Back to Basics Acute Renal Failure 1 of
Back to Basics: Acute Renal Failure
• 1% of patients have ARF at time of admission • 2 -5% develop ARF during hospitalization • Important to recognize and manage patients early since mortality rate increases in patients with ARF - 40 -50% in general ward - 80 -90% in patients in the ICU
Acute Renal Failure: Definition • Acute rise in serum creatinine from baseline (increase of at least 0. 5 mg/dl) • Oliguria or anuria may or may not be present – Oliguria - < 400 ml/day – Anuria - < 50 ml/day
Anuria vs. oliguria vs. non-oliguria § Anuria - < 50 ml/day • If abrupt, consider: • Obstruction • vast majority of patients with anuria • Bilateral renal cortical necrosis • Fulminant glomerulonephritis • usually some type of rapidly progressive glomerulonephritis • Acute bilateral renal artery or vein occlusion (rare) § Oliguria - <400 ml/day
• Is it ARF or acute on chronic renal failure? • Is there renal tract obstruction • Is there a reduction in effective ECF? • Has there been a major vascular occlusion? • Is there parenchymal disease other than ATN?
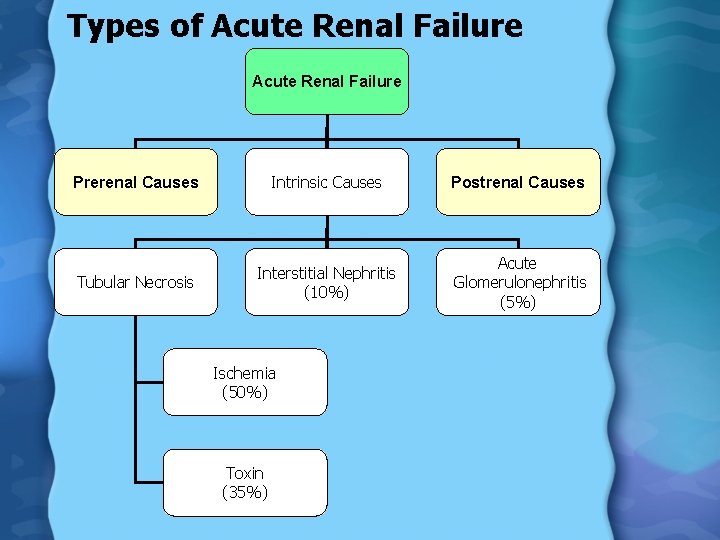
Types of Acute Renal Failure Prerenal Causes Intrinsic Causes Postrenal Causes Tubular Necrosis Interstitial Nephritis (10%) Acute Glomerulonephritis (5%) Ischemia (50%) Toxin (35%)
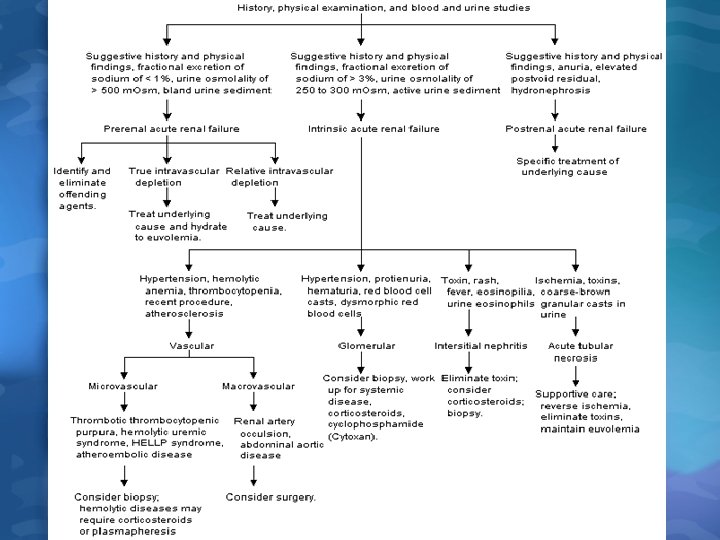
Exclude pre-renal and postobstructive first then look for possible causes of intrinsic renal failure
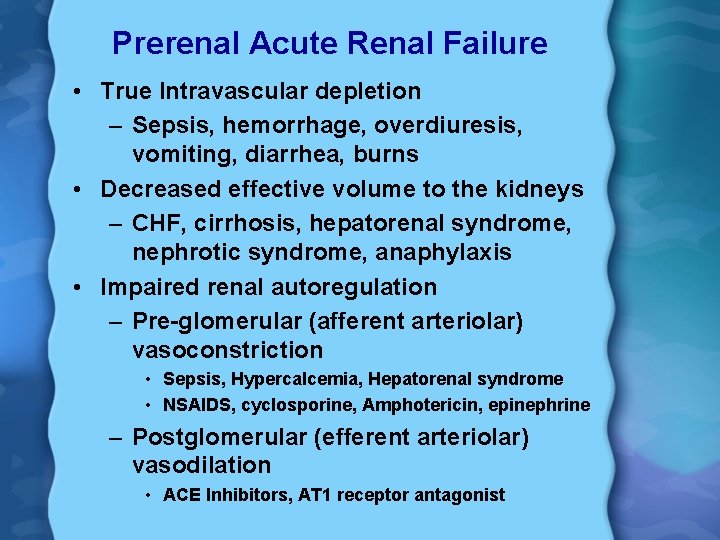
