Autonomic Nervous System ANS Nervous System n n


- Slides: 119
Autonomic Nervous System (ANS)
Nervous System n n Central NS - Brain - Spinal cord Peripheral NS - Somatic NS - Sympathetic (adrenergic)=Thoracolumbar - Parasympathetic (Cholinergic)=Craniosacral (III, IV, IX, X=Vagus)
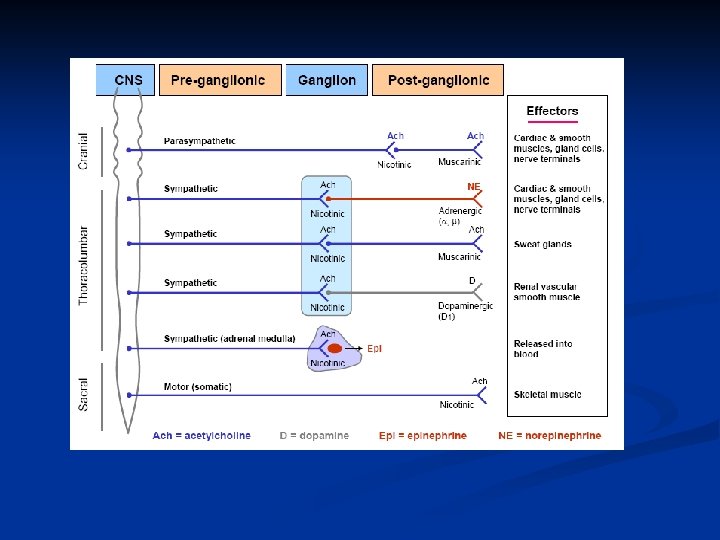
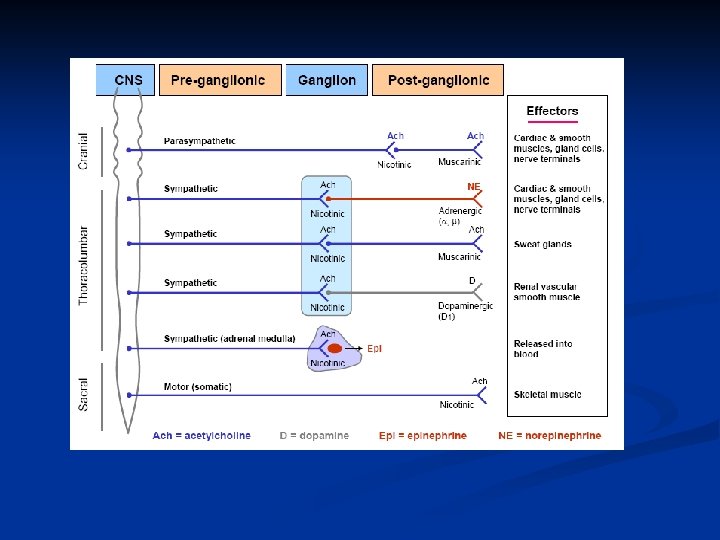
n n Pre-synaptic neuron: Where a neurotransmitter is synthesized, stored and released upon cell activation Post-synaptic neuron or effector cells: Where neurotransmitter is detected and its action translated into cellular activities Synapse: A junctional connection across which a signal can pass Ganglionic transmission is cholinergic and could be blocked by ganglionic blockers
n Sympathetic nervous system has the property of adjusting the response to stressful situation, such as trauma, fear, clod, exercise (Fight or flight response) n Stimulating this system results in an increase heart rate and blood pressure, mobilize energy stores of the body, increase blood flow to skeletal muscles and the heart and dilates pupils and bronchi n The parasympathetic nervous system maintains essential bodily functions, such as digestive processes and elimination of wastes (feed and breed response) n It usually acts opposite or in balance with the sympathetic division, and generally dominates in the rest situation
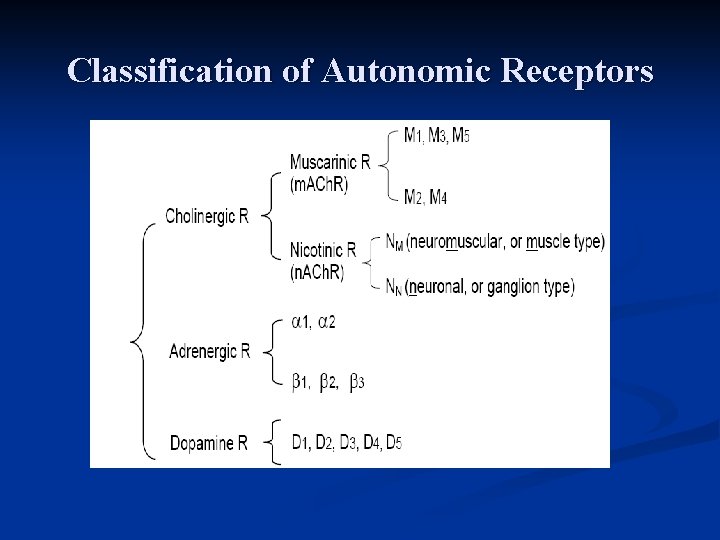
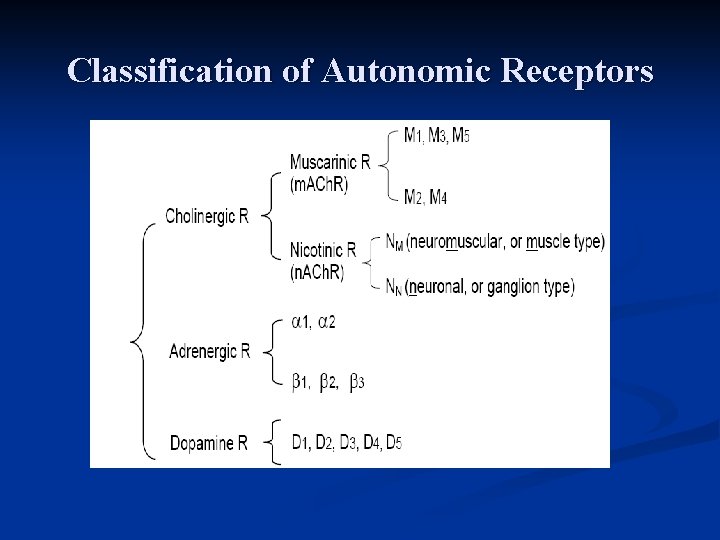
Classification of Autonomic Receptors
Sympathetic receptors (responses): n α 1 -receptors (NE=NA; E=A; …agonists) Mediate: - Vasoconstriction of cutaneous; visceral; pulmonary; coronary arteries and arterioles and veins - Dilatation of pupils (mydriasis) ** α 1 -receptor antagonists (blockers) Phentolamine; Prazocin… n α 2 - receptors (Clonidine…agonist) Presynaptic and inhibitory in nature n
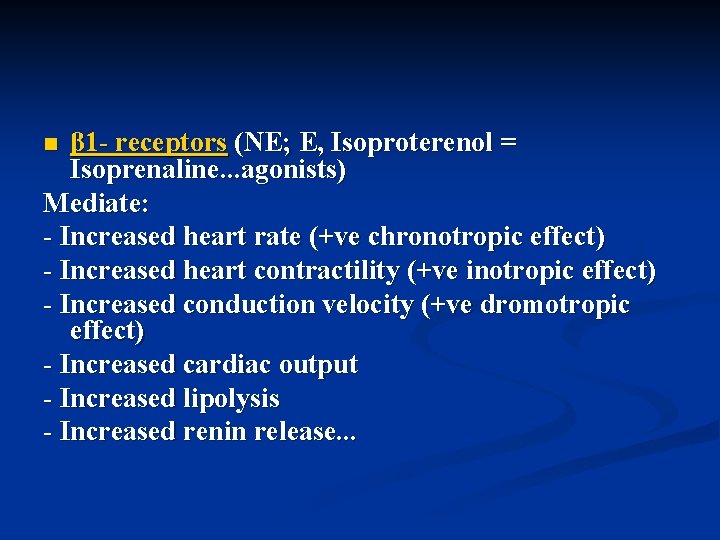
β 1 - receptors (NE; E, Isoproterenol = Isoprenaline. . . agonists) Mediate: - Increased heart rate (+ve chronotropic effect) - Increased heart contractility (+ve inotropic effect) - Increased conduction velocity (+ve dromotropic effect) - Increased cardiac output - Increased lipolysis - Increased renin release. . . n
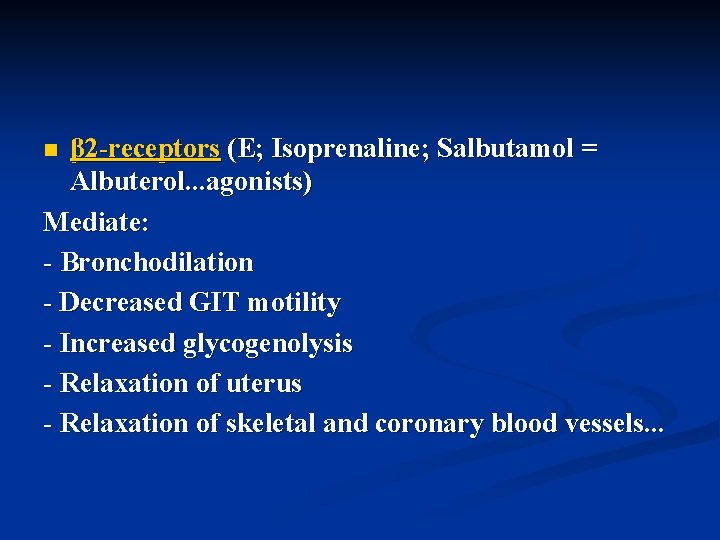
