Atopic Eczema Sharon Wong Suzy Tinker Classification Endogenous









































- Slides: 78
Atopic Eczema Sharon Wong Suzy Tinker
Classification • Endogenous vs Exogenous • Acute vs Chronic

Acute eczema • Acute: pruritus, erythema, vesiculation


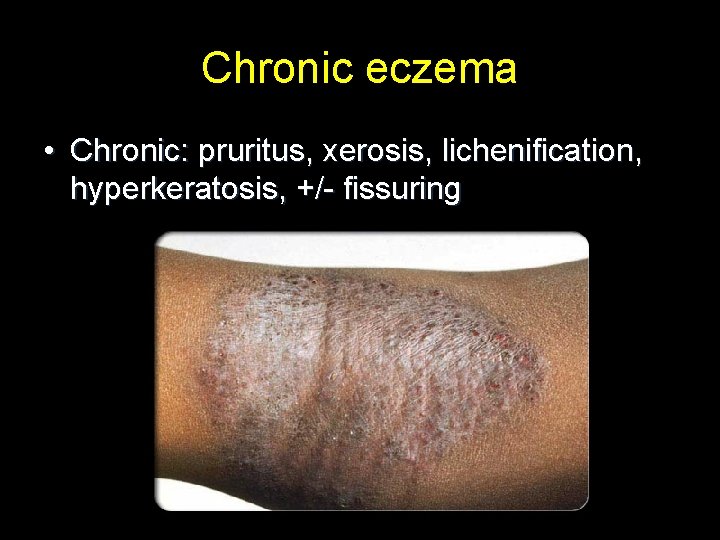
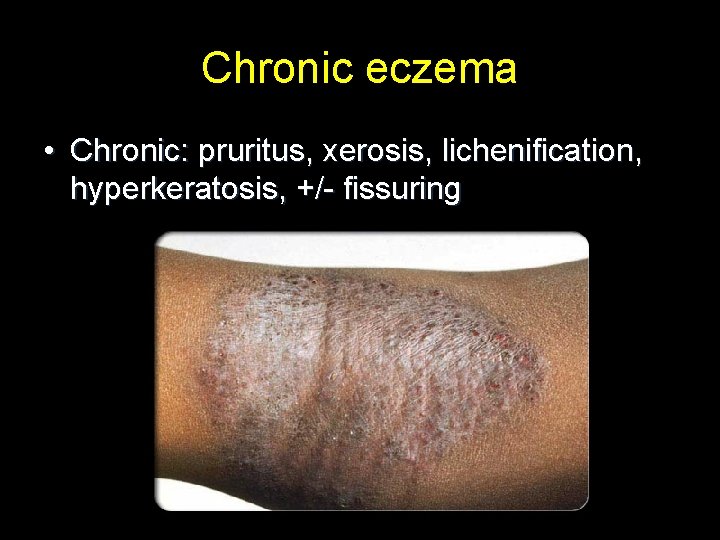
Chronic eczema • Chronic: pruritus, xerosis, lichenification, hyperkeratosis, +/- fissuring

