AUTONOMIC NERVOUS SYSTEM The autonomic nervous system is
- Slides: 54
AUTONOMIC NERVOUS SYSTEM
�The autonomic nervous system is concerned with the innervation of viscera, glands, blood vessels & non striated muscle. �The peripheral autonomic nervous system is comprised of - SYMPATHETIC SYSTEM(THORACOLUMBAR OUTFLOW) - PARASYMPATHETIC SYSTEM (CRANIOSACRAL OUTFLOW) 2
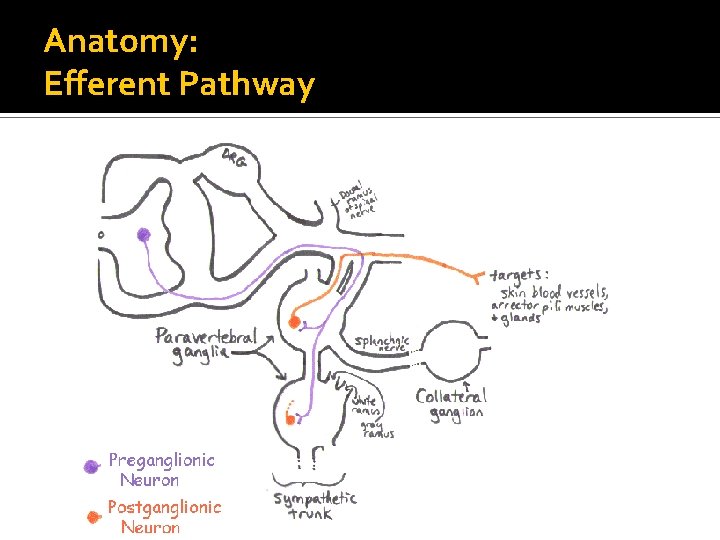
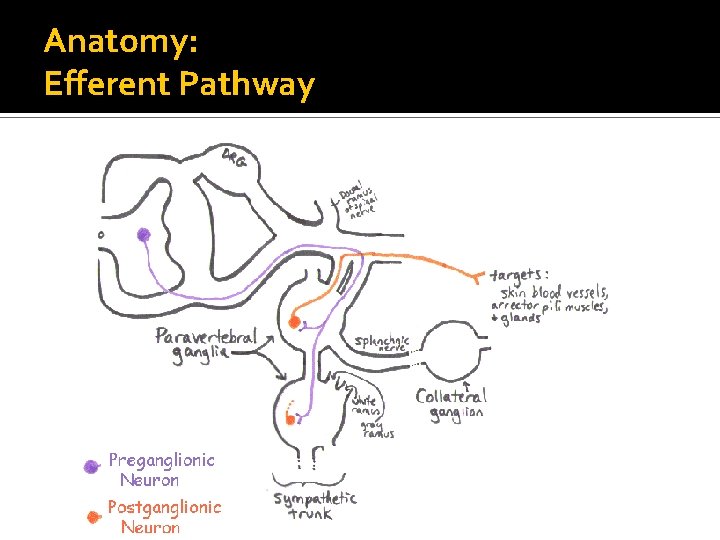
GENERAL ARRANGEMENT � EFFERENT AUTONOMIC NERVE FIBRES ü All efferent fibres of the sympathetic & parasympathetic nervous system are interrupted in their course by a synapse in the peripheral ganglion. ü The preganglionic fibres are medullated while the post ganglionic fibres are non medullated. ü The preganglionic fibres synapse with the nerve cells in: a) The paravertebral sympathetic trunk b) Prevertebral nerve plexuses c) Adrenal medulla 3
�In the parasympathetic nervous system, the preganglionic cranial fibres arise from the Edinger-Westphal(IIIrd nerve), salivary (7 th & 9 th nerves)ambiguus & dorsal motor (10 th nerve) nuclei in the brain stem. �The preganglionic sympathetic fibres are usually short & synapse with many post ganglionic nerves. In contrast preganglionic parasympathetic fibres which are long & synapse with only few post ganglionic fibres 4
Divisions of the autonomic nervous system �Parasympathetic division �Sympathetic division Serve most of the same organs but cause opposing or antagonistic effects Parasysmpathetic: routine maintenance “rest &digest” Sympathetic: mobilization & increased metabolism “fight, flight or fright” or “fight, flight or freeze” 5
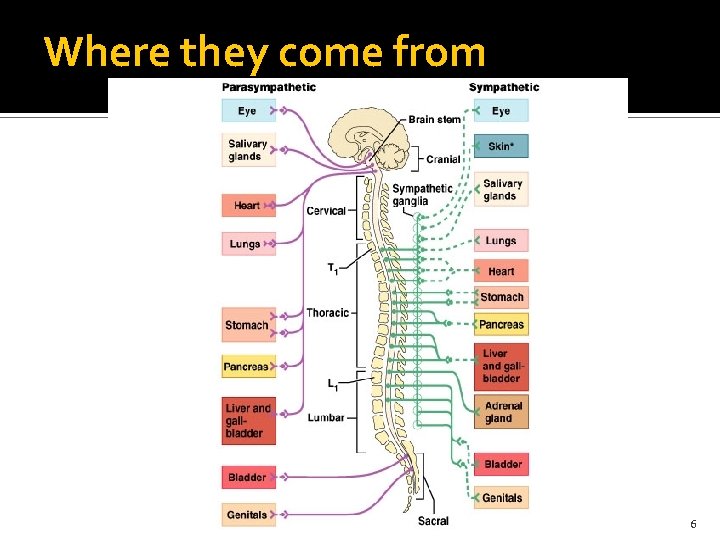
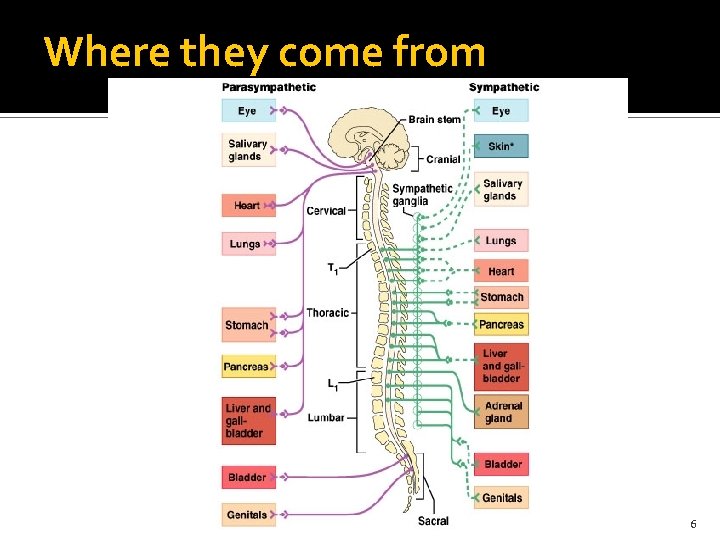
Where they come from 6
TRANSMITTER SUBSTANCES SYMPATHETIC NERVOUS SYSTEM �Preganglionic nerve endings- Acetylcholine �Postganglionic nerve endings- Noradrenaline PARASYMPATHETIC NERVOUS SYSTEM Acetlycholine is the transmitter substance 7
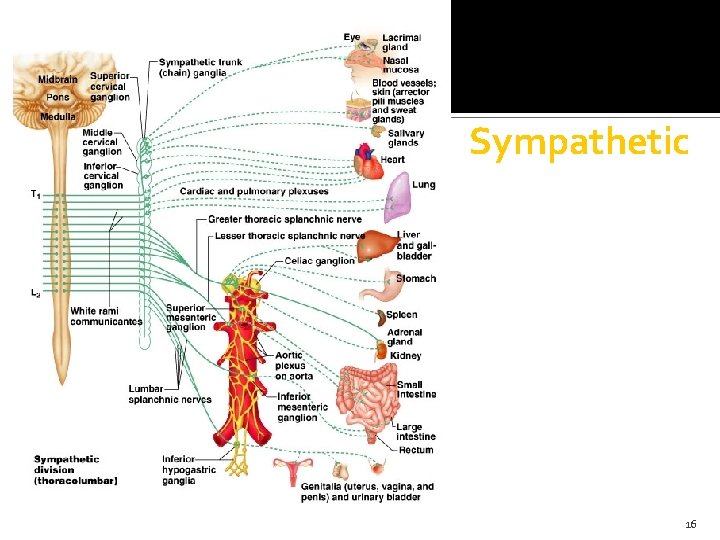
THE SYMPATHETIC NERVOUS SYSTEM 8
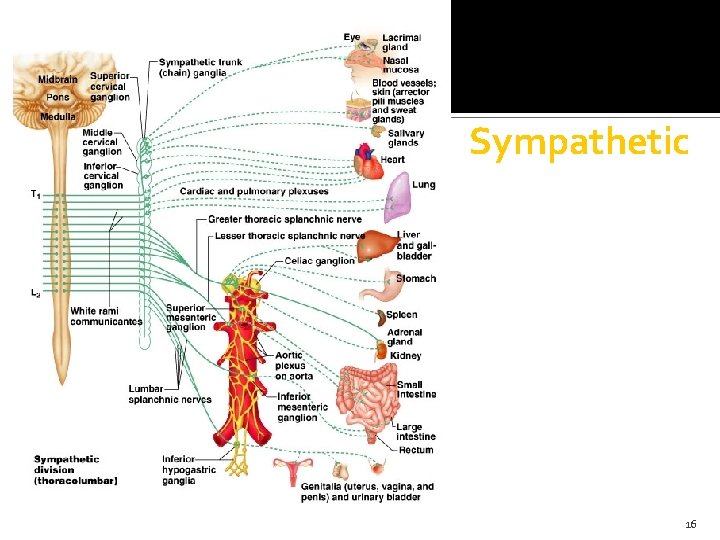
Sympathetic nervous system “fight, flight or fright” � Also called thoracolumbar system: all its neurons are in lateral horn of gray matter from T 1 -L 2 � Lead to every part of the body (unlike parasymp. ) Easy to remember that when nervous, you sweat; when afraid, hair stands on end; when excited blood pressure rises (vasoconstriction): these sympathetic only Also causes: dry mouth, pupils to dilate, increased heart & respiratory rates to increase O 2 to skeletal muscles, and liver to release glucose � Norepinephrine (aka noradrenaline) is neurotransmitter released by most postganglionic fibers (acetylcholine in preganglionic): “adrenergic” 9