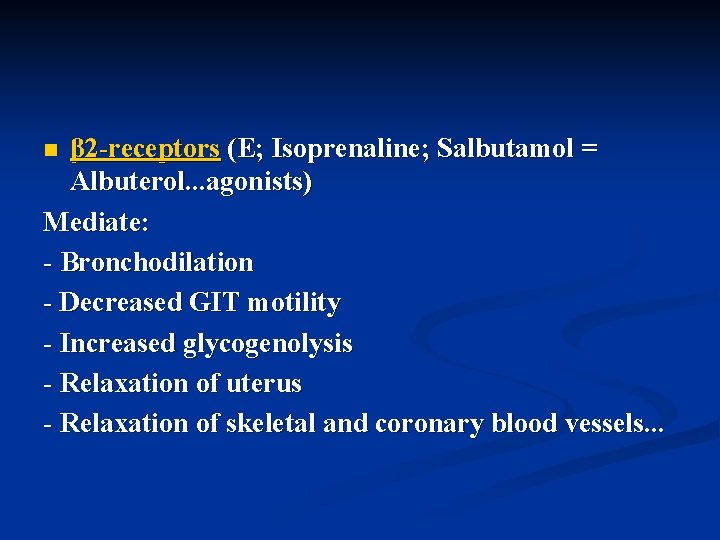
β 2 -receptors (E; Isoprenaline; Salbutamol = Albuterol. . . agonists) Mediate: - Bronchodilation - Decreased GIT motility - Increased glycogenolysis - Relaxation of uterus - Relaxation of skeletal and coronary blood vessels. . . n
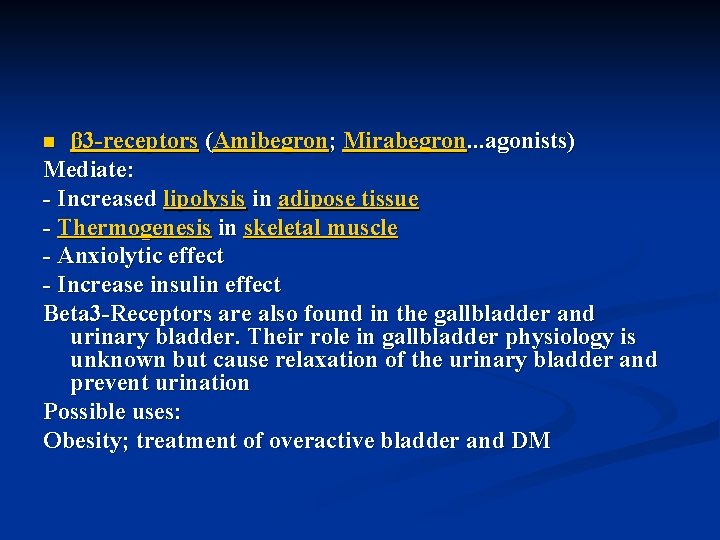
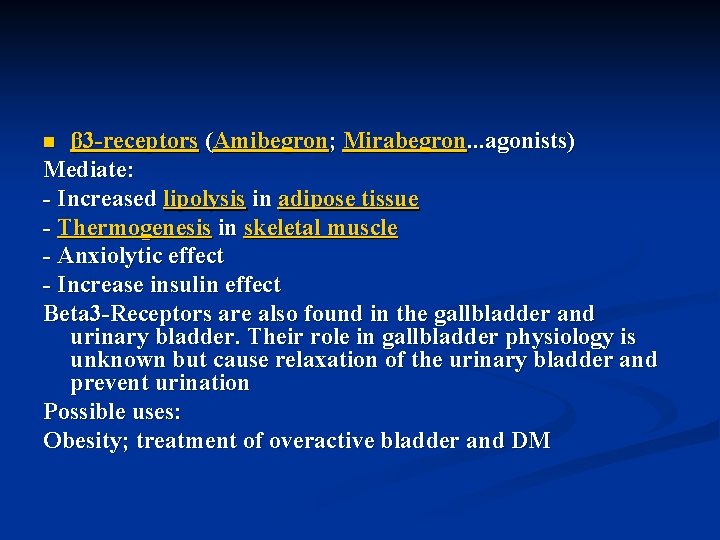
β 3 -receptors (Amibegron; Mirabegron. . . agonists) Mediate: - Increased lipolysis in adipose tissue - Thermogenesis in skeletal muscle - Anxiolytic effect - Increase insulin effect Beta 3 -Receptors are also found in the gallbladder and urinary bladder. Their role in gallbladder physiology is unknown but cause relaxation of the urinary bladder and prevent urination Possible uses: Obesity; treatment of overactive bladder and DM n
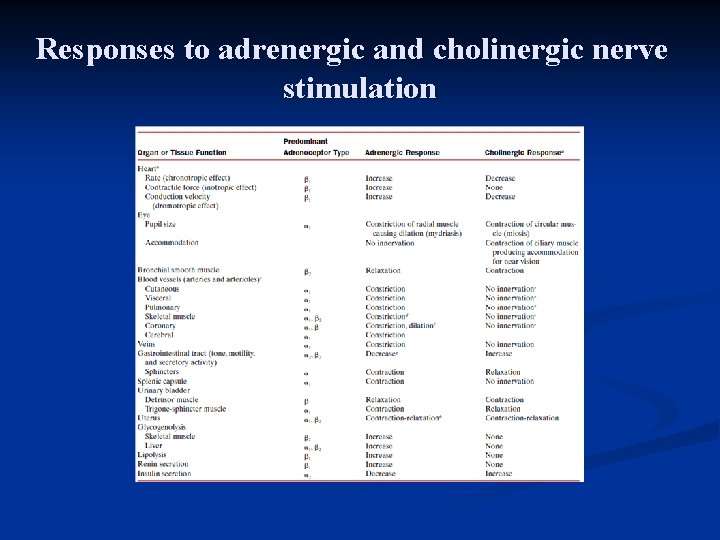
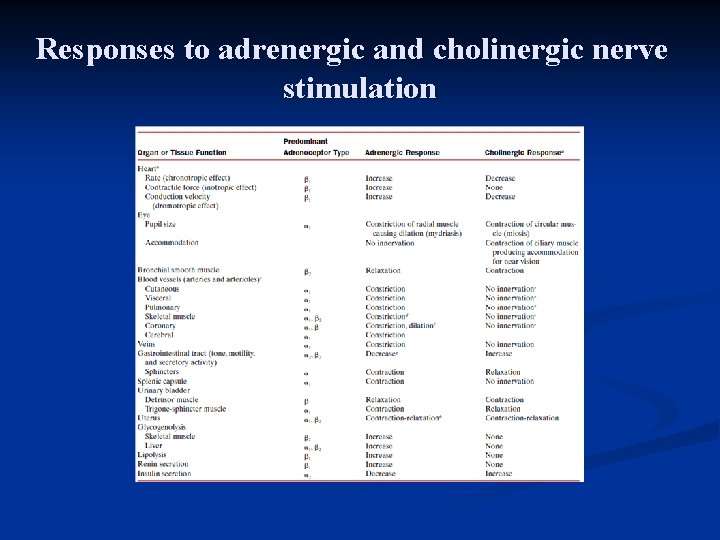
Responses to adrenergic and cholinergic nerve stimulation
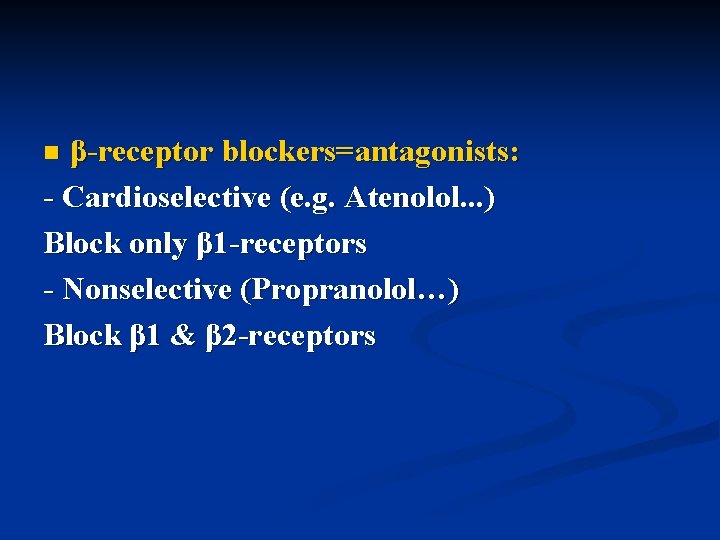
β-receptor blockers=antagonists: - Cardioselective (e. g. Atenolol. . . ) Block only β 1 -receptors - Nonselective (Propranolol…) Block β 1 & β 2 -receptors n
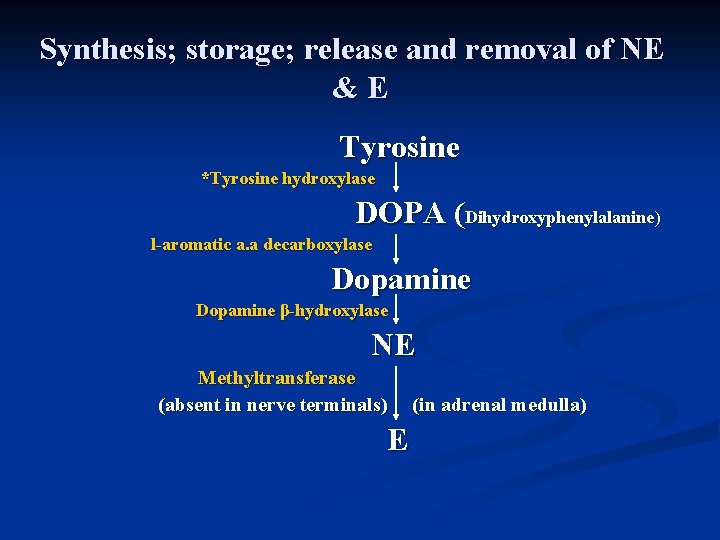
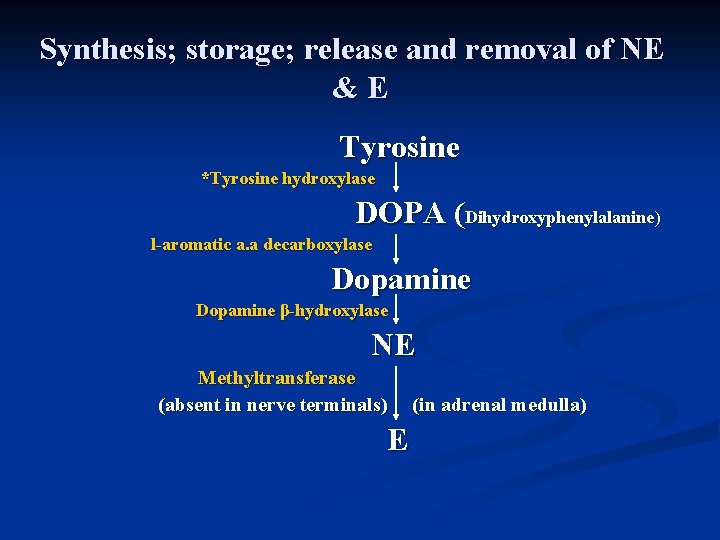
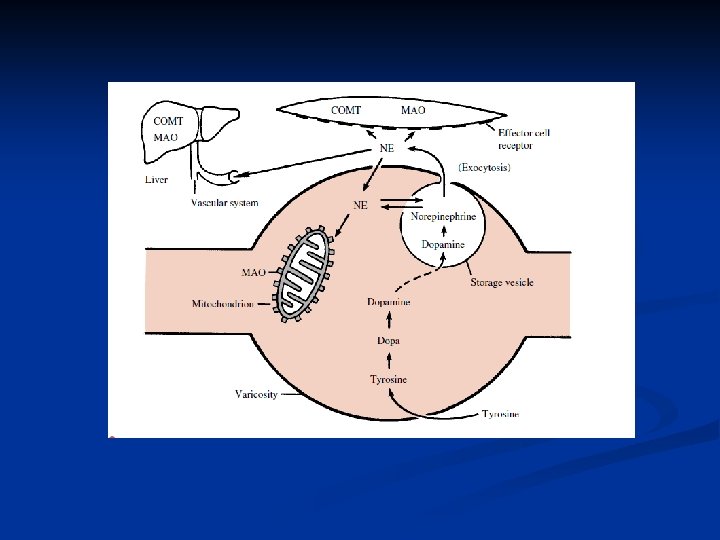
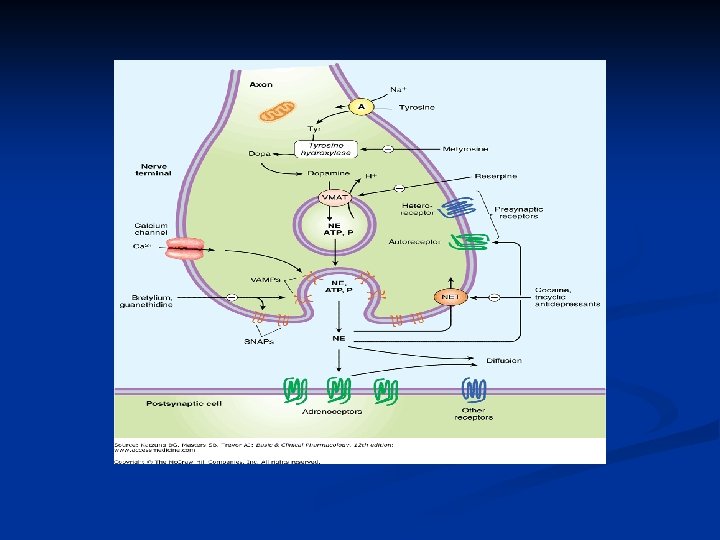
Synthesis; storage; release and removal of NE &E Tyrosine *Tyrosine hydroxylase DOPA (Dihydroxyphenylalanine) l-aromatic a. a decarboxylase Dopamine β-hydroxylase NE Methyltransferase (absent in nerve terminals) E (in adrenal medulla)
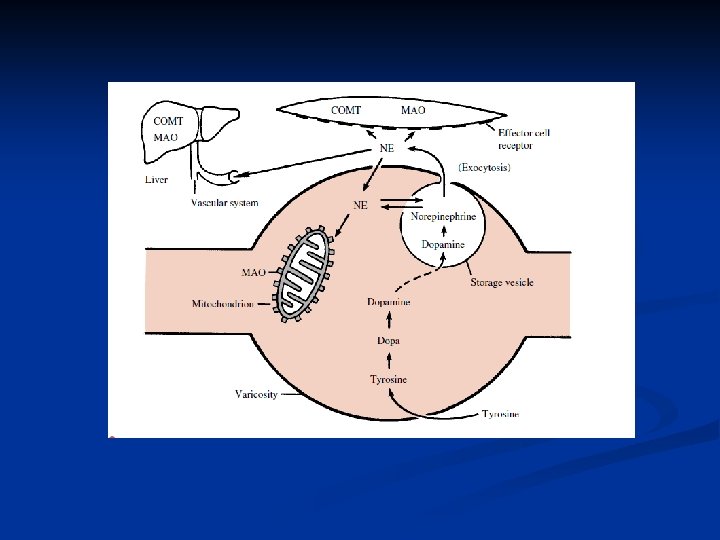
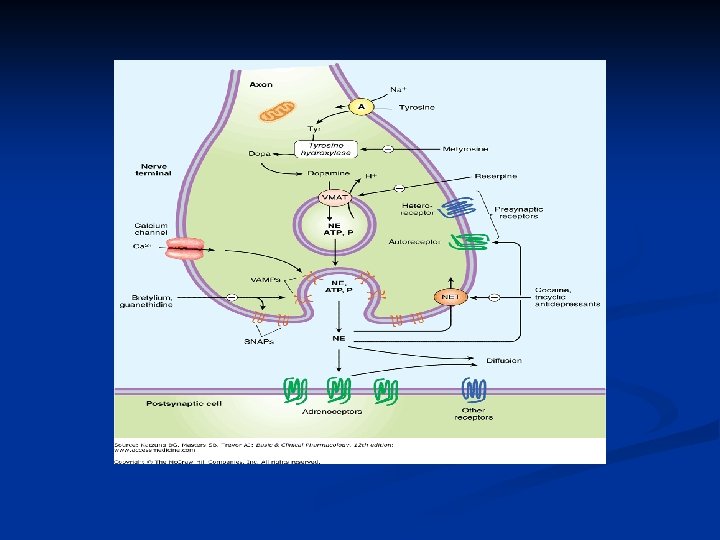
Adrenal medulla contains more E n Adrenergic neurons synthesize only NE n * Tyrosine hydroxylase step is the rate limiting one n Major inactivation of most neurotransmitters is by a high specific reuptake mechanism n TCA’s & Cocaine block NE & E reuptake n
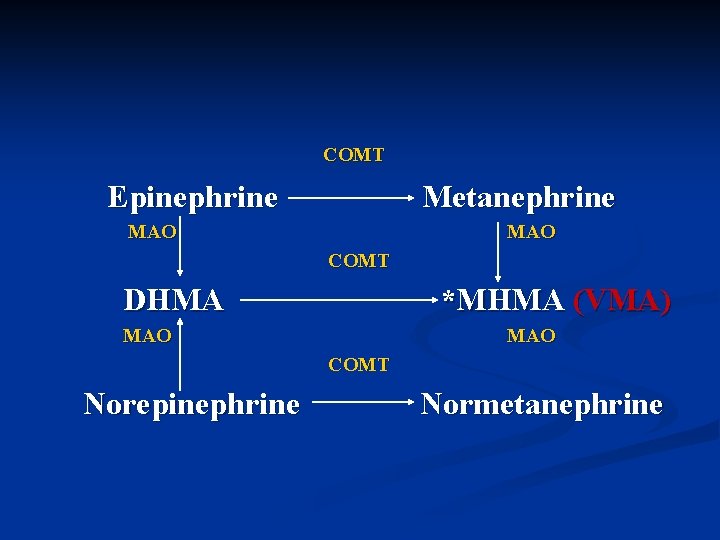
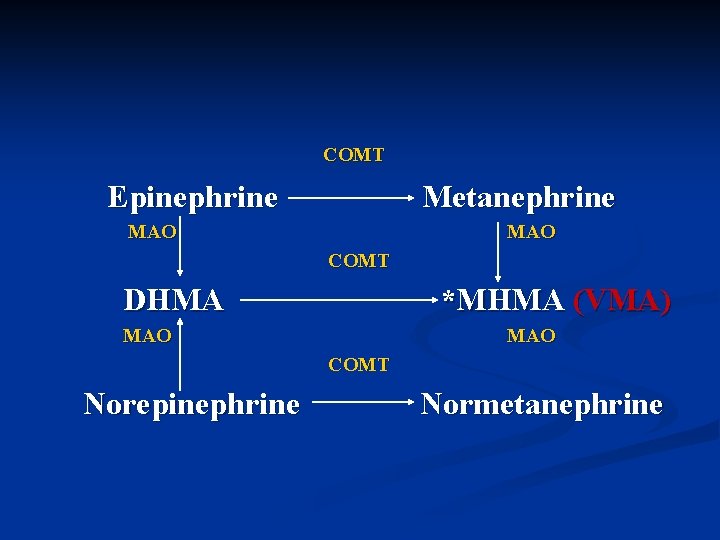
COMT Epinephrine Metanephrine MAO COMT DHMA *MHMA (VMA) MAO COMT Norepinephrine Normetanephrine
Metabolism of NE &E
Vanillylmandelic acid = VMA A major metabolite to both NE & E, excreted in urine (good indicator of the adrenal medulla tumor pheochromocytoma) n Little NE & E are excreted unchanged in urine n
