BACTERIOLOGY 1 THE GENUS STAPHYLOCOCCUS Dr T V
BACTERIOLOGY 1
THE GENUS STAPHYLOCOCCUS Dr. T. V. Rao MD 2
What are Staphylococcus • Sir Alexander Ogston, a Scottish surgeon, first showed in 1880 that a number of human pyogenic diseases were associated with a cluster-forming micro-organism. He introduced the name 'staphylococcus' (Greek: staphyle = bunch of grapes; kokkos = grain or berry), now used as the genus name for a group of facultatively anaerobic, catalase-positive, Grampositive cocci. 3
Staphylococci: Gram positive cocci ( from Greek staphyle, means bunch of grapes ) that occur singly and in pairs, short chains and irregular grape-like clusters. Dr. T. V. Rao MD 4
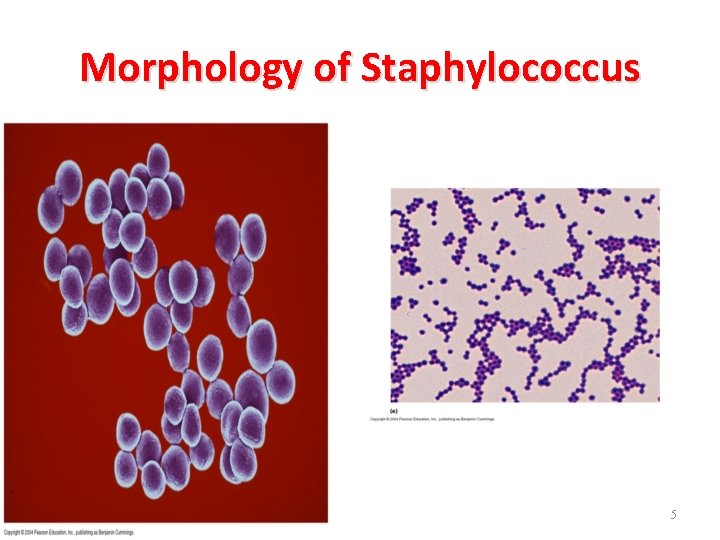
Morphology of Staphylococcus 5
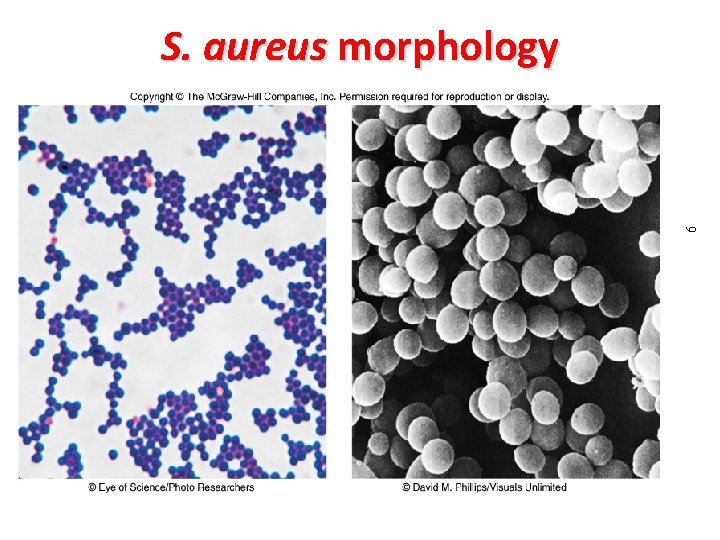
6 S. aureus morphology
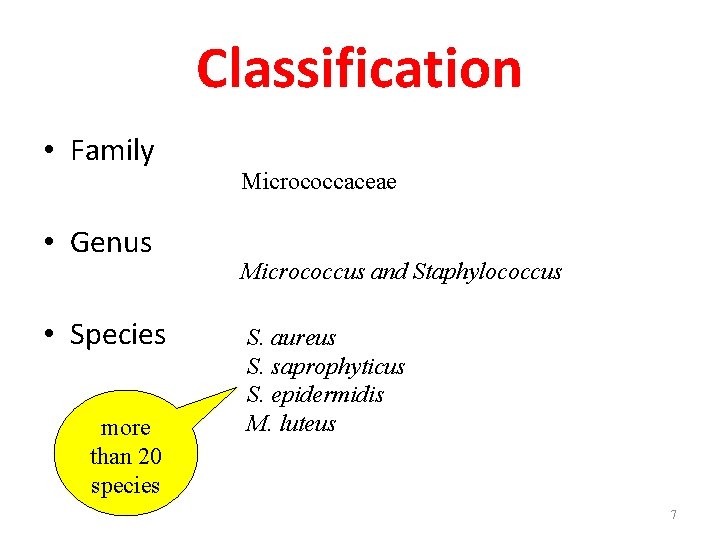
Classification • Family • Genus • Species more than 20 species Micrococcaceae Micrococcus and Staphylococcus S. aureus S. saprophyticus S. epidermidis M. luteus 7
The genus Staphylococcus contains about forty species and subspecies today. • Only some of them are important as human pathogens: –Staphylococcus aureus –Staphylococcus epidermidis –Staphylococcus hominis –Staphylococcus haemolyticus –Staphylococcus saprophyticus –others 8
Morphology and Physiology • Gram-positive cocci, nonmotile, facultative anaerobes • Cells occur in grapelike clusters because cells division occurs along different planes and the daughter cells remain attached to one another • Salt-tolerant: allows them to tolerate the salt present on human skin • Tolerant of desiccation: allows survival on environmental surfaces (fomites) 9
The species Staphylococcus aureus • Morphology – Polysaccharide capsule is only rarely found on cells. – The peptidoglycan layer is the major structural component of the cell wall. It is important in the pathogenesis of staphylococcal infections. Other important component of cell wall is teichoic acid. – Protein A is the major protein component of the cell wall. It is located on the cell surface but is also released into the culture medium during the cell growth. A unique property of protein A is its ability to bind to the Fc part of all Ig. G molecules except Ig. G 3. It is not an antigen-antibody specific reaction. 10
Cultural characters • • Grow readily on ordinary media Temperature – optimum 37 C Ph 7. 4 to 7. 6 Aerobes and facultative anaerobes. 11
Cultural Characters Nutrient agar : • large, circular, convex, smooth, shiny, opaque and easily emulsifiable. • Golden yellow pigment. • Some may produce white , orange or yellow. • Pigment production is enhanced – 1% glycerol monoacetate or milk is added. • NA slope – oil paint appearance. 12
