Autoimmune disease related with periodontal disease 2011 03









- Slides: 42
Auto-immune disease related with periodontal disease 치주과 인턴 최상훈 2011. 03. 29 KHU PERIO
- CONTENT I II IV V KHU • Auto-immue diseae related with periodontal disease • Differential Diagnosis of MMP, PV & OLP • Treatmet • New approach : Hypothesis • Conclusion PERIO
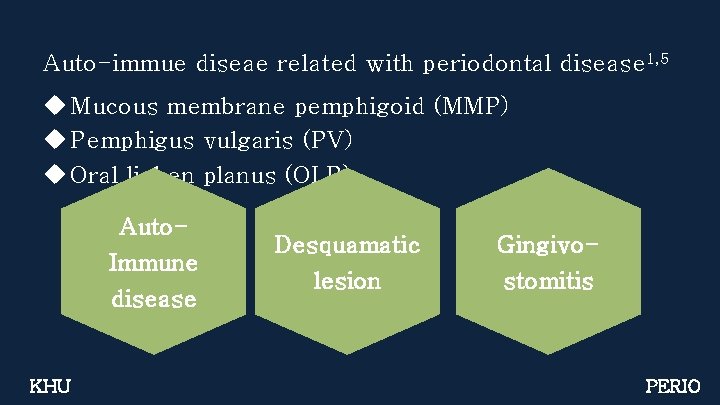
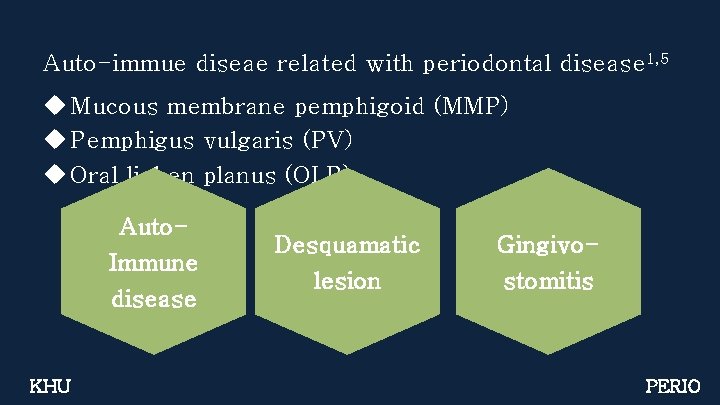
Auto-immue diseae related with periodontal disease 1, 5 u Mucous membrane pemphigoid (MMP) u Pemphigus vulgaris (PV) u Oral lichen planus (OLP) Auto. Immune disease KHU Desquamatic lesion Gingivostomitis PERIO

Auto-immue diseae related with periodontal disease MUCOUS MEMBRANE PEMPHIGOID (MMP)1, 5 Histopathology § § KHU Chronic inflammation Subepithelial blistering - Epithelial separation from underlyng lamina propria - Intact basal layer Onset : 60 to 80 years 1 in 12, 000 ~ 1 in 20, 000 PERIO
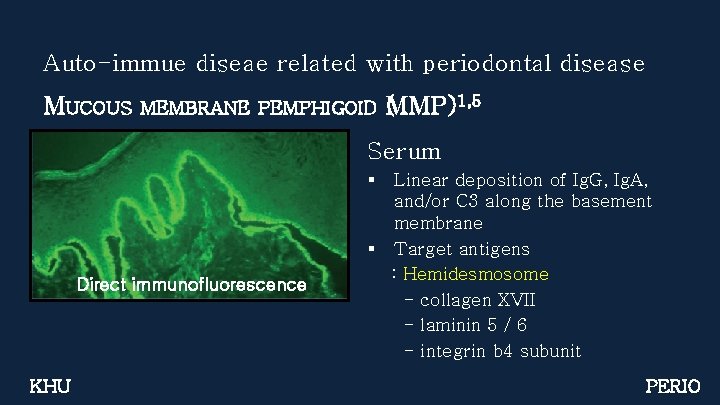
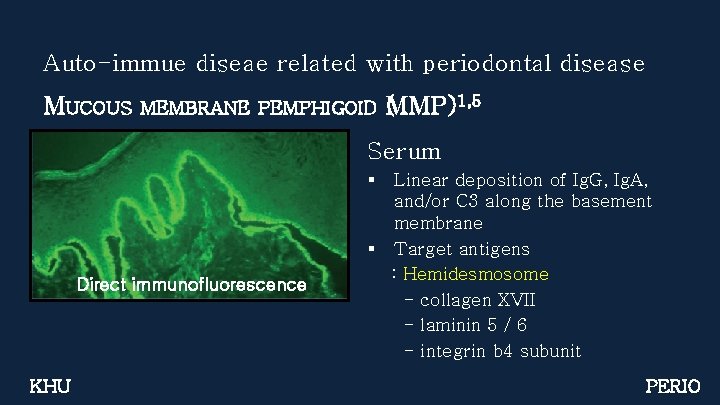
Auto-immue diseae related with periodontal disease MUCOUS MEMBRANE PEMPHIGOID (MMP)1, 5 Serum § Direct immunofluorescence KHU Linear deposition of Ig. G, Ig. A, and/or C 3 along the basement membrane § Target antigens : Hemidesmosome - collagen XVII - laminin 5 / 6 - integrin b 4 subunit PERIO
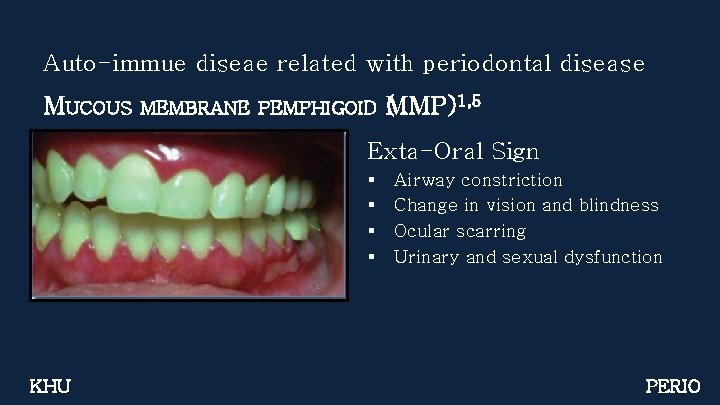
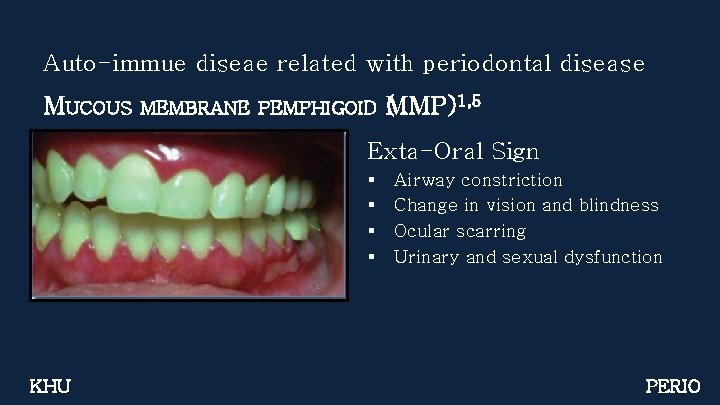
Auto-immue diseae related with periodontal disease MUCOUS MEMBRANE PEMPHIGOID (MMP)1, 5 Exta-Oral Sign § § KHU Airway constriction Change in vision and blindness Ocular scarring Urinary and sexual dysfunction PERIO
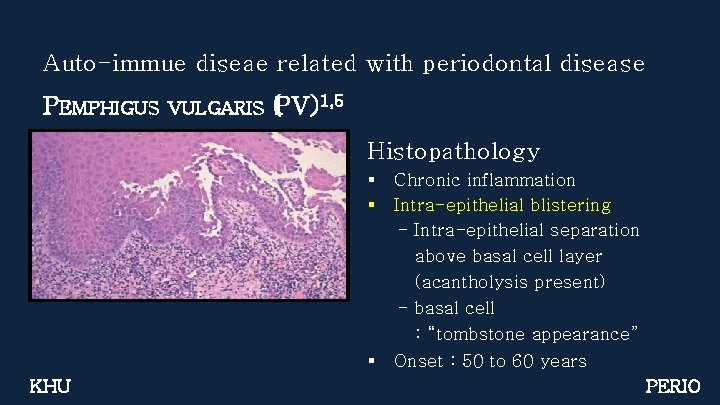
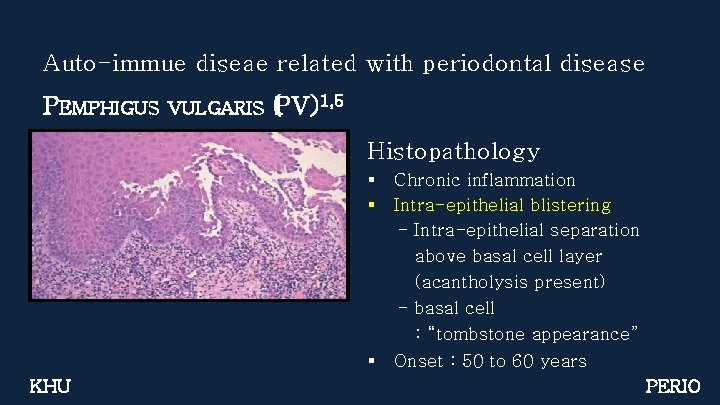
Auto-immue diseae related with periodontal disease PEMPHIGUS VULGARIS (PV)1, 5 Histopathology § § § KHU Chronic inflammation Intra-epithelial blistering - Intra-epithelial separation above basal cell layer (acantholysis present) - basal cell : “tombstone appearance” Onset : 50 to 60 years PERIO
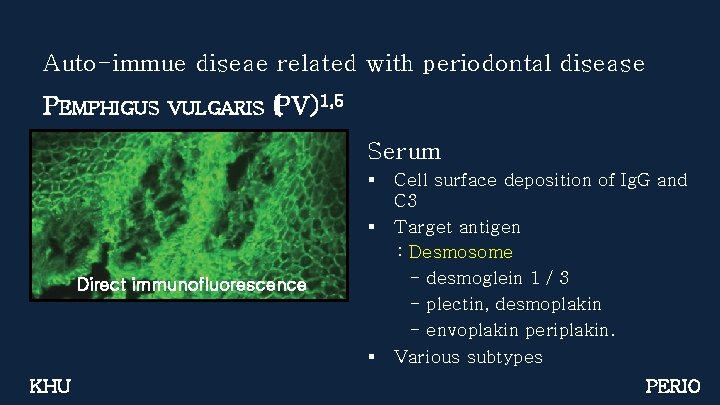
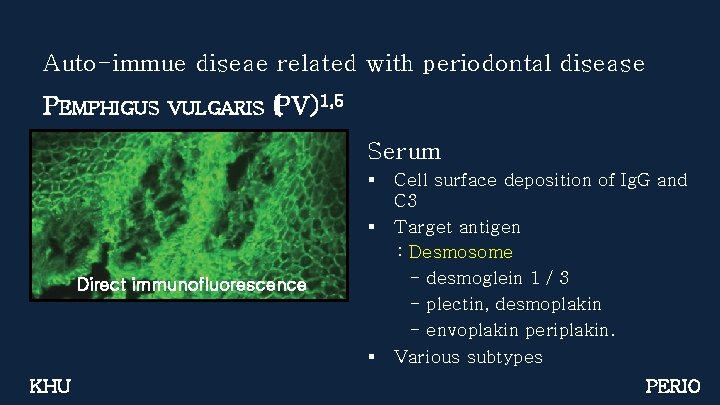
Auto-immue diseae related with periodontal disease PEMPHIGUS VULGARIS (PV)1, 5 Serum § § Direct immunofluorescence § KHU Cell surface deposition of Ig. G and C 3 Target antigen : Desmosome - desmoglein 1 / 3 - plectin, desmoplakin - envoplakin periplakin. Various subtypes PERIO

