Atypical Bacterial Pneumonia Dina Abouelkheir Lecturer of chest
Atypical Bacterial Pneumonia Dina Abouelkheir Lecturer of chest medicine-MUH 2015
Why it is called “Atypical”? ? ? The atypical organisms cannot be cultured on standard media, nor can they be seen on Gram’s stain. Have atypical presentation Often cause extrapulmonary manifestations Intrinsically resistant to all β-lactam agents as most of the atypical pathogens do not have a bacterial cell wall
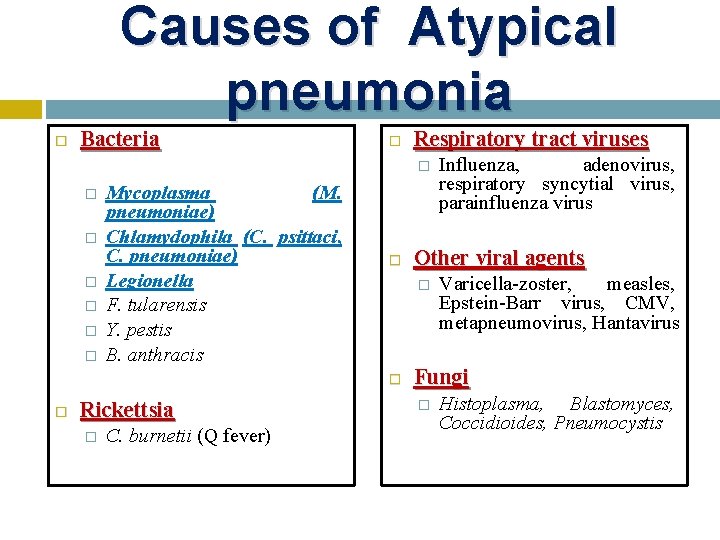
Causes of Atypical pneumonia Bacteria Respiratory tract viruses � � � � Mycoplasma (M. pneumoniae) Chlamydophila (C. psittaci, C. pneumoniae) Legionella F. tularensis Y. pestis B. anthracis Rickettsia � C. burnetii (Q fever) Other viral agents � Influenza, adenovirus, respiratory syncytial virus, parainfluenza virus Varicella-zoster, measles, Epstein-Barr virus, CMV, metapneumovirus, Hantavirus Fungi � Histoplasma, Blastomyces, Coccidioides, Pneumocystis

Epidemiology Atypical CAPs represent approximately 15% of all CAPs. Legionella Sources of infection include domestic hot and cold water systems, wet cooling systems, natural spas, humidifiers, ultrasonic mist machines, respiratory therapy equipment. - The attack rate is higher in: the elderly � tobacco smokers, alcoholism � those with chronic lung disease � diabetes mellitus � ICH �
Mycoplasma (M. pneumoniae) The organism is spread by droplet aerosol Chlamydophila (C. psittaci, C. pneumoniae) C. psittaci may be hosted by many avian species Psittacine infection is an occupational hazard of veterinarians, pet-shop workers, zoo staff and poultry workers.