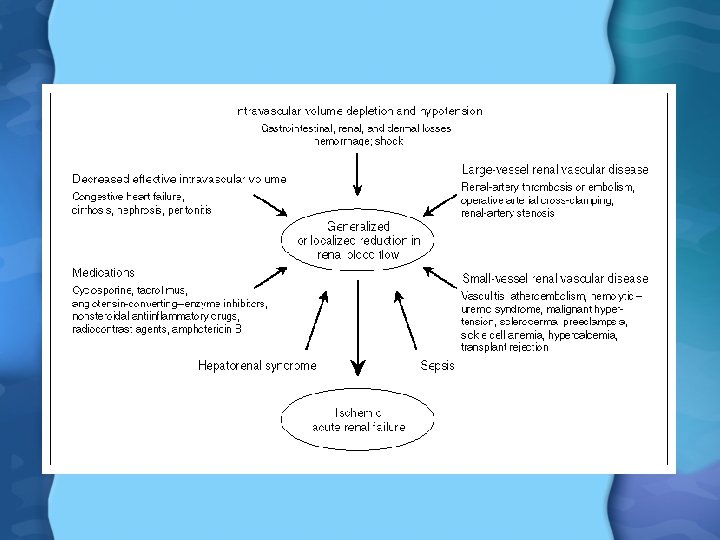
Prerenal Acute Renal Failure • True Intravascular depletion – Sepsis, hemorrhage, overdiuresis, vomiting, diarrhea, burns • Decreased effective volume to the kidneys – CHF, cirrhosis, hepatorenal syndrome, nephrotic syndrome, anaphylaxis • Impaired renal autoregulation – Pre-glomerular (afferent arteriolar) vasoconstriction • Sepsis, Hypercalcemia, Hepatorenal syndrome • NSAIDS, cyclosporine, Amphotericin, epinephrine – Postglomerular (efferent arteriolar) vasodilation • ACE Inhibitors, AT 1 receptor antagonist
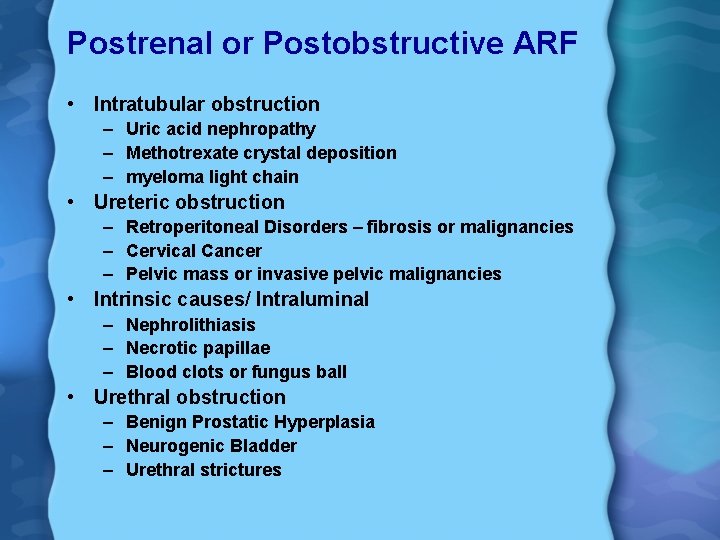
Postrenal or Postobstructive ARF • Intratubular obstruction – Uric acid nephropathy – Methotrexate crystal deposition – myeloma light chain • Ureteric obstruction – Retroperitoneal Disorders – fibrosis or malignancies – Cervical Cancer – Pelvic mass or invasive pelvic malignancies • Intrinsic causes/ Intraluminal – Nephrolithiasis – Necrotic papillae – Blood clots or fungus ball • Urethral obstruction – Benign Prostatic Hyperplasia – Neurogenic Bladder – Urethral strictures
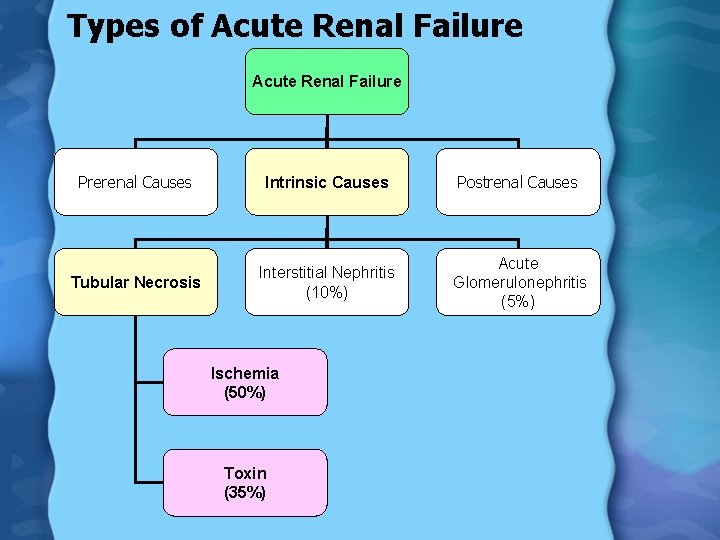
Types of Acute Renal Failure Prerenal Causes Intrinsic Causes Postrenal Causes Tubular Necrosis Interstitial Nephritis (10%) Acute Glomerulonephritis (5%) Ischemia (50%) Toxin (35%)