Chronic eczema
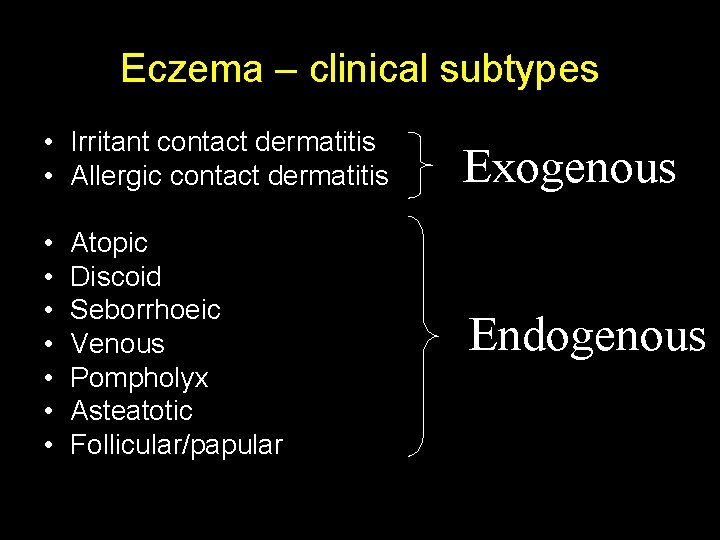
Eczema – clinical subtypes • Irritant contact dermatitis • Allergic contact dermatitis Exogenous • • Endogenous Atopic Discoid Seborrhoeic Venous Pompholyx Asteatotic Follicular/papular
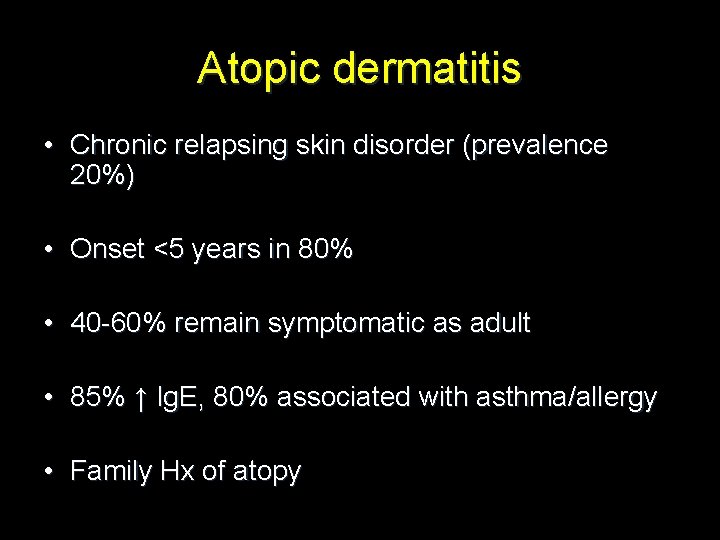
Atopic dermatitis • Chronic relapsing skin disorder (prevalence 20%) • Onset <5 years in 80% • 40 -60% remain symptomatic as adult • 85% ↑ Ig. E, 80% associated with asthma/allergy • Family Hx of atopy
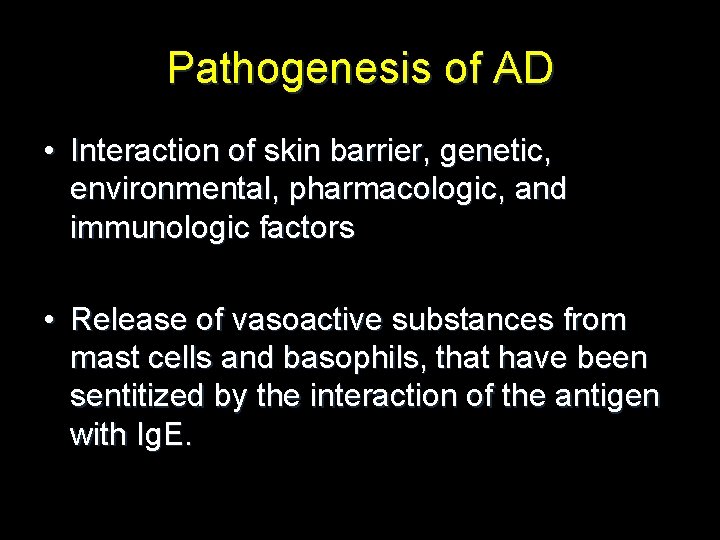
Pathogenesis of AD • Interaction of skin barrier, genetic, environmental, pharmacologic, and immunologic factors • Release of vasoactive substances from mast cells and basophils, that have been sentitized by the interaction of the antigen with Ig. E.
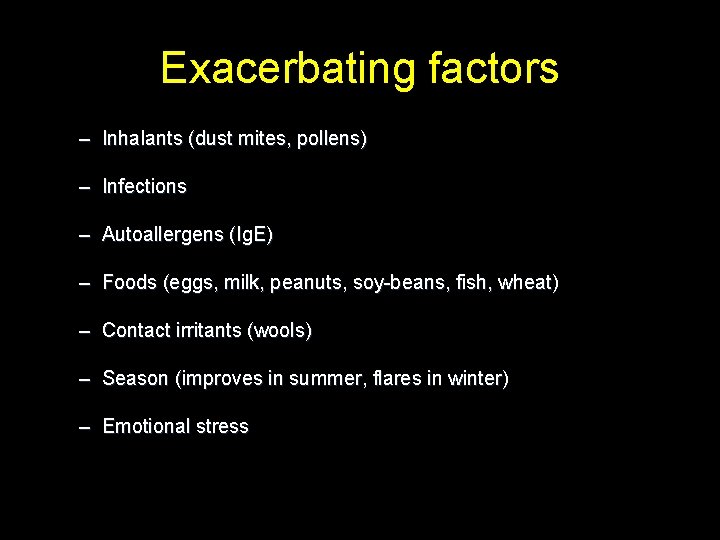
Exacerbating factors – Inhalants (dust mites, pollens) – Infections – Autoallergens (Ig. E) – Foods (eggs, milk, peanuts, soy-beans, fish, wheat) – Contact irritants (wools) – Season (improves in summer, flares in winter) – Emotional stress
Clinical features
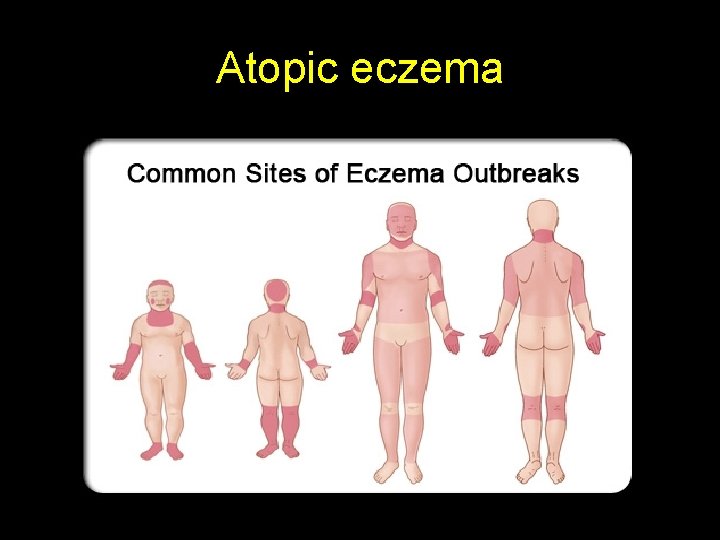
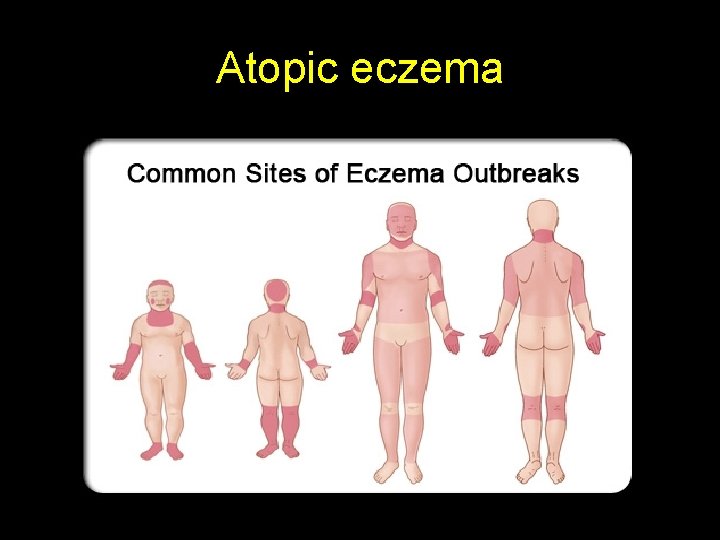
Atopic eczema