COMT= Catechol-O-methyltransferase Present in liver and peripheral tissues n MAO= Monoamine oxidase Present in liver; peripheral tissues and neuronal mitochondria MAO-A. . . Metabolizes NE & E MAO-B. . . Specific for Dopamine (present in brain) n
Sympathomimetic (adrenomimetic) agents Directly acting: -Norepinephrine=Noradrenaline (NE; NAD) - Epinehrine=Adrenaline (E; AD) - Isoproterenol (Isoprenaline) - Dopamine - Dobutamine - Salbutamol (Albuterol); Terbutaline; Perbuterol - Phenylephrine; Metaraminol; Methoxamine n Indirectly acting: - Ephedrine - Amphetamine n
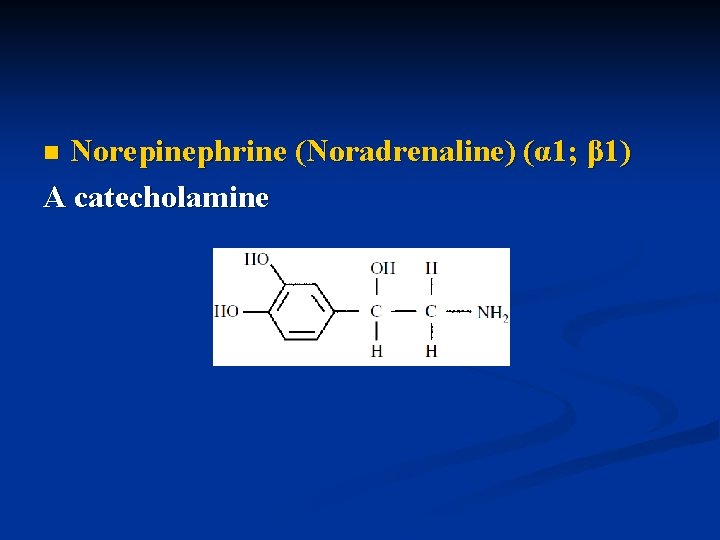
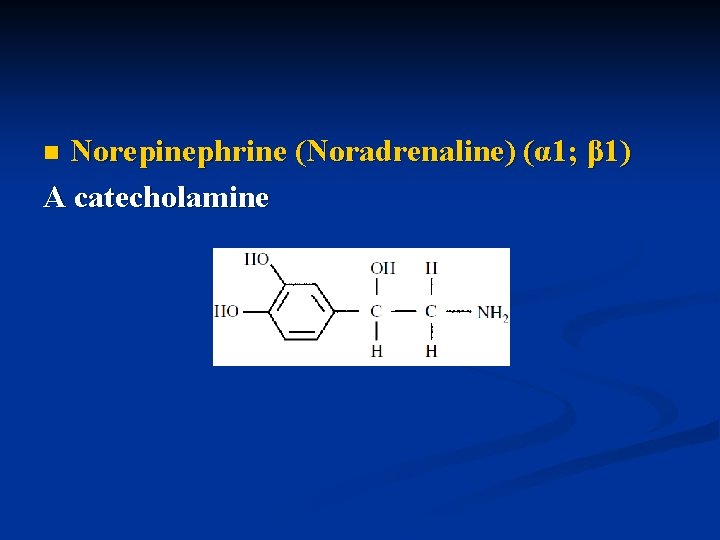
Norepinephrine (Noradrenaline) (α 1; β 1) A catecholamine n
NE actions: - Its prominent effect is a widespread vasoconstriction of both arterioles and veins leading to significant increase in total peripheral resistance and an increase in BP - Leads to bradycardia (because direct effect of NE on heart rate is masked by over activity of parasympathetic system on the heart and unmasked by Atropine) n
MOA of catecholamines: Through a second messenger - β-receptors: c. AMP Catecholamine → β-receptors → G-protein → adenylate cyclase n ATP → c. AMP → activation of specific kinases that mediate phosphorylation of many proteins → opening of Ca++ channels and activation of other enzymes leading to the final physiological or pharmacological responses c. AMP is degraded by phosphodiesterase enzyme

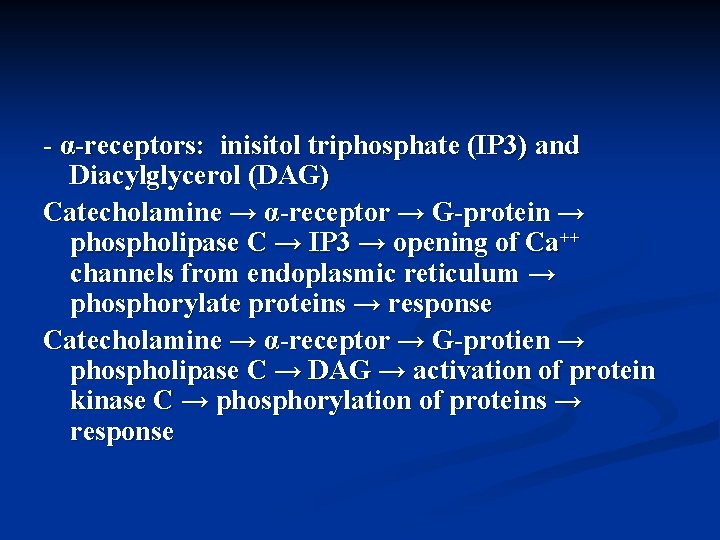
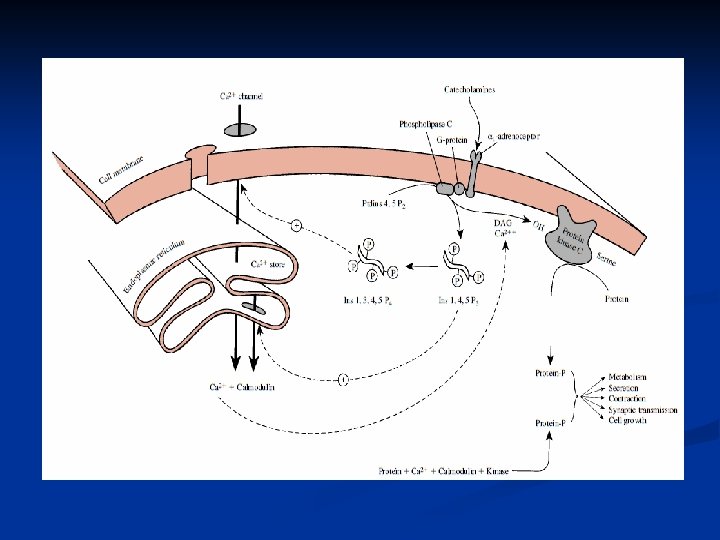
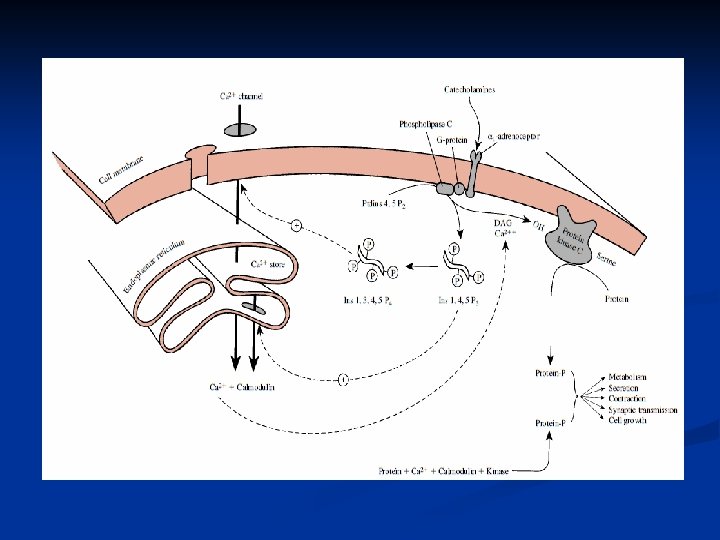
- α-receptors: inisitol triphosphate (IP 3) and Diacylglycerol (DAG) Catecholamine → α-receptor → G-protein → phospholipase C → IP 3 → opening of Ca++ channels from endoplasmic reticulum → phosphorylate proteins → response Catecholamine → α-receptor → G-protien → phospholipase C → DAG → activation of protein kinase C → phosphorylation of proteins → response
Clinical uses to NE: - Shock and severe drop in BP - + local anaesthetics Could be given SC and IV infusion n Side effects to NE: - Headache; tremors; ↑BP - ↑ or ↓ in heart rate (↓ more likely) - Palpitations and cardiac arrhythmias (overdose) n
