BACK PAIN A Pain Specialists Perspective INTERVENTIONAL PAIN
BACK PAIN A Pain Specialist's Perspective
INTERVENTIONAL PAIN MANAGEMENT DR J KURIAN MD MRCP FRCA FFPM CONSULTANT ANAESTHESIA AND PAIN MEDICINE
Background • Neurosurgical ablative treatments for pain since 19 th century but now infrequently used • Ablation eclipsed by percutaneous injections or therapies that target central or peripheral pathways
Pain An unpleasant sensory and emotional experience which we primarily associate with tissue damage or describe in terms of such damage, or both
Pain Pathophysiology • Nociceptive pain • Neuropathic pain
Nociception The detection of tissue damage by specialized transducers connected to A-delta and C-fibers

Classification of Pain Nociception • Proportionate to the stimulation of the nociceptor • When acute – Physiologic pain – Serves a protective function – Normal pain • Pathologic when chronic
Classification of Pain: Neuropathic Pain • Sustained by aberrant processes in PNS or CNS • Disproportionate to the stimulation of nociceptor • Serves no protective function • Pathologic pain
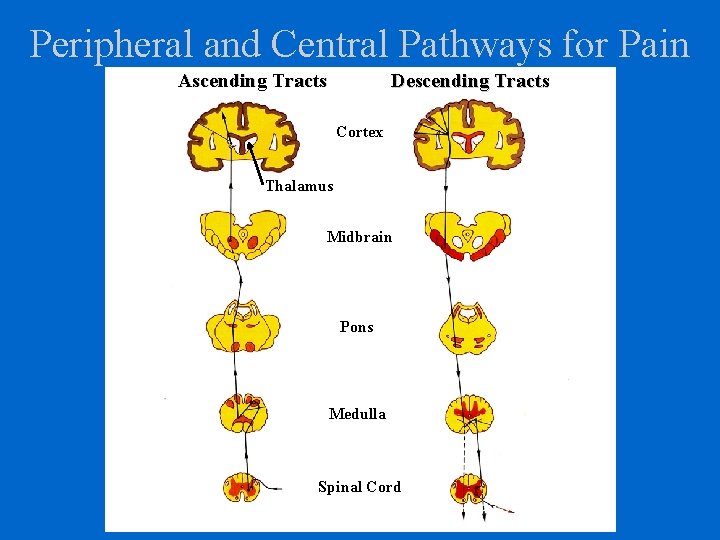
Peripheral and Central Pathways for Pain Ascending Tracts Descending Tracts Cortex Thalamus Midbrain Pons Medulla Spinal Cord
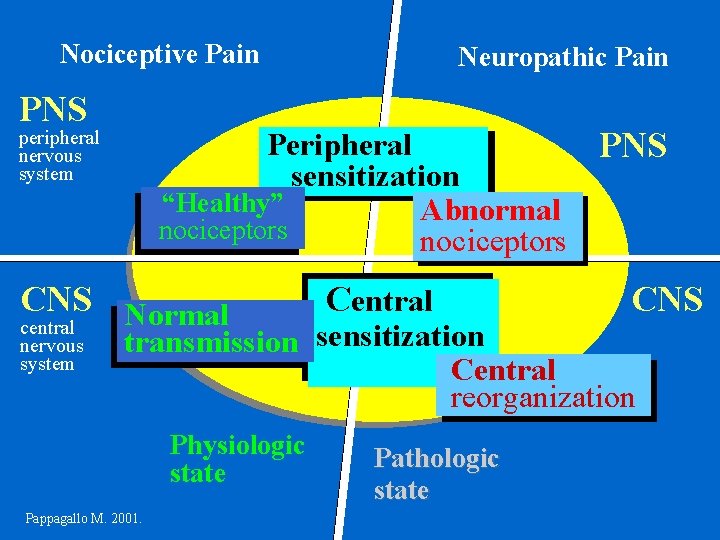
Nociceptive Pain PNS Peripheral PNS sensitization “Healthy” Abnormal nociceptors peripheral nervous system CNS Normal central nervous system Neuropathic Pain Central CNS transmission sensitization Central reorganization Physiologic state Pappagallo M. 2001. Pathologic state
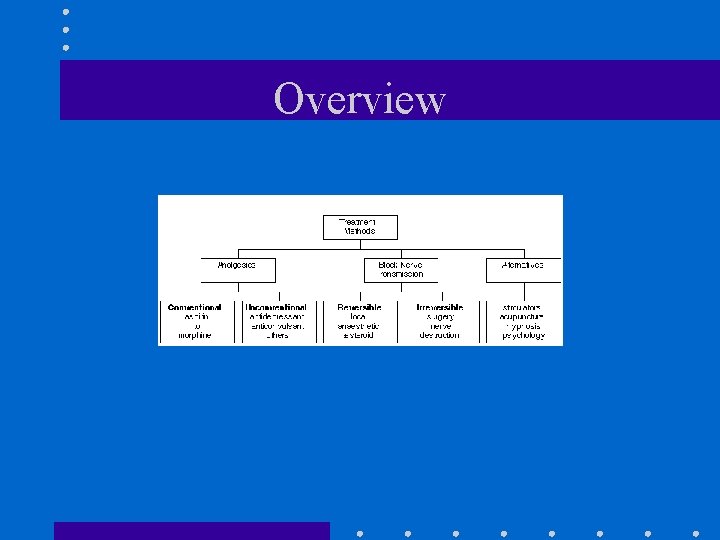
Overview