Auto-immue diseae related with periodontal disease PEMPHIGUS VULGARIS (PV)1, 5 § 1950 s, the mortality : 75% Corticosteroid § Today, the mortality : 10% KHU PERIO
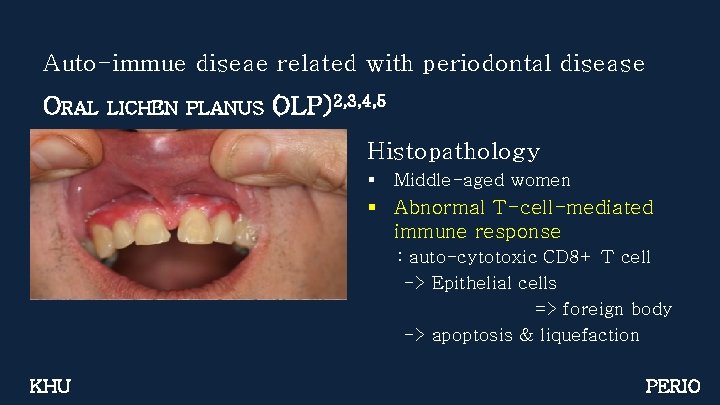
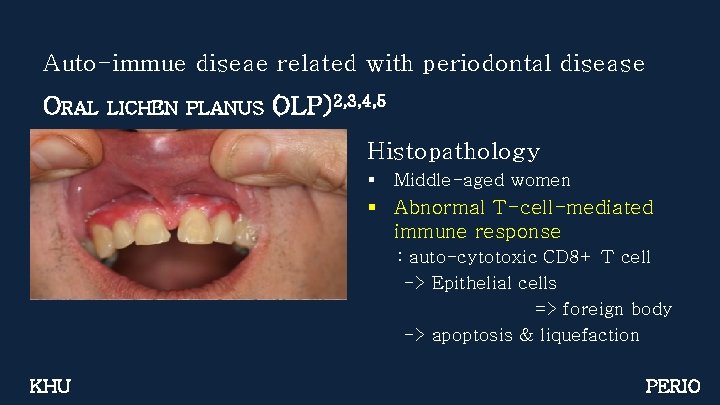
Auto-immue diseae related with periodontal disease ORAL LICHEN PLANUS (OLP)2, 3, 4, 5 Histopathology § Middle-aged women § Abnormal T-cell-mediated immune response : auto-cytotoxic CD 8+ T cell -> Epithelial cells => foreign body -> apoptosis & liquefaction KHU PERIO
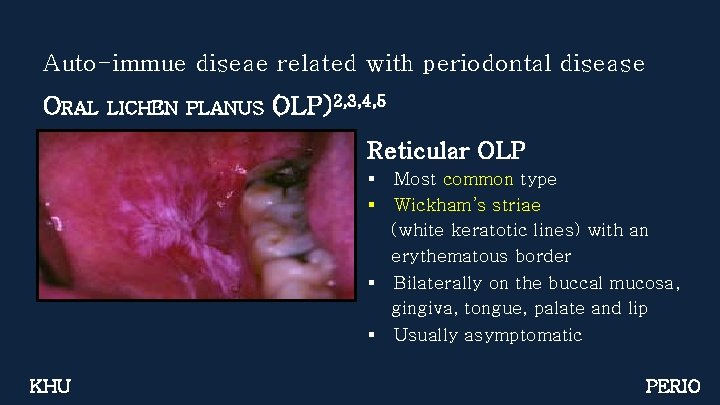
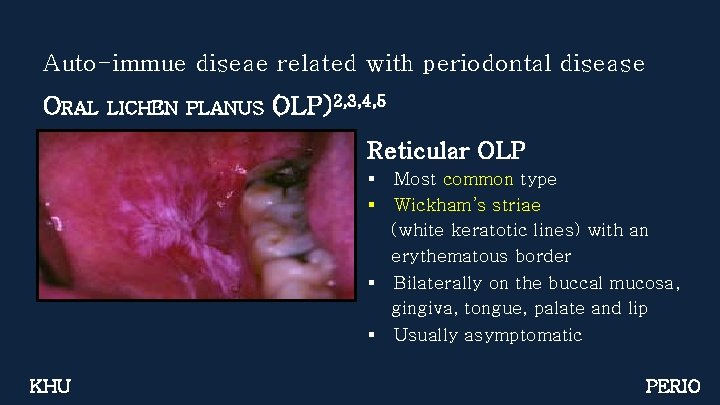
Auto-immue diseae related with periodontal disease ORAL LICHEN PLANUS (OLP)2, 3, 4, 5 Reticular OLP § § Most common type Wickham’s striae (white keratotic lines) with an erythematous border § Bilaterally on the buccal mucosa, gingiva, tongue, palate and lip § Usually asymptomatic KHU PERIO
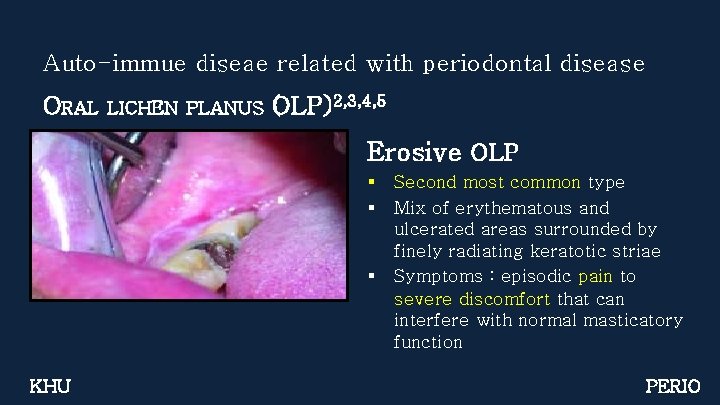
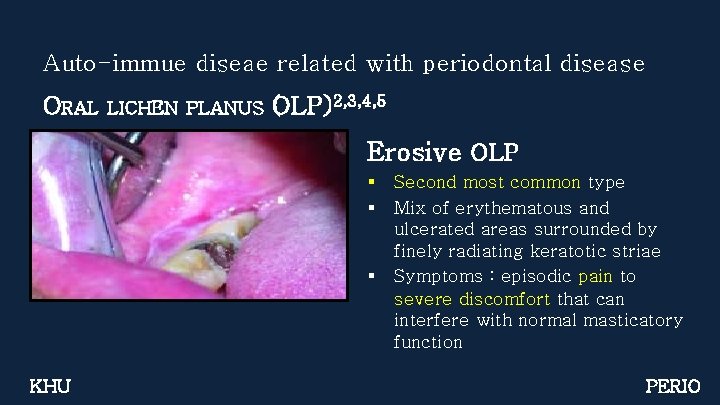
Auto-immue diseae related with periodontal disease ORAL LICHEN PLANUS (OLP)2, 3, 4, 5 Erosive OLP § § § KHU Second most common type Mix of erythematous and ulcerated areas surrounded by finely radiating keratotic striae Symptoms : episodic pain to severe discomfort that can interfere with normal masticatory function PERIO
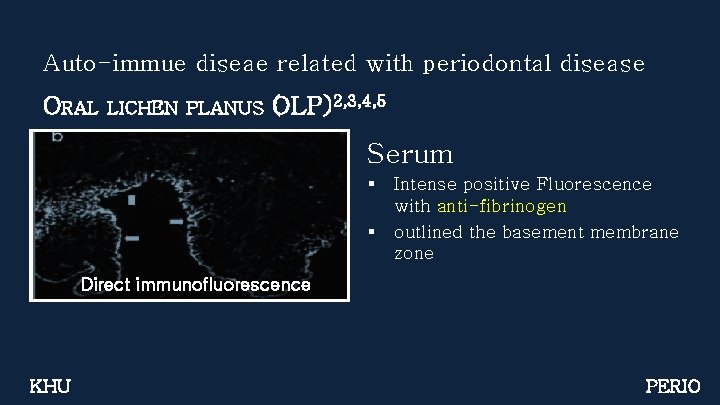
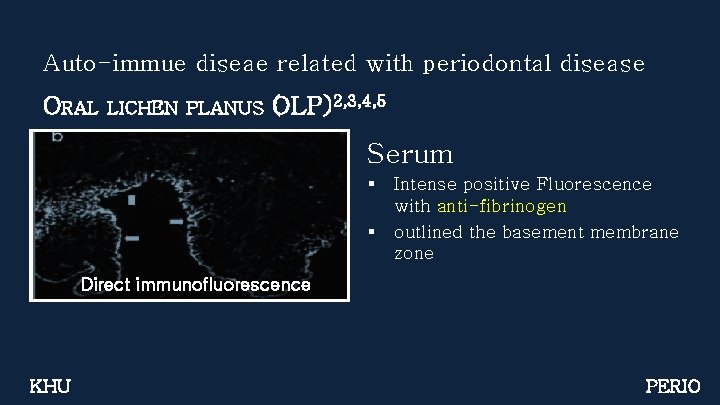
Auto-immue diseae related with periodontal disease ORAL LICHEN PLANUS (OLP)2, 3, 4, 5 Serum § § Intense positive Fluorescence with anti-fibrinogen outlined the basement membrane zone Direct immunofluorescence KHU PERIO
Auto-immue diseae related with periodontal disease ORAL LICHENOID REACTION(OLR)2, 3 Clinical features § Exacervation of an existing OLP or disease by itself § By the presence of medication or dental materials § indistinguishable from idiopathic OLP, clinically or histologically Indirect immunofluorescence study and cutaneous patch test may play a role in differentiating these lesions KHU PERIO

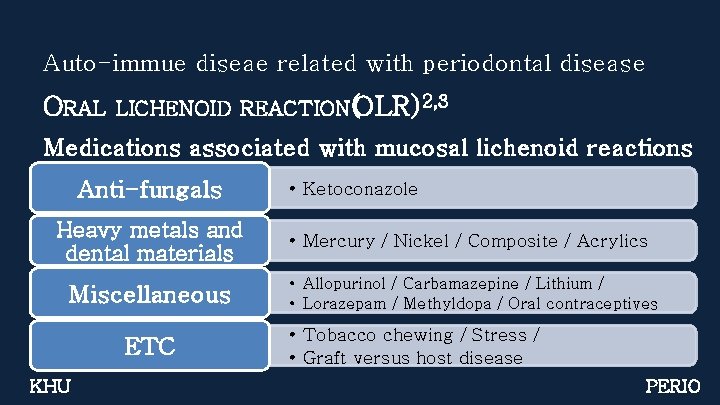
