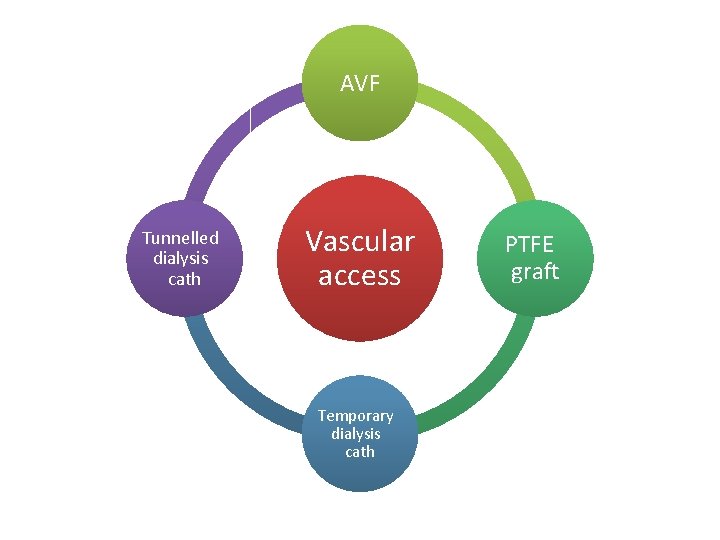
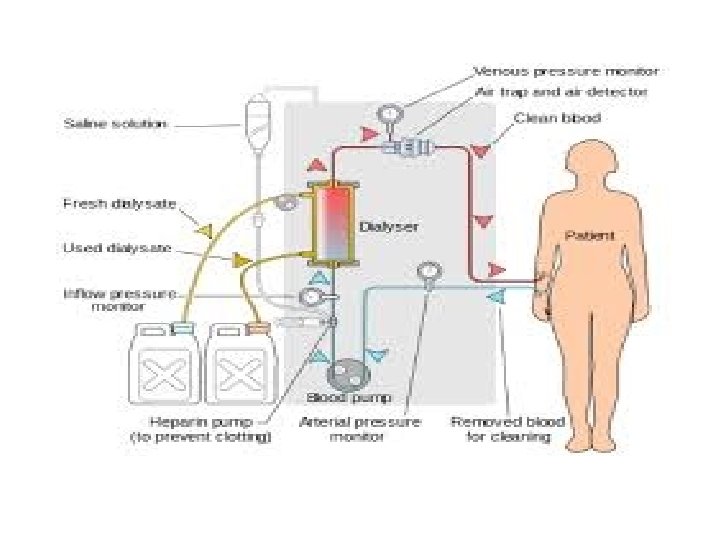
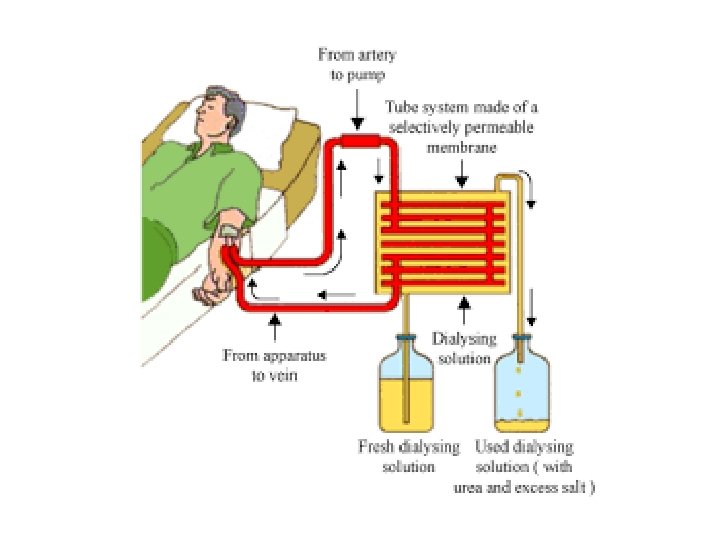
AVF Tunnelled dialysis cath Vascular access Temporary dialysis


































- Slides: 107





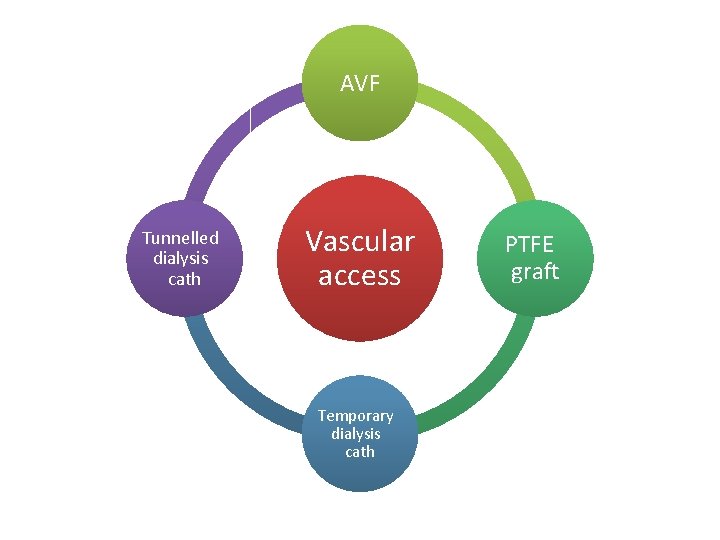
AVF Tunnelled dialysis cath Vascular access Temporary dialysis cath PTFE graft
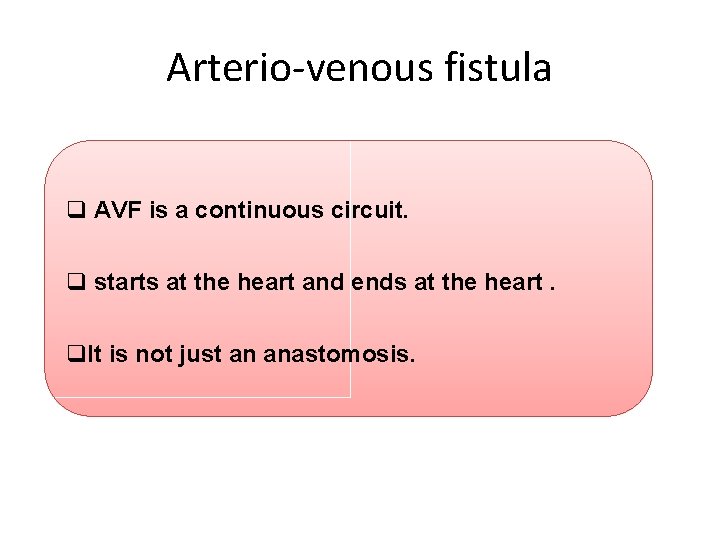
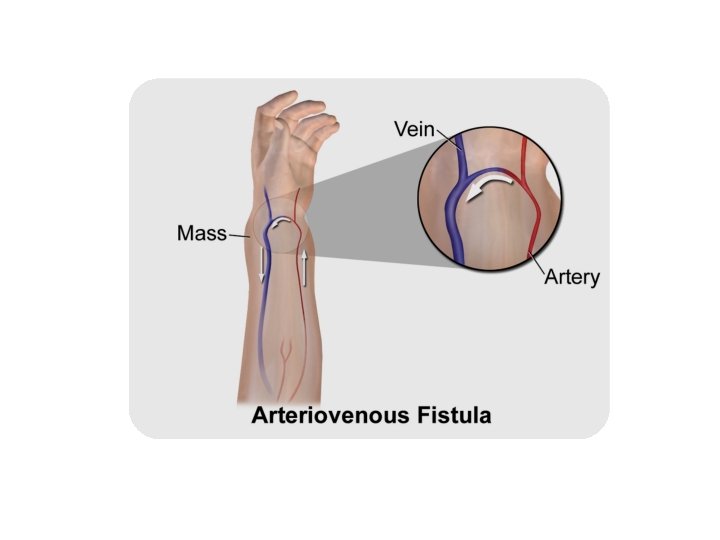
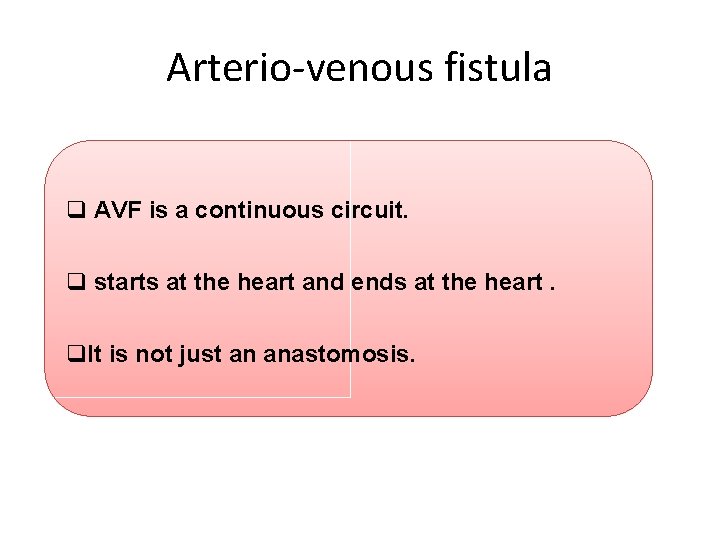
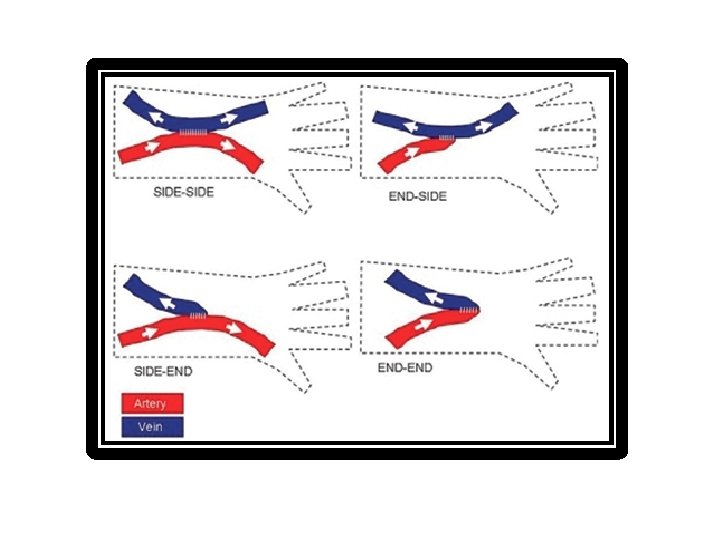
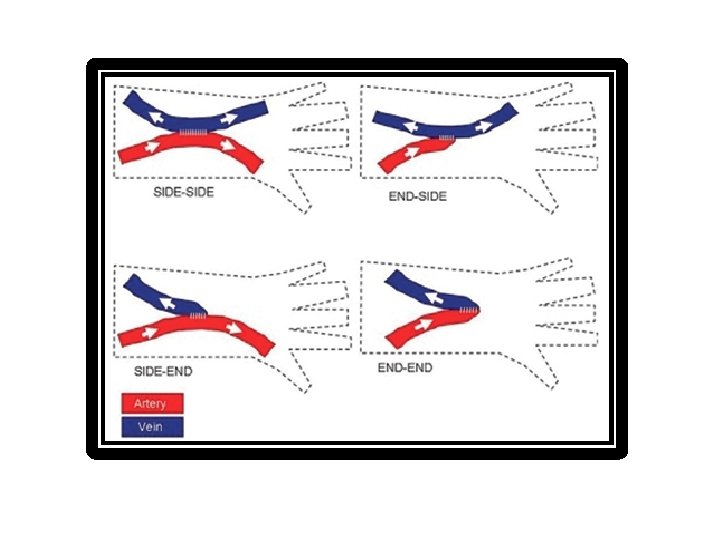
Arterio-venous fistula q AVF is a continuous circuit. q starts at the heart and ends at the heart. q. It is not just an anastomosis.