The Itch-Scratch cycle • Pruritus usually begins and causes itch sensation • Scratch causes skin trauma and precipitates skin inflammation • Chronic inflammation leads to lichenification
Clinical variants
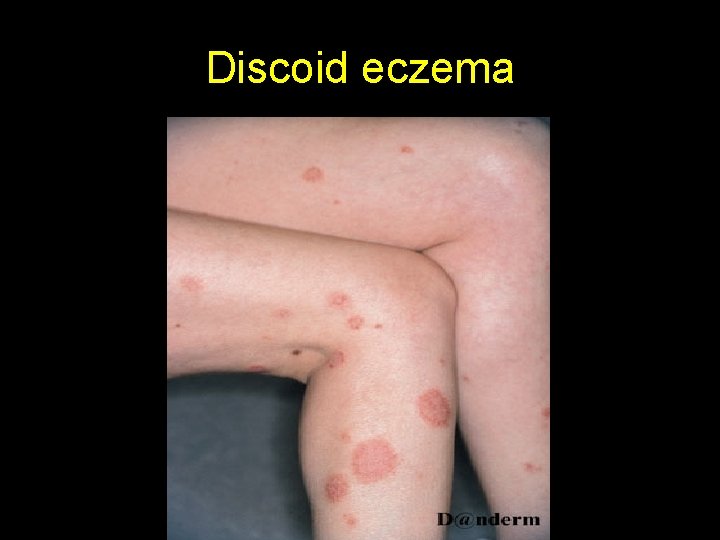
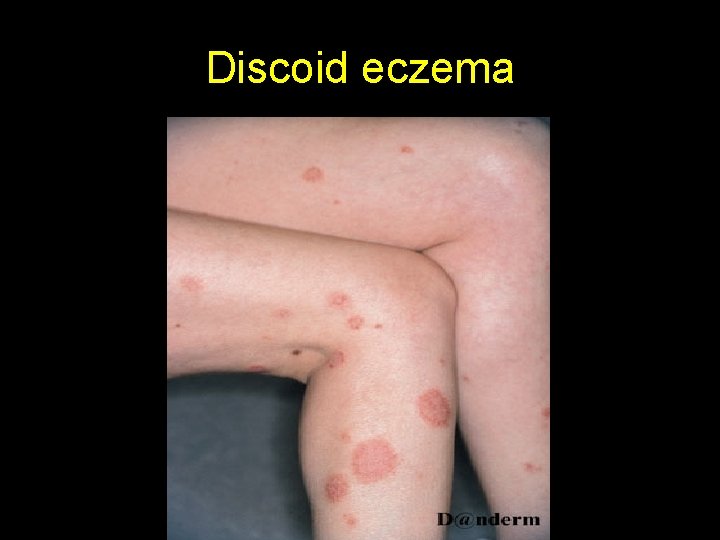
Discoid eczema


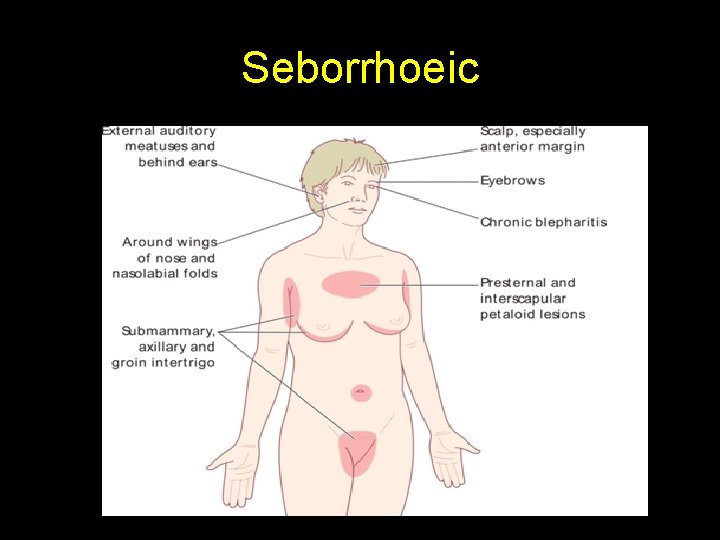
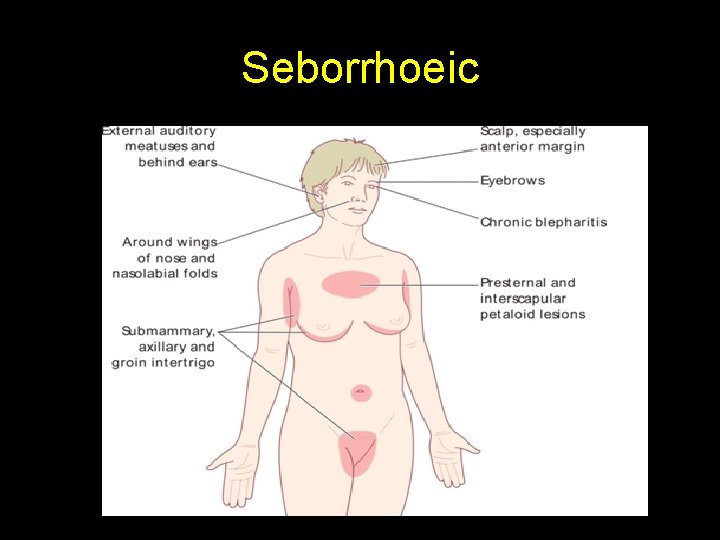
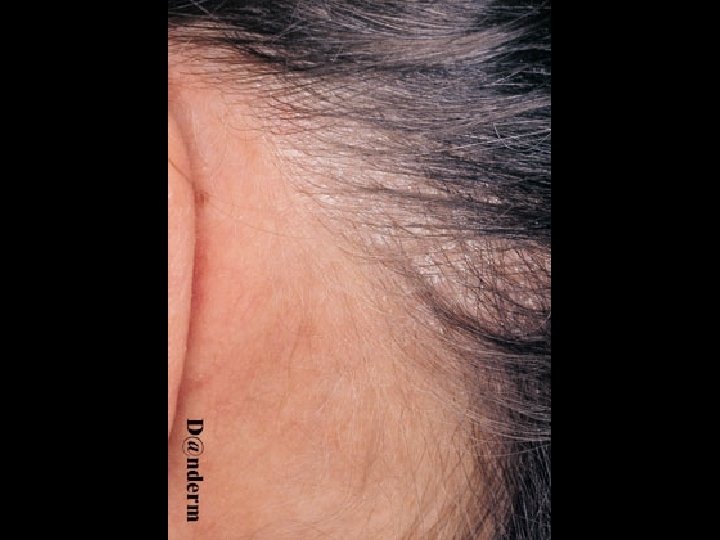
Seborrhoeic