Auto-immue diseae related with periodontal disease ORAL LICHENOID REACTION(OLR)2, 3 Medications associated with mucosal lichenoid reactions NSAIDs Diuretics KHU • Indomethacin / Naproxen / Phenylbutazone • Furosemide / Hydrochlorothiazide Anti-HTN • Angiotensin-converting enzyme inhibitors • Captopril / Beta-blockers /Propranolol Antibiotics • Penicillin / Sulfonamides / Tetracycline PERIO
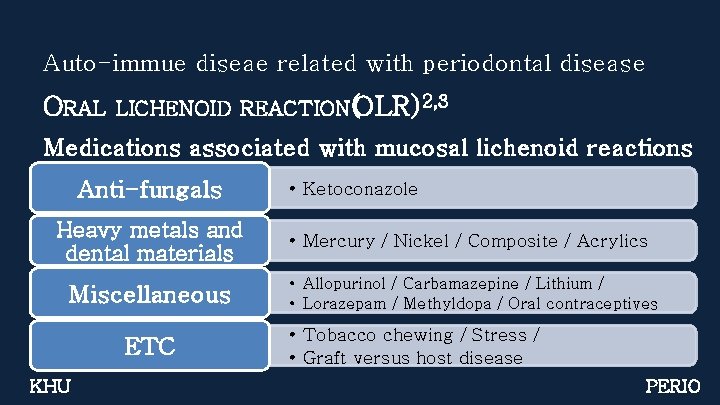
Auto-immue diseae related with periodontal disease ORAL LICHENOID REACTION(OLR)2, 3 Medications associated with mucosal lichenoid reactions Anti-fungals Heavy metals and dental materials Miscellaneous ETC KHU • Ketoconazole • Mercury / Nickel / Composite / Acrylics • Allopurinol / Carbamazepine / Lithium / • Lorazepam / Methyldopa / Oral contraceptives • Tobacco chewing / Stress / • Graft versus host disease PERIO
- CONTENT I II KHU • Auto-immue diseae related with periodontal disease • Differential Diagnosis of MMP, PV & OLP PERIO
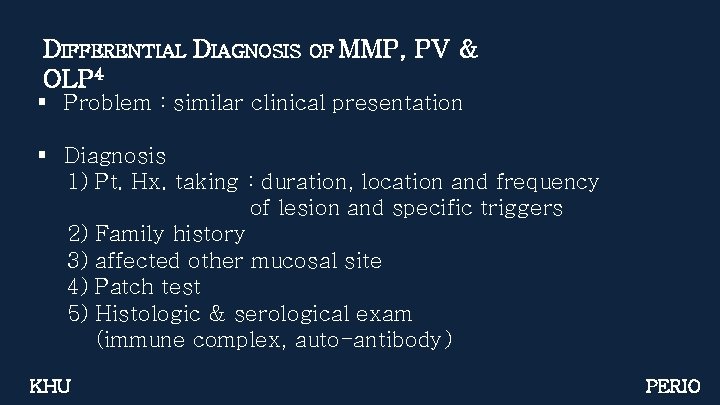
DIFFERENTIAL DIAGNOSIS OLP 4 OF MMP, PV & § Problem : similar clinical presentation § Diagnosis 1) Pt. Hx. taking : duration, location and frequency of lesion and specific triggers 2) Family history 3) affected other mucosal site 4) Patch test 5) Histologic & serological exam (immune complex, auto-antibody) KHU PERIO
- CONTENT I II III KHU • Auto-immue diseae related with periodontal disease • Differential Diagnosis of MMP, PV & OLP • Treatmet PERIO

TREATMENT OF MMP, 5, 10 Disease Erosive OLP Cicatrical pemphigoid Pemphigus KHU PV & OLP Therapy mild Lidex(0. 05% Flucinonide) gel, pc & hs calcitrant Protopic(0. 1% tacrolimus) ointment, bid mild Lidex(0. 05% Flucinonide) gel, pc & hs severe Refer to dermatologist Prednisone : 20 -30 mg/day PERIO

TREATMENT 5, 10 § § § OF MMP, PV & OLP Immunosuppressive therapy Immunomodulatory procedure PUVA therapy Surgical therapy Other treatment modalities KHU PERIO

IMMUNOSUPPRESSIVE THERAPY Topical corticosteroids 10, 11, 12 § Mainstay of the treatment / first-line therapy § Intraoral use of topical steroids - safe and well tolerated § Dose tapering : symptoms improved § The most common adverse effect - candidiasis ( minimized with use of prophylactic anti-fungal therapy ) ※ avoid eating, drinking, and excessive speaking for at least 60 minutes KHU PERIO
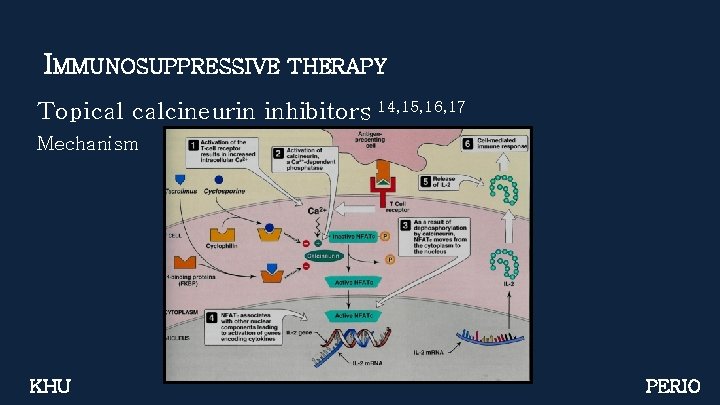
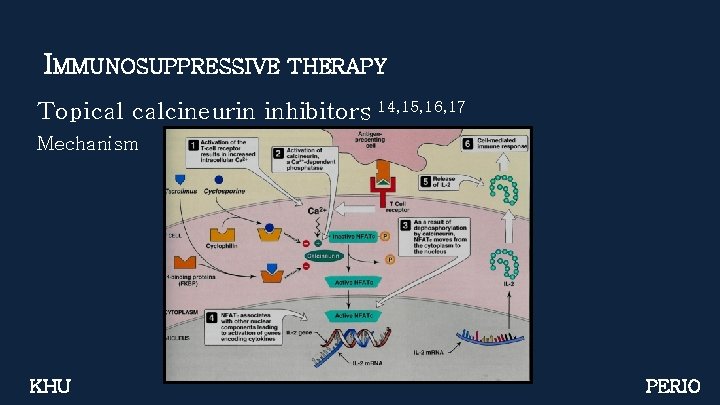
