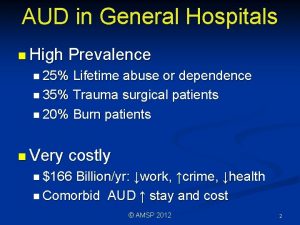
AUD in General Hospitals n High Prevalence n






![Withdrawal Tx n Benzodiazepines (e. g. diazepam [Valium]) n. Correct transmitter problems n. Day Withdrawal Tx n Benzodiazepines (e. g. diazepam [Valium]) n. Correct transmitter problems n. Day](https://slidetodoc.com/presentation_image_h/12e89761a371315fd0858825aca96267/image-23.jpg)


- Slides: 44
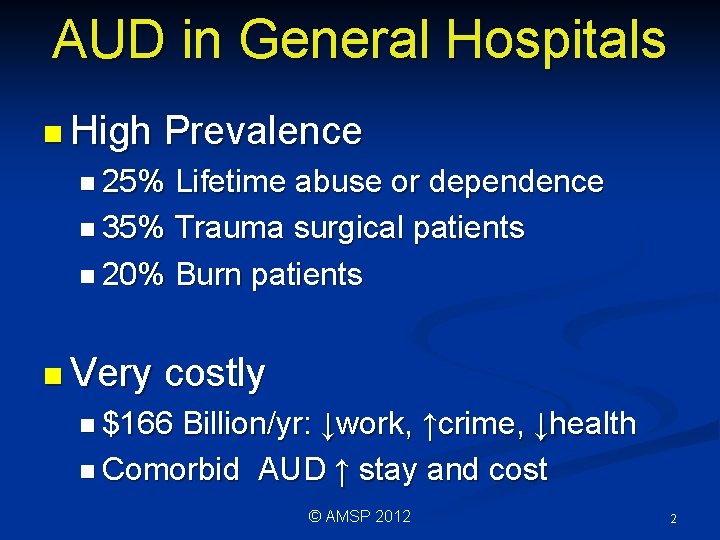
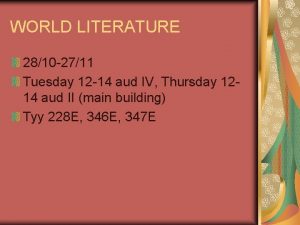
AUD in General Hospitals n High Prevalence n 25% Lifetime abuse or dependence n 35% Trauma surgical patients n 20% Burn patients n Very costly n $166 Billion/yr: ↓work, ↑crime, ↓health n Comorbid AUD ↑ stay and cost © AMSP 2012 2

↑ Medical Complications n. Alcohol n↓ interacts with meds General health n. Poor nutrition © AMSP 2012 3
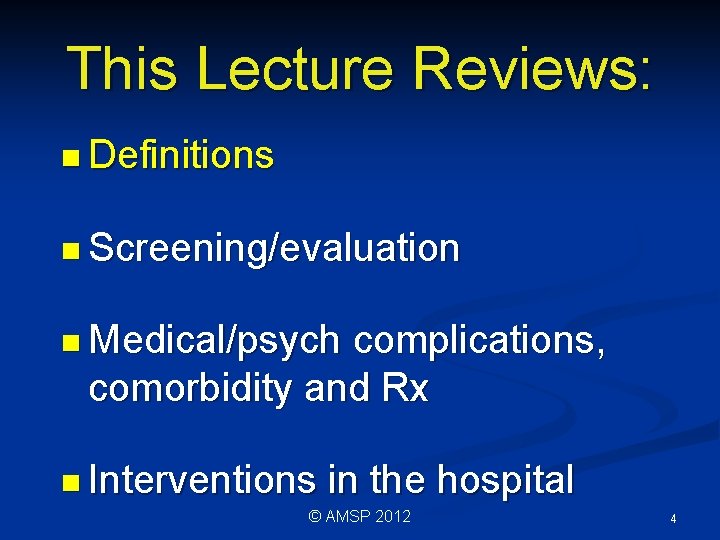
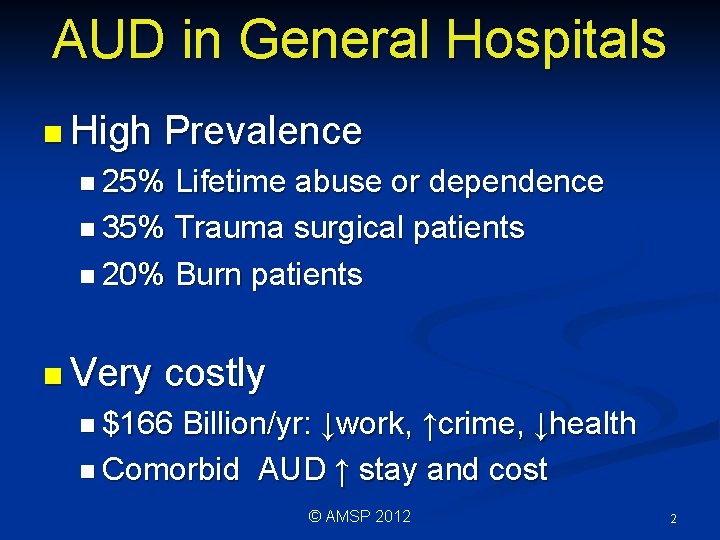
This Lecture Reviews: n Definitions n Screening/evaluation n Medical/psych complications, comorbidity and Rx n Interventions in the hospital © AMSP 2012 4
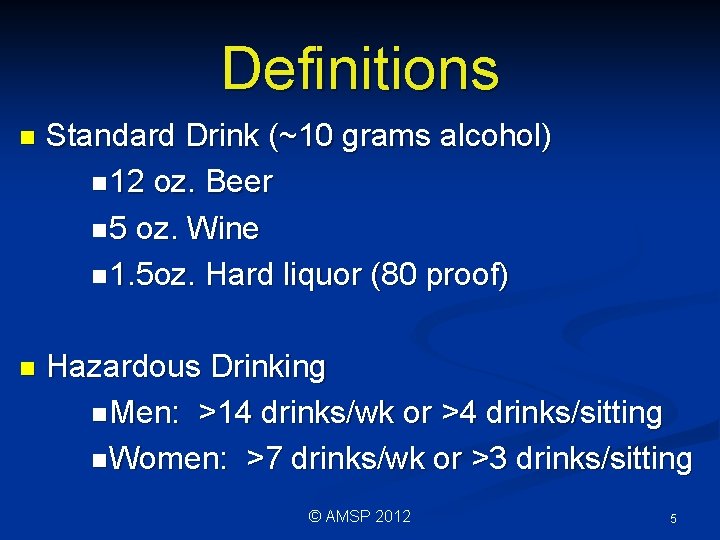
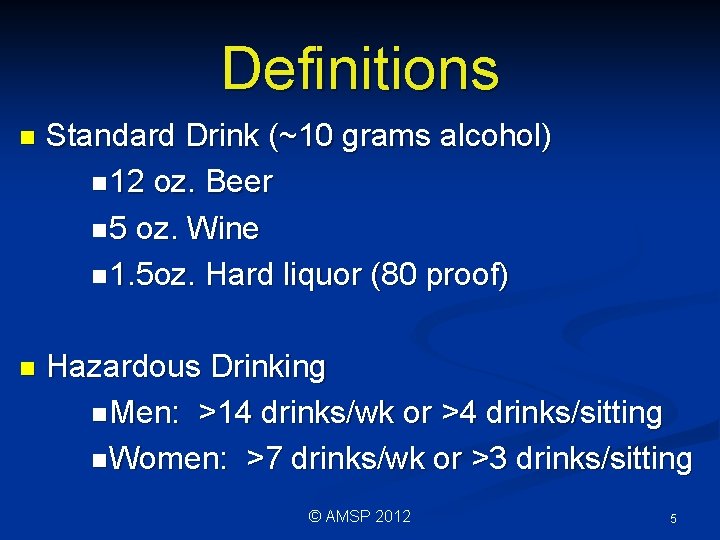
Definitions n Standard Drink (~10 grams alcohol) n 12 oz. Beer n 5 oz. Wine n 1. 5 oz. Hard liquor (80 proof) n Hazardous Drinking n Men: >14 drinks/wk or >4 drinks/sitting n Women: >7 drinks/wk or >3 drinks/sitting © AMSP 2012 5
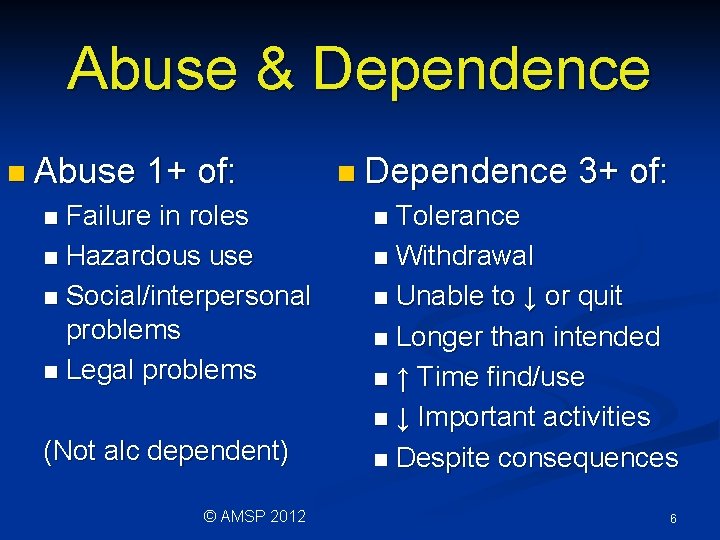
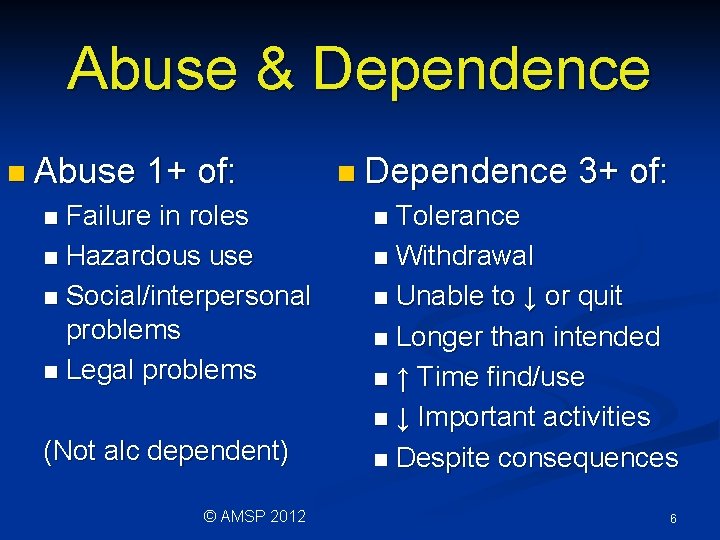
Abuse & Dependence n Abuse 1+ of: Failure in roles n Hazardous use n Social/interpersonal problems n Legal problems n (Not alc dependent) © AMSP 2012 n Dependence 3+ of: Tolerance n Withdrawal n Unable to ↓ or quit n Longer than intended n ↑ Time find/use n ↓ Important activities n Despite consequences n 6