Epinephrine (Adrenaline)(α 1 α 2 ; β 1 β 2) Effects: - ↑ heart rate and contractility and ↑ CO - ↑ systolic BP - Bronchodilatation - ↑ blood sugar - ↓ GIT motility - Dilatation of pupils - ↓ salivary secretions n
Epinephrine clinical uses: - Anaphylactic shock - Open angle glaucoma (↑ drainage of eye fluid) - + local anaesthetic E is ineffective orally; given SC or IM IV→ administration is contraindicated → fatal ventricular fibrillation Metabolized by MAO & COMT n
Epinephrine side effects: Manifestations of sympathetic over activity - Anxiety - Nervousness - Sweating - Headache - Palpitations - Cardiac arrhythmias - ↑BP n
Isoprenaline (Isoproterenol) - A catecholamine; β 1 & β 2 stimulant - ↑ heart rate; contractility and CO - A good bronchodilator - ↓ in peripheral resistance (due to predominant dilating effect on skeletal muscle B. V’s and no α effect) - No change or little ↑ in BP (due to ↑ in CO) n Clinical uses: - Bronchial asthma given by inhalation - Shock & cardiac arrest given by an IV infusion n
Dopamine A catecholamine; precursor to NE Present in adrenergic neurons, adrenal medulla and dopaminergic neurons and in the CNS (neurotransmitter; and hormone); so it produces unique cardiovascular effects through: - ↑ release of NE - Interacting with α and β 1 -receptors - Interacting with specific dopaminergic receptors n
Dopamine pharmacological actions (dosedependent): - Low doses (2 -3 μg/Kg/min) dopamine acts as a vasodilator increasing renal and splanchnic (mesenteric) blood flow, keeps the kidney perfused and leads to natriuresis and diuresis(D 1 & D 2 receptors) - Intermediate doses (4 -8 μg/Kg/min) it stimulates β 1 receptors → ↑ heart rate and contractility - Large doses (more than 10 μg/Kg/min) it activates α 1 -receptors → ↑BP n
Dopamine is considered the best inotropic agent in the management of shock states ± NE and it is given in an IV infusion n Dopamine side effects: Tachyarrhythmias → IHD n Effects of dopamine on: - α-receptors are blocked by α-blockers - β-receptors are blocked by β-blockers - D-receptors are blocked by dopamine antagonists n
Terbutaline & Salbutamol (Albuterol) & Perbuterol - Selective β 2 agonists - Good bronchodilators - Have long DOA (not metabolized by MAO or COMT) - Salbutamol (Albuterol) is the most widely used one in the management of bronchial asthma and bronchospasm associated with bronchitis - Given orally, by inhalation and SC n