Drugs Associated with ARF Mechanism Drug Reduction in renal perfusion through alteration of intrarenal hemodynamics NSAIDS, ACE In, cyclosporine, tacrolimus, radiocontrast agents, Amphotericin B, Interleukin-2 Direct tubular injury Aminoglycoside, radiocontrast agents, cisplatin, cyclosporine, tacrolimus, Amphotericin B, methotrexate, foscarnet, pentamidine, organic solvents, heavy metals, IV Ig Heme-pigment induced Cocaine, ethanol, lipid lowering agents tubular toxicity (rhabdomyolysis Intratubular obstruction Acyclovir, sulfonamides, ethylene glycol, chemotherapeutic agents, methotrexate Allergic Interstitial nephritis Penicillin, cephalosporin, sulfonamide, rifampicin, ciprofloxacin, NSAIDS, thiazide diuretics, furosemide, phenytoin, allopurinol Hemolytic- uremic Cyclosporine, tacrolimus, mitomycin, cocaine,

Types of Acute Renal Failure Prerenal Causes Intrinsic Causes Postrenal Causes Tubular Necrosis Interstitial Nephritis (10%) Acute Glomerulonephritis (5%) Ischemia (50%) Toxin (35%)

History • Pulmonary symptoms – Sinus or URI or hemoptysis • Cardiac – CHF, Valvular Disease • GI – Diarrhea, vomiting, poor intake – Flank pain, colicky abdominal pain • Musculoskeletal – Trauma, joint pain, arthritis • GU – BPH, history of stones, recurrent UTI
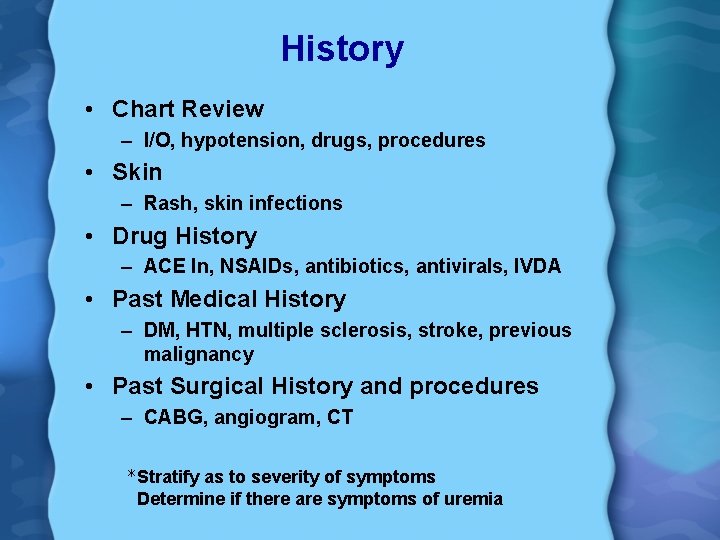
History • Chart Review – I/O, hypotension, drugs, procedures • Skin – Rash, skin infections • Drug History – ACE In, NSAIDs, antibiotics, antivirals, IVDA • Past Medical History – DM, HTN, multiple sclerosis, stroke, previous malignancy • Past Surgical History and procedures – CABG, angiogram, CT *Stratify as to severity of symptoms Determine if there are symptoms of uremia
What P. E. findings would be helpful?