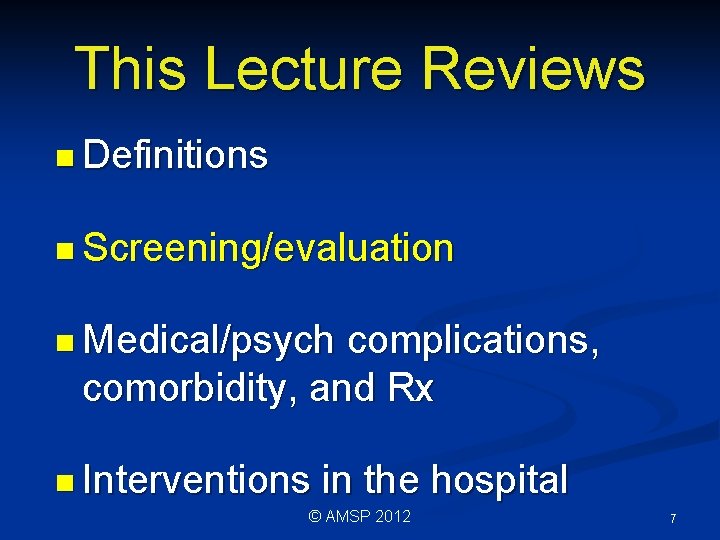
This Lecture Reviews n Definitions n Screening/evaluation n Medical/psych complications, comorbidity, and Rx n Interventions in the hospital © AMSP 2012 7

Screening/Evaluation n Often undetected by MDs n Reasons include: n. Inadequate training n. Misperceptions/stereotyping n. Uncertain about what to do © AMSP 2012 8
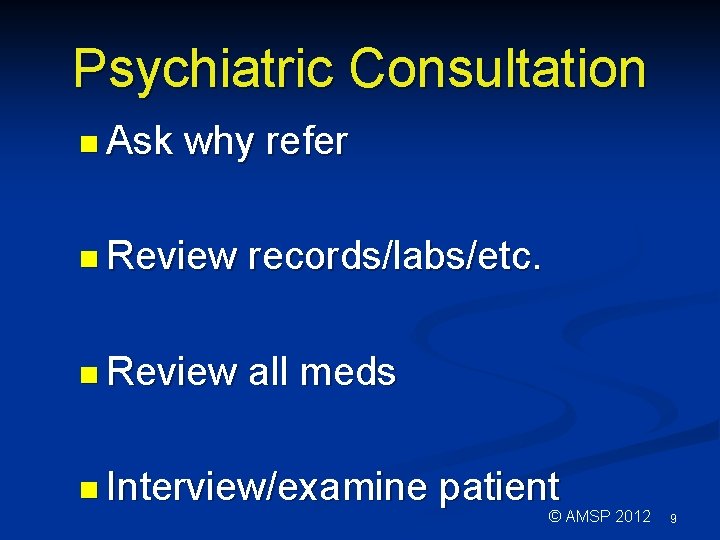
Psychiatric Consultation n Ask why refer n Review records/labs/etc. n Review all meds n Interview/examine patient © AMSP 2012 9

Psychiatric Consultation n Interview n Order collateral diagnostic tests n Formulate n Discuss assessment & plan w/ referring clinician © AMSP 2012 10
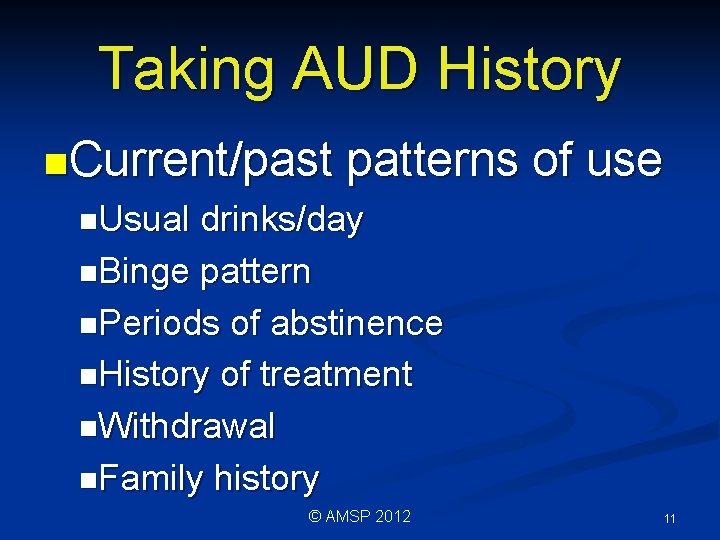
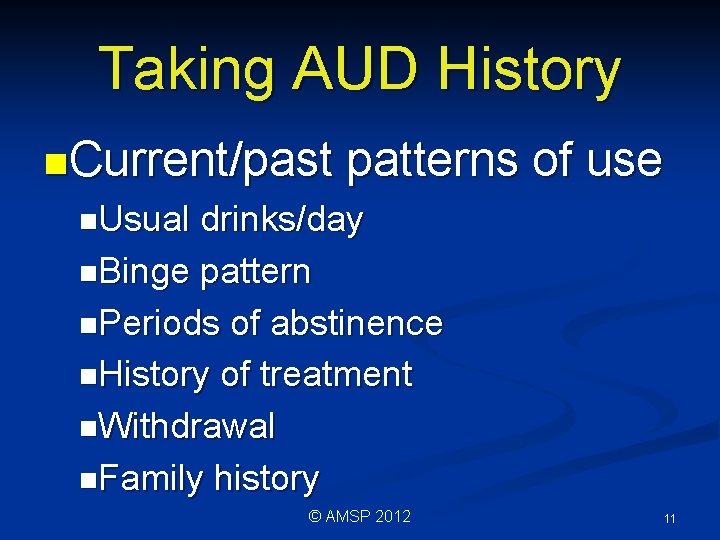
Taking AUD History n. Current/past patterns of use n. Usual drinks/day n. Binge pattern n. Periods of abstinence n. History of treatment n. Withdrawal n. Family history © AMSP 2012 11
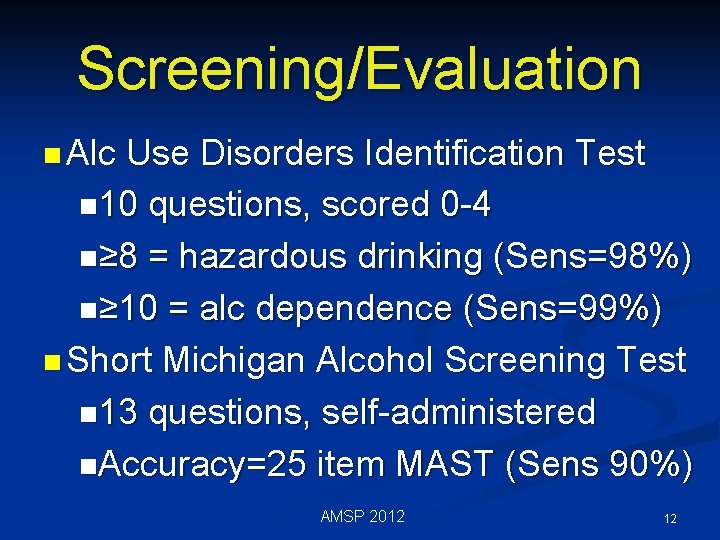
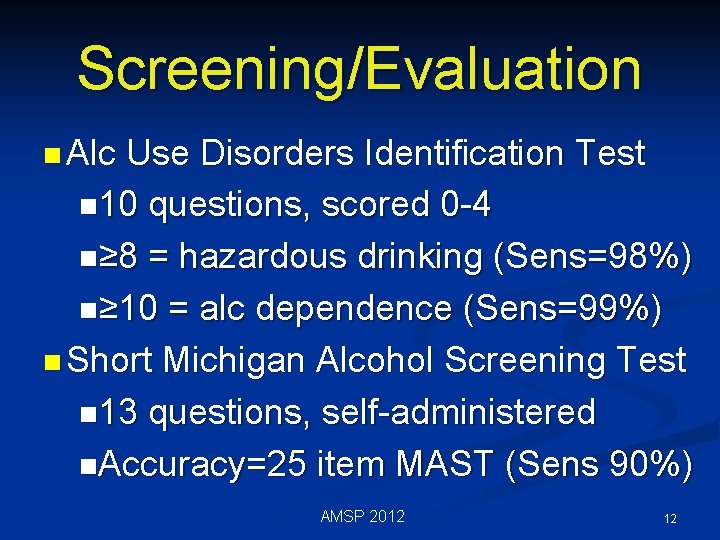
Screening/Evaluation n Alc Use Disorders Identification Test n 10 questions, scored 0 -4 n≥ 8 = hazardous drinking (Sens=98%) n≥ 10 = alc dependence (Sens=99%) n Short Michigan Alcohol Screening Test n 13 questions, self-administered n. Accuracy=25 item MAST (Sens 90%) AMSP 2012 12
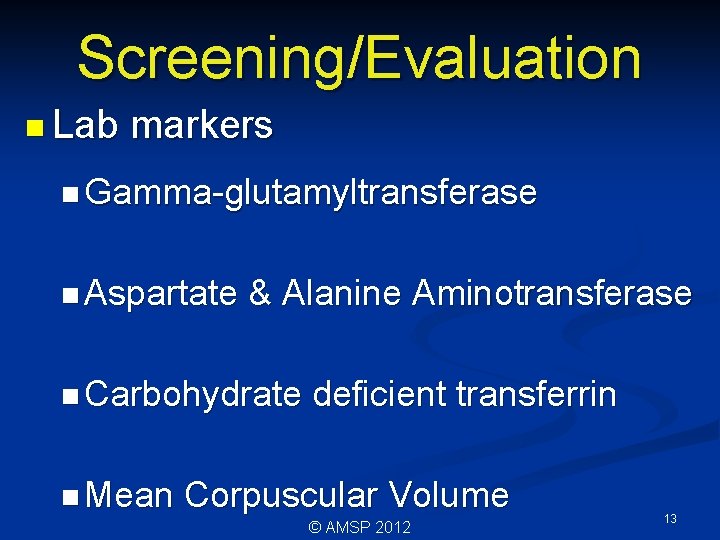
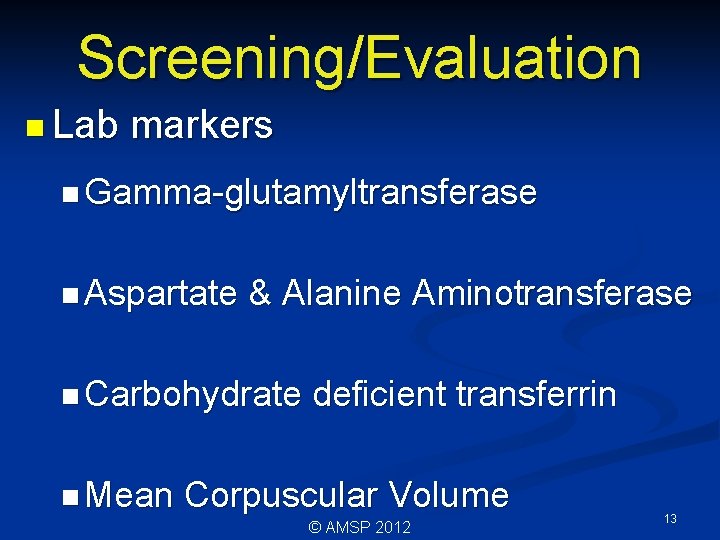
Screening/Evaluation n Lab markers n Gamma-glutamyltransferase n Aspartate & Alanine Aminotransferase n Carbohydrate n Mean deficient transferrin Corpuscular Volume © AMSP 2012 13

Lab Markers 1 (GGT) n Gamma-glutamyltransferase n n n ↑ With heavy drinking ↑ In: heart disease, kidney disease, preg GGT >35 -Heavy drinking -↑ Before liver damage -Sensitivity for heavy drinking ~75% GGT >50 may indicate liver damage Normalizes ~5 weeks of abstinence © AMSP 2012 14

