AUSTRALIAN PATIENT ORGANISATION NETWORK AUSTRALIAN PATIENT ORGANISATION NETWORK




- Slides: 36
AUSTRALIAN PATIENT ORGANISATION NETWORK
AUSTRALIAN PATIENT ORGANISATION NETWORK ONLINE QUESTIONNAIRE RESULTS: AUSTRALIA’S PATIENT ORGANISATIONS
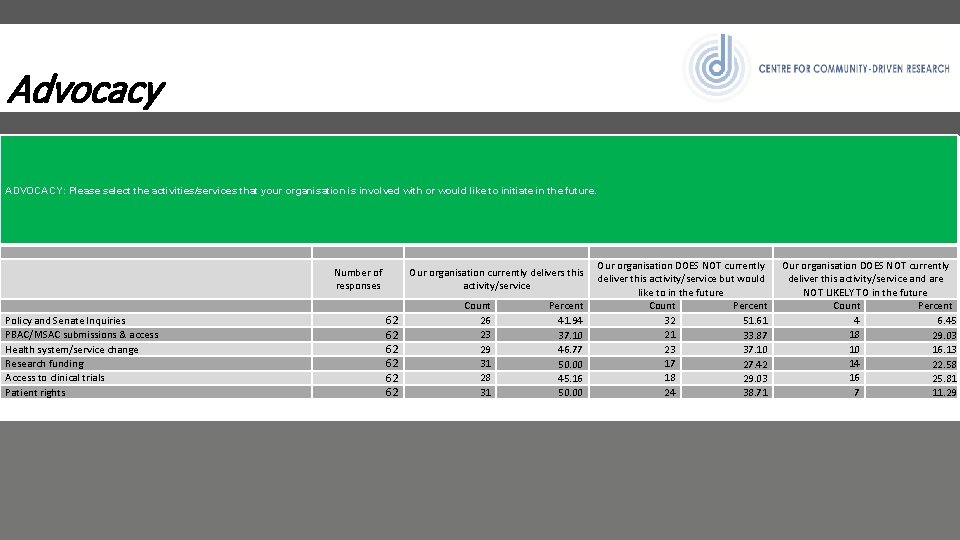
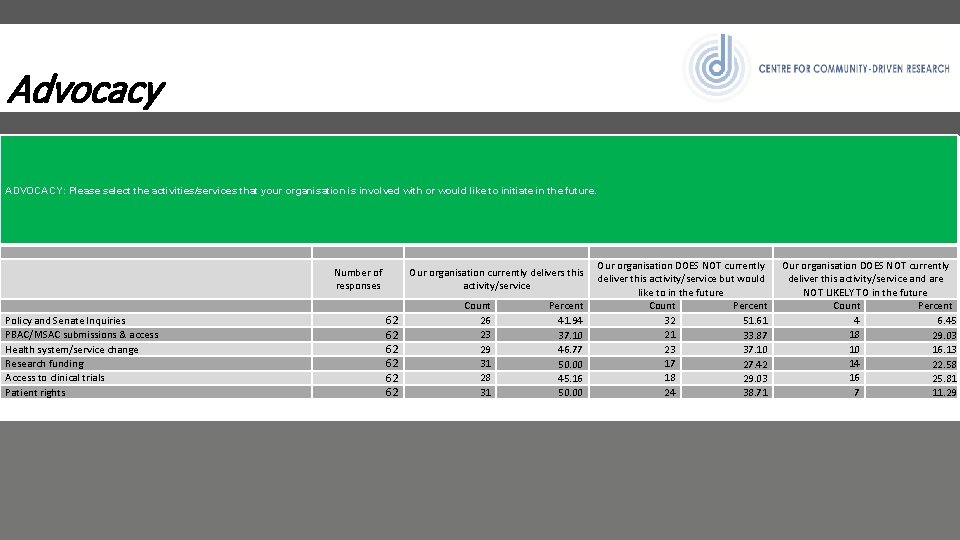
Advocacy ADVOCACY: Please select the activities/services that your organisation is involved with or would like to initiate in the future. Policy and Senate Inquiries PBAC/MSAC submissions & access Health system/service change Research funding Access to clinical trials Patient rights Number of responses Our organisation currently delivers this activity/service 62 62 62 Count 26 23 29 31 28 31 Percent 41. 94 37. 10 46. 77 50. 00 45. 16 50. 00 Our organisation DOES NOT currently deliver this activity/service but would like to in the future Count Percent 32 51. 61 21 33. 87 23 37. 10 17 27. 42 18 29. 03 24 38. 71 Our organisation DOES NOT currently deliver this activity/service and are NOT LIKELY TO in the future Count Percent 4 6. 45 18 29. 03 10 16. 13 14 22. 58 16 25. 81 7 11. 29
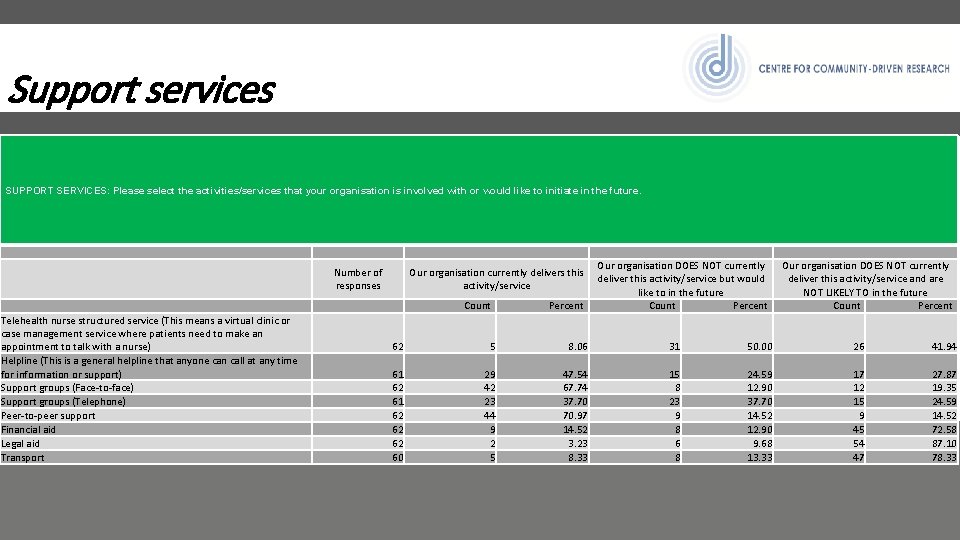
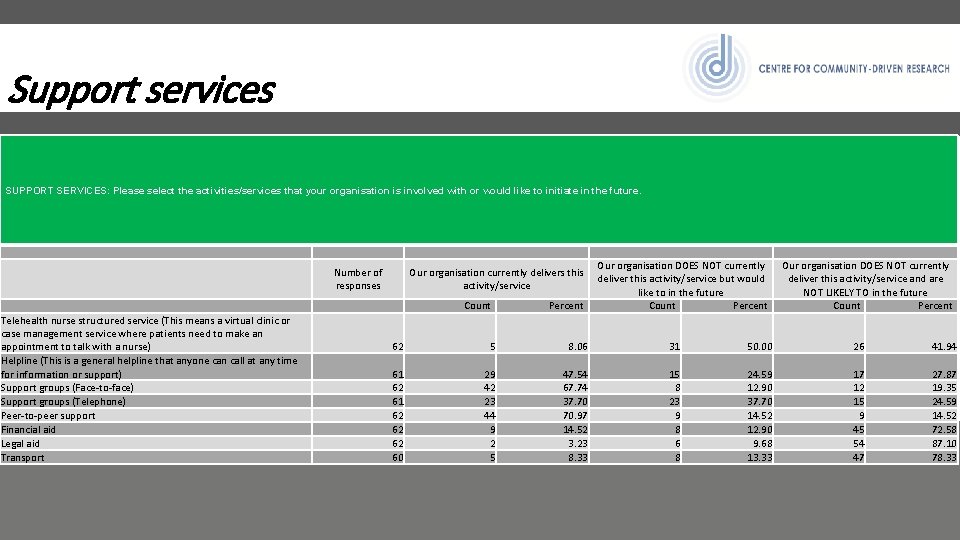
Support services SUPPORT SERVICES: Please select the activities/services that your organisation is involved with or would like to initiate in the future. Number of responses Our organisation currently delivers this activity/service Count Telehealth nurse structured service (This means a virtual clinic or case management service where patients need to make an appointment to talk with a nurse) Helpline (This is a general helpline that anyone can call at any time for information or support) Support groups (Face-to-face) Support groups (Telephone) Peer-to-peer support Financial aid Legal aid Transport Percent Our organisation DOES NOT currently deliver this activity/service but would like to in the future Count Percent Our organisation DOES NOT currently deliver this activity/service and are NOT LIKELY TO in the future Count Percent 62 5 8. 06 31 50. 00 26 41. 94 61 62 62 62 60 29 42 23 44 9 2 5 47. 54 67. 74 37. 70 70. 97 14. 52 3. 23 8. 33 15 8 23 9 8 6 8 24. 59 12. 90 37. 70 14. 52 12. 90 9. 68 13. 33 17 12 15 9 45 54 47 27. 87 19. 35 24. 59 14. 52 72. 58 87. 10 78. 33
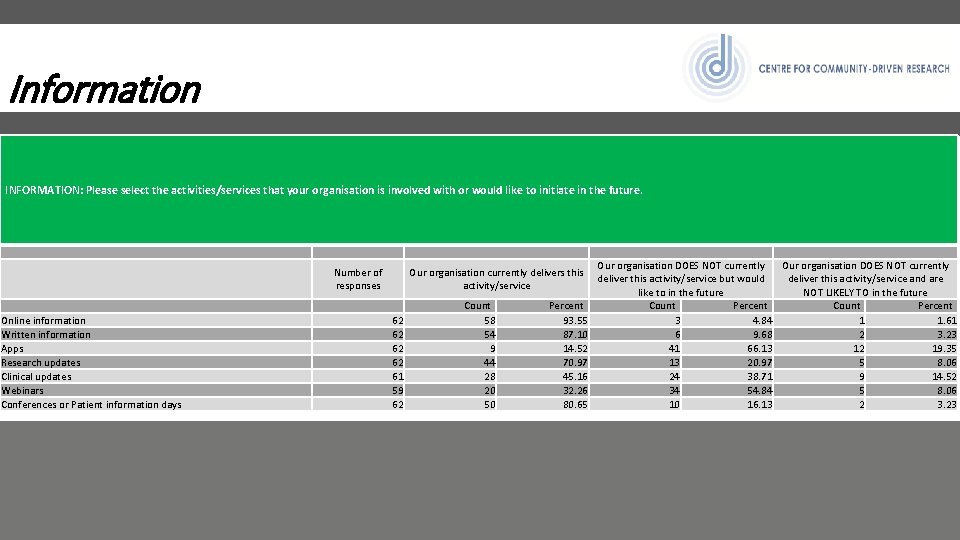
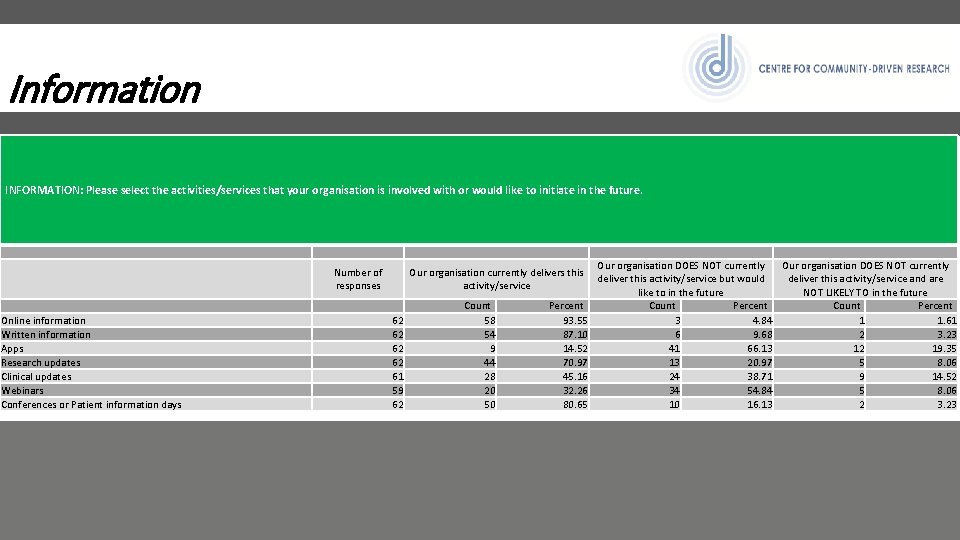
Information INFORMATION: Please select the activities/services that your organisation is involved with or would like to initiate in the future. Online information Written information Apps Research updates Clinical updates Webinars Conferences or Patient information days Number of responses Our organisation currently delivers this activity/service 62 62 61 59 62 Count 58 54 9 44 28 20 50 Percent 93. 55 87. 10 14. 52 70. 97 45. 16 32. 26 80. 65 Our organisation DOES NOT currently deliver this activity/service but would deliver this activity/service and are like to in the future NOT LIKELY TO in the future Count Percent 3 4. 84 1 1. 61 6 9. 68 2 3. 23 41 66. 13 12 19. 35 13 20. 97 5 8. 06 24 38. 71 9 14. 52 34 54. 84 5 8. 06 10 16. 13 2 3. 23
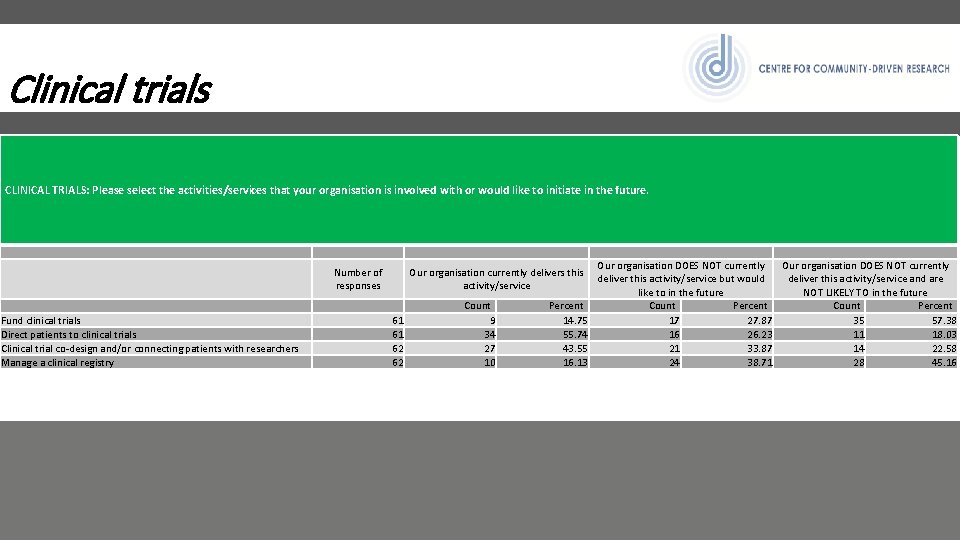
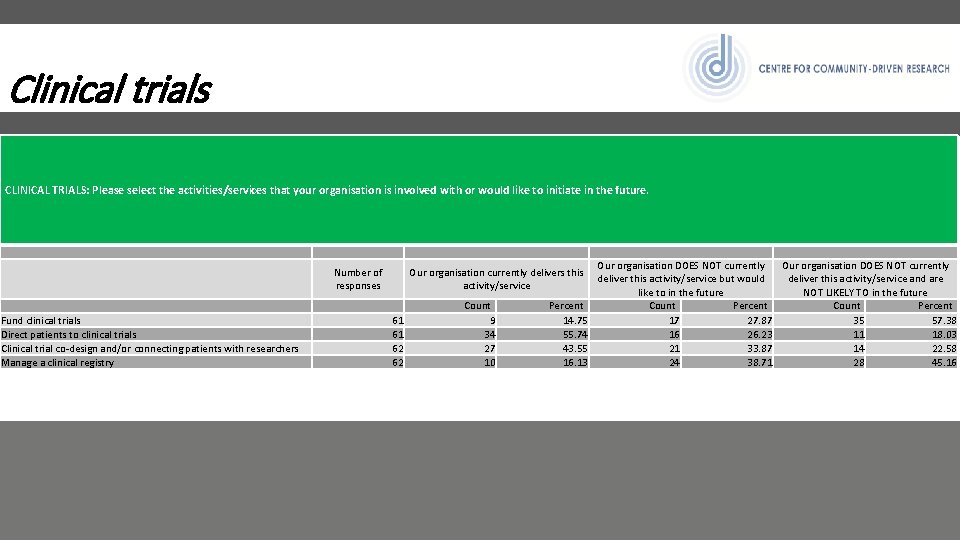
Clinical trials CLINICAL TRIALS: Please select the activities/services that your organisation is involved with or would like to initiate in the future. Fund clinical trials Direct patients to clinical trials Clinical trial co-design and/or connecting patients with researchers Manage a clinical registry Number of responses Our organisation currently delivers this activity/service 61 61 62 62 Count 9 34 27 10 Percent 14. 75 55. 74 43. 55 16. 13 Our organisation DOES NOT currently deliver this activity/service but would deliver this activity/service and are like to in the future NOT LIKELY TO in the future Count Percent 17 27. 87 35 57. 38 16 26. 23 11 18. 03 21 33. 87 14 22. 58 24 38. 71 28 45. 16
