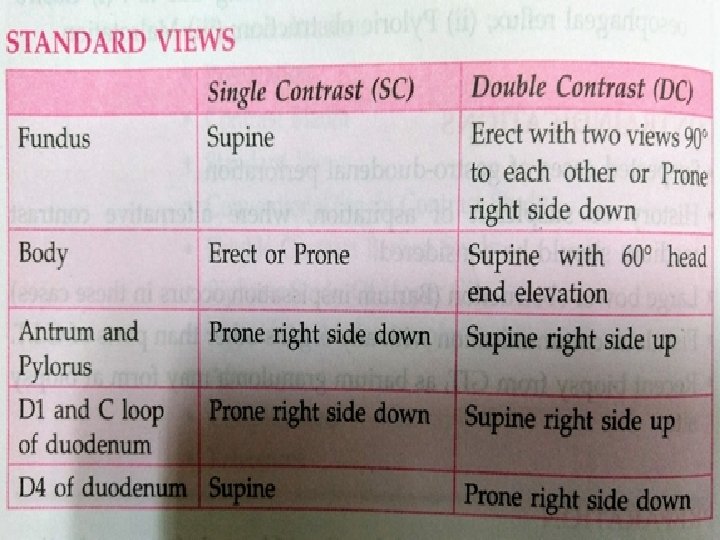
Basic views for stomach 1. Prone - mucosa of the anterior wall 2. Supine –body and proximal antrum 3. Supine RAO -body and whole antrum 4. Supine LAO –fundus and upper body Ø Basic views for duodenum 1. RAO – duodenal cap 2. Prone with left side up – ‘c’ loop of the duodenum.
ØAFTER CARE : Patient should be warned that his bowel motion will be white for a few days Patient should be told to drink adequate ammount of water to prevent impaction Patient must not leave till the side effects of buscopan have subsided
Complications Leakage from unsuspected perforation Aspiration due to buscopan Impaction leading to large bowel obstruction or appendicitis
Few added points Single contrast high k. V technique– 120 -130 k. V, low density barium 30 % w/v Retrogastric space – evaluated with additional 200 ml barium , supine position with translateral film Erect RAO- for incisura angularis, c loop of duodenum
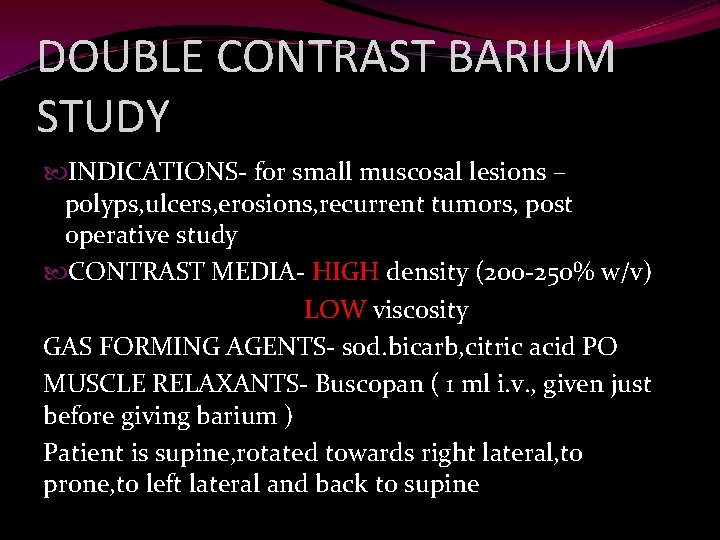
DOUBLE CONTRAST BARIUM STUDY INDICATIONS- for small muscosal lesions – polyps, ulcers, erosions, recurrent tumors, post operative study CONTRAST MEDIA- HIGH density (200 -250% w/v) LOW viscosity GAS FORMING AGENTS- sod. bicarb, citric acid PO MUSCLE RELAXANTS- Buscopan ( 1 ml i. v. , given just before giving barium ) Patient is supine, rotated towards right lateral, to prone, to left lateral and back to supine
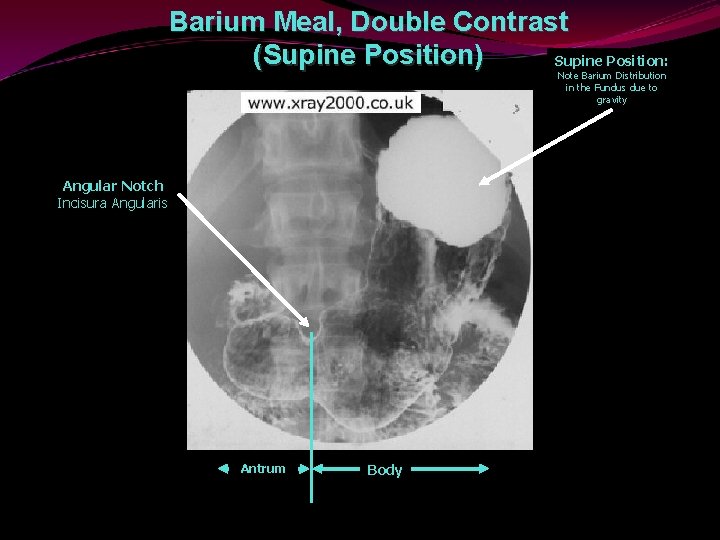
Barium Meal, Double Contrast (Supine Position) Supine Position: Note Barium Distribution in the Fundus due to gravity Angular Notch Incisura Angularis Antrum Body
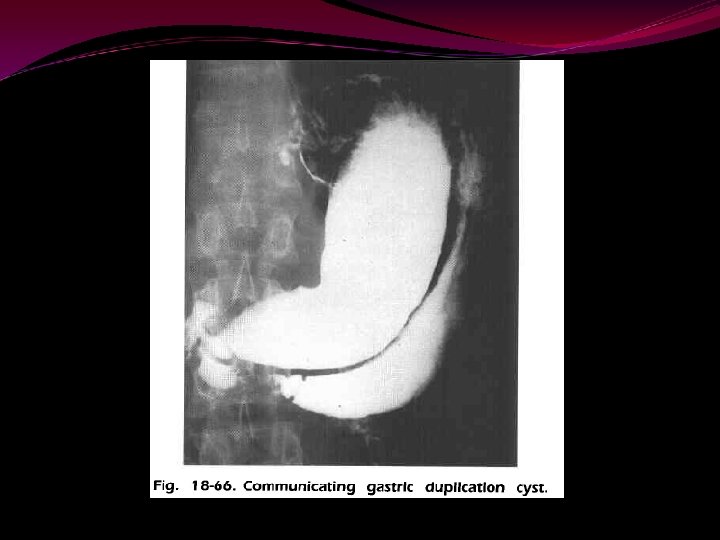
PATHOLOGY
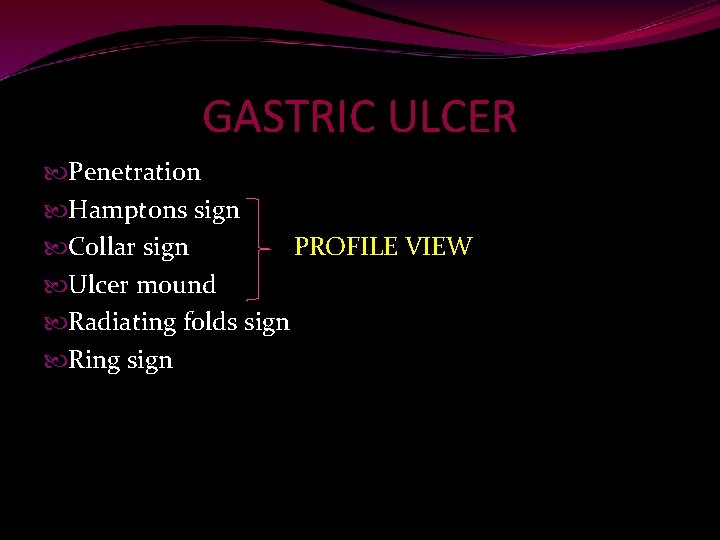
GASTRIC ULCER Penetration Hamptons sign Collar sign PROFILE VIEW Ulcer mound Radiating folds sign Ring sign
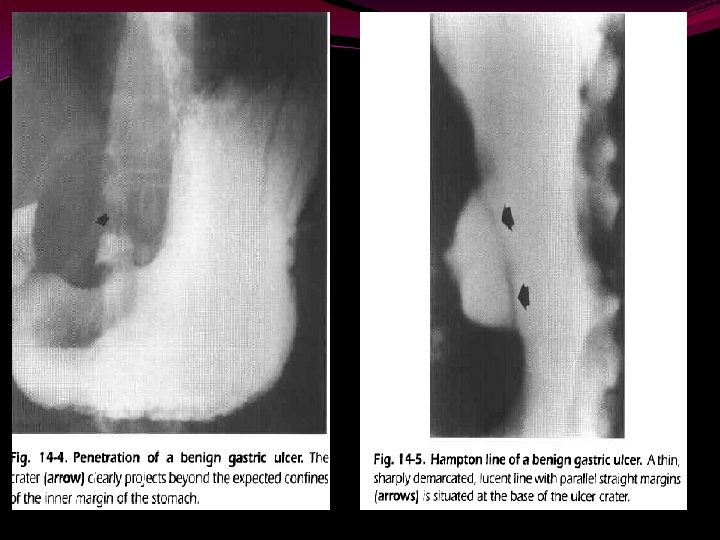

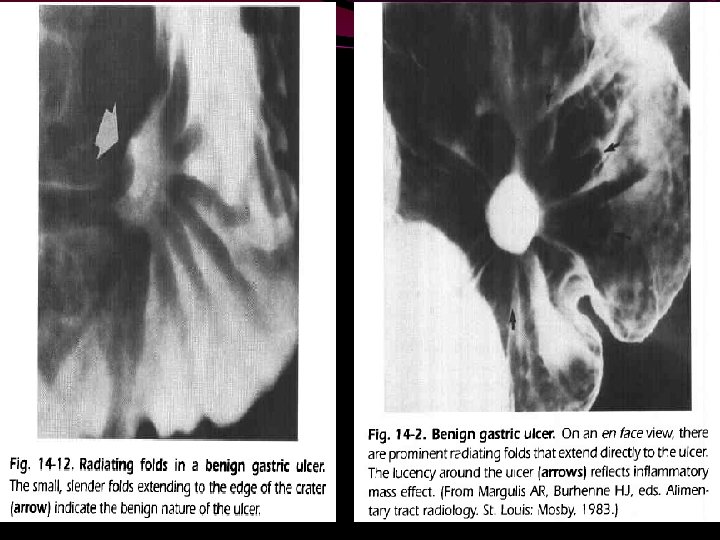
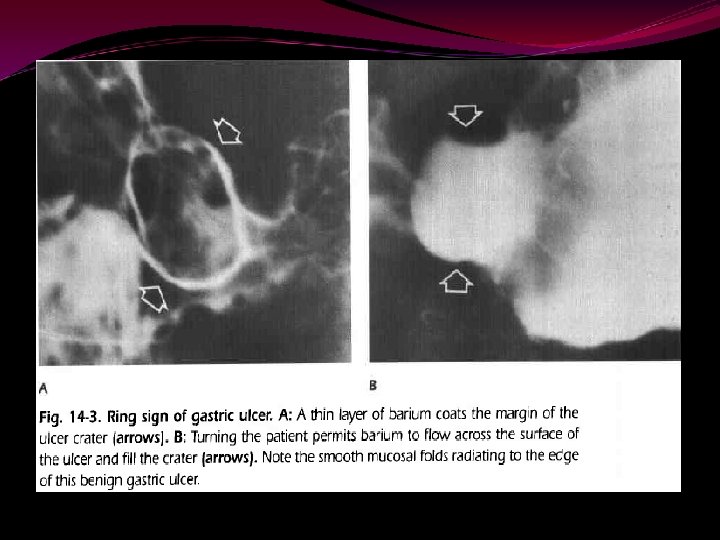