Salbutamol side effects: - Palpitations - Tachycardia - Sweating - Tremors - Headache - Nausea & vomiting n
Phenylephrine; Metaraminol; Methoxamine - Directly acting adrenomimetic agents - Good α 1 stimulants (have little effect on heart) - Increase systolic and diastolic BP - Used in cases of hypotensive states, especially hypotension associated with spinal anaesthesia and given IV - Phenylephrine is also used as a nasal decongestant and mydriatic in ophthalmology - Could be used with L. A’s as vasoconstrictors - Major side effect: Hypertensive crises n
Indirectly-acting sympathomimetic agents: - Ephedrine An alkaloid with marked CNS stimulant effect Its peripheral actions are mainly due to ↑ NE release Has little direct effects on adrenergic receptors particularly β 2 Unlike NE, it is not metabolized by MAO or COMT so it has longer DOA and it is effective orally n
Ephedrine (Cont. ) - ↑ systolic and diastolic BP - ↑ heart contractility and CO - Leads to bronchodilatation - Dilates pupils n Ephedrine clinical uses: - Bronchoconstriction of bronchitis and bronchial asthma - Nasal decongestant - Mydriatic
Ephedrine (Cont. ) n Ephedrine side effects: - Tachycardia - Nervousness - Insomnia Ephedrine is contraindicated in patients with hypertension, hyperthyroidism and patients with heart disease
Amphetamine - Has marked CNS stimulant effect > Ephedrine (disomer more potent than l-isomer) - ↑ NE release - ↑ BP - ↑ alertness & thinking, ↑ activity, ↓ Fatigue - Leads to addiction - May be used in the management of severe narcolepsy (frequent sleep) and hyperkinetic syndrome n
Adrenergic Blockers=Antagonists
Sympatholytic Agents 1. β-adrenergic blockers (antagonists) Their use (alone or with other antihypertensives e. g. diuretics) proved to ↓ incidence of stroke, MI and CHF Previously considered 1 st line Rx for HTN Recently diuretics are considered 1 st line Rx and β-blockers could be added for proper ↓ in BP if required
Still β-blockers are considered 1 st line therapy in patients with hypertension and have certain compelling indications e. g. : Pts with high coronary risk or post myocardial infarction. . .