Lab Markers 2 (LFT) n Liver enzymes: AST and ALT n ALT in liver, AST in many tissues n ↑ In high use AND liver damage n Absolute value &ratio important -AST (14 -38 U/L normal range) -ALT (15 -48 U/L normal range) -AST: ALT ratio >2 suggestive of alcohol n Less sensitive than GGT © AMSP 2012 15
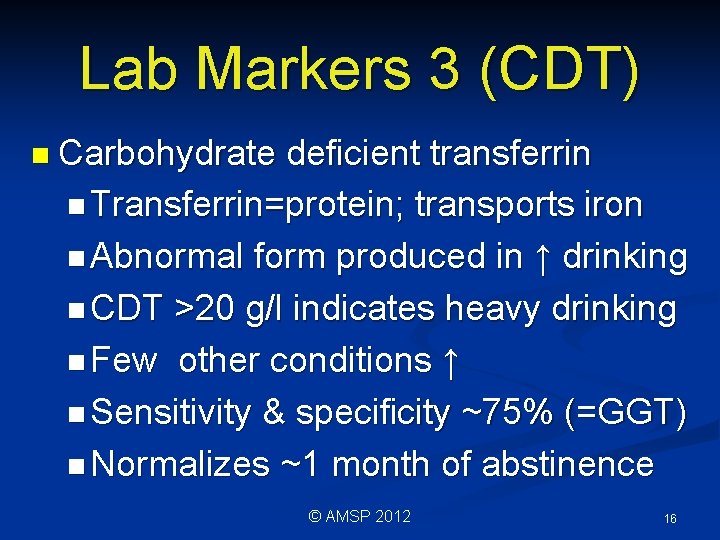
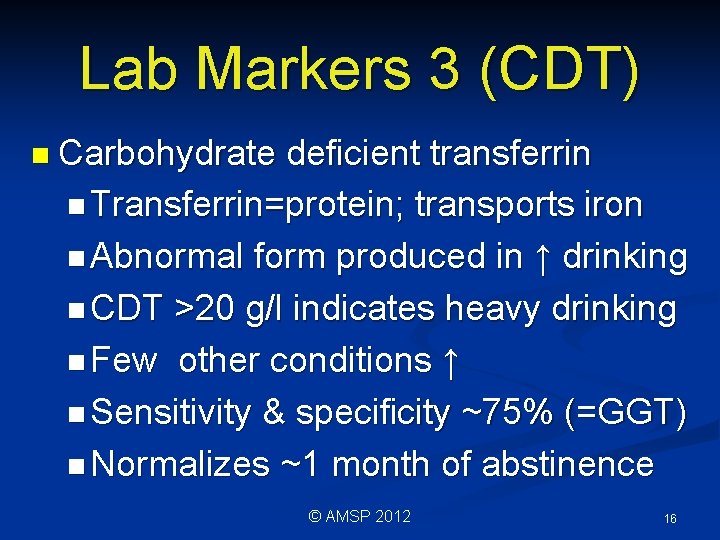
Lab Markers 3 (CDT) n Carbohydrate deficient transferrin n Transferrin=protein; transports iron n Abnormal form produced in ↑ drinking n CDT >20 g/l indicates heavy drinking n Few other conditions ↑ n Sensitivity & specificity ~75% (=GGT) n Normalizes ~1 month of abstinence © AMSP 2012 16
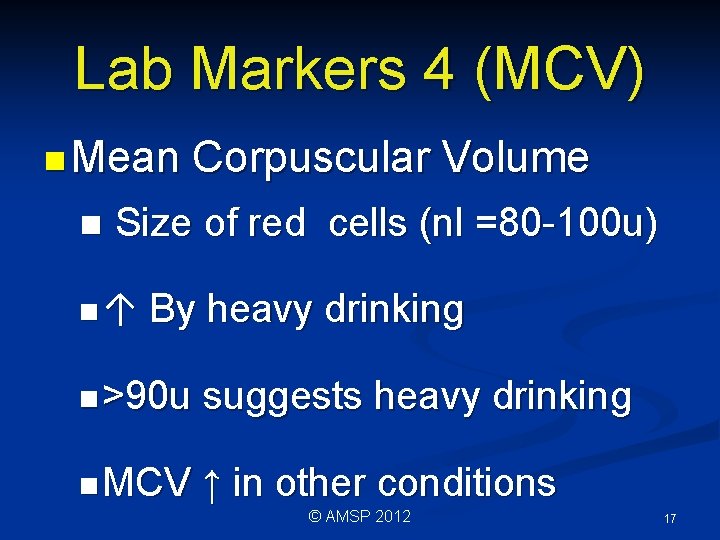
Lab Markers 4 (MCV) n Mean n Corpuscular Volume Size of red cells (nl =80 -100 u) n↑ By heavy drinking n >90 u suggests heavy drinking n MCV ↑ in other conditions © AMSP 2012 17
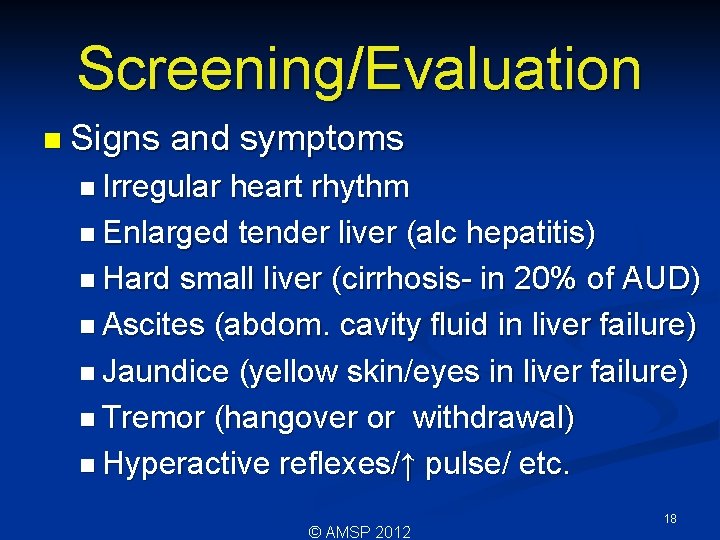
Screening/Evaluation n Signs and symptoms n Irregular heart rhythm n Enlarged tender liver (alc hepatitis) n Hard small liver (cirrhosis- in 20% of AUD) n Ascites (abdom. cavity fluid in liver failure) n Jaundice (yellow skin/eyes in liver failure) n Tremor (hangover or withdrawal) n Hyperactive reflexes/↑ pulse/ etc. © AMSP 2012 18
This Lecture Reviews n Definitions n Screening/evaluation n Medical/psych complications, comorbidity, and Rx n Interventions in the hospital © AMSP 2012 19
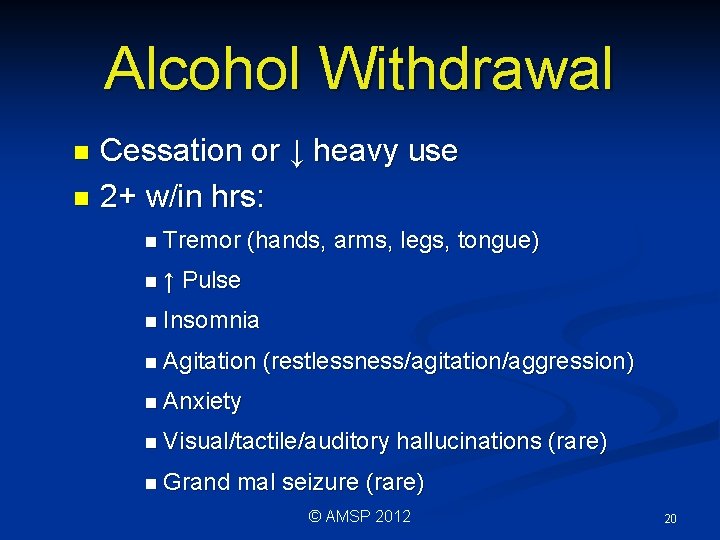
Alcohol Withdrawal Cessation or ↓ heavy use n 2+ w/in hrs: n n Tremor n↑ (hands, arms, legs, tongue) Pulse n Insomnia n Agitation (restlessness/agitation/aggression) n Anxiety n Visual/tactile/auditory n Grand hallucinations (rare) mal seizure (rare) © AMSP 2012 20