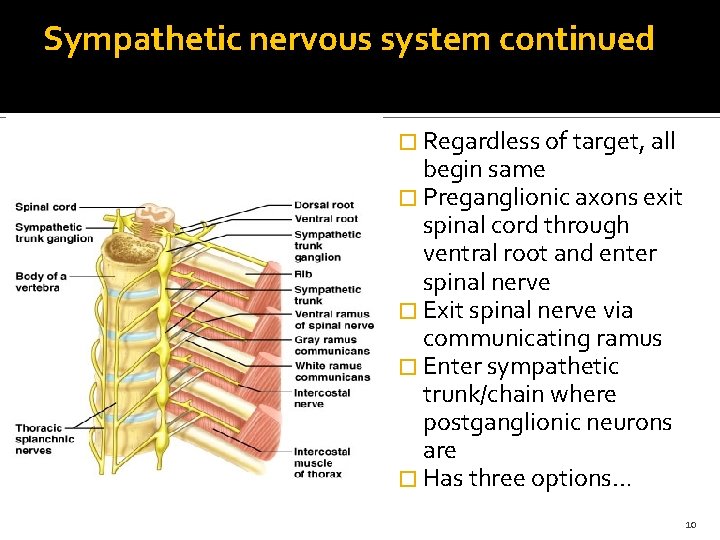
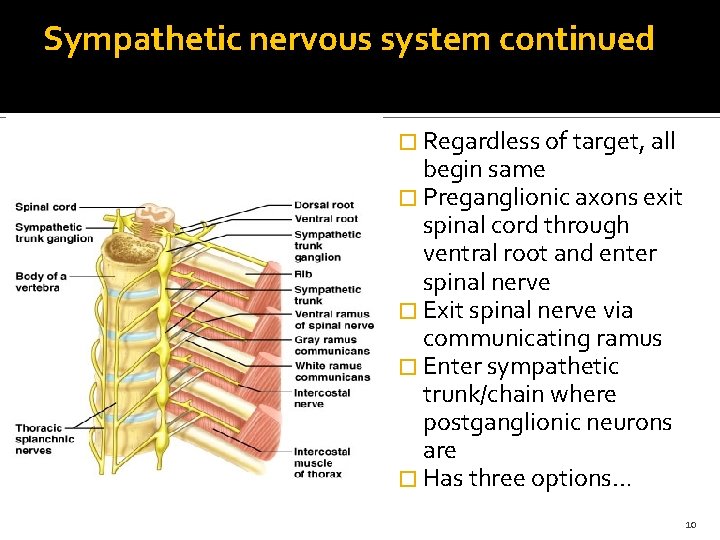
Sympathetic nervous system continued � Regardless of target, all begin same � Preganglionic axons exit spinal cord through ventral root and enter spinal nerve � Exit spinal nerve via communicating ramus � Enter sympathetic trunk/chain where postganglionic neurons are � Has three options… 10
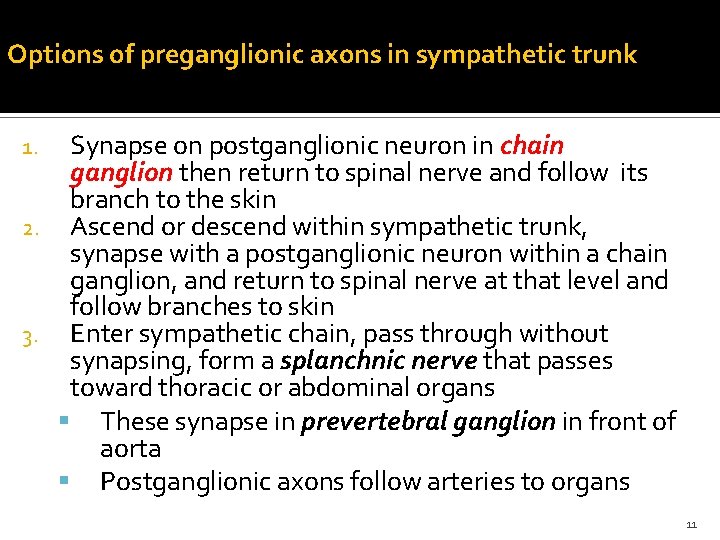
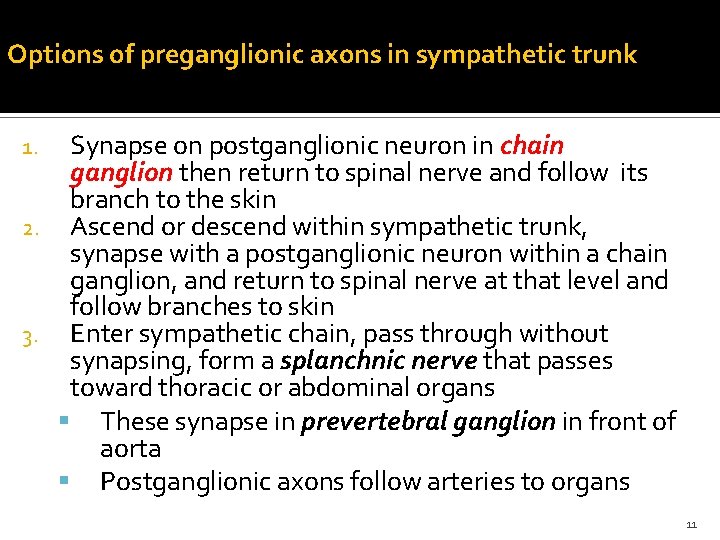
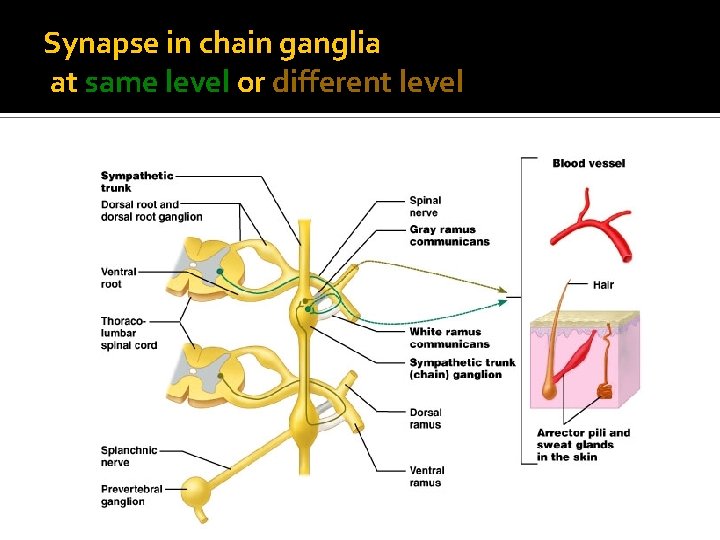
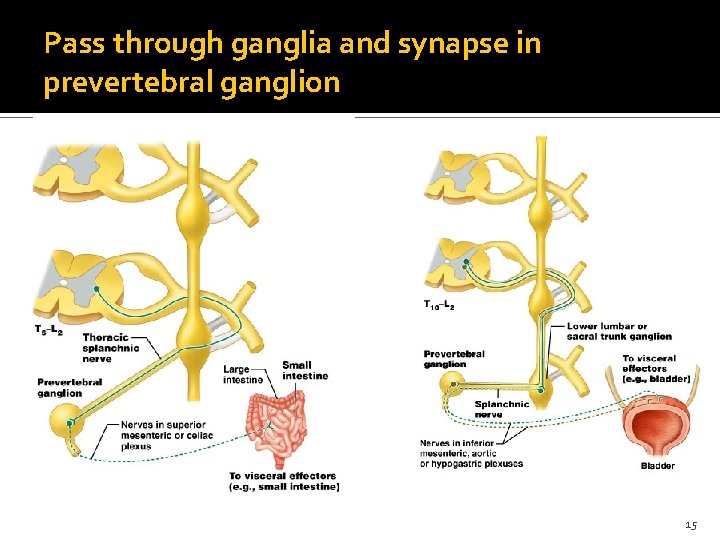
Options of preganglionic axons in sympathetic trunk Synapse on postganglionic neuron in chain ganglion then return to spinal nerve and follow its branch to the skin 2. Ascend or descend within sympathetic trunk, synapse with a postganglionic neuron within a chain ganglion, and return to spinal nerve at that level and follow branches to skin 3. Enter sympathetic chain, pass through without synapsing, form a splanchnic nerve that passes toward thoracic or abdominal organs These synapse in prevertebral ganglion in front of aorta Postganglionic axons follow arteries to organs 1. 11
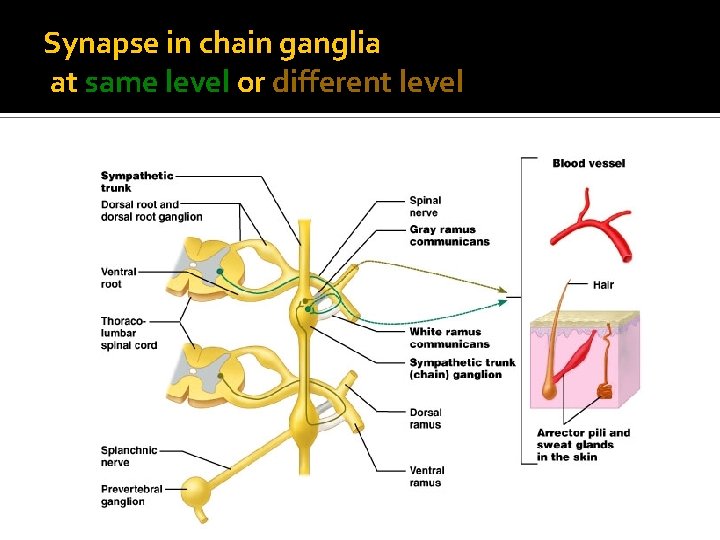
Synapse in chain ganglia at same level or different level 12
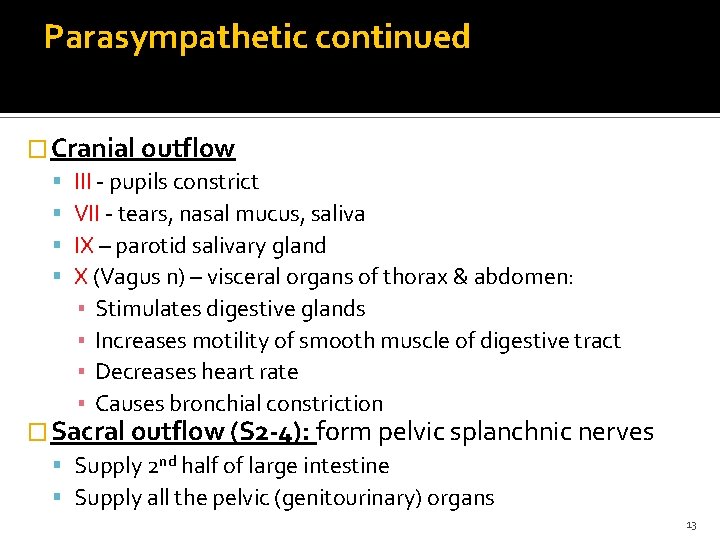
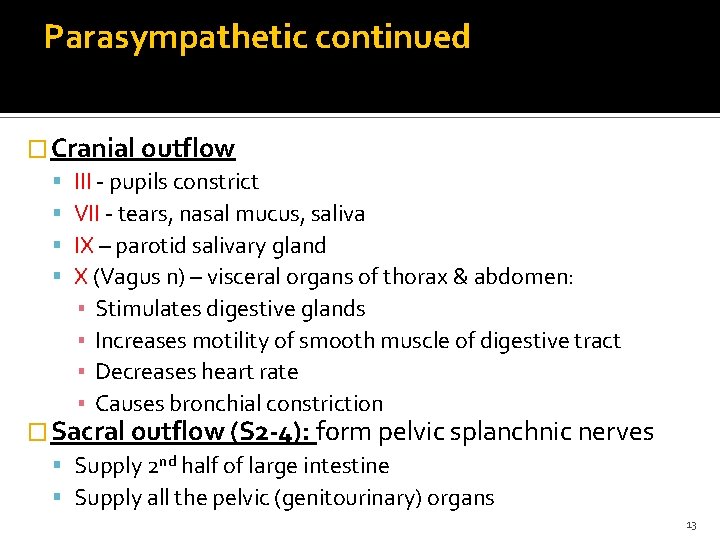
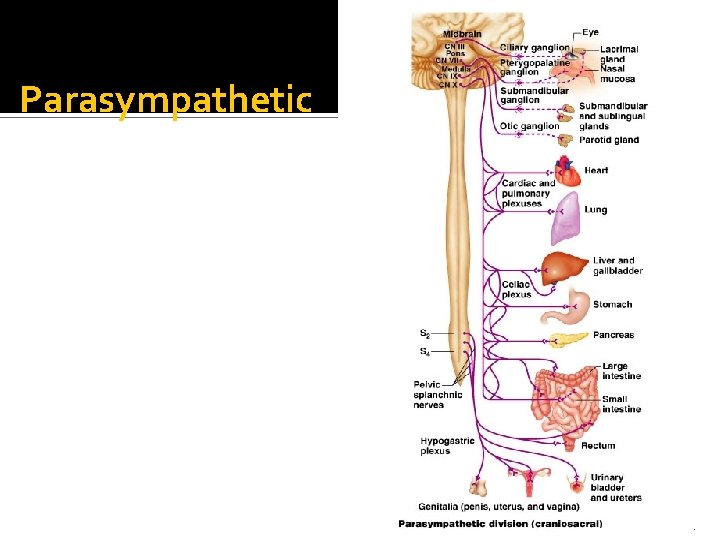
Parasympathetic continued � Cranial outflow III - pupils constrict VII - tears, nasal mucus, saliva IX – parotid salivary gland X (Vagus n) – visceral organs of thorax & abdomen: ▪ Stimulates digestive glands ▪ Increases motility of smooth muscle of digestive tract ▪ Decreases heart rate ▪ Causes bronchial constriction � Sacral outflow (S 2 -4): form pelvic splanchnic nerves Supply 2 nd half of large intestine Supply all the pelvic (genitourinary) organs 13
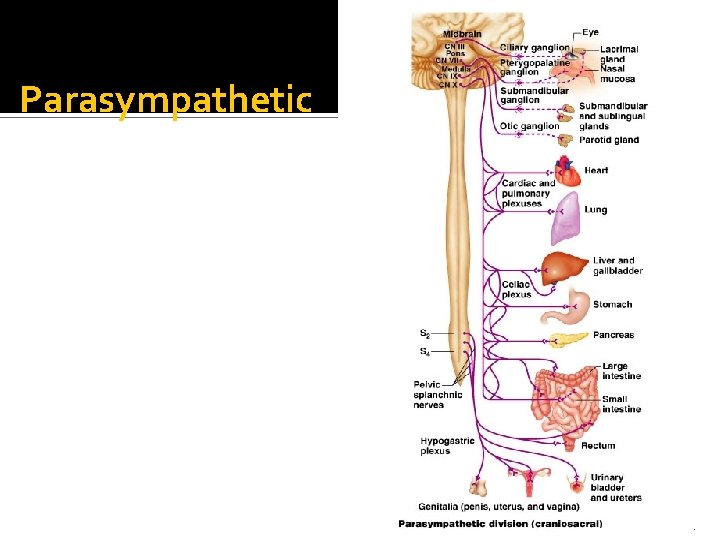
Parasympathetic 14
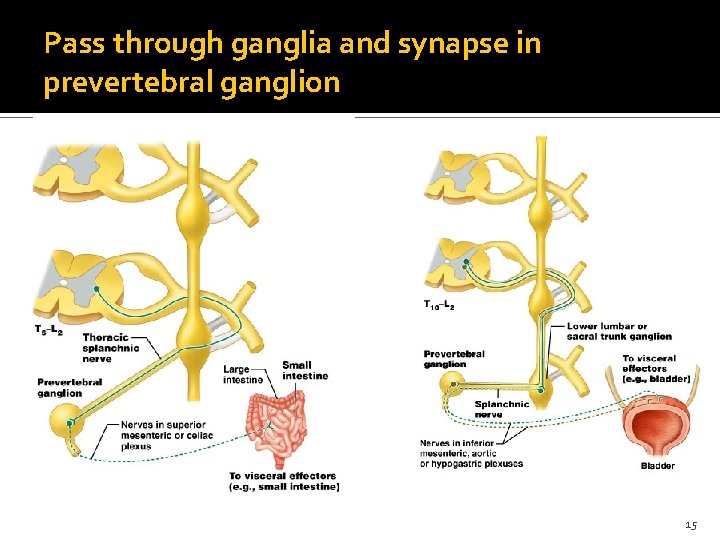
Pass through ganglia and synapse in prevertebral ganglion 15
Sympathetic 16
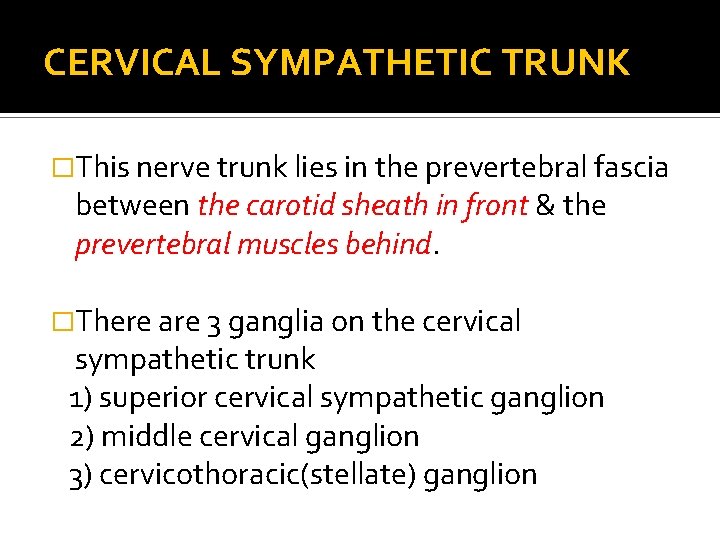