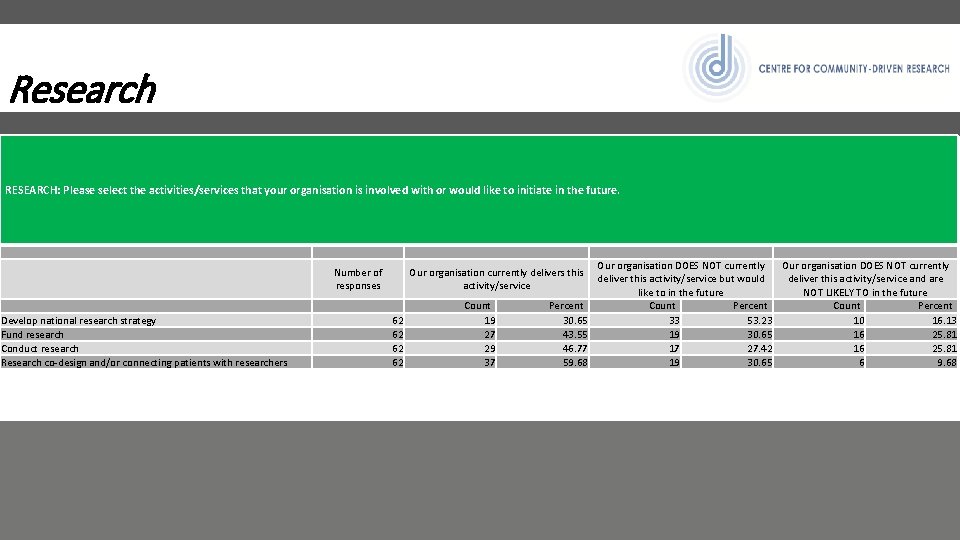
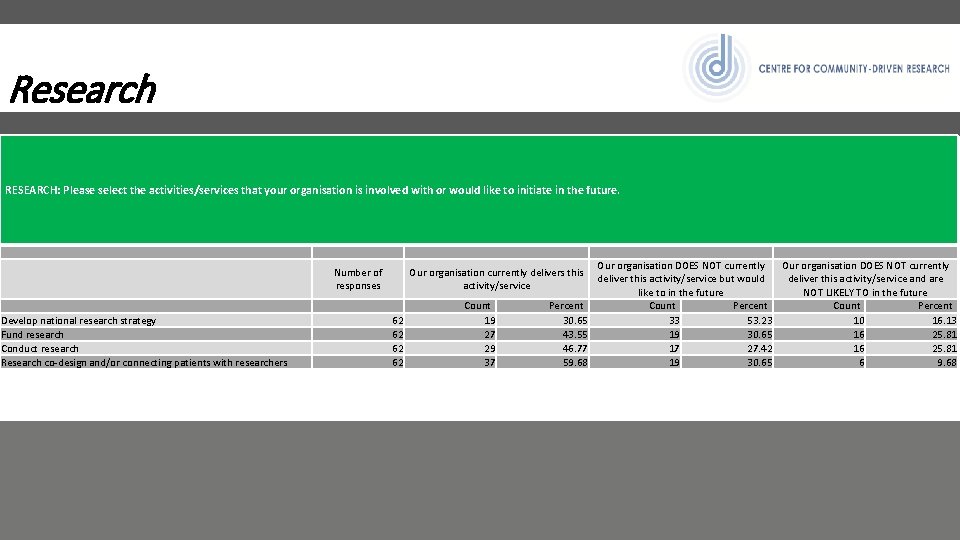
Research RESEARCH: Please select the activities/services that your organisation is involved with or would like to initiate in the future. Develop national research strategy Fund research Conduct research Research co-design and/or connecting patients with researchers Number of responses Our organisation currently delivers this activity/service 62 62 Count 19 27 29 37 Percent 30. 65 43. 55 46. 77 59. 68 Our organisation DOES NOT currently deliver this activity/service but would deliver this activity/service and are like to in the future NOT LIKELY TO in the future Count Percent 33 53. 23 10 16. 13 19 30. 65 16 25. 81 17 27. 42 16 25. 81 19 30. 65 6 9. 68
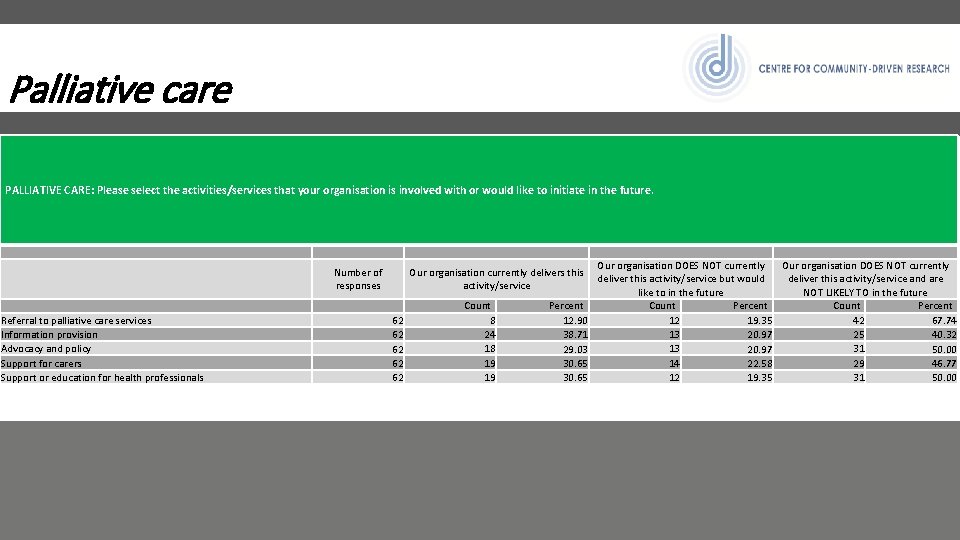
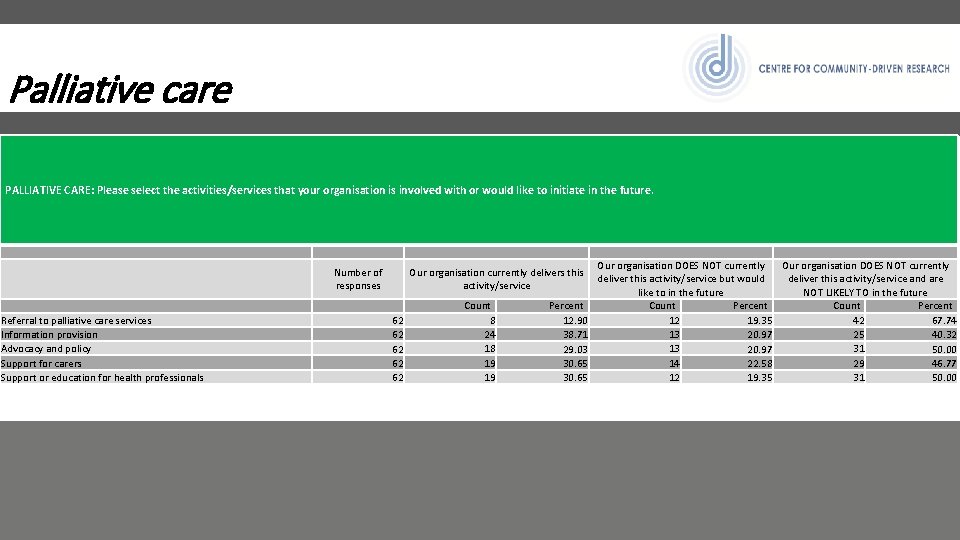
Palliative care PALLIATIVE CARE: Please select the activities/services that your organisation is involved with or would like to initiate in the future. Referral to palliative care services Information provision Advocacy and policy Support for carers Support or education for health professionals Number of responses Our organisation currently delivers this activity/service 62 62 62 Count 8 24 18 19 19 Percent 12. 90 38. 71 29. 03 30. 65 Our organisation DOES NOT currently deliver this activity/service but would deliver this activity/service and are like to in the future NOT LIKELY TO in the future Count Percent 12 42 19. 35 67. 74 13 25 20. 97 40. 32 13 31 20. 97 50. 00 14 29 22. 58 46. 77 12 31 19. 35 50. 00
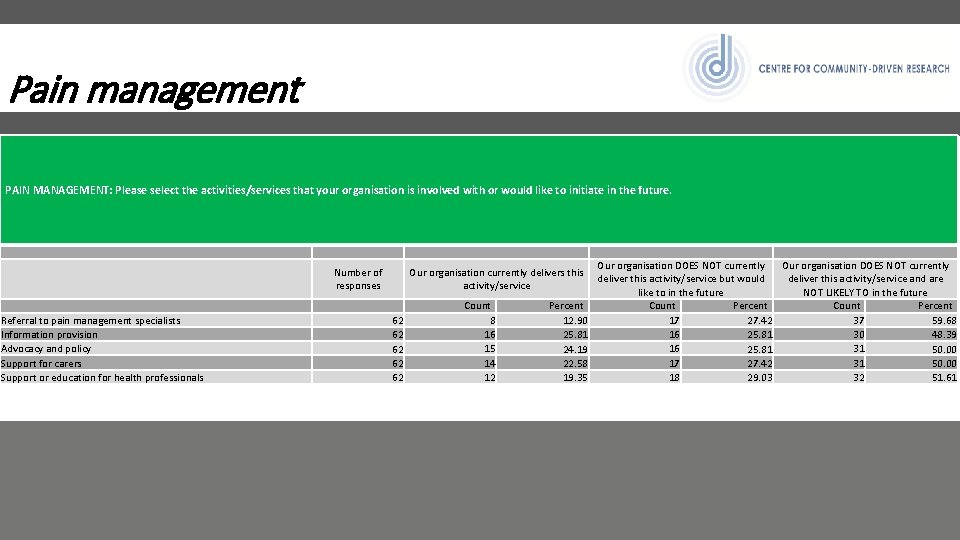
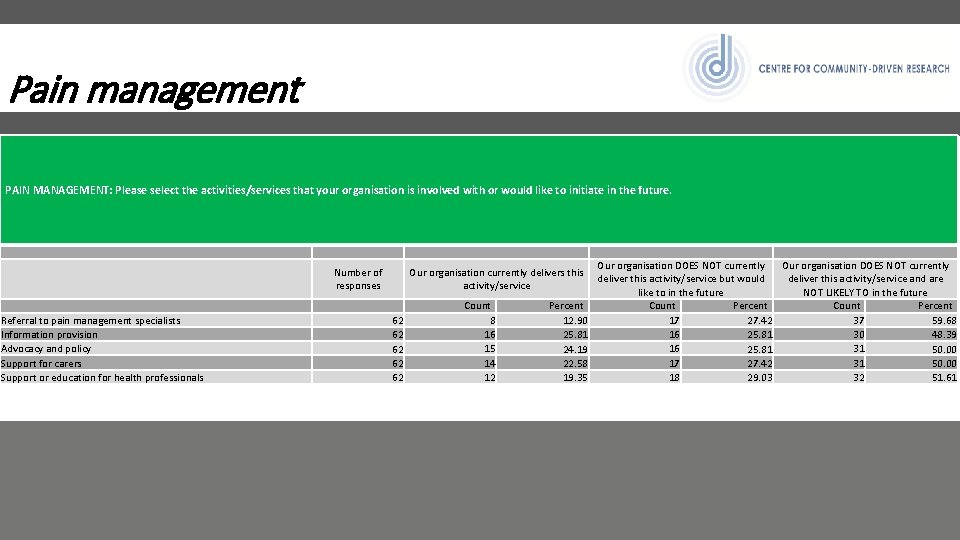
Pain management PAIN MANAGEMENT: Please select the activities/services that your organisation is involved with or would like to initiate in the future. Referral to pain management specialists Information provision Advocacy and policy Support for carers Support or education for health professionals Number of responses Our organisation currently delivers this activity/service 62 62 62 Count 8 16 15 14 12 Percent 12. 90 25. 81 24. 19 22. 58 19. 35 Our organisation DOES NOT currently deliver this activity/service but would deliver this activity/service and are like to in the future NOT LIKELY TO in the future Count Percent 17 37 27. 42 59. 68 16 30 25. 81 48. 39 16 31 25. 81 50. 00 17 31 27. 42 50. 00 18 32 29. 03 51. 61
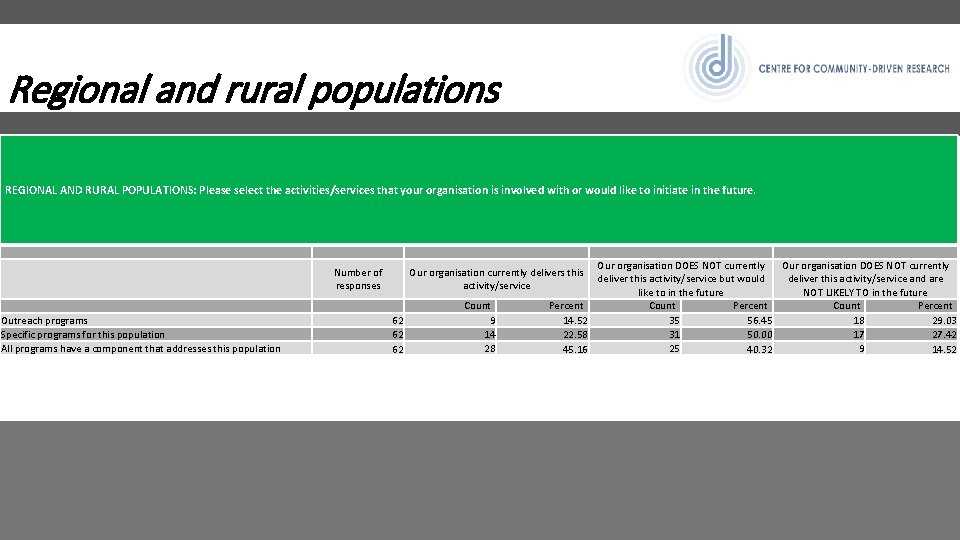
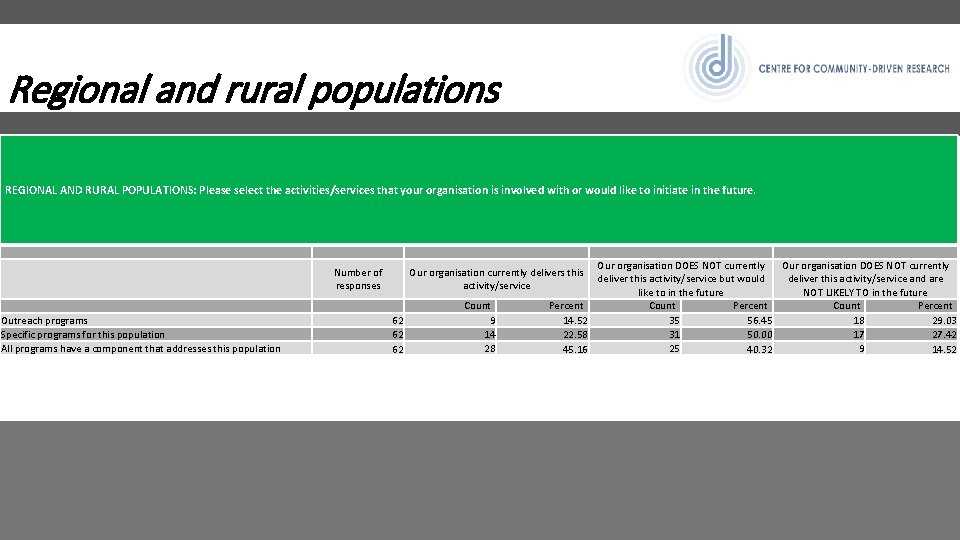
Regional and rural populations REGIONAL AND RURAL POPULATIONS: Please select the activities/services that your organisation is involved with or would like to initiate in the future. Outreach programs Specific programs for this population All programs have a component that addresses this population Number of responses Our organisation DOES NOT currently deliver this activity/service but would deliver this activity/service and are like to in the future NOT LIKELY TO in the future Percent Count Percent 35 18 14. 52 56. 45 29. 03 31 17 22. 58 50. 00 27. 42 25 9 45. 16 40. 32 14. 52 Our organisation currently delivers this activity/service 62 62 62 Count 9 14 28
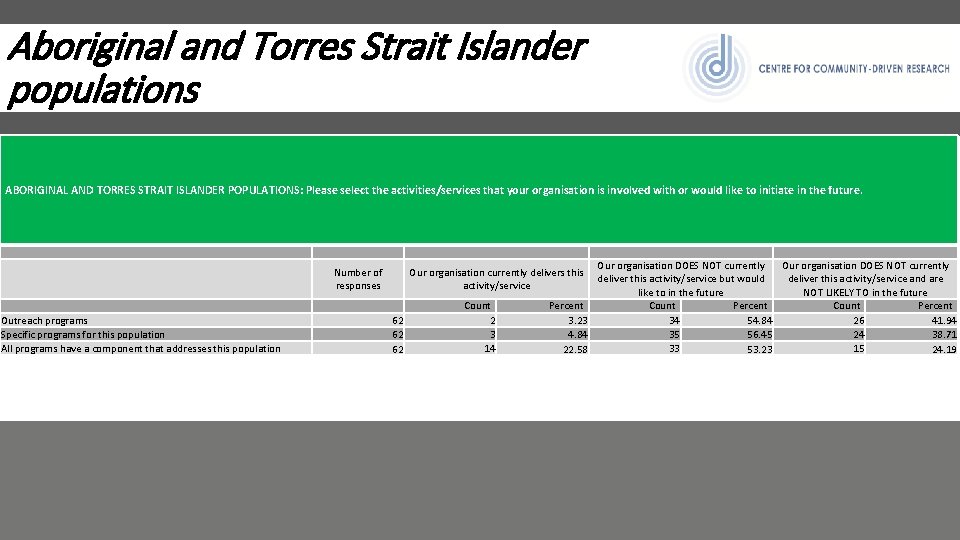
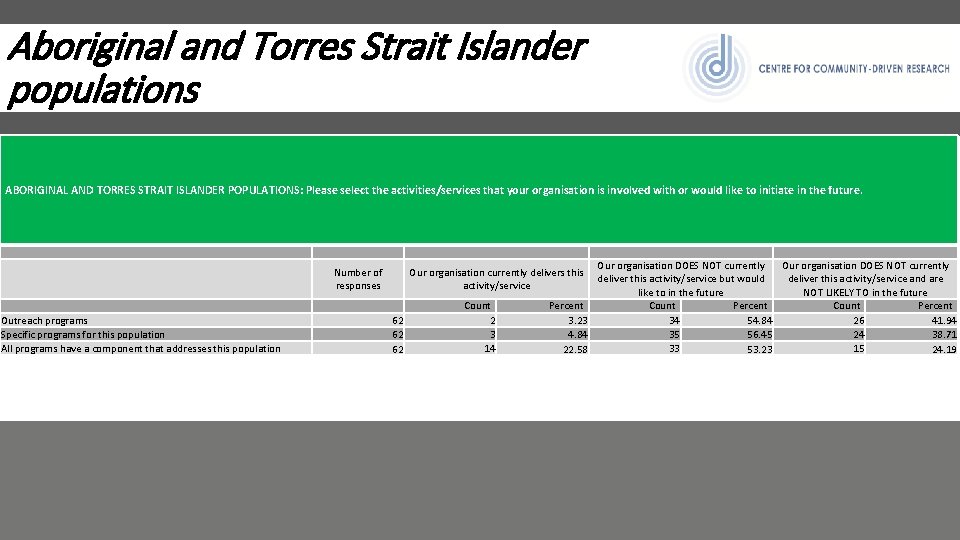
Aboriginal and Torres Strait Islander populations ABORIGINAL AND TORRES STRAIT ISLANDER POPULATIONS: Please select the activities/services that your organisation is involved with or would like to initiate in the future. Outreach programs Specific programs for this population All programs have a component that addresses this population Number of responses Our organisation DOES NOT currently deliver this activity/service but would deliver this activity/service and are like to in the future NOT LIKELY TO in the future Percent Count Percent 34 26 3. 23 54. 84 41. 94 35 24 4. 84 56. 45 38. 71 33 15 22. 58 53. 23 24. 19 Our organisation currently delivers this activity/service 62 62 62 Count 2 3 14
