Atelectasis acute respiratory distress syndrome pulmonary edema Morphology

- Slides: 10
Atelectasis, acute respiratory distress syndrome & pulmonary edema Morphology will be discussed in the lab Ali Al Khader, M. D. Faculty of Medicine Al-Balqa’ Applied University Email: ali. alkhader@bau. edu. jo
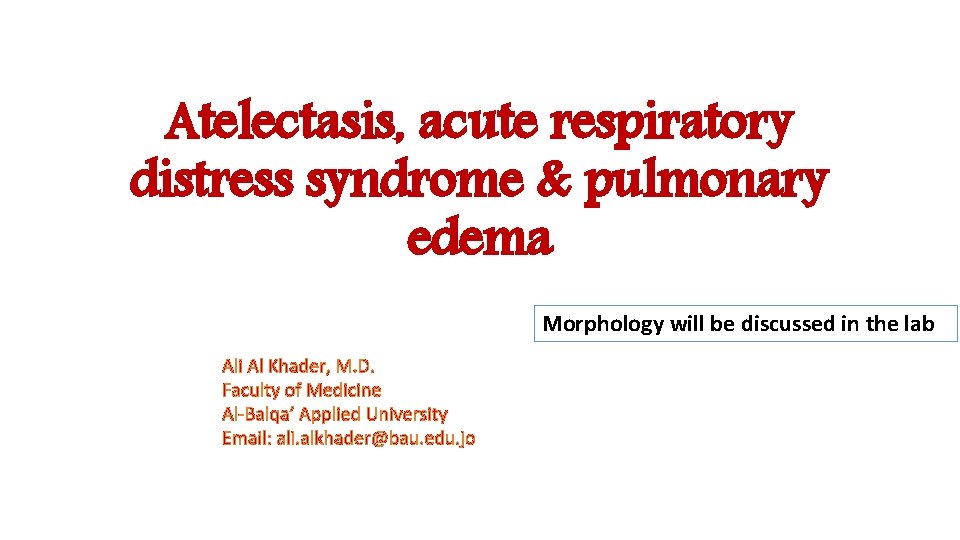
Atelectasis = Collapse = Inadequate expansion and subsequently: No lung volume • It will cause hypoxia and may be complicated by infection of the collapsed lung tissue • 3 main types: 1 -Resorption atelectasis…reversible 2 -Compression atelectasis…reversible 3 -Contraction (cicatrization) atelectasis…irreversible
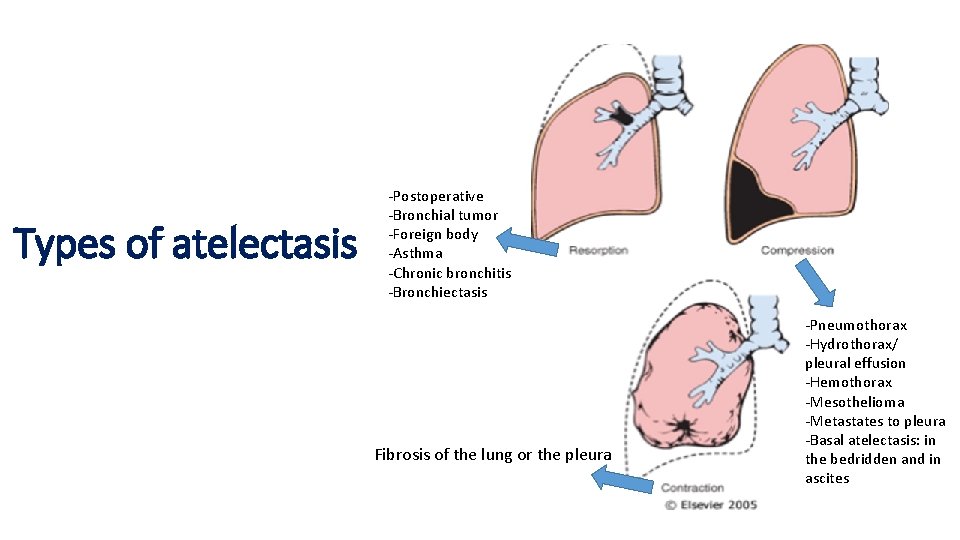
Types of atelectasis -Postoperative -Bronchial tumor -Foreign body -Asthma -Chronic bronchitis -Bronchiectasis Fibrosis of the lung or the pleura -Pneumothorax -Hydrothorax/ pleural effusion -Hemothorax -Mesothelioma -Metastates to pleura -Basal atelectasis: in the bedridden and in ascites
Acute respiratory distress syndrome (ARDS) • The severe end of acute lung injury (ALI) spectrum…but no more use of the term “Acute lung injury” • Defined as: respiratory failure occurring within 1 week of a known clinical insult with bilateral opacities on chest imaging, not fully explained by effusions, atelectasis, cardiac failure, or fluid overload • It is an extensive bilateral alveolar damage with resultant bilateral non-cardiogenic edema due to the material spilled from the blood to the alveolar spaces