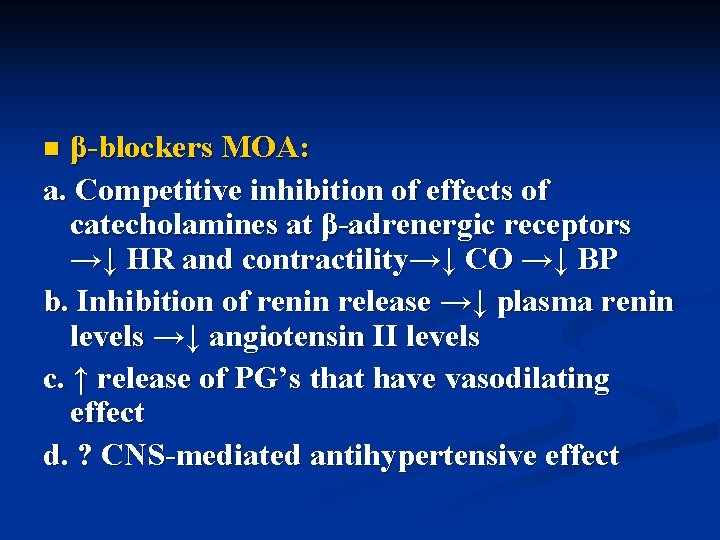
β-blockers MOA: a. Competitive inhibition of effects of catecholamines at β-adrenergic receptors →↓ HR and contractility→↓ CO →↓ BP b. Inhibition of renin release →↓ plasma renin levels →↓ angiotensin II levels c. ↑ release of PG’s that have vasodilating effect d. ? CNS-mediated antihypertensive effect n
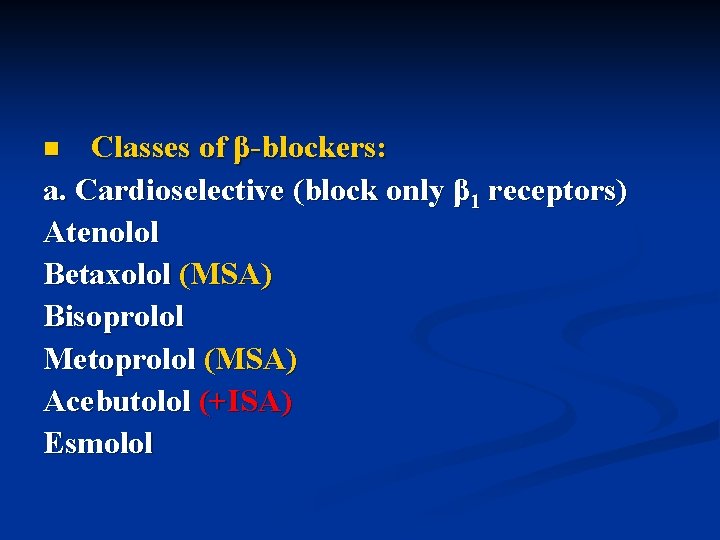
Classes of β-blockers: a. Cardioselective (block only β 1 receptors) Atenolol Betaxolol (MSA) Bisoprolol Metoprolol (MSA) Acebutolol (+ISA) Esmolol n
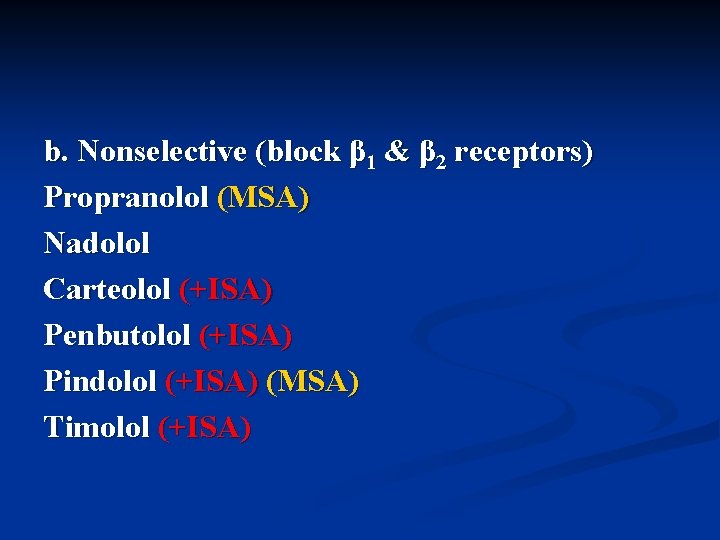
b. Nonselective (block β 1 & β 2 receptors) Propranolol (MSA) Nadolol Carteolol (+ISA) Penbutolol (+ISA) Pindolol (+ISA) (MSA) Timolol (+ISA)
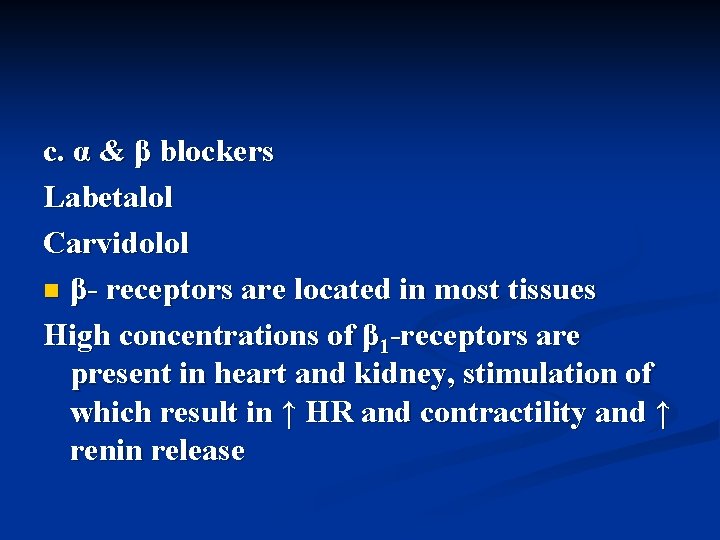
c. α & β blockers Labetalol Carvidolol n β- receptors are located in most tissues High concentrations of β 1 -receptors are present in heart and kidney, stimulation of which result in ↑ HR and contractility and ↑ renin release
High concentrations of β 2 -receptors are present in lungs and vascular smooth muscles, stimulation of which result in bronchodilatation, vasodilatation and ↑ insulin release Cardioselective β-blockers are safer in pts with bronchial asthma, COPD, peripheral arterial disease and diabetes mellitus Large doses of cardioselective β-blockers block β 2 receptors as well (this effect is subject to great individual variation)
ISA (Intrinsic Sympathomimetic Activity) Some β-blockers have ISA (act as partial agonists) which is weak as compared to their β-blocking activity. Such blockers would be advantageous in patients with heart failure and bradycardia β-blockers with ISA are rarely used because they increase risk after MI
MSA (Membrane Stabilizing Activity) β-blockers depress cellular membrane excitability (they have Quinidine-like effect or local anesthetic effect= they have similarity in structure to LA’s) In large doses all β-blockers have this property This property is important when β-blockers are used in the management of cardiac arrhythmias
Pharmacokinetics of β-blockers: - Well absorbed following oral administration Differ in t 1/2 & DOA (long t 1/2 with Atenolol & Nadolol, short with Esmolol) - Protein binding (extensive with Propranolol ≈ 90%, modest with Metoprolol ≈ 10%) - First-pass effect (extensive with Propranolol & Metoprolol) n
- Route of elimination and metabolism Propranolol & Metoprolol undergo extensive hepatic metabolism and metabolites are excreted renally, Atenolol undergoes little metabolism and excreted mainly unchanged by the kidney
Remember that the duration of hypotensive action of β-blockers does not correlate always with their serum t 1/2’s n Some β-blockers are given once daily despite their short t 1/2 e. g. Acebutelol’s t 1/2 ≈ 4 hrs but metabolized to a pharmacologically active metabolites with t 1/2 ≈ 10 hrs n
- Lipid solubility: All β-blockers are lipid soluble Some have high lipid solubility e. g. Propranolol which has the most lipid solubility among β-blockers Others have low lipid solubility e. g. Atenolol which has the least lipid solubility among βblockers
β-blockers with high lipid solubility penetrate well the BBB (this accounts for dizziness & headache side effects) n Lipid solubility has no effect on the antihypertensive activity of β-blockers, but has the benefit of utilizing highly lipid soluble ones in the management of migraine and essential tremors n
β-blockers clinical uses: - HTN - Angina pectoris - Mild to moderate HF Not good for pts with HF with severe ↓ in CO and bradycardia, but good in certain pts with HF who are largely dependent on enhanced sympathetic activity to maintain sufficient CO n
- Cardiac arrhythmias - Prevention of recurrent MI - Hyperthyroidism - Glaucoma (Timolol is particularly effective; it ↓ production of eye fluid) - Anxiety states - Migraine
β-blockers side effects: - High degree of atrioventricular block - Bradycardia - Acute HF - ED - Bronchoconstriction - Raynaud's phenomenon n
- Hypoglycemia ↓ blood glucose + mask manifestations of Hypoglycemia - ↑ serum triglycerides, ↓ HDL More common with nonselective β-blockers Pindolol (has the best ISA among β-blockers), ↑HDL Combined α & β blockers have no effects on blood lipids - Central effects Dizziness, headache, hallucinations, depression…
β-blockers contraindications: - Pts with COPD, bronchial asthma - Pts with severe CHF or LV dysfunction - Allergy to β-blockers (not frequent) - Diabetics on high dose of insulin or with hypoglycemia n
β-blockers should not be stopped abruptly n Sudden withdrawal of β-blockers could lead to unstable angina, ↑BP, MI and even death n Chronic use of β-blockers is usually associated with increased β-receptor density, therefore abrupt withdrawal → acute withdrawal syndrome and life threatening rebound hypertension n
2. α-adrenergic antagonists Chemically classified into: - Haloalkylamines Phenoxybenzamine O, I. V - Imidazolines Phentolamine O, I. V - Quinazoline derivatives Prazosin O Terazosin O Doxazosin O Trimazosin O
n n n Phenoxybenzamine and Phentolamine are nonselective (block α 1 & α 2 receptors), effective orally and IV mainly used in the management of hypertension associated with pheochromocytoma Quinazoline derivatives are selective α 1 -receptor antagonists which replaced nonselective blockers in the management of essential HTN Selective blockers are less efficacious than diuretics, Ca++ channel blockers and ACE inhibitors in reducing primary end points of cardiovascular disease, stroke or HF when used alone in the management of HTN
Thus, α 1 -blockers are considered alternative agents when other 1 st line therapy fails to control HTN and usually used in combination with other antihypertensive drugs n α 1 -blockers MOA: Competitive antagonism to postsynaptic α 1 receptors leading to arterial and venous vasodilatation n
High doses of α 1 -blockers could lead to blockade to α 2 -receptors → ↑ NE release → ↑ β-adrenergic receptors → cardiac stimulation and ↑ renin release (this effect is less prominent with Prazosin) n Also high doses of Prazosin lead to direct vasodilating effect due to inhibition of phosphodiesterase enzyme n
α 1 -blockers clinical uses: - HTN Alone could be effective in mild HTN Moderate to severe HTN, Prazosin + thiazide or β-blocker Prazosin has no effects on uric acid or blood glucose levels (good to pts with gout or diabetes) - Benign hyperplasia of the prostate n
α 1 -blockers side effects: - First-dose phenomenon Severe drop in BP with the 1 st dose more than with subsequent doses - Orthostatic hypotension (postural hypotension), this leads to dizziness, headache, drowsiness and syncope (so it is advised to take these drugs at bedtime) n