CERVICAL SYMPATHETIC TRUNK �This nerve trunk lies in the prevertebral fascia between the carotid sheath in front & the prevertebral muscles behind. �There are 3 ganglia on the cervical sympathetic trunk 1) superior cervical sympathetic ganglion 2) middle cervical ganglion 3) cervicothoracic(stellate) ganglion
� Superior cervical sympathetic ganglion: 1) LATERAL BRANCHES a) Grey rami communicantes to upper 4 cervical nerves b) Twigs to glossopharangeal nerve c) Jugular bulb 2) MEDIAL BRANCHES a)Laryngopharyngeal to carotid body & the pharyngeal plexus b)Cardiac branches to cardiac plexus c) Anterior branches to the internal & external carotid arteries
� MIDDLE CERVICAL GANGLION � It is the smallest of the 3 � Lies on the 6 th cervical vertebra in front or behind the inferior thyroid artery at the level of the cricoid cartilage & transverse process of c 6 � It gives rise to: a) Grey rami communicantes to the 5 th & 6 th cervical nerves b) Cardiac nerve which is the largest of the sympathetic cardiac branches c) A vascular branch which runs with the inferior thyroid artery
CERVICOTHORACIC (STELLATE) GANGLION � Formed by the fusion of the lower two cervical segmental ganglia with the 1 st thoracic ganglion. � It lies behind the vertebral artery between the neck of the 1 st rib & transverse process of 7 th cervical vertebra � It gives rise to : 1) Grey rami communicantes to 7 th, 8 th cervical & 1 st thoracic spinal nerves. 2) A plexus to the subclavian artery & its branches.
THORACIC SYMPATHETIC TRUNK � Usually comprised of 11 ganglia of which the 1 st is fused to inferior cervical ganglion. � Upper 10 ganglia lie outside the parietal pleura against the heads of the ribs & lower 2 ganglia lie on the sides of the bodies of corresponding vertebrae. � BRANCHES : 1) Grey rami communicantes to all spinal nerves 2) Visceral branches from upper 6 ganglia to pulmonary & cardiac plexus 3) The splanchnic nerves
COELIAC PLEXUS � This plexus is formed largely by contributions from the greater splanchnic & 1 st lumbar splanchnic nerves � The plexus is situated around the origin of the coeliac artery, there being a large nerve mass on each side of this vessel known as coeliac ganglion � This plexus is continuous with a network of sympathetic nerves in relation to the aorta- aortic plexus � Nerves from these plexus run to the abdominal viscera via the blood vessels
SURGICAL SYMPATHECTOMY 23