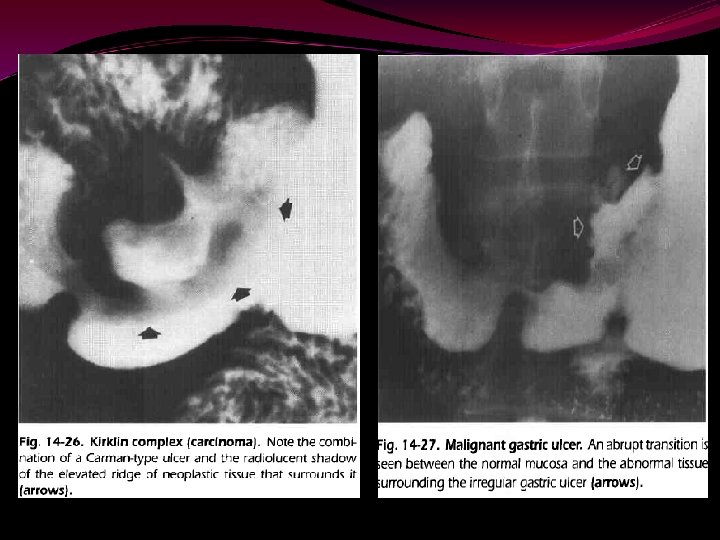
MALIGNANT NATURE OF ULCER Carmans meniscus sign Kirklins complex Abrupt transition between normal mucosa and abnormal mucosa Nodular ulcer mound Distortion/obliteration of adjacent area gastricae Radiating folds- amputation/clubbing/effusion/nodularity Penetration sign- ulcer doesn’t penetrate beyond the normal gastric lumen


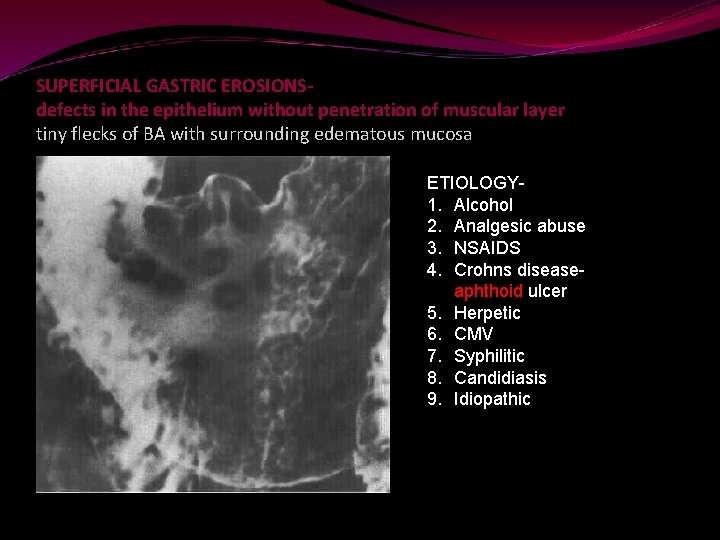
SUPERFICIAL GASTRIC EROSIONSdefects in the epithelium without penetration of muscular layer tiny flecks of BA with surrounding edematous mucosa ETIOLOGY 1. Alcohol 2. Analgesic abuse 3. NSAIDS 4. Crohns diseaseaphthoid ulcer 5. Herpetic 6. CMV 7. Syphilitic 8. Candidiasis 9. Idiopathic
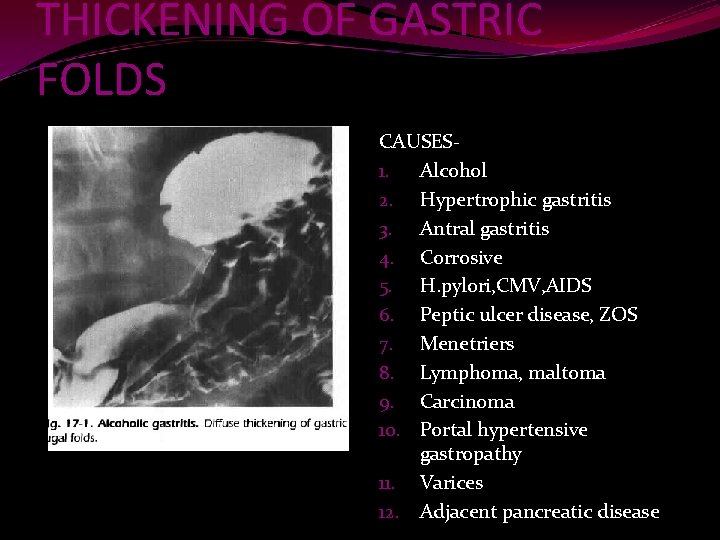
THICKENING OF GASTRIC FOLDS CAUSES 1. Alcohol 2. Hypertrophic gastritis 3. Antral gastritis 4. Corrosive 5. H. pylori, CMV, AIDS 6. Peptic ulcer disease, ZOS 7. Menetriers 8. Lymphoma, maltoma 9. Carcinoma 10. Portal hypertensive gastropathy 11. Varices 12. Adjacent pancreatic disease
Antral folds >5 mm----abnormal All neoplastic processes will show thickened IRREGULAR rugae Gastric varices- multiple filling defects which are variable in size and shape ( df from neoplastic processes) ; also may show extrinsic compression from enlarged spleen
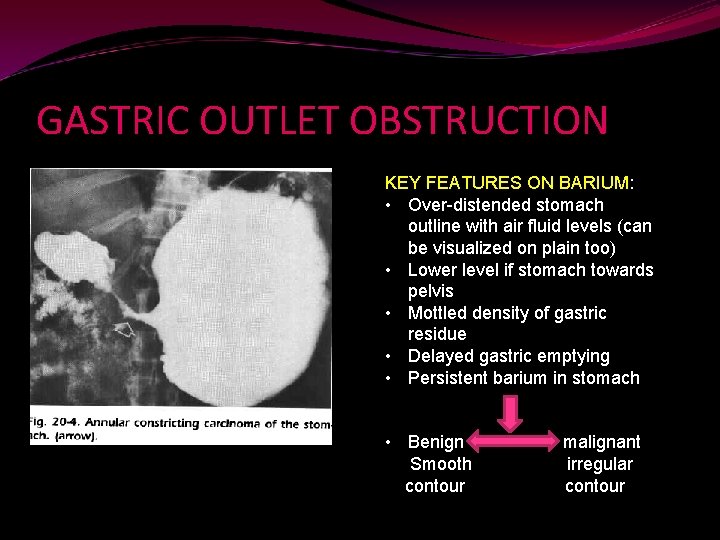
GASTRIC OUTLET OBSTRUCTION KEY FEATURES ON BARIUM: • Over-distended stomach outline with air fluid levels (can be visualized on plain too) • Lower level if stomach towards pelvis • Mottled density of gastric residue • Delayed gastric emptying • Persistent barium in stomach • Benign Smooth contour malignant irregular contour
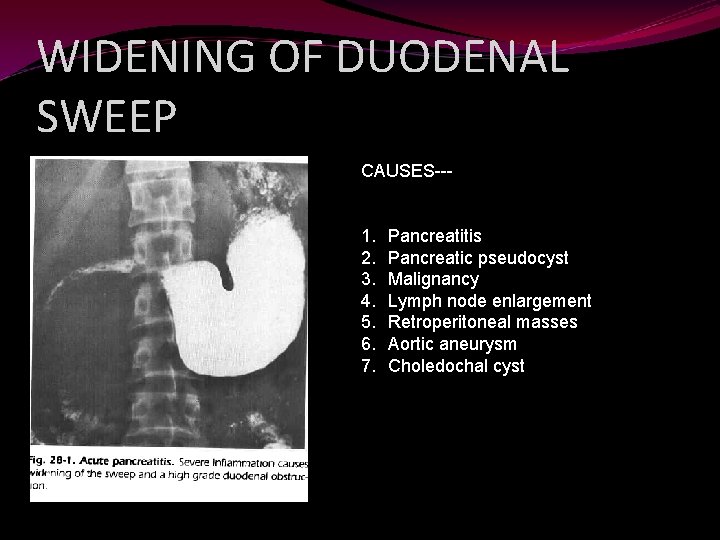
WIDENING OF DUODENAL SWEEP CAUSES--- 1. 2. 3. 4. 5. 6. 7. Pancreatitis Pancreatic pseudocyst Malignancy Lymph node enlargement Retroperitoneal masses Aortic aneurysm Choledochal cyst

BARIUM MEAL FOLLOW THROUGH To evaluate small bowel and the IC junction.