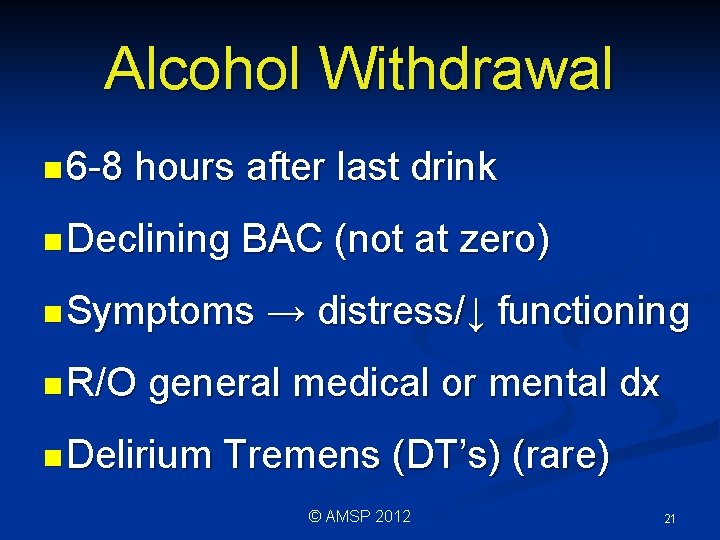
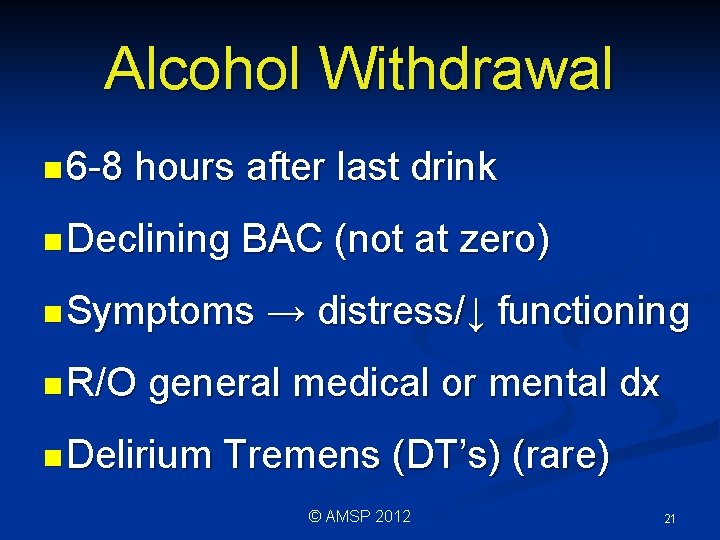
Alcohol Withdrawal n 6 -8 hours after last drink n Declining BAC (not at zero) n Symptoms n R/O → distress/↓ functioning general medical or mental dx n Delirium Tremens (DT’s) (rare) © AMSP 2012 21
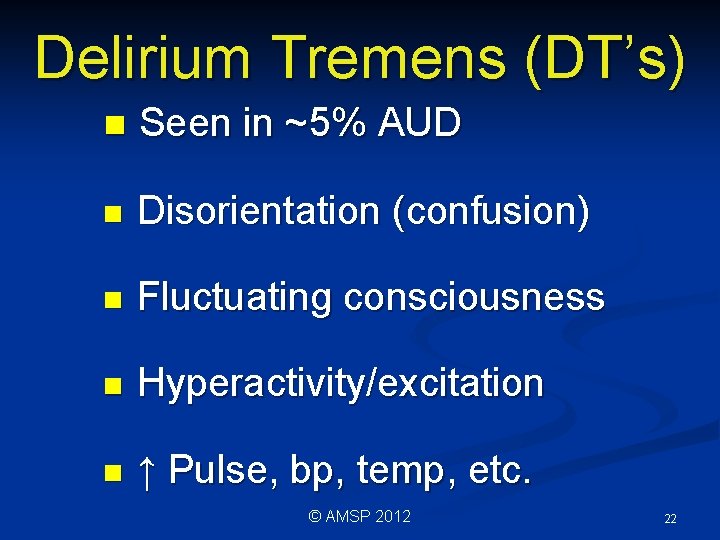
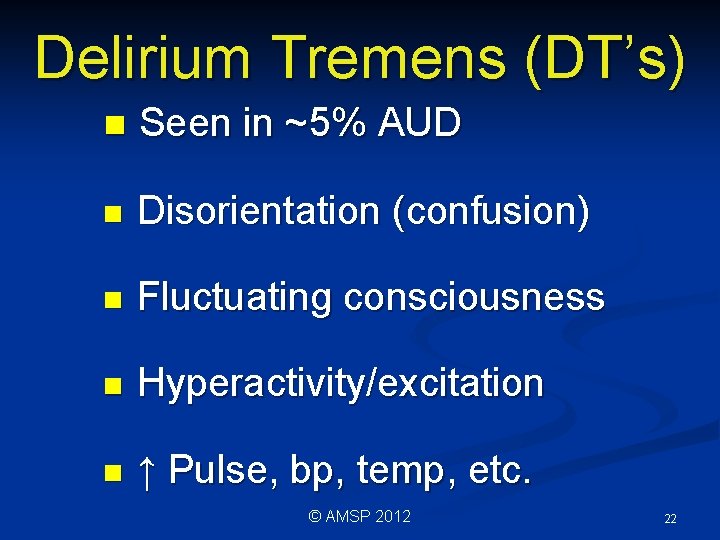
Delirium Tremens (DT’s) n Seen in ~5% AUD n Disorientation (confusion) n Fluctuating consciousness n Hyperactivity/excitation n ↑ Pulse, bp, temp, etc. © AMSP 2012 22

Delirium Tremens (DT’s) n Hallucinations n Can be fatal if med problems n Onset n↑ 48 -96 hours after last drink Risk prior episodes/med probs n R/ O other causes © AMSP 2012 23
![Withdrawal Tx n Benzodiazepines e g diazepam Valium n Correct transmitter problems n Day Withdrawal Tx n Benzodiazepines (e. g. diazepam [Valium]) n. Correct transmitter problems n. Day](https://slidetodoc.com/presentation_image_h/12e89761a371315fd0858825aca96267/image-23.jpg)
Withdrawal Tx n Benzodiazepines (e. g. diazepam [Valium]) n. Correct transmitter problems n. Day 1: give enough to ↓ symptoms n↓ Dose ~20% day 1 dose each day n↑ Dose if symp ↑; ↓ dose next day n Anticonvulsants not needed © AMSP 2012 24
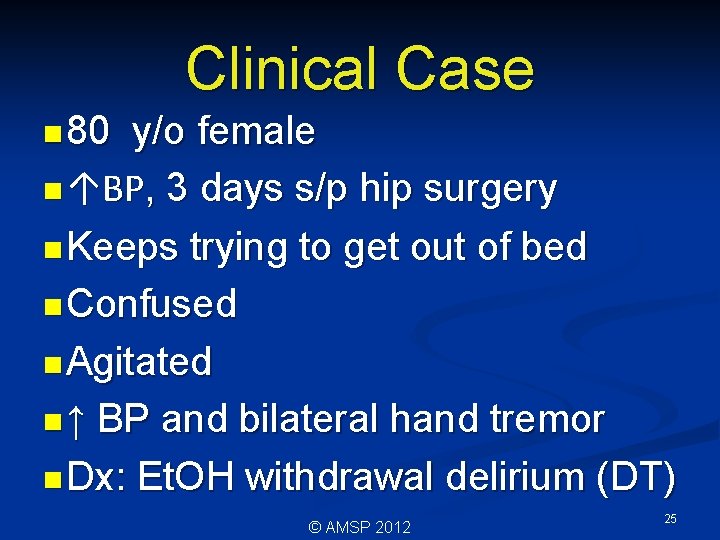
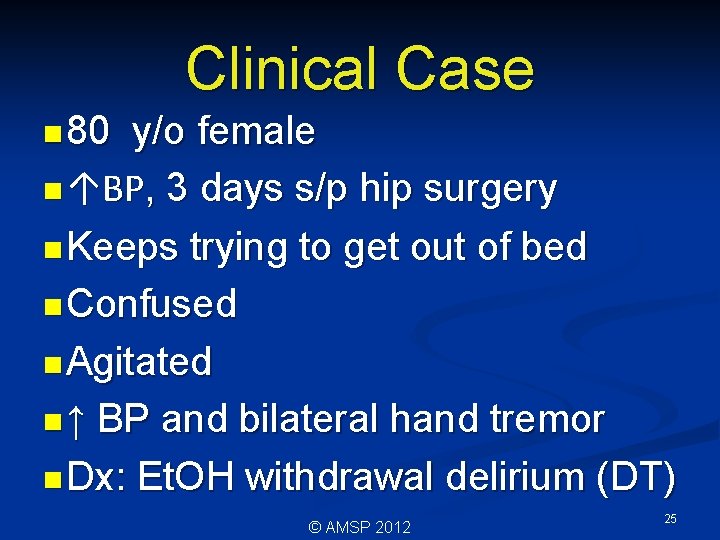
Clinical Case n 80 y/o female n ↑BP, 3 days s/p hip surgery n Keeps trying to get out of bed n Confused n Agitated n ↑ BP and bilateral hand tremor n Dx: Et. OH withdrawal delirium (DT) © AMSP 2012 25
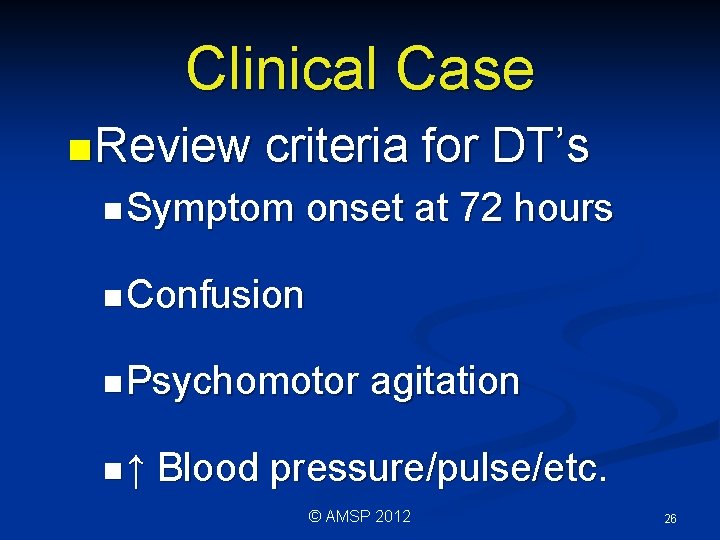
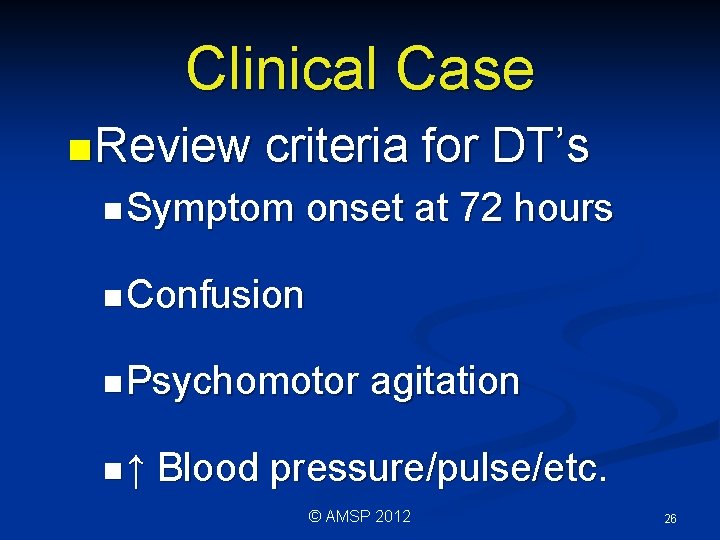
Clinical Case n Review criteria for DT’s n Symptom onset at 72 hours n Confusion n Psychomotor n↑ agitation Blood pressure/pulse/etc. © AMSP 2012 26