Cultural Characters Blood agar: • Similar colonies like blood agar • Hemolytic at 20 -25% CO 2. • Hemolysis – rabbit or sheep blood, weak – horse blood • Human blood should not be used. 13
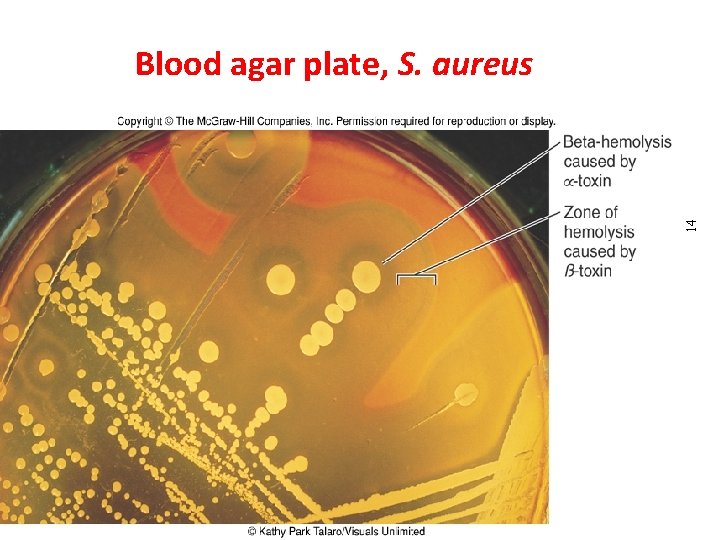
14 Blood agar plate, S. aureus Dr. T. V. Rao MD
Cultural Characters Maconkey agar • Small pink LF colonies Liquid media : • Uniform turbidity 15
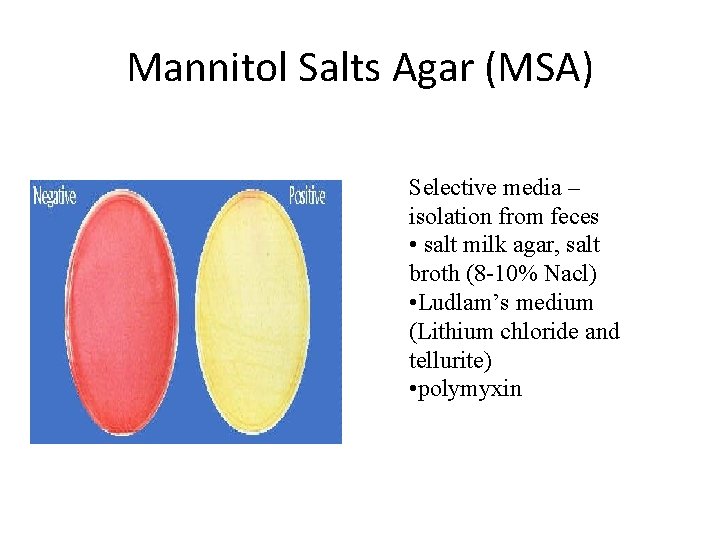
Mannitol Salts Agar (MSA) Selective media – isolation from feces • salt milk agar, salt broth (8 -10% Nacl) • Ludlam’s medium (Lithium chloride and tellurite) • polymyxin
Biochemical Reactions • • • Catalase positive Hydrolyse urea Reduce nitrates to nitrites Liquefy gelatin MR and VP positive 17
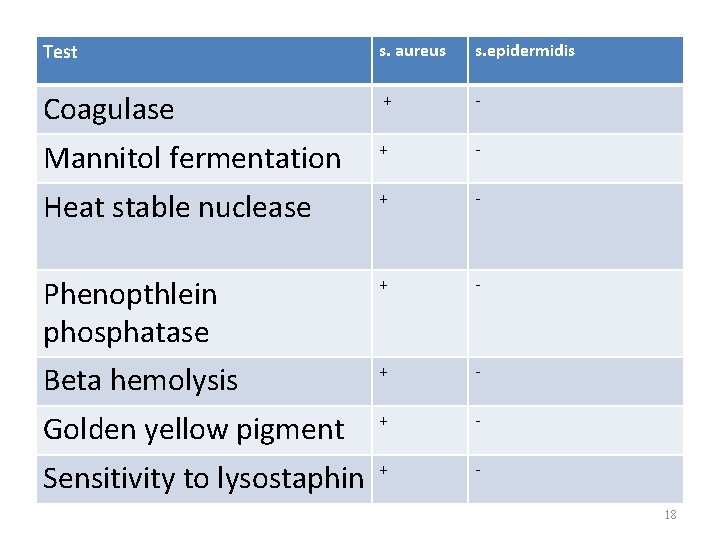
Test s. aureus s. epidermidis Coagulase + - Mannitol fermentation + - Heat stable nuclease + - Phenopthlein phosphatase + - Beta hemolysis + - Golden yellow pigment + - Sensitivity to lysostaphin + 18
Resistance • • • Withstand 60°C for 30 minutes. Thermal death point – 62°C for 30 minutes. Resist 1% phenol for 15 minutes. Resistant to lysozymes Generally sensitive to lysostaphin. Sensitive to penicillin 19
Penicillin Resistance • Production of beta lactamase • Changes in bacterial surface receptors • Tolerance to penicillin 20
The genus Staphylococcus can be divided into two subgroups (on the basis of its ability to clot blood plasma by enzyme coagulase): • coagulase-positive, • coagulase-negative. 21
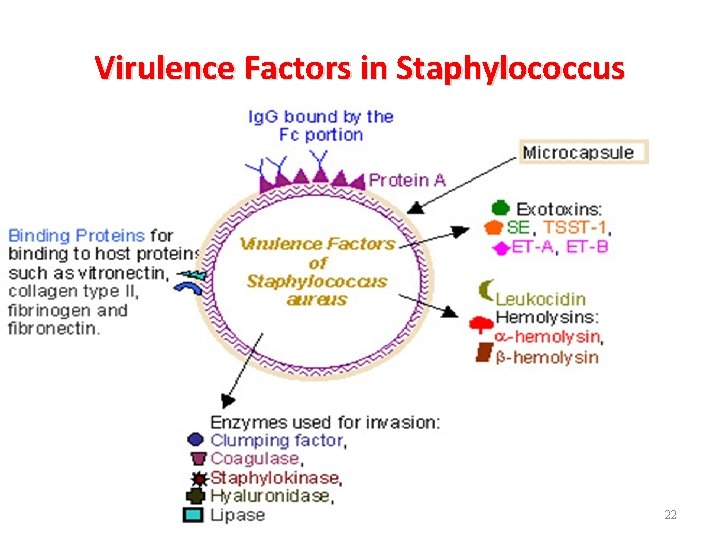
Virulence Factors in Staphylococcus Dr. T. V. Rao MD 22
Virulence factors Cell associated polymers • Capsule or polysaccharide slime layer • Peptidoglycan layer • Teichoic acid Cell surface proteins • Protein A • Cytoplasmic membrane • Clumping factor 23
Capsule or polysaccharide slime layer • A loose-fitting, polysaccharide layer (slime layer) is only occasionally found in staphylococci cultured in vitro, but is believed to be more commonly present in vivo. • Eleven capsular serotypes have been identified in S. aureus, with serotypes 5 and 7 associated with majority of infections. • Inhibits opsonisation. 24
Capsule helps Staphylococcus • The capsule protects the bacteria by inhibiting the chemotaxis and phagocytosis of staphylococci by polymorph nuclear leukocytes, as well as by inhibiting the proliferation of mononuclear cells. • It is also facilitates the adherence of bacteria to catheters and other synthetic material. 25
Peptidoglycan • Half of the cell wall by weight is peptidoglycan, a feature common to gram-positive bacteria. • The subunits of peptidoglycan are N-acetylmuramic acid and N-acetylglucosoamine. • Elicits production of IL-1 and opsonic antibodies by monocytes, chemoattractant fpr polymorphonuclear leukocytes (endotoxin like activity) and activate complement. 26