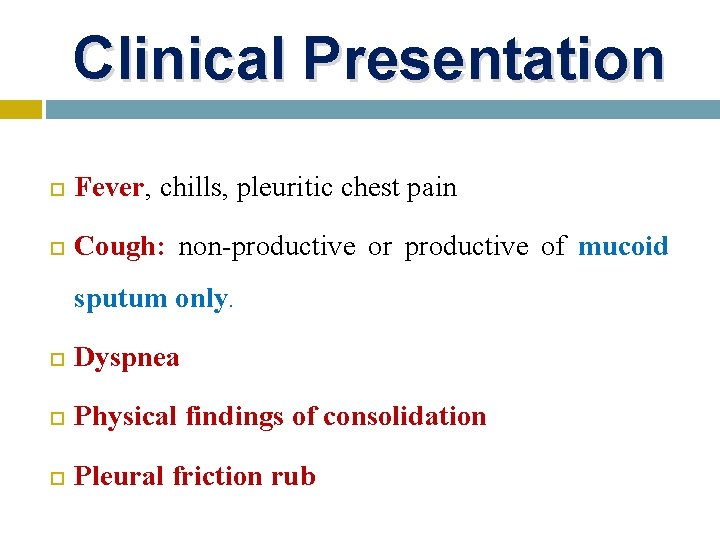
Clinical Presentation Fever, chills, pleuritic chest pain Cough: non-productive or productive of mucoid sputum only. Dyspnea Physical findings of consolidation Pleural friction rub
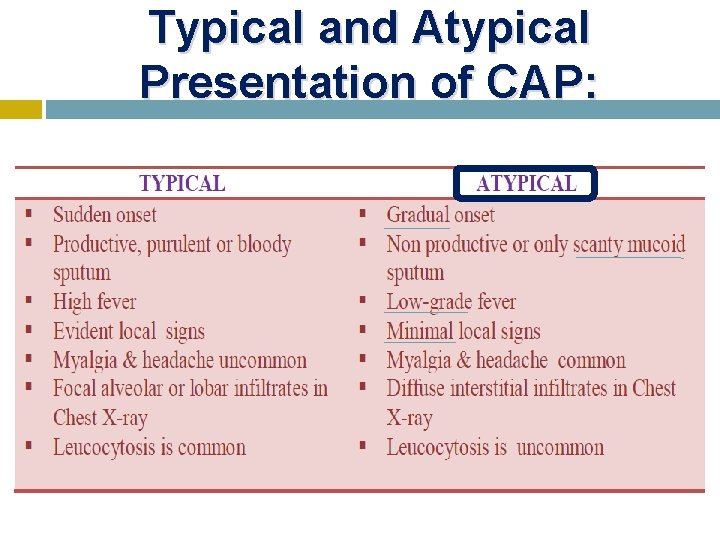
Typical and Atypical Presentation of CAP:
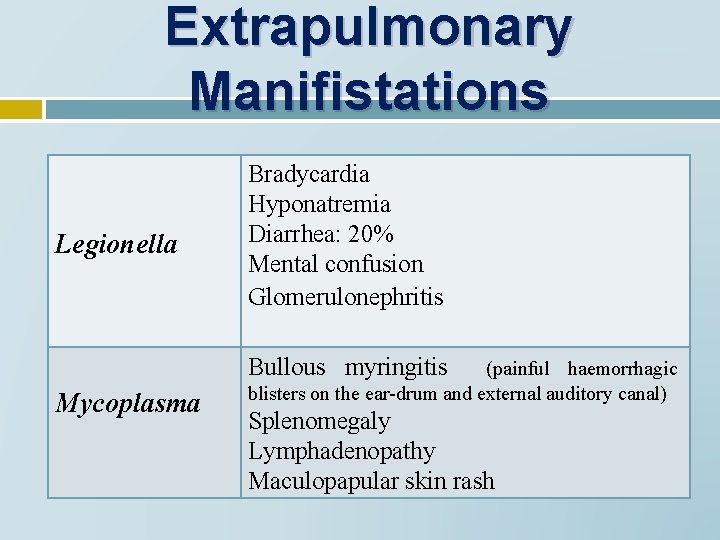
Extrapulmonary Manifistations Legionella Bradycardia Hyponatremia Diarrhea: 20% Mental confusion Glomerulonephritis Bullous myringitis Mycoplasma (painful haemorrhagic blisters on the ear-drum and external auditory canal) Splenomegaly Lymphadenopathy Maculopapular skin rash
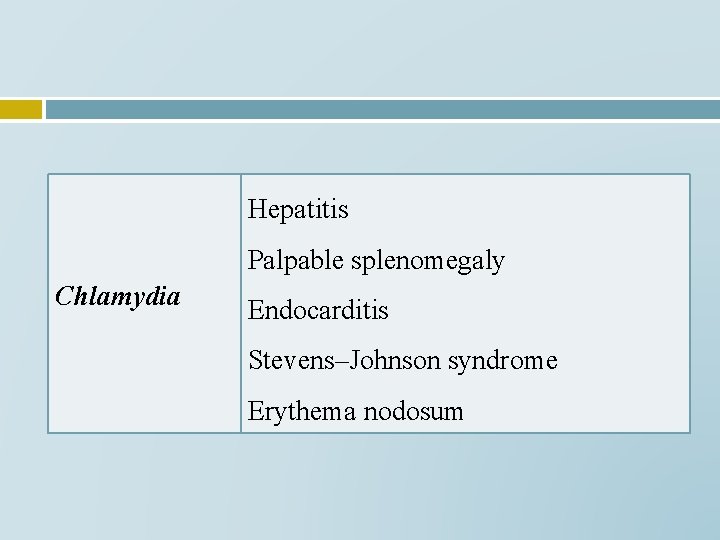
Hepatitis Palpable splenomegaly Chlamydia Endocarditis Stevens–Johnson syndrome Erythema nodosum