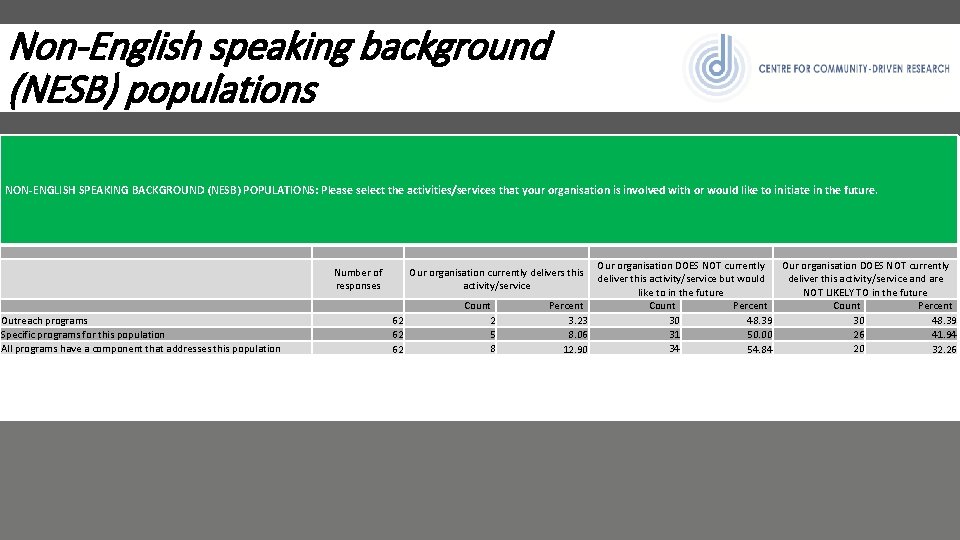
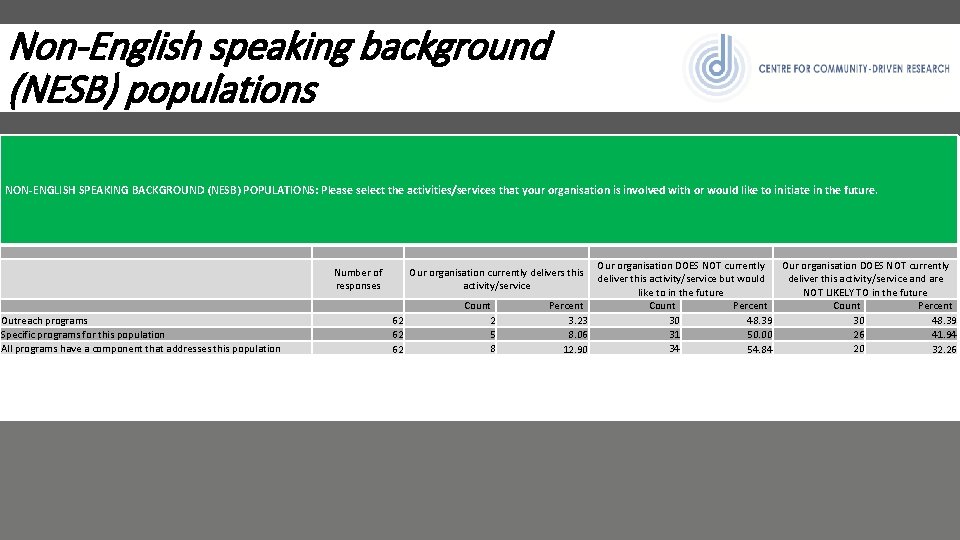
Non-English speaking background (NESB) populations NON-ENGLISH SPEAKING BACKGROUND (NESB) POPULATIONS: Please select the activities/services that your organisation is involved with or would like to initiate in the future. Outreach programs Specific programs for this population All programs have a component that addresses this population Number of responses Our organisation DOES NOT currently deliver this activity/service but would deliver this activity/service and are like to in the future NOT LIKELY TO in the future Percent Count Percent 30 30 3. 23 48. 39 31 26 8. 06 50. 00 41. 94 34 20 12. 90 54. 84 32. 26 Our organisation currently delivers this activity/service 62 62 62 Count 2 5 8
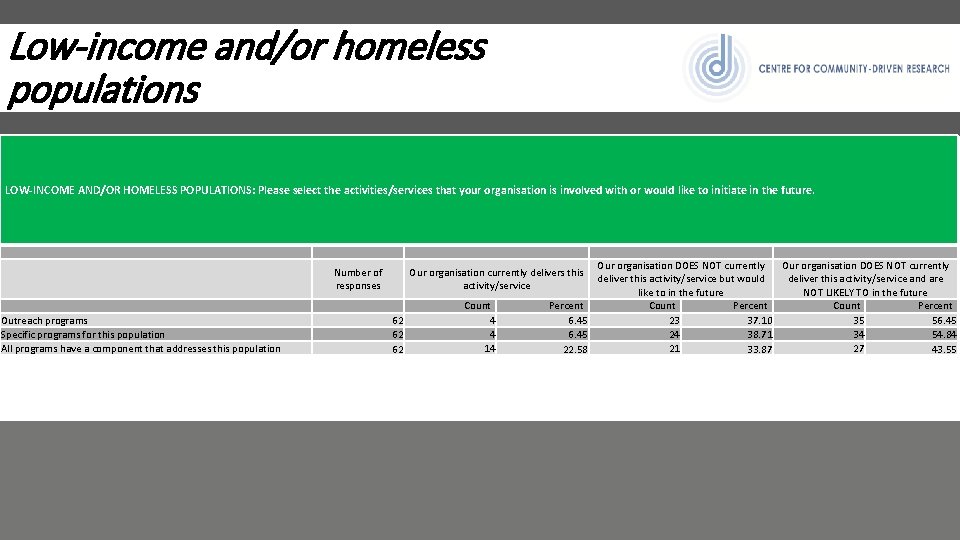
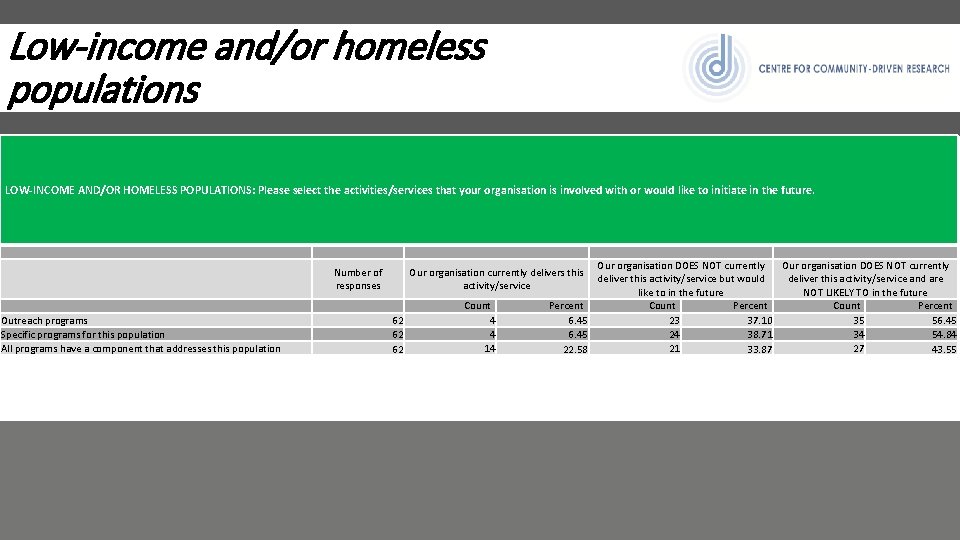
Low-income and/or homeless populations LOW-INCOME AND/OR HOMELESS POPULATIONS: Please select the activities/services that your organisation is involved with or would like to initiate in the future. Outreach programs Specific programs for this population All programs have a component that addresses this population Number of responses Our organisation DOES NOT currently deliver this activity/service but would deliver this activity/service and are like to in the future NOT LIKELY TO in the future Percent Count Percent 23 35 6. 45 37. 10 56. 45 24 34 6. 45 38. 71 54. 84 21 27 22. 58 33. 87 43. 55 Our organisation currently delivers this activity/service 62 62 62 Count 4 4 14
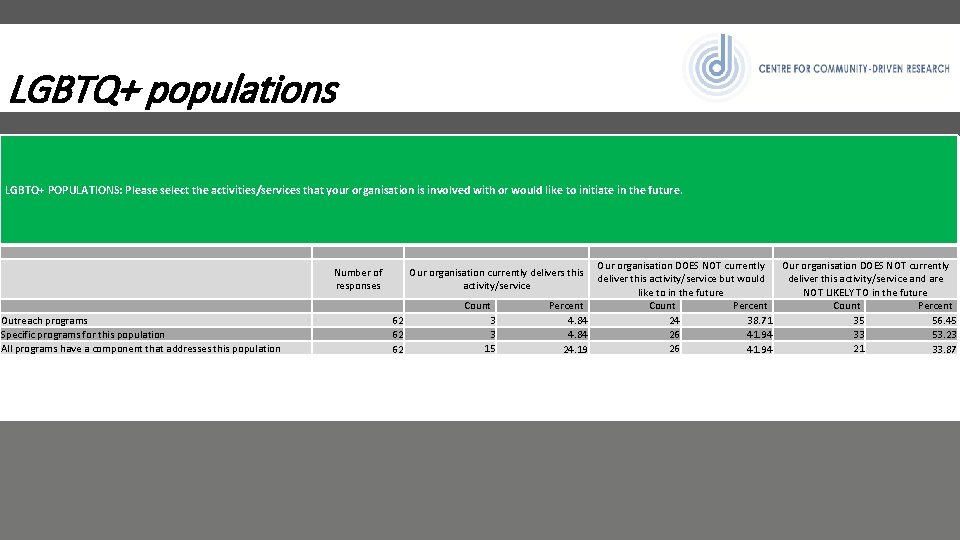
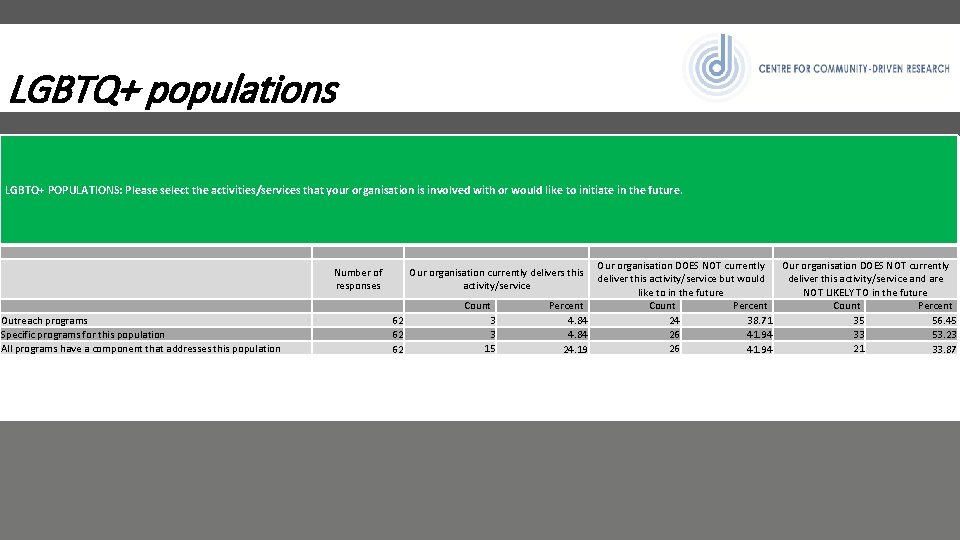
LGBTQ+ populations LGBTQ+ POPULATIONS: Please select the activities/services that your organisation is involved with or would like to initiate in the future. Outreach programs Specific programs for this population All programs have a component that addresses this population Number of responses Our organisation DOES NOT currently deliver this activity/service but would deliver this activity/service and are like to in the future NOT LIKELY TO in the future Percent Count Percent 24 35 4. 84 38. 71 56. 45 26 33 4. 84 41. 94 53. 23 26 21 24. 19 41. 94 33. 87 Our organisation currently delivers this activity/service 62 62 62 Count 3 3 15
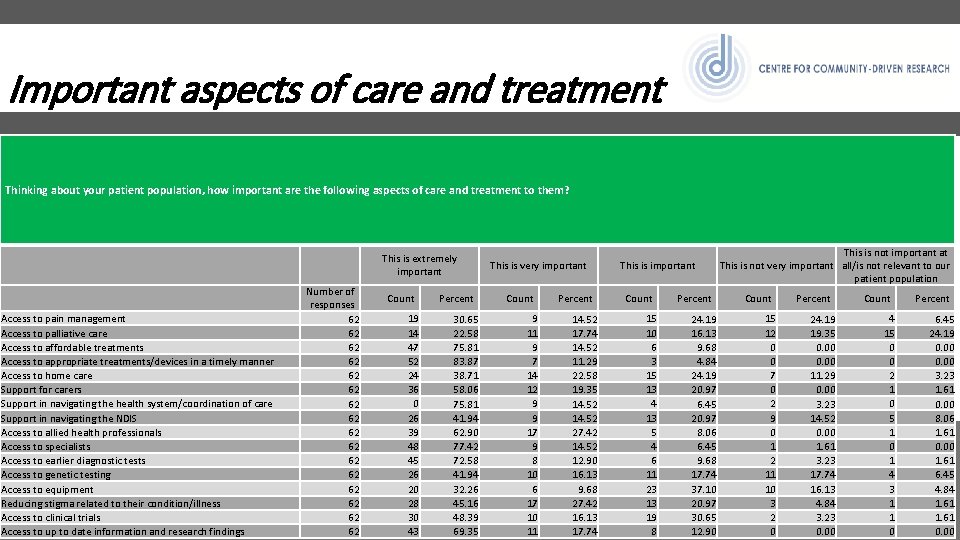
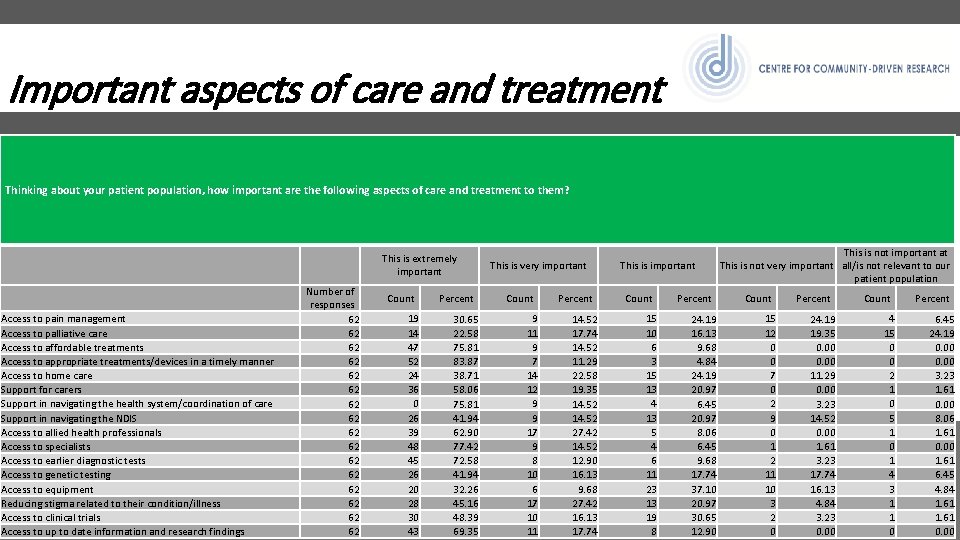
Important aspects of care and treatment Thinking about your patient population, how important are the following aspects of care and treatment to them? This is extremely important Access to pain management Access to palliative care Access to affordable treatments Access to appropriate treatments/devices in a timely manner Access to home care Support for carers Support in navigating the health system/coordination of care Support in navigating the NDIS Access to allied health professionals Access to specialists Access to earlier diagnostic tests Access to genetic testing Access to equipment Reducing stigma related to their condition/illness Access to clinical trials Access to up to date information and research findings Number of responses 62 62 62 62 Count 19 14 47 52 24 36 0 26 39 48 45 26 20 28 30 43 Percent 30. 65 22. 58 75. 81 83. 87 38. 71 58. 06 75. 81 41. 94 62. 90 77. 42 72. 58 41. 94 32. 26 45. 16 48. 39 69. 35 This is very important Count 9 11 9 7 14 12 9 9 17 9 8 10 6 17 10 11 Percent 14. 52 17. 74 14. 52 11. 29 22. 58 19. 35 14. 52 27. 42 14. 52 12. 90 16. 13 9. 68 27. 42 16. 13 17. 74 This is important Count 15 10 6 3 15 13 4 13 5 4 6 11 23 13 19 8 Percent 24. 19 16. 13 9. 68 4. 84 24. 19 20. 97 6. 45 20. 97 8. 06 6. 45 9. 68 17. 74 37. 10 20. 97 30. 65 12. 90 This is not important at This is not very important all/is not relevant to our patient population Count 15 12 0 0 7 0 2 9 0 1 2 11 10 3 2 0 Percent 24. 19 19. 35 0. 00 11. 29 0. 00 3. 23 14. 52 0. 00 1. 61 3. 23 17. 74 16. 13 4. 84 3. 23 0. 00 Count 4 15 0 0 2 1 0 5 1 0 1 4 3 1 1 0 Percent 6. 45 24. 19 0. 00 3. 23 1. 61 0. 00 8. 06 1. 61 0. 00 1. 61 6. 45 4. 84 1. 61 0. 00
