Bacteria host relationship Saprophytic Pathogenic Parasitic Commensals Symbiotic
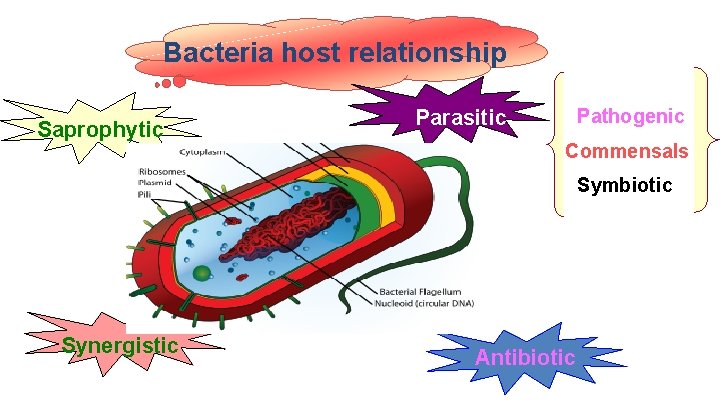
Bacteria host relationship Saprophytic Pathogenic Parasitic Commensals Symbiotic Synergistic Antibiotic
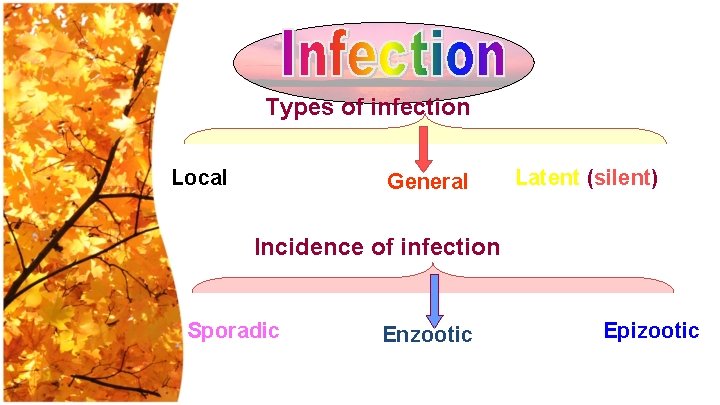
Types of infection Local General Latent (silent) Incidence of infection Sporadic Enzootic Epizootic
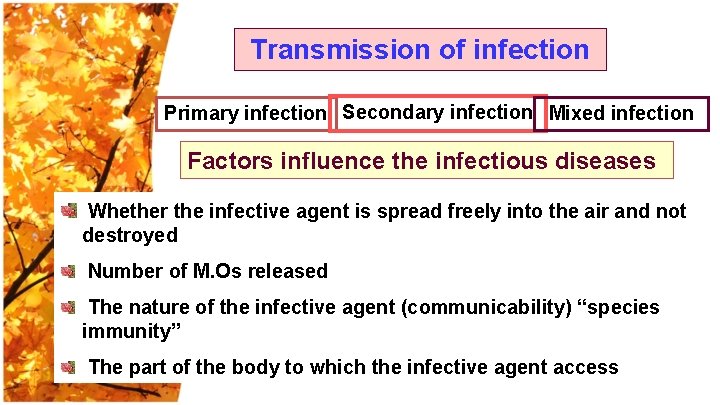
Transmission of infection Primary infection Secondary infection Mixed infection Factors influence the infectious diseases Whether the infective agent is spread freely into the air and not destroyed Number of M. Os released The nature of the infective agent (communicability) “species immunity” The part of the body to which the infective agent access
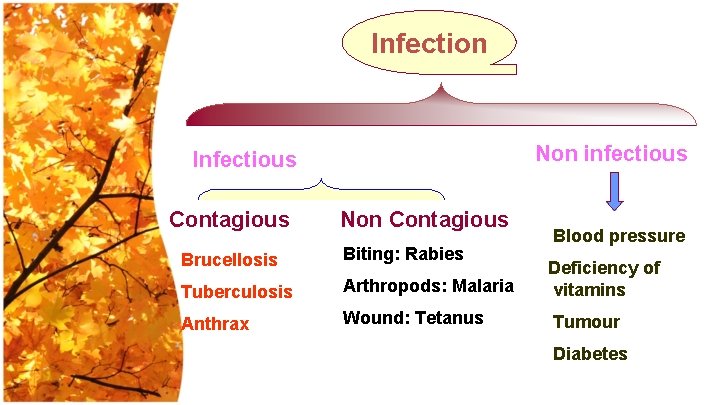
Infection Non infectious Infectious Contagious Non Contagious Blood pressure Brucellosis Biting: Rabies Tuberculosis Arthropods: Malaria Deficiency of vitamins Anthrax Wound: Tetanus Tumour Diabetes
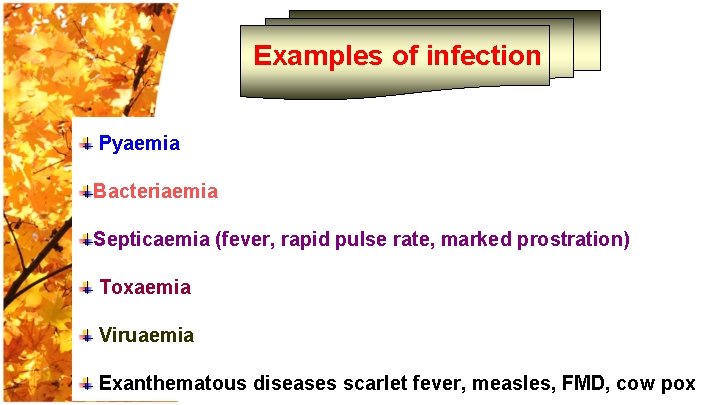