IMMUNOSUPPRESSIVE THERAPY Topical calcineurin inhibitors 14, 15, 16, 17 Mechanism KHU PERIO
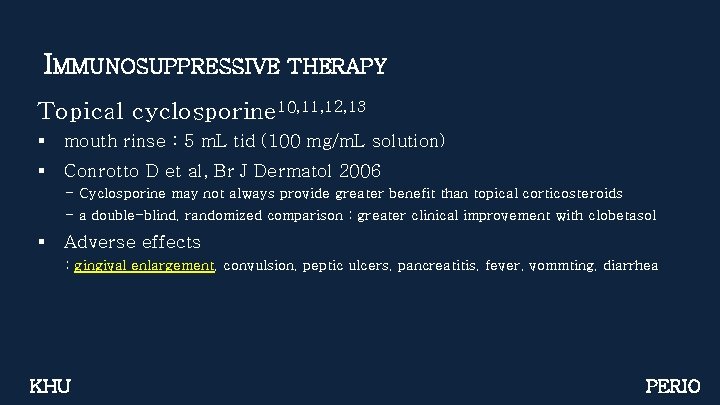
IMMUNOSUPPRESSIVE THERAPY Topical cyclosporine 10, 11, 12, 13 § mouth rinse : 5 m. L tid (100 mg/m. L solution) § Conrotto D et al, Br J Dermatol 2006 - Cyclosporine may not always provide greater benefit than topical corticosteroids - a double-blind, randomized comparison : greater clinical improvement with clobetasol § Adverse effects : gingival enlargement, convulsion, peptic ulcers, pancreatitis, fever, vommting, diarrhea KHU PERIO
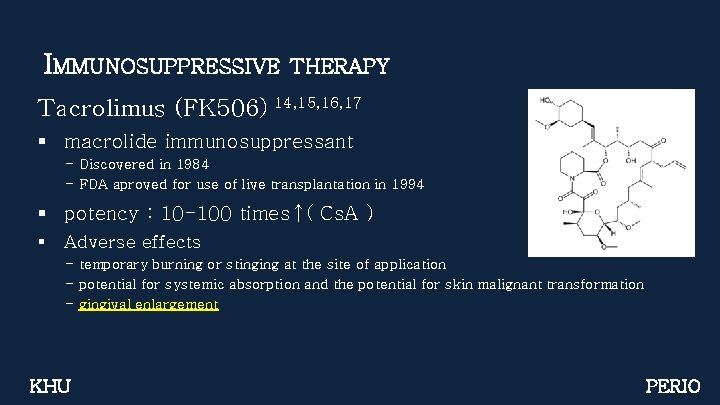
IMMUNOSUPPRESSIVE THERAPY Tacrolimus (FK 506) 14, 15, 16, 17 § macrolide immunosuppressant - Discovered in 1984 - FDA aproved for use of live transplantation in 1994 § potency : 10 -100 times↑( Cs. A ) § Adverse effects - temporary burning or stinging at the site of application - potential for systemic absorption and the potential for skin malignant transformation - gingival enlargement KHU PERIO
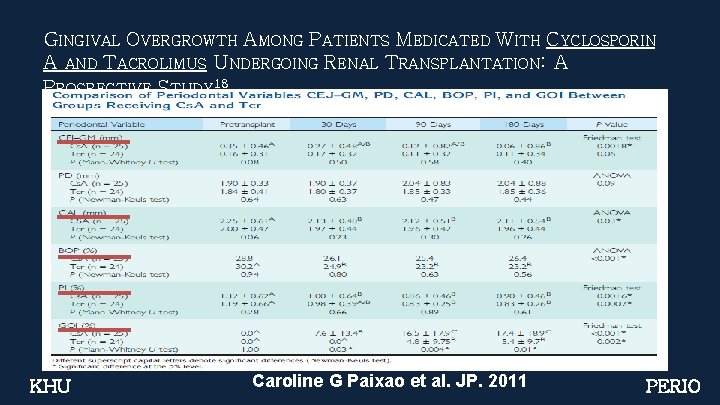
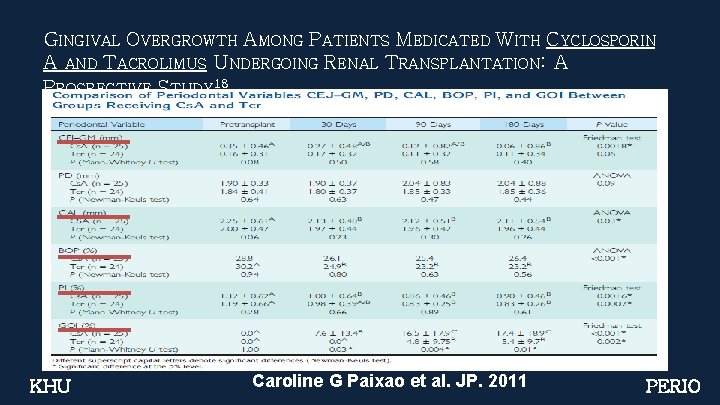
GINGIVAL OVERGROWTH AMONG PATIENTS MEDICATED WITH CYCLOSPORIN A AND TACROLIMUS UNDERGOING RENAL TRANSPLANTATION: A PROSPECTIVE STUDY 18 KHU Caroline G Paixao et al. JP. 2011 PERIO
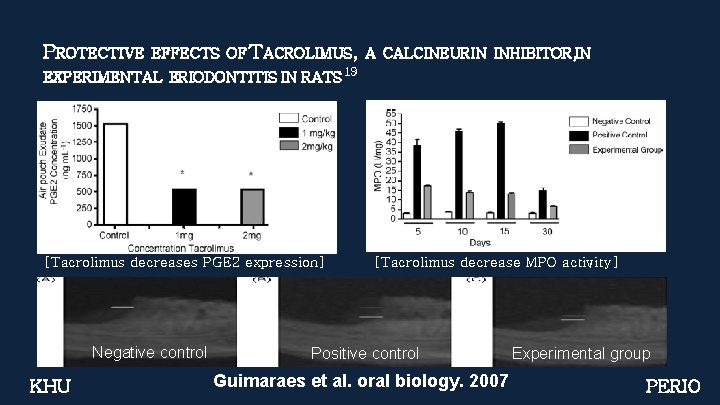
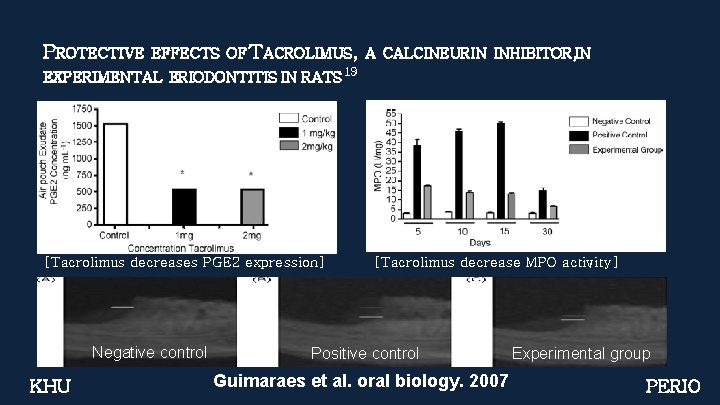
PROTECTIVE EFFECTS OF TACROLIMUS, A CALCINEURIN INHIBITOR, IN EXPERIMENTAL ERIODONTITIS IN RATS 19 [Tacrolimus decreases PGE 2 expression] Negative control KHU [Tacrolimus decrease MPO activity] Positive control Guimaraes et al. oral biology. 2007 Experimental group PERIO
PROTECTIVE EFFECTS OF TACROLIMUS, A CALCINEURIN INHIBITOR, IN EXPERIMENTAL ERIODONTITIS IN RATS 19 SUMMERY 1) Tacrolimus down-regulates(in experimental periodontitis) - IL-1 b, IL-6 and TNF-a, PGE-2 2) Tacrolimus prevented the increase in cytokine expression 3) Tacrolimus minimized progression of periodontal disease 4) Clues for host modulation therapies - Prevention of tissue destruction associated with periodontal disease KHU PERIO
IMMUNOSUPPRESSIVE ADJUVANT 10, 11, 12 § Azathioprine : 1 -2 mg/kg - the first choice of adjuvant therapy in MMP - (hepatotoxic, neutopenia) § Mycophenolate mofetil 2 -2. 5 g/day, bid - MMP & PV - combination with systemic corticosteroid § Cyclophosphamide : 1 -2 mg/kg - aggressive lesion KHU PERIO