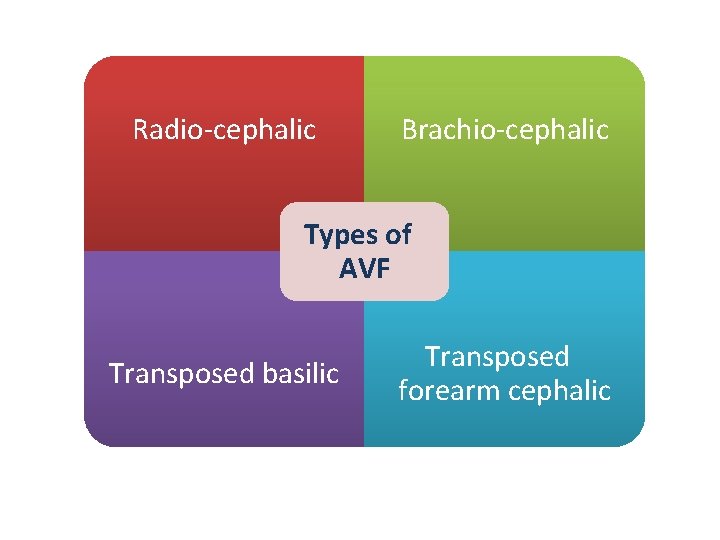
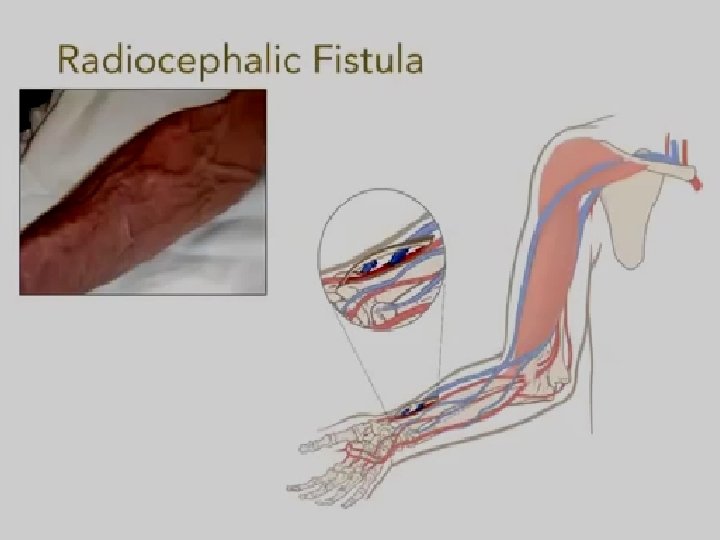
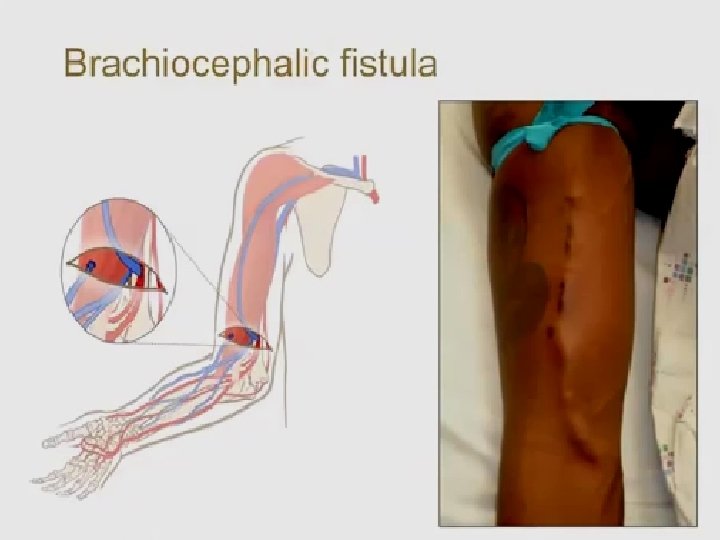
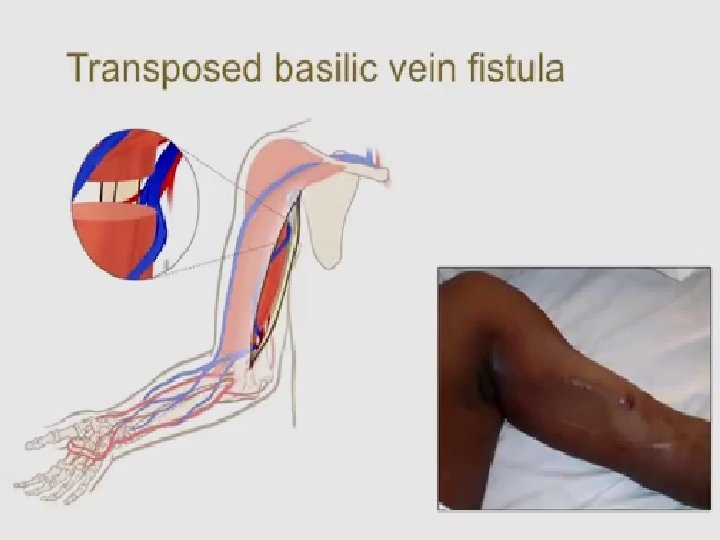
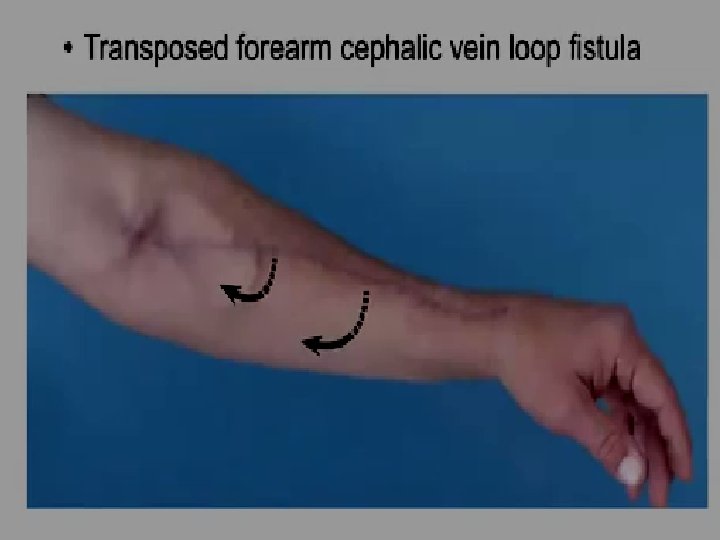
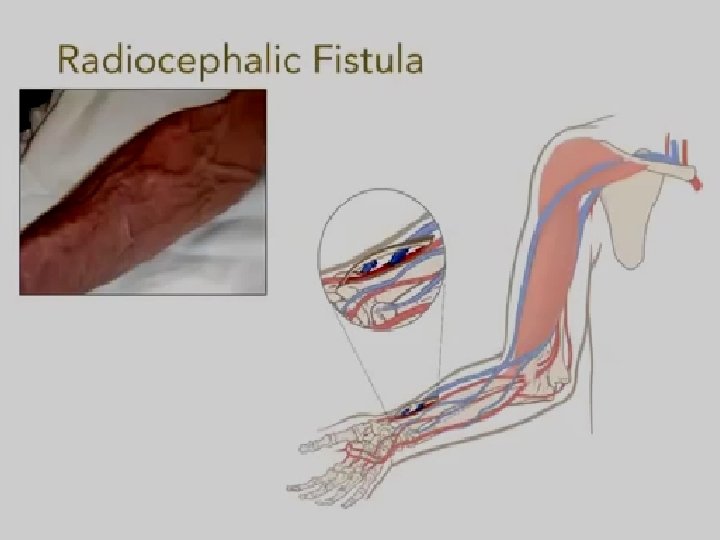
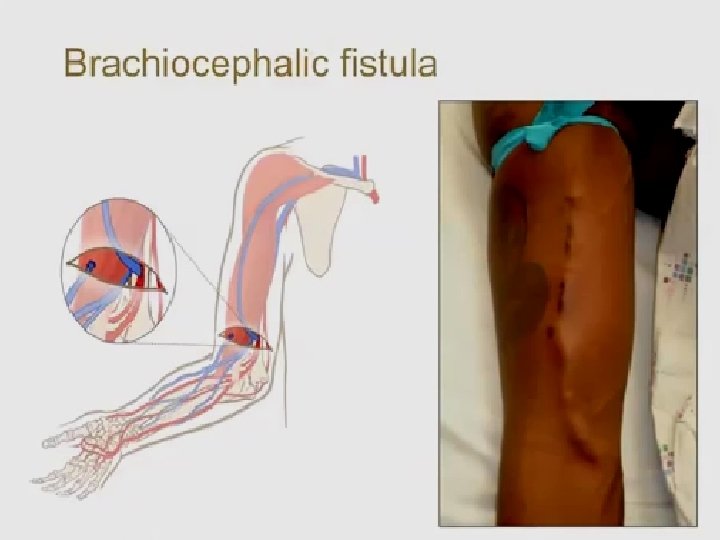
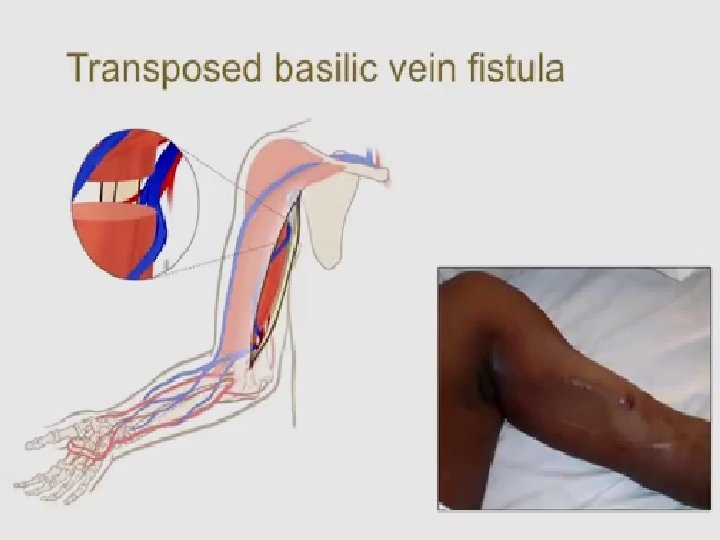
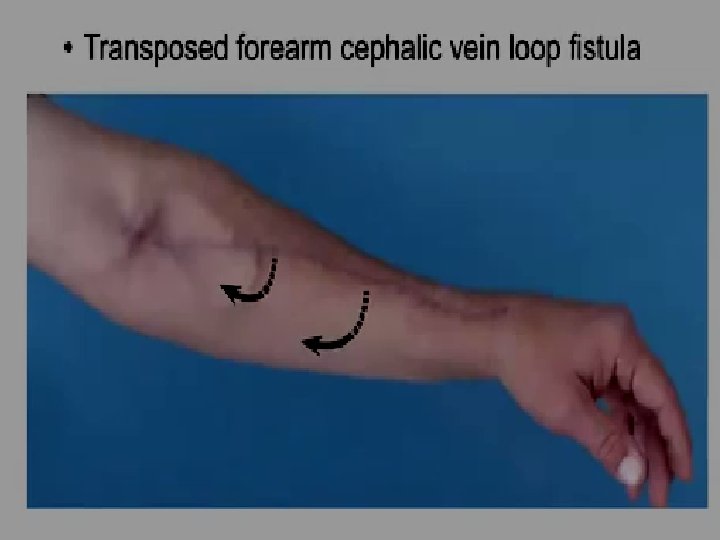
Radio-cephalic Brachio-cephalic Types of AVF Transposed basilic Transposed forearm cephalic
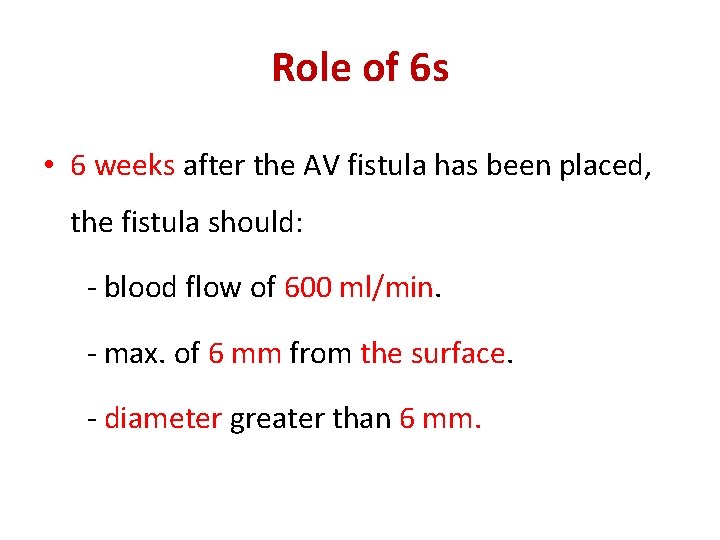
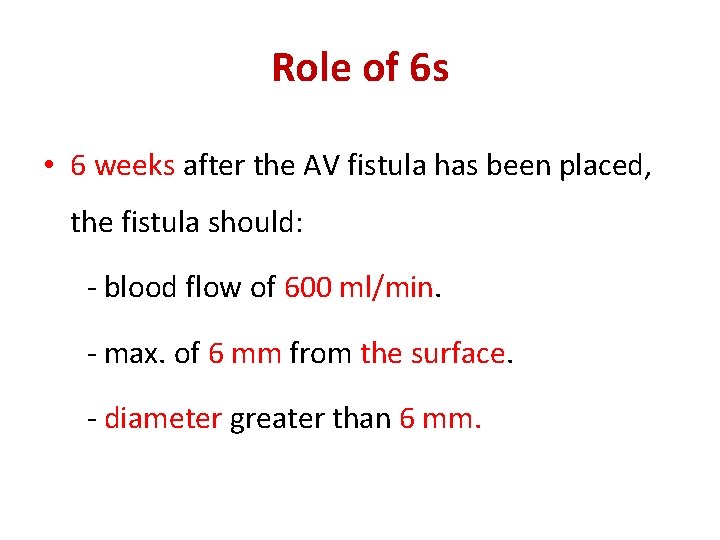
Role of 6 s • 6 weeks after the AV fistula has been placed, the fistula should: - blood flow of 600 ml/min. - max. of 6 mm from the surface. - diameter greater than 6 mm.
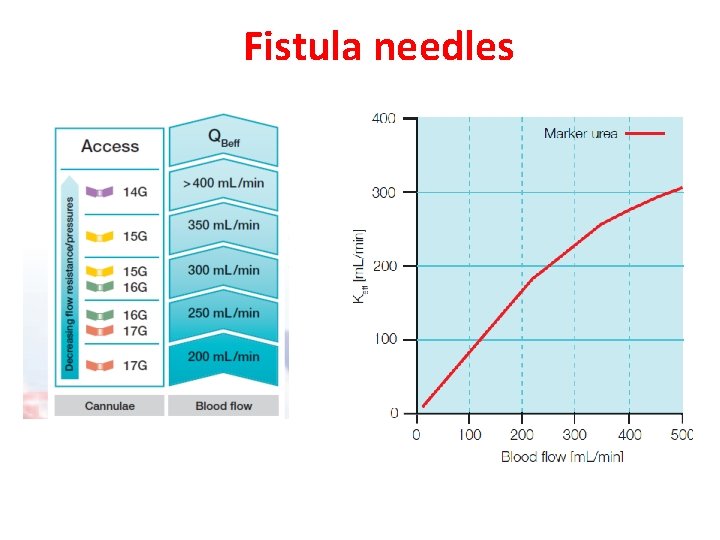
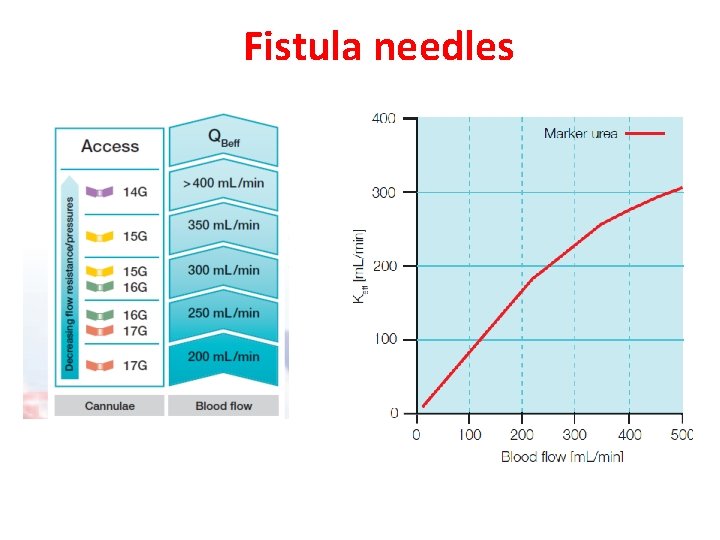
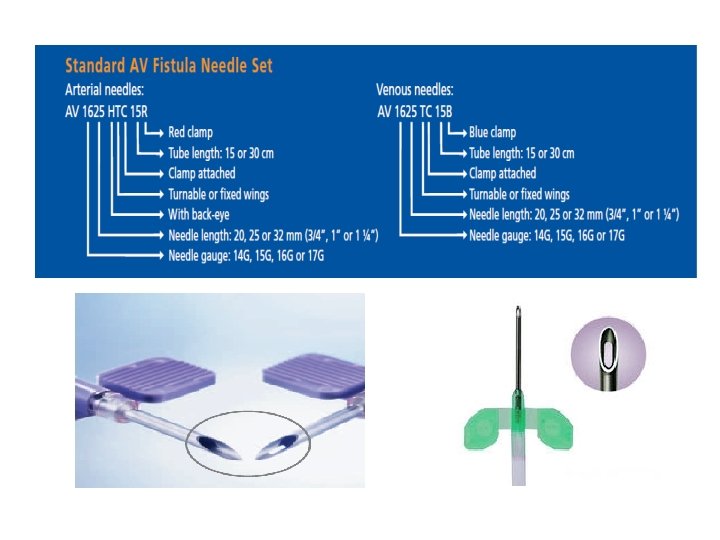
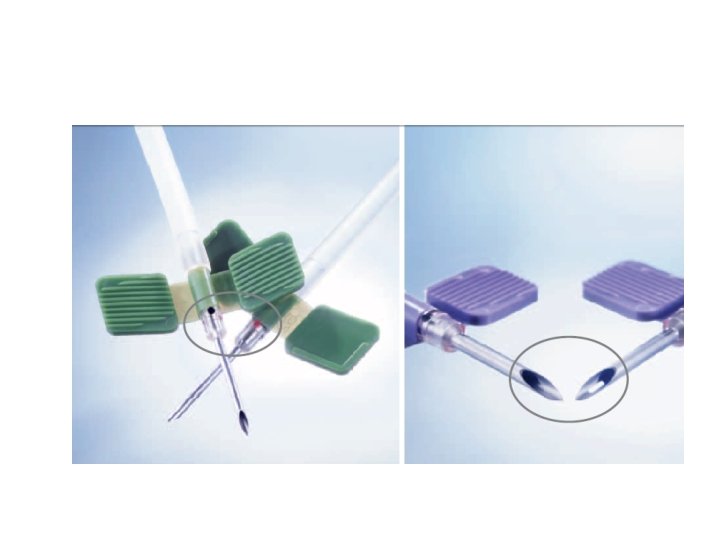
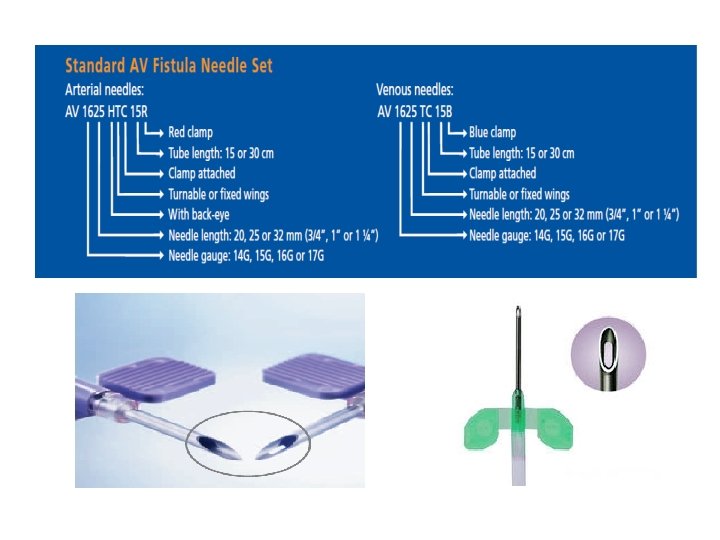