Teichoic acid • Teichoic acid is species-specific, phosphatecontaining polymers that are bound covalently to the peptidoglycan layer or through lipophilic linkage to the cytoplasmic membrane (lipoteichoic acid). • Teichoic acid mediates the adhesion of cocci to the host cell surface and protects them from complement mediated opsonisation. 27
CELL SURFACE PROTEINS 28
Protein A • The surface of most S. aureus strains (but not the coagulase-negative staphylococci) is uniformly coated with protein A. • This protein is covalently linked to the peptidoglycan layer and has a unique affinity for binding to the Fc receptor of immunoglobulin Ig. G. • The presence of protein A has been exploited in some serological tests, in which protein A-coated S. aureus is used as a nonspecific carrier of antibodies directed against other antigens. • Additionally, detection of protein A can be used as a specific identification test for S. aureus. 29
Coagulase and other surface proteins • The outer surface of most strains of S. aureus contains clumping factor (also called bound coagulase). • This protein binds fibrinogen, converts it to insoluble fibrin, causing the staphylococci to clump or aggregate. • Detection of this protein is the primary test for identifying S. aureus. 30
• Other surface proteins that appear to be important for adherence to host tissues include: • collagen-binding protein • elastin-binding protein • fibronectin-binding protein 31
Staphylococcal enzymes –Coagulase –Lipases –Hyaluronidase –Nuclease –Fibrinolysin –Penicillinase 32
Enzymes 1. Coagulase – Triggers blood clotting 2. Hyaluronidase or Staphylokinase – Breaks down hyaluronic acid, enabling the bacteria to spread between cells 33
Enzymes (cont. ) 3. Lipases – Digest lipids, allowing staphylococcus to grow on the skin’s surface and in cutaneous oil glands 4. -lactamase – Breaks down penicillin – Allows the bacteria to survive treatment with -lactam antimicrobial drugs 34
Coagulase • S. aureus strains possess two forms of coagulase: – bound, – free. • Coagulase bound to the staphylococcal cell wall can directly convert fibrinogen to insoluble fibrin and cause the staphylococci to clump. • The cell-free coagulase accomplishes the same result by reacting with a globulin plasma factor. 35
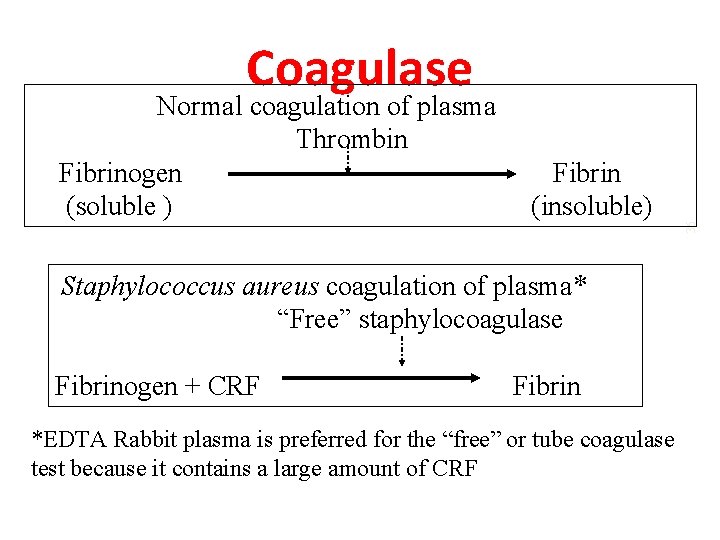
Normal coagulation of plasma Thrombin Fibrinogen (soluble ) Fibrin (insoluble) Staphylococcus aureus coagulation of plasma* “Free” staphylocoagulase Fibrinogen + CRF Fibrin *EDTA Rabbit plasma is preferred for the “free” or tube coagulase test because it contains a large amount of CRF 36 Coagulase
What is the role of Coagulase • The role of coagulase in the pathogenesis of disease is speculative, but coagulase may cause the formation of fibrin layer around a staphylococcal abscess, thus localizing the infection and protecting the organisms from phagocytosis.