Seborrhoeic eczema




Lichen simplex

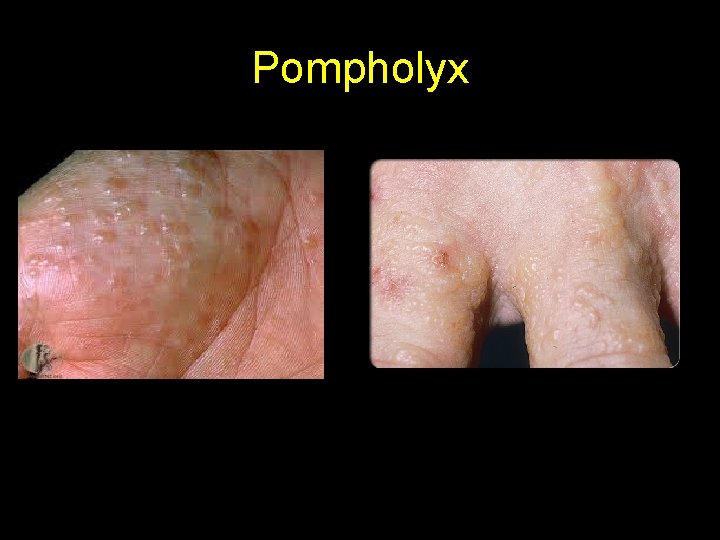
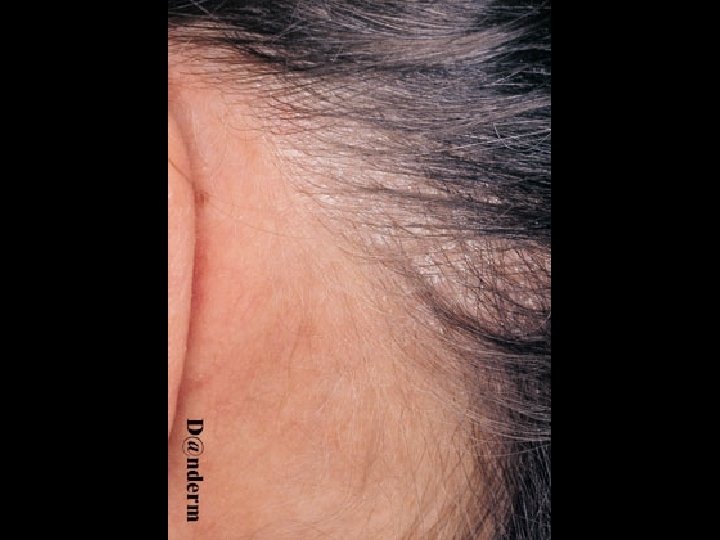
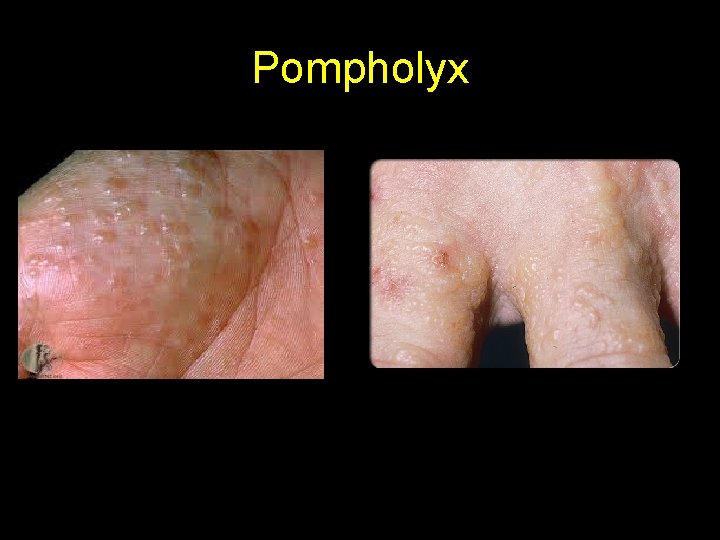
Pompholyx