Fistula needles
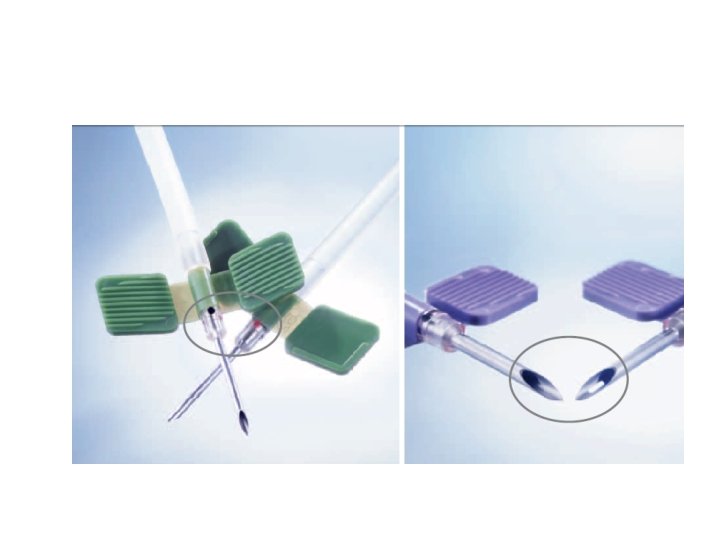
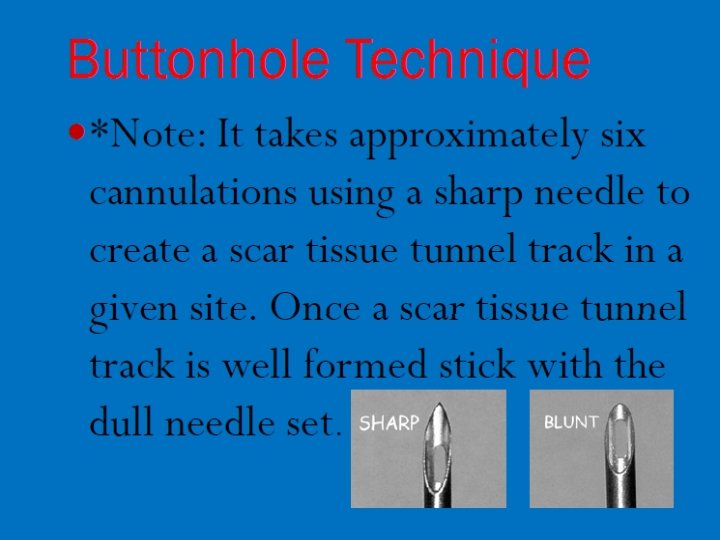
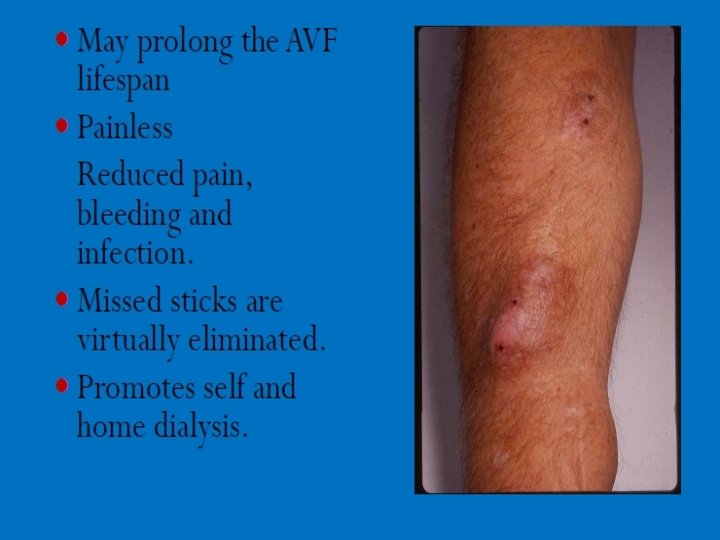
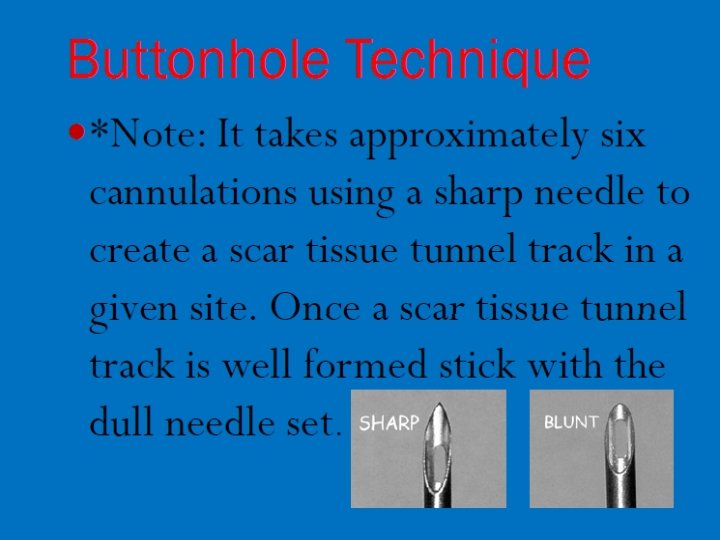
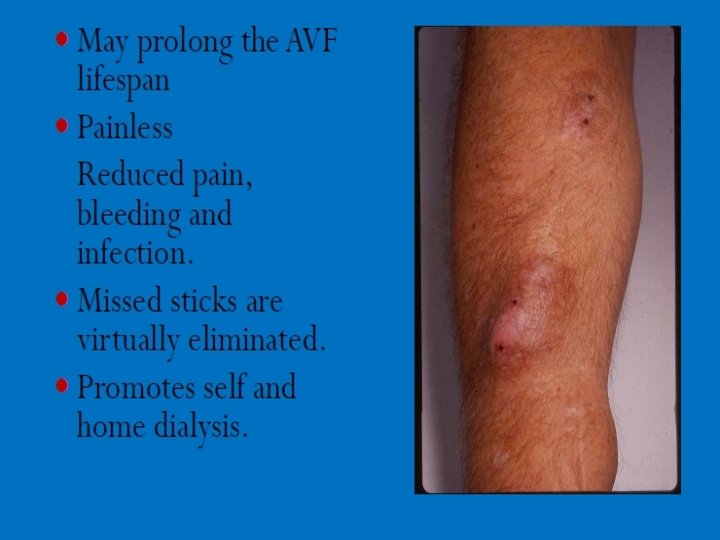
Cannulation techniques











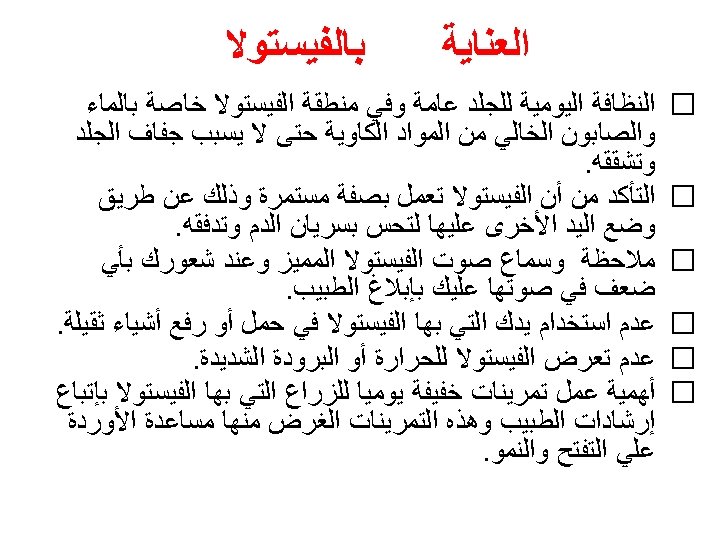
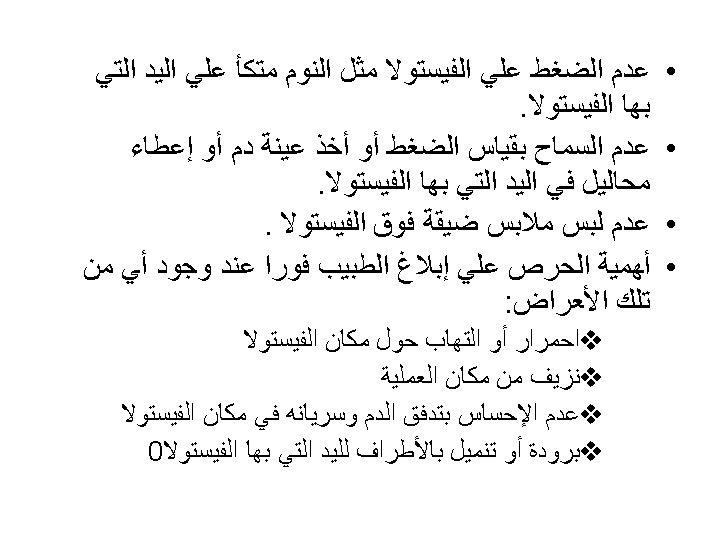
Fistula care
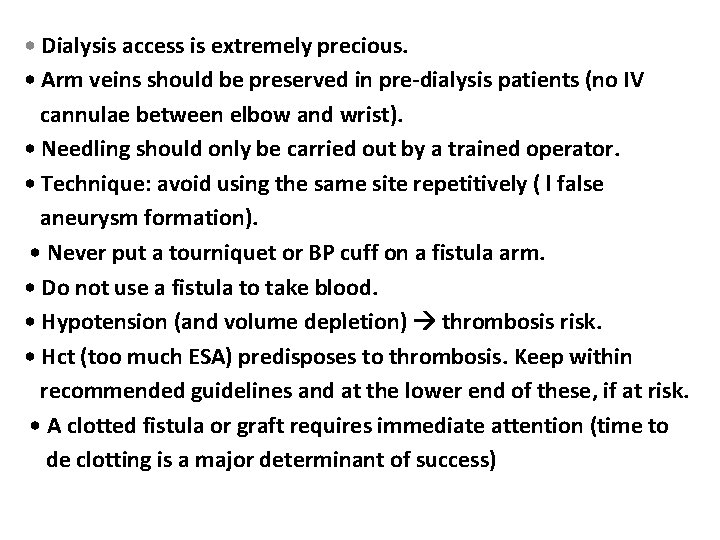
• Dialysis access is extremely precious. • Arm veins should be preserved in pre-dialysis patients (no IV cannulae between elbow and wrist). • Needling should only be carried out by a trained operator. • Technique: avoid using the same site repetitively ( l false aneurysm formation). • Never put a tourniquet or BP cuff on a fistula arm. • Do not use a fistula to take blood. • Hypotension (and volume depletion) thrombosis risk. • Hct (too much ESA) predisposes to thrombosis. Keep within recommended guidelines