IMMUNOMODULATORY 10, 11, 12 PROCEDURE IVIg § Rapidly progressive or treatment-resistant MMP or PV § Rapid onset of action (useful for ocular MMP) § Indication - failure of conventional therapy - significant adverse reaction for conventional therapy § Extremely expansive § Adverse reaction - Fever, chills, flushing, myalgias, nausea, vomiting, and headache KHU PERIO

IMMUNOMODULATORY 10, 11, 12 PROCEDURE Plasmapheresis § Removal of auto-antibody from blood plasma § Considered in difficult case of MMP, PV § Short-therm bridging therapy to longer-term therapy KHU PERIO

PUVA THERAPY 2, 10, 11, 12 PUVA § Psoralens and Long-wave Ultra. Violet-A § Treatment - OLP, eczema, psoriasis, GVHD § Healing of improvement of OLP 81. 2% (13/16) § Side effect - nausea, dizziness, parethesia, headache KHU PERIO
SURGICAL THERAPY 2, 10, 11, 12 § Free gingival graft § Cryosurgery- plaque like lesion § Co 2 laser, Nd: YAG laser NOT RECOMMANDED AS THE FIST CHOICE (recurring of the inflammatory condition) KHU PERIO
- CONTENT I II IV KHU • Auto-immue diseae related with periodontal disease • Differential Diagnosis of MMP, PV & OLP • Treatmet • New approach : Hypothesis PERIO
NEW APPROACH (HYPOTHESIS) 20, 21, 22 § Djouad F et al, Blood 2003 - MSCs are able to suppress T cell activation and proliferation in vitro (MSC source: human, baboon or rodent) § Gang Ding et al, Medical Hypothesis 2011 - OLP is a T cell mediated immune disease - Mesenchymal stem cells(MSCs)’s properties 1) immunosuppressive property affect OLP 2) immunosuppressive properties in vitro and in vivo 3) easily isolated and expanded in vitro MSCs affect OLP via systemic or local application KHU PERIO
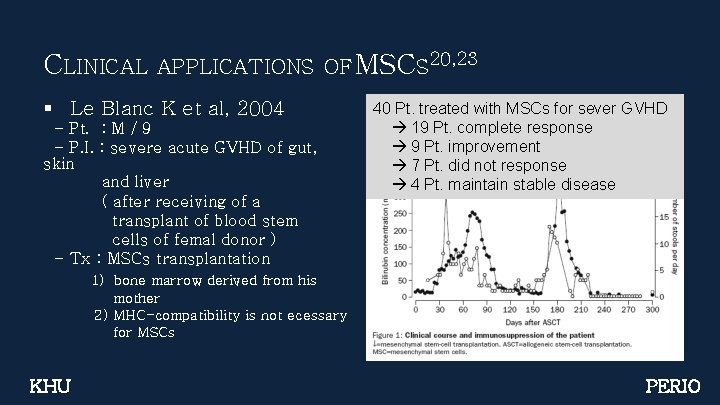
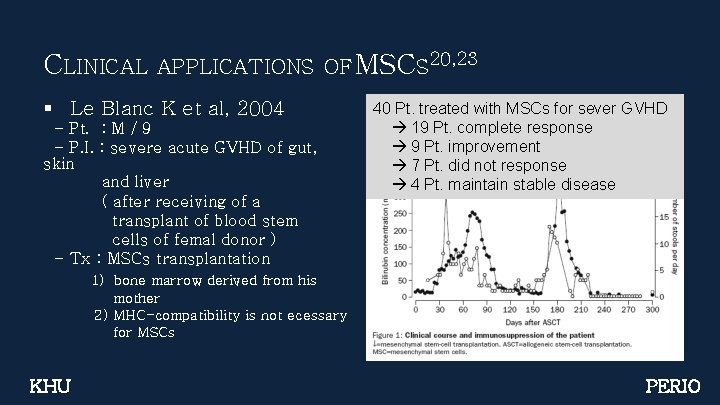
CLINICAL APPLICATIONS OF MSCS 20, 23 § Le Blanc K et al, 2004 - Pt. : M / 9 - P. I. : severe acute GVHD of gut, skin and liver ( after receiving of a transplant of blood stem cells of femal donor ) - Tx : MSCs transplantation 40 Pt. treated with MSCs for sever GVHD 19 Pt. complete response 9 Pt. improvement 7 Pt. did not response 4 Pt. maintain stable disease 1) bone marrow derived from his mother 2) MHC-compatibility is not ecessary for MSCs KHU PERIO