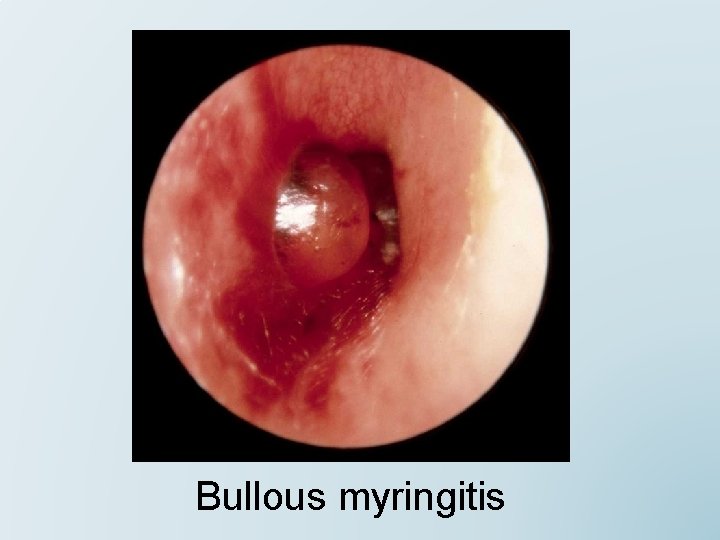
Bullous myringitis

Steven Johnson Syndrome
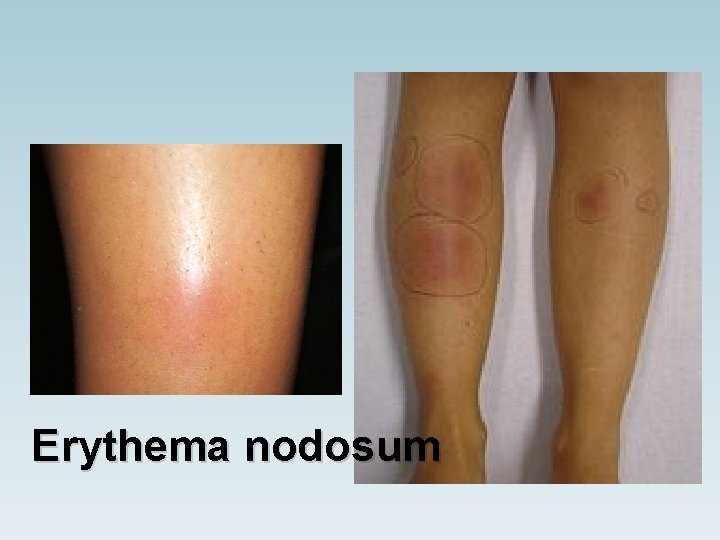
Erythema nodosum
Radiology
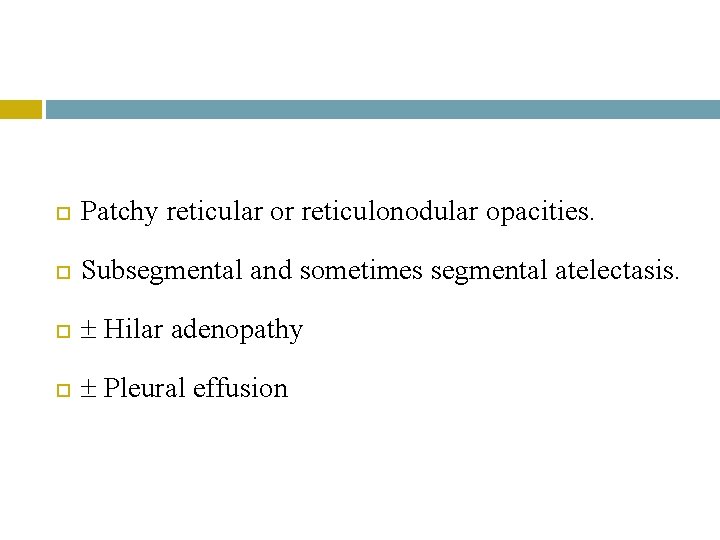
Patchy reticular or reticulonodular opacities. Subsegmental and sometimes segmental atelectasis. Hilar adenopathy Pleural effusion
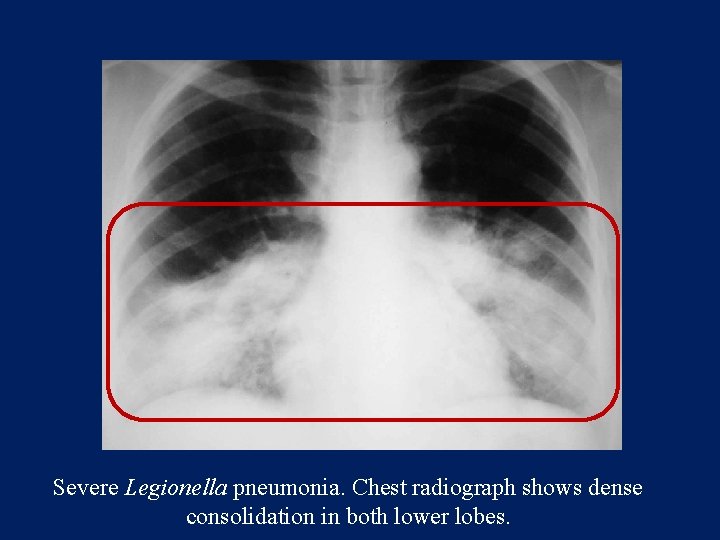
Severe Legionella pneumonia. Chest radiograph shows dense consolidation in both lower lobes.
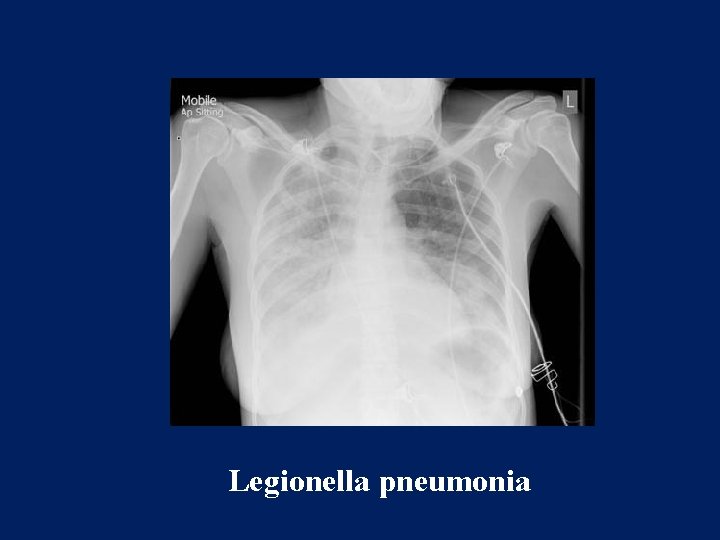
Legionella pneumonia
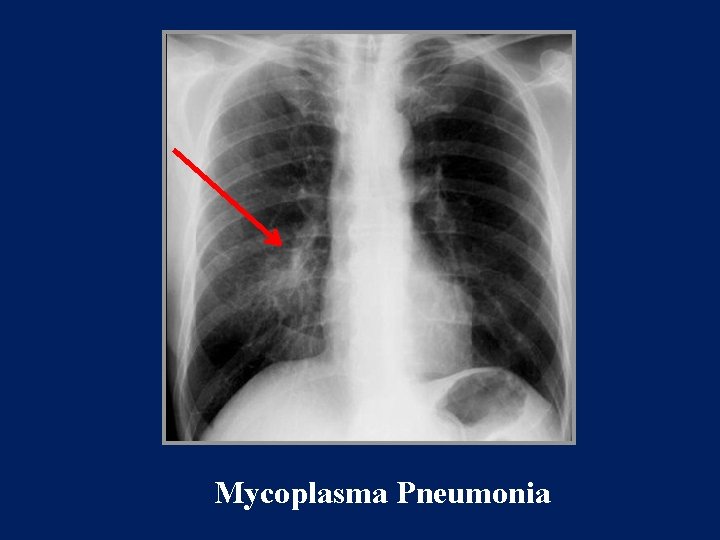
Mycoplasma Pneumonia
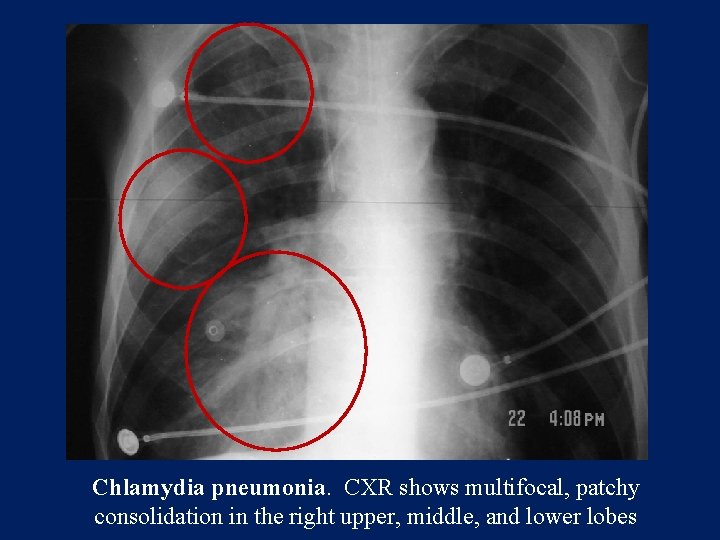
Chlamydia pneumonia. CXR shows multifocal, patchy consolidation in the right upper, middle, and lower lobes