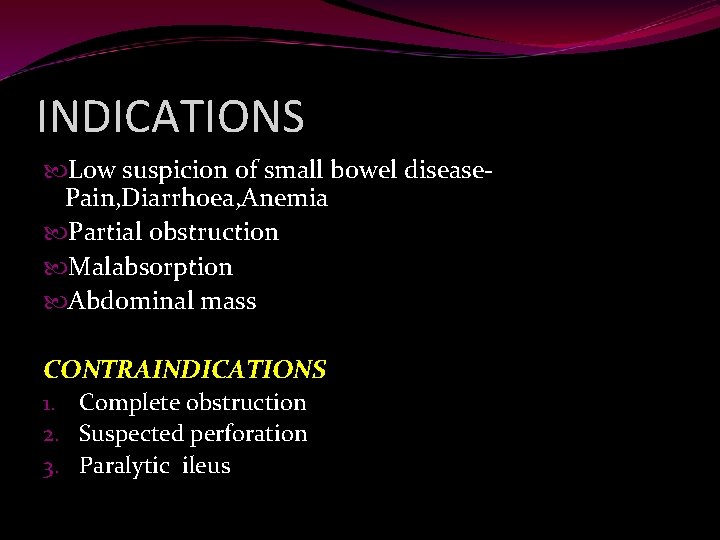
INDICATIONS Low suspicion of small bowel disease. Pain, Diarrhoea, Anemia Partial obstruction Malabsorption Abdominal mass CONTRAINDICATIONS 1. Complete obstruction 2. Suspected perforation 3. Paralytic ileus
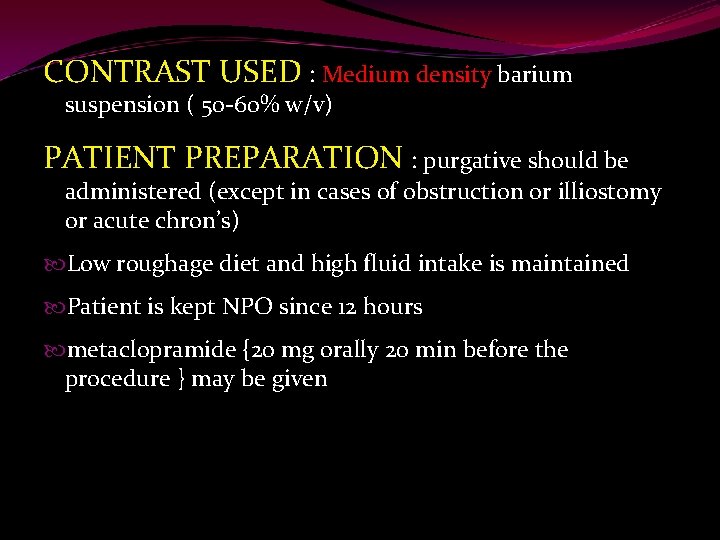
CONTRAST USED : Medium density barium suspension ( 50 -60% w/v) PATIENT PREPARATION : purgative should be administered (except in cases of obstruction or illiostomy or acute chron’s) Low roughage diet and high fluid intake is maintained Patient is kept NPO since 12 hours metaclopramide {20 mg orally 20 min before the procedure } may be given
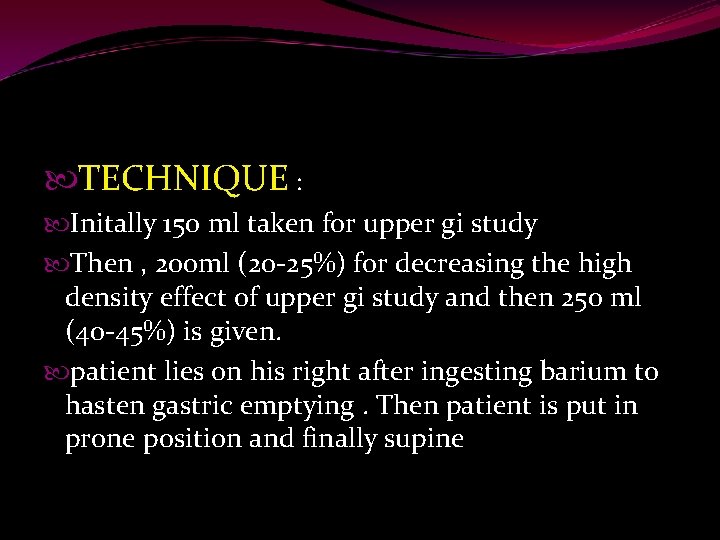
TECHNIQUE : Initally 150 ml taken for upper gi study Then , 200 ml (20 -25%) for decreasing the high density effect of upper gi study and then 250 ml (40 -45%) is given. patient lies on his right after ingesting barium to hasten gastric emptying. Then patient is put in prone position and finally supine
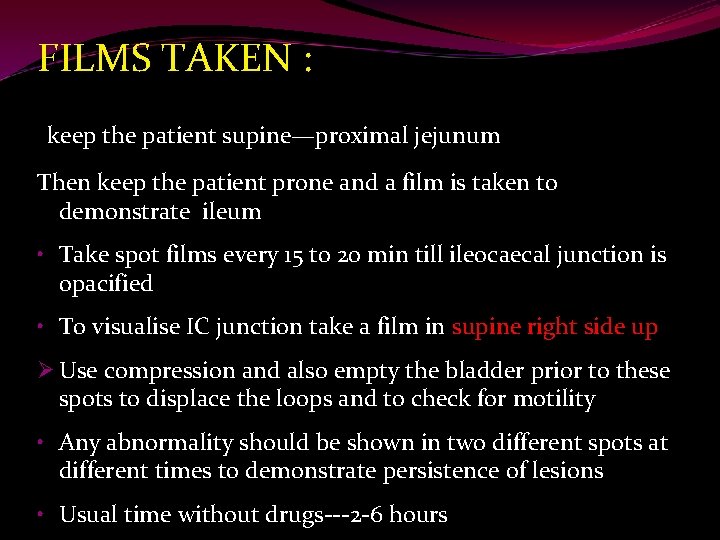
FILMS TAKEN : keep the patient supine—proximal jejunum Then keep the patient prone and a film is taken to demonstrate ileum • Take spot films every 15 to 20 min till ileocaecal junction is opacified • To visualise IC junction take a film in supine right side up Ø Use compression and also empty the bladder prior to these spots to displace the loops and to check for motility • Any abnormality should be shown in two different spots at different times to demonstrate persistence of lesions • Usual time without drugs---2 -6 hours
Advantages of prone position Better separation of bowel loops Compression of abdomen ensuring uniformity of abdomen Ileal loops migrate cephalad
DISADVANTAGES: Overlap may decrease information that can be btained Poor distension of bowel loops Operator dependence Time consuming Intermittent obstruction may be missed ADVANTAGES: -Easy to perform -No intubation is necessary -Transit time can be determined
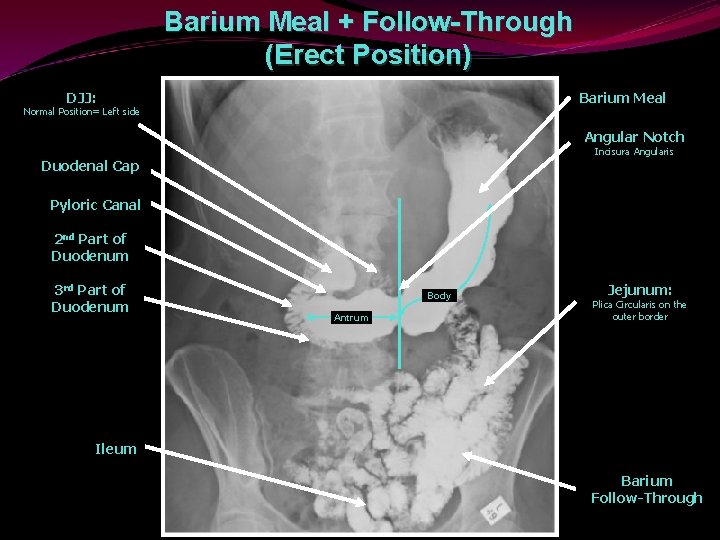
Barium Meal + Follow-Through (Erect Position) DJJ: Barium Meal Normal Position= Left side Angular Notch Incisura Angularis Duodenal Cap Pyloric Canal 2 nd Part of Duodenum 3 rd Part of Duodenum Body Antrum Jejunum: Plica Circularis on the outer border Ileum Barium Follow-Through
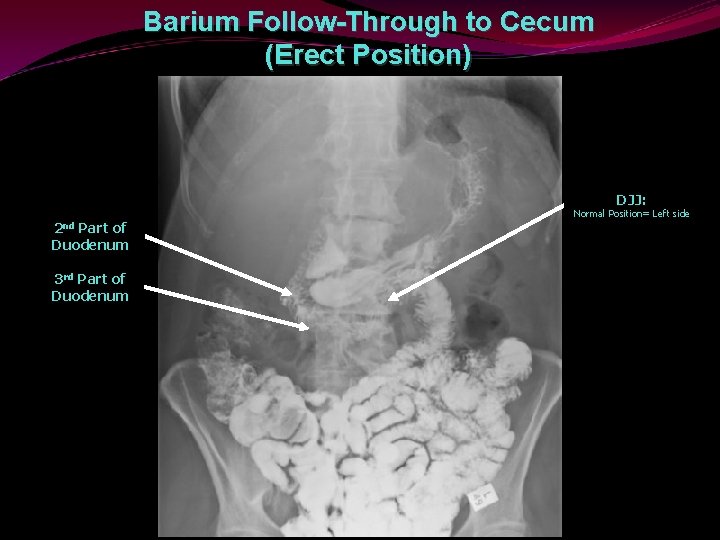
Barium Follow-Through to Cecum (Erect Position) DJJ: 2 nd Part of Duodenum 3 rd Part of Duodenum Normal Position= Left side
ENTEROCLYSIS Indications : Unexplained pain Unexplained diarrhoea Unexplained weight loss To evaluate morphology in a. Crohn’s disease b. Intestinal tuberculosis c. Neoplasms d. Radiation damage
TECHNIQUE: 800 ml of 15 to 20 % w/v suspension used for single contrast technique at 75 -120 ml/min. Naso jejunal [Bilbao- Dotter tube] tube is placed in the proximal jejunum to prevent gastric reflux and vomiting. Spot and prone over head films are taken , high k. V technique For double contrast views 80% w/v of Ba. So 4 & aqueous solution of methylcellulose is used.