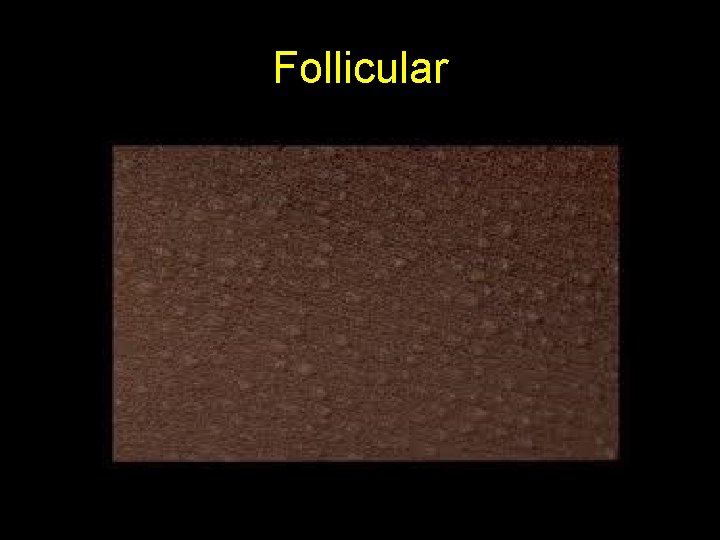
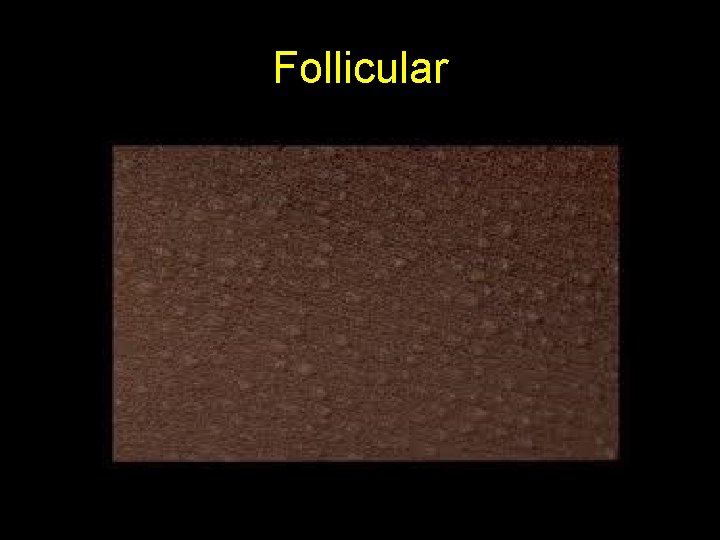
Follicular

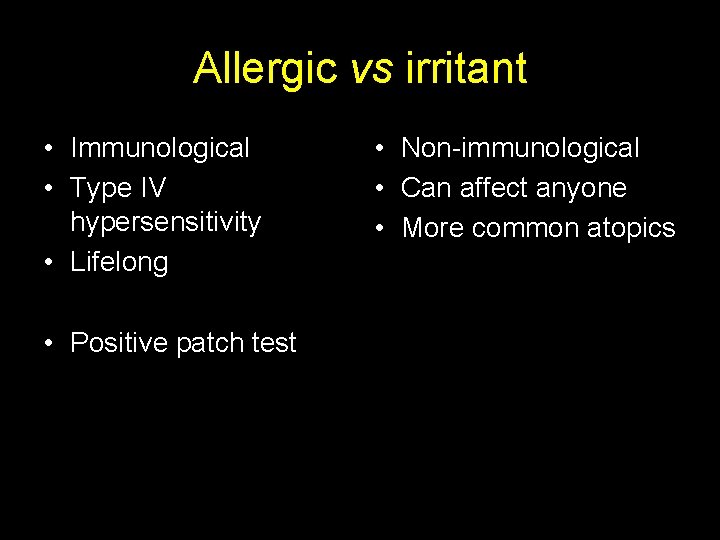
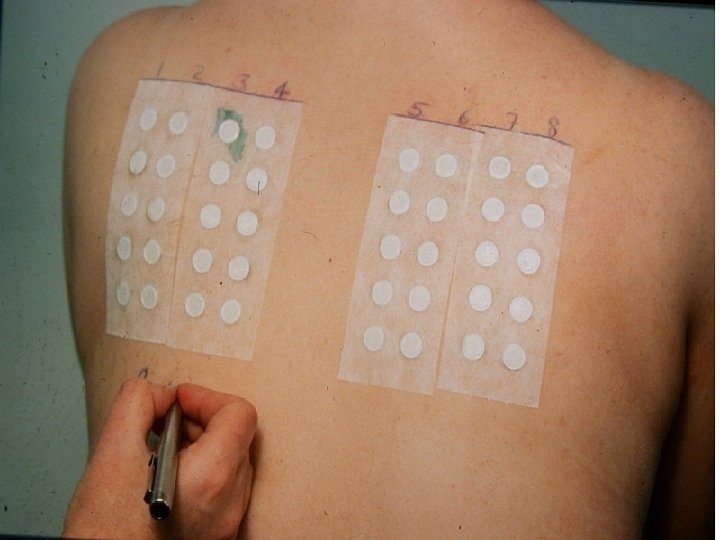
Contact dermatitis (exogenous)