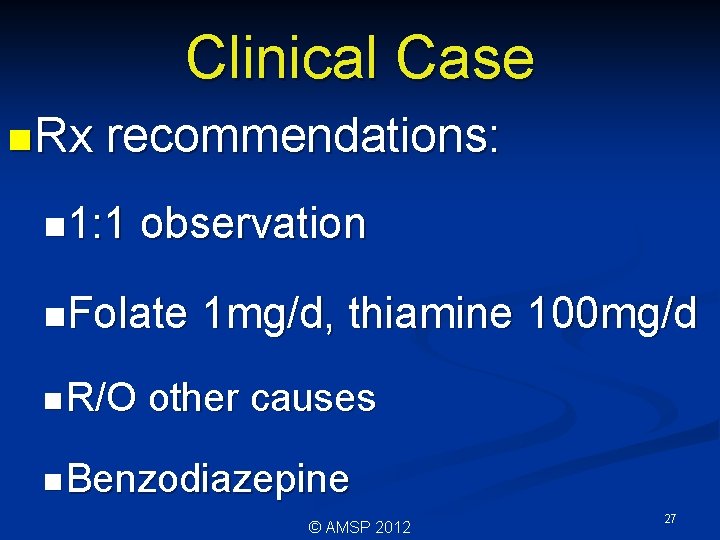
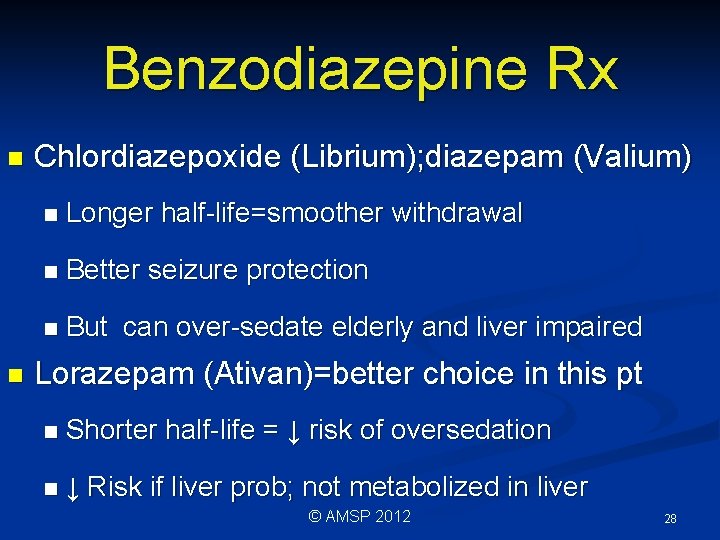
Clinical Case n Rx recommendations: n 1: 1 observation n. Folate n R/O 1 mg/d, thiamine 100 mg/d other causes n Benzodiazepine © AMSP 2012 27
Benzodiazepine Rx n n Chlordiazepoxide (Librium); diazepam (Valium) n Longer half-life=smoother withdrawal n Better seizure protection n But can over-sedate elderly and liver impaired Lorazepam (Ativan)=better choice in this pt n Shorter half-life = ↓ risk of oversedation n ↓ Risk if liver prob; not metabolized in liver © AMSP 2012 28
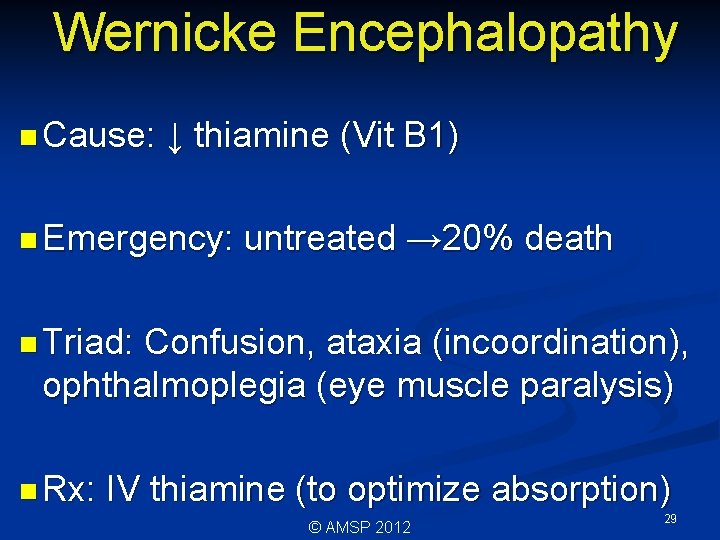
Wernicke Encephalopathy n Cause: ↓ thiamine (Vit B 1) n Emergency: untreated → 20% death n Triad: Confusion, ataxia (incoordination), ophthalmoplegia (eye muscle paralysis) n Rx: IV thiamine (to optimize absorption) © AMSP 2012 29
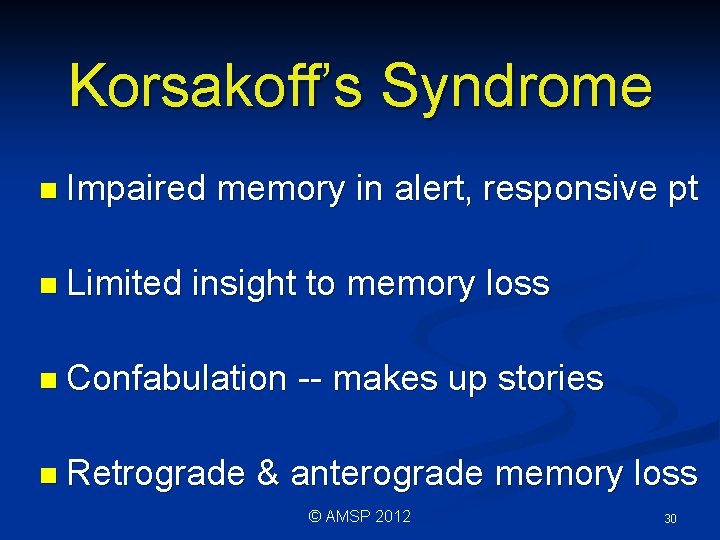
Korsakoff’s Syndrome n Impaired n Limited memory in alert, responsive pt insight to memory loss n Confabulation n Retrograde -- makes up stories & anterograde memory loss © AMSP 2012 30
Psychiatric Disorders: MDE n Co-morbid n Gen major depression pop major depressive episode (MDE) ~15% n AUD slightly ↑ even when not drinking n MDE unrelated to drinking -Alcohol ↑ depressive symptoms -Alcohol intoxication/withdrawal ↑ suicidal ideation © AMSP 2012 31
Psychiatric Disorders: AID n Alcohol induced: severe intoxication → temporary MDE in ~30% n Causal relationship--psychiatric disorder not predating AUD n Treatment = abstinence (≠ meds) n Depression ↓↓ in 2 d to 4 wks abstinence © AMSP 2012 32
Psychiatric Disorders: Psychosis n Psychosis – Hallucinations n Delirium (e. g. post surgery, DT’s) --usually disappear as delirium resolves n ~3% AUD during severe intoxication -No delirium -Alcohol-induced psychosis -Disappears 2 d to 4 wks without meds -Antipsychotics (e. g. risperidone) control symp © AMSP 2012 33