Doxazosin is less effective than thiazides in lowering systolic BP and may be associated with a higher risk of cardiovascular disease particularly HF and stroke in pts with HTN n Selective α 1 -blockers ↓ cholesterol and triglycerides blood levels and ↑ HDL levels (so they could improve the negative effects on lipids induced by thiazides or β-blockers) n
3. Agents with mixed properties Labetalol Carvidolol Have α and β antagonistic activity β: α=3: 1 orally β: α=7: 1 IV (thus they are considered β-blockers with some αantagonistic activity) They have 1/10 potency of Phentolamine and 1/3 potency of Propranolol
α and β blockers clinical uses: - HTN - IHD ( Carvidolol has an antioxidant effect) - Hypertensive emergencies (IV Labetalol) The α-receptor antagonistic activity of Labetalol ↓ with chronic administration & disappears in few months n
α and β blockers side effects: - Postural hypotension - Liver damage - Tremors - Lupus like syndrome - +ve ANA (antinuclear antibody test) - Reflex tachycardia n
Parasympathetic System=Cholinergic System Cholinomimetic agents
Acetylcholine (Ach) n Major neurotransmitter at: - Parasympathetic nerve terminals - Sympathetic and parasympathetic ganglia - Motor nerves - Sympathetic terminals to sweat glands - Sympathetic terminals to adrenal
Directly-acting parasympathomimetic (cholinomimetic) agents - Acetylcholine (an ester of choline & acetic acid) Methacholine Carbachol Bethanechol n
Indirectly-acting parasympathomimetic (cholinomimetic) agents Inhibitors of acetylcholinesterase (ACHE) = Anticholinesterases A. Reversible competitive anticholinesterase - Quaternary ammonium agents Edrophonium Ambenonium n
- Carbamates Neostigmine (quaternary amine; positively charged) Pyridostigmine (quaternary amine) Physostigmine (tertiary amine) Quaternary amines are more polar and do not enter the CNS readily Reversible anticholinesterases bind anionic site of ACHE B. Irreversible anticholinesterases Organophosphates (Malethion; Parathion; Sarin) Mainly used as insecticides and bind esteratic site of ACHE
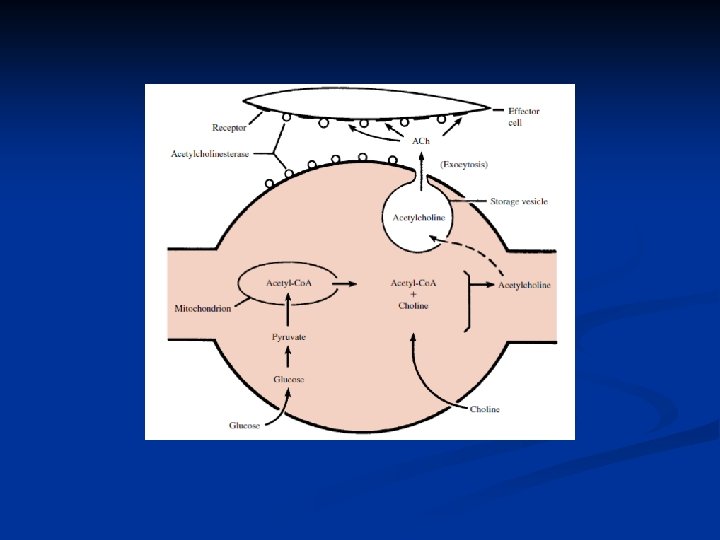
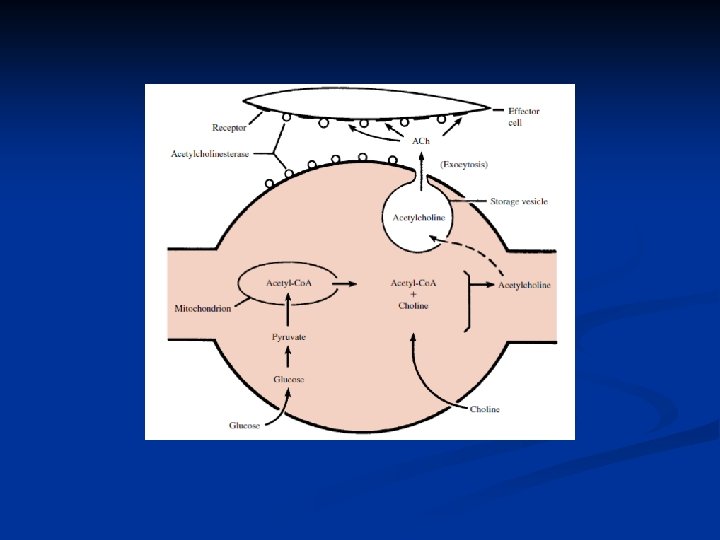
Acetylcholine (Ach) n Synthesis; storage; release & metabolism From choline and acetyl-Co. A Choline acetyl transferase Choline + Acetyl-Co. A Ach degradation (metabolism) by ACHE= acetylcholinesterase - Plasma cholinesterase (pseudo cholinesterase) - Tissue cholinesterase (true cholinesterase)
Acetylcholine (Ach) Interacts with 2 major types of receptors distributed allover the body - Muscarinic receptors (5 subtypes M 1 to M 5) - Nicotinic receptors (2 subtypes: Nn=neuronal or ganglionic type & Nm=neuromuscular or muscular type)
Muscarinic receptors A. Stimulatory muscarinic receptors: parasympathetic nerve terminal → release Ach → interact with muscarinic receptors → ↑ IP 3, DAG and stimulation of adenylate cyclase → all mediate stimulatory responses of cholinergic system e. g. ↑ gland secretion (salivation); contraction of smooth muscles of GIT…etc n
B. Inhibitory muscarinic receptors: Ach → interaction with muscarinic receptors → ↓ activity of adenylate cyclase which mediate the inhibitory effects of Ach e. g. decreased heart rate
Nicotinic receptors A. In voluntary muscles → Ach → nicotinic receptors → depolarization of voluntary muscles →↑ influx of Na+ and Ca++ → generation of action potential → contraction of voluntary muscles n
B. In autonomic ganglia Stimulation of nicotinic receptors in sympathetic and parasympathetic ganglia results in a complex sympathetic and parasympathetic activities C. In CNS Stimulation of CNS nicotinic receptors leads to complex excitatory and inhibitory effects D. In adrenal medulla Stimulation of nicotinic receptors in adrenal medulla leads to an increase in E release
Aetylcholine (Ach) A quaternary positively charged ammonium compound (present in the choline portion of Ach), for this Ach is very hydrophilic and hydrolyzed quickly, therefore it is not used clinically
Ach actions - Relaxation of arterial smooth muscles → vasodilatation → ↓ BP - ↓ heart rate (direct effect) - Miosis; accommodation to near vision - ↑ salivation - ↑ gastric acid secretion - ↑ GIT motility - Relaxation of GIT and urinary system sphincters - ↑ respiratory secretions and bronchoconstriction n
Methacholine; Carbachol; Bethanechol; Pilocarpine - Synthetic; directly acting Ach-like agents - Resist degradation by ACHE so they may have prolonged action and could be given orally or SC - IM & IV administration is contraindicated → severe side effects (nausea, abdominal pain, severe drop in BP with reflex tachyarrhythmias, bronchoconstriction…etc) n
Clinical uses to directly-acting cholinomimetics: - Glaucoma Pilocarpine eye drops and ophthalmic gel → ↓ resistance to movement of aqueous humor out of the eye → open angle glaucoma →↓ intraocular pressure Carbachol could be used in patients resistant to Pilocarpine therapy n
- Urine retention following surgery or child birth Bethanechol is highly effective orally and SC - Clear bowel gases before x-ray or surgery Carbachol or Bethanechol, orally - Diagnosis of bronchial hypersensitivity Methacholine is given by inhalation to a patient and if the patient develops exaggerated airway contraction or bronchoconstriction he or she most likely may develop the disease bronchial asthma
Side effects to directly-acting cholinomimetics: - Abdominal colic, nausea, diarrhea - Vasodilatation and drop in BP - Bronchoconstriction - Sweating and salivation n
Indirectly-acting cholinomimetics - Physostigmine Activates muscarinic and nicotinic receptors (↑ Ach actions at all sites including neuromuscular junction) ↑ intestinal movement ↑ bladder motility Effective orally; SC and as an ophthalmic drops n
Physostigmine clinical uses - Myasthenia gravis Autoimmune disease mainly due to antibodies directed against nicotinic receptors leading to muscle weakness and rapid fatigue Physostigmine increases concentration of Ach at this site - Paralytic ileus and urinary bladder atony which may occur postoperatively or after child birth - Glaucoma - Overdose with anticholinergic drugs e. g. Atropine; TCA’s, Phenothiazines. . . etc n
Physostigmine side effects - Convulsions - Decreased heart rate - Paralysis of voluntary muscles with large doses n
Neostigmine - Has similar actions to Physostigmine but with more effect on skeletal muscles - Considered the drug of choice to treat myasthenia gravis and as an antidote to d-tubocurarine n Side effects - Salivation - Decrease in BP - Bradycardia n