Chronic Pain Syndrome • End result of a variety of pathological and psychological mechanisms that may have included, at some stage tissue or nerve damage.
Pain Interventions • Nerve blocks and injections should be seen as part of a process of education and rehabilitation, allowing an opportunity for mobilization and return to normal activity.
Nerve Blocks (1) • Diagnostic: local anaesthetic only, to clarify mechanism or simulate effects of therapy • Therapeutic: anaesthetise a site or pathway temporarily(local anaesthetic) or “permanently”(lytic agent, cryo, radiofrequency) or reduce inflammation (corticosteroids) • A block may be diagnostic and therapeutic eg. Symapthetic block or trigger point injection
Nerve Blocks (1) • Diagnostic: local anaesthetic only, to clarify mechanism or simulate effects of therapy • Therapeutic: anaesthetise a site or pathway temporarily(local anaesthetic) or “permanently”(lytic agent, cryo, radiofrequency) or reduce inflammation (corticosteroids) • A block may be diagnostic and therapeutic eg. Symapthetic block or trigger point injection
Nerve Blocks (II) Common blocks for chronic pain include -Trigger-point injection -Bier block -Peripheral nerve injection (eg. Ilioinguinal, lateral femoral cutaenous, greater occipital) -Epidural injection -Intra-articular(eg. facet, SI joint) Sympathetic block(cervical, lumbar) Plexus block (coeliac, hypogastric)
Nerve Blocks (III) • Case reports, preclinical data support long lasting effects of local anaesthetic blockade - RCTs support lytic coeliac block • However, unclear how much clinical improvement reflects placebo effects, irrevelant cues, systematic absorption of local anaesthetic, expectations • Side effects possible • Rarely successful as a stand alone strategy for chronic pain