� INDICATIONS ü Peripheral vascular disease-It maybe be used in organic occlusion of arteries in which direct vascular surgery will not relieve obstruction. It is also used in certain vasospastic conditions like Raynauds disease ü Hyperhidrosis- gross sweating of the hands, axillae & feet. Sympathectomy gives permanent relief Relief of Pain – a)Visceral Pain: Excision of Coeliac ganglion or its destruction by injection of absolute alcohol or phenol has been used to relieve pain of pancreatic cancer or chronic pancreatitis b) Causalgia: Characterised by intense pain at the site of previous injury or operation. ü 24
� CERVICOTHORACIC SYMPATHECTOMY ü It is the upper thoracic & cervical sympathectomy ü Aim is to obtain sympathetic denervation of the upper limb without diving the occulopupillary fibres ü The sympathetic supply to the upper limb comes from T 2 -T 6. ü This is achieved by either Ganglionectomy or Division of the rami 25
Ganglionectomy �The stellate ganglion is best left undisturbed to prevent damage to the oculopupillary fibres from 1 st thoracic nerve �But the 2 nd & 3 rd ganglia are freed from all rami & the trunk is divided above the 2 nd & below the 3 rd ganglion 26
DIVISION OF THE RAMI TO THE 2 ND & 3 RD GANGLIA �The trunk is divided below the 3 rd ganglion & the rami of 2 nd & 3 rd ganglia are sectioned
Operative technique SUPRACLAVICULAR APPROACH: � A horizontal skin incision is made a finger breadth above the medial half of the clavicle � The platysma & external jugular veins are divided & atleast the lateral 2 supraclavicular cutaneous nerves are preserved � The clavicular head of the sternomastoid & inferior belly of the omohyoid is divided � The phrenic nerve is identified lying deep to the fascia of the scalenus anterior
contd � The nerve & internal jugular vein are displaced medially & the muscle is divided � The lower margin of the brachial plexus is identified & the subclavian artery is exposed & retracted downwards � The sibsons fascia is divided. � The parietal pleura is then peeled off the vertebral column & the posterior portions of the ribs to the level of the 4 th rib. � The sympathetic trunk is identified by palpation as a thick cord with nodular arrangements of ganglia along its length
TRANSAXILLARY � Patient in lateral position, upper arm raised � 15 cm incision made between anterior & posterior axillary folds along the line of the 3 rd rib � Pectoralis major & latissimus dorsi retracted, nerve to serratus anterior & latissimus dorsi protected � The lung is retracted downwards � The sympathetic trunk can be seen where it lies deep to mediastinal pleura which is incised