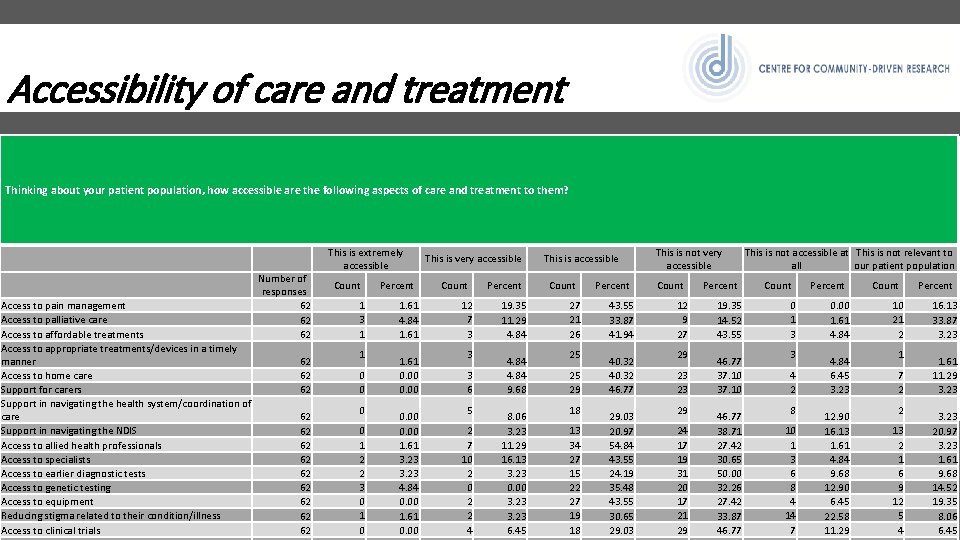
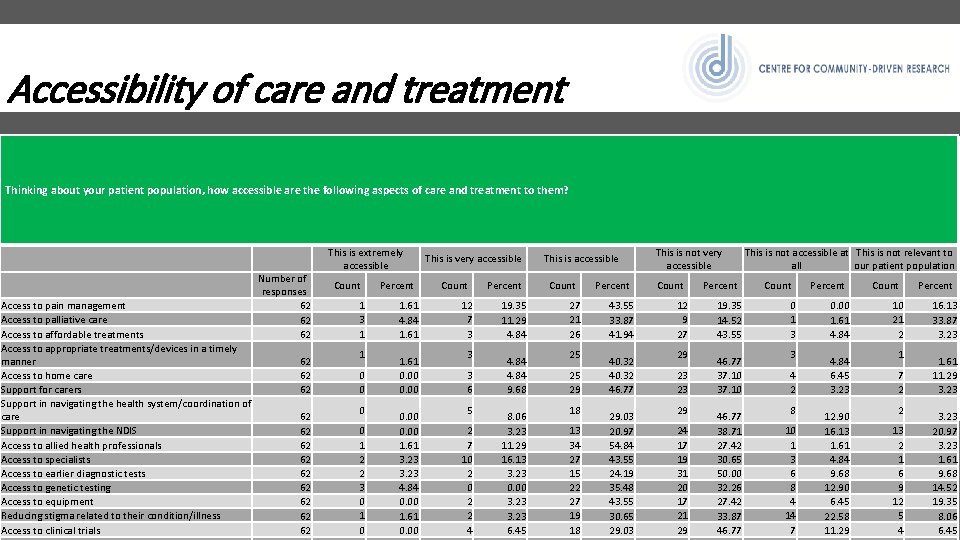
Accessibility of care and treatment Thinking about your patient population, how accessible are the following aspects of care and treatment to them? Access to pain management Access to palliative care Access to affordable treatments Access to appropriate treatments/devices in a timely manner Access to home care Support for carers Support in navigating the health system/coordination of care Support in navigating the NDIS Access to allied health professionals Access to specialists Access to earlier diagnostic tests Access to genetic testing Access to equipment Reducing stigma related to their condition/illness Access to clinical trials Number of responses 62 62 62 62 This is extremely accessible Count 1 3 1 1 0 0 1 2 2 3 0 1 0 Percent 1. 61 4. 84 1. 61 0. 00 1. 61 3. 23 4. 84 0. 00 1. 61 0. 00 This is very accessible Count 12 7 3 3 3 6 5 2 7 10 2 2 4 Percent 19. 35 11. 29 4. 84 9. 68 8. 06 3. 23 11. 29 16. 13 3. 23 0. 00 3. 23 6. 45 This is accessible Count 27 21 26 25 25 29 18 13 34 27 15 22 27 19 18 Percent 43. 55 33. 87 41. 94 40. 32 46. 77 29. 03 20. 97 54. 84 43. 55 24. 19 35. 48 43. 55 30. 65 29. 03 This is not very accessible Count 12 9 27 29 23 23 29 24 17 19 31 20 17 21 29 Percent 19. 35 14. 52 43. 55 46. 77 37. 10 46. 77 38. 71 27. 42 30. 65 50. 00 32. 26 27. 42 33. 87 46. 77 This is not accessible at This is not relevant to all our patient population Count 0 1 3 3 4 2 8 10 1 3 6 8 4 14 7 Percent 0. 00 1. 61 4. 84 6. 45 3. 23 12. 90 16. 13 1. 61 4. 84 9. 68 12. 90 6. 45 22. 58 11. 29 Count 10 21 2 1 7 2 2 13 2 1 6 9 12 5 4 Percent 16. 13 33. 87 3. 23 1. 61 11. 29 3. 23 20. 97 3. 23 1. 61 9. 68 14. 52 19. 35 8. 06 6. 45
AUSTRALIAN PATIENT ORGANISATION NETWORK CONFERENCE THEMES
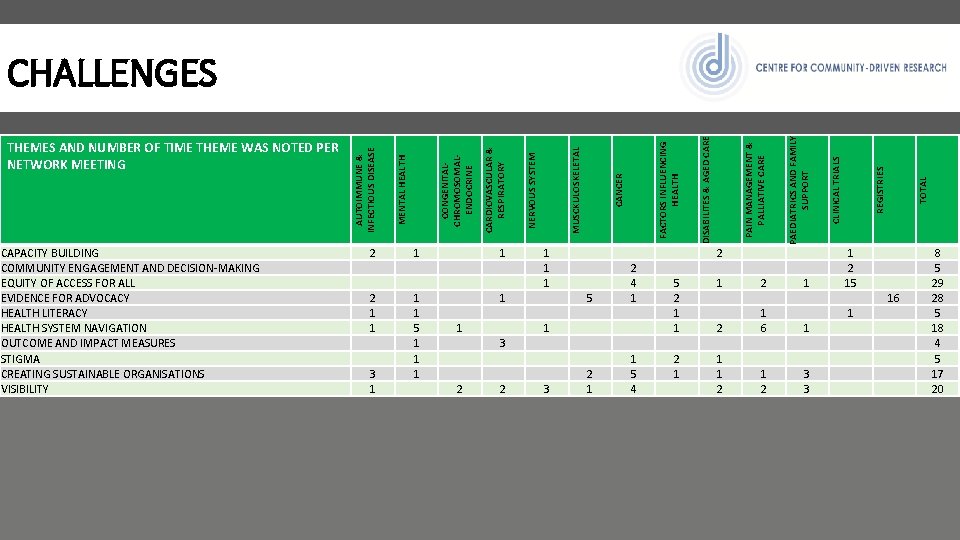
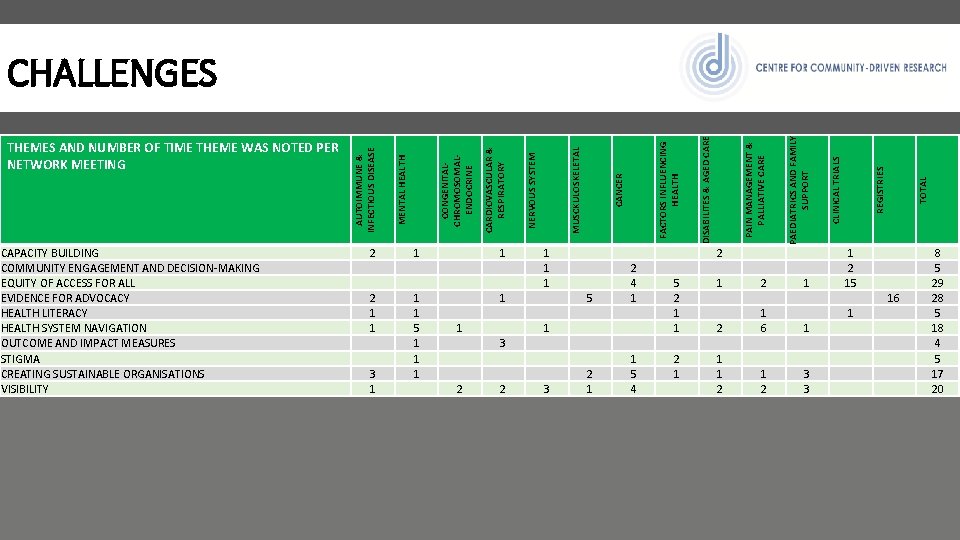
1 2 1 1 3 2 1 1 3 5 2 1 2 4 1 1 5 4 5 2 1 1 2 1 1 2 15 1 TOTAL 1 1 3 3 REGISTRIES 2 1 6 1 2 CLINICAL TRIALS DISABILITES & AGED CARE FACTORS INFLUENCING HEALTH CANCER MUSCKULOSKELETAL NERVOUS SYSTEM CARDIOVASCULAR & RESPIRATORY CONGENITALCHROMOSOMALENDOCRINE 1 1 1 5 1 1 1 PAEDIATRICS AND FAMILY SUPPORT 2 2 1 1 3 1 PAIN MANAGEMENT & PALLIATIVE CARE CAPACITY BUILDING COMMUNITY ENGAGEMENT AND DECISION-MAKING EQUITY OF ACCESS FOR ALL EVIDENCE FOR ADVOCACY HEALTH LITERACY HEALTH SYSTEM NAVIGATION OUTCOME AND IMPACT MEASURES STIGMA CREATING SUSTAINABLE ORGANISATIONS VISIBILITY MENTAL HEALTH THEMES AND NUMBER OF TIME THEME WAS NOTED PER NETWORK MEETING AUTOIMMUNE & INFECTIOUS DISEASE CHALLENGES 16 8 5 29 28 5 18 4 5 17 20
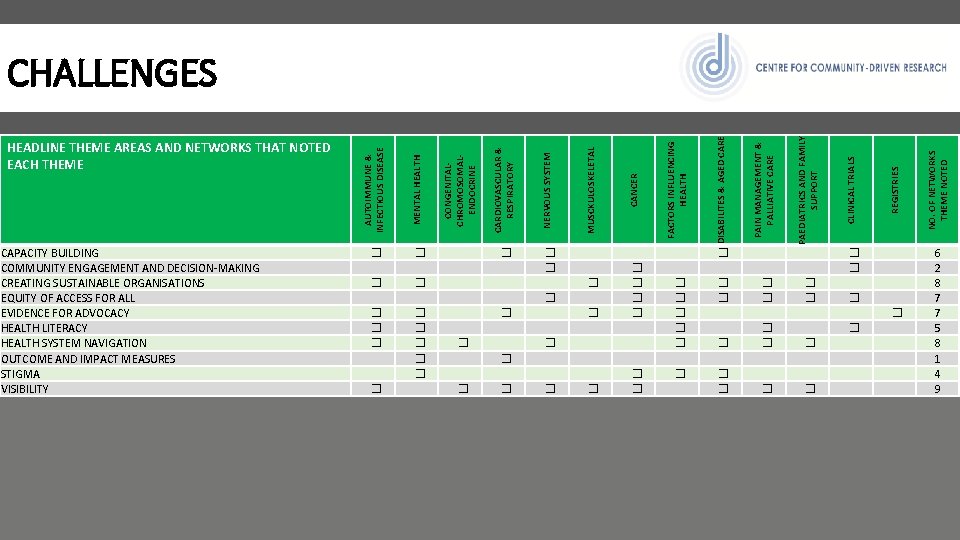
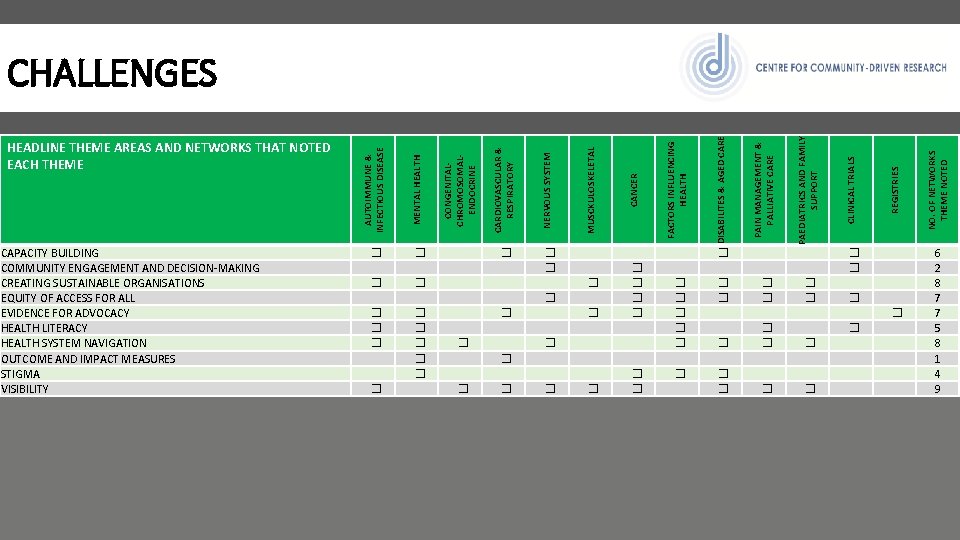
CONGENITALCHROMOSOMALENDOCRINE CARDIOVASCULAR & RESPIRATORY NERVOUS SYSTEM MUSCKULOSKELETAL CANCER FACTORS INFLUENCING HEALTH DISABILITES & AGED CARE PAIN MANAGEMENT & PALLIATIVE CARE PAEDIATRICS AND FAMILY SUPPORT CLINICAL TRIALS REGISTRIES NO. OF NETWORKS THEME NOTED CAPACITY BUILDING COMMUNITY ENGAGEMENT AND DECISION-MAKING CREATING SUSTAINABLE ORGANISATIONS EQUITY OF ACCESS FOR ALL EVIDENCE FOR ADVOCACY HEALTH LITERACY HEALTH SYSTEM NAVIGATION OUTCOME AND IMPACT MEASURES STIGMA VISIBILITY MENTAL HEALTH HEADLINE THEME AREAS AND NETWORKS THAT NOTED EACH THEME AUTOIMMUNE & INFECTIOUS DISEASE CHALLENGES � � � � � � � � � � � � � � � � � � � � � � � � 6 2 8 7 7 5 8 1 4 9
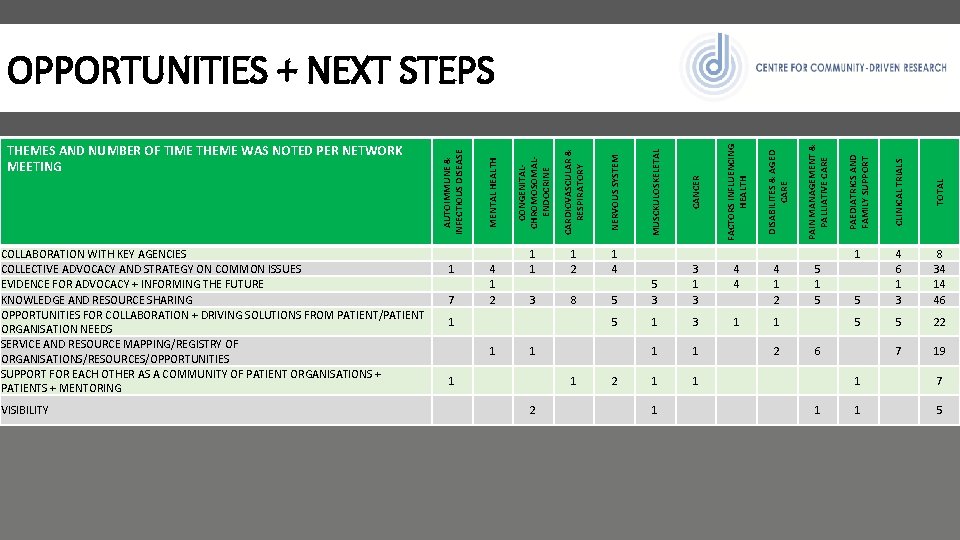
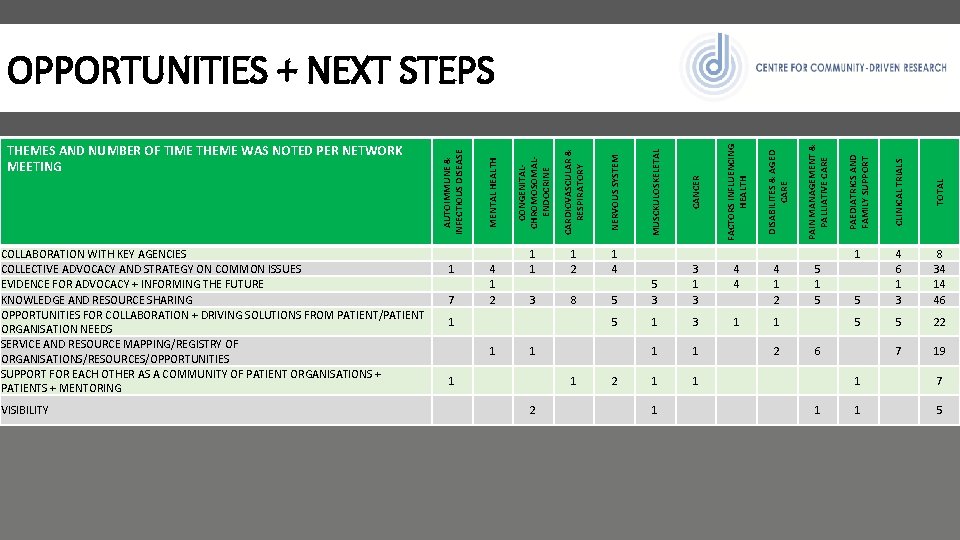