Examples of infection Pyaemia Bacteriaemia Septicaemia (fever, rapid pulse rate, marked prostration) Toxaemia Viruaemia Exanthematous diseases scarlet fever, measles, FMD, cow pox

Infection : - Mean to mix with refer to relationship between the organism and host. Disease: - Mean living a part or separation of ill individuals , change in general health person may be infected without becoming diseased. Normal flora: - M. O. infect the body without causing disease (Symbiosis). Only the Benefit for the m. o. Opportunistic m. o. : - Still commensalisms until suppression of normal defines
• Ability of an organism to cause disease under natural or experimental conditions. It is used to describe a large group of bacteria like genus. • It classifies bacteria into pathogenic and nonpathogenic
• Refers to the degree of pathogenicity within a group or species of microorganisms. • Highly virulent, moderately virulent, and/or avirulent strains may occur within a species or group of organisms.
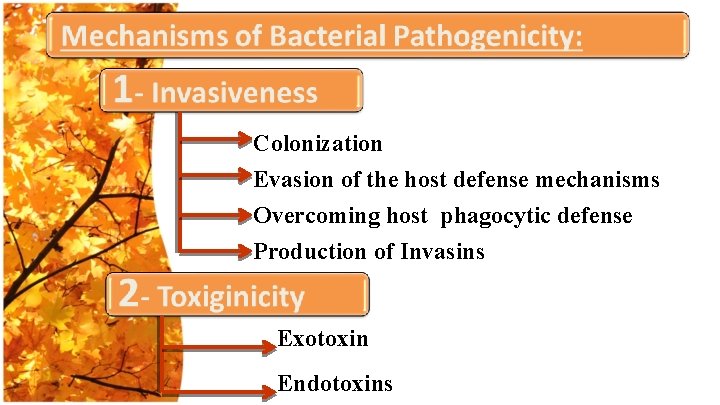
Colonization Evasion of the host defense mechanisms Overcoming host phagocytic defense Production of Invasins Exotoxin Endotoxins