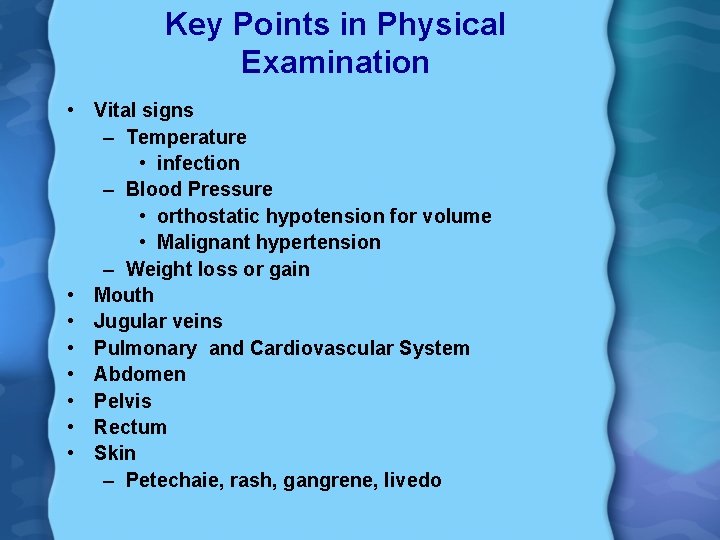
Key Points in Physical Examination • Vital signs – Temperature • infection – Blood Pressure • orthostatic hypotension for volume • Malignant hypertension – Weight loss or gain • Mouth • Jugular veins • Pulmonary and Cardiovascular System • Abdomen • Pelvis • Rectum • Skin – Petechaie, rash, gangrene, livedo
What laboratory tests will you order?
Laboratory Evaluation • • • BUN and creatinine Electrolytes Arterial blood gas CBC and peripheral blood smear Radiologic procedures Urinalysis – Urine electrolytes – Urinary sediment
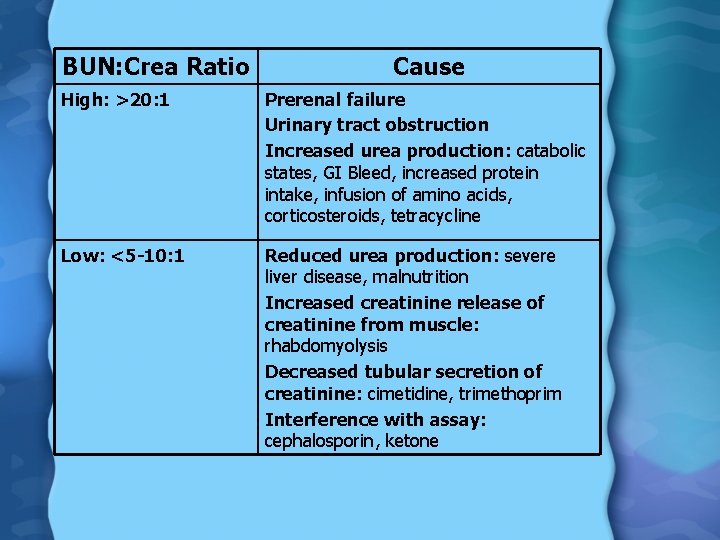
BUN: Crea Ratio Cause High: >20: 1 Prerenal failure Urinary tract obstruction Increased urea production: catabolic states, GI Bleed, increased protein intake, infusion of amino acids, corticosteroids, tetracycline Low: <5 -10: 1 Reduced urea production: severe liver disease, malnutrition Increased creatinine release of creatinine from muscle: rhabdomyolysis Decreased tubular secretion of creatinine: cimetidine, trimethoprim Interference with assay: cephalosporin, ketone
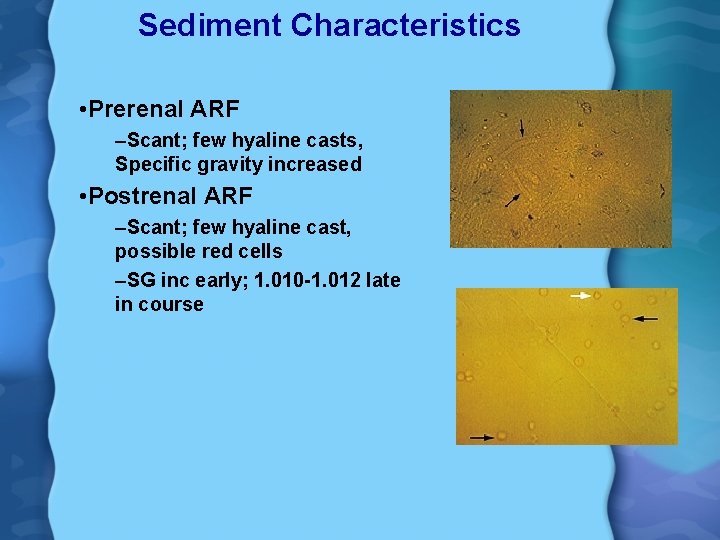
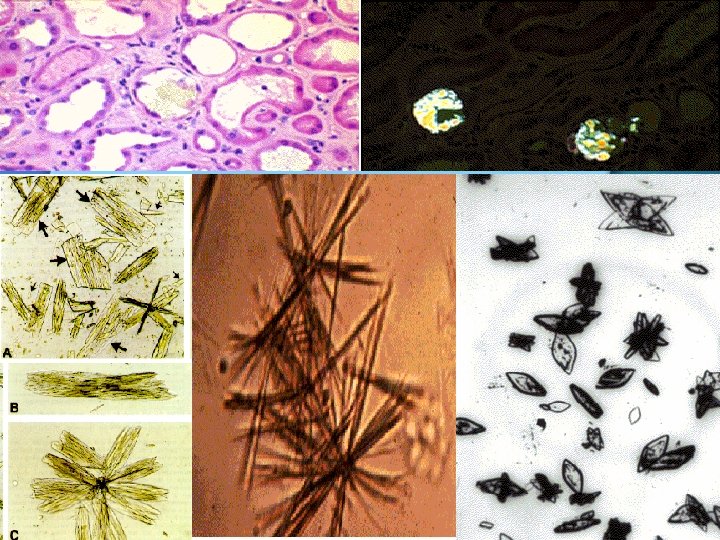
Sediment Characteristics • Prerenal ARF –Scant; few hyaline casts, Specific gravity increased • Postrenal ARF –Scant; few hyaline cast, possible red cells –SG inc early; 1. 010 -1. 012 late in course
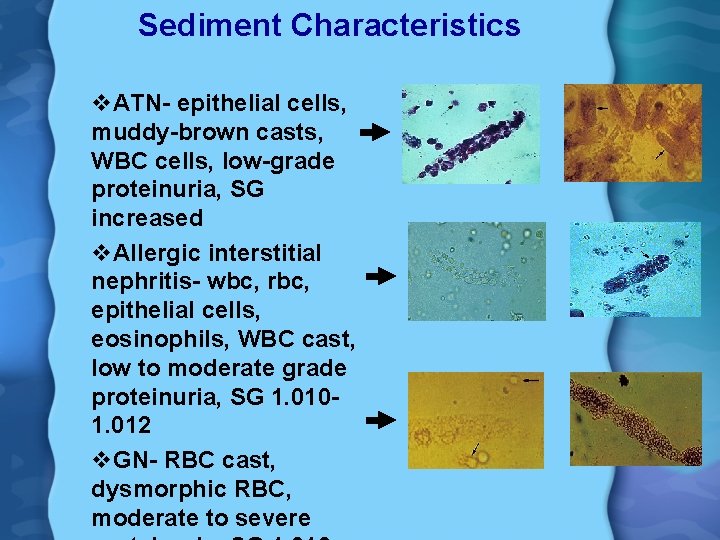
Sediment Characteristics v. ATN- epithelial cells, muddy-brown casts, WBC cells, low-grade proteinuria, SG increased v. Allergic interstitial nephritis- wbc, rbc, epithelial cells, eosinophils, WBC cast, low to moderate grade proteinuria, SG 1. 0101. 012 v. GN- RBC cast, dysmorphic RBC, moderate to severe