Investigations Sputum microscopy: The absence of large numbers of organisms in an adequate sputum sample raises the possibility of Legionella pneumophila, Mycoplasma pneumoniae, Coxiella burnetii or a viral pneumonia.
Sputum culture Legionella spp. → selective charcoal yeast extract medium. Result is relatively slow, taking about 3 days. Urine Antigen detection Legionella spp.
Standard acute and convalescent serological testing Complement-fixing antibody levels in the blood Enzyme-linked immunosorbent assay (ELISA) Immunofluorescent tests PCR
Haematological measurements and biochemical White cell count: normal or increased (Legionella ) ESR : raised. Mild abnormalities of liver and renal function including proteinuria and microscopic haematuria Raised LDH and creatine kinase (Legionella ) Hyponatraemia (Legionella )
Ig. M cold agglutinins: Mycoplasma This test is usually done by combining the patient’s serum with type O red cells in the laboratory. If clumping is noted, the serum is serially diluted and the test repeated, the titre reported being the highest dilution at which clumping occurs at 4°C
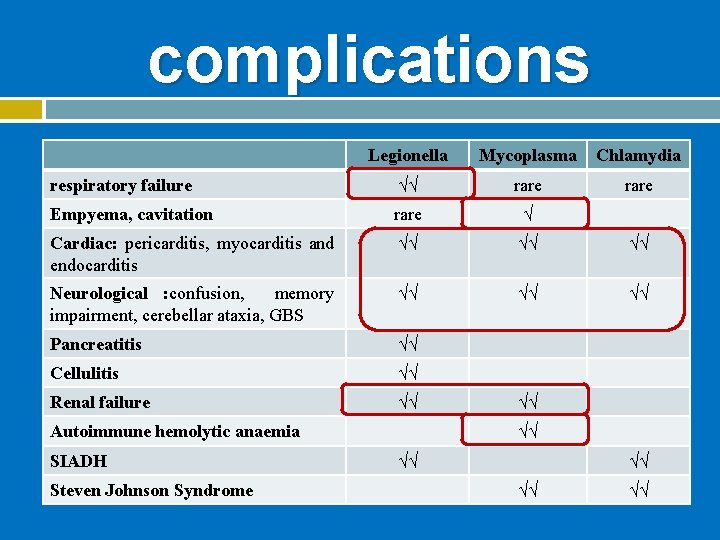
complications Legionella Mycoplasma Chlamydia respiratory failure √√ rare Empyema, cavitation rare √ Cardiac: pericarditis, myocarditis and endocarditis √√ √√ √√ Neurological : confusion, memory impairment, cerebellar ataxia, GBS √√ √√ √√ Pancreatitis √√ Cellulitis √√ Renal failure √√ Autoimmune hemolytic anaemia SIADH Steven Johnson Syndrome √√ √√ √√
Treatment Can we use B-LACTAM ANTIBIOTICS to treat Atypical Pneumonia? ?