ANTERIOR THORACOTOMY � Incision overlies 3 rd interspace � Extends from lateral margin of the sternum to mid axillary line � Pectoralis major is incised in the line of the fibres � Chest is opened through an incision in 3 rd intercostal space � The lung is retracted downwards & sympathetic trunk is identified
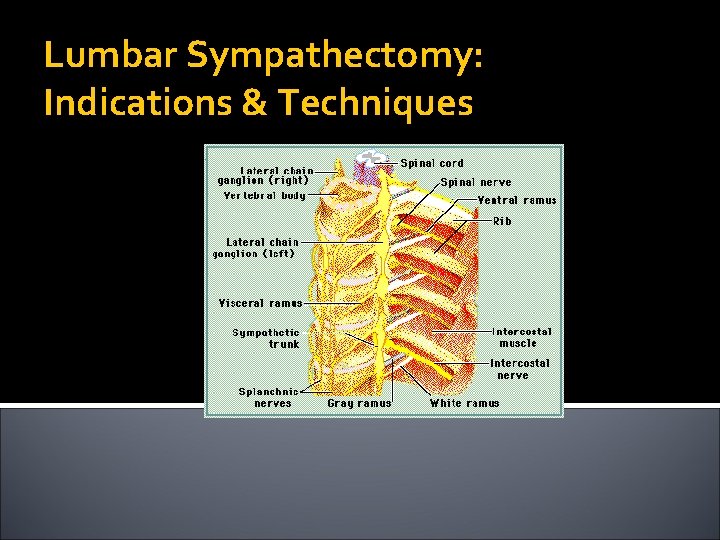
Lumbar Sympathectomy: Indications & Techniques
Overview �History �Anatomy �Physiology �Clinical Findings �Techniques of Blocks �Clinical Indications �Operative Technique
History � Concept of sympathetic denervation to treat occlusive arterial disease Jaboulay (1889): periarterial sympathectomy on femoral artery Leriche (1921): results disappointing due to reinnervation and vasospasm within weeks of operation Royle (1924): observed after lumbar sympathectomy that skin and toes of ipsilateral foot became warm and dry � 1930 s-1950 s: widely used for occlusive arterial disease because it was often the only alternative to amputation Experience proved to provide only short-term palliation � 1960 s: direct surgical revascularization supplanted sympathectomy
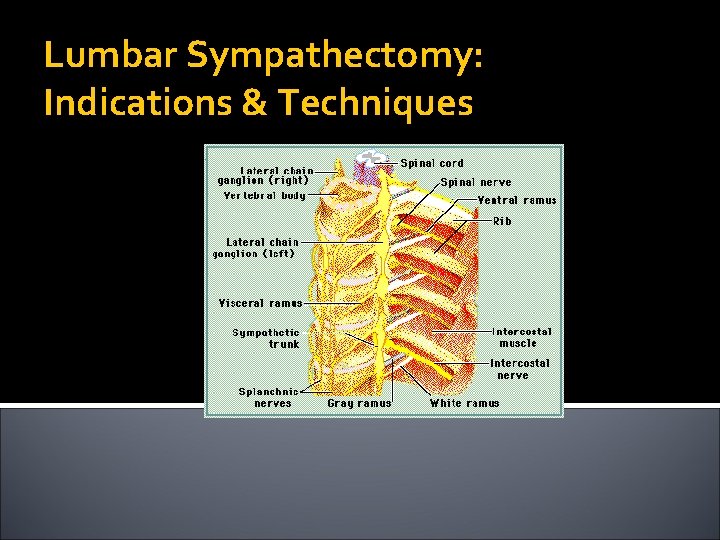
Anatomy �THE LUMBAR SYMPATHETIC TRUNK ü There is a lumbar sympathetic trunk on each side & lies retroperitoneally. ü Lies on the anterolateral surface of the bodies of the lumbar vertebrae along the medial margin of the psoas major muscle. ü On the right side the trunk is overlapped by inferior venecava & on the left side by aorta ü There are usually 4 ganglia on each side
�BRANCHES Ø Splanchnic nerves pass from the ganglia to join the coeliac, intermesentric & superior hypogastric plexus Ø Grey rami communicantes from all ganglia to lumbar spinal nerves
THE HYPOGASTRIC PLEXUS �The nerves from these plexuses run to the abdominal viscera via blood vessels �The superior hypogastric plexus lies in front of the sacral promontory �The plexus divides into 2 nerves which run down on either side of the rectum to form inferior hypogastric plexus behind the base of the bladder
Anatomy: Efferent Pathway
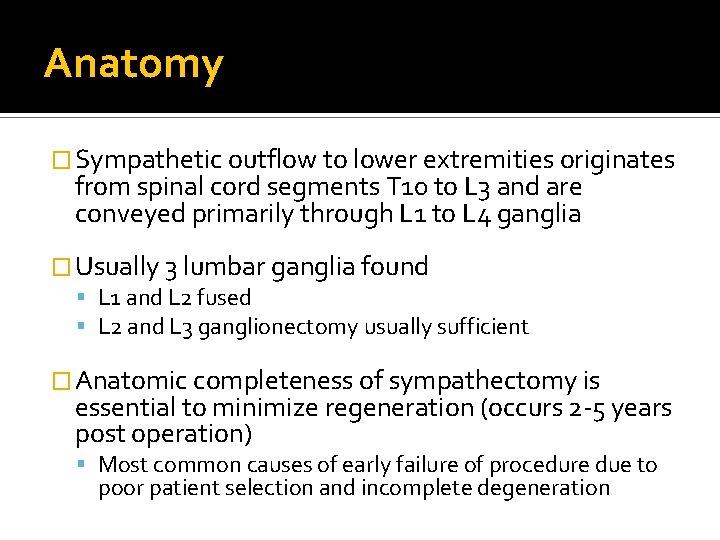