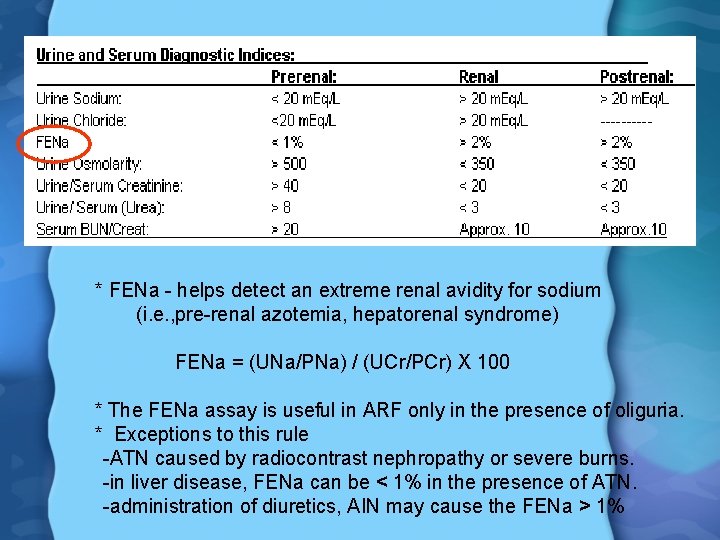
* FENa - helps detect an extreme renal avidity for sodium (i. e. , pre-renal azotemia, hepatorenal syndrome) FENa = (UNa/PNa) / (UCr/PCr) X 100 * The FENa assay is useful in ARF only in the presence of oliguria. * Exceptions to this rule -ATN caused by radiocontrast nephropathy or severe burns. -in liver disease, FENa can be < 1% in the presence of ATN. -administration of diuretics, AIN may cause the FENa > 1%
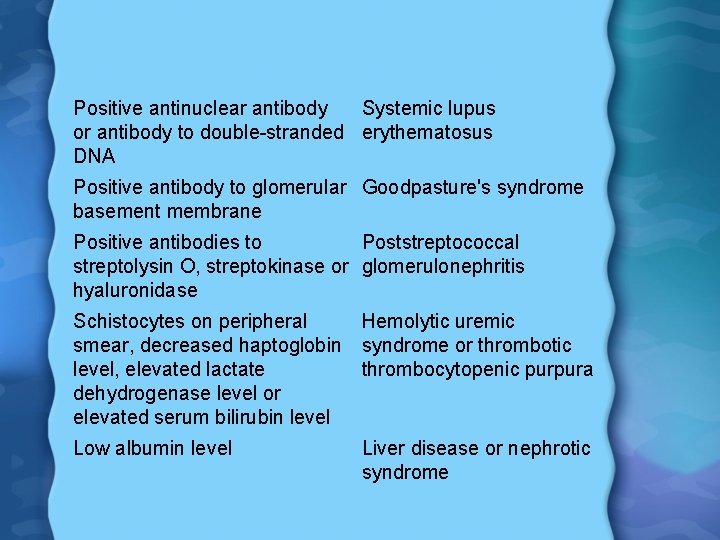
Positive antinuclear antibody Systemic lupus or antibody to double-stranded erythematosus DNA Positive antibody to glomerular Goodpasture's syndrome basement membrane Positive antibodies to Poststreptococcal streptolysin O, streptokinase or glomerulonephritis hyaluronidase Schistocytes on peripheral Hemolytic uremic smear, decreased haptoglobin syndrome or thrombotic level, elevated lactate thrombocytopenic purpura dehydrogenase level or elevated serum bilirubin level Low albumin level Liver disease or nephrotic syndrome
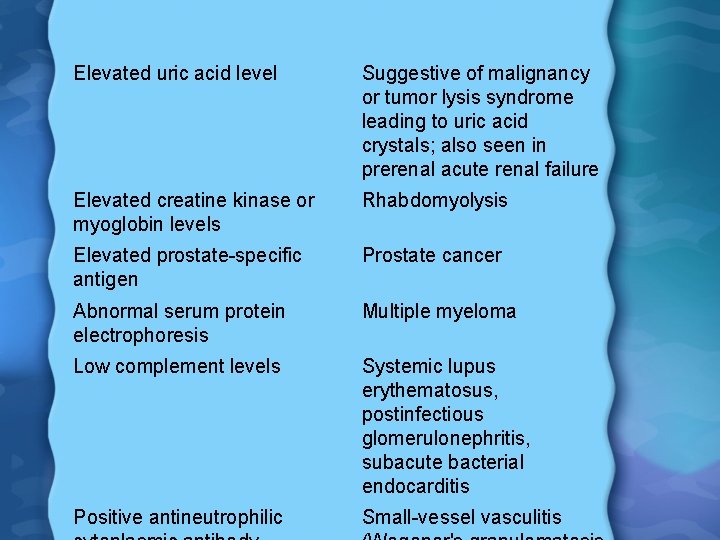
Elevated uric acid level Suggestive of malignancy or tumor lysis syndrome leading to uric acid crystals; also seen in prerenal acute renal failure Elevated creatine kinase or myoglobin levels Rhabdomyolysis Elevated prostate-specific antigen Prostate cancer Abnormal serum protein electrophoresis Multiple myeloma Low complement levels Systemic lupus erythematosus, postinfectious glomerulonephritis, subacute bacterial endocarditis Positive antineutrophilic Small-vessel vasculitis