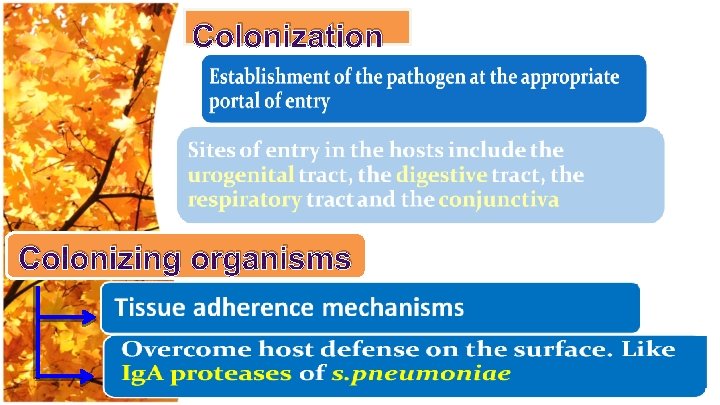
Colonization Colonizing organisms
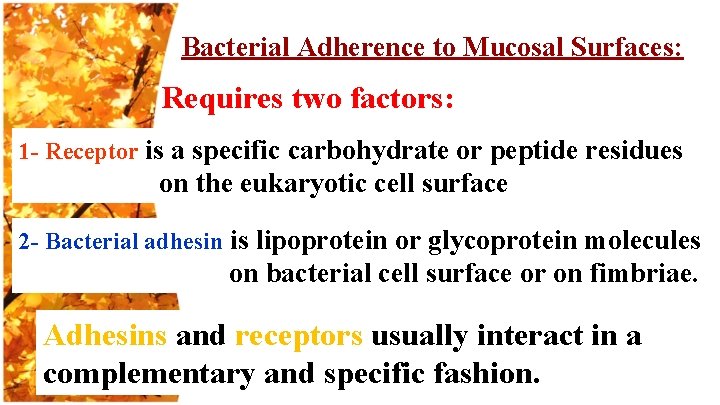
Bacterial Adherence to Mucosal Surfaces: Requires two factors: 1 - Receptor is a specific carbohydrate or peptide residues on the eukaryotic cell surface 2 - Bacterial adhesin is lipoprotein or glycoprotein molecules on bacterial cell surface or on fimbriae. Adhesins and receptors usually interact in a complementary and specific fashion.
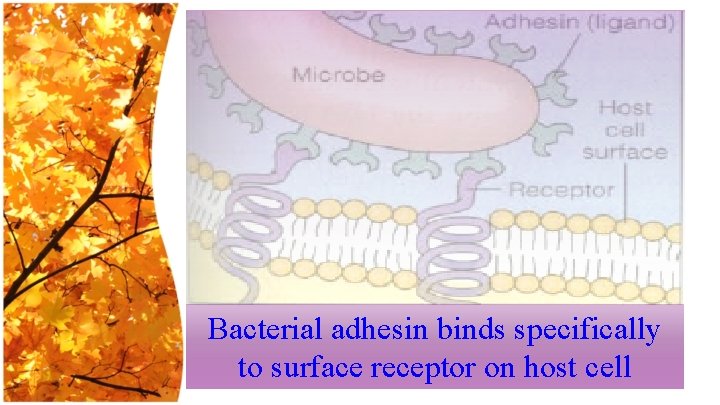
Bacterial adhesin binds specifically to surface receptor on host cell
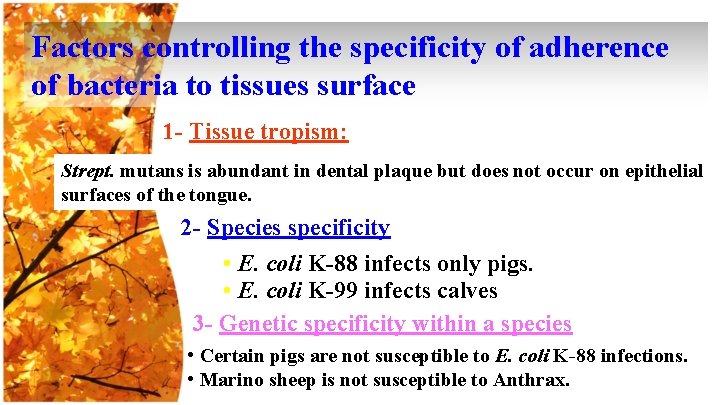
Factors controlling the specificity of adherence of bacteria to tissues surface 1 - Tissue tropism: Strept. mutans is abundant in dental plaque but does not occur on epithelial surfaces of the tongue. 2 - Species specificity • E. coli K-88 infects only pigs. • E. coli K-99 infects calves 3 - Genetic specificity within a species • Certain pigs are not susceptible to E. coli K-88 infections. • Marino sheep is not susceptible to Anthrax.