OPPORTUNITIES + NEXT STEPS AUTOIMMUNE & INFECTIOUS DISEASE MENTAL HEALTH CONGENITALCHROMOSOMALENDOCRINE CARDIOVASCULAR & RESPIRATORY NERVOUS SYSTEM MUSCKULOSKELETAL CANCER FACTORS INFLUENCING HEALTH DISABILITES & AGED CARE PAIN MANAGEMENT & PALLIATIVE CARE PAEDIATRICS AND FAMILY SUPPORT CLINICAL TRIALS TOTAL THEMES AND NUMBER OF TIME THEME WAS NOTED PER NETWORK MEETING COLLABORATION WITH KEY AGENCIES COLLECTIVE ADVOCACY AND STRATEGY ON COMMON ISSUES EVIDENCE FOR ADVOCACY + INFORMING THE FUTURE KNOWLEDGE AND RESOURCE SHARING OPPORTUNITIES FOR COLLABORATION + DRIVING SOLUTIONS FROM PATIENT/PATIENT ORGANISATION NEEDS SERVICE AND RESOURCE MAPPING/REGISTRY OF ORGANISATIONS/RESOURCES/OPPORTUNITIES SUPPORT FOR EACH OTHER AS A COMMUNITY OF PATIENT ORGANISATIONS + PATIENTS + MENTORING 1 7 4 1 2 1 1 3 1 2 8 1 4 5 5 3 3 1 3 4 4 4 1 2 5 1 5 4 6 1 3 8 34 14 46 1 5 1 3 1 1 5 5 22 1 1 2 6 7 19 1 1 2 1 1 1 7 VISIBILITY 2 1 1 1 5
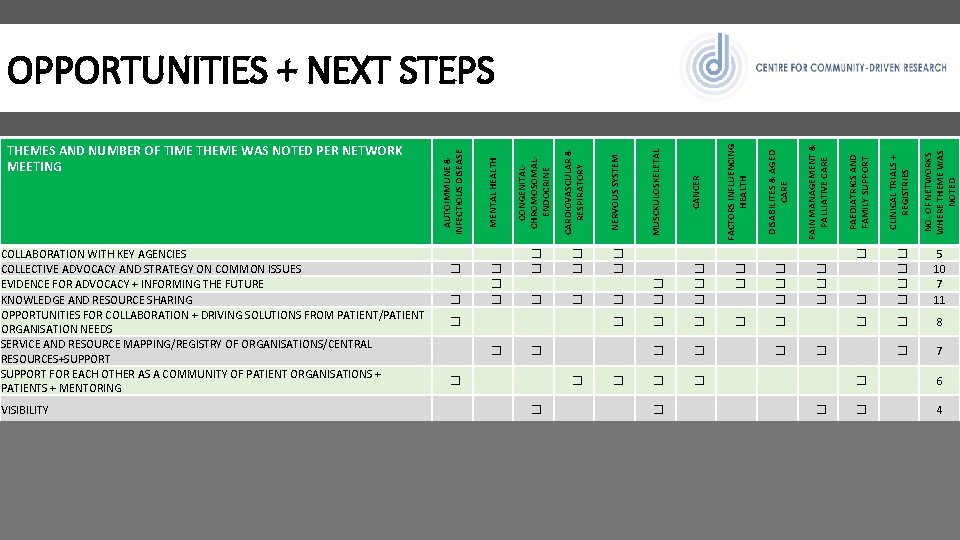
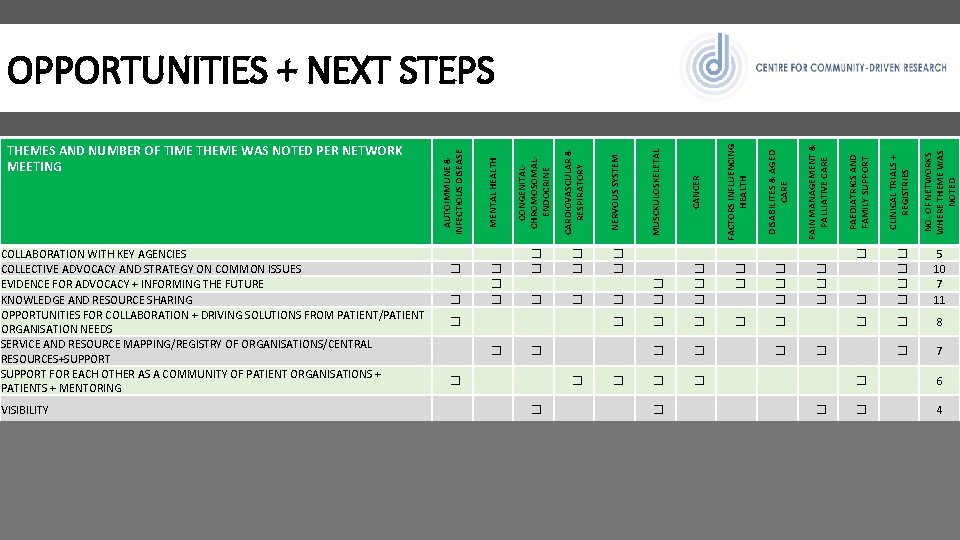
OPPORTUNITIES + NEXT STEPS AUTOIMMUNE & INFECTIOUS DISEASE MENTAL HEALTH CONGENITALCHROMOSOMALENDOCRINE CARDIOVASCULAR & RESPIRATORY NERVOUS SYSTEM MUSCKULOSKELETAL CANCER FACTORS INFLUENCING HEALTH DISABILITES & AGED CARE PAIN MANAGEMENT & PALLIATIVE CARE PAEDIATRICS AND FAMILY SUPPORT CLINICAL TRIALS + REGISTRIES NO. OF NETWORKS WHERE THEME WAS NOTED THEMES AND NUMBER OF TIME THEME WAS NOTED PER NETWORK MEETING COLLABORATION WITH KEY AGENCIES COLLECTIVE ADVOCACY AND STRATEGY ON COMMON ISSUES EVIDENCE FOR ADVOCACY + INFORMING THE FUTURE KNOWLEDGE AND RESOURCE SHARING OPPORTUNITIES FOR COLLABORATION + DRIVING SOLUTIONS FROM PATIENT/PATIENT ORGANISATION NEEDS SERVICE AND RESOURCE MAPPING/REGISTRY OF ORGANISATIONS/CENTRAL RESOURCES+SUPPORT FOR EACH OTHER AS A COMMUNITY OF PATIENT ORGANISATIONS + PATIENTS + MENTORING � � � � � � � � � � � � 5 10 7 11 � � � � � 8 � � � � � 7 � � 6 VISIBILITY � � � � 4
AUSTRALIAN PATIENT ORGANISATION NETWORK PROPOSED PROGRAM OF WORK
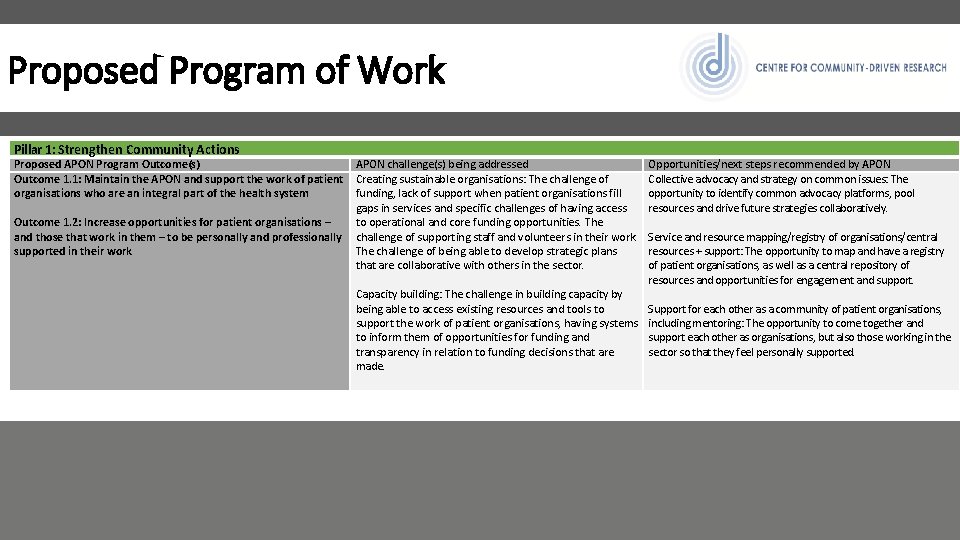
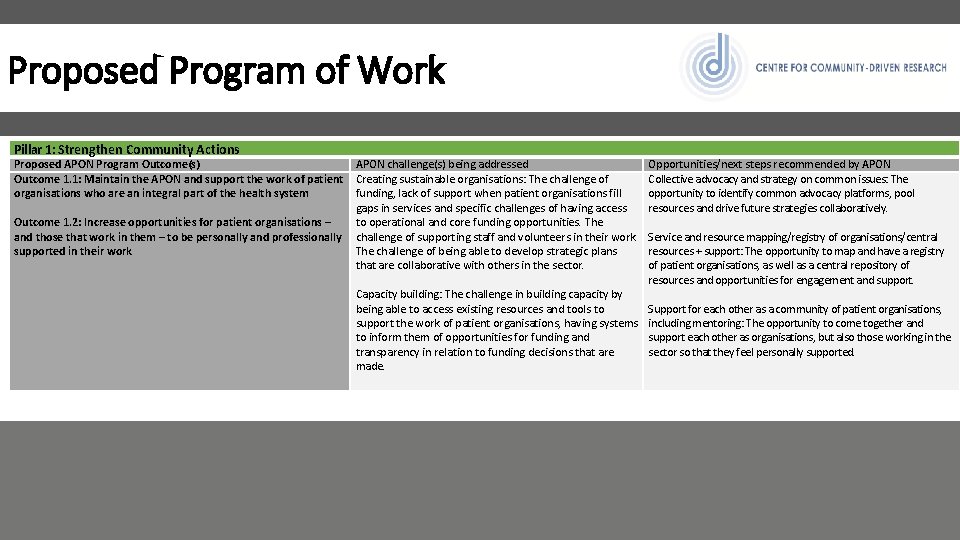
Proposed Program of Work Pillar 1: Strengthen Community Actions Proposed APON Program Outcome(s) Outcome 1. 1: Maintain the APON and support the work of patient organisations who are an integral part of the health system Outcome 1. 2: Increase opportunities for patient organisations – and those that work in them – to be personally and professionally supported in their work APON challenge(s) being addressed Creating sustainable organisations: The challenge of funding, lack of support when patient organisations fill gaps in services and specific challenges of having access to operational and core funding opportunities. The challenge of supporting staff and volunteers in their work. The challenge of being able to develop strategic plans that are collaborative with others in the sector. Capacity building: The challenge in building capacity by being able to access existing resources and tools to support the work of patient organisations, having systems to inform them of opportunities for funding and transparency in relation to funding decisions that are made. Opportunities/next steps recommended by APON Collective advocacy and strategy on common issues: The opportunity to identify common advocacy platforms, pool resources and drive future strategies collaboratively. Service and resource mapping/registry of organisations/central resources + support: The opportunity to map and have a registry of patient organisations, as well as a central repository of resources and opportunities for engagement and support. Support for each other as a community of patient organisations, including mentoring: The opportunity to come together and support each other as organisations, but also those working in the sector so that they feel personally supported.