and at the lower end of these, if at risk. • A clotted fistula or graft requires immediate attention (time to de clotting is a major determinant of success)
Fistula assessment Feel See Hear



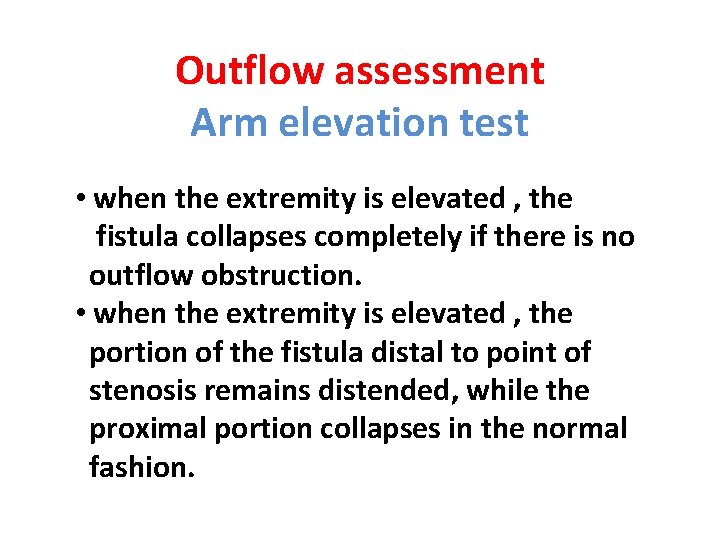
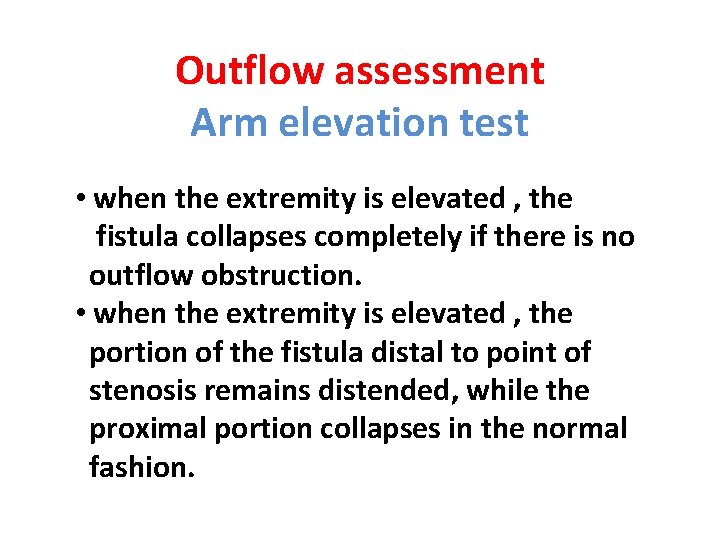
Outflow assessment Arm elevation test • when the extremity is elevated , the fistula collapses completely if there is no outflow obstruction. • when the extremity is elevated , the portion of the fistula distal to point of stenosis remains distended, while the proximal portion collapses in the normal fashion.
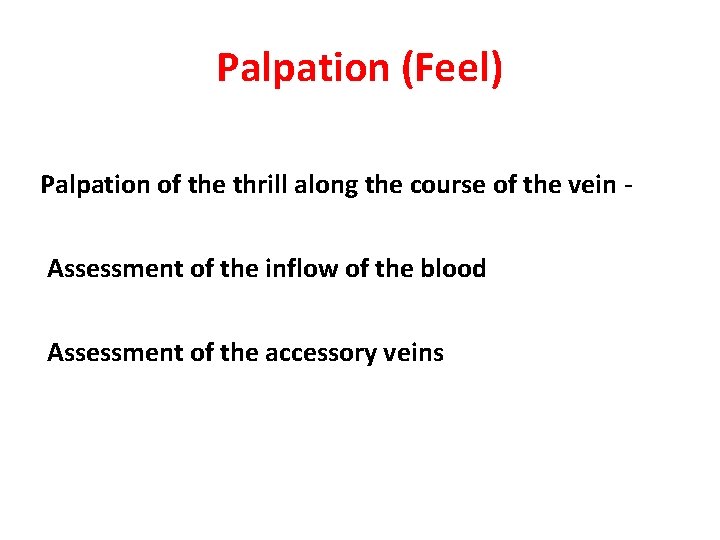
Palpation (Feel) Palpation of the thrill along the course of the vein Assessment of the inflow of the blood Assessment of the accessory veins
Augmentation test
Assessment of the accessory veins
Auscultation the bruit along the course of the vein to the heart
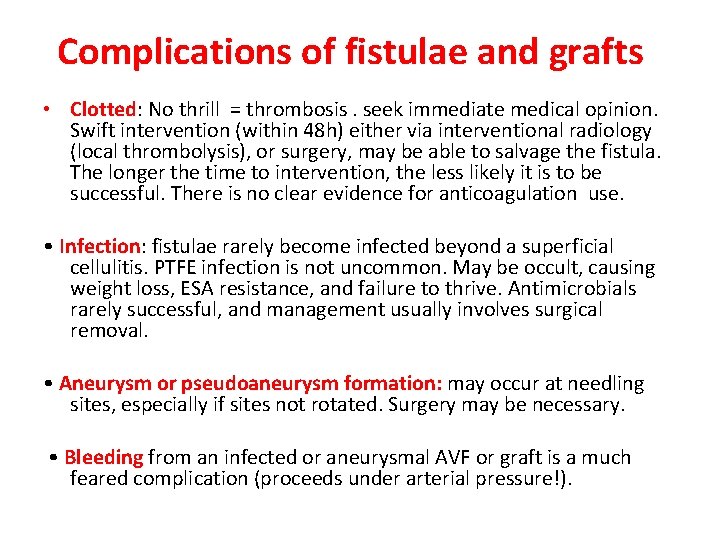
Complications of fistulae and grafts • Clotted: No thrill = thrombosis. seek immediate medical opinion. Swift intervention (within 48 h) either via interventional radiology (local thrombolysis), or surgery, may be able to salvage the fistula. The longer the time to intervention, the less likely it is to be successful. There is no clear evidence for anticoagulation use. • Infection: fistulae rarely become infected beyond a superficial cellulitis. PTFE infection is not uncommon. May be occult, causing weight loss, ESA resistance, and failure to thrive. Antimicrobials rarely successful, and management usually involves surgical removal. • Aneurysm or pseudoaneurysm formation: may occur at needling sites, especially if sites not rotated. Surgery may be necessary. • Bleeding from an infected or aneurysmal AVF or graft is a much feared complication (proceeds under arterial pressure!).