Hyaluronidase • Hyaluronidase hydrolyzes hyaluronic acid, the acidic mucopolysaccharides present in the acellular matrix of connective tissue. • This enzyme facilitates the spread of S. aureus in tissues. • More than 90% of S. aureus strains produce this enzyme. 38
Catalase • All staphylococci produce catalase, which catalyzes the conversion of toxic hydrogen peroxide to water and oxygen. • Hydrogen peroxide can accumulate during bacterial metabolism or after phagycytosis. 39
Toxins • S. aureus produce five cytolytic or membranedamaging toxins: are membrane active substances • Consists of 4 hemolysins and a leucocidin. – alpha toxin – beta toxin – gamma toxin – delta toxin - leucocidin ( Panton-Valentin toxin) 40
Alpha haemolysin • Most potent membrane damaging toxin • Susceptible cells have specific receptor for alpha toxin which allows the toxin to bind causing small pores through which monovalent cations pass • Function : osmotic lysis. • Toxic to macrophages, lysosomes, muscle tissues, renal cortex and circulatory system. 41
Beta hemolysin • Sphingomyelinase, cleaves spinogomyelin • Damages lipid rich membranes • Hemolytic for sheep cells Gamma hemolysin • Hemolytic activity Delta hemolysin • Detergent like effect on cell membranes of RBC, leucocytes, macrophages and platelets. 42
Panton-Valentine Leukocidin • Panton-Valentine Leukocidin (PVL) consists of 2 components S and F, together with γ exotoxin lyses WBC resulting in massive release of inflammatory mediators responsible for necrosis and severe inflammation • PVL is an important virulence factor in MRSA infections 43
Staphylococcal toxins • S. aureus produces many virulence factors, including – eight enterotoxins (A-E, G-I) – Toxic Shock Syndrome Toxin 1 (TSST-1) – Exfoliative toxins 44
Enterotoxins • 15 serologically distinct staphylococcal enterotoxins (A-E, G-P) and three subtypes of enterotoxin C have been identified. • The enterotoxin are stable to heating at 100 °C for 30 minutes and are resistant to hydrolysis by gastric and jejunal enzymes. 45
Enterotoxins • Thus, once a food product has been contaminated with enterotoxin-producing staphylococci and the toxin have been produced, neither reheating the food nor the digestive process will be protective. • These toxins are produced by 30% to 50% of all S. aureus strains. • Enterotoxin A is most commonly associated with disease. Enterotoxins C and D are found in contamined milk products, and enterotoxin B causes staphylococcal pseudomembranous enterocolitis. • Preformed, heat-resistant enterotoxin mediates staphylococcal food poisoning (symptoms in 2 -6 hours; usually self-limiting) 46
Toxic Shock Syndrome Toxin - 1 • TSST-1, formerly called pyrogenic exotoxin C and enterotoxin F, is a heat and proteolysis resistant, chromozomally mediated exotoxin. • The ability of TSST-1 to penetrate mucosal barriers, even though the infection remains localized in the vagina or at the site of a wound, is responsible for the systemic effects of TSS. • Death in patients with TSS is due to hypovolemic shock leading to multiorgan failure. 47