Renal Ultrasound • Pelvicalyceal dilatation- obstruction • Shrunken kidneys- Chronic kidney disease • Normal size- echogenic: acute GN, ATN – Normal echo pattern: pre-renal, renal artery occlusion • Enlarged kidneys: malignancy, HIV, renal vein thrombosis, amyloid
General Treatment Guidelines • Correct fluid and electrolyte imbalance – Volume depletion – Hyperkalemia – Metabolic acidosis • Nutritional support – 30 -45 kcal/ kg/ day – 0. 6 g/kg protein restriction (1 -1. 5 g/kg if on dialysis) – restrict K (<40 mmol/day) – restrict phosphate <800 mg/day – Fluid restriction if anuria or oliguria present • Look for underlying cause • Avoid nephrotoxic agents and adjust medications • Uremia management – Indications for dialysis
Complications of ARF • Metabolic – Hyponatremia, hyperkalemia, hypocalcemia, hyperphosphatemia, hypermagnesemia, hyperuricemia • Cardiovascular – CHF, arrhythmias, HTN, pericarditis • Neurologic – Asteixis, somnolence, coma, seizures • Hematologic – Anemia, coagulopathies, hemorrhagic diathesis • Gastrointestinal – Nausea, vomiting • Infectious
Indications for Dialysis • Uremia • Refractory hyperkalemia • Refractory fluid overload – Use diuretics- use step-wise approach • Refractory metabolic acidosis – If p. H<7. 2 despite Na. HCO 3 – If patient cannot tolerate bicarbonate infusion due to fluid overload
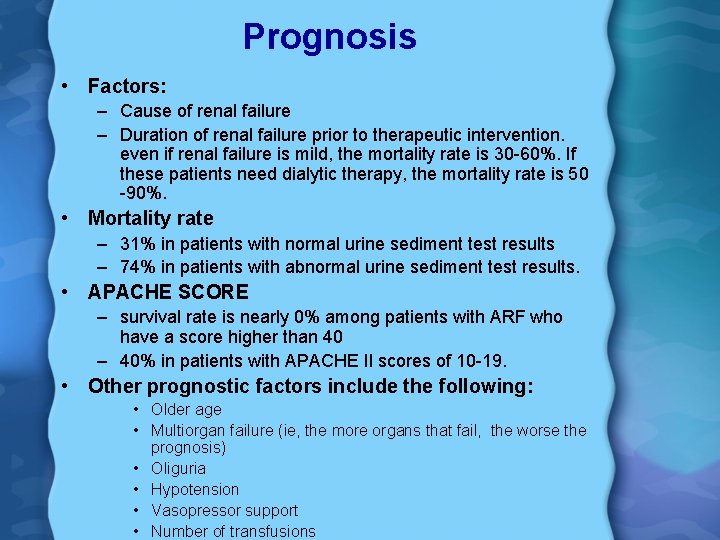