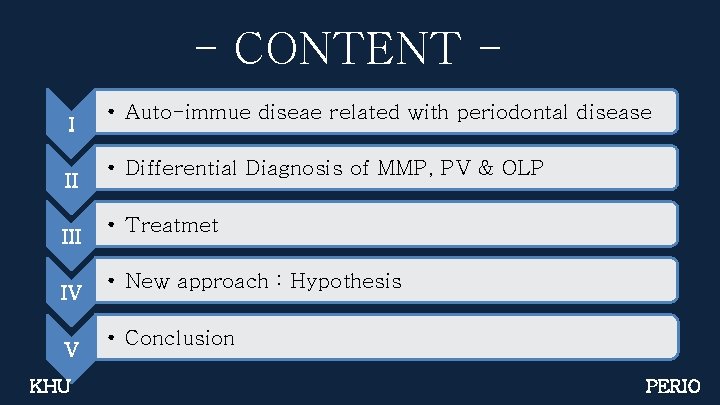
CLINICAL APPLICATIONS OF MSCS 20, 23 § Clinical significance of MSC-mediated trearment for OLP : Immunosuppressive drug related cytotoxities will be decreased. § Evaluation of the hypothesis in OLP Pt. 1) 2) 3) 4) 5) KHU MSC’s colony-forming capacity Cell proliferation stem cell marker expression in vivo tissue formation capability immunosuppressive function PERIO
- CONTENT I II IV V KHU • Auto-immue diseae related with periodontal disease • Differential Diagnosis of MMP, PV & OLP • Treatmet • New approach : Hypothesis • Conclusion PERIO
CONCLUSION 6, 7 1. Evidence-based treatment recommendations are lacking 2. Tx. Goals ① Reducing symptoms ② healing erosive lesions ③ minimizing the functional impact of MMP, MP & OLP 3. Physicians need to be educated ① proper use of medications ( topical and systemic ) ② side effects / risk of concomitant infection ③ Optimization of oral hygiene is fundamental KHU PERIO
REFERENCE 1. Richelle M et al. “The management of mucous membrane pemphigoid and pemphigus. Dermatologic therapy 2010; 23: 268 - 280” 2. Sumairi b. Ismail, Satish K. S. Kumar, Rosnah B. Zain. “Oral lichen planus and lichenoid reactions: etiopathogenesis, diagnosis, management and malignant transformation. Journal of Oral Science 2007; 49; 2: 89 -106” 3. Paul C. Edwards, Robert Kelsch “Oral lichen planus: Clinical presentation and management JCDA 2002; 68(8): 494 -9” 4. D. M. WILLIAMS, “Non-infectious disease of th Oral soft tissue: A new approach. Adv Dent Res 1993; 7(2): 213 -219” 5. Clinical periodontology. Caranza, 10 th edi: 413 -424 6. Scully C, Eisen D, Carrozzo M “Management of oral lichen planus. Am J Clin Dermatol 2000: 1 (5): 287– 306. “ 7. Zakrzewska JM et al. “A systematic review of placebo-controlled randomized clinical trials of treatments used in oral lichen planus. Br J Dermatol 2005: 153 (2): 336– 341. ” 8. Holmstrup P et al. “Effect of dental plaque control on gingival lichen planus. Oral Surg Oral Med Oral Pathol 1990: 69 (5): 585– 590. ” 9. Lodi G et al. “Current controversies in oral lichen planus: report of an international consensus meeting. Part 1. Viral infections and