Trigger Point Injection • Myofascial pain syndrome • • Taut band palpable (if muscle is accessible) Exquisite spot tenderness of a nodule in a taut band Pressure on tender nodule reproduces pain Range of motion with stretch limited by pain • Techniques • • Dry needling Local anaesthetic only Local anaesthetic and steroid Botulinum toxin
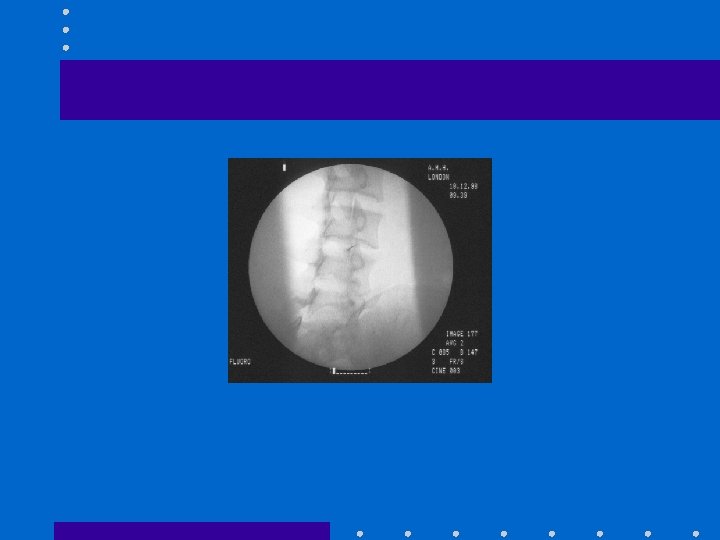
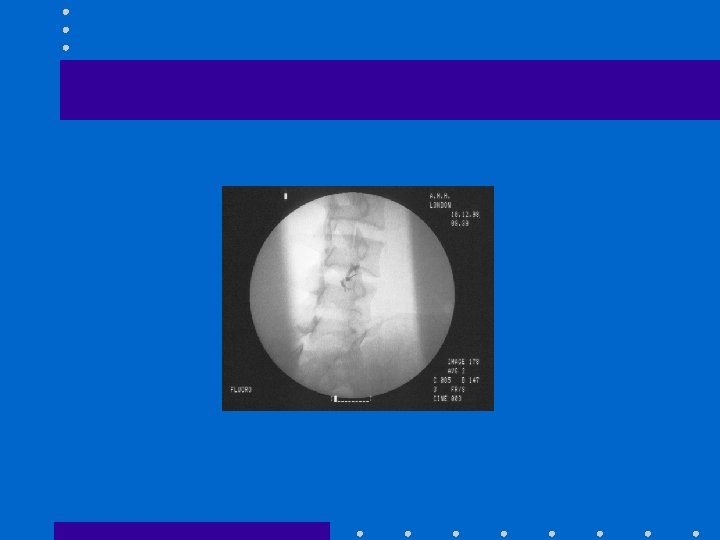
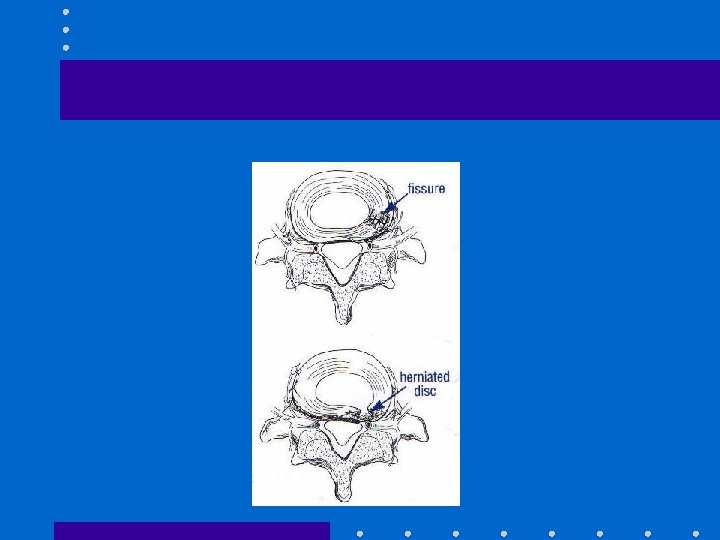
Epidural Injection (I) • Employed for decades using various techniques materials and patients • Limited RCT evidence of efficacy • Cervical, Thoracic, Lumbar , Caudal • Trans laminar • Transforaminal