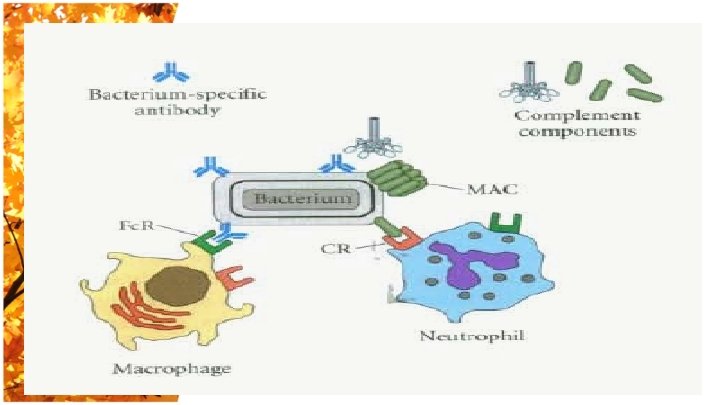
Capsule Protects the organisms against phagocytosis. Cover features of the cell surface from the immune system. Waxy cell wall of pathogenic mycobacterium resists attack or digestion by most tissue bactericides.
(LPS) of Gram negative pathogens protects against complement-mediated lysis or the action of lysozyme. Cell bound Coagulase S. aureus, converts fibrinogen to fibrin on bacterial surface providing what is called antigenic disguise
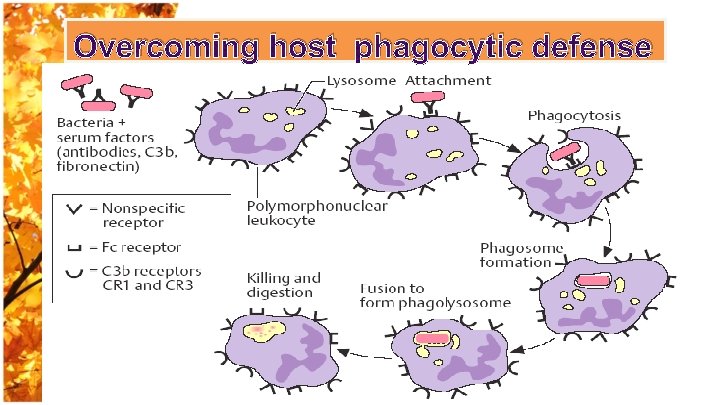
Overcoming host phagocytic defense
Bacteria that readily attract phagocytes, easily ingested and killed, are generally unsuccessful as pathogen. In contrast, successful pathogens interfere to some extent with the activities of phagocytes or in some way avoid their attention. These pathogens may have one of the following: 1 - Avoiding Contact with Phagocytes. 2 - Inhibition of Phagocytic Engulfment. 3 - Survival Inside of Phagocytes
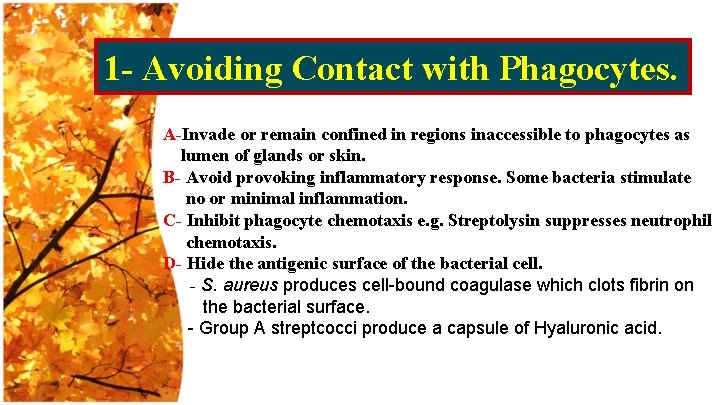
1 - Avoiding Contact with Phagocytes. A-Invade or remain confined in regions inaccessible to phagocytes as lumen of glands or skin. B- Avoid provoking inflammatory response. Some bacteria stimulate no or minimal inflammation. C- Inhibit phagocyte chemotaxis e. g. Streptolysin suppresses neutrophil chemotaxis. D- Hide the antigenic surface of the bacterial cell. - S. aureus produces cell-bound coagulase which clots fibrin on the bacterial surface. - Group A streptcocci produce a capsule of Hyaluronic acid.