Toxin-mediated • Enterotoxins and Toxic shock syndrome toxin (TSST-1) are super-antigens capable of activating large number of T cells • Was associated with use of tampons but is also known to be associated with postoperative wound or soft tissue infections 48
How to prevent TSS in women? • Changing the tampon every four to eight hours • Wearing a low absorbency tampon or sanitary napkin during mensturation • Cleaning hands when changing it. 49
TSST and other Toxins • Staphylococcus aureus strains produce several other extracellular, biologically active substances, including proteases, phosphatases, lipases, lysozyme etc. 50
TSS Symptoms • • Fever Hypotension Myalgia Vomitting Diarrhea Multiple Organ System Failure Erythroderma (rash) 51
Exfoliative toxins • Staphylococcal scalded skin syndrome (SSSS), a spectrum of diseases characterized by exfoliative dermatitis, is mediated by exfoliative toxins. • Outer layer of skin get separated from underlying tissues. 52
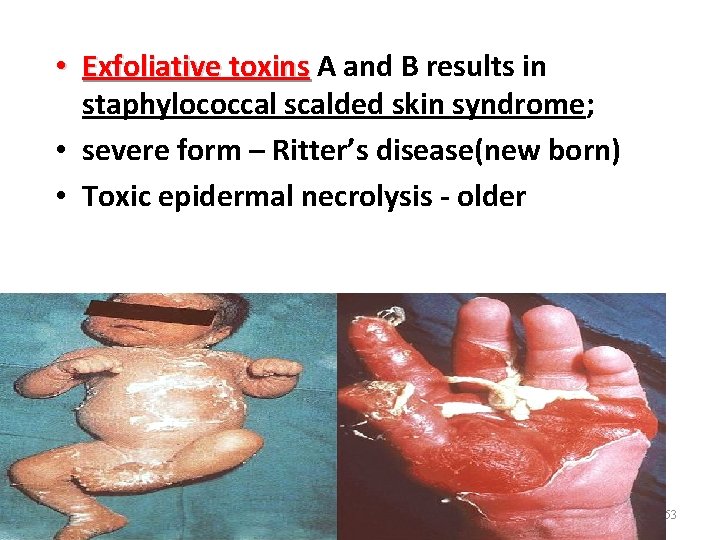
• Exfoliative toxins A and B results in staphylococcal scalded skin syndrome; • severe form – Ritter’s disease(new born) • Toxic epidermal necrolysis - older Dr. T. V. Rao MD 53
The species Staphylococcus aureus pathogenicity • S. aureus is pathogenic for human as well as for all domestic and freeliving warm-blooded animals. • S. aureus causes disease through the production of toxin or through direct invasion and destruction of tissue. 54
Clinical Manifestations • The clinical manifestations of some staphylococcal diseases are almost exclusively the result of toxin activity (e. g. staphylococcal food poisoning and TSS), whereas other diseases result from the proliferation of the staphylococci, leading to abscess formation and tissue destruction (e. g. cutaneous infection, endocarditis, pneumonia, empyema, osteomyelitis, septic arthritis). 55
Clinical diseases • Stahylococccal intoxications: – staphylococcal food poisoning (enterotoxicosis), – exfoliative intoxications (Ritter´s disease or SSSS), – staphylococcal toxic shock syndrome (TSS). 56
Staphylococcal Diseases – Systemic Disease • Toxic shock syndrome-TSS toxin is absorbed into the blood and causes shock • Bacteremia-presence of bacteria in the blood • Endocarditis-occurs when bacteria attack the lining of the heart • Pneumonia-inflammation of the lungs in which the alveoli and bronchioles become filled with fluid • Osteomyelitis-inflammation of the bone marrow and the surrounding bone 57
Range from localized to systemic • Localized cutaneous infections – invade skin through wounds, follicles, or glands – Folliculitis – superficial inflammation of hair follicle; usually resolved with no complications but can progress – Furuncle – boil; inflammation of hair follicle or sebaceous gland progresses into abscess or pustule – Carbuncle – larger and deeper lesion created by aggregation and interconnection of a cluster of furuncles – Impetigo – bubble-like swellings that can break and peel away; most common in newborns 58 Defining Staphylococcal Diseases