Anatomy � Sympathetic outflow to lower extremities originates from spinal cord segments T 10 to L 3 and are conveyed primarily through L 1 to L 4 ganglia � Usually 3 lumbar ganglia found L 1 and L 2 fused L 2 and L 3 ganglionectomy usually sufficient � Anatomic completeness of sympathectomy is essential to minimize regeneration (occurs 2 -5 years post operation) Most common causes of early failure of procedure due to poor patient selection and incomplete degeneration
Physiology Sympathetic denervation increases blood flow to a normal limb � Impact on an extremity affected by arterial occlusive disease less clear � 1. Increase in blood flow 2. Effect of collateral circulation 3. Nutritive value of blood flow increase 4. Alteration of pain impulse transmission
Physiology 1. Increase in Blood Flow � Abolishing basal and reflex constriction of arterioles and precapillary sphincters Flow increases of 10 -200% are observed ▪ Depends on degree of occlusive disease ▪ Severe, multilevel occlusions may derive no benefit due to already being maximally dilated at rest Alters distribution of blood flow by shunting through cutaneous arteriovenous anastomoses ▪ Maximized by distributing to distal cutaneous circulation ▪ Leads to characteristic warm, pink foot ▪ Not necessarily an increase in tissue perfusion ▪ Canine model (Rutherford ’ 71, Cronenwett ‘ 80) showed neither resting or exertional muscle perfusion improved by sympathectomy ▪ Explains why sympathectomy not useful for claudication
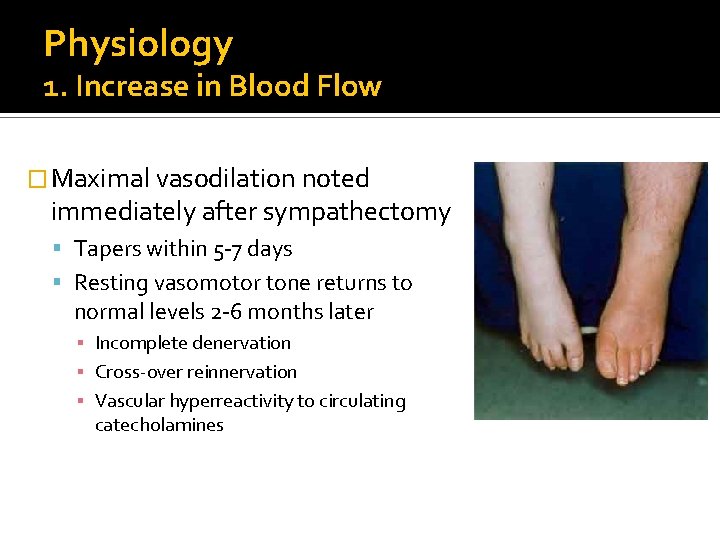
Physiology 1. Increase in Blood Flow � Maximal vasodilation noted immediately after sympathectomy Tapers within 5 -7 days Resting vasomotor tone returns to normal levels 2 -6 months later ▪ Incomplete denervation ▪ Cross-over reinnervation ▪ Vascular hyperreactivity to circulating catecholamines
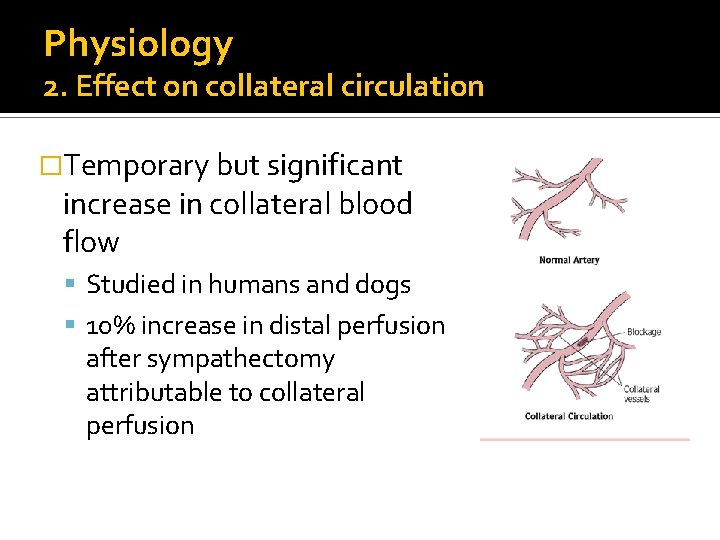
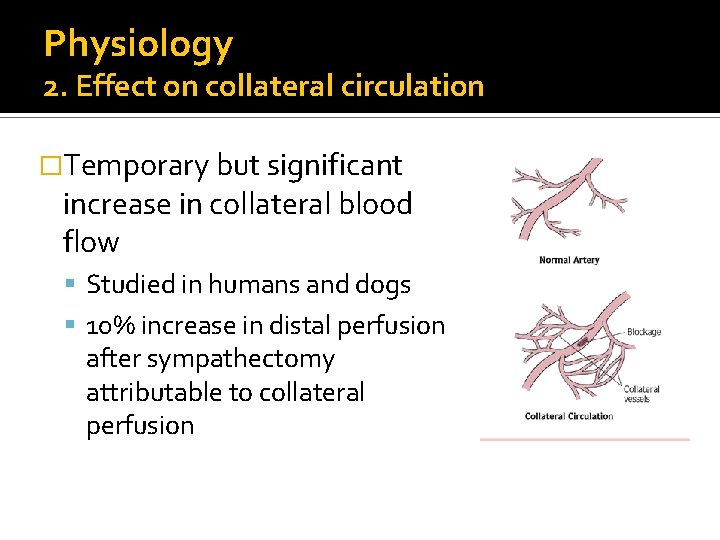
Physiology 2. Effect on collateral circulation �Temporary but significant increase in collateral blood flow Studied in humans and dogs 10% increase in distal perfusion after sympathectomy attributable to collateral perfusion
Physiology 3. Nutritive value of blood flow increase �Shunting through cutaneous arteriovenous anastomoses bypasses capillary perfusion Presumably makes blood non-nutritive Conflicting studies regarding clearance of radio- labeled isotopes �Uncontrolled clinical series (Moore ’ 71) reported ischemic ulcer healing in 40 -67% of patients after sympathectomy