Epidural Injection(II) • Applied for symptomatic relief in • • Disc protrusion with radiculopathy Spinal stenosis(circumferential or transforaminal) Acute pain, local inflammation of vertebral fracture Acute herpes Zoster • May facilitate rehabilitation, avert surgery when applied within multidisciplinary frame work
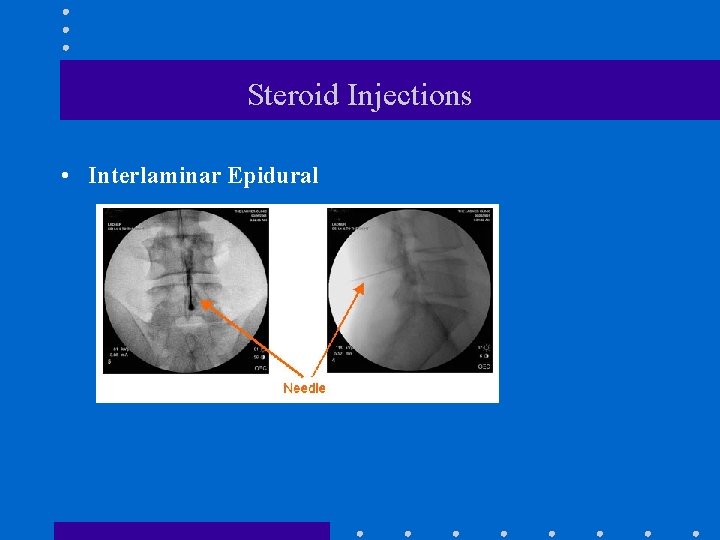
Steroid Injections • Interlaminar Epidural
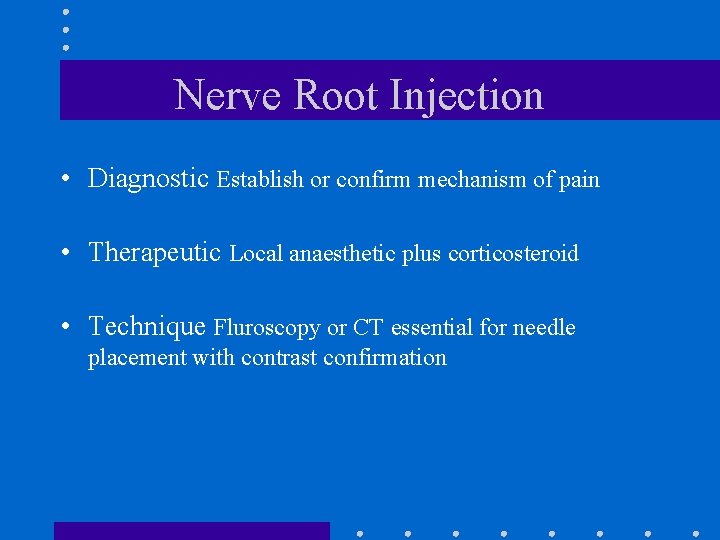
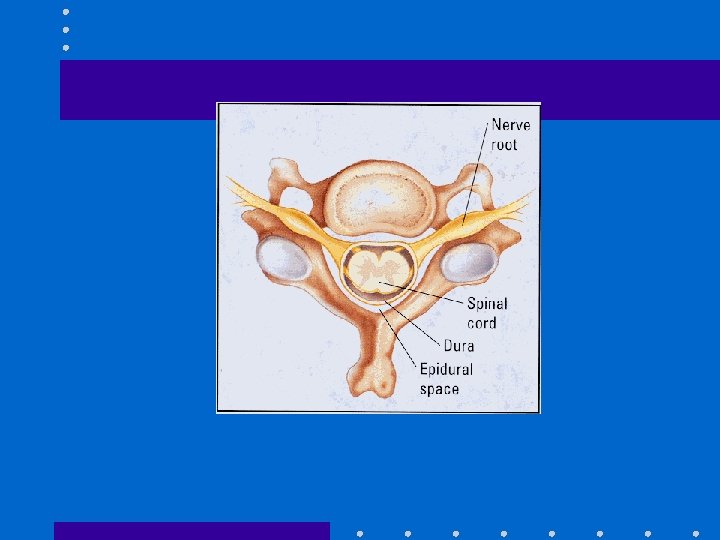
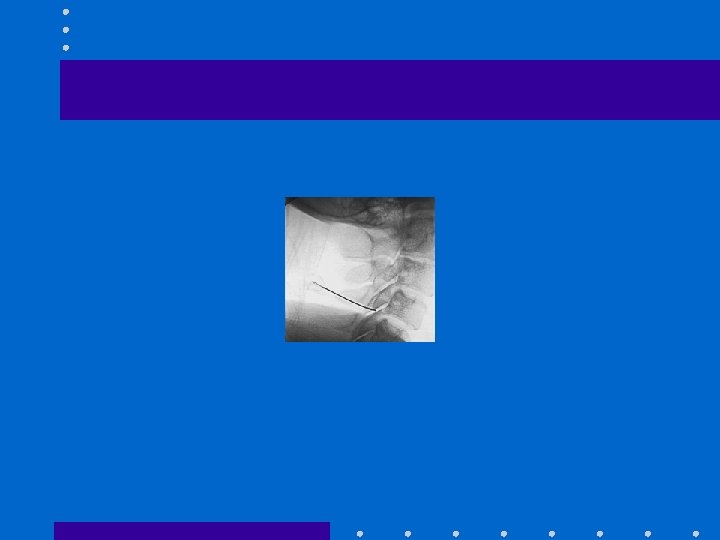
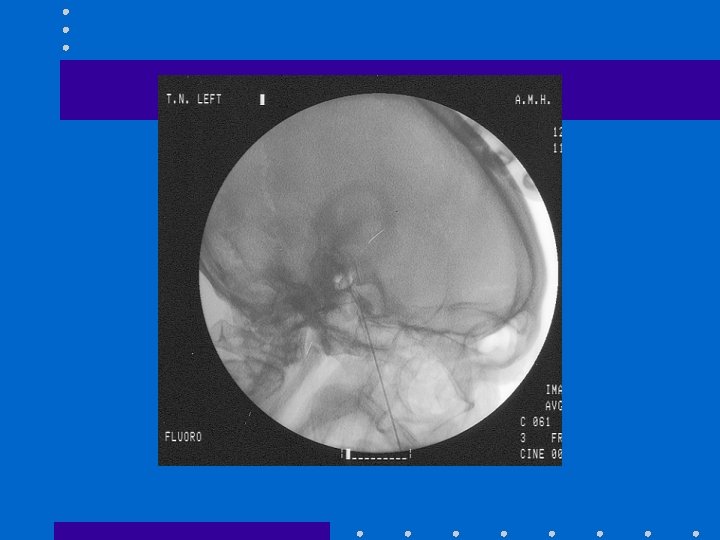
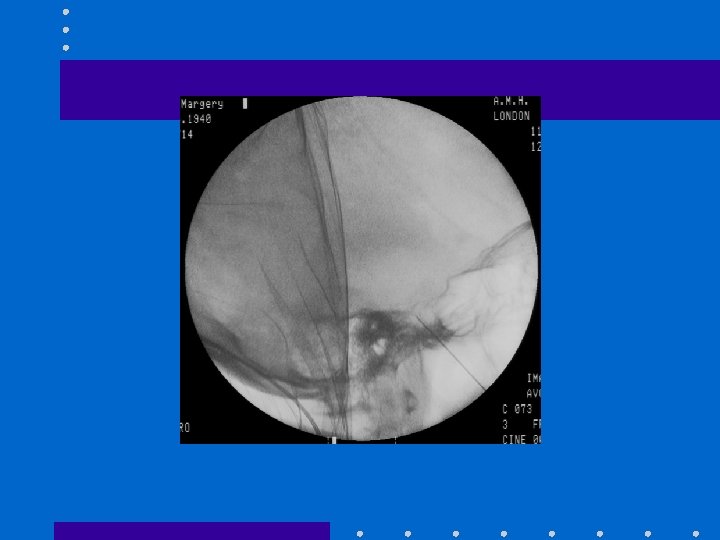
Nerve Root Injection • Diagnostic Establish or confirm mechanism of pain • Therapeutic Local anaesthetic plus corticosteroid • Technique Fluroscopy or CT essential for needle placement with contrast confirmation
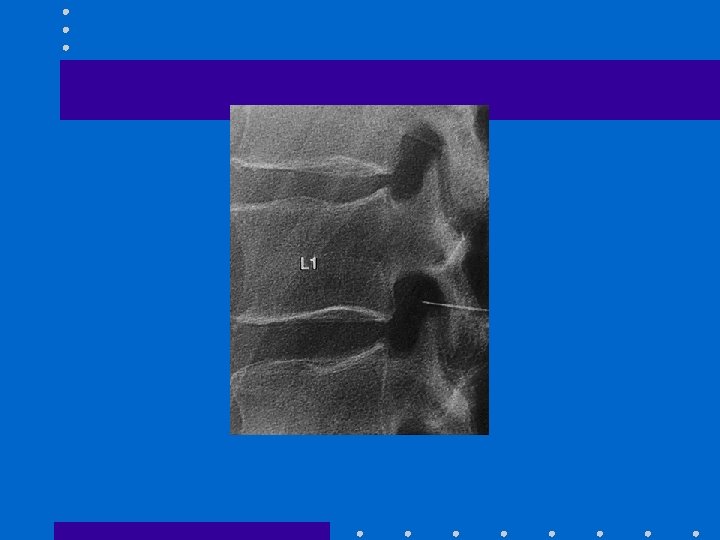