ARDS, cont’d …graded based on the severity of the changes in arterial blood oxygenation …rapid onset of life-threatening respiratory insufficiency, cyanosis, and severe arterial hypoxemia that is refractory to oxygen therapy ***Diffuse alveolar damage (DAD) is the histological manifestation*** Remember: hyaline membranes
ARDS, causes • Pneumonia The most common • Sepsis • Aspiration • Trauma (including brain injury, abdominal surgery, and multiple fractures) • Pancreatitis • Transfusion reactions Respiratory distress syndrome of the newborn is different from ARDS and is caused by surfactant deficiency
ARDS, pathogenesis • Alveolar-capillary membrane damage due to endothelial and epithelial injury with loss of surfactant • Mainly by an inflammatory reaction due to pro-inflammatory mediators • A role of IL-8, IL-1 & TNF…especially neutrophil recruitment
ARDS, clinical features • In 85% of cases, it develops within 72 hours of the initial insult • The overall hospital mortality rate is 38. 5%. . . high mortality • Most patients who survive the acute insult recover normal respiratory function within 6 to 12 months …the rest develop diffuse interstitial fibrosis leading to chronic respiratory insufficiency
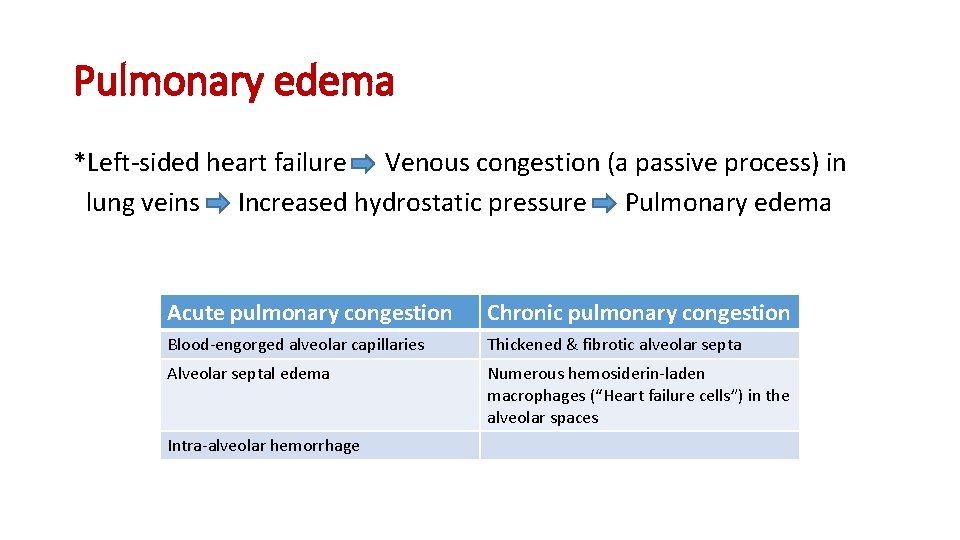
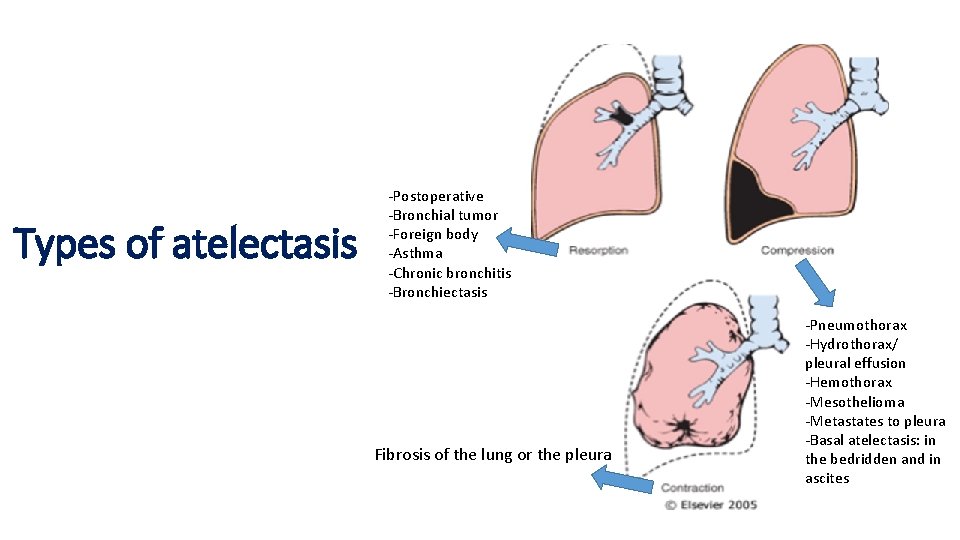
Pulmonary edema *Left-sided heart failure Venous congestion (a passive process) in lung veins Increased hydrostatic pressure Pulmonary edema Acute pulmonary congestion Chronic pulmonary congestion Blood-engorged alveolar capillaries Thickened & fibrotic alveolar septa Alveolar septal edema Numerous hemosiderin-laden macrophages (“Heart failure cells”) in the alveolar spaces Intra-alveolar hemorrhage

Thank You