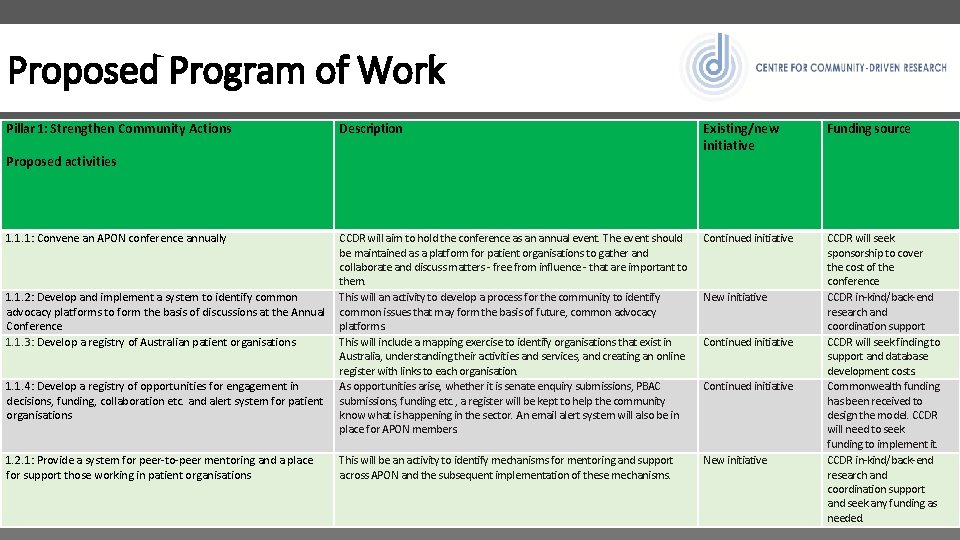
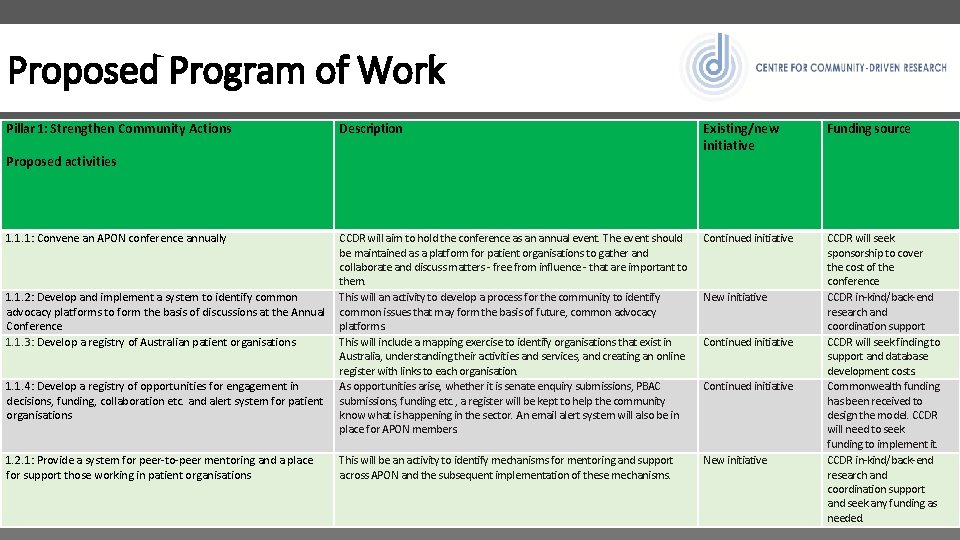
Proposed Program of Work Pillar 1: Strengthen Community Actions Description Existing/new initiative Funding source CCDR will aim to hold the conference as an annual event. The event should be maintained as a platform for patient organisations to gather and collaborate and discuss matters - free from influence - that are important to them. 1. 1. 2: Develop and implement a system to identify common This will an activity to develop a process for the community to identify advocacy platforms to form the basis of discussions at the Annual common issues that may form the basis of future, common advocacy Conference platforms. 1. 1. 3: Develop a registry of Australian patient organisations This will include a mapping exercise to identify organisations that exist in Australia, understanding their activities and services, and creating an online register with links to each organisation. 1. 1. 4: Develop a registry of opportunities for engagement in As opportunities arise, whether it is senate enquiry submissions, PBAC decisions, funding, collaboration etc. and alert system for patient submissions, funding etc. , a register will be kept to help the community organisations know what is happening in the sector. An email alert system will also be in place for APON members. Continued initiative 1. 2. 1: Provide a system for peer-to-peer mentoring and a place for support those working in patient organisations New initiative CCDR will seek sponsorship to cover the cost of the conference CCDR in-kind/back-end research and coordination support CCDR will seek finding to support and database development costs. Commonwealth funding has been received to design the model. CCDR will need to seek funding to implement it. CCDR in-kind/back-end research and coordination support and seek any funding as needed. Proposed activities 1. 1. 1: Convene an APON conference annually This will be an activity to identify mechanisms for mentoring and support across APON and the subsequent implementation of these mechanisms. New initiative Continued initiative

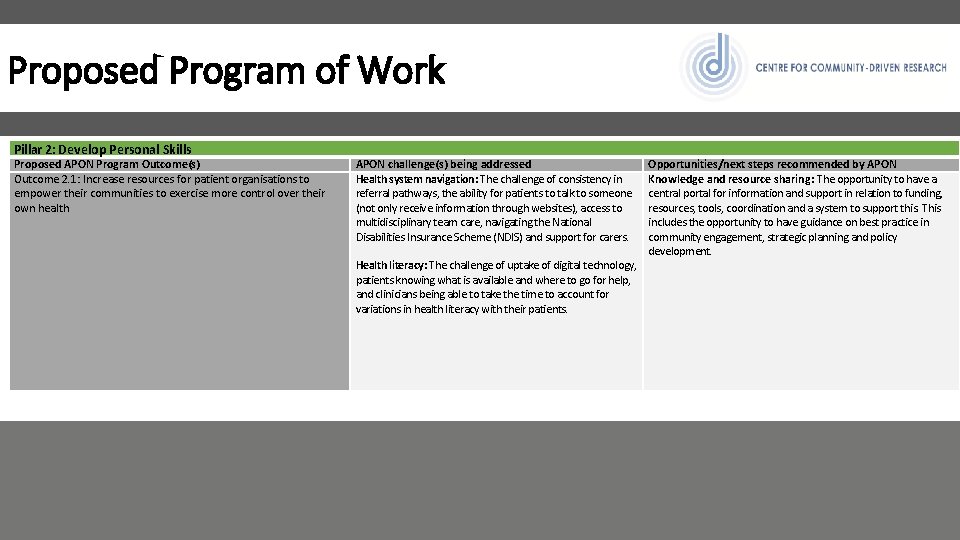
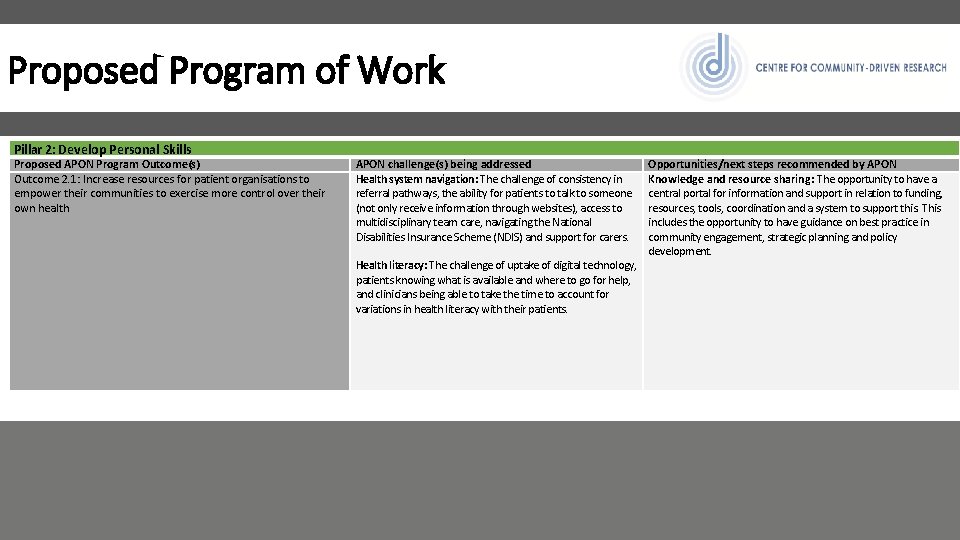
Proposed Program of Work Pillar 2: Develop Personal Skills Proposed APON Program Outcome(s) Outcome 2. 1: Increase resources for patient organisations to empower their communities to exercise more control over their own health APON challenge(s) being addressed Health system navigation: The challenge of consistency in referral pathways, the ability for patients to talk to someone (not only receive information through websites), access to multidisciplinary team care, navigating the National Disabilities Insurance Scheme (NDIS) and support for carers. Health literacy: The challenge of uptake of digital technology, patients knowing what is available and where to go for help, and clinicians being able to take the time to account for variations in health literacy with their patients. Opportunities/next steps recommended by APON Knowledge and resource sharing: The opportunity to have a central portal for information and support in relation to funding, resources, tools, coordination and a system to support this. This includes the opportunity to have guidance on best practice in community engagement, strategic planning and policy development.

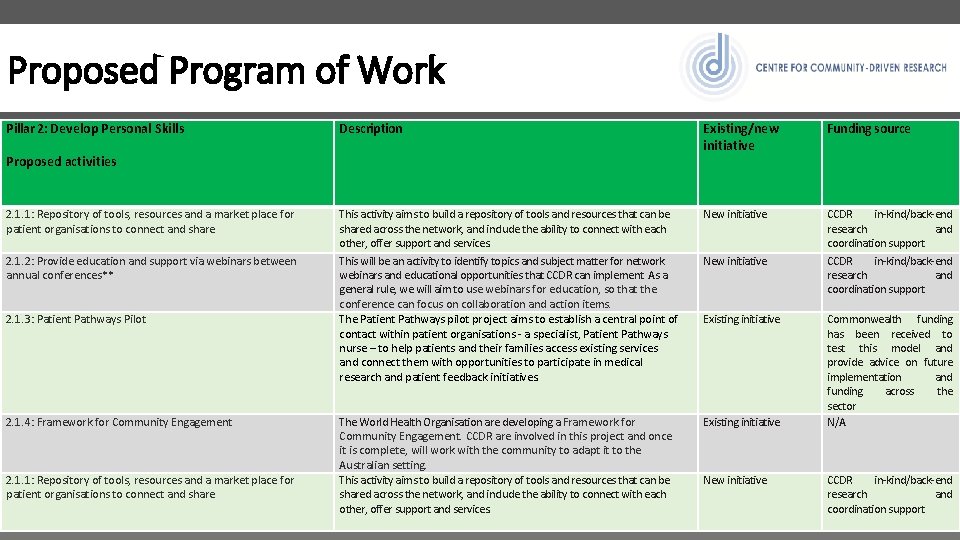
Proposed Program of Work Pillar 2: Develop Personal Skills Description Existing/new initiative Funding source This activity aims to build a repository of tools and resources that can be shared across the network, and include the ability to connect with each other, offer support and services. This will be an activity to identify topics and subject matter for network webinars and educational opportunities that CCDR can implement. As a general rule, we will aim to use webinars for education, so that the conference can focus on collaboration and action items. The Patient Pathways pilot project aims to establish a central point of contact within patient organisations - a specialist, Patient Pathways nurse – to help patients and their families access existing services and connect them with opportunities to participate in medical research and patient feedback initiatives. New initiative CCDR in-kind/back-end research and coordination support The World Health Organisation are developing a Framework for Community Engagement. CCDR are involved in this project and once it is complete, will work with the community to adapt it to the Australian setting. Existing initiative Proposed activities 2. 1. 1: Repository of tools, resources and a market place for patient organisations to connect and share 2. 1. 2: Provide education and support via webinars between annual conferences** 2. 1. 3: Patient Pathways Pilot 2. 1. 4: Framework for Community Engagement New initiative Existing initiative Commonwealth funding has been received to test this model and provide advice on future implementation and funding across the sector N/A
Proposed Program of Work Pillar 2: Develop Personal Skills Proposed APON Program Outcome(s) Outcome 2. 1: Increase resources for patient organisations to empower their communities to exercise more control over their own health APON challenge(s) being addressed Health system navigation: The challenge of consistency in referral pathways, the ability for patients to talk to someone (not only receive information through websites), access to multidisciplinary team care, navigating the National Disabilities Insurance Scheme (NDIS) and support for carers. Health literacy: The challenge of uptake of digital technology, patients knowing what is available and where to go for help, and clinicians being able to take the time to account for variations in health literacy with their patients. Opportunities/next steps recommended by APON Knowledge and resource sharing: The opportunity to have a central portal for information and support in relation to funding, resources, tools, coordination and a system to support this. This includes the opportunity to have guidance on best practice in community engagement, strategic planning and policy development.