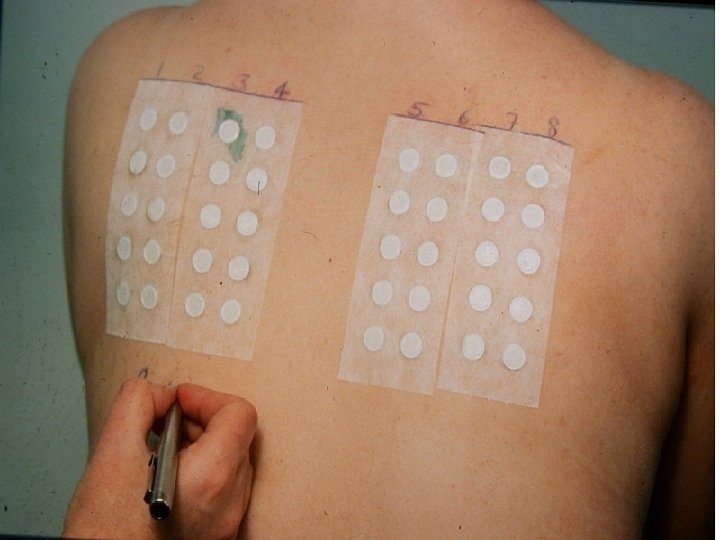
Allergic vs irritant • Immunological • Type IV hypersensitivity • Lifelong • Positive patch test • Non-immunological • Can affect anyone • More common atopics

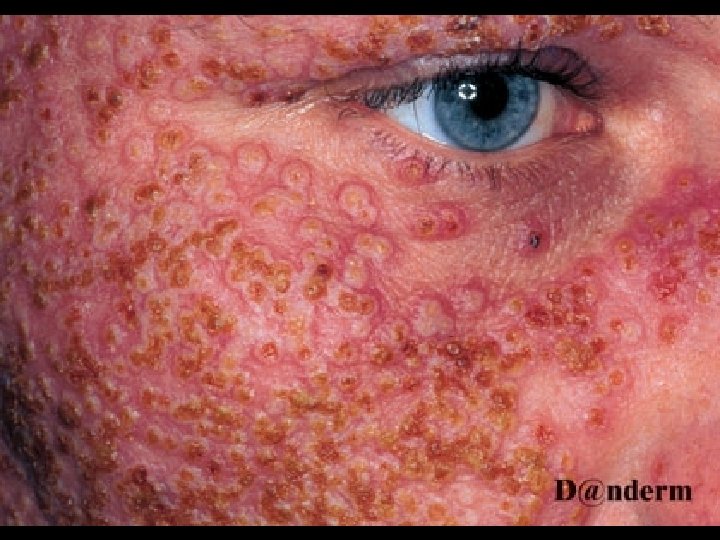
Complications of Atopic Dermatitis

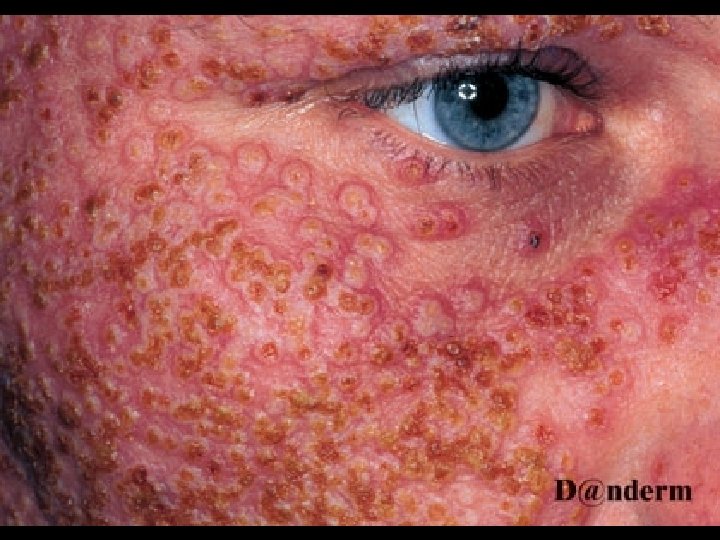





Impact of Atopic Dermatitis • Hinders social interactions • Disrupts sleep • Disturbs schooling • Failure to thrive • Affects entire family

Treatment
Aim • To get the eczema under control • Keep the eczema under control
Basic stuff • Avoid provoking factors (wool, bubble baths, soaps, perfumes) • Avoid dryness: Bath oils (Oilatum, Hydromol, Aveeno, Dermol) Soap substitutes (Aqueous cream, Dermol) Emollients (500 g in 2 weeks) • Treat any infection • Antihistamines • Reduce inflammation

Reduce inflammation • Topical steroids • Topical immunomodulators • Oral prednisolone • Oral immunosuppressives • Phototherapy