Factors predisposing to S. aureus infections • Host factors – Breach in skin – Chemotaxis defects – Opsinization defects – Neutrophil functional defects – Diabetes mellitus – Presence of foreign bodies • Pathogen Factors – Catalase (counteracts host defenses) – Coagulase – Hyaluronidase – Lipases (Imp. in disseminating infection) – B lactamase(ass. With antibiotic resistance) 59
Staphylococcal pyogenic infections Skin and soft tissue – folliculitis – furuncle – Carbuncle – Abscess (breast) – bullous impetigo – Paronychia(nail) – wound infections Musculoskeletal – osteomyelitis, arthritis, bursitis Respiratory - Tonsiltis - Pharyngitis - sinusitis – Lung abscess, empyema(pus at pleural space), rarely pneumonia 60
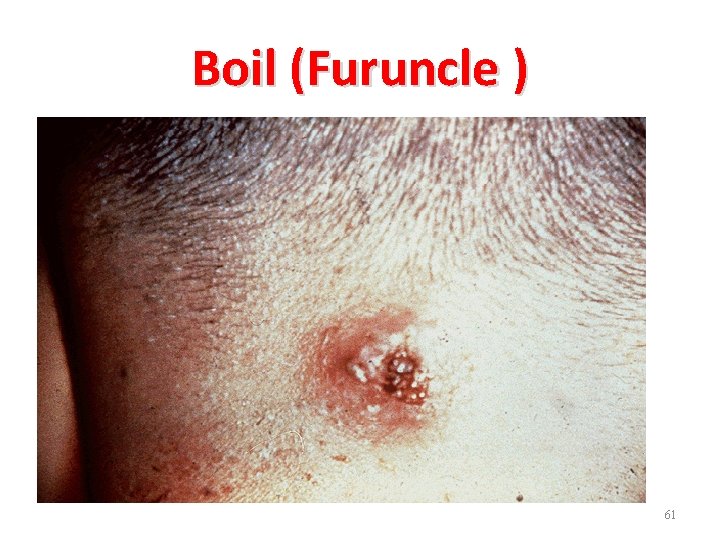
Boil (Furuncle ) 61

Stye 62

Surgical wound infections: many causes including S. aureus 63
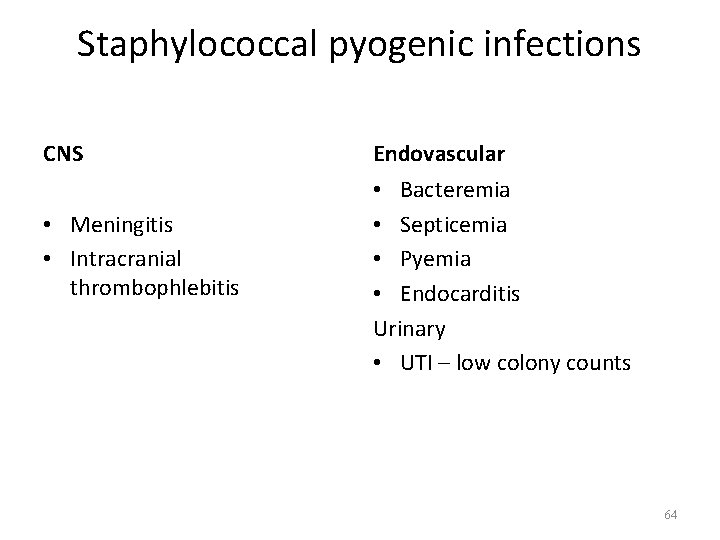
Staphylococcal pyogenic infections CNS • Meningitis • Intracranial thrombophlebitis Endovascular • Bacteremia • Septicemia • Pyemia • Endocarditis Urinary • UTI – low colony counts 64
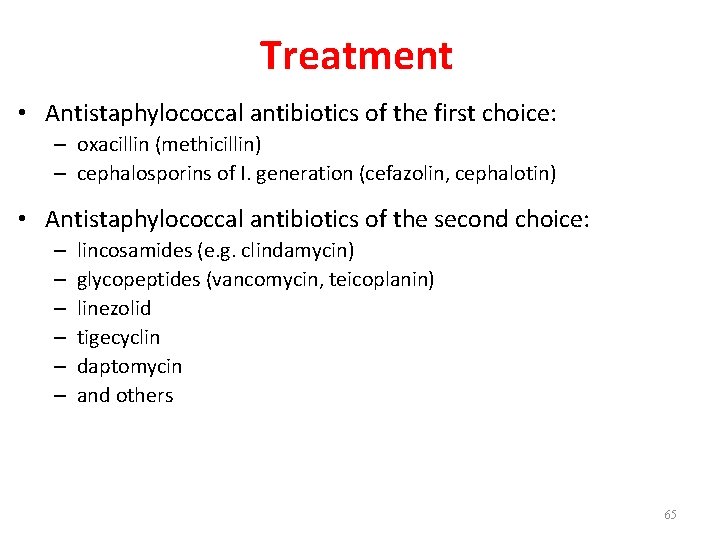
Treatment • Antistaphylococcal antibiotics of the first choice: – oxacillin (methicillin) – cephalosporins of I. generation (cefazolin, cephalotin) • Antistaphylococcal antibiotics of the second choice: – – – lincosamides (e. g. clindamycin) glycopeptides (vancomycin, teicoplanin) linezolid tigecyclin daptomycin and others 65
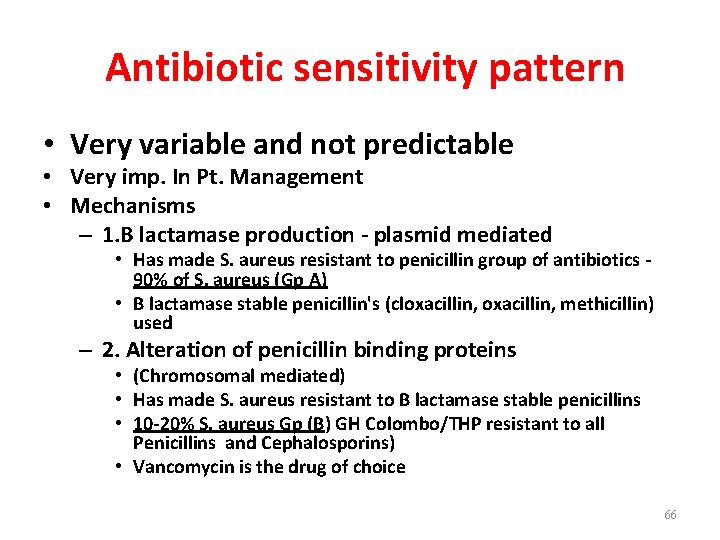
Antibiotic sensitivity pattern • Very variable and not predictable • Very imp. In Pt. Management • Mechanisms – 1. B lactamase production - plasmid mediated • Has made S. aureus resistant to penicillin group of antibiotics 90% of S. aureus (Gp A) • B lactamase stable penicillin's (cloxacillin, methicillin) used – 2. Alteration of penicillin binding proteins • (Chromosomal mediated) • Has made S. aureus resistant to B lactamase stable penicillins • 10 -20% S. aureus Gp (B) GH Colombo/THP resistant to all Penicillins and Cephalosporins) • Vancomycin is the drug of choice 66
MRSA • Methicillin-resistant S. aureus • Resistant to all penicillins, cephalosporins, and penems • Usually multiply-resistant • Vancomycin resistance is very rare – so far • Hospital-acquired • Community-acquired cases now (CA MRSA) 67
Diagnosis • Microscopy – smears of clinical materials are stained according to Gram stain • Cultivation on solid media (agar, usually blood agar) • Biochemical tests • Phage typing – susceptibility of S. aureus strains to various temperature phages 68
Diagnosis • Specimen • Smear • Culture • Coagulase test • Biochemical Reactions • Antibiograms • Typing 69
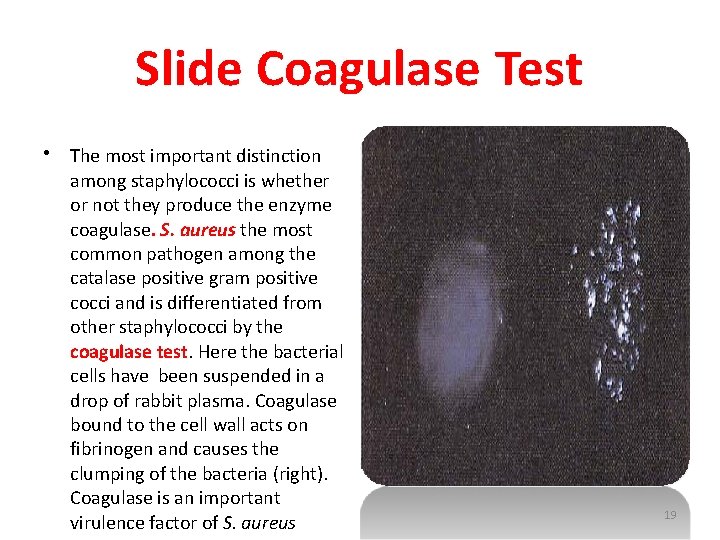