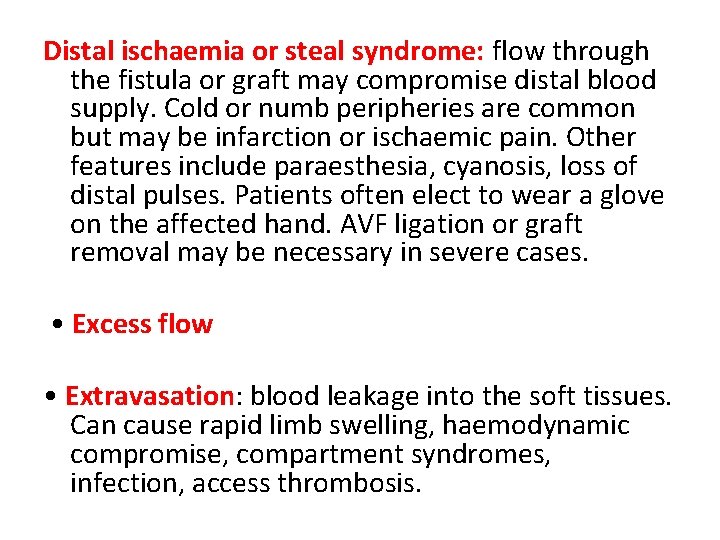
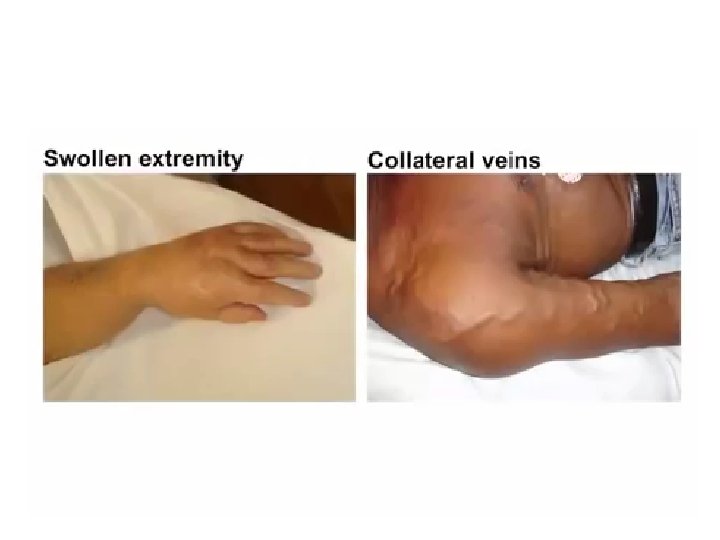
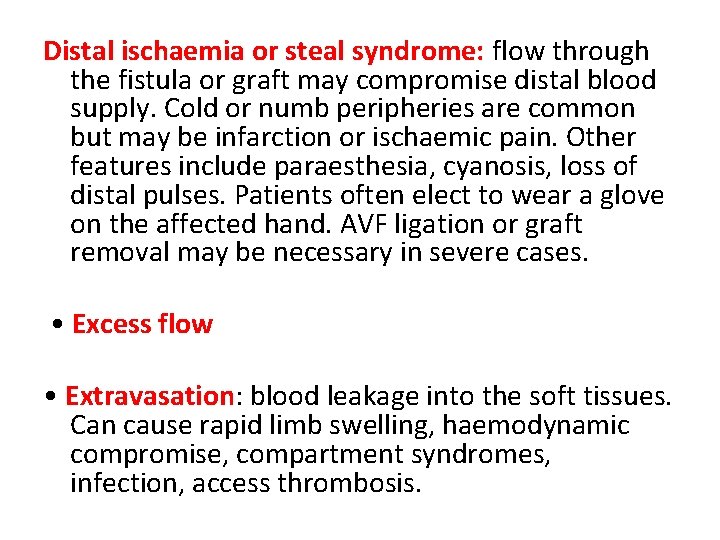
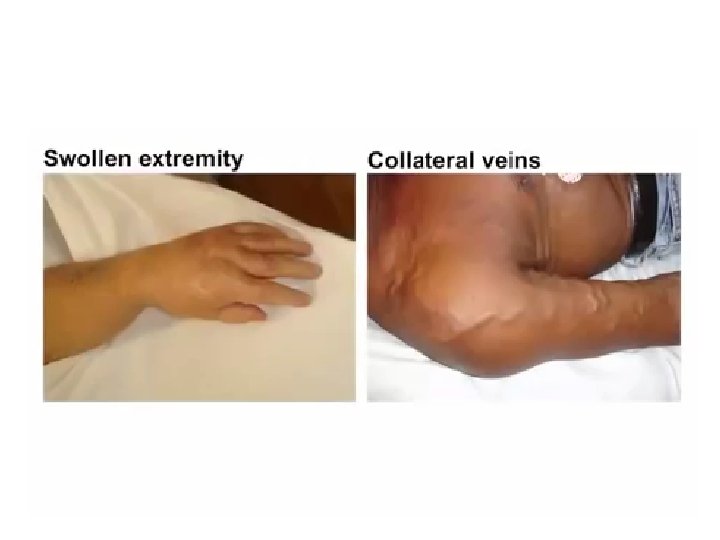
Distal ischaemia or steal syndrome: flow through the fistula or graft may compromise distal blood supply. Cold or numb peripheries are common but may be infarction or ischaemic pain. Other features include paraesthesia, cyanosis, loss of distal pulses. Patients often elect to wear a glove on the affected hand. AVF ligation or graft removal may be necessary in severe cases. • Excess flow • Extravasation: blood leakage into the soft tissues. Can cause rapid limb swelling, haemodynamic compromise, compartment syndromes, infection, access thrombosis.













n a Th u o y k T k n a h u o y
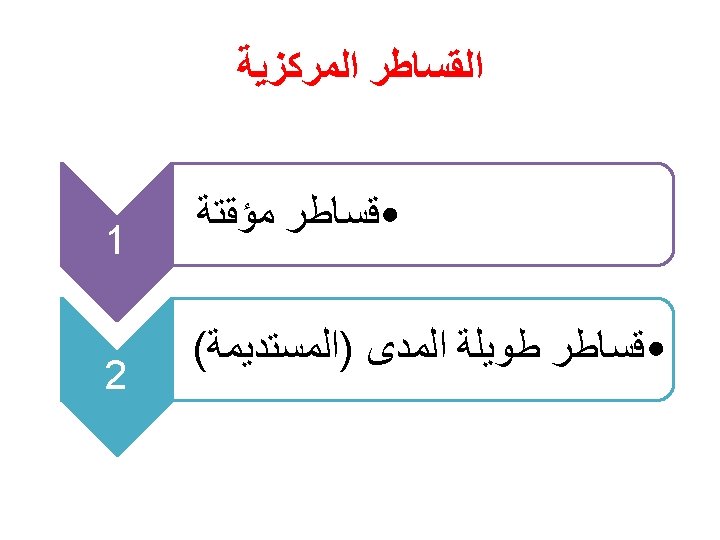
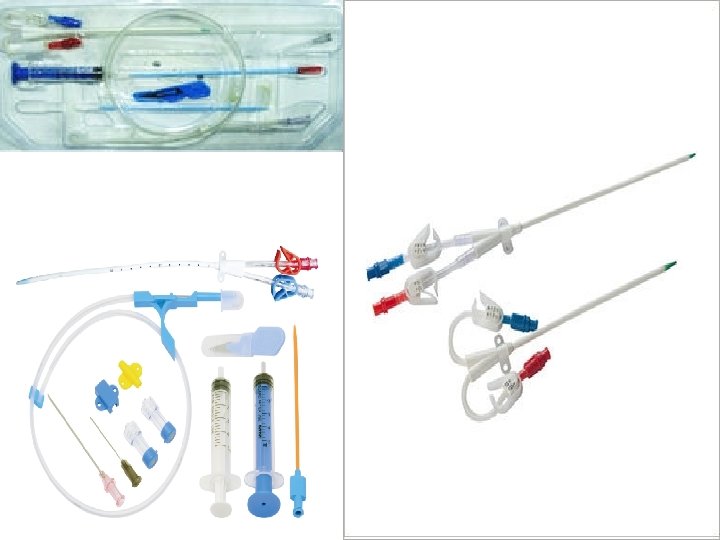
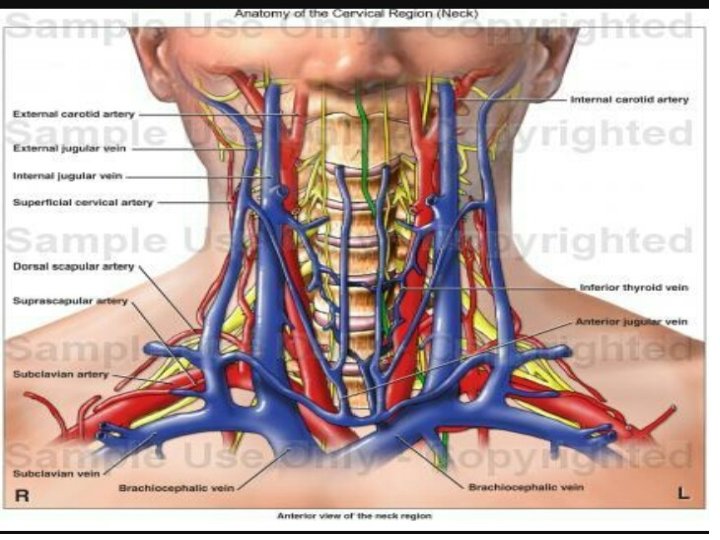
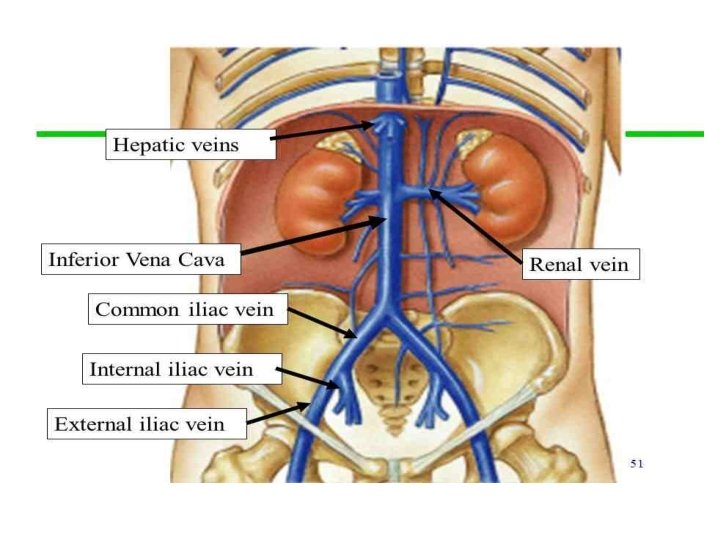
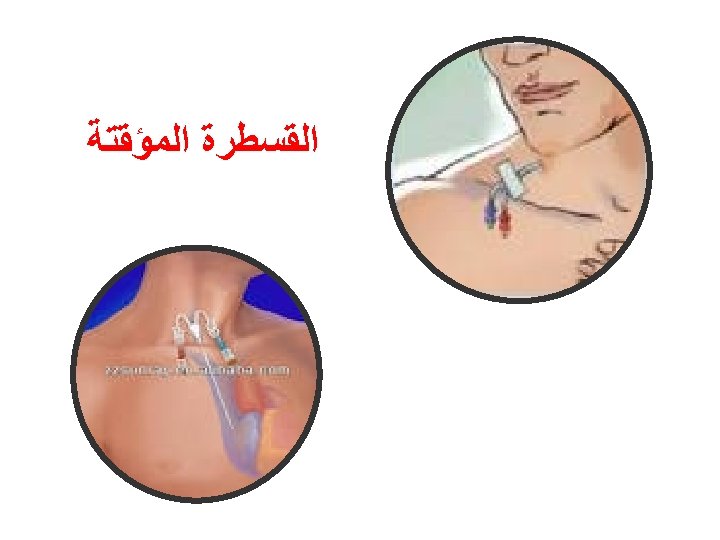
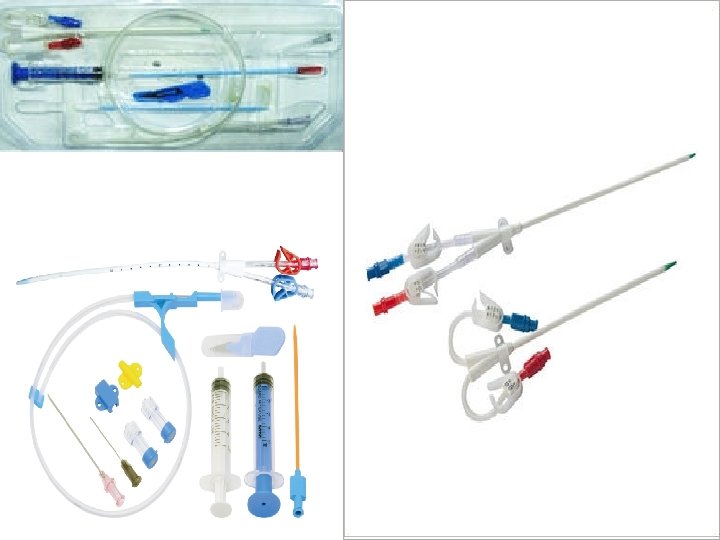
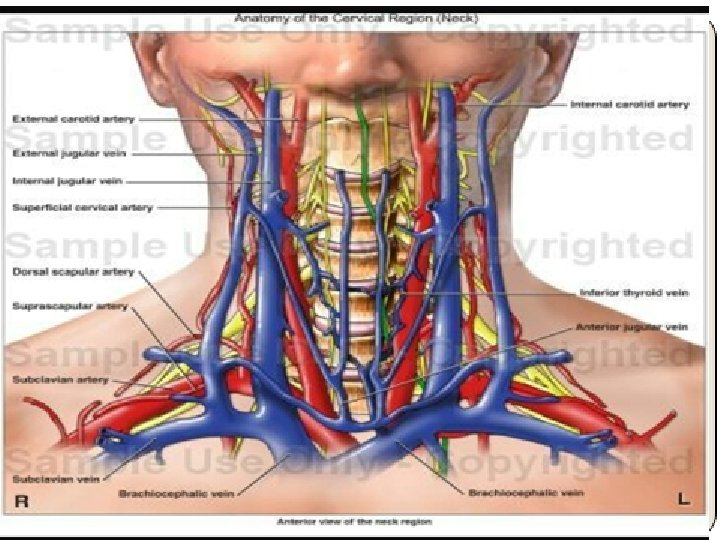
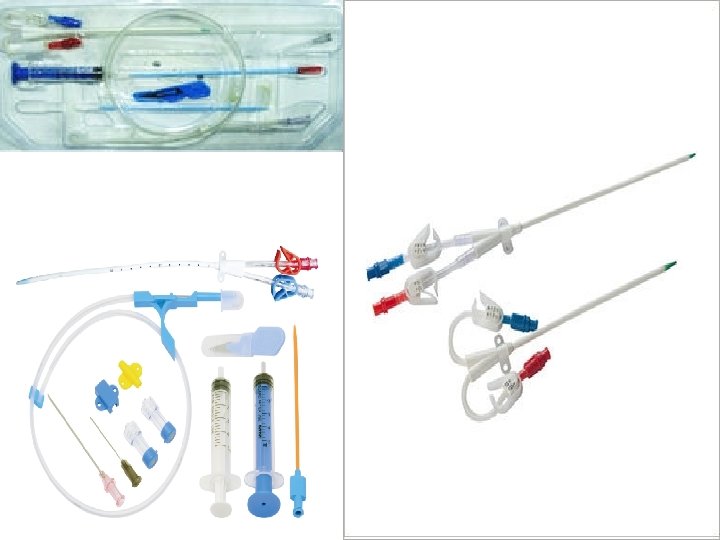
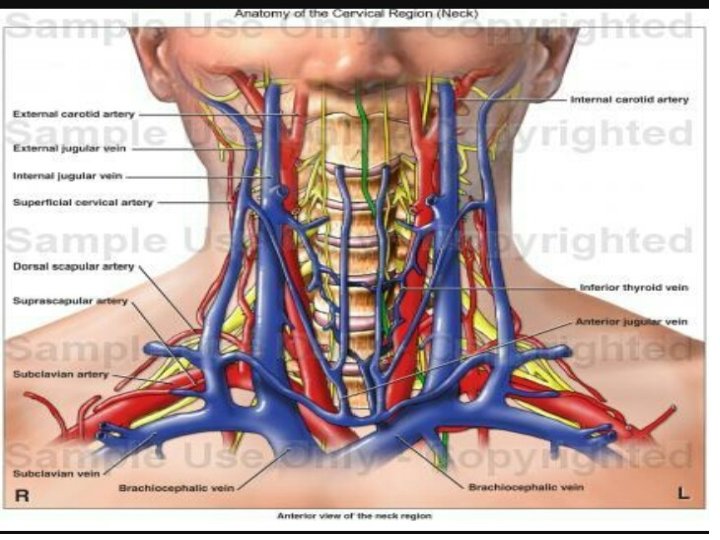
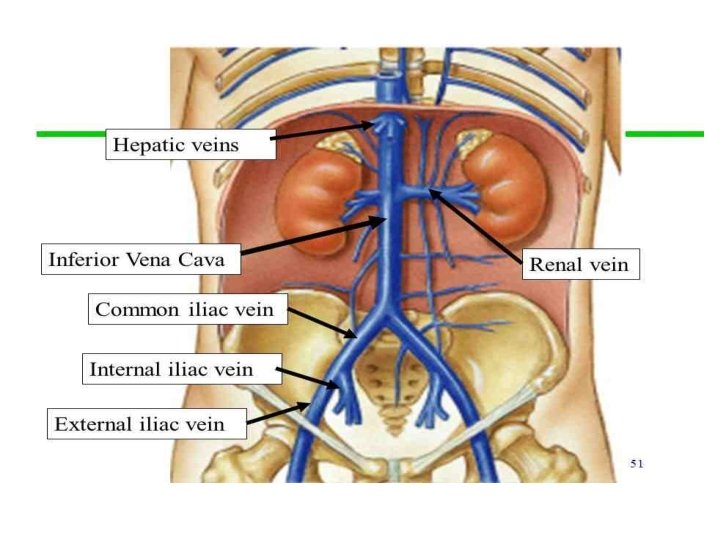
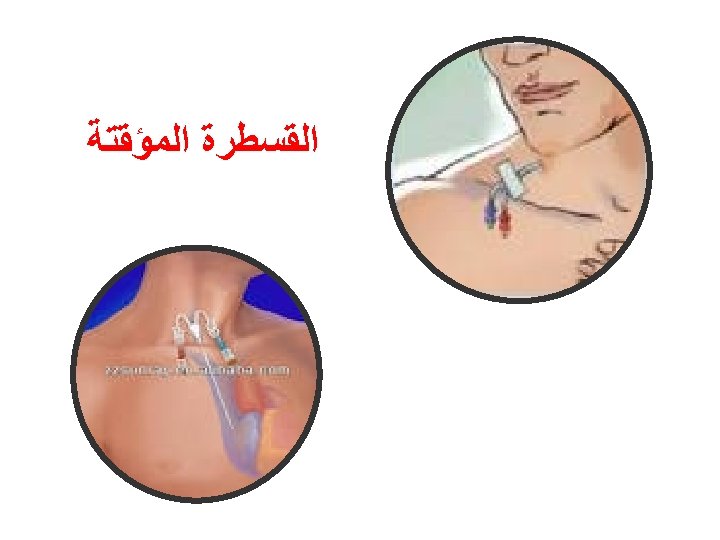