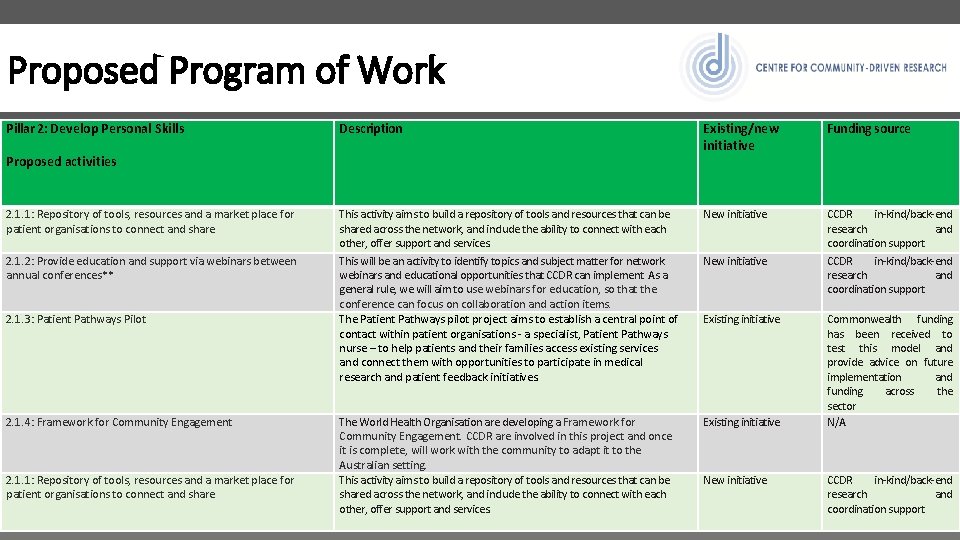
Proposed Program of Work Pillar 2: Develop Personal Skills Description Existing/new initiative Funding source This activity aims to build a repository of tools and resources that can be shared across the network, and include the ability to connect with each other, offer support and services. This will be an activity to identify topics and subject matter for network webinars and educational opportunities that CCDR can implement. As a general rule, we will aim to use webinars for education, so that the conference can focus on collaboration and action items. The Patient Pathways pilot project aims to establish a central point of contact within patient organisations - a specialist, Patient Pathways nurse – to help patients and their families access existing services and connect them with opportunities to participate in medical research and patient feedback initiatives. New initiative CCDR in-kind/back-end research and coordination support The World Health Organisation are developing a Framework for Community Engagement. CCDR are involved in this project and once it is complete, will work with the community to adapt it to the Australian setting. This activity aims to build a repository of tools and resources that can be shared across the network, and include the ability to connect with each other, offer support and services. Existing initiative Proposed activities 2. 1. 1: Repository of tools, resources and a market place for patient organisations to connect and share 2. 1. 2: Provide education and support via webinars between annual conferences** 2. 1. 3: Patient Pathways Pilot 2. 1. 4: Framework for Community Engagement 2. 1. 1: Repository of tools, resources and a market place for patient organisations to connect and share New initiative Existing initiative New initiative Commonwealth funding has been received to test this model and provide advice on future implementation and funding across the sector N/A CCDR in-kind/back-end research and coordination support
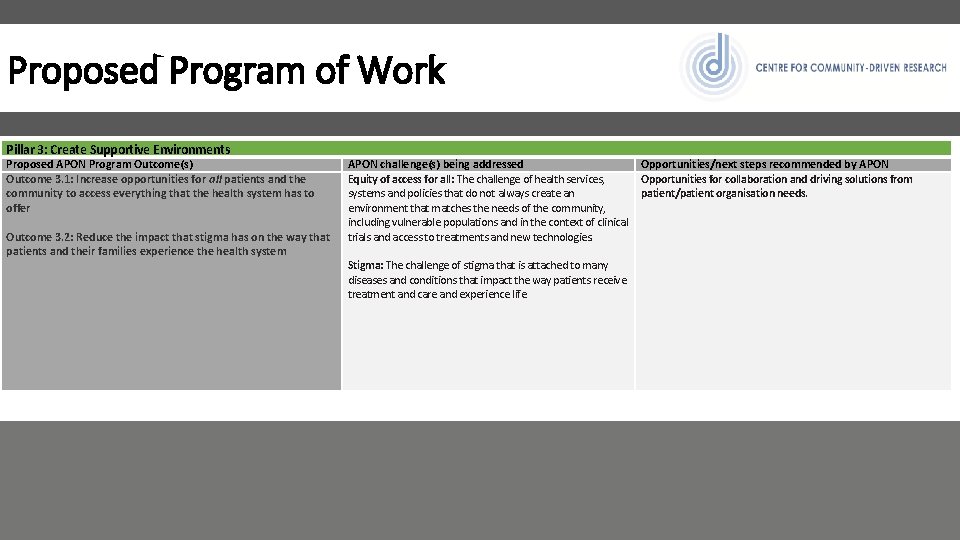
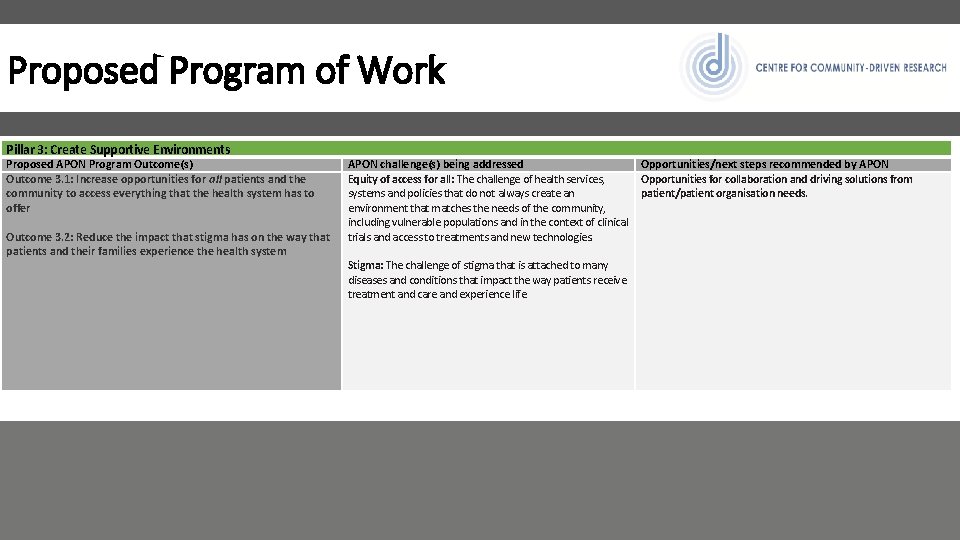
Proposed Program of Work Pillar 3: Create Supportive Environments Proposed APON Program Outcome(s) Outcome 3. 1: Increase opportunities for all patients and the community to access everything that the health system has to offer Outcome 3. 2: Reduce the impact that stigma has on the way that patients and their families experience the health system APON challenge(s) being addressed Opportunities/next steps recommended by APON Equity of access for all: The challenge of health services, Opportunities for collaboration and driving solutions from systems and policies that do not always create an patient/patient organisation needs. environment that matches the needs of the community, including vulnerable populations and in the context of clinical trials and access to treatments and new technologies. Stigma: The challenge of stigma that is attached to many diseases and conditions that impact the way patients receive treatment and care and experience life.

Proposed Program of Work Pillar 3: Create Supportive Environments Description Proposed activities 3. 1. 1: Create a mechanism to ensure that equitable access is addressed in each of the APON activities and program of work** Equitable access to treatments, services, support and information is a concern to many organisations. This includes equitable access for vulnerable populations but also equitable and systematic access to mental health services, pain management and palliative care services. This will be an activity that has a focus on vulnerable populations and those in vulnerable situations, and how we as a community can better support those most in need. 3. 2. 1: Develop research question(s) to implements across a range Through the PEEK program, CCDR routinely talk with patients about their of disease areas in relation to the impact of stigma** experience in the health system. This activity will result in the addition of a question to understand which patient groups experience stigma, how this affects the treatment and care they receive, and their life. Existing/new initiative Funding source New initiative CCDR in-kind/back-end research and coordination support New initiative/Existing platform CCDR in-kind/back-end research and coordination support
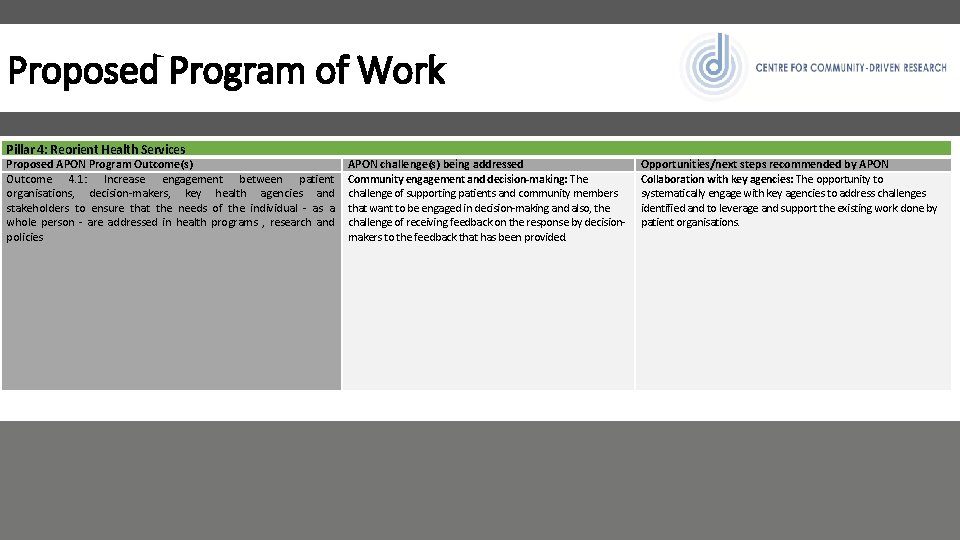
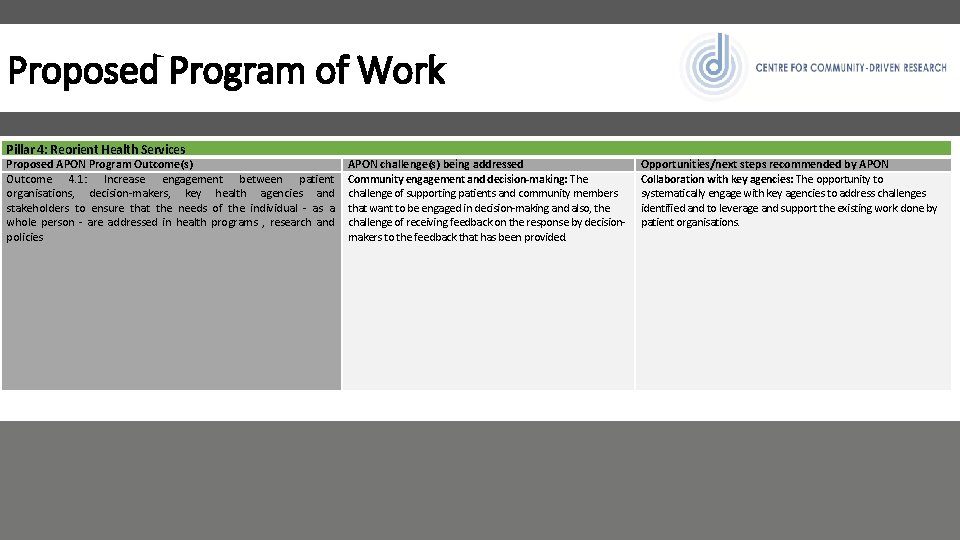
Proposed Program of Work Pillar 4: Reorient Health Services Proposed APON Program Outcome(s) Outcome 4. 1: Increase engagement between patient organisations, decision-makers, key health agencies and stakeholders to ensure that the needs of the individual - as a whole person - are addressed in health programs , research and policies APON challenge(s) being addressed Community engagement and decision-making: The challenge of supporting patients and community members that want to be engaged in decision-making and also, the challenge of receiving feedback on the response by decisionmakers to the feedback that has been provided. Opportunities/next steps recommended by APON Collaboration with key agencies: The opportunity to systematically engage with key agencies to address challenges identified and to leverage and support the existing work done by patient organisations.
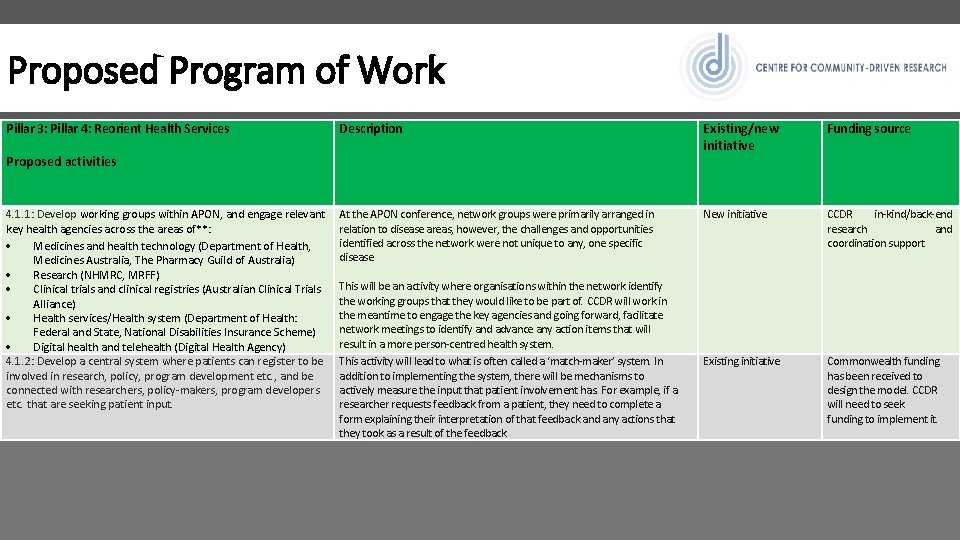
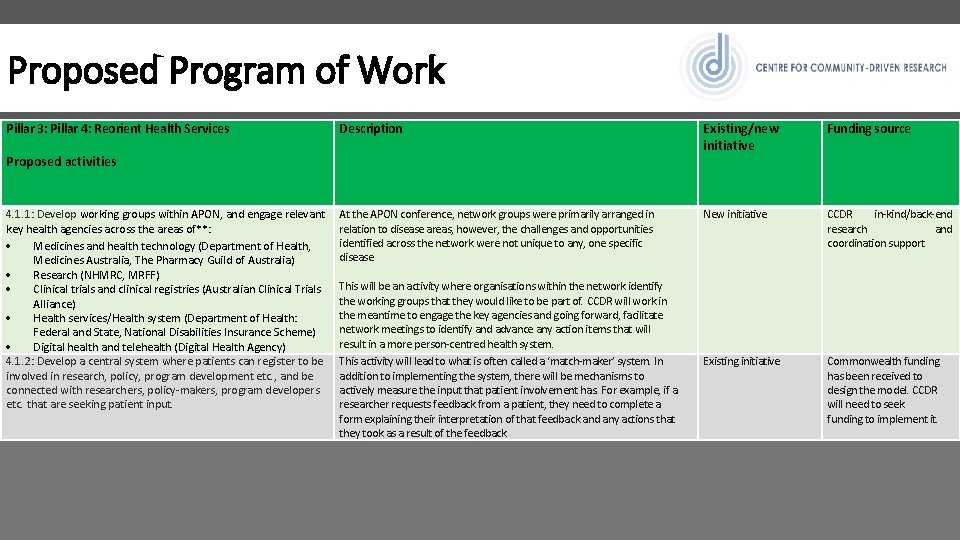
Proposed Program of Work Pillar 3: Pillar 4: Reorient Health Services Description Existing/new initiative Funding source At the APON conference, network groups were primarily arranged in relation to disease areas, however, the challenges and opportunities identified across the network were not unique to any, one specific disease. This will be an activity where organisations within the network identify the working groups that they would like to be part of. CCDR will work in the meantime to engage the key agencies and going forward, facilitate network meetings to identify and advance any action items that will result in a more person-centred health system. This activity will lead to what is often called a ‘match-maker’ system. In addition to implementing the system, there will be mechanisms to actively measure the input that patient involvement has. For example, if a researcher requests feedback from a patient, they need to complete a form explaining their interpretation of that feedback and any actions that they took as a result of the feedback. New initiative CCDR in-kind/back-end research and coordination support. Existing initiative Commonwealth funding has been received to design the model. CCDR will need to seek funding to implement it. Proposed activities 4. 1. 1: Develop working groups within APON, and engage relevant key health agencies across the areas of**: Medicines and health technology (Department of Health, Medicines Australia, The Pharmacy Guild of Australia) Research (NHMRC, MRFF) Clinical trials and clinical registries (Australian Clinical Trials Alliance) Health services/Health system (Department of Health: Federal and State, National Disabilities Insurance Scheme) Digital health and telehealth (Digital Health Agency) 4. 1. 2: Develop a central system where patients can register to be involved in research, policy, program development etc. , and be connected with researchers, policy-makers, program developers etc. that are seeking patient input.