This Lecture Reviews n Definitions n Screening/evaluation n Medical/psych complications, comorbidity, and Rx n Interventions in the hospital © AMSP 2012 34
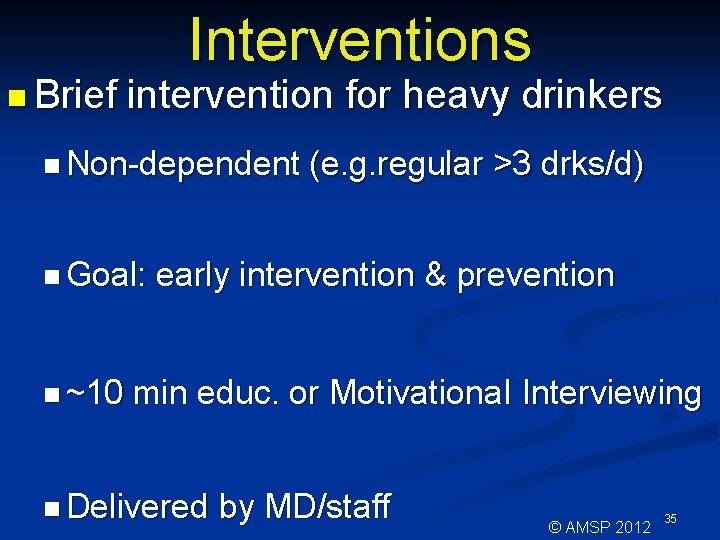
n Brief Interventions intervention for heavy drinkers n Non-dependent n Goal: n ~10 (e. g. regular >3 drks/d) early intervention & prevention min educ. or Motivationa. I Interviewing n Delivered by MD/staff © AMSP 2012 35
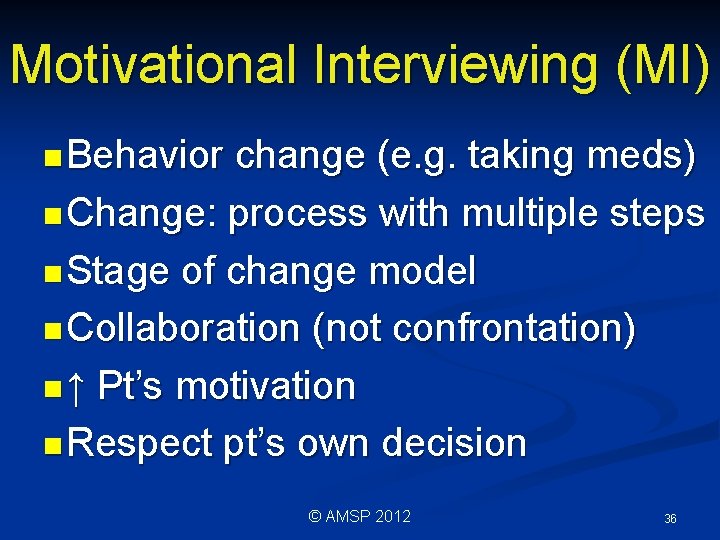
Motivational Interviewing (MI) n Behavior change (e. g. taking meds) n Change: process with multiple steps n Stage of change model n Collaboration (not confrontation) n ↑ Pt’s motivation n Respect pt’s own decision © AMSP 2012 36
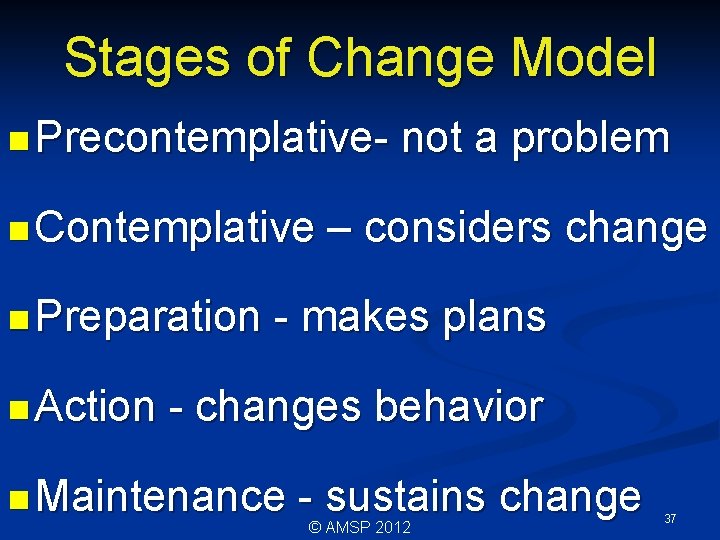
Stages of Change Model n Precontemplativen Contemplative n Preparation n Action not a problem – considers change - makes plans - changes behavior n Maintenance - sustains change © AMSP 2012 37
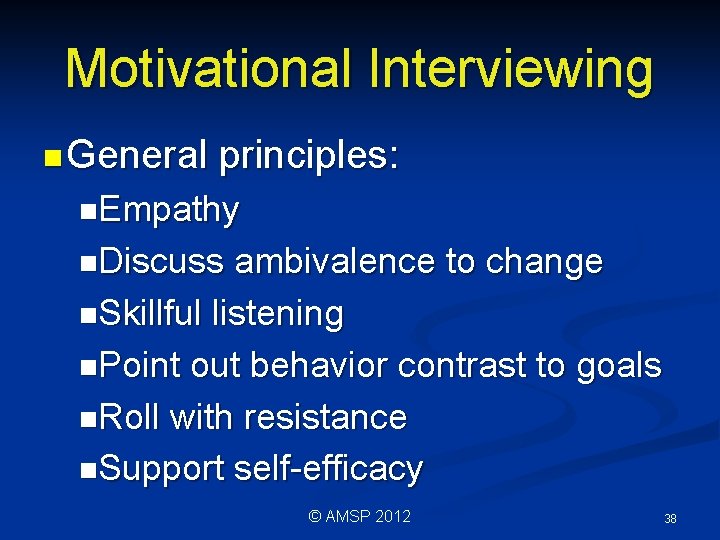
Motivational Interviewing n General principles: n. Empathy n. Discuss ambivalence to change n. Skillful listening n. Point out behavior contrast to goals n. Roll with resistance n. Support self-efficacy © AMSP 2012 38
Clinical Case n 45 year old male high school principal n 3 rd admission for alcoholic pancreatitis n Given AUD treatment options in past n No follow up n Now: marital discord, job lay-off, etc. n Admits alcohol a problem © AMSP 2012 39
Clinical Case n Stage of change: contemplative n Express empathy for situation/stressors n Discuss barriers to change n Discuss goals vs behavior n Support ability to change if desired n Result: pt takes initiative n Stage : contemplation→preparation © AMSP 2012 40