Problems Prolonged examination Incomplete distension of small bowel Prolapse of small bowel into the pelvis Faecal material in the terminal ileum Reflux into duodenum and stomach

CT ENTEROCLYSIS 8 F NJ tube is inserted Distilled water infused with a pressure controlled pump i. v. antispasmodic given Helical scanning started 70 s after i. v. contrast ADVANTAGES- intraluminal/extraluminal /intramural pathologies 5 -35 mm pathologies detected Bowel wall thickness can be measured
MR ENTEROCLYSIS Basic procedure is same Iron based and posititve gado contrast agents ADVANTAGES Bowel wall enhancement – assessment of IBD Activity like in UC, CD No radiation- pediatric / pregnant patients
PATHOLOGY
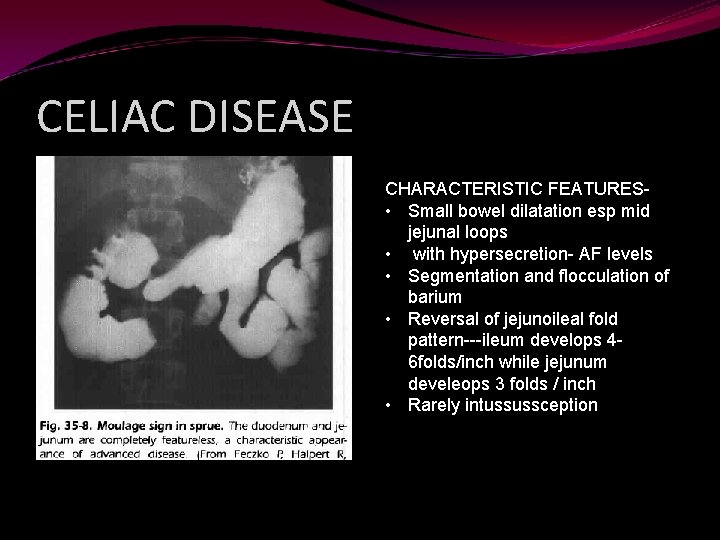
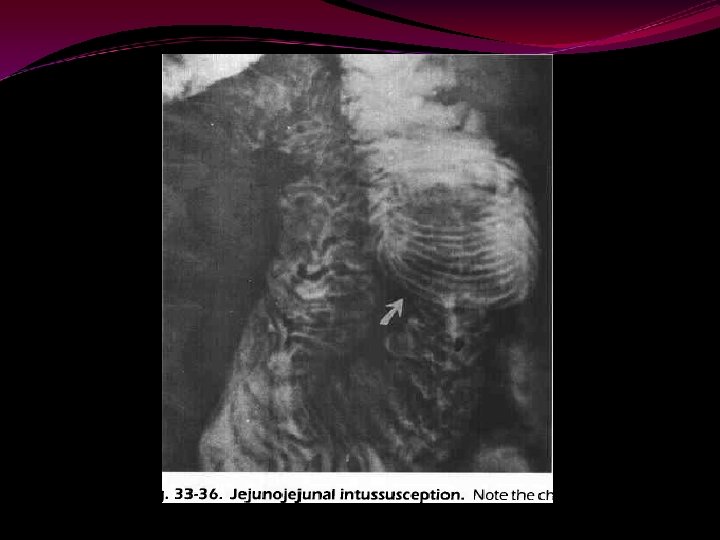
CELIAC DISEASE CHARACTERISTIC FEATURES • Small bowel dilatation esp mid jejunal loops • with hypersecretion- AF levels • Segmentation and flocculation of barium • Reversal of jejunoileal fold pattern---ileum develops 46 folds/inch while jejunum develeops 3 folds / inch • Rarely intussussception
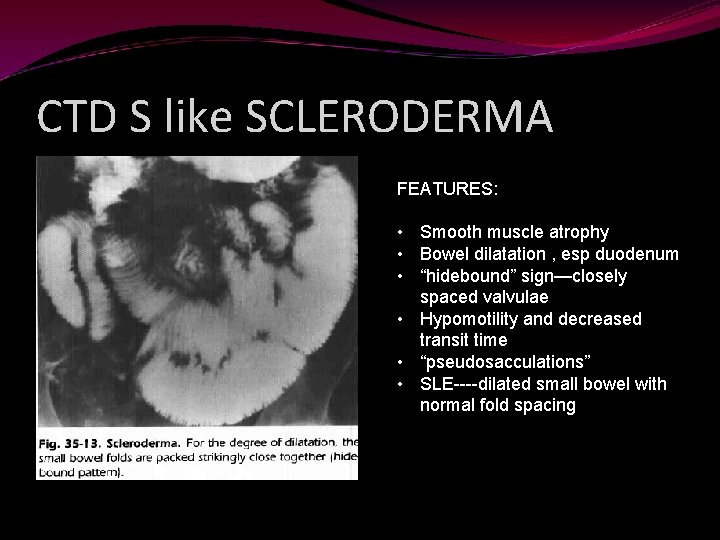
CTD S like SCLERODERMA FEATURES: • Smooth muscle atrophy • Bowel dilatation , esp duodenum • “hidebound” sign—closely spaced valvulae • Hypomotility and decreased transit time • “pseudosacculations” • SLE----dilated small bowel with normal fold spacing
Whipples disease Irregular thickened bowel wall loops
Primary intestinal lymphoma Loss of valvular conniventes
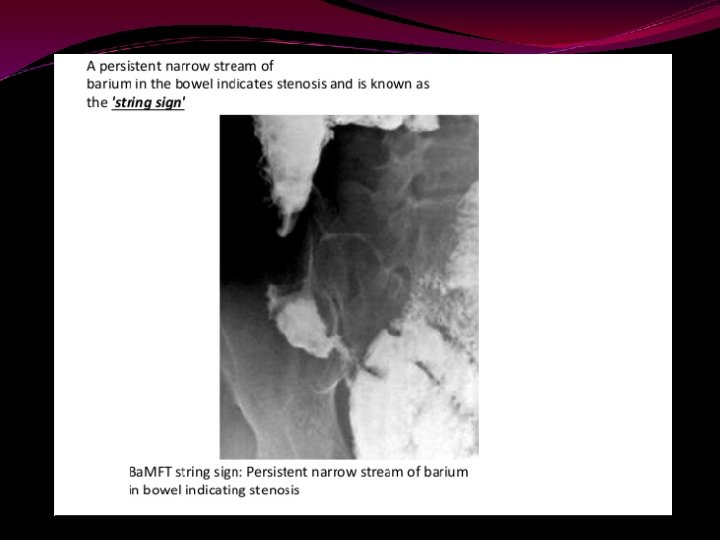
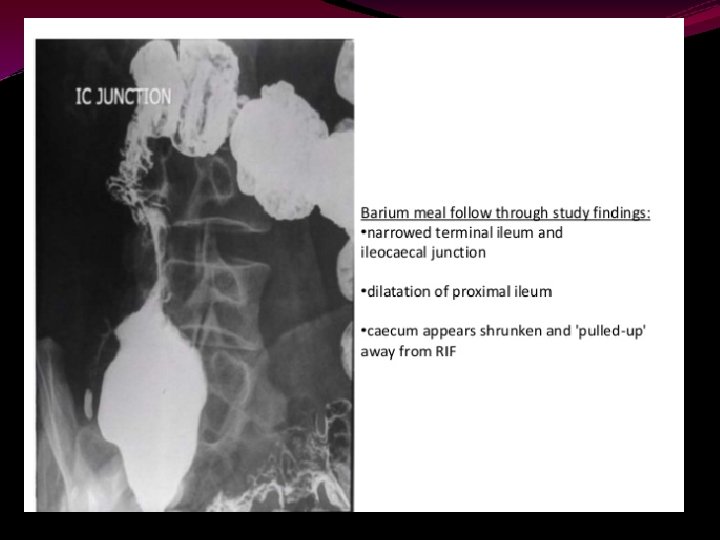
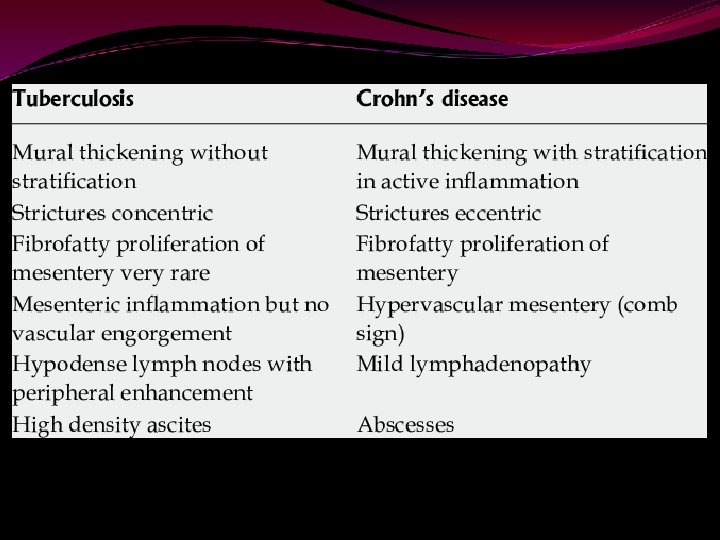
CROHNS DISEASE RADIOGRAPHIC FINDINGS-- diffuse granular mucosal pattern irregular thickening of valvulae conniv cobblestone appearance pipe like narrowing------- “string sign” OTHER FEATURES- skip lesions Mass effect due to adjacent abscesses, indurated mesentery , enlarged lymph nodes Local perforation, fistulae
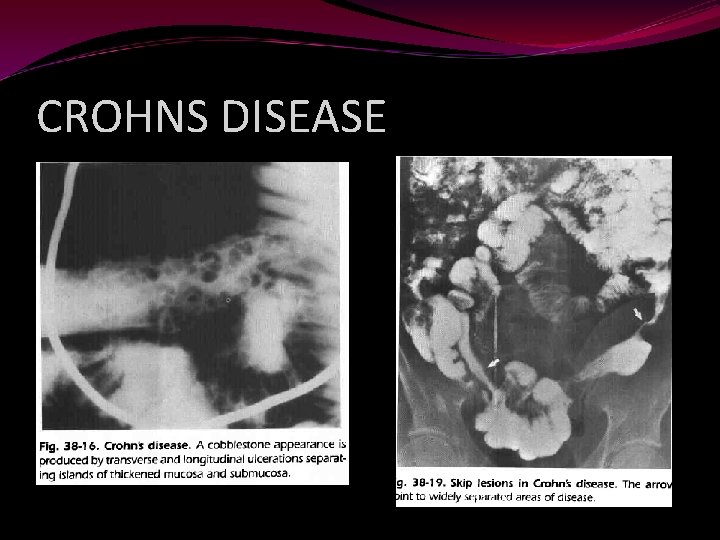
CROHNS DISEASE
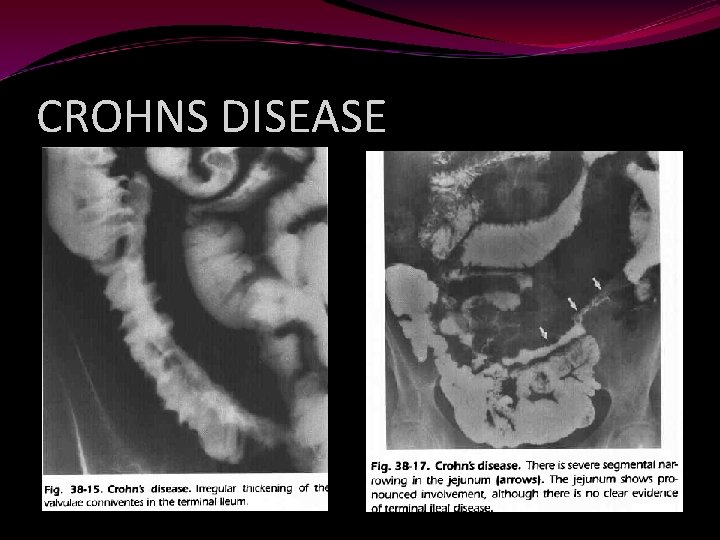
CROHNS DISEASE
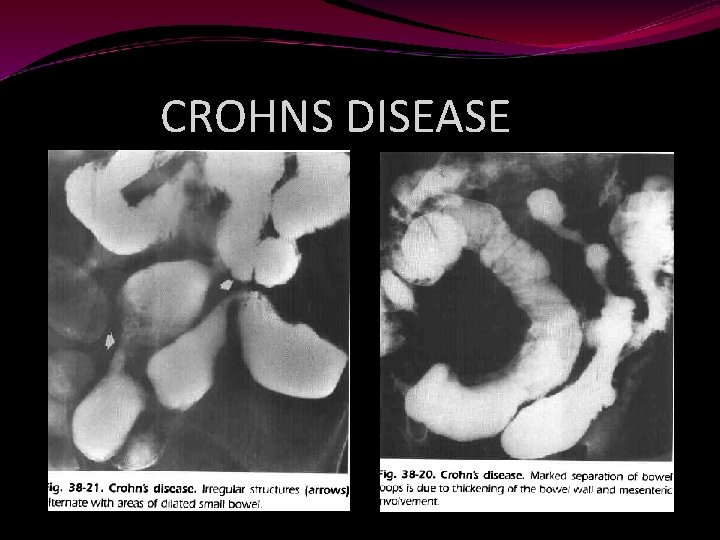
CROHNS DISEASE
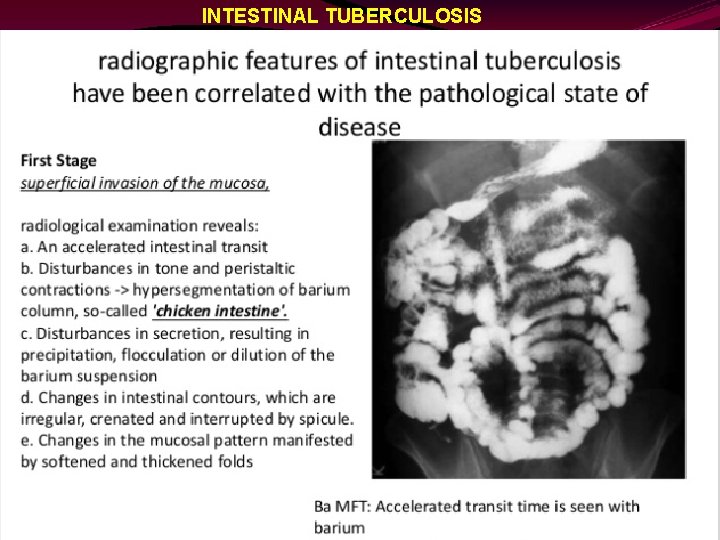
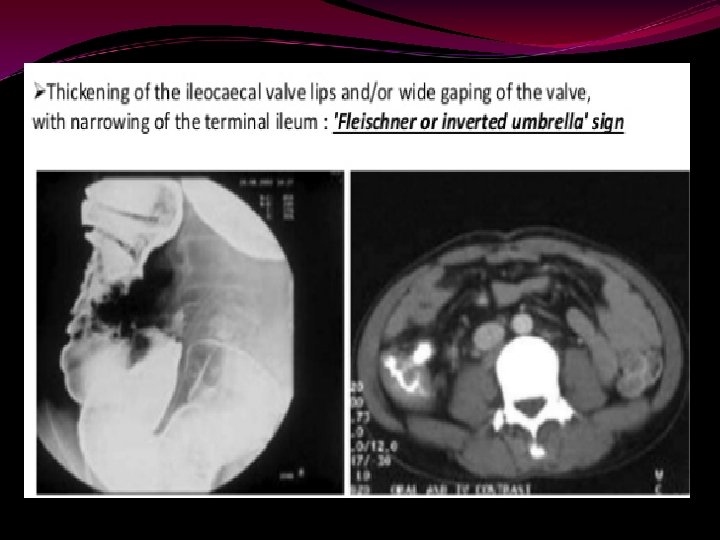
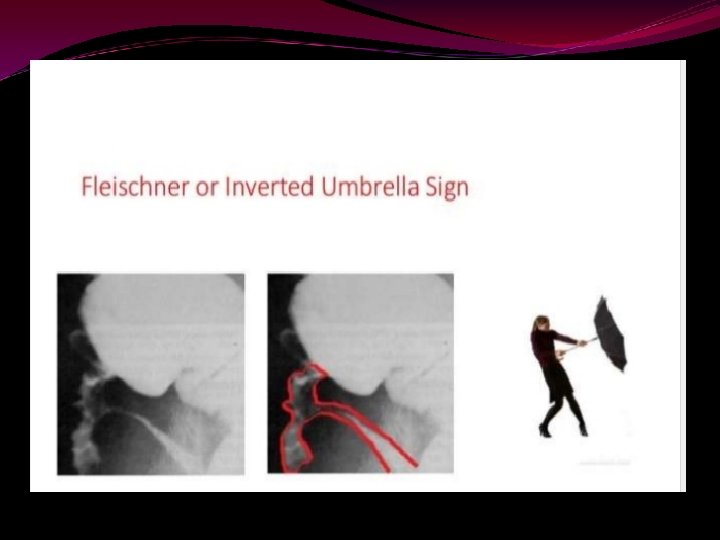