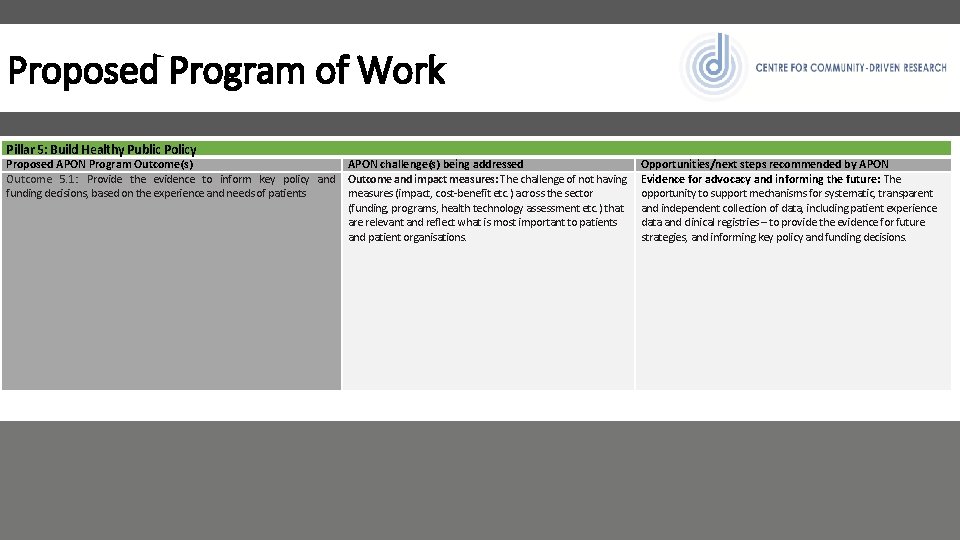
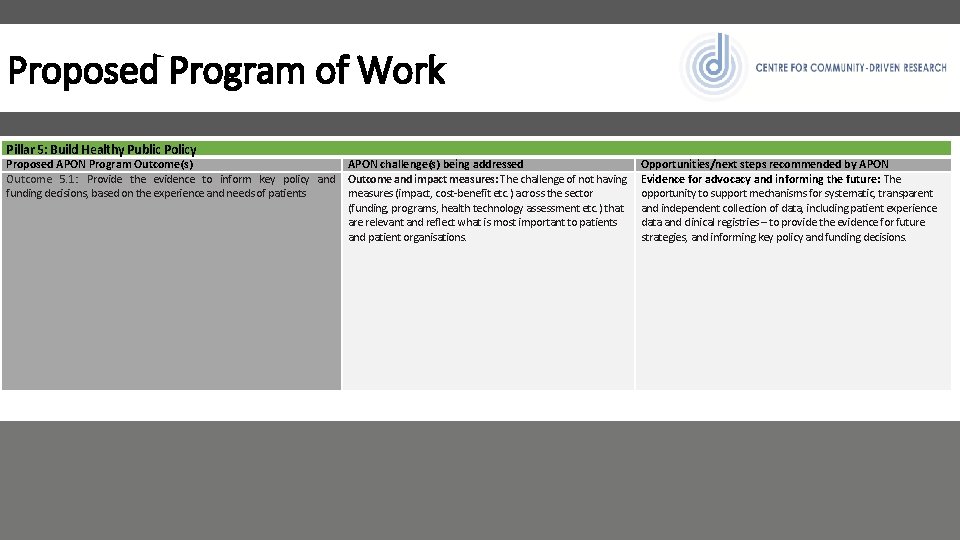
Proposed Program of Work Pillar 5: Build Healthy Public Policy Proposed APON Program Outcome(s) APON challenge(s) being addressed Outcome 5. 1: Provide the evidence to inform key policy and Outcome and impact measures: The challenge of not having funding decisions, based on the experience and needs of patients measures (impact, cost-benefit etc. ) across the sector (funding, programs, health technology assessment etc. ) that are relevant and reflect what is most important to patients and patient organisations. Opportunities/next steps recommended by APON Evidence for advocacy and informing the future: The opportunity to support mechanisms for systematic, transparent and independent collection of data, including patient experience data and clinical registries – to provide the evidence for future strategies, and informing key policy and funding decisions.

Proposed Program of Work Pillar 3: Pillar 4: Reorient Health Services Description Proposed activities 5. 1. 1: Develop health program and research impact measures that reflect the values that are important to patients and patient organisations This will be an activity where CCDR design a process to identify the values that are important to patients and patient organisations, and then design and test evaluation measure that reflect these values. APON members will be engaged in this process from start to finish. 5. 1. 2: Prospective research methodologies and pilots to test best CCDR already run pilot projects and activities to test approaches to practice community engagement systems in various contexts community engagement in decision-making. As we test these including health technology assessment, health services, research approaches, we will report back to the community on what has and community-based programs has not worked. Where approached have bee successful, we will aim to develop templates so that others can adapt these approaches. We will also be open to hearing from APON about other pilot projects that address their needs. 5. 1. 3: Develop and validate levels of evidence for patient Just as we have levels of evidence for clinical data to guide clinical experience, patient feedback and real-world data guidelines for example, the concept of this activity is to develop levels of evidence for patient experience, patient feedback and real-world data. This will lead to more transparency in the use of this kind of data in decision-making. 5. 1. 4: PEEK repository of patient experience and expectation data and integration of this data into decision-making processes Understanding patient referral systems and how patients travel through the health system, including access to support from patient organisations. This also includes asking what they expect from future treatments, care, support and information, what they have appreciated in the health system and what their message to decision-makers about their condition would be. The PEEK protocol can be implemented in any disease area so that we have a systematic approach to collecting patient experience data. Existing/new initiative Funding source New initiative CCDR in-kind/back-end research and coordination support New initiative/Existing platform CCDR Existing CCDR-led initiative in collaboration with the World Health Organisation and University of Warwick Existing CCDR initiative CCDR funding to develop the methodology. Funding will be sought for the validation process and future implementation. CCDR currently apply for ad-hoc funding (grants and sponsorships). CCDR will seek funding so that studies can be done more equitably across disease areas.
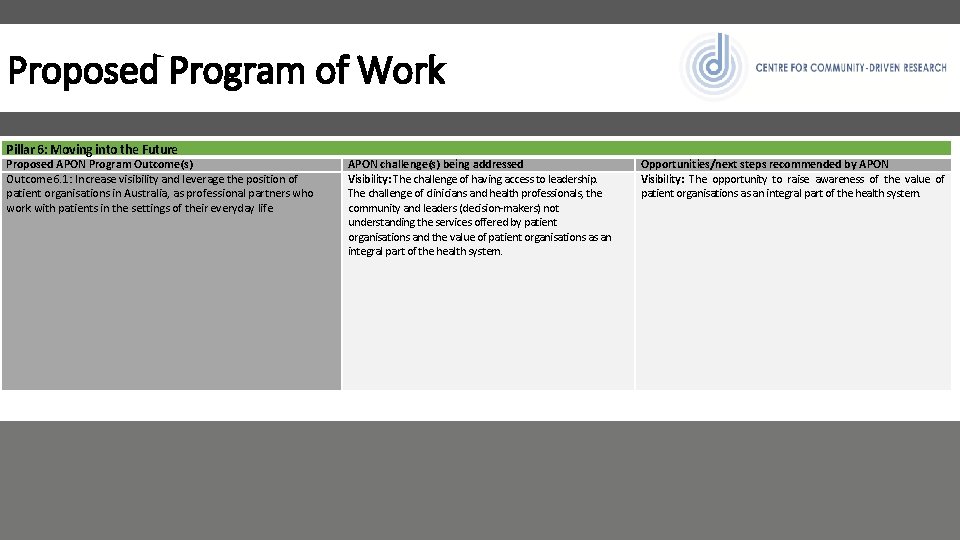
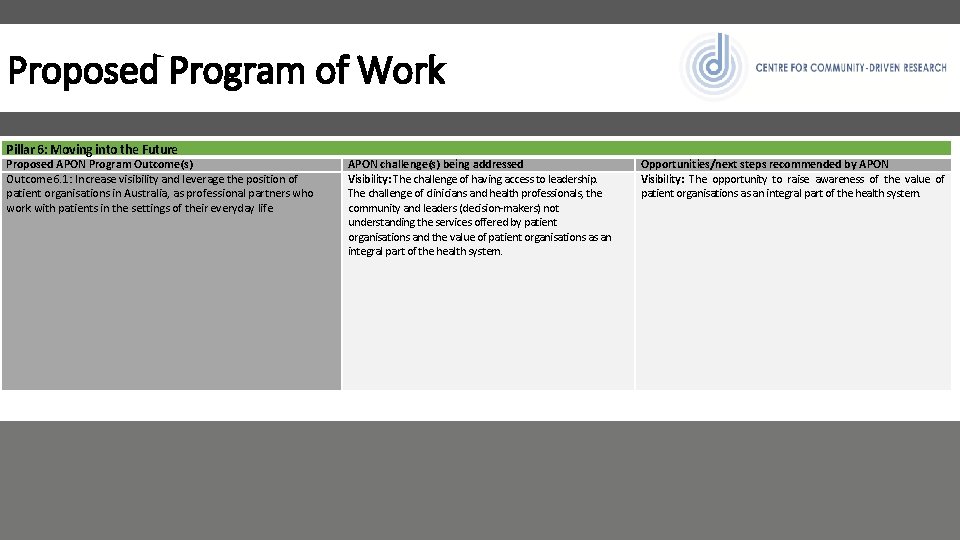
Proposed Program of Work Pillar 6: Moving into the Future Proposed APON Program Outcome(s) Outcome 6. 1: Increase visibility and leverage the position of patient organisations in Australia, as professional partners who work with patients in the settings of their everyday life APON challenge(s) being addressed Visibility: The challenge of having access to leadership. The challenge of clinicians and health professionals, the community and leaders (decision-makers) not understanding the services offered by patient organisations and the value of patient organisations as an integral part of the health system. Opportunities/next steps recommended by APON Visibility: The opportunity to raise awareness of the value of patient organisations as an integral part of the health system.
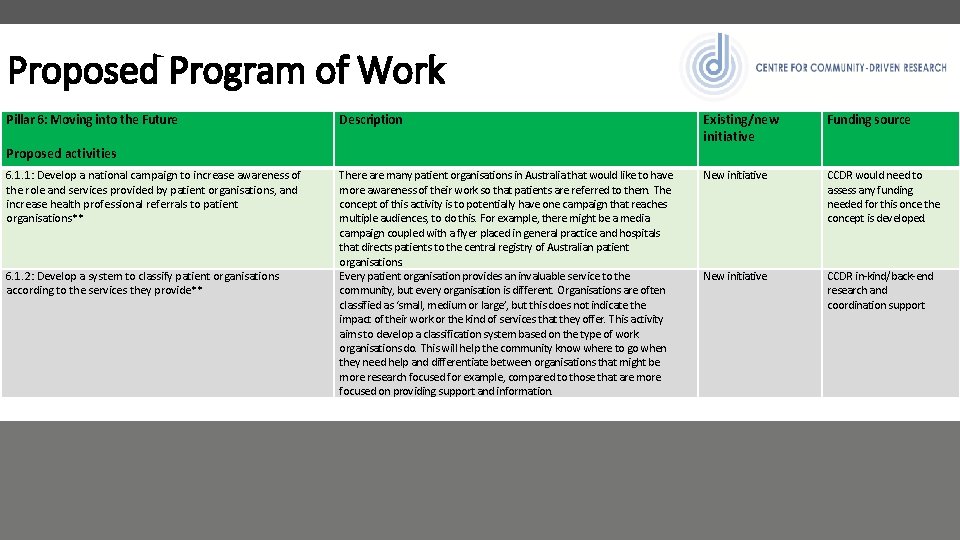
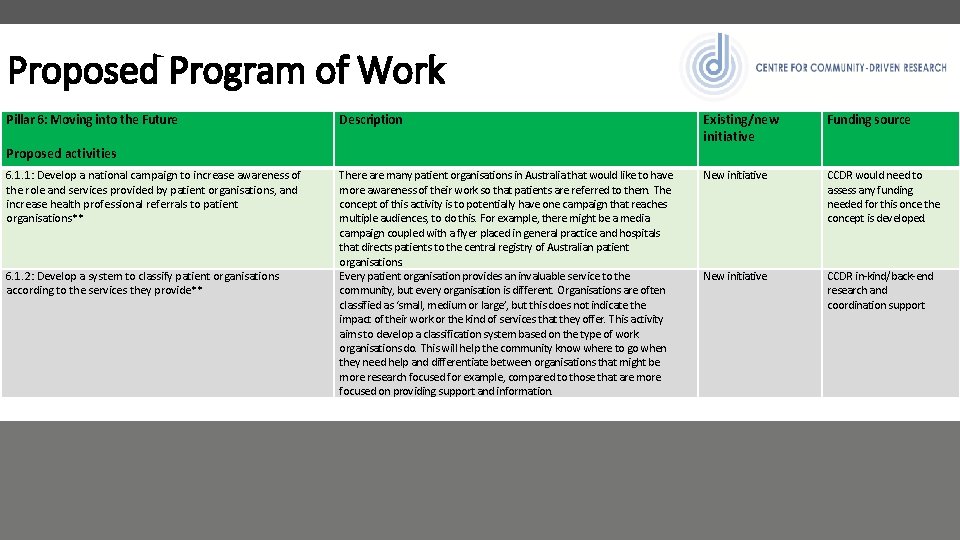
Proposed Program of Work Pillar 6: Moving into the Future Description Existing/new initiative Funding source There are many patient organisations in Australia that would like to have more awareness of their work so that patients are referred to them. The concept of this activity is to potentially have one campaign that reaches multiple audiences, to do this. For example, there might be a media campaign coupled with a flyer placed in general practice and hospitals that directs patients to the central registry of Australian patient organisations. Every patient organisation provides an invaluable service to the community, but every organisation is different. Organisations are often classified as ‘small, medium or large’, but this does not indicate the impact of their work or the kind of services that they offer. This activity aims to develop a classification system based on the type of work organisations do. This will help the community know where to go when they need help and differentiate between organisations that might be more research focused for example, compared to those that are more focused on providing support and information. New initiative CCDR would need to assess any funding needed for this once the concept is developed. New initiative CCDR in-kind/back-end research and coordination support Proposed activities 6. 1. 1: Develop a national campaign to increase awareness of the role and services provided by patient organisations, and increase health professional referrals to patient organisations** 6. 1. 2: Develop a system to classify patient organisations according to the services they provide**
 Australian labyrinth network
Australian labyrinth network Patient 2 patient
Patient 2 patient Central european lung cancer patient network
Central european lung cancer patient network Currents waves
Currents waves Performance and development framework
Performance and development framework What are the 13 australian privacy principles?
What are the 13 australian privacy principles? Australian primary health care research institute
Australian primary health care research institute Australian gothic definition
Australian gothic definition When did the gold rush start and end in australia
When did the gold rush start and end in australia Australian blueprint for career development
Australian blueprint for career development Stair nosing australian standards
Stair nosing australian standards Australian physical features
Australian physical features Australian vs new zealand accent
Australian vs new zealand accent Australian standards for texture modified foods and fluids
Australian standards for texture modified foods and fluids Information and communication technology capability.
Information and communication technology capability. Funeral service of the unknown australian soldier
Funeral service of the unknown australian soldier Australian desert animals
Australian desert animals Australian business arts foundation
Australian business arts foundation Australian society for simulation in healthcare
Australian society for simulation in healthcare Australian nursing and midwifery education centre
Australian nursing and midwifery education centre Ratel army
Ratel army Australian antarctic data centre
Australian antarctic data centre Australian ruokakulttuuri wikipedia
Australian ruokakulttuuri wikipedia Literacy progressions australian curriculum
Literacy progressions australian curriculum Australian flag stars represent
Australian flag stars represent Australian philanthropic services
Australian philanthropic services Australian aboriginal creation myth
Australian aboriginal creation myth Aehrc
Aehrc Australian curriculum framework for junior doctors
Australian curriculum framework for junior doctors New zealand vs australian accent
New zealand vs australian accent Australian barcode
Australian barcode Defence school of languages
Defence school of languages The australian connection zusammenfassung kapitel 7
The australian connection zusammenfassung kapitel 7 Australian data cube
Australian data cube Australian bomb data centre
Australian bomb data centre Australian curriculum lessons
Australian curriculum lessons Aboriginal art platypus outline
Aboriginal art platypus outline