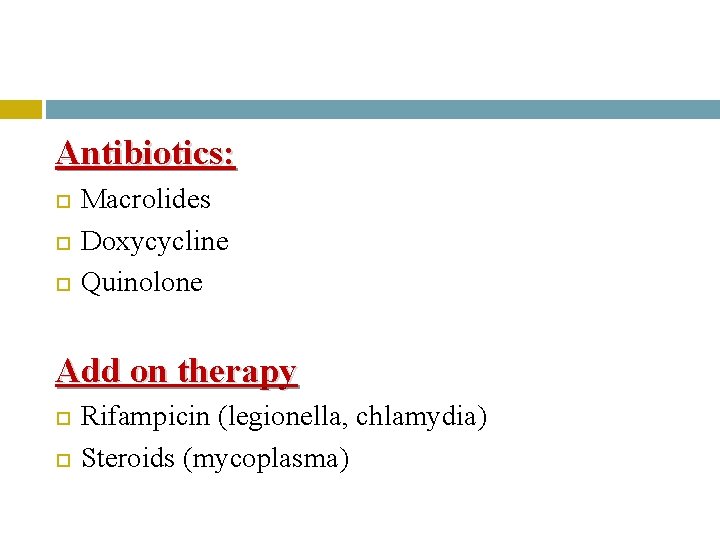
Antibiotics: Macrolides Doxycycline Quinolone Add on therapy Rifampicin (legionella, chlamydia) Steroids (mycoplasma)
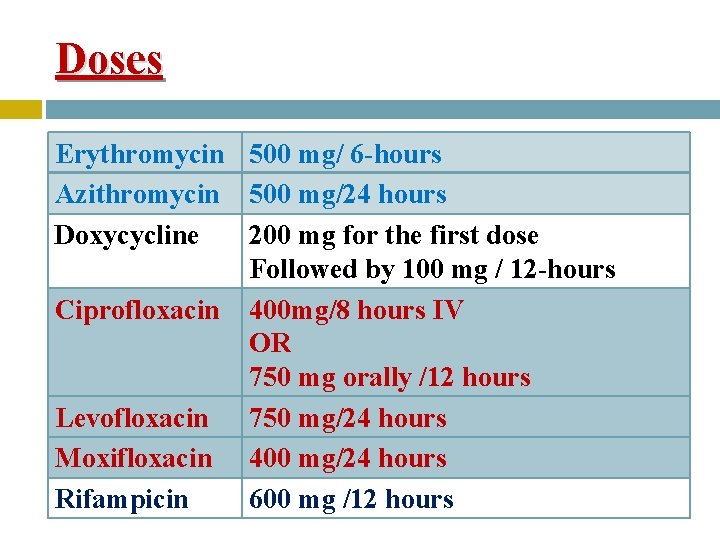
Doses Erythromycin 500 mg/ 6 -hours Azithromycin 500 mg/24 hours Doxycycline 200 mg for the first dose Followed by 100 mg / 12 -hours Ciprofloxacin 400 mg/8 hours IV OR 750 mg orally /12 hours Levofloxacin 750 mg/24 hours Moxifloxacin 400 mg/24 hours Rifampicin 600 mg /12 hours
Duration It is recommended that treatment is continued for 2 – 3 weeks for fear that shorter periods may result in delayed resolution or relapse, particularly in those who are immunosuppressed or who have extensive disease.
Prevention of Legionella pneumonia Identification of the sources where epidemics or case clustering have occurred. Hot water supplies are usually decontaminated by hyperchlorination, or by superheating water supplies to 70– 80°C, and by the removal of rubber washers from shower fittings.

- Slides: 30