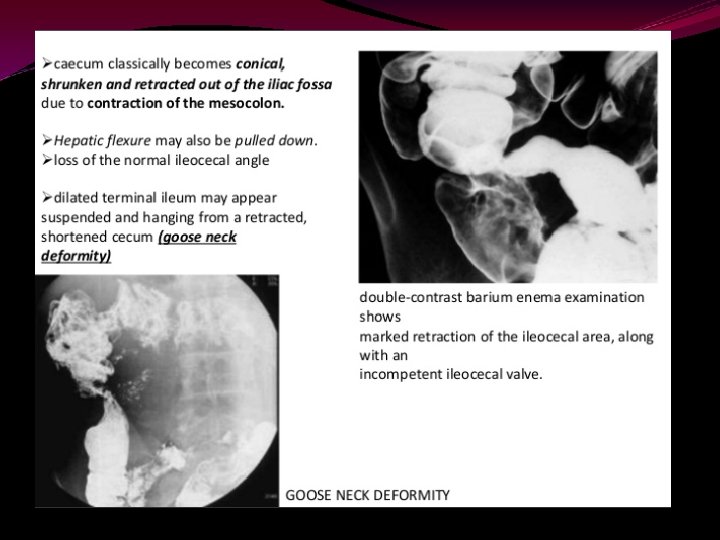
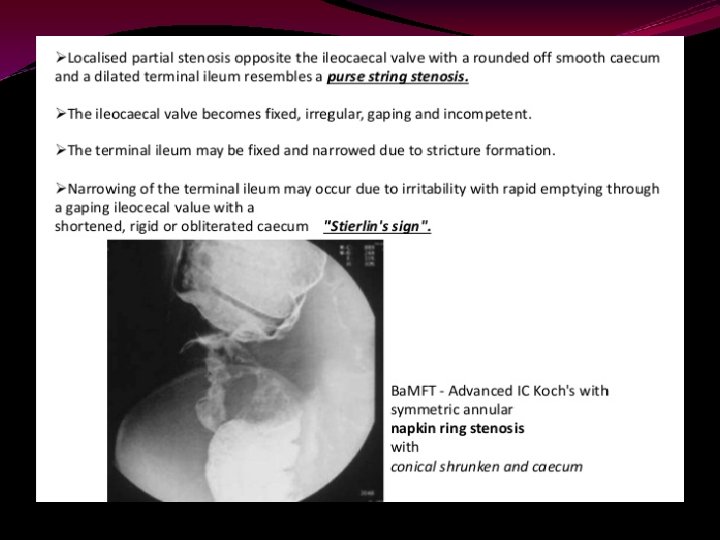
INTESTINAL TUBERCULOSIS
BARIUM ENEMA
INDICATIONS: 1. Change in bowel habbit 2. Pain 3. Mass 4. Melaena/Anaemia 5. Obstruction CONTRAINDICATIONS 1. Toxic megacolon 2. Prior biopsy
Single contrast BE needs low density preparations (12 – 20%w/v)to achieve a see through effect Double contrast BE needs higher density barium (60 – 110%w/v) so that there will be high radiographic density in the thin coating Features of an ideal suspension for DCBE: 1 - should flow easily 2 - should not flocculate 3 - should remain plastic when it dries out 4 - foaming should be minimal {Anti foaming agents like dimethyl polysiloxane are added to destablise bubbles}
BOWEL PREPARATION DIET: Low fiber diet for three days before examination Patient should not have fatty foods Patient is instructed to increase water intake Iron containing medications to be stopped 2 days before the procedure as iron causes adherence of the stool to the mucosa LAXATIVES: Castor oil : cheap unpleasant irritant cathartic Bisacodyl : irritant cathartic , has direct effect on the bowel
MAGNISIUM CITRATE : • saline laxative which is more pleasant • Causes osmotic retention of fluid and increased peristalsis SUMMARY • Tab dulcolax 2 HS • Tap water enema to be done the previous night and 2 hours prior to the procedure • Patient to come on empty stomach on the day of examination
Antibiotic prophylaxis is to be given to patients with Prosthetic heart valves Previous h/o endocarditis Surgically constructed pulmonary shunt Regimens Amoxycillin 1 g + gentamycin 120 mg i. v 15 minutes prior to procedure + amoxycillin 500 mg 6 hours later Vancomycin 1 g slow i. v over 100 min +gentamycin 120 mg i. v prior to start of procedure for penecillin sensitive patients
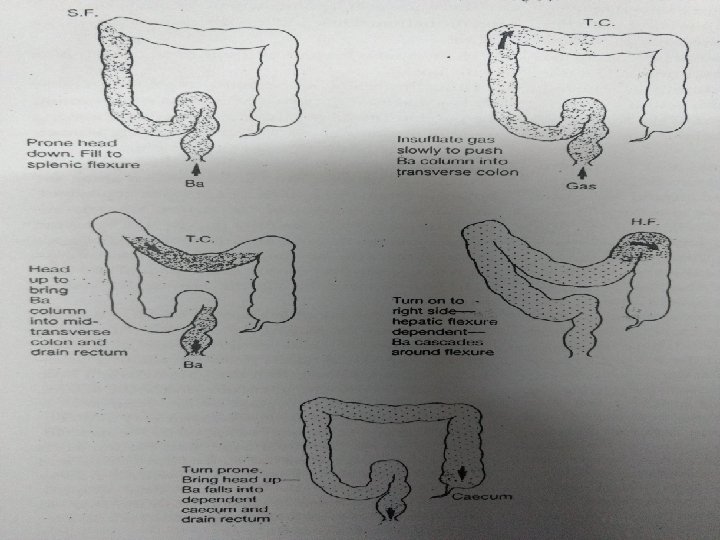
Preliminary film only if: Severe constipation renders bowel preparation ineffective Toxic megacolon is suspected TECHNIQUE Patient lies on one side on an incontinence sheet and the rectal catheter is inserted gently A muscle relaxant may be given i. v Infusion of barium is commenced. Intermittent screening is needed to check progress of barium.