Prognosis • Factors: – Cause of renal failure – Duration of renal failure prior to therapeutic intervention. even if renal failure is mild, the mortality rate is 30 -60%. If these patients need dialytic therapy, the mortality rate is 50 -90%. • Mortality rate – 31% in patients with normal urine sediment test results – 74% in patients with abnormal urine sediment test results. • APACHE SCORE – survival rate is nearly 0% among patients with ARF who have a score higher than 40 – 40% in patients with APACHE II scores of 10 -19. • Other prognostic factors include the following: • Older age • Multiorgan failure (ie, the more organs that fail, the worse the prognosis) • Oliguria • Hypotension • Vasopressor support • Number of transfusions
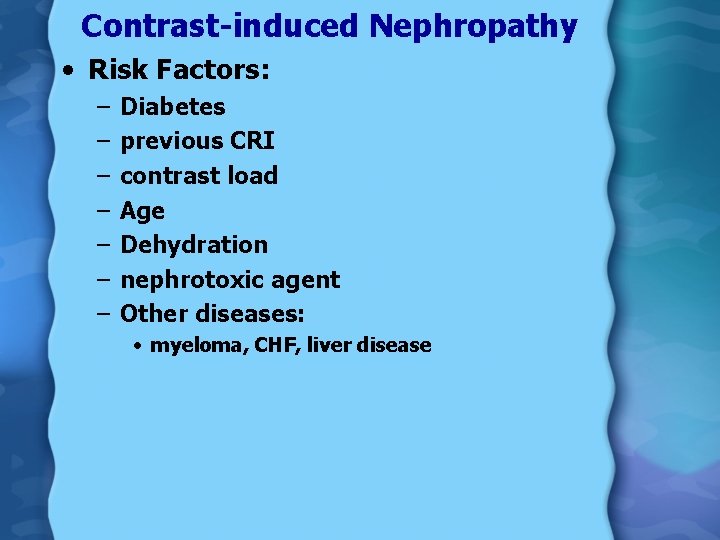
Contrast-induced Nephropathy • Risk Factors: – – – – Diabetes previous CRI contrast load Age Dehydration nephrotoxic agent Other diseases: • myeloma, CHF, liver disease

Contrast-induced Nephropathy • Intervention – Identify risk prior to procedure – Avoid volume depletion – Hydrate to keep urine output >150 ml/hr preproc, during and 12 hours postprocedure – Use non-ionic low osmolality in diabetics and CKD patients – Minimize contrast volume – N-acetylcysteine 600 mg twice a day starting one day before and until 48 hours postprocedure – Space contrast procedures by at least five days • Prognosis – Increased risk of mortality especially in patients needing dialytic therapy (35% vs. 7. 1% vs. 1%)
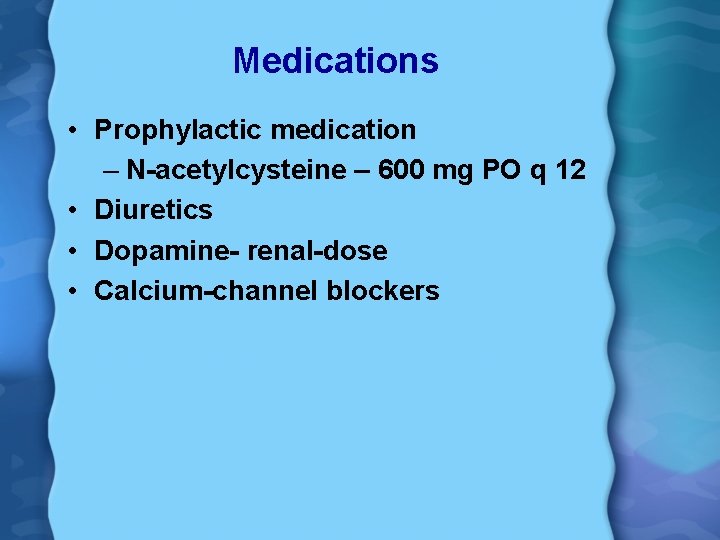
Medications • Prophylactic medication – N-acetylcysteine – 600 mg PO q 12 • Diuretics • Dopamine- renal-dose • Calcium-channel blockers
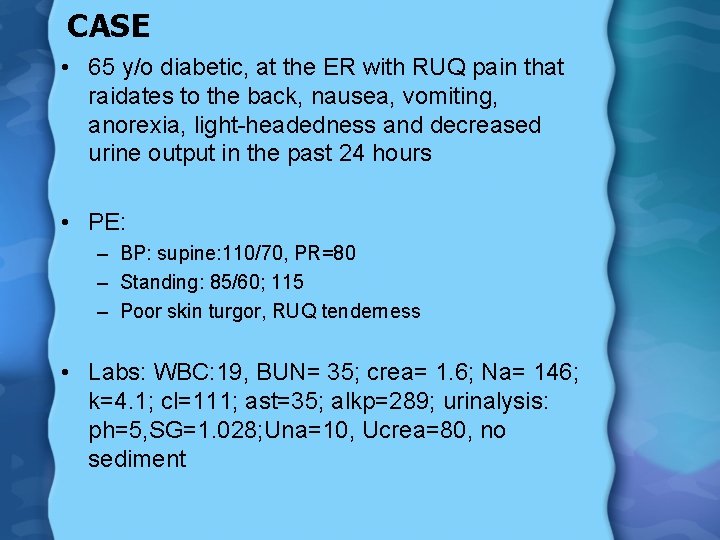