etiopathogenesis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2005: 100 (1): 40– 51. ” 10. BJ Schlosser. “Lichen planus and lichenoid reactions of the oral mucosa Dermatologic Therapy, Vol. 23, 2010, 251– 267” 11. M Carbone et al. “Systemic and topical corticosteroid treatment of oral lichen planus: a comparative study with long-term follow-up. J Oral Pathol Med. 2003 Jul; 32(6): 323 -9. ” 12. Ho VC et al. “Treatment of severe lichen planus with cyclosporine. J Am Acad Dermatol. 1990 Jan; 22(1): 64 -8. “ 13. D Conrotto et al. “Ciclosporin vs. clobetasol in the topical management of atrophic and erosive oral lichen planus: a double-blind, randomized controlled trial. Br J Dermatol 2006: 154 (1): 139– 145. ” KHU PERIO
REFERENCE 14. V Büsing et al. “Recalcitrant Pemphigus Vulgaris Responding to Systemic Tacrolimus Dermatology 2010; 221: 122– 126” 15. Lener EV et al. “Successful treatment of erosive lichen planus with topical tacrolimus. Arch Dermatol. 2001 Apr; 137(4): 419 -22”. 16. Topical tacrolimus in the treatment of symptomatic oral lichen planus: a series of 13 patients. J Am Acad Dermatol. 2002 Jan ; 46(1): 27 -34. 17. Rozycki TW et al. “Management of recalcitrant ulcerative oral lichen planus with topical tacrolimus. J Am Acad Dermatol. 2002 Jan; 46(1): 35 -41” 18. Caroline G Paixao et al. “Gingival Overgrowth Among Patients Medicated With Cyclosporin A and Tacrolimus Undergoing Renal Transplantation: A Prospective Study J Periodontol • February 2011; 251 -258” 19. Guimares MR et al. “Protective effects of Tacrolimus, a calcineurin inhibitor, in experimental periodontitis in rats, oral biology 52(2007) 882– 888” 20. Ding G et al. “Mesenchymal stem cell transplantation: A potential therapy for oral lichen planus, Medical Hypoheses, 76; 3; 322324” 21. Djouad F et al. “Immunosuppressive effect of mesenchymal stem cells favors tumor groth in allogenic animals. Blood 2003; 102; 3837 -3844” 22. Krampera M et al. "Bone marrow mesenchymal stem cells inhibit the response of naïve and memory antigen-specific T cell to their cognate peptide. Blood 2003; 101: 3722 -3729” 23. Le Blanc k et al. “Treatment of severe aucute graft versus host disease with third party haploidentical mesencymal stem cell. Lancet 2004; 363; 1439 -1441” KHU PERIO