Physiology 4. Alteration of pain impulse transmission �Relief of ischemic rest pain due to loss of attenuation of painful stimulus transmission �Relationship between lumbar sympathectomy and pain threshold Sympathectomy decreases noxious stimulus by decreasing tissue norepi levels Explains why in clinical series that rest pain improves without hemodynamic evidence of improved tissue perfusion
Clinical Findings � Lumbar sympathetic block Significant increase in warmth (subjective or objective) Increased filling of veins Increase in arterial pulsations shown by oscillometry or plethysmography Abolished secretion of sweat � Noninvasive Lab ABI<0. 3 indicates low likelihood to improve after sympathectomy (Yao ’ 73) Presence of sympathetic vasomotor tone assessed by noting response of digit pulse amplitude to deep breath ▪ Loss of vasoconstrictive reflex in DM, surgical sympathectomy, or advanced ischemia Ability of digit circulation to increase pulse amplitude by inducing temporary ischemia using pneumatic cuff
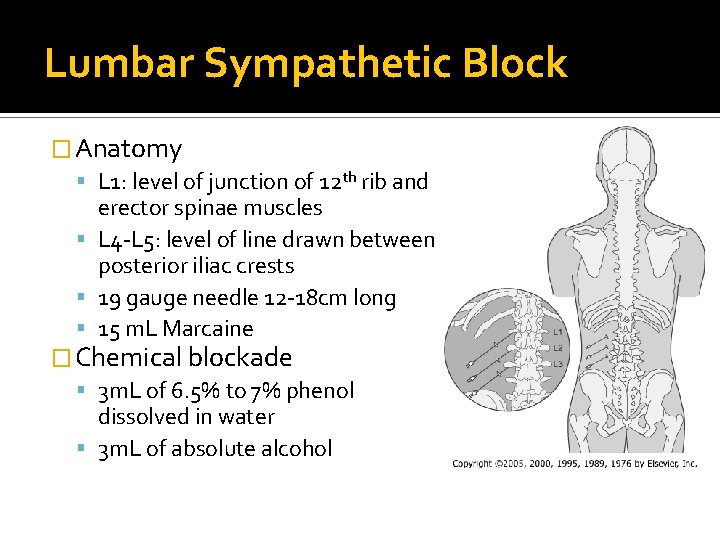
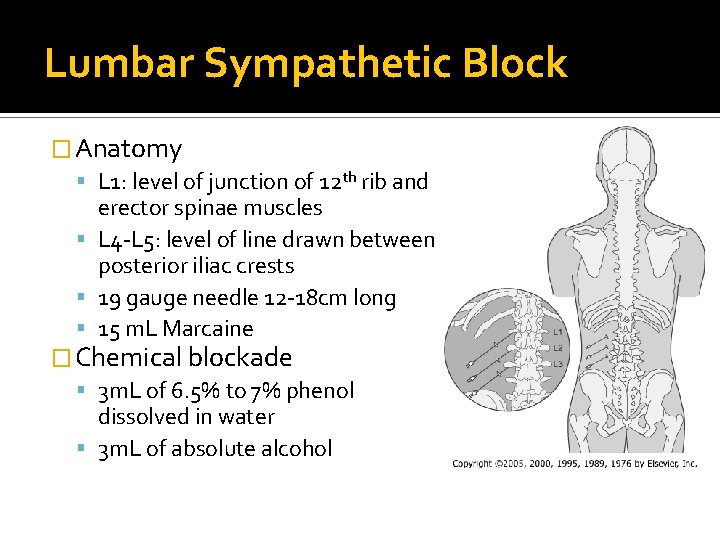
Lumbar Sympathetic Block � Anatomy L 1: level of junction of 12 th rib and erector spinae muscles L 4 -L 5: level of line drawn between posterior iliac crests 19 gauge needle 12 -18 cm long 15 m. L Marcaine � Chemical blockade 3 m. L of 6. 5% to 7% phenol dissolved in water 3 m. L of absolute alcohol
Clinical Indications � Review of the history of clinical papers regarding lumbar sympathectomy (Cross ’ 99) Sympathectomy does not improve claudication May improve ischemic rest pain Does not improve long-term patency of peripheral vascular bypass grafts � Subjective and objective preoperative assessment of response to sympathetic blockade greatly enhances probability of therapeutic success � Three main indications Causalgia Inoperative arterial occlusive disease with limb-threatening ischemia causing rest pain, limited ulceration, or superficial digital gangrene Symptomatic vasospastic disorders
Causalgia � Stage I-Acute (warmth, erythema, burning, edema) 40 -60% respond to intensive medical therapy including mild analgesics, physiotherapy, TCAs, anticonvulsants, adrenergic blockers Surgical sympathectomy considered after 3 months Translumbar sympathetic blocks can be used � Stage 2 -Dystrophic (coolness, mottling, cyanosis Sympathectomy should be applied as soon as there is relief from blockade � Stage 3 -Atrophic Not indicated