Slide Coagulase Test • The most important distinction among staphylococci is whether or not they produce the enzyme coagulase. S. aureus the most common pathogen among the catalase positive gram positive cocci and is differentiated from other staphylococci by the coagulase test. Here the bacterial cells have been suspended in a drop of rabbit plasma. Coagulase bound to the cell wall acts on fibrinogen and causes the clumping of the bacteria (right). Coagulase is an important virulence factor of S. aureus 19
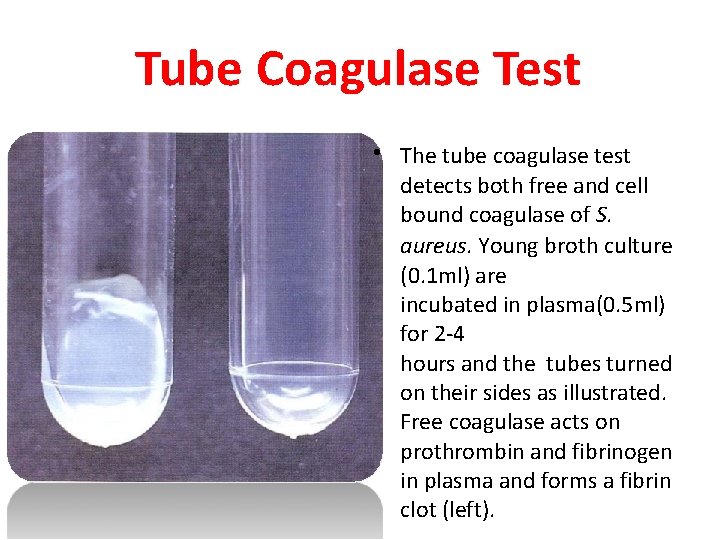
Tube Coagulase Test • The tube coagulase test detects both free and cell bound coagulase of S. aureus. Young broth culture (0. 1 ml) are incubated in plasma(0. 5 ml) for 2 -4 hours and the tubes turned on their sides as illustrated. Free coagulase acts on prothrombin and fibrinogen in plasma and forms a fibrin clot (left).
Serology • Deep seated infections – anti- staphylolysin titres more than 2 units per ml. • Bone abscess 72
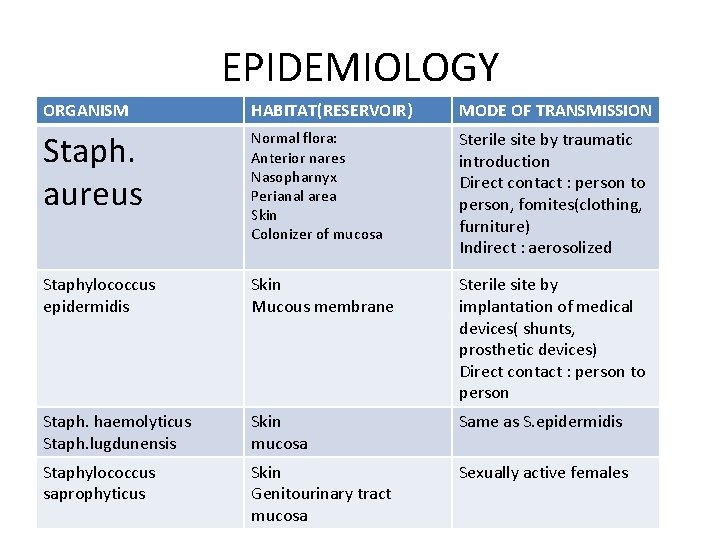
EPIDEMIOLOGY ORGANISM HABITAT(RESERVOIR) MODE OF TRANSMISSION Staph. aureus Normal flora: Anterior nares Nasopharnyx Perianal area Skin Colonizer of mucosa Sterile site by traumatic introduction Direct contact : person to person, fomites(clothing, furniture) Indirect : aerosolized Staphylococcus epidermidis Skin Mucous membrane Sterile site by implantation of medical devices( shunts, prosthetic devices) Direct contact : person to person Staph. haemolyticus Staph. lugdunensis Skin mucosa Same as S. epidermidis Staphylococcus saprophyticus Skin Genitourinary tract mucosa Sexually active females
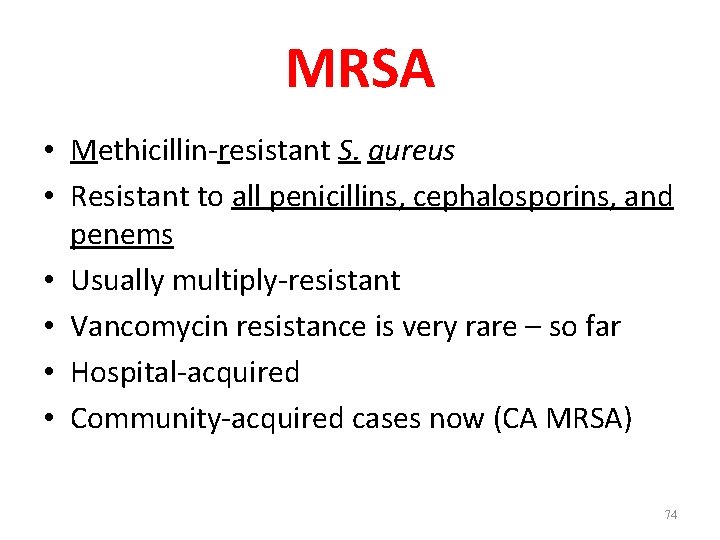
MRSA • Methicillin-resistant S. aureus • Resistant to all penicillins, cephalosporins, and penems • Usually multiply-resistant • Vancomycin resistance is very rare – so far • Hospital-acquired • Community-acquired cases now (CA MRSA) 74
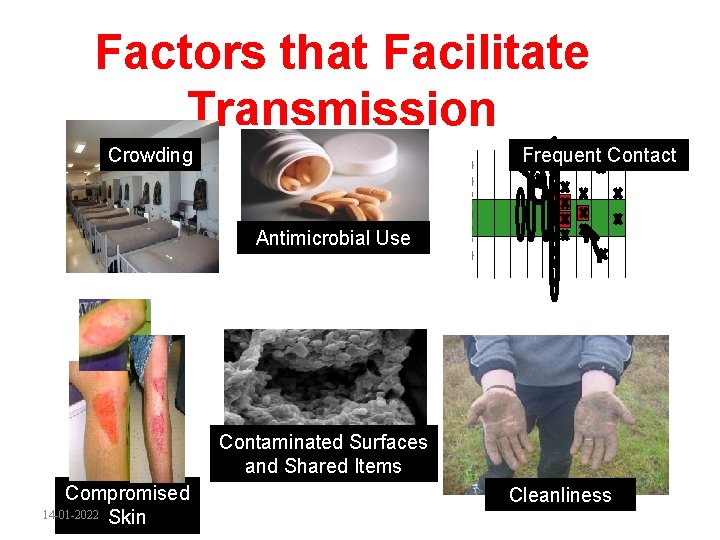
Factors that Facilitate Transmission Crowding Frequent Contact Antimicrobial Use Contaminated Surfaces and Shared Items Compromised 14 -01 -2022 Skin Cleanliness
Definitions of different MRSA • CA-MRSA: Community-acquired MRSA • HA-MRSA: Healthcare-associated MRSA • Nosocomial: infection acquired while in the hospital. 14 -01 -2022
Other coagulase positive staphylococci • • S. intermedius S. hyicus Both of them are animal parasites Does not infect humans 77
CONS • Normal flora of human body • Some species produce infections. S. epidermidis, S. haemolyticus, S. saprophyticus. 78
Coagulase-negative staphylococcal spp (Cons) • S. epidermidis – most frequently isolated staphylococcal spp. • Colonizes moist body areas such as axilla, inguinal and perianal areas, anterior nares and toe webs • Important cause of nosocomial infection esp. S. epidermidis • Usually causes nosocomial infections in patients with predisposing factors such as immunodeficiency/ immunocompromised or presence of foreign bodies 79