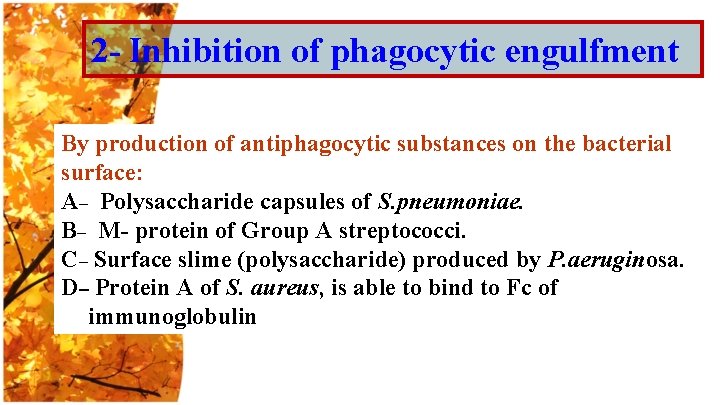
2 - Inhibition of phagocytic engulfment By production of antiphagocytic substances on the bacterial surface: A– Polysaccharide capsules of S. pneumoniae. B– M- protein of Group A streptococci. C– Surface slime (polysaccharide) produced by P. aeruginosa. D– Protein A of S. aureus, is able to bind to Fc of immunoglobulin
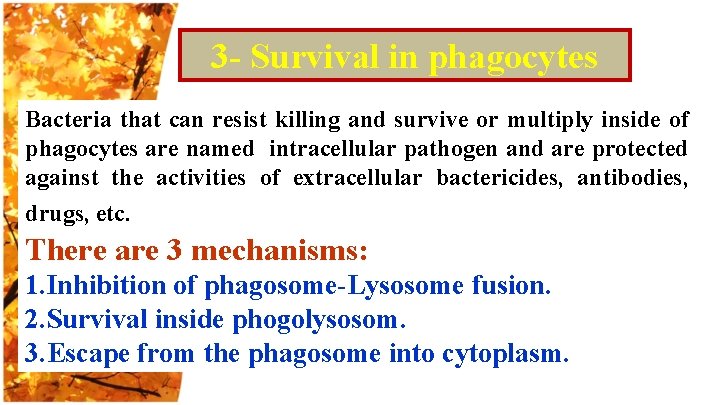
3 - Survival in phagocytes Bacteria that can resist killing and survive or multiply inside of phagocytes are named intracellular pathogen and are protected against the activities of extracellular bactericides, antibodies, drugs, etc. There are 3 mechanisms: 1. Inhibition of phagosome-Lysosome fusion. 2. Survival inside phogolysosom. 3. Escape from the phagosome into cytoplasm.
Inhibition of phagosome-Lysosome fusion The bacteria survive inside of phagosomes because they prevent the discharge of lysosomal contents into the phagosome environment. e. g: M. tuberculosis and Brucella Survival inside the phago-lysosome Phagosome-lysosome fusion occurs but the bacteria are resistant to killing by the lysozymes. e. g. , M. tuberculosis
Escape from the phagosome into cytoplasm Some bacteria produce a phospholipase enzyme that lyses the phagosome membrane after 30 seconds of ingestion. Listeria mononcytogenes
Production of invasins: Invasins are proteins (enzymes) that act locally to damage host cells and/or have the immediate effect of facilitating the growth and spread of the pathogen. Invasins usually act at a short range around bacterial growth differing from Exotoxin.