Inoperable Arterial Occlusive Disease � Lumbar sympathectomy can be considered prior to amputation ABI>0. 3 Absent neuropathy Symptomatic relief obtained by trial block � Relief of rest pain expected in 50 -85% of patients meeting these criteria � For tissue loss patients, need to limit treatment to patients who only have limited ulceration or singledigit gangrene and absence of major deep infection Healing seen in 35 -65% of patients
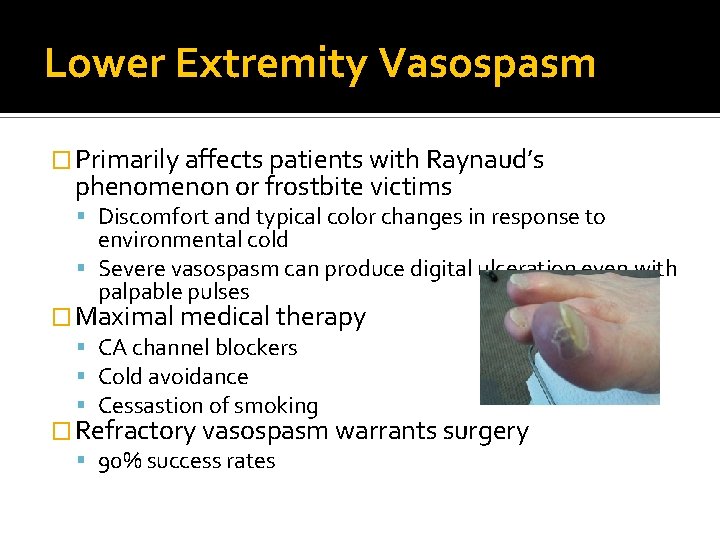
Lower Extremity Vasospasm � Primarily affects patients with Raynaud’s phenomenon or frostbite victims Discomfort and typical color changes in response to environmental cold Severe vasospasm can produce digital ulceration even with palpable pulses � Maximal medical therapy CA channel blockers Cold avoidance Cessastion of smoking � Refractory vasospasm warrants surgery 90% success rates
Operative Technique � Retroperitoneal positioning on table on bean bag � Oblique incision from lateral edge of rectus towards middle of space between ribs and iliac crest ending at anterior axillary line � Lumbar sympathetic chain located medial to psoas muscle overlying transverse processes of lumbar spine Left: adjacent and lateral to aorta Right: beneath edge of IVC Tactile identification by plucking the chain causes a “snap” (genitofemoral nerve nearby is less taut) Clips placed proximal and distal to proposed sites of transection ▪ Send specimen to pathology to confirm sympathetic fibers
Complications � Major complications result from failure to appreciate normal anatomic relationships � Most common complication is postsympathectomy neuralgia 50% of patients 5 -20 days post operation Annoying “ache” in anterolateral thigh worse at night unaffected by activity Responds to analgesics and spontaneously resolves 8 -12 weeks � Sexual problems 25 -50% of patients undergoing bilateral surgery � 2 nd most common complication is failure to achieve desired objectives of pain relief or tissue healing
Summary � Sympathectomy increases peripheral blood flow by vasodilation of arterioles in cutaneous vascular beds � Some patients may receive sufficient increases to help heal superficial ischemic ulcers and relieve rest pain � Blood flow effects are comparatively small in the long run � Protection against an exaggerated vasoconstrictor response to cold, improvement against sympathetic pain, and suppression of sweating are long-lasting results