. Staphylococcus epidermidis • Skin commensal • Common cause of stitch abscess • Ass. With infection of IV lines, prosthetic heart valves, shunts • Causes urinary tract infection in catheterized patients • Has variable ABS pattern • Treatment should be aided with ABST 80
Importance of S. saprophyticus • S. saprophyticus frequently isolated in rectum and genitourinary tract of young women • Can be causative agent in UTI in young healthy women • 2 nd most common urinary pathogen (other than E. coli) in uncomplicated cystitis in young women • Colony counts of ≥ 105 CFU/ml usu. indicative of significant Bacteriuria 81
. Staphylococcus saprophyticus • Novobiocin resistant • Not sensitive to nalidixic acid • Imp. Cause of UTI in sexually active young women • Usually sensitive to wide range of antibiotics Dr. T. V. Rao MD 82
Related microorganisms- Micrococcus • The genus Micrococcus (the genus contains two species) – Micrococcus luteus – Micrococcus lyla • Found in nature and colonize humans, primarily on the surface of the skin. 83
Micrococcus • • Gram positive, pairs, tetrads, irregular cluster Catalase, modified oxidase positive Differentiate – OF test( Hugh Leifson) Although micrococci may be found in patients with opportunistic infections, their isolation in clinical specimen usually represents clinically insignificant contamination with skin flora. 84
Related microorganisms • The genus Stomatococcus – Stomatococcus mucilaginosus, the only species in this genus, is a commensal microorganism that resides in the oropharynx and upper respiratory tract. • In recent years, this microorganism has been reported to be the cause of an increasing number of opportunistic infections (endocarditis, septicemia, catheter-related infections) in immunocompromised patients. 85
• 95% have penicillinase and are resistant to penicillin and ampicillin • MRSA – methicillin-resistant S. aureus – carry multiple resistance – Some strains have resistance to all major drug groups except vancomycin • Abscesses have to be surgically perforated • Systemic infections require intensive lengthy therapy 86 Clinical Concerns and Treatment
Antimicrobial susceptibility • MRSA can be due to 3 different resistance mechanisms – Production of penicillin-binding protein 2 a (PBP 2 a) encoded by mec. A gene – Production of beta-lactamase – Production of modified intrinsic PBPs • Resistance due to mec. A can be detected via cefoxitin disk diffusion or dilution methods according to CLSI breakpoints (≤ 21 mm – resistant, ≥ 8µg/ml – resistant, respectively) • Resistance due to beta-lactamase production can be detected via the use of beta-lactamase inhibitor such as clavulanic acid which would result in an increase in zone size (disk diffusion method) or decrease of 2 dilutions 87
Prevention • Prevention – Hand antisepsis is the most important measure in preventing nosocomial infections – Also important is the proper cleansing of wounds and surgical openings, aseptic use of catheters or indwelling needles, an appropriate use of antiseptics 88
- Slides: 88