Bacterial Invasins: (spreading factors) 1 - Hyaluronidase: The enzyme attacks the interstitial cement of connective tissue by depolymerizing hyaluronic acid. 2 - Collagenase: It breaks down collagen, the framework of muscles. 3 -Neuraminidase: It degrades neuraminic acid, an intercellular cement of the epithelial cells of the intestinal mucosa. 4 -Streptokinase and Staphylokinase: convert inactive plasminogen to plasmin which digests fibrin.
Antigenic variation Bacteria can avoid forces of the immune response by periodically changing surface antigens. i. e. Changing one type of fimbriae to another, by switching fimbrial tips and other surface proteins that are targets of antibodies.
There are two types of antigenic variation: • Changing antigens during the same course of infection i. e. Relapsing fever in human. • Changing antigens between infections. e. g. Salmonella serotypes according O and H antigens. St. pyogenes antigenic types according to M. antigen.
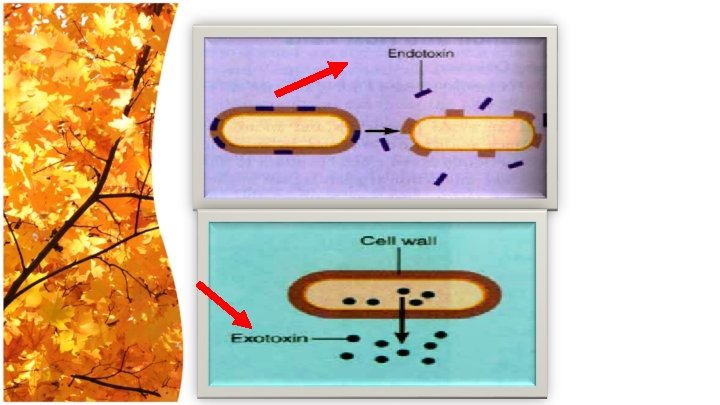
TOXIGENESIS Two types of bacterial toxins: Lipopolysaccharides (Endotoxins) which are associated with the cell walls of Gram-negative bacteria. 2. Proteins (Exotoxins) which may be released into the extracellular environment of pathogenic bacteria.
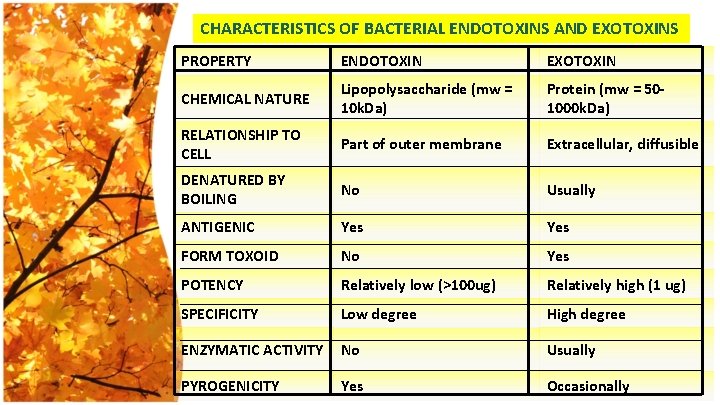