Topical steroids • Ointments better than creams • Learn 3 topical steroids I) Hydrocortisone ii) Eumovate iii) Betnovate/Elocon
Common topical steroid myths • Can’t apply to infected or broken skin • Can’t use topical steroids for more than 1 week non stop • Hydrocortisone topically can thin the skin • Cannot use potent topical steroids on the face
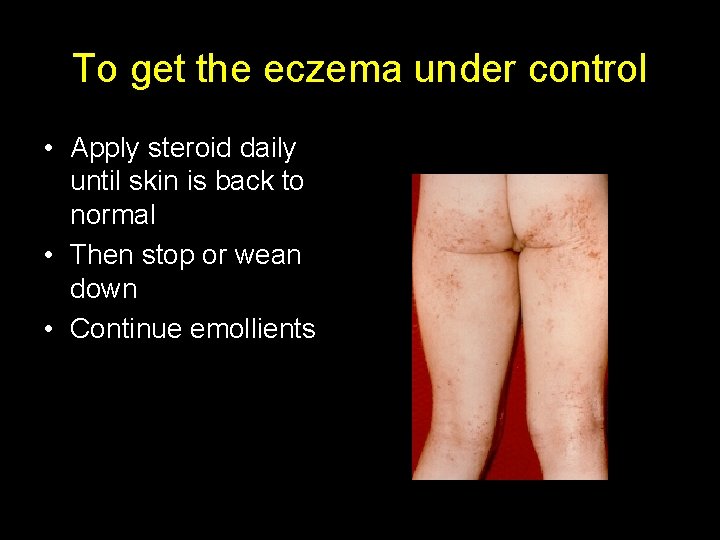
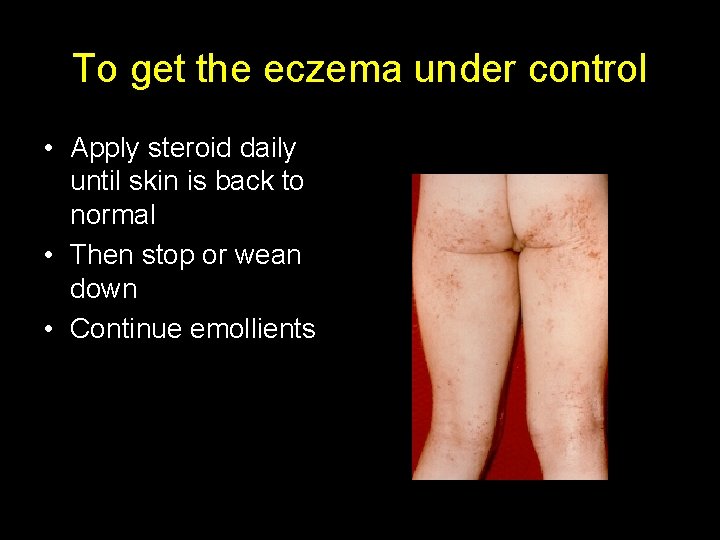
To get the eczema under control • Apply steroid daily until skin is back to normal • Then stop or wean down • Continue emollients
To keep the eczema under control • Apply topical steroid immediately the eczema flares • Consider maintenance Rx (eg Protopic) • Eumovate >30 g per month- baby- refer • Betnovate>60 g per month –child-refer
Tacrolimus ointment • Inhibits T cell activation & suppresses cytokine gene transcription • Inhibits Ig. E-induced histamine release from mast cells and basophils • Down-regulates high affinity Ig. E receptor on Langerhans cells
Important instructions to patients • Burning/stinging sensation following application which will spontaneously resolve • Avoid application after a hot bath or shower • Recommend adequate application of tacrolimus ointment, it is NOT a topical steroid • Care in sun - long term immunosuppression? ? ?
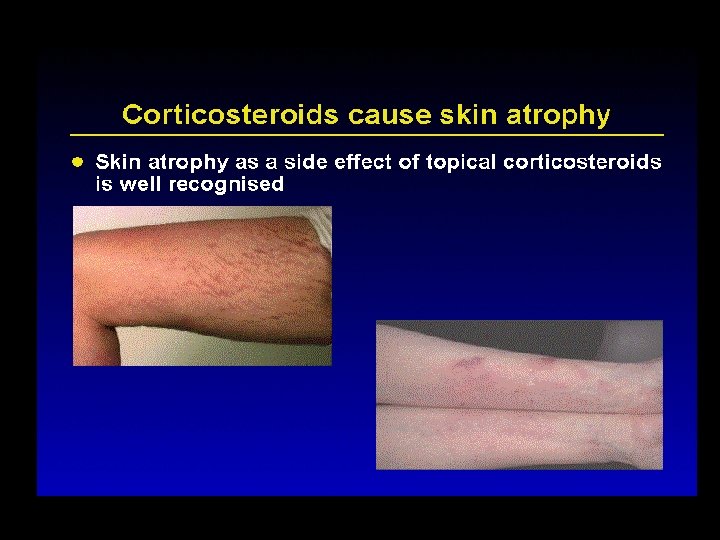
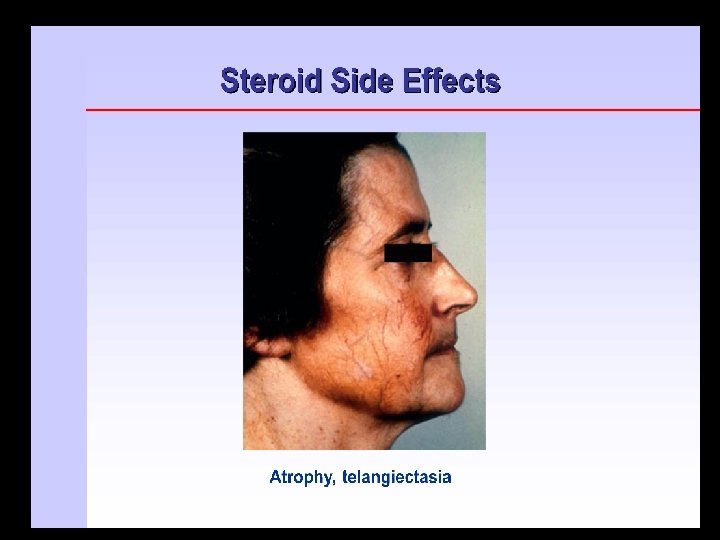
Particular indications for topical tacrolimus ointment • Peri-ocular involvement • Flexural involvement • Facial involvement • Requirement for maintenance treatment with moderately potent or potent topical steroids • Presence of topical steroid-induced cutaneous atrophy or striae • Pigmented skin
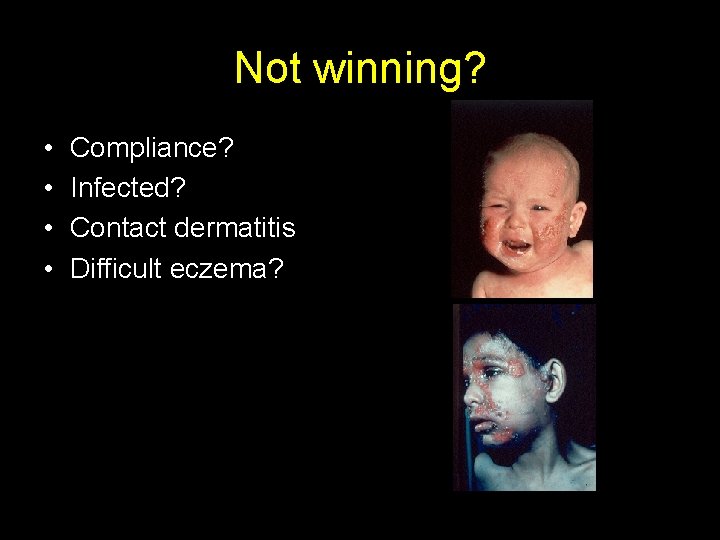
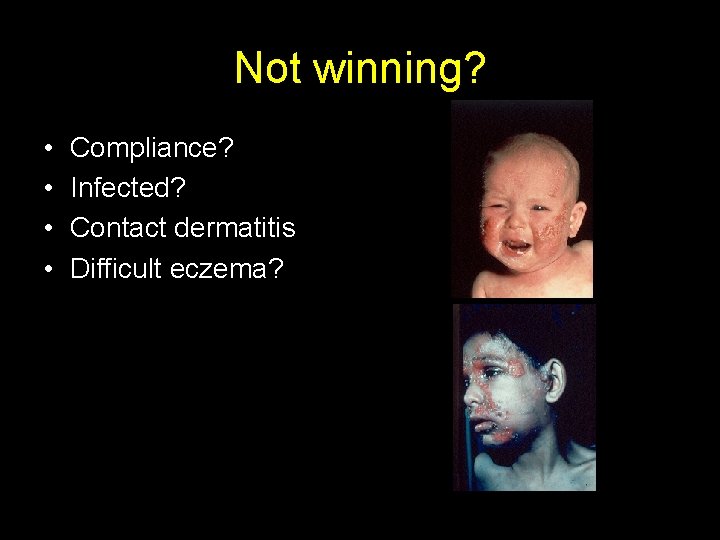
Not winning? • • Compliance? Infected? Contact dermatitis Difficult eczema?