Films are taken to demonstrate each segment clearly Left lateral position for rectum Supine or prone film for the colon Spot films for flexures and caecum Post evacuation films are taken for ulcerative colitis or crohn’s disease. Spot films to be taken of any abnormality seen
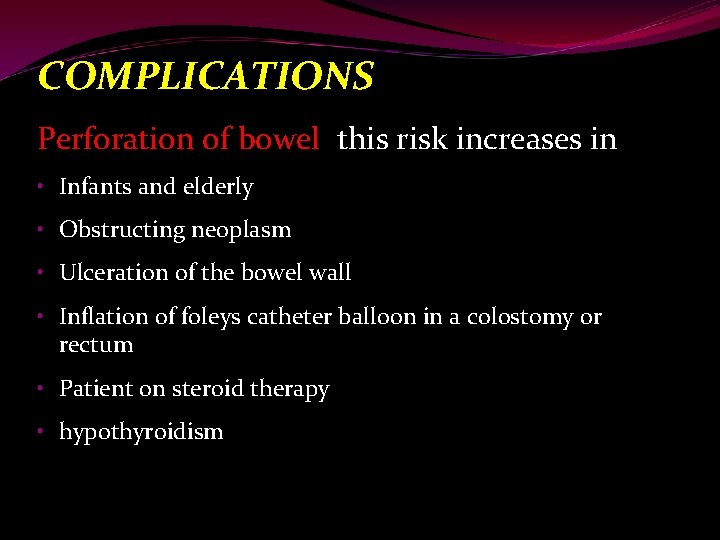
COMPLICATIONS Perforation of bowel this risk increases in • Infants and elderly • Obstructing neoplasm • Ulceration of the bowel wall • Inflation of foleys catheter balloon in a colostomy or rectum • Patient on steroid therapy • hypothyroidism
• Transient bacteremia • Cardiac arrhythmias due to rectal distension • Intramural barium • Venous intravasation
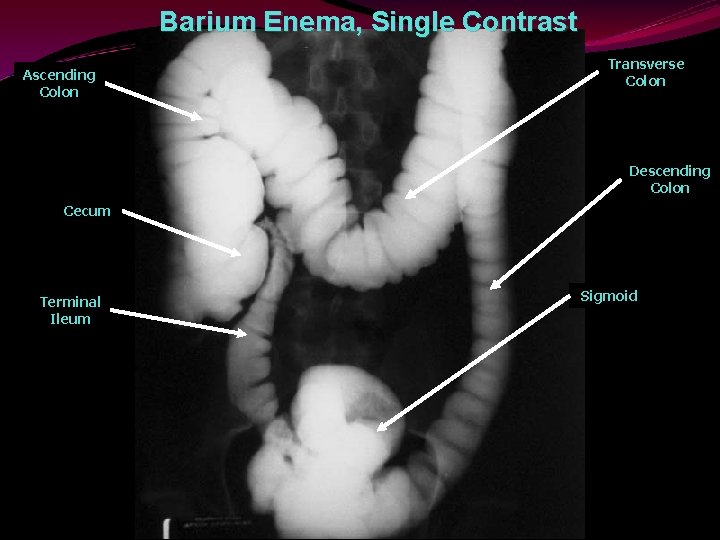
Barium Enema, Single Contrast Ascending Colon Transverse Colon Descending Colon Cecum Terminal Ileum Sigmoid
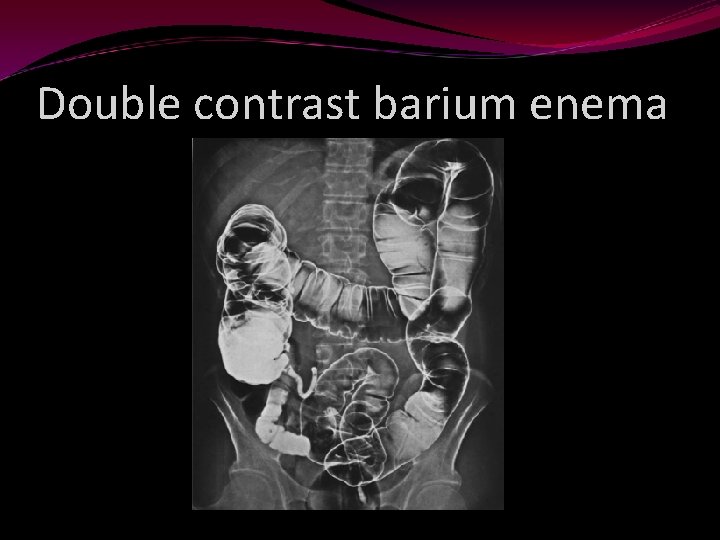
Double contrast barium enema
PATHOLOGY
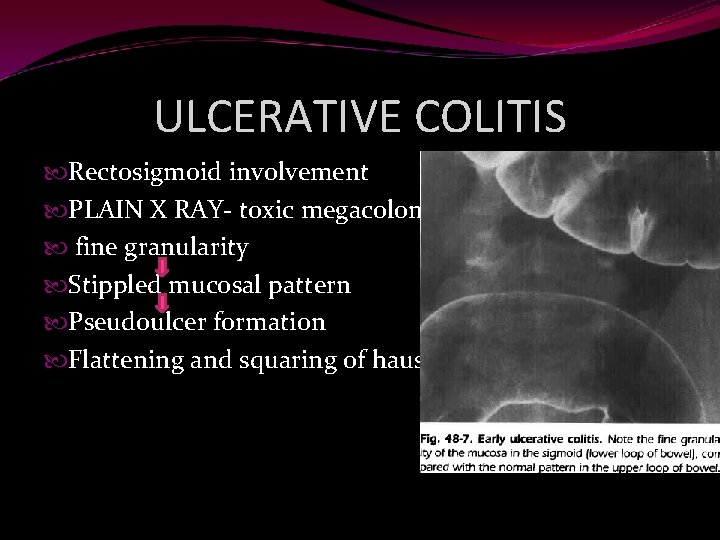
ULCERATIVE COLITIS Rectosigmoid involvement PLAIN X RAY- toxic megacolon/free gas fine granularity Stippled mucosal pattern Pseudoulcer formation Flattening and squaring of haustrae
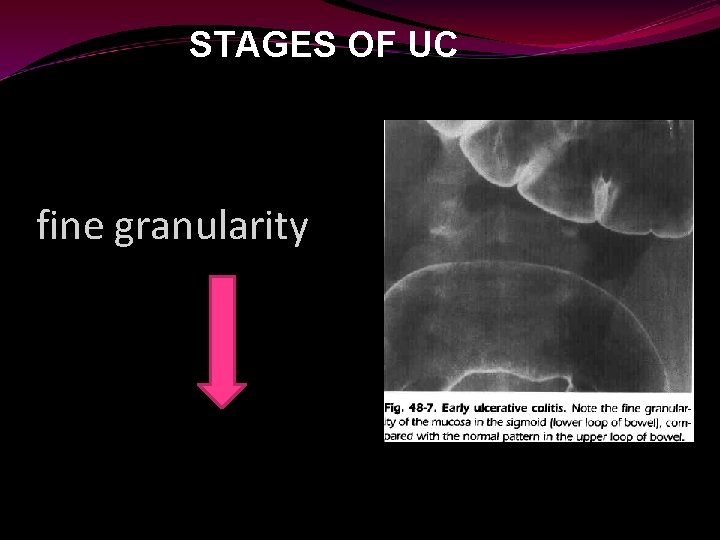
STAGES OF UC fine granularity
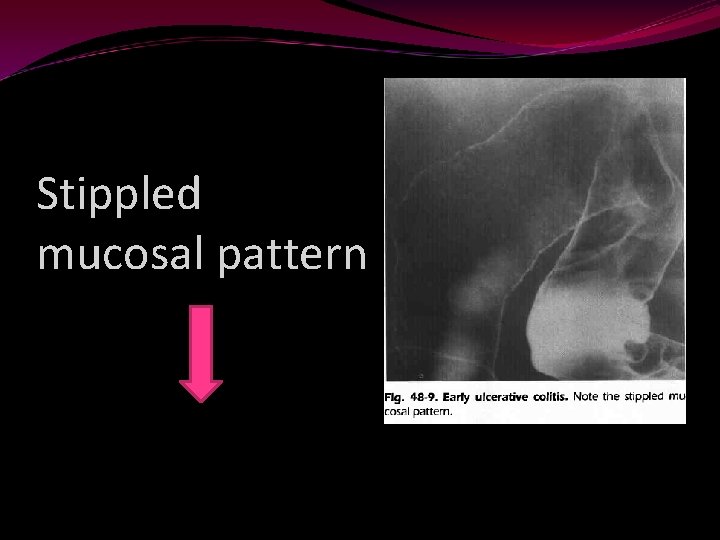
Stippled mucosal pattern
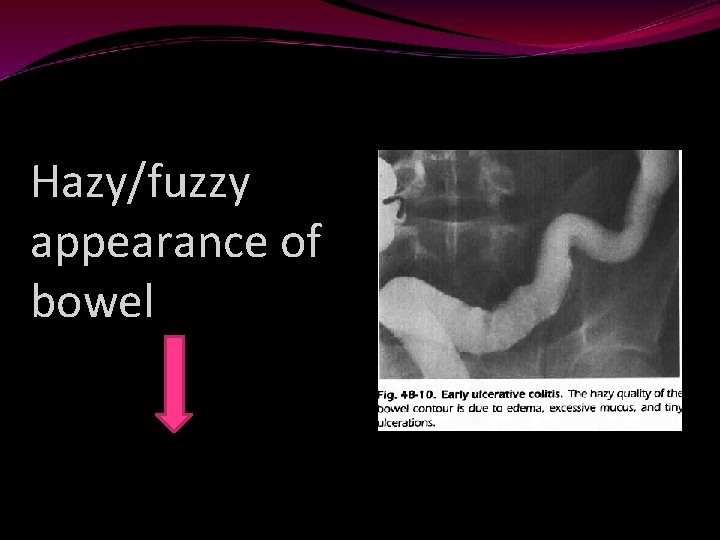
Hazy/fuzzy appearance of bowel
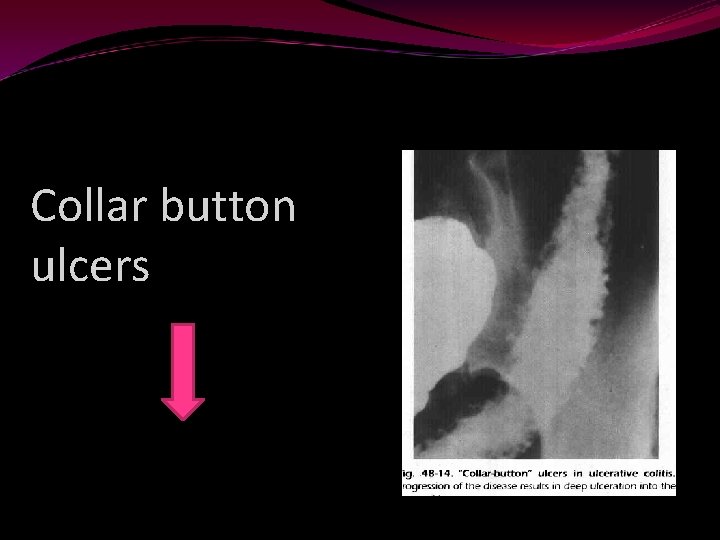
Collar button ulcers
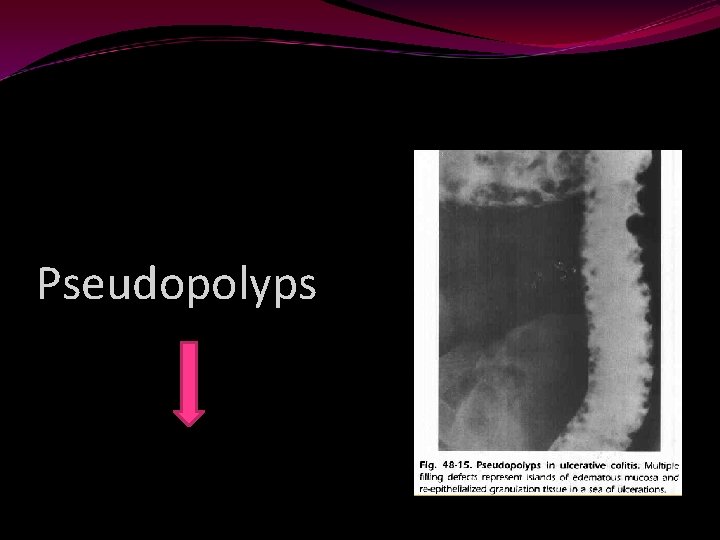
Pseudopolyps
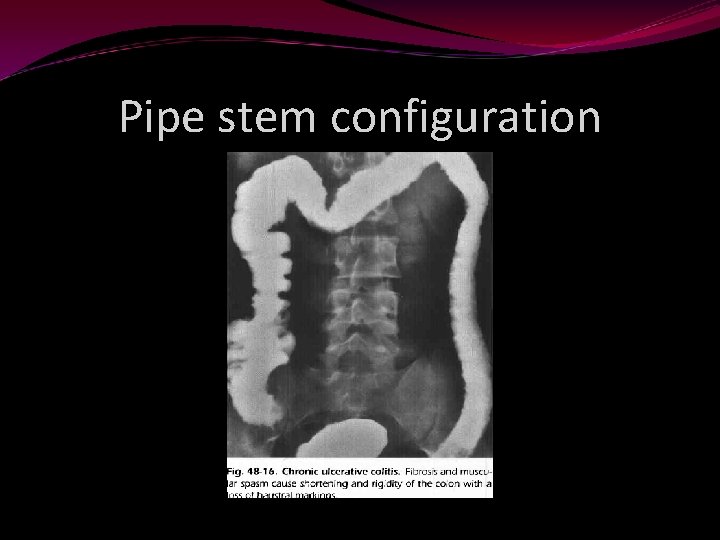
Pipe stem configuration
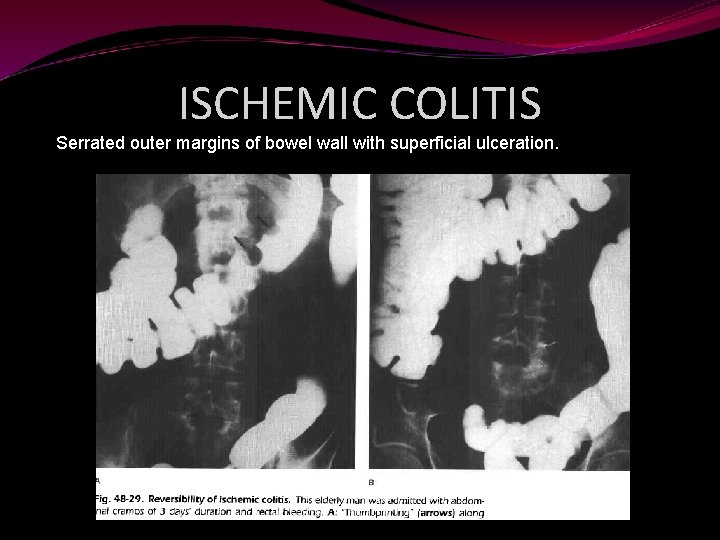