n All Treatment options work to: n. Change thinking about AUD -Chronic disorder -Can be managed n. Help prevent relapse -Recognize triggers -Avoid high risk situations -Cope with cravings © AMSP 2012 41
Referral Option 1 n Inpatient/residential rehabilitation n Lessons/support in 24 hr milieu n Typically 14 -28 days n Learn through group discussions n Intensive Outpatient Treatment (IOP) n Groups multiple days of week n Provided in “real world” setting © AMSP 2012 42
Referral Option 2 n Outpatient treatment n Substance or mental health Rx provider n Provided in variety of settings n Self-help groups (AA) n Introduced in rehab or IOP n Requires only desire to stop drinking n Change through working “ 12 steps” © AMSP 2012 43
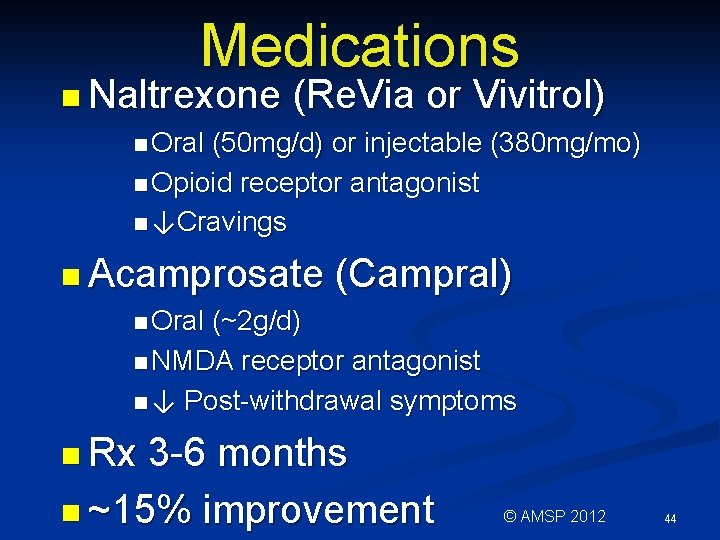
Medications n Naltrexone (Re. Via or Vivitrol) n Oral (50 mg/d) or injectable (380 mg/mo) n Opioid receptor antagonist n ↓Cravings n Acamprosate (Campral) n Oral (~2 g/d) n NMDA receptor antagonist n ↓ Post-withdrawal symptoms n Rx 3 -6 months n ~15% improvement © AMSP 2012 44

Conclusions n AUD important issue in general hospital n Effective n Multiple screening and evaluation medical/psychiatric complications n Effective interventions for Rx and referral © AMSP 2012 45
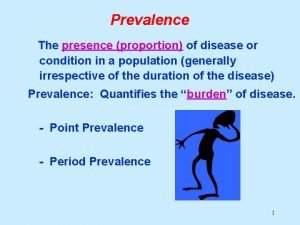
 Period prevalence vs point prevalence
Period prevalence vs point prevalence Proportion defination
Proportion defination Period prevalence vs point prevalence
Period prevalence vs point prevalence Period prevalence vs point prevalence
Period prevalence vs point prevalence Aud nistov
Aud nistov Se aud pasii domnului venind
Se aud pasii domnului venind Autodesk
Autodesk Tu bs algorithmen und datenstrukturen
Tu bs algorithmen und datenstrukturen Aud202