Dressings & bandaging • Dressings • Wet wraps • Comfifast, tubifast, dermasilk garments – Over emollient / weak steroids Quality Nursing Care
Phototherapy • UVB/TLO 1 • Psoralen + UVA = PUVA – Methoxypsoralen – Topical or systemic • Whole body or regional
Systemic treatments • Short courses prednisolone • • Ciclosporin Azathioprine Methotrexate Mycophenolate mofetil
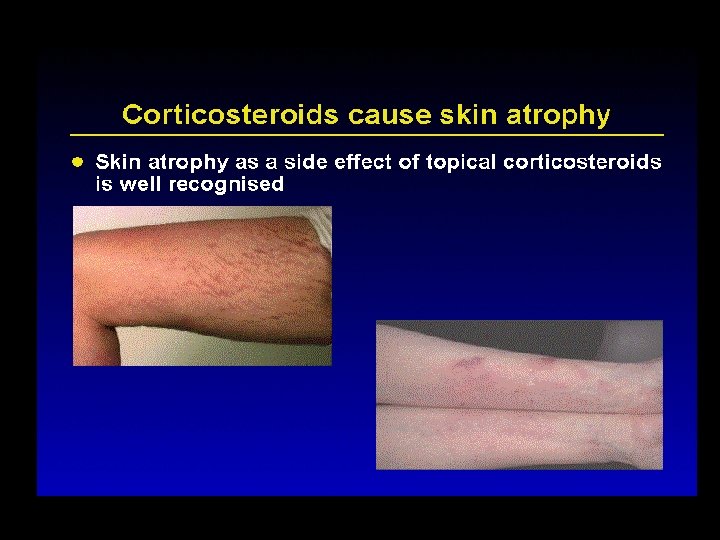
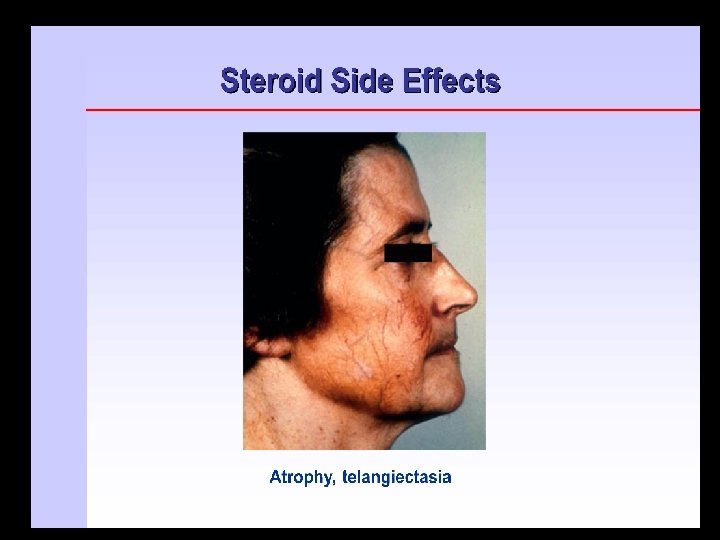
Steroid side effects - local • • Skin atrophy Telangiectasiae Acne Pigmentaion change ALL MORE MARKED IN FLEXURAL SITES!
Steroid side effects - systemic • • • suppression HPA axis cataracts growth suppression loss bone density diabetes cushings
Take home messages • Bath oils, soap substitutes and emollients - all stages/severity of eczema • Use the most appropriate strength of steroid for the severity and site • Steroids can be used for longer than a week – arrange follow-up to review and step down when skin improved • Check compliance – ask how long a tube of steroid/pot of emollient lasts • Prompt treatment of coexistent infection • Assess severity by asking about sleep/school disturbance, weight/height gain (red book), mood, family dynamics