ISCHEMIC COLITIS Serrated outer margins of bowel wall with superficial ulceration.
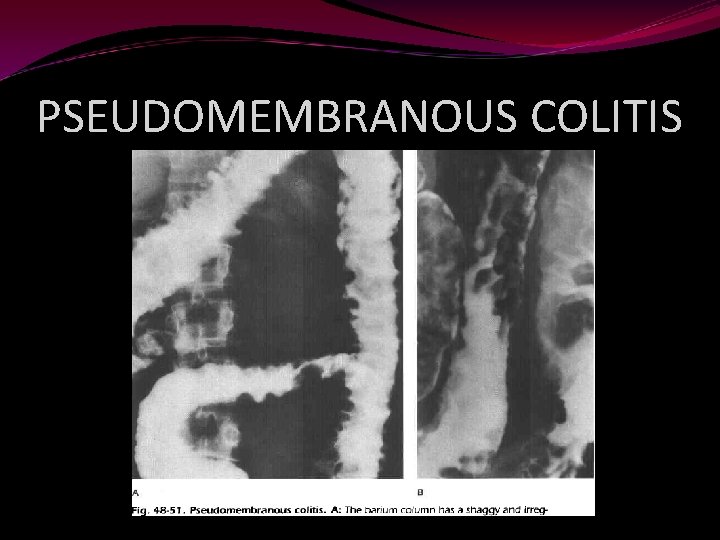
PSEUDOMEMBRANOUS COLITIS
COLONIC POLYPS 1. adenomatous 2. hyperplastic 1. sessile 2. pedunculates On DCBE-- Polyps may be confused with other filling defects likeair bubbles, oil droplets, fecal matter and intraluminal appearing diverticula ( air fluid level, Different projections)
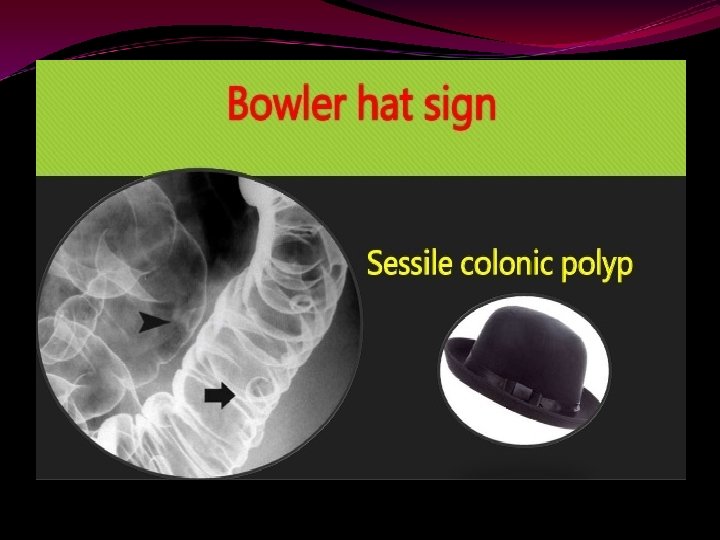
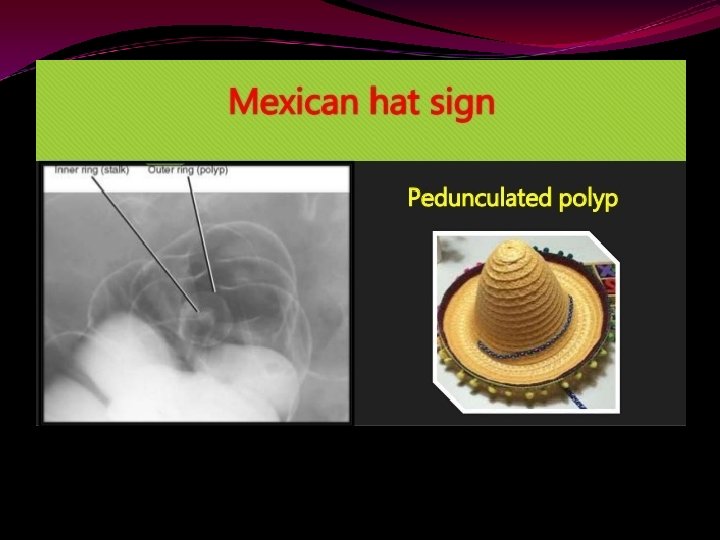
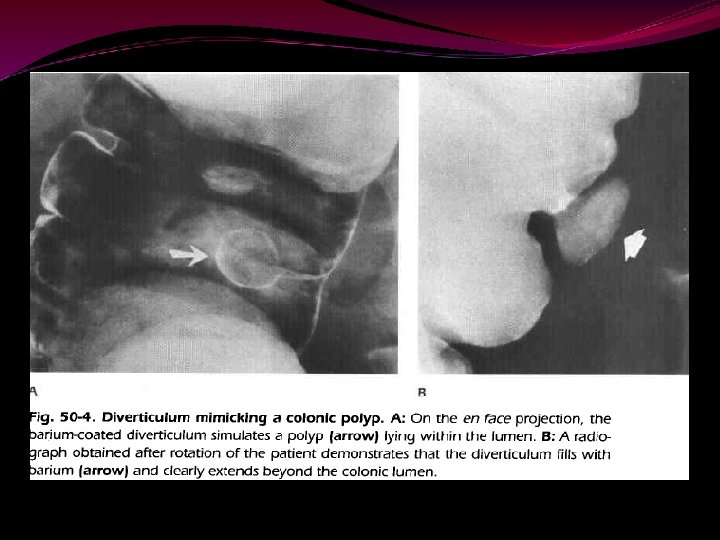
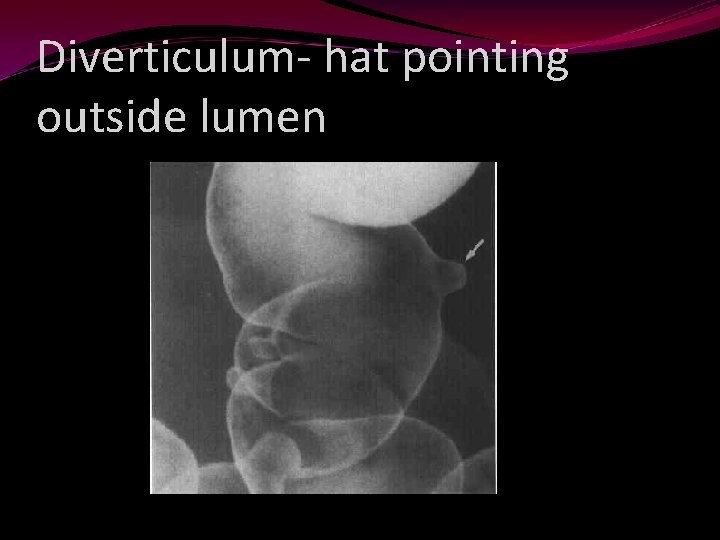
Diverticulum- hat pointing outside lumen
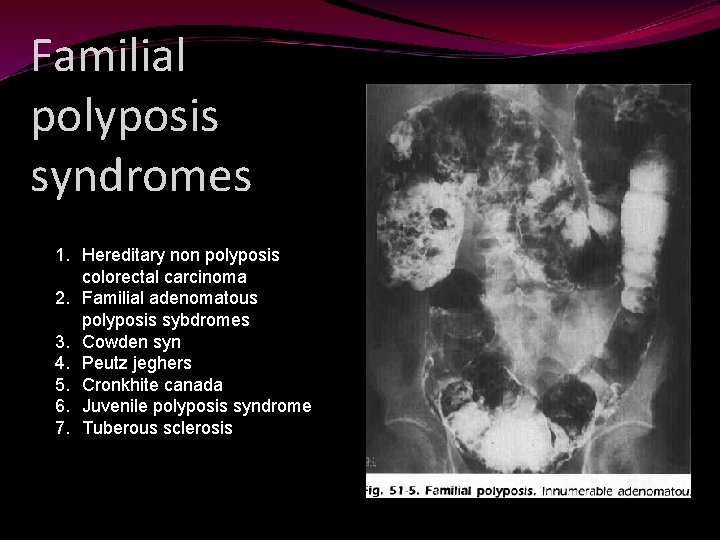
Familial polyposis syndromes 1. Hereditary non polyposis colorectal carcinoma 2. Familial adenomatous polyposis sybdromes 3. Cowden syn 4. Peutz jeghers 5. Cronkhite canada 6. Juvenile polyposis syndrome 7. Tuberous sclerosis
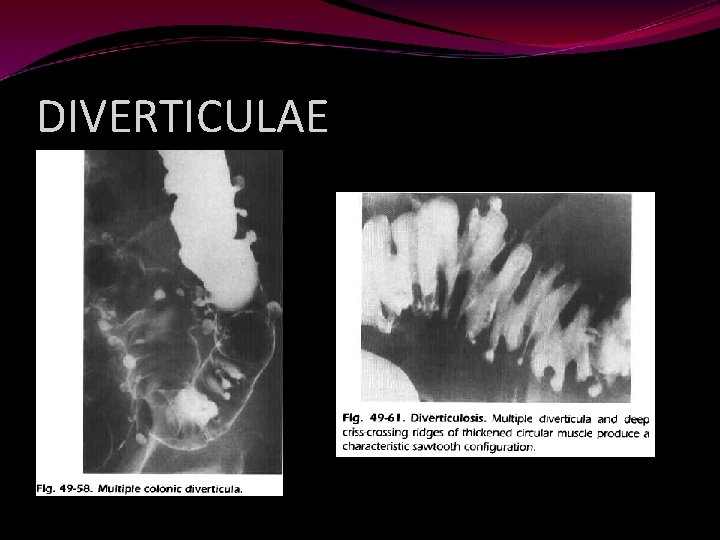
DIVERTICULAE
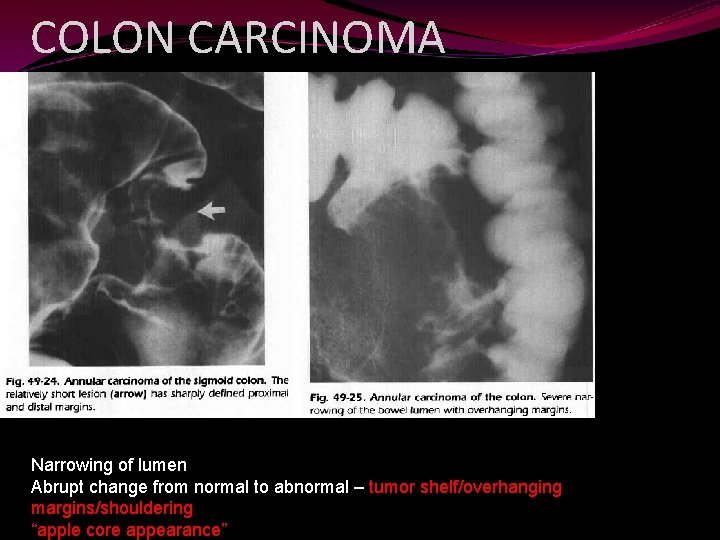
COLON CARCINOMA Narrowing of lumen Abrupt change from normal to abnormal – tumor shelf/overhanging margins/shouldering “apple core appearance”

SPOTTERS
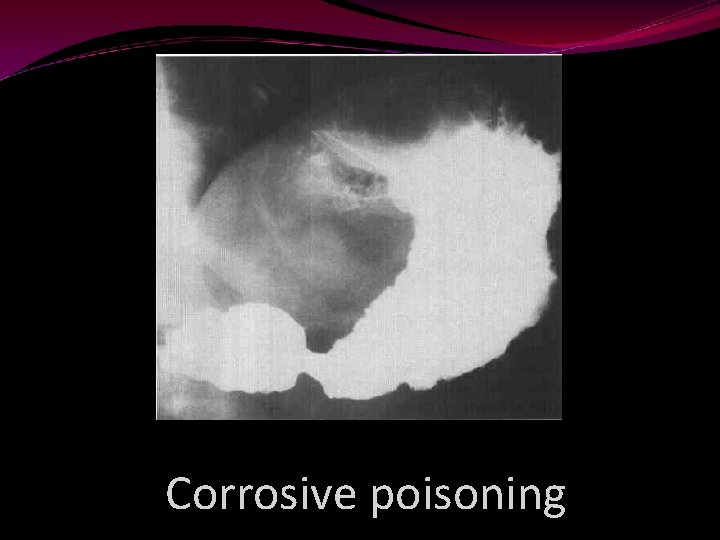
Corrosive poisoning
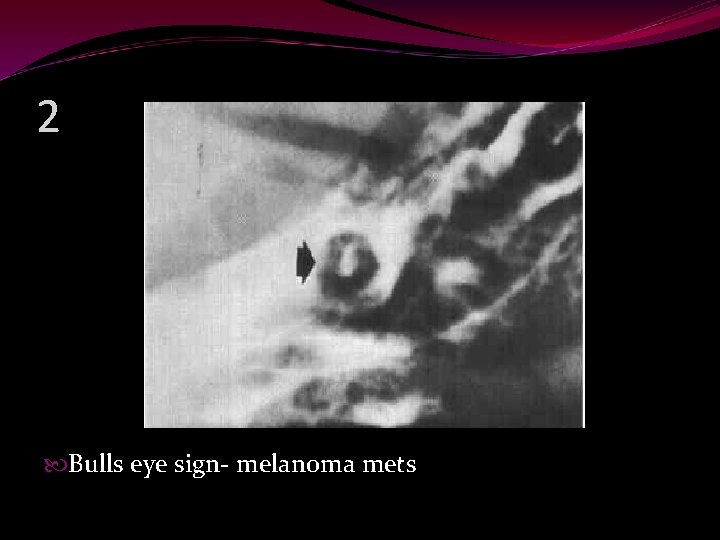
2 Bulls eye sign- melanoma mets

3 Gall stone ileus

4 Gall stone ileus
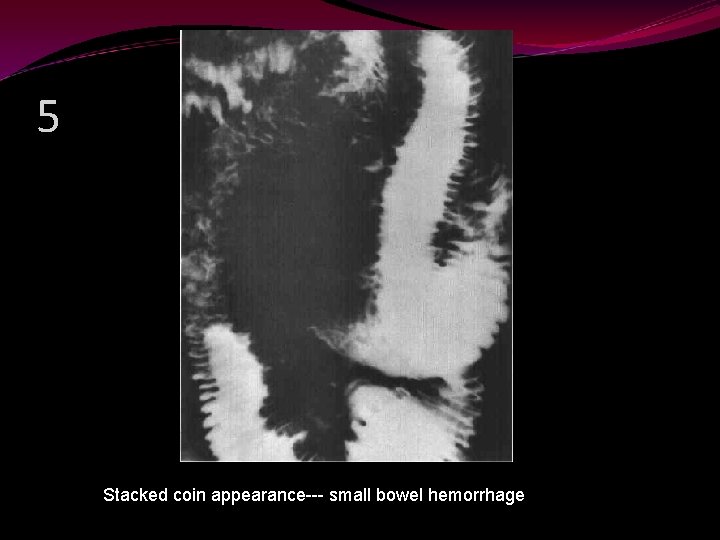
5 Stacked coin appearance--- small bowel hemorrhage

6 Solitary rectal ulcer syndrome
1 corrosive poisoning 2 bull eye – melanoma mets 3 gall stone ileus 4 gall stone ileus 5 picket fence appearance- small bowel h’age 6 solitary rectal ulcer syndrome