Temporary dialysis catheter
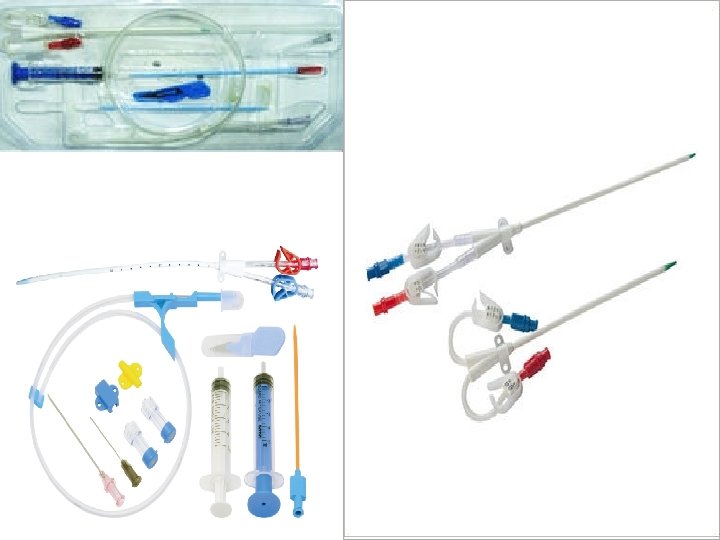
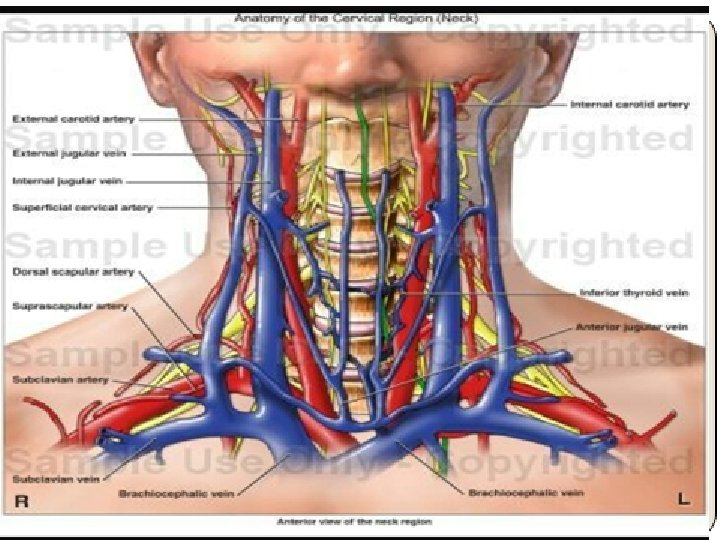
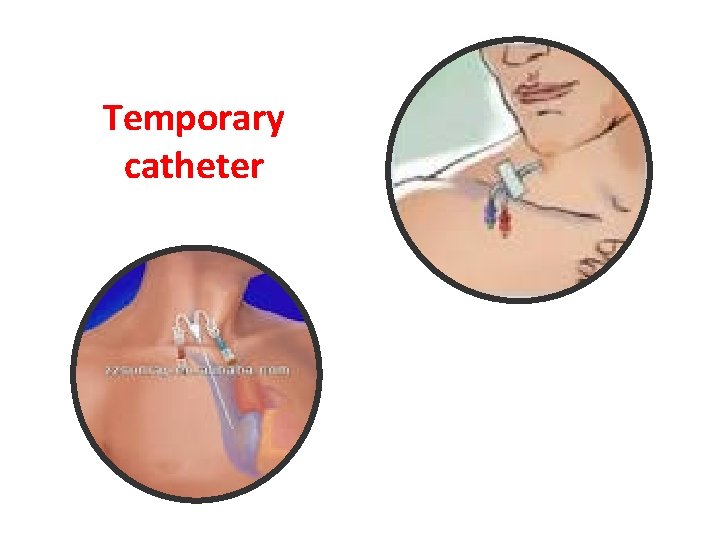
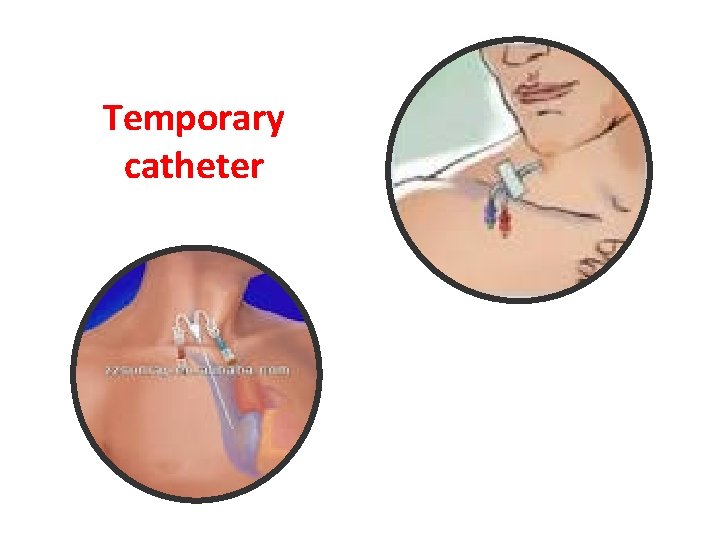
Temporary catheter
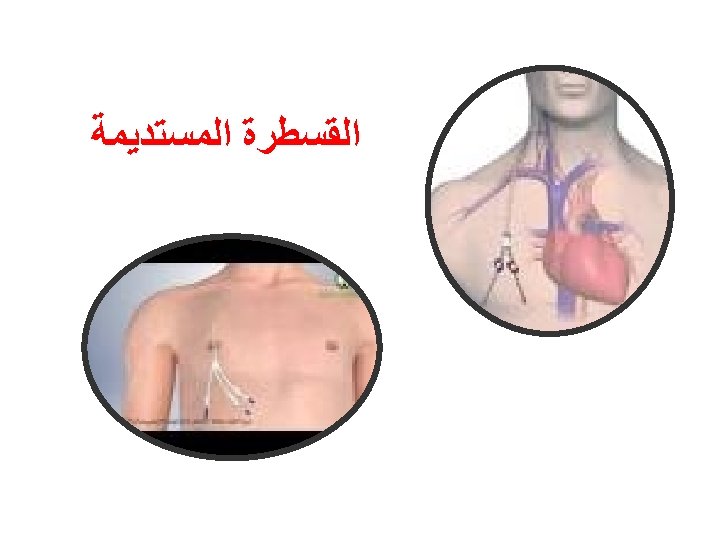
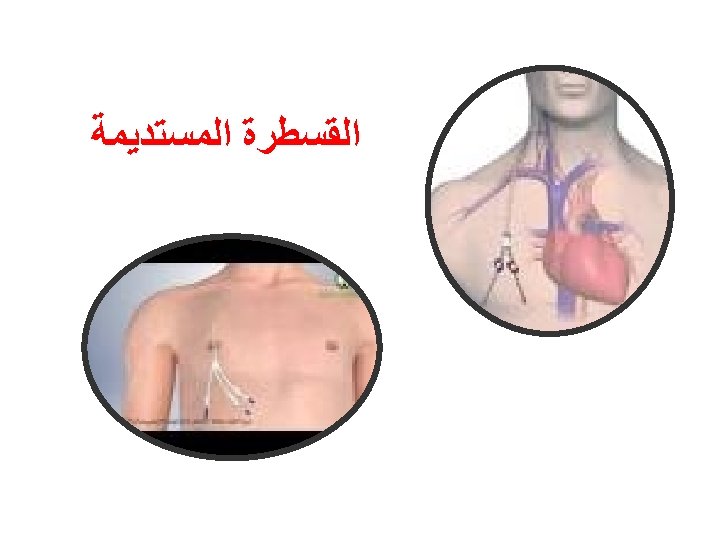
Tunneled dialysis catheter

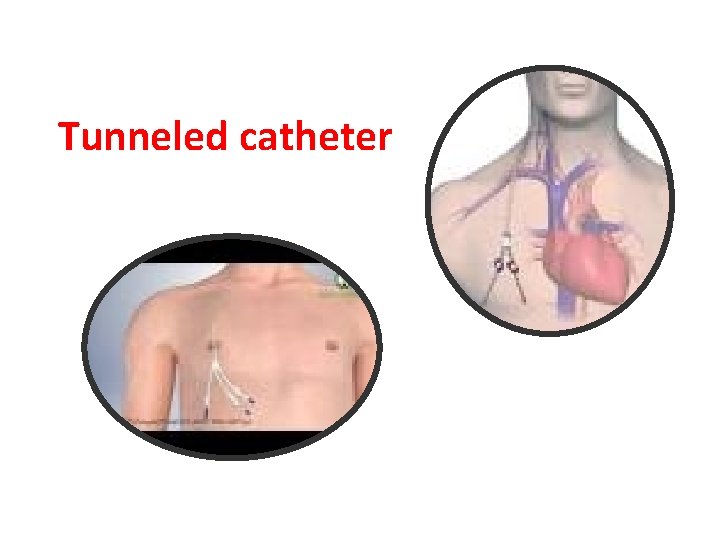
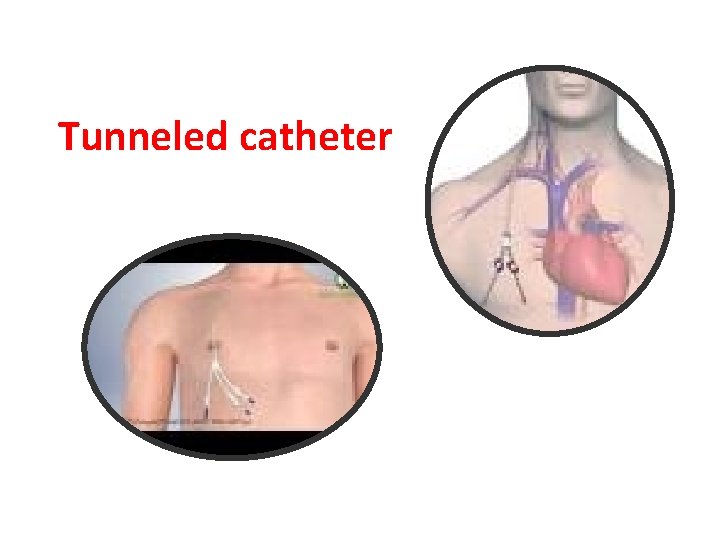
Tunneled catheter
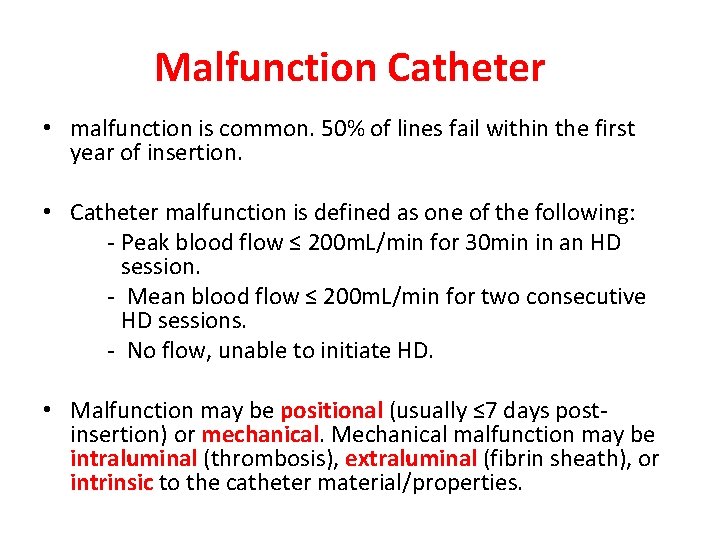
Malfunction Catheter • malfunction is common. 50% of lines fail within the first year of insertion. • Catheter malfunction is defined as one of the following: - Peak blood flow ≤ 200 m. L/min for 30 min in an HD session. - Mean blood flow ≤ 200 m. L/min for two consecutive HD sessions. - No flow, unable to initiate HD. • Malfunction may be positional (usually ≤ 7 days postinsertion) or mechanical. Mechanical malfunction may be intraluminal (thrombosis), extraluminal (fibrin sheath), or intrinsic to the catheter material/properties.
Primary prevention • Strategies include heparin, rt. PA, or trisodium citrate catheter lumen lock between sessions. • The Pre. CLOT trial showed that rt. PA for primary prevention of catheter malfunction (1 mg/lumen