Aud202 Rosemary aud
Rosemary aud Aud materia plangand
Aud materia plangand Aud skrudland
Aud skrudland Difference between voluntary and mandatory
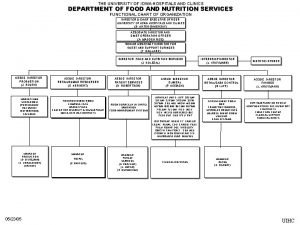
Difference between voluntary and mandatory University of iowa hospitals and clinics
University of iowa hospitals and clinics Qah
Qah Louisiana health standards
Louisiana health standards Jci
Jci Echs polyclinic visakhapatnam
Echs polyclinic visakhapatnam Uses of computers in hospitals
Uses of computers in hospitals Dnv vs jcaho
Dnv vs jcaho Bcp for hospitals
Bcp for hospitals Va hospital fairbanks alaska
Va hospital fairbanks alaska Uhcw map
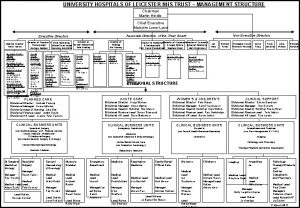
Uhcw map Simon sheppard nhs birmingham
Simon sheppard nhs birmingham Strength of hospital
Strength of hospital Lean hospitals
Lean hospitals Graban lean hospitals download
Graban lean hospitals download Fhpl corporate id
Fhpl corporate id Administrator plus hospital software
Administrator plus hospital software Medisep hospitals in kerala
Medisep hospitals in kerala Dr sue carr
Dr sue carr Bed management in hospitals
Bed management in hospitals Mghs wheelers
Mghs wheelers Portsmouth hospitals nhs trust jobs
Portsmouth hospitals nhs trust jobs National accreditation board for hospitals
National accreditation board for hospitals Lokmanya orthopedic hospital pune
Lokmanya orthopedic hospital pune Inventory cycle time
Inventory cycle time Process governance
Process governance Rumus angka kematian bayi
Rumus angka kematian bayi Epidemiologi adalah
Epidemiologi adalah Obesity prevalence europe
Obesity prevalence europe Prevalence ratio
Prevalence ratio Prevalence
Prevalence Prevalence of obesity
Prevalence of obesity Calculate prevalence rate
Calculate prevalence rate