Pyridostigmine Mainly used in the management of myasthenia gravis and has longer duration of action as compared to Neostigmine n Edrophonium Produces similar actions to Neostigmine but more rapidly acting and has longer DOA Mainly used to diagnose myasthenia gravis IV Edrophonium → rapid improvement in muscle strength n
Also, IV Edrophonium could differentiate between over dosage with anticholinesterase (cholinergic crisis) and inadequate treatment with anticholinesterase (myasthenia crisis) Cholinergic crisis → IV Edrophonium → more muscle weakness Myasthenia crisis → IV Edrophonium → ↑ muscle strength
The use of anticholinesterases in Alzheimer’s disease: Alzheimer’s disease is characterized by progressive loss of memory and dementia, believed to be due to decreased or loss of cholinergic transmission in the neocortex Anticholinesterases found to be of benefit in such patients include: Rivasigmine; Tacrine; Galanthamine & Donepezil Such agents produce reversible inhibition of ACHE, they are lipid soluble, cross BBB well and improve the cognitive function in patients with Alzheimer n
The use of anticholinesterases in glaucoma: Demecarium Physostigmine Isoflurophate Echothiophate Available as ophthalmic drops and gel ↑ drainage of eye fluid and possibly ↓ its secretion Long use is not advised (may lead to cataract) n
Organophosphates - Cause irreversible inhibition of ACHE - Many (Malathion; Parathion) are used as insecticides - Many others (Sarin) are used as chemical weapons; known as nerve gases - Therefore, toxicity with such agents should be known well - They are readily absorbed through skin n
Toxicity with organophosphates - Nausea & vomiting - Abdominal pain & diarrhea - Excessive salivation & sweating - Respiratory distress, bronchospasm → death - Drop in BP → death - Muscle weakness → death - Bradycardia, A-V block - Agitation, dizziness. . . n
Management of organophosphate toxicity - Support of ventilation - Atropine SC - Pralidoxime IV Cholinesterase reactivator Quaternary amine does not activate CNS CHE Effective only in the 1 st 12 -24 hrs of poisoning n
Parasympatholytic agents Antimuscarinic; Anticholinergic agents Prototype: Atropine Effective orally, locally and parenterally (SC; IV) Atropine is a belladona alkaloid (plant Atropa Belladona) Blocks selectively muscarinic receptors; has no Ach intrinsic-like activity and has no effect on nicotinic receptors
Atropine pharmacological actions - Small doses produce slight bradycardia; therapeutic and large doses lead to tachycardia & ↑ CO - ↓ salivation; ↓ gastric acidity; ↓ biliary and pancreatic secretions - ↓ intestinal movement (↓ spasm) - ↓ respiratory secretions and dilates bronchi - Dilates pupils & leads to cycloplegia (relaxation of ciliary muscles)=loss of accommodation to near vision n
Atropine pharmacological actions (Cont. ) - ↓ sweating - Urinary retention - CNS effects: Drowsiness, Sedation, ataxia, hallucinations, coma, ↓ concentration and memory… n
Clinical uses to anticholinergics: - Bradycardia - Preanaesthetic medication to ↓ salivary & bronchial secretions SC or IM Atropine; IM Glycopyrrolate bromide = Atropine-like associated with less postoperative agitation - Overdosage of ACHE inhibitors - Bronchial asthma Ipratropium bromide; given by inhalation n
Clinical uses to anticholinergics (Cont. ) - Locally in ophthalmology to produce mydriasis & cycloplegia Atropine DOA 7 -10 days; Scopolamine DOA 3 -7 days; Homatropine DOA 1 -3 days; Cyclopentolate DOA 1 day; Tropicamide DOA 2 -6 hrs (preferred) - Parkinson’s disease Trihexyphenidyl=Benzhexol (Artane®) Benztropine mesylate n
Clinical uses to anticholinergics (Cont. ) - Abdominal spasm & pain & diarrhea - Atropine; Scopolamine; Propantheline; Dicyclomine; Oxybutynin. . . - Motion sickness Scopolamine (oral & transdermal patches) - Congenital pyloric stenosis (Atropine relaxes the pylorus) - Peptic ulcer disease n
Clinical uses to anticholinergics (Cont. ) - Urinary uses Urinary bladder spasm; enuresis; incontinence. . . Propantheline Oxybutynin Dicyclomine Tolterodine n
Side effects to anticholinergics (Anticholinergic manifestations) - Dry mouth - Blurred vision - Tachyarrhythmias - Headache; restlessness; hallucinations; delirium - Constipation - Difficulty in micturition - Loss of accommodation n
Management of anticholinergics overdosage - Rx of severe manifestations (e. g. hypertension; cardiac arrhythmias) - ↓ absorption of tablets - Antidote ACHE inhibitor Physostigmine n
Nicotine & ganglionic blockers Ganglionic transmission is very complex Nicotine is not used clinically, likewise clinical uses to ganglionic blockers are limited because of lack of selectivity to either symp. or parasymp. ganglia
n n n Nicotine Its clinical use is restricted to smoking cessation programs Its importance lies in the fact that it is a CNS stimulant and it is an abused substance and consumed by many people through smoking In low doses, Nicotine stimulates ganglia by depolarization and in large doses it blocks ganglia both in periphery and in CNS It has no effect on neuromuscular junction Nicotine is very lipid soluble
Actions to nicotine - Euphoria; arousal, improves attention, learning and problem solving - In high doses could lead to medullary paralysis and ↓ BP & respiratory depression - ↑ BP due to action on symp. ganglia in periphery - ↑ heart rate - Vasoconstriction of coronary arteries → IHD - ↑ GIT motility (parasymp. ganglia) - Large doses ↓ GIT motility and lead to urine retention (block parasymp. ganglia) n
Side effects to Nicotine - Irritability - Tremors - ↑ heart rate and ↑ BP - Diarrhea - Induction of metabolism of drugs n

Withdrawal manifestations to Nicotine - Irritability - Anxiety - Insomnia - Restlessness - Difficulty in concentration - Abdominal pain n
Trimethaphan & Mecamylamine n Competitive nicotinic ganglionic blockers n They could also block nicotinic receptors at neuromuscular junction n Their use is limited because of lack of specificity to ganglia and development of tolerance to their beneficial effects and due to severe side effects they produce
Trimethaphan is given in an IV infusion and was used to treat hypertensive crisis caused by pulmonary edema or dissecting aortic aneurysm n Mecamylamine is orally effective n Ganglionic blockers are also used to induce hypotension needed in certain plastic surgeries and ophthalmic surgeries n
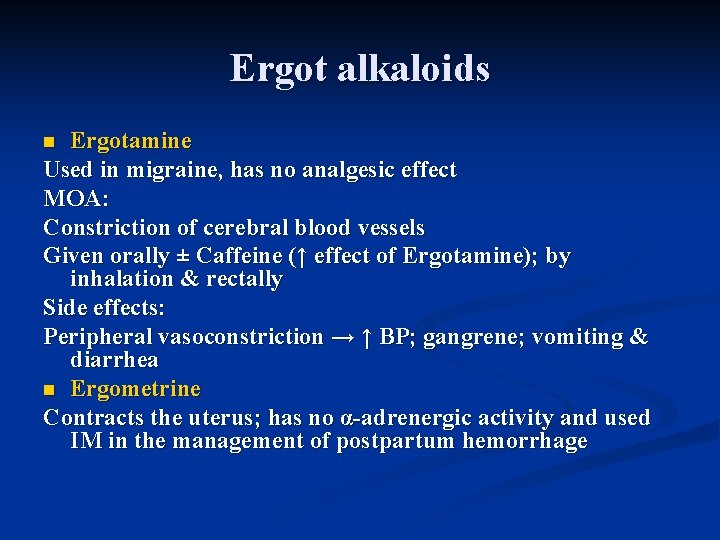
Ergot alkaloids Ergotamine Used in migraine, has no analgesic effect MOA: Constriction of cerebral blood vessels Given orally ± Caffeine (↑ effect of Ergotamine); by inhalation & rectally Side effects: Peripheral vasoconstriction → ↑ BP; gangrene; vomiting & diarrhea n Ergometrine Contracts the uterus; has no α-adrenergic activity and used IM in the management of postpartum hemorrhage n