once/week + heparin for the other two sessions) vs standard heparin (5, 000 U/m. L to fill lumen) was associated with significantly less catheter malfunction and bacteraemia, with no increase in bleeding events. • Trisodium citrate (4, 30, or 46. 7%) has also been shown to be more effective than heparin and causes less bleeding, less biofilm formation, and a significant reduction in catheter-related bacteraemia. • There are no convincing data for low-dose warfarin, ticlopidine, or other antiplatelet agents with respect to primary prevention.
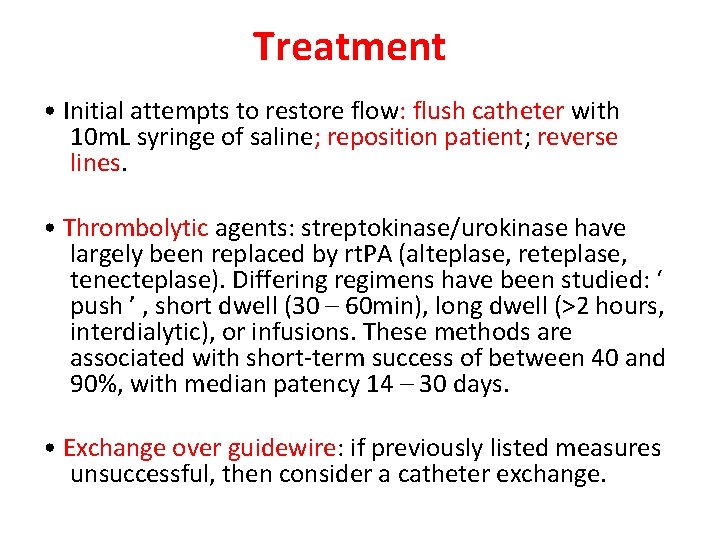
Treatment • Initial attempts to restore flow: flush catheter with 10 m. L syringe of saline; reposition patient; reverse lines. • Thrombolytic agents: streptokinase/urokinase have largely been replaced by rt. PA (alteplase, reteplase, tenecteplase). Differing regimens have been studied: ‘ push ’ , short dwell (30 – 60 min), long dwell (>2 hours, interdialytic), or infusions. These methods are associated with short-term success of between 40 and 90%, with median patency 14 – 30 days. • Exchange over guidewire: if previously listed measures unsuccessful, then consider a catheter exchange.

n a Th u o y k T k n a h u o y