INTRA ARTICULAR INJECTIONS • Facet and Sacroiliac joints most common • Diagnostic facet syndrome or SI joint pain Simulate results of potential spinal fusion or denervation of medial branch of dorsal ramus • Therapeutic (local anaesthetic + corticosteroid) Reduce inflammation, pain Increase mobility, facilitate rehabilitation
Specific anatomic syndromes • Facet syndrome Continuous pain worsened by rotation and extension Radiation into the leg or gluteal area, in a non-dermatomal distribution Tenderness over the joints and paravertebral muscle spasm
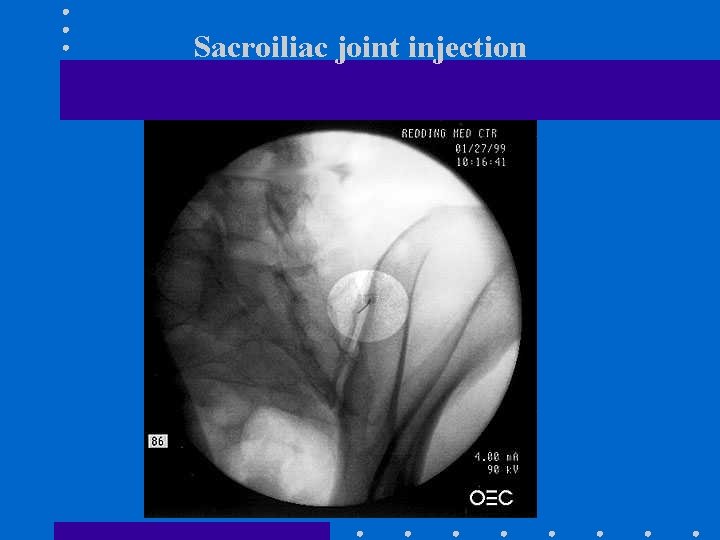
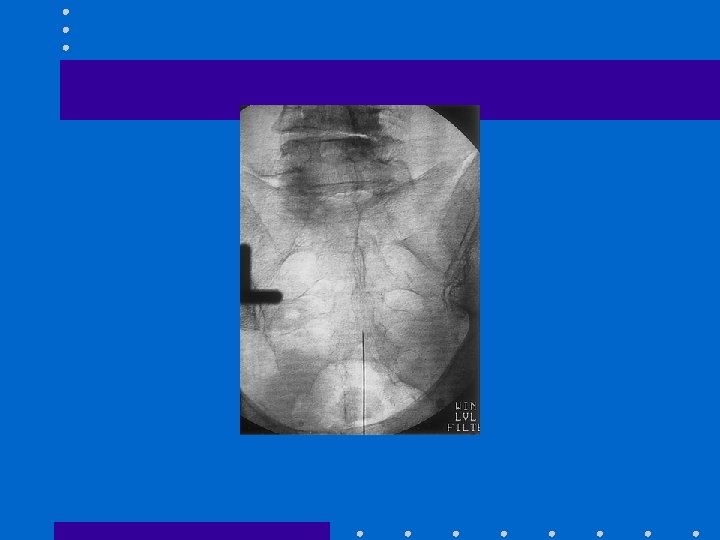
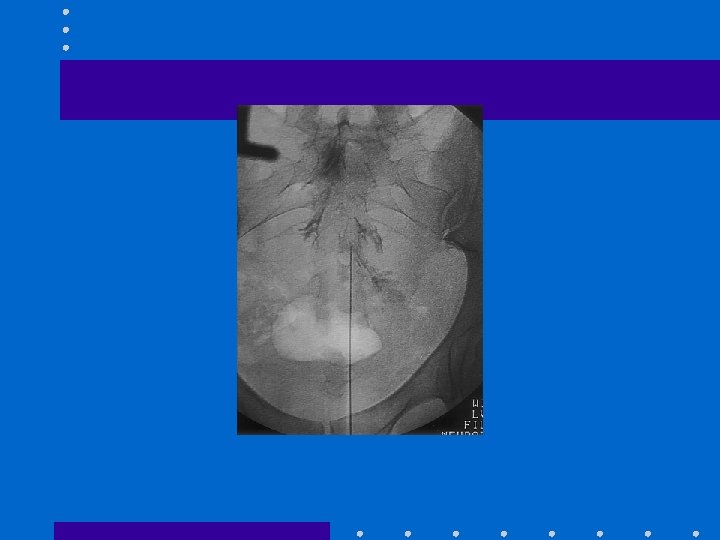
Sacroiliac joint injection
Symapthetic Blocks • Diagnostic • Stellate ganglion • Lumbar • Therapeutic • CRPS of upper and lower extremity • Vascular insufficiency • Refractory angina • Technique • Local anaesthetic, Neurolytic