CHARACTERISTICS OF BACTERIAL ENDOTOXINS AND EXOTOXINS PROPERTY ENDOTOXIN EXOTOXIN CHEMICAL NATURE Lipopolysaccharide (mw = 10 k. Da) Protein (mw = 501000 k. Da) RELATIONSHIP TO CELL Part of outer membrane Extracellular, diffusible DENATURED BY BOILING No Usually ANTIGENIC Yes FORM TOXOID No Yes POTENCY Relatively low (>100 ug) Relatively high (1 ug) SPECIFICITY Low degree High degree ENZYMATIC ACTIVITY No Usually PYROGENICITY Yes Occasionally
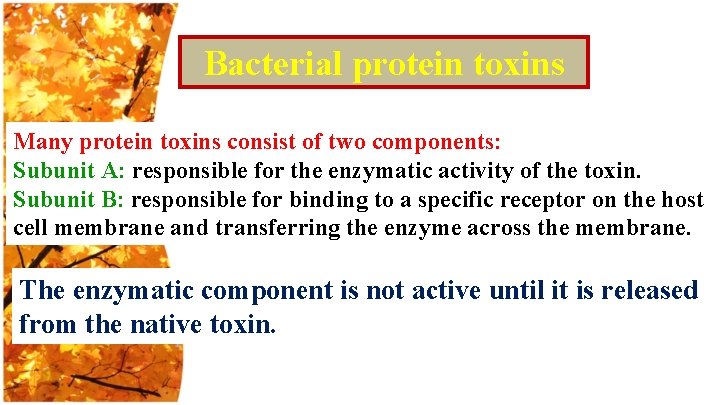
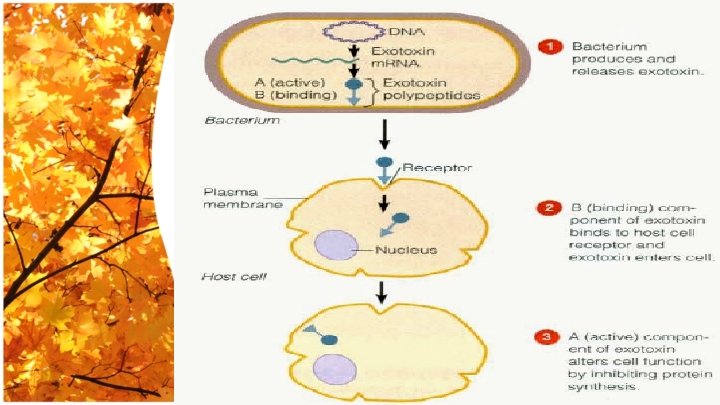
Bacterial protein toxins Many protein toxins consist of two components: Subunit A: responsible for the enzymatic activity of the toxin. Subunit B: responsible for binding to a specific receptor on the host cell membrane and transferring the enzyme across the membrane. The enzymatic component is not active until it is released from the native toxin.
Methods of attenuation of bacteria 1. Prolonged incubation on artificial media. 2. Unfavorable conditions of cultivation i. e. high temperature more than optimum. 3. Presence of antibacterial substance in the medium. 4. Addition of antisera to the medium. 5. Passage into another unsusceptible animal host. 6. Deletion of virulence genes.
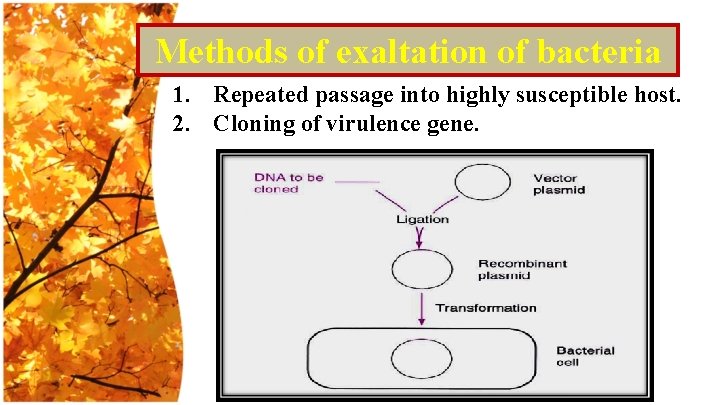
Methods of exaltation of bacteria 1. Repeated passage into highly susceptible host. 2. Cloning of virulence gene.
Measurement of virulence 1. Minimal lethal dose (MLD): The smallest dose that kill all experimental animals in the group. 2. Lethal dose 50 ( LD 50): The dose that kill 50% of experimental animals
- Slides: 36