 Cupping for thyroid
Cupping for thyroid Beau's lines autoimmune disease
Beau's lines autoimmune disease Iatrogenic factors in periodontal disease
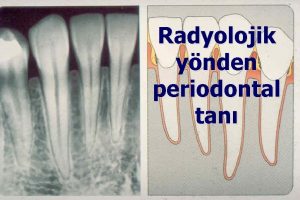
Iatrogenic factors in periodontal disease Diagnosis of periodontal disease
Diagnosis of periodontal disease Periodontal disease
Periodontal disease How is crohn's disease diagnosed
How is crohn's disease diagnosed Autoimmune diet
Autoimmune diet 2 types of fitness
2 types of fitness Health-related
Health-related Communicable disease and non communicable disease
Communicable disease and non communicable disease Corrective phase periodontal therapy
Corrective phase periodontal therapy Grupos de fibras del ligamento periodontal
Grupos de fibras del ligamento periodontal Periodontal abscess
Periodontal abscess Sement dokusu
Sement dokusu Periodonto de insercion
Periodonto de insercion Pdl space
Pdl space Supra and infrabony pocket
Supra and infrabony pocket Alveolar crest
Alveolar crest Gtr indications
Gtr indications Técnica step back (técnica de retroceso)
Técnica step back (técnica de retroceso) Enap periodontal adalah
Enap periodontal adalah Undisplaced flap surgery
Undisplaced flap surgery Principles of scaling and root planing
Principles of scaling and root planing Periodontal ligament injection definition
Periodontal ligament injection definition Corticated margin
Corticated margin Glickman's concept
Glickman's concept Russell periodontal index
Russell periodontal index Stress strain curve physiotherapy
Stress strain curve physiotherapy Murat alikan
Murat alikan Periodontal case study
Periodontal case study General principles of periodontal surgery
General principles of periodontal surgery Prevalencia
Prevalencia Rationale for periodontal treatment
Rationale for periodontal treatment Ligamento periodontal
Ligamento periodontal Periodontal therapy in female patients
Periodontal therapy in female patients Kista primordial adalah
Kista primordial adalah Cva
Cva Ligamento periodontal
Ligamento periodontal Maintenance phase of periodontal therapy
Maintenance phase of periodontal therapy Periodontal case study
Periodontal case study Plica lingualis
Plica lingualis Periodontium definition
Periodontium definition Periapical
Periapical