MISCELLANEOUS • Trigeminal ganglion • Glossopharyngeal nerve • Sphenopalatine ganglion
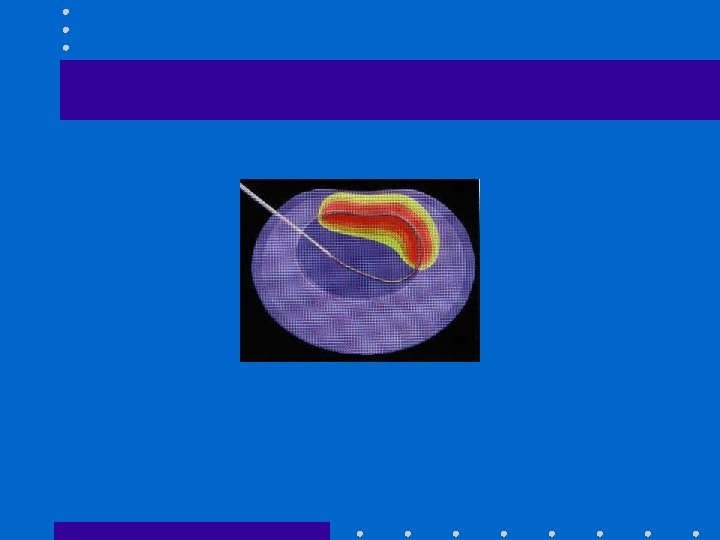
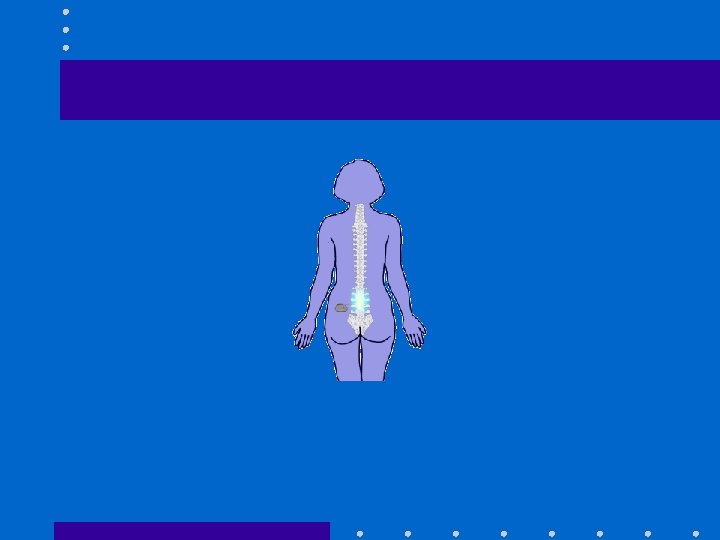
NEWER DEVELOPMENTS • • PULSED RADIOFREQUENCY VERTEBROPLASTY IDET, DISCTRODE DORSAL COLUMN STIMULATORS PERIPHERAL NERVE STIMULATORS DEEP BRAIN STIMULATORS IMPLANTABLE PUMPS
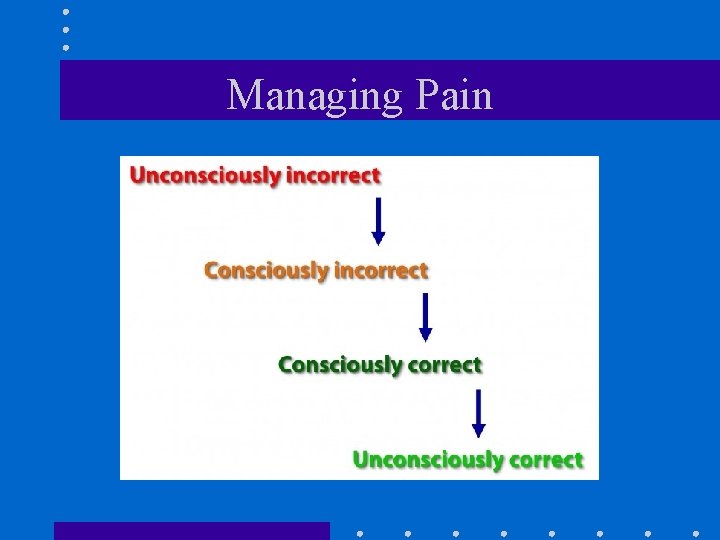
Managing Pain
CONCLUSION • Interventional approaches are often reserved for patients with well established problems, failure of other treatments and pronounced disability. • Do we miss an opportunity for early cost effective preventive treatment by reserving interventions for those least likely to benefit? • “Doctors think a lot of patients are cured who have simply quit in disgust” • DON HEROLD 1889
- Slides: 46