INTERESTING QUESTIONS 1. “WATERMELON STOMACH” 2. ONE LOCATION WHERE THE GASTRIC ULCERS ARE DEFINITELY MALIGNANT Rams horn appearance ? ?
1. CHRONIC GI BLEED 2. FUNDUS , ABOVE THE LEVEL OF THE CARDIA 3. appearance of stomach in crohns disease
IT IS PRUDENT TO MENTION HERE, THAT, BARIUM EXAMINATIONS CANNOT BE MADE OBSOLETE! There areas where endoscopy, axial imaging, and physiologic monitoring are inadequate; they are invasive, time consuming, expensive, and not without their shortfallings, ambiguity, and complications. [2, 3] It is primarily the financially driven initiatives that have propagated the use of other complementary modalities as a primary modality(s) of choice over the conventional barium examination. Barium studies, till date, remains the safest, fastest, and cheapest diagnostic investigation to evaluate vague abdominal symptoms and the art has to be revived. [4, 5] Motility disorders of the gastrointestinal tract from pharynx to anus and submucosal lesions are best and quickly evaluated by barium studies. No other modality can be as faster, safer, and more accurate than this age-old barium evaluation. [4, 5] The role of barium evaluation of the bowel in patients with malabsorption is irrefutable. It is useful for both, diagnostic as well as for follow-up to evaluate response to therapy. [5, 6]
REFERENCES EISENBERG-GIT RADIOLOGY 4 TH ED Status of barium studies in the present era of oncology: Are they a history? Abhishek Mahajan, Subash Desai, Nilesh Pandurang Sable, and Meenakshi Haresh Thakur White textbook of procedures Radiology procedures- Lakhar

THANK YOU !
- Slides: 117