CASE • 65 y/o diabetic, at the ER with RUQ pain that raidates to the back, nausea, vomiting, anorexia, light-headedness and decreased urine output in the past 24 hours • PE: – BP: supine: 110/70, PR=80 – Standing: 85/60; 115 – Poor skin turgor, RUQ tenderness • Labs: WBC: 19, BUN= 35; crea= 1. 6; Na= 146; k=4. 1; cl=111; ast=35; alkp=289; urinalysis: ph=5, SG=1. 028; Una=10, Ucrea=80, no sediment
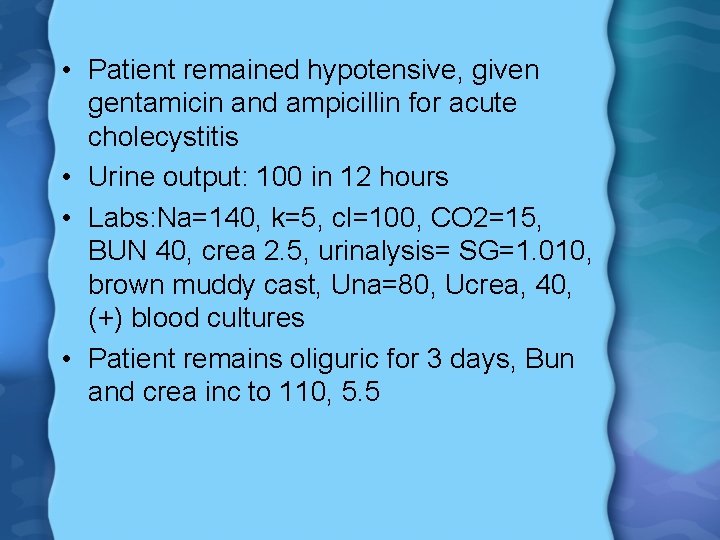
• Patient remained hypotensive, given gentamicin and ampicillin for acute cholecystitis • Urine output: 100 in 12 hours • Labs: Na=140, k=5, cl=100, CO 2=15, BUN 40, crea 2. 5, urinalysis= SG=1. 010, brown muddy cast, Una=80, Ucrea, 40, (+) blood cultures • Patient remains oliguric for 3 days, Bun and crea inc to 110, 5. 5
• What is your diagnosis? • What treatment would you give?
Back to Basics: Acute Renal Failure Yvette Talusan- Tomacruz, M. D. National Kidney and Transplant Institute
Patient Evaluation • Determine if pre-renal, intrinsic or postobstructive – 60 -70 % - pre-renal – 25 -40 % - intrinsic – 5 -10 % - obstruction • KEY: History and Physical examination
Intrinsic Acute Renal Failure • Acute tubular necrosis – Ischemia – Toxins • drugs, contrast agents, pigments • Glomerular disease – RPGN, SLE, small-vessel vasculitis, HSP, Goodpasture’s syndrome , Acute proliferative GNPSGN, PIGN, endocarditis • Vascular disease – Microvascular disease • Atheroembolic disease, TTP, HUS, HELLP – Macrovascular disease • RAS, Aneurysm • Others – – Allergic reaction to drugs Autoimmune Disease Pyelonephritis Infiltrative Disease
- Slides: 42